Supplemental Digital Content is available in the text.
Summary:
Direct-to-implant reconstruction after mastectomy is routinely performed with excellent oncologic and aesthetic outcomes. Several different techniques for placement of the prosthesis including total and partial subpectoral coverage have been described. Prepectoral implant placement is increasingly reported as a safe method, while patient selection and techniques are areas of further work. Most prepectoral prosthesis placement techniques describe complete acellular dermal matrix (ADM) coverage of the implant, often requiring multiple or larger ADM sheets than a comparable subpectoral implant procedure, resulting in high cost per reconstructed breast. This article describes the use of a vicryl mesh pocket and ADM support in prepectoral breast reconstruction achieving predicable and safe results at a lower cost.
INTRODUCTION
Nipple- and skin-sparing mastectomy followed by direct-to-implant reconstruction is routinely performed with excellent oncologic and aesthetic outcome.1,2 Until recently, prostheses were commonly placed in either a total or partial subpectoral plane. With partial submuscular coverage of implants, additional support at the inferior pole is required.3 Several different materials including acellular dermal matrix (ADM) and vicryl mesh have been used with no reported difference in safety profile or early cosmetic results.4,5
Prepectoral implant placement is nothing new, but has been gaining traction with improvements in mastectomy flap viability.6–8 With robust soft-tissue coverage and appropriate patient selection, prepectoral implant breast reconstruction is becoming a safe alternative to total and partial submuscular reconstruction.9,10 Disadvantages of pectoralis disinsertion and stretch (animation deformity, postoperative pain) can be avoided.11 Most recent studies on prepectoral implant reconstruction use ADM for complete implant coverage, either anteriorly or completely, resulting in increased cost per reconstruction compared with submuscular procedures.12–14
This article describes the use of a vicryl mesh pocket and ADM for prepectoral breast reconstruction. This technique utilizes vicryl to control implant position during the early postoperative period, where inferolateral support is provided by the ADM. This approach provides inferolateral support for the implant without incurring additional cost for the ADM compared with more traditional submuscular approaches.
Surgical Technique
Place an implant sizer onto a 12 × 12 vicryl mesh (woven or knit) and fold into a pocket over the sizer. The pocket can be held in place by a towel clamp or snap. Suture the pocket closed with 2-0 vicryl interrupted figure of 8 stitches. Ensure maintenance of the pocket opening so the sizer can be removed and you can insert the implant later. Turn the pocket over and place an 8 × 16 cm or appropriately sized ADM sheet on the anterior surface of the vicryl pocket (opposite to the side that was sutured closed). This surface with the ADM will now be the “anterior” surface, sitting between the implant and the underside of the mastectomy skin flap. Remove the sizer and suture the ADM to anterior side of pocket. Only the superior edge of the ADM has to be sutured in place. The inferior edge (that will be at the inframammary fold) can remain free, as it will be sutured to the chest wall (see video, Supplementary Digital Content 1, which displays creation of vicryl pocket with ADM sling. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A733). Suture the vicryl pocket and inferior edge of the ADM sling to the chest wall using 2.0 vicryl on a CT02 needle. Start inferior, at the most medial end of your pocket with a horizontal mattress stitch, and continue with a running baseball or mattress stitch to the inferior lateral end of the pocket. Then proceed to the superior lateral edge of your pocket, toward the convergence of the pectoralis major, pectoralis minor, and serratus anterior. Again, start with a 2.0 vicryl horizontal mattress stitch and run a baseball stitch to the inferior border to meet your first running suture (see video, Supplementary Digital Content 2, which displays insertion of vicryl pocket with ADM sling. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A734). Open the vicryl pocket on the chest wall, place implant into Keller Funnel, and insert into pocket. Make sure the implant is oriented correctly and push it down toward the sutured blind end of the vicryl/ADM pocket.
Gather the excess vicryl over the superior pole of the implant and fold the excess vicryl material over the superior pole of the implant so it lies posterior to the implant. Ensure that the ADM material covers the inferior pole of the implant. Insert drains and close the skin. Given the particular importance of the skin closure, we utilize a de-epithelialization technique to enhance the dermal layered closure15 (see video, Supplementary Digital Content 3, which displays insertion of implant and closure. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A735).
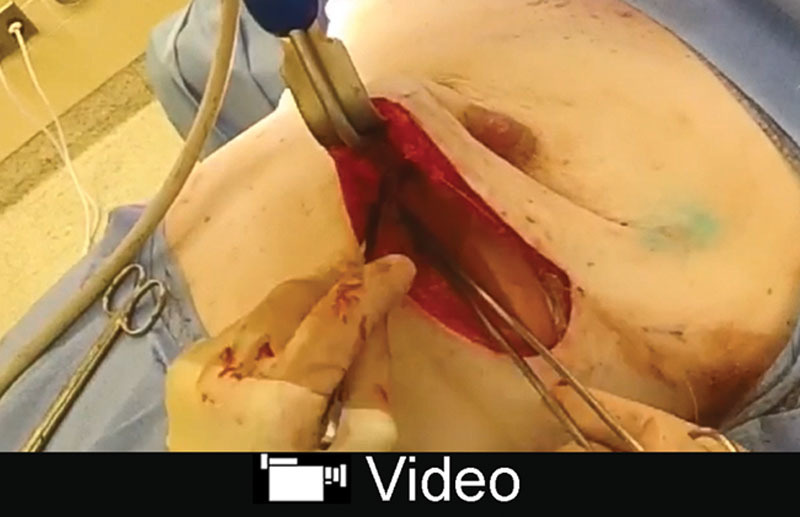
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays creation of vicryl pocket with ADM sling. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A733.
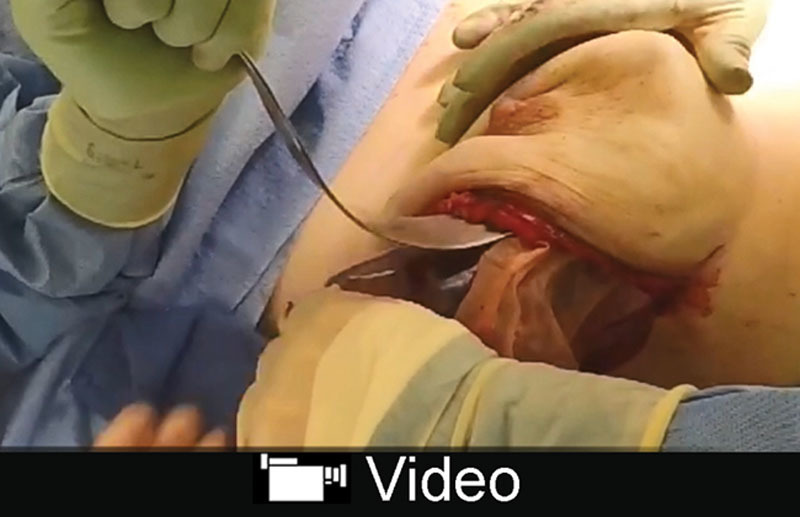
Video Graphic 2.
See video, Supplemental Digital Content 2, which displays insertion of vicryl pocket with ADM sling. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A734.
Video Graphic 3.
See video, Supplemental Digital Content 3, which displays insertion of implant and closure. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A735.
Video Graphic 4.

See video, Supplemental Digital Content 4, which displays postoperative outcome. This video is available in the “Related Video” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A736.
Outcome
Please see Supplemental Digital Content 4 for postoperative outcome. Please note that there is no animation deformity.
DISCUSSION
Prepectoral breast reconstruction has been shown to confer excellent cosmetic and functional outcomes in select patients. However, the cost per reconstructed breast is high when anterior or complete ADM coverage of the implant is used. The technique described in this article utilizes a vicryl mesh pocket and ADM sling to control the implant position, selectively applies ADM to inferolateral support where it is needed long term, and lowers the cost per reconstruction. ADM cost varies between institutions and type of ADM used. However, instead of using 2 sheets of ADM as in complete ADM coverage of prepectoral implants, we use 1 sheet. Therefore, the cost is cut in half.
This technique is designed for direct-to-implant reconstruction in the prepectoral plane. For direct-to-implant breast reconstruction, a robust skin flap is critical, even more important in prepectoral breast reconstruction. The importance of the skin flap has been emphasized in other case series of prepectoral breast reconstruction and in our own series.8,11 In patients with very challenged skin flaps, direct-to-implant or prepectoral breast reconstruction would not be recommended, in which case we would recommend placement of a deflated or minimally filled tissue expander either total or partially under muscle with ADM coverage.
One can adopt this technique for tissue expander placement in patients with robust skin flaps, but the prosthesis cannot be squeezed into the sleeve as we show here.
Modifications of this technique could include ADM inset with the sizer in place, a variation in technique the senior author used to prefer. However, over the decade, as the senior author gained experience in direct-to-implant placement, it became less or unnecessary to keep the sizer in place during inset of the vicryl/ADM sleeve or ADM in general. Technically, it became very expeditious to suture the ADM to the pocket when the sizer is removed, especially in patients with smaller breasts or when the inframammary incision was short. The ADM fits well contoured along the inframammary fold, and we have not had problems with contouring. However, it is certainly possible to suture the ADM in place with the sizer in the pocket, which may allow for improved visualization of contour before insertion, or test the contour after inset with the sizer. This is left to preferences and experience of the surgeon.
It is further possible to perform this technique with vicryl mesh only. However, inferolateral ADM provides support to the implant and prohibits migration downward or laterally until a capsule is formed. ADM further helps prevent implant rippling in patients at risk (limited preoperative soft-tissue envelopes, thin mastectomy flaps, and small-volume implant reconstructions).11
This article is intended to be a description of surgical technique. We previously published our clinical outcomes experience in PRS Go.11 In this series, 23 breasts underwent prepectoral breast reconstruction over a period of 18 months. None of the 13 patients had breast animation deformity postoperatively. There was 1 early hematoma requiring operative intervention. One morbidly obese patient undergoing chemotherapy using a nearby chest port ultimately experienced infection requiring implant removal. Three patients developed small seromas that resolved uneventfully. One patient demonstrated implant rippling postoperatively but did not seek revision. There were no instances of implant extrusion or skin flap necrosis requiring operative intervention. No instances of implant malposition developed, as the vicryl mesh is folded neatly posterior to the implant. It is contained in the vicryl/ADM pocket and should not move.
There has been no bunching of excess vicryl mesh, as this is folded neatly posterior to the implant, and no excess material remains anterior. The excess posterior material is not noticeable on the operating room table nor postoperatively. The vicryl hydrolyzes over 2 months and is not palpable long term.
Long-term follow-up is needed to understand the risk of capsular contracture in prepectoral breast reconstruction and to determine the role of prepectoral breast reconstruction in patients who require postmastectomy radiation therapy.
CONCLUSIONS
The technique described in this article utilizes a vicryl mesh pocket and ADM to control the implant position. It selectively applies ADM to provide inferolateral support where it is needed long term, and lowers the cost per reconstruction. Short-term results are promising. Long-term data are currently being acquired to confirm initial results.
Supplementary Material
Footnotes
Published online 9 April 2018.
Disclosure: Dr. Gfrerer has no conflict of interest to disclose. Dr. Liao has consultancy agreements with manufacturers of Alloderm (Allergan, Inc) and FlexHD (Musculoskeletal Transplant Foundation). The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg. 2014;133:496–506.. [DOI] [PubMed] [Google Scholar]
- 2.Smith BL, Tang R, Rai U, et al. Oncologic safety of nipple-sparing mastectomy in women with breast cancer. J Am Coll Surg. 2017;225:361–365.. [DOI] [PubMed] [Google Scholar]
- 3.Spear SL, Sher SR, Al-Attar A. Focus on technique: supporting the soft-tissue envelope in breast reconstruction. Plast Reconstr Surg. 2012;130:89S–94S.. [DOI] [PubMed] [Google Scholar]
- 4.Tessler O, Reish RG, Maman DY, et al. Beyond biologics: absorbable mesh as a low-cost, low-complication sling for implant-based breast reconstruction. Plast Reconstr Surg. 2014;133:90e–99e.. doi: 10.1097/01.prs.0000437253.55457.63. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez-Unda N, Leiva S, Cheng HT, et al. Low incidence of complications using polyglactin 910 (vicryl) mesh in breast reconstruction: a systematic review. J Plast Reconstr Aesthet Surg. 2015;68:1543–1549.. [DOI] [PubMed] [Google Scholar]
- 6.Scarfì A, Ordemann K, Hüter J. Reconstruction of an ablated breast. Eur J Gynaecol Oncol. 1986;7:93–96.. [PubMed] [Google Scholar]
- 7.Gruber RP, Kahn RA, Lash H, et al. Breast reconstruction following mastectomy: a comparison of submuscular and subcutaneous techniques. Plast Reconstr Surg. 1981;67:312–317.. [DOI] [PubMed] [Google Scholar]
- 8.Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral implant-based breast reconstruction: rationale, indications, and preliminary results. Plast Reconstr Surg. 2017;139:287–294.. [DOI] [PubMed] [Google Scholar]
- 9.Bernini M, Calabrese C, Cecconi L, et al. Subcutaneous direct-to-implant breast reconstruction: surgical, functional, and aesthetic results after long-term follow-up. Plast Reconstr Surg Glob Open. 2015;3:e574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sbitany H, Piper M, Lentz R. Prepectoral breast reconstruction: a safe alternative to submuscular prosthetic reconstruction following nipple sparing mastectomy. Plast Reconstr Surg. 2017;140(3):432–443..Sep; [DOI] [PubMed] [Google Scholar]
- 11.Kobraei EM, Cauley R, Gadd M, et al. Avoiding breast animation deformity with pectoralis-sparing subcutaneous direct-to-implant breast reconstruction. Plast Reconstr Surg Glob Open. 2016;4:e708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nadeem R. Prepectoral implant-based breast reconstruction; complete acellular dermal matrix wrap or anterior circumferential cover. Breast J. 2018 Mar;24(2):223–224.. [DOI] [PubMed] [Google Scholar]
- 13.Vidya R. Prepectoral breast reconstruction or muscle-sparing technique with the Braxon porcine acellular dermal matrix. Plast Reconstr Surg Glob Open. 2017;5:e1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jansen LA, Macadam SA. The use of AlloDerm in postmastectomy alloplastic breast reconstruction: part II. A cost analysis. Plast Reconstr Surg. 2011;127:2245–2254.. [DOI] [PubMed] [Google Scholar]
- 15.Cauley RP, Liao EC. Deepithelialization and extended dermal apposition: a technique for closure of high-risk incisions in breast reconstruction. Plast Reconstr Surg Glob Open. 2016;4:e802. [DOI] [PMC free article] [PubMed] [Google Scholar]


