Abstract
A family-based behavioral nutrition intervention grounded in Social Cognitive and Self-Determination Theories showed an increased intake of whole plant foods. This study examined 1) whether the intervention changed parent diet-related attitudes/beliefs, 2) whether these attitudes/beliefs were associated with youth diet quality, and 3) the moderating roles of youth age and parent nutritional knowledge. Youth with type 1 diabetes and their parents (n = 136, mean ± SD youth age = 12.6 ± 2.8 years) participated in an 18-month trial targeting intake of whole plant foods. Parents reported attitudes/beliefs (self-efficacy, outcome expectations, perceived barriers, autonomous and controlled motivation) for providing healthy food to their families, and type 1 diabetes-specific nutrition knowledge at 6, 12, and 18 months. Whole Plant Food Density (WPFD; cup or ounce equivalents per 1000 kcal of whole grains, fruit, vegetables, legumes, nuts and seeds) was calculated from 3-day youth food records. Linear mixed models estimated the intervention effect on parent attitudes/beliefs, associations of parent attitudes/beliefs with youth WPFD and the moderating roles of parent nutrition knowledge and youth age. There was no effect of the intervention on parent attitudes/beliefs. Across groups, higher parent self-efficacy and autonomous motivation were positively associated with youth WPF. Parent perceived barriers and negative outcome expectations were inversely associated with youth WPFD, especially when parents had higher nutrition knowledge. Youth age did not modify any associations. Parent diet-related attitudes/beliefs were associated with youth diet quality, highlighting the importance of parent psychosocial factors across this age range. Despite a positive effect on youth diet, the intervention did not affect parent attitudes/beliefs, suggesting it worked through a different mechanism.
Keywords: diet, type 1 diabetes, nutrition knowledge, self-efficacy, outcome expectations, perceived barriers, autonomous motivation, adolescents
Introduction
Eating healthfully is critical for promoting optimal long-term health among youth with type 1 diabetes (T1D) (Smart, Aslander-van Vliet, & Waldron, 2009). Medical nutrition therapy includes education on healthful eating, carbohydrate estimation, and carbohydrate intake from low-fat milk and whole plant foods (fruits, vegetables, whole grains, and legumes) (ADA, 2008; Bantle et al., 2008). Despite this, plant food intake among youth with T1D is below recommendations while intake from saturated fats, sweets and refined grains is high, increasing risk of adverse health outcomes (Mehta, Volkening, Quinn, & Laffel, 2014; Nansel, Haynie, Lipsky, Laffel, & Mehta, 2012; Patton, 2011; Rovner & Nansel, 2009; Rovner et al., 2012). This presents a need to identify factors associated with improved diet quality in this population. Previous research indicates that parents influence their children’s diets by modelling dietary habits and regulating access to food in the home (Videon & Manning, 2003). Additionally, while diet-related attitudes and beliefs delineated by Social Cognitive Theory (SCT) and Self-Determination Theory (SDT) impact one’s own diet (e.g., Anderson, Winett, & Wojcik, 2007; Teixeira, Patrick, & Mata, 2011), less is known about how these parent psychosocial factors impact their children’s diets.
SCT posits that people learn and acquire behaviors by observing others and that this process relies on self-efficacy (the belief that one has the ability to engage in the target behavior), outcome expectations (perceived positive and negative consequences of the behavior) and perceived barriers (factors inhibiting the behavior; Bandura, 1977; Bandura, 2001). Theoretically, the target behavior results from high self-efficacy and positive outcome expectations and low perceived barriers and negative outcome expectations (Bandura, 1977, 2001). These attitudes are associated with one’s own healthful eating in adults, college students, and children (Anderson-Bill, Winett, & Wojcik, 2011; Anderson et al., 2007; Bruening, Kubik, Kenyon, Davey, & Story, 2010; Resnicow et al., 1997; Strachan & Brawley, 2009), and parent self-efficacy is associated with young children’s healthful eating (Campbell, Hesketh, Silverii, & Abbott, 2010). However, no research has examined the influence of parent psychosocial factors on diet quality of older children and adolescents, and their importance in families of youth with T1D is unclear.
According to SDT, behaviors are influenced by the degree to which motivation is internalized. Behaviors such as healthy dietary intake are more likely when they are motivated by one’s own volition (“autonomous motivation”) (Teixeira et al., 2011), as opposed to when motivated by external sources such as to garner approval or to avoid feeling guilty (“controlled motivation”) (E L Deci & Ryan, 2008). Autonomous, compared to controlled, motivation is associated with reducing fat intake and increasing fruit and vegetable consumption in adults in the general population (Fuemmeler et al., 2006; Teixeira et al., 2011). Additionally, among adolescents with T1D, autonomous motivation is associated with better diabetes self-care (e.g., adherence to recommended caloric intake, adding high-fibre foods to meals, limiting sweets and deserts; Austin, Senécal, Guay, & Nouwen, 2011). Alternatively, controlled motivation is associated with less healthful eating and more disordered eating behaviors (Eisenberg, Lipsky, Dempster, Liu, & Nansel, In Press; Leong, Madden, Gray, & Horwath, 2012). Given the influence of parent modelling and home food access on youth diet (Larsen et al., 2015), SDT would posit that stronger autonomous motivation for serving healthful foods would be associated with better youth diet quality.
Additionally, the interplay of nutrition knowledge with parent psychosocial factors is not known. For families of youth with T1D, relevant aspects of nutrition knowledge include healthful eating, nutrition label reading, carbohydrate counting, and blood glucose response to food (Rovner et al., 2012). Nutrition knowledge is a necessary but not sufficient precursor for dietary behavior change (Axelson, Federline, & Brinberg, 1985; Hoelscher, Evans, Parcel, & Kelder, 2002). This suggests that the effect of parent psychosocial factors on youth diet quality would be contingent on parents’ level of nutrition knowledge, whereby positive parental attitudes and beliefs about providing healthy foods to their families would be associated with better youth diet quality, only given sufficient nutrition knowledge for effectively carrying out these intentions.
An 18-month efficacy trial of a family-based behavioral nutrition intervention for youth with type 1 diabetes grounded in SDT and SCT showed increased intake of whole plant foods compared to the control group (Nansel et al, 2015). The aims of this study were to examine the intervention effect on parent SDT and SCT-based attitudes and beliefs and the overall relationship of parent attitudes and beliefs with youth diet quality. The study hypotheses were:
Parents in the intervention group will report higher self-efficacy, positive outcome expectations, and autonomous motivation and lower negative outcome expectations, perceived barriers, and controlled motivation than parents in the control group.
Higher parent self-efficacy, positive outcome expectations, and autonomous motivation and lower negative outcome expectations, perceived barriers, and controlled motivation will be associated with better youth diet quality across intervention groups..
Associations of parent attitudes and beliefs with youth diet quality will be stronger when parent nutrition knowledge is high (versus low).
Methods
Participants
Single parent-youth dyads (n = 136) participated in a randomized controlled trial of a family-based behavioral nutrition intervention, described previously (Nansel et al., 2015). Eligibility criteria for youth included age 8.0-16.9 years, diagnosis of T1D ≥ 1 year, daily insulin dose ≥ 0.5 units per kilogram, insulin regimen of ≥ 3 injections daily or use of insulin pump, at least one clinic visit in the past year, and ability to communicate in English. Exclusion criteria included daily use of premixed insulin, transition to insulin pump in the last three months, real-time continuous glucose monitoring use in the last three months, participation in another intervention study in the last six months, and presence of gastrointestinal disease such as celiac disease, multiple food allergies, use of medications that interfere significantly with diabetes management or glucose metabolism, or significant mental illness. It was also required that participants’ most recent hemoglobin AIC be ≥ 6.5% and ≤ 10.0% in order to avoid asking those already struggling to manage the essential diabetes tasks required for moderate glycemic control to extend added effort to improve healthful eating.
Design
The study employed a two-group design with one control group and one group participating in a behavioral nutrition intervention grounded in SCT (Bandura, 1977) and SDT (E.L. Deci & Ryan, 2000). Randomization was stratified by age (<13 years and ≥13 years), A1C (<8.5% and ≥8.5%), and insulin regimen (injection and insulin pump), with a permuted block randomization scheme. Randomization was conducted by the data coordinating centre; research team members with direct involvement in recruitment and enrolment did not have access to randomization schedules.
Procedures
The study was conducted from August 2010 through May 2013 at an outpatient, free-standing, multidisciplinary tertiary diabetes centre in Boston, Massachusetts. At baseline, six, twelve, and 18 months, parents completed all self-report measures. Families completed three-day youth diet records at each of these time-points as well as 3 and 9 months (which were not used in these analyses). All study materials and procedures were approved by the institutional review boards of the participating institutions. All youth provided assent; parents and youth turning 18 during the trial provided written informed consent.
Intervention
The intervention comprised nine in-person sessions led by trained research assistants that included behavioral techniques and educational content to promote increased intake of whole plant foods. It covered a broad scope of behaviors to facilitate skill building and engagement with educational information (Nansel et al., 2015). The intervention focus for parents was on improving the family food environment, including availability of healthful foods in the home at at meals, increasing family meals, and food choices outside the home. Participants in the control condition received an equal number of contacts with research staff (such as case management within the diabetes health care system) and completed identical assessments. Each session involved one single parent-youth dyad.
Sessions were tailored specifically to target parent outcome and efficacy expectations as well as increase autonomous motivation for consuming whole plant foods. To address outcome and efficacy expectations, families identified strategies to improve diet quality and personal motivators for healthful eating. Sessions also included hands-on activities, tailored family-based goal setting, monitoring and reinforcement for success, and practice through role plays regarding difficult social settings (Bandura, 2004; Brown et al., 2012; Michie, Abraham, Whittington, McAteer, & Gupta, 2009; Michie et al., 2011). Motivational interviewing (e.g., Knight, McGowan, Dickens, & Bundy, 2006; Taylor et al., 2010) was used to enhance autonomous motivation by allowing participants to examine and build their own reasons for change. Motivational interviewing is a directive, client-centered counselling style for eliciting behavior change that helps participants explore and resolve ambivalence. Although the intervention was grounded in SCT and SDT, none of these parent psychosocial variables have been evaluated in the context of this intervention yet.
Measures
Self-Efficacy for Healthy Eating
This 11-item measure assesses parents’ perceived ability to provide healthful foods for the family (Nansel et al., 2013). Responses are on a 5-point scale from “strongly disagree” to “strongly agree”; internal consistency is high (α=.91). An example item is, “I am sure I can serve whole grain foods that my family will like.”
Outcome Expectations for Healthy Eating
This 14-item measure assesses parents’ perceived positive and negative consequences of providing healthy foods to their family (Nansel et al., 2013). Responses are on a 5-point scale from “strongly disagree” to “strongly agree.” The measure includes subscales for positive and negative outcome expectations. Both the positive (α=.85) and negative (α=.85) subscales showed high internal consistency. An example of a positive outcome expectation is, “It would help my family manage their weight.” An example of a negative outcome expectation is, “My family would not enjoy the food.”
Barriers to Healthy Eating
This 7-item measure assesses perceived obstacles (i.e., environmental or skill impediments) that parents encounter when providing healthy foods to their families (Nansel et al., 2013). Responses are on a 5-point scale from “strongly disagree” to “strongly agree”; internal consistency is good (α=.81). A sample question is “My family is so busy that it’s hard to eat healthy.”
Treatment Self-Regulation questionnaire (TSRQ)
This 15-item measure assesses autonomous motivation, controlled motivation, and amotivation for eating healthfully (Williams, Grow, Freedman, Ryan, & Deci, 1996). For the current study, the measure was modified to query motivation for providing healthful diet to the family. Responses were on a 7-point scale ranging from “not at all true” to “very true,” with higher scores indicating greater autonomous motivation, controlled motivation, or amotivation. Both the autonomous (α=.85) and controlled (α=.85) subscales demonstrated high internal consistency, but the three items assessing amotivation did not (α = .37) and so were not used in the current analysis. Previous research showed that two items from the controlled motivation subscale loaded moderately on both controlled and autonomous motivation (Quick, Nansel, Lipsky, Laffel, & Mehta, 2015); these items were also removed from analysis. The final measure included 10 items (six autonomous motivation items and four controlled motivation items). All questions began with “The reason I would provide healthy food for the family is…” an example of an autonomous motivation question is, “Because I want to take responsibility for my family’s health.” An example of a controlled motivation question is, “Because others would be upset with me if I did not.”
Parent Nutrition Knowledge
This 23-item questionnaire covers content areas including healthful eating, carbohydrate counting, blood glucose response to food, and nutrition label reading (Rovner et al., 2012). The measure has shown acceptable internal consistency (KR-20 = 0.59) and association with dietary intake. Higher scores reflect greater nutrition knowledge (score range is 0-100%). An example question is, “which of the following are benefits of eating fruits and vegetables?” with response options of “good source of fibre; low in fat; good source of vitamins and minerals; and all of these.”
Dietary intake
Families completed three-day youth food records together following instruction on accurately measuring and reporting food and beverage intake. Scales, measuring cups, and spoons were provided to all participants to facilitate portion-size estimation. Participants were reminded to include all necessary details for each food item including brand names. Research staff reviewed the records and contacted participants if needed to solicit any missing necessary information. Records were analysed using Nutrition Data System for Research (Nutrition Coordinating Centre, University of Minnesota, and Minneapolis, MN, USA). Diet quality was measured by calculating Whole Plant Food Density (WPFD), the sum number of cup or ounce equivalents per 1000 kcal of whole grains, whole fruit, vegetables, legumes, nuts, and seeds (Lipsky, Cheon, Nansel, & Albert, 2012). This measure was used based on its consistency with food groups targeted by the intervention and specified in the psychosocial measures.
Clinical and Demographic Data
Youth biomedical data were collected through medical record review. Youth age at baseline was dichotomized as pre-adolescent (12 years of age or younger) or adolescent (older than 12 years) (CDC, 2015; Valkenburg, 2011). Parents reported education level, household income and number of people in the home. The poverty income ratio (PIR) was calculated as reported household income divided by the 2008 US census poverty threshold for household size and composition adjusted for inflation (Poverty Thresholds 2008, 2010). Higher PIR indicates greater income relative to the poverty threshold.
Analysis
The intervention effect on each of the parent psychosocial variables was tested using linear mixed effects models. A series of models estimated the association of each time-varying psychosocial variable with time-varying youth WPFD, adjusting for treatment group, youth age, sex, parent education, and PIR, since these are all theoretically associated with youth diet quality. Multiplicative interaction terms were used to test whether parent nutrition knowledge moderated the associations of parent psychosocial variables with youth diet quality. Interpretation of any significant interactions with parent psychosocial factors was based on simple slopes analyses using a median split on nutrition knowledge. Because the sample spanned a large developmental age range, posthoc linear mixed effects models tested whether associations of parent psychosocial variables with youth WPFD were moderated by youth age.
Results
Of those invited to participate, 24% provided informed consent and 22% completed baseline assessment. Subject retention through study completion was 92% and all of the withdrawals were from the intervention group (Figure 1). Baseline characteristics were well-balanced between groups for parents and youth (Table 1). There was no intervention effect on any of the parent psychosocial variables (p-values>.10). Bivariate correlations between variables are in Table 2.
Figure 1.
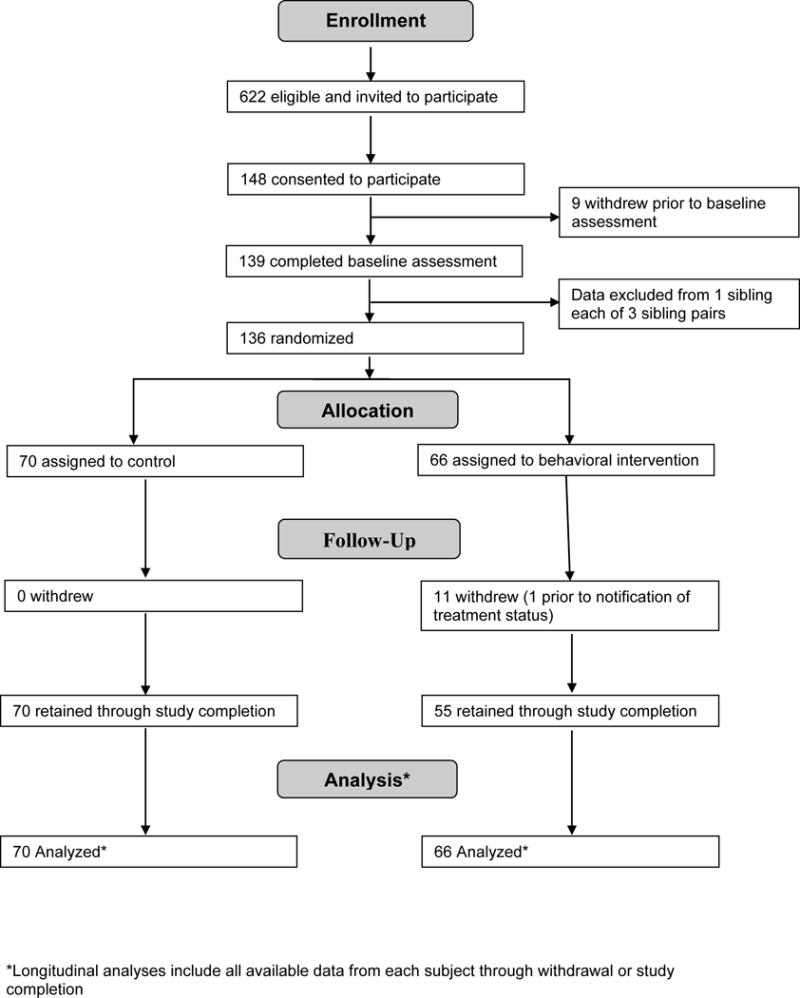
Participant Flow through a Randomized Clinical Trial of a Behavioral Nutrition Intervention for Adolescents and Pre-adolescents with Type 1 Diabetes.
Table 1.
Baseline sample characteristics of youth with type 1 diabetes participating in a behavioral nutrition intervention efficacy trial
| All Participants (N=136) | Treatment (N=66) | Control (N=70) | p-value* | |
|---|---|---|---|---|
| Youth Sample Characteristics | ||||
| Demographics | Mean ± SD or N (%) | Mean ± SD or N (%) | Mean ± SD or N (%) | |
| Age (years) | 12.8±2.6 | 12.6±2.7 | 13.0±2.5 | 0.27 |
| Sex | ||||
| Male | 66 (48.5) | 35 (53.0) | 31 (44.3) | 0.31 |
| Female | 70 (51.5) | 31 (47.0) | 39 (55.7) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 123 (90.4) | 58 (87.9) | 65 (92.9) | 0.17 |
| Hispanic | 7 (5.2) | 6 (9.1) | 1 (1.4) | |
| Black | 5 (3.7) | 2 (3.0) | 3 (4.3) | |
| Other | 1 (0.7) | 0 (0.0) | 1 (1.4) | |
| Duration of diabetes (years) | 6.0±3.1 | 5.6±2.5 | 6.3±3.6 | 0.15 |
| BMI z-score | 0.68±0.82 | 0.65±0.81 | 0.71±0.84 | 0.65 |
| Whole plant food density | 1.89±0.09 | 1.87±0.13 | 1.91±0.13 | 0.84 |
| Parent Sample Characteristics | ||||
| Relationship to child | ||||
| Mother | 115 (84.6) | 54 (81.8) | 61 (87.1) | 0.30 |
| Father | 17 (12.5) | 10 (15.2) | 7 (10.0) | |
| Stepmother | 1(0.7) | 1 (1.5) | 0 (0) | |
| Stepfather | 1(0.7) | 1 (1.5) | 0 (0) | |
| Other | 2 (1.5) | 0 (0) | 2(2.9) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 123 (90.4) | 58 (87.9) | 65 (92.9) | 0.17 |
| Hispanic | 7 (5.2) | 6 (9.1) | 1 (1.4) | |
| Black | 5 (3.7) | 2 (3.0) | 3 (4.3) | |
| Other | 1 (0.7) | 0 (0.0) | 1 (1.4) | |
| Highest parent education level | ||||
| High school or equivalent | 8 (5.9) | 4 (6.1) | 4 (5.7) | 0.48 |
| Junior college, technical or some college | 27 (19.9) | 11 (16.7) | 16 (22.9) | |
| College degree | 46 (33.8) | 20 (30.3) | 26 (37.1) | |
| Graduate education | 55 (40.4) | 31 (47.0) | 24 (34.3) | |
| Family poverty income ratio† | 5.2±3.1 | 5.5±3.2 | 4.9±3.0 | 0.23 |
| Parent BMI | 28.89±7.37 | 28.31±8.07 | 29.42±6.68 | 0.39 |
| Whole plant food density | 1.89±0.09 | 1.87±0.13 | 1.91±0.13 | 0.84 |
| Self-efficacy | 3.98±0.57 | 4.03±0.60 | 3.94±0.55 | 0.36 |
| Healthy eating barriers | 1.95±0.70 | 1.87±0.67 | 2.03±0.72 | 0.19 |
| Positive outcome expectations | 4.21±0.51 | 4.23±0.56 | 4.20±0.47 | 0.69 |
| Negative outcome expectations | 2.31±0.72 | 2.22±0.73 | 2.41±0.70 | 0.12 |
| Autonomous motivation | 6.00±0.94 | 6.05±0.84 | 5.97±1.03 | 0.62 |
| Controlled motivation | 2.89±1.03 | 2.71±0.89 | 3.06±1.12 | 0.05 |
| Nutrition knowledge | 79.64±9.54 | 79.75±9.30 | 79.54±9.83 | 0.90 |
Table 2.
Bivariate Correlations between Study Variables by Treatment Group
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Treatment group (N = 66) | |||||||||
| 1. Age | ____ | ||||||||
| 2. WPFD | .07 | ____ | |||||||
| 3. Healthy Eating Barriers | −.02 | −.10 | _____ | ||||||
| 4. Self-efficacy | −.08 | .07 | −.61*** | ____ | |||||
| 5. Positive Outcome Expectations | −.07 | −.16 | −.05 | .21 Ϯ | ____ | ||||
| 6. Negative Outcome Expectations | −.02 | −.14 | .63*** | −.67*** | −.08 | ____ | |||
| 7. Autonomous Motivation | −.05 | .03 | −.23* | .37** | .40** | −.31* | ______ | ||
| 8. Controlled Motivation | −.12 | −.15 | .21 Ϯ | −.18 | .19 | .22 Ϯ | .15 | ____ | |
| 9. Amotivation | −.04 | .06 | .21 | −.13 | −.10 | .16 | −.43*** | .01 | ____ |
| 10. Nutrition knowledge | .03 | .02 | −.06 | −.16 | .05 | −.06 | .07 | .00 | −.28* |
| Control Group (N = 70) | |||||||||
| 1. Age | ____ | ||||||||
| 2. WPFD | .22 Ϯ | ____ | |||||||
| 3. Healthy Eating Barriers, Parent | −.01 | −.20 | ____ | ||||||
| 4. Self-efficacy | .02 | .14 | −.63*** | ____ | |||||
| 5. Positive Outcome Expectations | −.00 | .16 | −.35** | .39** | ____ | ||||
| 6. Negative Outcome Expectations | −.11 | −.31** | .67*** | −.73** | −.29* | ____ | |||
| 7. Autonomous Motivation | −.14 | .18 | −.36** | .36** | .33** | −.29* | ____ | ||
| 8. Controlled Motivation | −.08 | −.08 | .09 | .01 | .09 | .21 Ϯ | .28* | ____ | |
| 9. Amotivation | .07 | .13 | .14 | .06 | −.22 Ϯ | .14 | −.01 | .36** | ____ |
| 10. Nutrition knowledge | .38** | .31** | −.06 | −.19 | .13 | .05 | .02 | −.11 | −.22 Ϯ |
Note
P<.10,
P<.05,
p<.01,
p<.001
Across intervention groups, greater parent self-efficacy (B=.21, p=.02), autonomous motivation (B=.17, p=.002), and nutrition knowledge (B=.01, p=.03) as well as lower barriers (B=-.19, p=.02) and negative outcome expectations (B= −.20, p=.008) were associated with greater youth WPFD. Parent positive outcome expectations (B=.07, p=.45) and controlled motivation (B=-.03, p=.56) were not associated with youth WPFD.
Significant interactions of parent nutrition knowledge with healthy eating barriers (B=-.02, p=.001) and negative outcome expectations (B=−.02, p=.008) were observed (Figures 1). Simple slopes analysis revealed that parent healthy eating barriers were inversely associated with youth diet quality for parents with higher nutrition knowledge (B=-.32, p=.005), but there was no association for those with lower nutrition knowledge (B=-.09, p=.42). Similarly, parent negative outcome expectations was inversely associated with youth WPFD for parents with higher nutrition knowledge (B=-.32, p=.001), but not those with lower nutrition knowledge (B=-.18, p=.08). There were no significant interactions of parent nutrition knowledge with self-efficacy, autonomous motivation, or controlled motivation on youth WPFD (p-values>.37).
Youth age did not modify associations of parent psychosocial variables with youth WPFD (p-values>.12), suggesting no difference in the influence of each psychosocial variable with diet quality for adolescents vs. pre-adolescents.
Given the lack of an intervention effect on parent attitudes and beliefs, post-hoc analyses were conducted using separate linear mixed effects models to test the effect of the intervention on youth attitudes and beliefs. All analyses were identical to those run for the parents. Results showed no significant effect of the intervention on any youth attitudes/beliefs (all p-values >0.23).
Discussion
This study examined whether the previously shown (Nansel, 2015) positive effect of a behavioral nutrition intervention grounded in SDT and SCT on youth diet quality is explained by changes in parent attitudes and beliefs. Contrary to our hypothesis, there was no effect of the intervention on any of the attitudes/beliefs. Thus, while the intervention did improve youth intake of whole plant foods (Nansel et al., 2015), this effect was not through the pathway of these theoretically-driven constructs. This conclusion is further supported by the lack of an effect on any of the youth attitudes/beliefs.
However, youth diet quality was associated positively with parent self-efficacy and autonomous motivation, and negatively with parent perceived barriers and negative outcome expectations, partially supporting hypothesis two. In contrast, neither positive outcome expectations nor controlled motivation was associated with youth diet quality. The association of youth diet quality with negative but not positive outcome expectations may indicate that parents’ outcome expectations work as an inhibitor, rather than a motivator of youth healthy diet. The lack of an association between controlled motivation and youth diet quality is consistent with previous findings that autonomous motivation is a relatively stronger predictor of healthful eating (Pelletier & Dion, 2007; Teixeira et al., 2011).
The hypothesis that parent nutrition knowledge would moderate the association between parent psychosocial variables and youth dietary quality was partially supported. Inverse associations of youth diet quality with parent perceived barriers and negative outcome expectations were observed only when parent nutrition knowledge was high, suggesting that efforts to improve youth diet quality by reducing parent perceived barriers and negative outcome expectations may be more impactful when coupled with nutrition education.
There was no significant interaction of youth age with any parent psychosocial variable, indicating that parent’s attitudes and beliefs regarding providing healthy food to their families influence youth diet throughout pre-adolescence and adolescence. This emphasizes the importance of parents when targeting youth diet quality. While adolescents, compared to pre-adolescents, may be less dependent on parents and more dependent on peers in their food choices, research shows that parents may continue influencing youth diet into adolescence, but due to behavioral modelling (Pedersen, Grønhøj, & Thøgersen, 2014) and parent social support (Piko & Brassai, 2009).
For youth with T1D, dietary intake is important for disease management and prevention of long-term complications, yet little research has examined how to improve dietary quality most effectively among this high-risk population. The current study tested whether the improvement in diet quality shown in the intervention group (Nansel et al., 2015) was driven by parents’ attitudes/beliefs. It could be hypothesized that parent attitudes/beliefs would mediate the intervention’s effect on youth diet quality, but our findings do not support this since the intervention had no effect on parent or youth attitudes/beliefs. Results highlight the difficulty in changing these attitudes/beliefs through intervention, despite these variables being associated with diet quality across conditions. This supports previous research showing an intervention effect on diet quality, but not always through the hypothesized psychosocial pathways (Burke, Dunbar-Jacob, Orchard, & Sereika, 2005; Glasgow, Toobert, Mitchell, Donnelly, & Calder, 1989; Spahn et al., 2010) and may reflect a possible inadequacy of these behavioral theories or the interventions based on these theories with respect to dietary change (Weinstein, 2007), at least in this specific population.
Study findings should be interpreted in light of the strengths and limitations. The longitudinal nature of the study is a considerable strength due to additional statistical power to detect associations, as are the three-day diet records which are among the most reliable and valid measures of dietary intake. While food records are susceptible to measurement error associated with reactivity bias, errors of self-assessment (e.g., portion size estimation), and social desirability bias, a number of steps were taken to mitigate measurement error in the food records like providing participants with instructions and tools to make their records as accurate and complete as possible, reviewing completed records upon receipt from the family to ensure completeness, and soliciting missing information from the family as needed. Generalizability was limited because participants were primarily white, drawn from a single clinic with a limited number of low-income families, and, despite the relatively high retention rate, reflect a 24% recruitment rate. The positive skew of some psychosocial variables may have created a ceiling effect, limiting the ability to detect an intervention effect.
Despite recommendations to consume a healthful diet, youth with T1D consume diets high in foods of minimal nutritional value and low in whole plant foods, markedly similar to the general population. This study examined the importance of parent food-related attitudes/beliefs, specifically those deriving from SCT and SDT, on the diet quality of youth with type 1 diabetes in the context of an 18-month behavioral nutrition intervention. Findings support the associations of already-held parent self-efficacy, perceived barriers, negative outcome expectations, and autonomous motivation with diet quality of youth with T1D across pre-adolescence and adolescence, especially among those with high nutrition knowledge. Findings also highlight the challenge of changing these already-held attitudes and beliefs among parents of youth with T1D and suggest that additional research is warranted to modify and refine behavioral theories to drive interventions more effectively. Recognizing and better understanding the role of parent attitudes, beliefs, and nutrition knowledge may improve youths’ diet quality and overall, long-term health.
Figure 2.
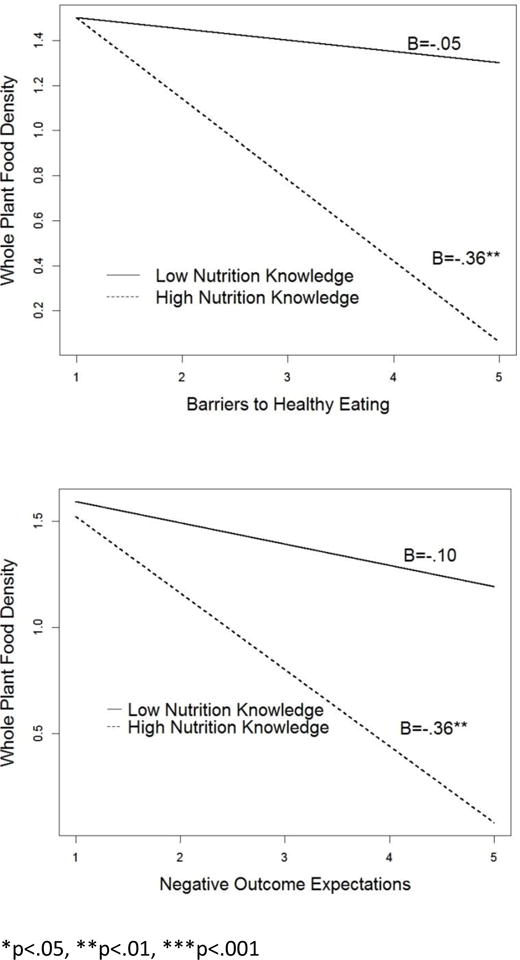
Nutrition knowledge moderates the influence of perceived barriers a healthy eating on diet quality and the influence of negative outcome expectations of healthy eating on diet quality.
Acknowledgments
The authors thank the research staff at the clinical site and the participants for their contributions to this study. This research was supported by the intramural research program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development, contract #’s #HHSN267200703434C and #HHSN2752008000031/HHSN275002.
Footnotes
ClinicalTrials.gov identifier: NCT00999375
References
- ADA. American Diabetes Association: Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31:S61–S78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- Anderson-Bill ES, Winett RA, Wojcik JR. Social cognitive determinants of nutrition and physical activity among web-health users enrolling in an online intervention: the influence of social support, self-efficacy, outcome expectations, and self-regulation. Journal of medical Internet research. 2011;13(1) doi: 10.2196/jmir.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Annals of Behavioral Medicine. 2007;34(3):304–312. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- Austin S, Senécal C, Guay F, Nouwen A. Effects of gender, age, and diabetes duration on dietary self-care in adolescents with type 1 diabetes: a Self-Determination Theory perspective. Journal of health psychology. 2011;16(6):917–928. doi: 10.1177/1359105310396392. [DOI] [PubMed] [Google Scholar]
- Axelson ML, Federline TL, Brinberg D. A meta-analysis of food- and nutrition-related research. Journal of Nutrition Education. 1985;17(2):51–54. doi: 10.1016/S0022-3182(85)80175-8. [DOI] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological review. 1977;84(2):191. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: An agentic perspective. Annual review of psychology. 2001;52(1):1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health Promotion by Social Cognitive Means. Health Education & Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Mooradian AD. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes care. 2008;31:S61–S78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- Brown MJ, Sinclair M, Liddle D, Hill AJ, Madden E, Stockdale J. A Systematic Review Investigating Healthy Lifestyle Interventions Incorporating Goal Setting Strategies for Preventing Excess Gestational Weight Gain. PLoS ONE. 2012;7(7):e39503. doi: 10.1371/journal.pone.0039503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruening M, Kubik MY, Kenyon D, Davey C, Story M. Perceived Barriers Mediate the Association between Self-Efficacy and Fruit and Vegetable Consumption among Students Attending Alternative High Schools. Journal of the American Dietetic Association. 2010;110(10):1542–1546. doi: 10.1016/j.jada.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Dunbar-Jacob J, Orchard TJ, Sereika SM. Improving adherence to a cholesterol-lowering diet: A behavioral intervention study. Patient Education and Counseling. 2005;57(1):134–142. doi: 10.1016/j.pec.2004.05.007. [DOI] [PubMed] [Google Scholar]
- Campbell K, Hesketh K, Silverii A, Abbott G. Maternal self-efficacy regarding children's eating and sedentary behaviours in the early years: Associations with children's food intake and sedentary behaviours. International Journal of Pediatric Obesity. 2010;5(6):501–508. doi: 10.3109/17477161003777425. [DOI] [PubMed] [Google Scholar]
- CDC. Child development: Young Teens (12–14 years of age) 2015 [Google Scholar]
- Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuits: human needs and the self-determination of behavior. Psychoanal Inq. 2000;11:227–268. [Google Scholar]
- Deci EL, Ryan RM. Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology/Psychologie canadienne. 2008;49(3):182. [Google Scholar]
- Eisenberg MH, Lipsky LM, Dempster KD, Liu A, Nansel TR. I should but I can't: Controlled motivation and self-efficacy are related to disordered eating behaviors in adolescents with type 1 diabetes. Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2016.06.008. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuemmeler BF, Masse LC, Yaroch AL, Resnicow K, Campbell MK, Carr C, Williams A. Psychosocial mediation of fruit and vegetable consumption in the body and soul effectiveness trial. Health Psychol. 2006;25(4):474–483. doi: 10.1037/0278-6133.25.4.474. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Mitchell DL, Donnelly JE, Calder D. Nutrition education and social learning interventions for type II diabetes. Diabetes Care. 1989;12(2):150–152. doi: 10.2337/diacare.12.2.150. [DOI] [PubMed] [Google Scholar]
- Hoelscher DM, Evans A, Parcel GS, Kelder SH. Designing effective nutrition interventions for adolescents. J Am Diet Assoc. 2002;102(3 Suppl):S52–63. doi: 10.1016/s0002-8223(02)90422-0. [DOI] [PubMed] [Google Scholar]
- Knight KM, McGowan L, Dickens C, Bundy C. A systematic review of motivational interviewing in physical health care settings. British Journal of Health Psychology. 2006;11(2):319–332. doi: 10.1348/135910705X52516. [DOI] [PubMed] [Google Scholar]
- Larsen JK, Hermans RCJ, Sleddens EFC, Engels RCME, Fisher JO, Kremers SPJ. How parental dietary behavior and food parenting practices affect children's dietary behavior. Interacting sources of influence? Appetite. 2015;89(0):246–257. doi: 10.1016/j.appet.2015.02.012. http://dx.doi.org/10.1016/j.appet.2015.02.012. [DOI] [PubMed] [Google Scholar]
- Leong S, Madden C, Gray A, Horwath C. Self-determined, autonomous regulation of eating behavior is related to lower body mass index in a nationwide survey of middle-aged women. J Acad Nutr Diet. 2012;112:1337–1346. doi: 10.1016/j.jand.2012.04.018. [DOI] [PubMed] [Google Scholar]
- Lipsky LM, Cheon K, Nansel TR, Albert PS. Candidate measures of whole plant food intake are related to biomarkers of nutrition and health in the US population (National Health and Nutrition Examination Survey 1999–2002) Nutrition Research. 2012;32(4):251–259. doi: 10.1016/j.nutres.2012.03.005. http://dx.doi.org/10.1016/j.nutres.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta SN, Volkening LK, Quinn N, Laffel LMB. Intensively managed young children with type 1 diabetes consume high-fat, low-fiber diets similar to age-matched controls. Nutrition Research. 2014;34(5):428–435. doi: 10.1016/j.nutres.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- Michie S, Ashford S, Sniehotta F, Dombrowski S, Bishop A, French D. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26:1479–1498. doi: 10.1080/08870446.2010.540664. [DOI] [PubMed] [Google Scholar]
- Nansel TR, Haynie DL, Lipsky LM, Laffel LM, Mehta SN. Multiple indicators of poor diet quality in children and adolescents with type 1 diabetes are associated with higher body mass index percentile but not glycemic control. J Acad Nutr Diet. 2012;112(11):1728–1735. doi: 10.1016/j.jand.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nansel TR, Haynie DL, Lipsky LM, Wang J, Mehta SN, Laffel LMB. Relationships among parent and youth healthful eating attitudes and youth dietary intake in a cross-sectional study of youth with type 1 diabetes. International Journal of Behavioral Nutrition and Physical Activity. 2013;10 doi: 10.1186/1479-5868-10-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nansel TR, Laffel LM, Haynie DL, Mehta SN, Lipsky LM, Volkening LK, Liu A. Improving dietary quality in youth with type 1 diabetes: randomized clinical trial of a family-based behavioral intervention. Int J Behav Nutr Phys Act. 2015;12(1):58. doi: 10.1186/s12966-015-0214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton SR. Adherence to Diet in Youth with Type 1 Diabetes. Journal of the American Dietetic Association. 2011;111(4):550–555. doi: 10.1016/j.jada.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen S, Grønhøj A, Thøgersen J. Following family or friends. Social norms in adolescent healthy eating. Appetite. 2014 doi: 10.1016/j.appet.2014.07.030. [DOI] [PubMed] [Google Scholar]
- Pelletier LG, Dion SC. An Examination of General and Specific Motivational Mechanisms for the Relations Between Body Dissatisfaction and Eating Behaviors. Journal of Social and Clinical Psychology. 2007;26(3):303–333. doi: 10.1521/jscp.2007.26.3.303. [DOI] [Google Scholar]
- Piko BF, Brassai L. The Role of Individual and Familial Protective Factors in Adolescents’ Diet Control. Journal of Health Psychology. 2009;14(6):810–819. doi: 10.1177/1359105309338971. [DOI] [PubMed] [Google Scholar]
- Poverty Thresholds 2008. (2010)
- Quick V, Nansel TR, Lipsky LM, Laffel LM, Mehta SN. Food and Nutrition Conference and Expo. Nashville, Tennessee: 2015. Autonomous and controlled motivation for healthful eating in youth with type 1 diabetes and their parents. [Google Scholar]
- Resnicow K, Davis-Hearn M, Smith M, Baranowski T, Lin LS, Baranowski J, Wang DT. Social-Cognitive Predictors of Fruit and Vegetable Intake in Children. Health Psychology. 1997;16(3):272–276. doi: 10.1037//0278-6133.16.3.272. [DOI] [PubMed] [Google Scholar]
- Rovner AJ, Nansel TR. Are children with type 1 diabetes consuming a healthful diet?: A review of the current evidence and strategies for dietary change. Diabetes Educator. 2009;35(1):97–107. doi: 10.1177/0145721708326699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovner AJ, Nansel TR, Mehta SN, Higgins LA, Haynie DL, Laffel LM. Development and validation of the type 1 diabetes nutrition knowledge survey. Diabetes Care. 2012;35(8):1643–1647. doi: 10.2337/dc11-2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart C, Aslander-van Vliet E, Waldron S. Nutritional management in children and adolescents with diabetes. Pediatric Diabetes. 2009;10:100–117. doi: 10.1111/j.1399-5448.2009.00572.x. [DOI] [PubMed] [Google Scholar]
- Spahn JM, Reeves RS, Keim KS, Laquatra I, Kellogg M, Jortberg B, Clark NA. State of the Evidence Regarding Behavior Change Theories and Strategies in Nutrition Counseling to Facilitate Health and Food Behavior Change. Journal of the American Dietetic Association. 2010;110(6):879–891. doi: 10.1016/j.jada.2010.03.021. http://dx.doi.org/10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Strachan SM, Brawley LR. Healthy-eater Identity and Self-efficacy Predict Healthy Eating Behavior: A Prospective View. Journal of Health Psychology. 2009;14(5):684–695. doi: 10.1177/1359105309104915. [DOI] [PubMed] [Google Scholar]
- Taylor RW, Brown D, Dawson AM, Haszard J, Cox A, Rose EA, William SM. Motivational interviewing for screening and feedback and encouraging lifestyle changes to reduce relative weight in 4-8 year old children: design of the MInT study. BMC Public Health. 2010;10(1):1–11. doi: 10.1186/1471-2458-10-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira PJ, Patrick H, Mata J. Why we eat what we eat: the role of autonomous motivation in eating behaviour regulation. Nutrition Bulletin. 2011;36(1):102–107. doi: 10.1111/j.1467-3010.2010.01876.x. [DOI] [Google Scholar]
- Valkenburg PM. Gender differences in online and offline self‐disclosure in pre‐adolescence and adolescence. The British journal of developmental psychology. 2011;29(2):253. doi: 10.1348/2044-835X.002001. [DOI] [PubMed] [Google Scholar]
- Videon TM, Manning CK. Influences on adolescent eating patterns: the importance of family meals. Journal of Adolescent Health. 2003;32(5):365–373. doi: 10.1016/s1054-139x(02)00711-5. http://dx.doi.org/10.1016/S1054-139X(02)00711-5. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Misleading tests of health behavior theories. Annals of Behavioral Medicine. 2007;33(1):1–10. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70(1):115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]


