Abstract
Objectives
Identifying characteristics associated with the use of new and emerging tobacco products is a priority. The enumeration and baseline characteristics of a new cohort of adult tobacco users are described.
Methods
Residents, ≥18 years of age, in urban Franklin County, or one of 6 rural Appalachian counties, and who were exclusive users of combustible, smokeless (SLT), or electronic nicotine delivery systems (ENDS) tobacco products, or were dual users, were targeted for recruitment. Participants were interviewed in-person at baseline on sociodemographic characteristics, tobacco product use, and cognitive/affective and purchasing factors.
Results
We recruited 1210 participants (urban, N = 595; rural, N = 615). Urban participants were less likely to use tobacco daily, began using tobacco later, used tobacco for less time, and had higher cessation interest. ENDS users were significantly less likely to have made a quit attempt than users of other tobacco products. Duration of tobacco use and nicotine dependence also differed by product type.
Conclusion
This cohort’s enumeration allowed us to compare factors associated with tobacco product preferences and the use of novel products. The inclusion of rural Appalachia—a region with high tobacco use and disease burden—may provide additional insights into the implementation of tobacco control interventions.
Keywords: Appalachia, cohort enumeration, electronic nicotine delivery systems (ENDS), smokeless tobacco, smoking
The landscape of tobacco products and their uses is rapidly evolving. Electronic Nicotine Delivery Systems (ENDS) have gained significant market share since their 2007 introduction.1 ENDS are making inroads among tobacco users especially and are also attracting new users.2 Use of small cigars is also increasing.3,4 In addition, the category of tobacco user who regularly consumes multiple tobacco products, the so-called “dual” or “poly” user, is increasing and includes individuals who typically smoke combustible tobacco products and also consume smokeless tobacco (SLT) and/or ENDS.5–7
Understanding the diversity of tobacco products used in the United States (US) represents a crucial area for tobacco regulatory science, as dual use might impact the use of any individual tobacco product.8 For example, products such as SLT and ENDS could discourage smokers from quitting because they can be used in environments where smoking is prohibited.9 Dual use also might have an adverse impact on nicotine dependence and abuse liability for any individual product. The current marketplace presents consumers with a wide selection of combustible and non-combustible products. Given that cigarettes are the predominant product causing significant population harm,10–12 an important goal is to shift combustible users to less harmful non-combustible products or quitting. Despite a wealth of data on tobacco-related behaviors among adults for SLT and combustible tobacco products, data for ENDS is only emerging. Current data only come from individual or repeated cross-sectional studies, many of which are Internet-based. The only tobacco-focused longitudinal cohort study that we are aware of is the Population Assessment of Tobacco and Health (PATH) study.13,14
At present, little is known about the factors that predict ENDS and dual use. Factors associated with adult ENDS uptake among smokers include quit intention, health concerns, convenience, and social acceptability compared to cigarettes.15–18 Characteristics associated with the uptake of ≥2 products include male sex, young age, white race, less education, and current alcohol and drug use.4,7,19–21 Additional factors to consider include abuse liability that fosters nicotine dependence, risk perceptions and health literacy, and nicotine and toxicant delivery due to product design. These factors interact with the environment via marketing and social norms. Dual use of cigarettes and SLT, for instance, is prevalent in rural settings,7 whereas urban dual users may choose combustible products and ENDS.4
Adult tobacco use in Ohio is high: 23.4% smoke (national median 19%); 4.4% use SLT (national median 4.3%); and 6.4% are dual users.22 The prevalence of combustible products and SLT are well-known to be much higher in rural than urban areas.23–25 Similarly, the burden of tobacco-related disease is higher in Appalachian Ohio (a rural, medically underserved, and socioeconomically depressed region) than other parts of the state.26,27 In response to this disparity, we have established a cohort of tobacco product users recruited from urban Ohio and rural Appalachian Ohio as the third project of the Ohio State University’s Center for Excellence in Regulatory Tobacco Science (OSU- CERTS; P50 CA180907-01). The goals of this ongoing cohort study are to: (1) identify and compare factors associated with the exclusive and dual use of new and emerging tobacco products, and how they relate to cessation; (2) compare associations of cognitive and affective, purchasing, and individual factors with use of specific tobacco products; and (3) identify whether the magnitude of these associations differ by urban versus rural regions in Ohio. Herein, we describe the cohort’s enumeration, methodology, and baseline sociodemographic and tobacco-related characteristics.
METHODS
Study Overview
The study design involved assembling a prospective cohort of adults who exclusively used combustible, SLT, ENDS, or who were dual (or poly) users of these products in urban Franklin County, Ohio, which includes the city of Columbus (the state capital) and 6 rural Appalachian Ohio counties (Brown, Guernsey, Lawrence, Muskingum, Scioto and Washington). These counties were chosen because they are counties in which we have an existing research infrastructure, have a high adult prevalence of smoking (27%–35%),28 and have a large rural population (46%–77%).29 Different from several national studies, this study did not aim to create a representative sample of tobacco users, but rather, to establish a generalizable cohort of adult regular users of diverse tobacco products in Ohio who could be reliably followed prospectively. A total of 1210 participants were recruited and completed a comprehensive baseline in-person interview with subsequent follow-up interviews every 6 months for 36 months. Cohort participants were interviewed in person at baseline and continue to be interviewed face-to-face every 6 months (6, 12, 18, 24, 30 and 36 months) for a total enrollment of 3 years. Three months after each interview, a retention letter was sent to the participant to verify that the contact information was still the same. Two weeks prior to the next appointment window, the participant was contacted by the interviewer to schedule the appointment. The day before each scheduled interview, a reminder email, phone call, or text was performed to confirm the interview. A $50 gift card was given after each follow-up interview.
Participant Recruitment
Address-based sampling using the US Postal Service’s Computerized Delivery Sequence File was used to randomly sample addresses in the 7 recruitment counties.30,31 Our recruitment goal was to achieve a sample size of 796 by the end of the 3-year study, consisting of 50% residing in urban and rural counties, after accounting for an anticipated 10% annual attrition rate. Between August 2014 and August 2015, postcards alerting households that a screener letter would be coming from OSU-CERTS researchers were sent to 180,075 addresses (urban, 89,763; rural, 90,312). The number of addresses was initially chosen based upon the prevalence of dual and SLT users in Ohio,22 with the intent of ensuring sufficient participation from users within these categories. The screener letter stated that OSU was seeking volunteers for health prevention studies and requested the recipient to return a short questionnaire about the household composition and some health behaviors. The letter included a $2 bill. Questions included the age, sex, and contact information of all household residents ≥18 years of age, current use of tobacco products, and information about diet and physical activity. These questions assisted in recruitment for related projects (including a separate cohort of adolescent male tobacco users and their families) as part of the OSU-CERTS. The household was asked to indicate whether they would be willing to be contacted about participating in a study and to return the questionnaire to OSU research staff in a self-addressed, stamped envelope. Upon return of the questionnaire, one potentially eligible adult from each household was randomly selected to participate. The selected household member was contacted by phone by a trained local field interviewer to confirm eligibility and schedule a time to meet face-to-face to explain the study, obtain informed consent, and conduct the baseline interview. Baseline interviews were conducted between October 2014 and January 2016. Households that did not respond to the initial letter received a second, identical letter 3 weeks later which contained the same package (ie, screener letter, questionnaire, and self-addressed stamped envelope) but no additional incentive. Recruitment was targeted to users of non-combustible tobacco products after sufficient numbers of combustible users were achieved.
Eligibility Criteria
Eligibility was determined by a screening phone interview conducted by a trained local field interviewer. Potential participants were asked if they were ≥18 years of age and if they resided in Franklin County or one of the 6 participating rural Appalachian counties. To determine tobacco use eligibility, participants were asked: (1) “Have you smoked >100 cigarettes (or small cigars/cigarillos, pipes filled with tobacco, cigars, filtered cigars, or hookahs) in your lifetime?” (2) “Do you currently smoke tobacco products, including cigarettes, small cigars/cigarillos, pipes filled with tobacco, cigars, filtered cigars, or hookahs) every day, some days per week, occasionally, rarely, or not at all?” (3) “Do you currently use smokeless tobacco products, such as chewing tobacco, snuff, snus, or dissolvable tobacco every day, some days per week, occasionally, rarely, or not at all?” and (4) “Do you currently use an electronic cigarette every day, some days per week, occasionally, rarely, or not at all?”
To be considered eligible for the study, respondents needed to be ≥18 years of age, reside in one of the 7 participating counties, and be: (1) an exclusive user of combustible tobacco, defined as self-reported smoking >100 combustible tobacco products in their lifetime and currently smoking ≥ some days each week; (2) exclusive user of an SLT product ≥some days each week; (3) exclusive user of an ENDS product, ≥ some days each week; or (4) a dual user, who used ≥ 2 of the 3 tobacco product categories above ≥ some days each week. Combustible tobacco from all sources is considered harmful to health.32 Therefore, combustible tobacco was decided a priori to be considered as a single category (ie, rather than recruit users of each individual product separately) to examine tobacco use in each region more completely.
Baseline Procedures
Survey responses were entered by a trained interviewer using the Research Electronic Data Capture (REDCap) secure management system.33 The only exceptions to the data entry process were the collection of information on drug and alcohol use, as well as prior diagnoses of mental health disorders. For these variables, the participant directly entered the information into REDCap, using audio computer-assisted self-interview software. Location sites for conducting the interview were determined by the participant and included the participant’s home, a county/city building (eg, library) or a local retail venue (eg, restaurant). The baseline interview session, including the consenting process, lasted about one hour. Participants were paid $50 for completion of the interview. To decrease the potential for loss to follow-up, participants were asked to provide contact information for 2 additional people who would know how to contact them.
Data Collection
The baseline and follow-up in-person interviews collected information on several research domains, including a variety sociodemographic variables, including age, sex, sexual orientation, race/ethnicity, level of education, marital status, residence, household income, occupation, and medical history (including assessments of physical and mental health, and current drug and alcohol use) and a variety of tobacco-related questions, such as: (1) past and current tobacco use, including data on current and past tobacco product use type(s), brand(s) and frequency of use, age of initiation of tobacco use, number of previous quit attempts, measures of nicotine dependence,34,35 tobacco use status of household, family members, and friends/co-workers, stage of change,36,37 cessation interest,38 cessation self-efficacy,38 and presence of indoor clean air policies at work and home;39 (2) cognitive/affective variables, including data on risk perceptions of tobacco product use,40 and risk-reduction beliefs;40,41 and (3) purchasing information, including brand loyalty42 and use of price promotions (including coupons, multi-pack specials, and special discounts to purchase tobacco products).43 To increase the generalizability of the collected data, we utilized multiple questions from the Food and Drug Administration’s Population Assessment of Tobacco and Health (PATH) national cohort study.13
For the present analysis, we assessed baseline characteristics for a select number of sociodemo-graphic variables, including age, sex, sexual orientation, race (Caucasian, African-American, Asian/ Pacific Islander, American Indian/Alaskan Native, Other), education (<high school, GED/high school diploma, ≥some college), household income (<$25,000, $25,000–$50,000, >$50,000), marital status (single/never married, married/cohabitating, separated/divorced, widowed), and employment status (full-time, part-time, unemployed). We also assessed baseline data for selected tobacco-related characteristics, including daily use (yes/ no), age of tobacco initiation, years tobacco products were consumed, time to first use (>30, ≤30 minutes), stage of change (pre-contemplation, contemplation, preparation), number of previous quit attempts, other household tobacco users (no/ yes), and the presence of work indoor air restrictions (smoking never allowed, sometimes allowed, always allowed). We also assessed data on cessation interest, which is derived from a question that asks participants to rate their likelihood of quitting on a scale of 0 (least likely) to 10 (most likely). Lastly, participants were asked the number of days in the past 30 that ≥ 5 alcoholic drinks were consumed in a row within a couple of hours. Participants who reported ≥1 day in the past 30 days were considered to binge drink.44,45
Data Analyses
Response and cooperation rates were calculated using the American Association for Public Opinion Research (AAPOR) RR1 and COOP1 formulas, respectively.46 Continuous data were summarized with means and standard deviations, and categorical data with frequencies and percentages. Differences were assessed for recruitment region (ie, urban versus rural) and product use type (ie, combustible, SLT, ENDS, dual) by ANOVA and chi-squared tests, as appropriate. The age at which participants began regular tobacco use was log-transformed in order to better approximate a normal distribution. All p-values were adjusted for multiple comparisons using a conservative Bonferroni correction. For perspective, a Bonferroni-adjusted p-value < .05, adjusted for 38 comparisons, corresponds to a raw p-value < .001. SAS 9.4 (SAS Institute Inc., Cary, NC) was used to conduct all analyses.
RESULTS
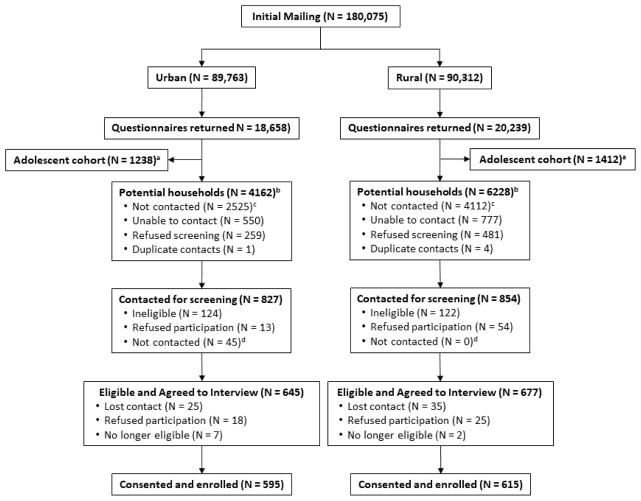
Figure 1 shows frequencies of the cohort enrollment. From 180,075 (urban, N = 89,763; rural, N = 90,312) mailings to unique addresses 38,897 were returned (urban, N = 18,658; rural, N = 20,239) with an overall response rate of 21.60% (urban, 20.8%; rural, 22.4%). Among these, 2650 households included an adolescent male. These households were prioritized for recruitment in a separate OSU-CERTS cohort of adolescents and their families. From the 36,247 returned questionnaires, 10,390 indicated at least one household member ≥18 years of age used tobacco products. Among them, 1681 (urban, N = 827; rural, N = 854) participants were contacted and screened for eligibility. Due to the success of the enrollment strategy, nearly two-thirds of potentially eligible addresses and participants (N = 6637) were not contacted as the target sample size was reached. Among the 1681 participants screened, 247 (14.7%) were deemed ineligible, 67 (4.0%) were eligible but refused participation, and 45 (2.7%) were eligible but not contacted further, leaving 1322 eligible tobacco users who consented to participate in the study. Among them, contact was lost in 60 (4.5%) participants, 43 (3.3%) refused participation, and 9 (<1%) quit using tobacco products at or before baseline, resulting in 1,210 (urban, N = 595; rural, N = 615) participants available for study. The response rate (RR1, (46)) among those contacted was 57.1% (urban, 65.4%; rural, 50.8%). Among the 1210 participants, 724 used combustible tobacco products, 208 used SLT, 133 used ENDS, and 145 were dual users (comprised of, N = 113 combustible/ENDS, N = 25 combustible/SLT, N = 4 SLT/ENDS, and N = 3 poly-users). Approximately 92% (urban, 95.1%; rural, 88.6%) of those who set up an appointment followed through and participated in the study (COOP1).46 At one year, the cohort’s retention rate was 95%.
Figure 1. Recruitment of Adult Tobacco Users in Ohio, Stratified on Region.
Note.
a: Returned mailings indicating that ≥1 household member was a male, 11–16 years of age.
b: Returned mailings indicating that ≥1 household member used tobacco products.
c: Individuals were not contacted towards the end of recruitment because the anticipated cohort size was reached.
d: Individuals were not contacted after the eligibility screen in order to focus recruitment on SLT, ENDS, and dual users.
Baseline Characteristics of Study Participants
Table 1 shows the baseline characteristics of the 1210 cohort participants. Participants were slightly more likely to be male (55.8%), identified as straight (93.5%), were middle-aged, Caucasian, and college-educated. A majority of participants were employed, with approximately equal distributions of household incomes across 3 categories (<$25,000, $25,001–$50,000, >$50,000). Several differences were apparent when urban (N = 595) and rural (N = 615) participants were compared. Relative to rural participants, urban participants were younger, more racially diverse, slightly more educated, were more likely to be employed and had higher household incomes.
Table 1.
Baseline Characteristics of Adult Tobacco Users in Ohio, Stratified by Region (N = 1210)
| Recruitment Region, N (%)
|
||||
|---|---|---|---|---|
| Total (N = 1210) N (%) | Urban (N = 595) | Rural (N = 615) | p-valuea | |
| Age, Years [mean (SD)] | 49.4 (15.3) | 47.3 (14.8) | 51.4 (15.4) | < .001 |
| Sex | 1.000 | |||
|
| ||||
| Male | 674 (55.8) | 332 (56.9) | 342 (55.6) | |
| Female | 535 (44.3) | 262 (44.1) | 273 (44.4) | |
|
| ||||
| Sexual Orientation | 1.000 | |||
|
| ||||
| Straight | 1,106 (93.5) | 540 (92.3) | 566 (94.7) | |
| Gay, Bisexual, or Other | 77 (6.5) | 45 (7.7) | 32 (5.4) | |
|
| ||||
| Race | < .001 | |||
|
| ||||
| Caucasian | 1,034 (85.6) | 442 (74.4) | 592 (96.4) | |
| African American | 154 (12.8) | 139 (23.4) | 15 (2.4) | |
| Asian/Pacific Islands | 5 (0.4) | 4 (0.7) | 1 (0.2) | |
| American Indian/Alaskan Native | 10 (0.8) | 5 (0.8) | 5 (0.8) | |
| Other | 5 (0.4) | 4 (0.7) | 1 (0.2) | |
|
| ||||
| Education | .014 | |||
|
| ||||
| <High School | 146 (12.1) | 71 (11.9) | 75 (12.2) | |
| GED/High School Graduate | 380 (31.4) | 156 (26.2) | 224 (36.4) | |
| ≥Some College | 684 (56.5) | 368 (61.9) | 316 (51.4) | |
|
| ||||
| Household Income | < .001 | |||
|
| ||||
| <$25,000 | 429 (37.5) | 175 (31.4) | 254 (43.3) | |
| $25,001–$50,000 | 355 (31.1) | 159 (28.6) | 196 (33.5) | |
| >$50,000 | 359 (31.4) | 223 (40.0) | 136 (23.2) | |
|
| ||||
| Marital Status | < .001 | |||
|
| ||||
| Single/Never Married | 348 (28.8) | 222 (37.3) | 126 (20.5) | |
| Married/Cohabitating | 514 (42.5) | 221 (37.1) | 293 (47.7) | |
| Separated/Divorced | 261 (21.6) | 120 (20.2) | 141 (23.0) | |
| Widowed | 86 (7.1) | 32 (5.4) | 54 (8.8) | |
|
| ||||
| Employment Status | < .001 | |||
|
| ||||
| Full-Time | 503 (41.6) | 302 (50.9) | 201 (32.7) | |
| Part-Time | 150 (12.4) | 71 (12.0) | 79 (12.9) | |
| Unemployed | 555 (45.9) | 220 (37.1) | 335 (54.5) | |
Note.
Bonferroni-adjusted
Table 2 provides baseline characteristics of participants stratified by their use of tobacco products. Results among exclusive combustible product users are further stratified by individual product type in Supplemental Table 1. ENDS and dual users tended to be younger (47 years and 45 years, respectively) than combustible and SLT users (each approximately 50 years). While combustible, ENDS, and dual use was near-equitably distributed by sex, SLT users were over 98% male. There was significant variation by race. Compared to users of SLT, ENDS, or dual products, users of combustible tobacco products were more likely to be non-white. Users of SLT and ENDS had the highest household incomes.
Table 2.
Baseline Characteristics of Adult Tobacco Users in Ohio, Stratified by Tobacco Product Category (N = 1210)
| Tobacco Product, N (%)
|
|||||
|---|---|---|---|---|---|
| Combustible (N = 724) | SLT (N = 208) | ENDS (N = 133) | Dual (N = 145) | p-valuea | |
| Age, Years [mean (SD)] | 50.37 (14.5) | 50.45 (16.7) | 47.25 (15.7) | 44.79 (15.8) | .007 |
| Sex | < .001 | ||||
|
| |||||
| Male | 321 (44.4) | 205 (98.6) | 68 (51.1) | 80 (55.2) | |
| Female | 402 (55.6) | 3 (1.4) | 65 (48.9) | 65 (44.8) | |
|
| |||||
| Sexual Orientation | .192 | ||||
|
| |||||
| Straight | 660 (93.2) | 201 (98.5) | 116 (89.9) | 129 (90.9) | |
| Gay, Bisexual, or Other | 48 (6.8) | 3 (1.5) | 13 (10.1) | 13 (9.2) | |
|
| |||||
| Race | < .001 | ||||
|
| |||||
| White | 575 (79.6) | 205 (98.6) | 125 (94.0) | 129 (89.0) | |
| Non-white | 147 (20.4) | 3 (1.4) | 8 (6.0) | 16 (11.0) | |
|
| |||||
| Education | .098 | ||||
|
| |||||
| <High School | 105 (14.5) | 15 (7.2) | 9 (6.8) | 17 (11.7) | |
| GED/High School Graduate | 230 (31.8) | 75 (36.1) | 31 (23.3) | 44 (30.3) | |
| ≥Some College | 389 (53.7) | 118 (56.7) | 93 (69.9) | 84 (57.9) | |
|
| |||||
| Household Income | < .001 | ||||
|
| |||||
| <$25,000 | 301 (43.9) | 36 (18.3) | 33 (26.6) | 59 (43.4) | |
| $25,001–$50,000 | 221 (32.2) | 60 (30.5) | 38 (30.7) | 36 (26.5) | |
| >$50,000 | 164 (23.9) | 101 (51.3) | 53 (42.7) | 41 (30.2) | |
|
| |||||
| Marital Status | < .001 | ||||
|
| |||||
| Single/Never Married | 231 (31.9) | 30 (14.5) | 43 (32.3) | 44 (30.3) | |
| Married/Cohabiting | 262 (36.2) | 133 (64.3) | 59 (44.4) | 60 (41.4) | |
| Separated/Divorced | 179 (24.7) | 34 (16.4) | 20 (15.0) | 28 (19.3) | |
| Widowed | 52 (7.2) | 10 (4.8) | 11 (8.3) | 13 (9.0) | |
|
| |||||
| Employment Status | 0.134 | ||||
|
| |||||
| Full-Time | 279 (38.6) | 107 (51.4) | 63 (47.4) | 54 (37.2) | |
| Part-Time | 97 (13.4) | 13 (6.3) | 20 (15.0) | 20 (13.8) | |
| Unemployed | 346 (47.9) | 88 (42.3) | 50 (37.6) | 71 (49.0) | |
Note.
Bonferroni-adjusted
Baseline Tobacco Use Behaviors
Table 3 presents distributions of participants’ tobacco-related characteristics given overall and by recruitment region. The majority (59.8%) of participants smoked combustible tobacco products, followed by use of SLT (17.2%), dual use (12.0%), and ENDS (11.0%). Almost all participants (94.1%) used tobacco products daily. Participants began regular use at approximately 18 years (SD 5.7) and used tobacco for 31.6 (SD 15.4) years on average. Participants used their current product type for 27.6 years (SD 16.8). About 60% used tobacco within 30 minutes of waking up. Consideration of quitting was moderate: the mean cessation interest was 6.1 (SD 3.1), 5% were in the preparation stage of change, and 30% (N = 358) attempted to quit at least once in the past year. Among them, 93 used another tobacco product as a quit aid (77 used an ENDS product) (not shown). The most commonly reported brands used for manufactured cigarettes, chewing tobacco, and ENDS, were Marlboro, Starr and Red Man (tied), and Vuse, respectively (Supplemental Table 2). The top purchase locations were convenience stores (including gas stations) and tobacco specialty stores.
Table 3.
Baseline Tobacco-related Behaviors among Adult Tobacco Users in Ohio, Stratified by Region (N = 1210)
| Recruitment Region, N (%)
|
||||
|---|---|---|---|---|
| Total (N = 1210) N (%) | Urban (N = 595) | Rural (N = 615) | p-valuea | |
| Tobacco Product | -- | |||
|
| ||||
| Combustible | 724 (59.8) | 376 (63.2) | 348 (56.6) | |
| SLT | 208 (17.2) | 64 (10.8) | 144 (23.4) | |
| ENDS | 133 (11.0) | 77 (12.9) | 56 (9.1) | |
| Dual | 145 (12.0) | 78 (13.1) | 67 (10.9) | |
|
| ||||
| Daily User | < .001 | |||
|
| ||||
| No | 71 (5.9) | 57 (9.6) | 14 (2.3) | |
| Yes | 1138 (94.1) | 538 (90.4) | 600 (97.7) | |
|
| ||||
| Age First Tried Tobaccob [mean (SD)] | 13.9 (5.3) | 14.5 (5.5) | 13.3 (5.0) | < .001 |
| Age Began Regular Useb [mean (SD)] | 17.8 (5.7) | 18.2 (6.0) | 17.3 (5.3) | .043 |
| Years Consumed Tobacco [mean (SD)] | 31.6 (15.4) | 29.0 (15.0) | 34.1 (15.4) | < .001 |
| Years Consumed Product [mean (SD)] | 27.6 (16.8) | 25.4 (16.3) | 29.8 (16.9) | < .001 |
| Time to First Use, Minutes | .095 | |||
|
| ||||
| >30 | 490 (40.7) | 266 (45.1) | 224 (36.5) | |
| ≤30 | 714 (59.3) | 324 (54.9) | 390 (63.5) | |
|
| ||||
| Cessation Interestc [mean (SD)] | 6.1 (3.1) | 6.6 (3.0) | 5.7 (3.1) | .016 |
| Stage of Change | .356 | |||
|
| ||||
| Pre-Contemplation | 648 (62.0) | 317 (59.0) | 331 (66.3) | |
| Contemplation | 345 (33.0) | 195 (35.7) | 150 (30.1) | |
| Preparation | 53 (5.1) | 35 (6.4) | 18 (3.6) | |
|
| ||||
| Previous Quit Attempts in Past Year | 1.000 | |||
|
| ||||
| None | 852 (70.4) | 399 (67.1) | 453 (73.7) | |
| 1–4 | 289 (23.9) | 158 (26.6) | 131 (21.3) | |
| ≥5 | 69 (5.7) | 38 (6.4) | 31 (5.0) | |
|
| ||||
| Other Household Tobacco Users | 1.000 | |||
|
| ||||
| No | 800 (66.1) | 389 (65.4) | 411 (66.8) | |
| Yes | 410 (33.9) | 206 (34.6) | 204 (33.2) | |
|
| ||||
| Binge Drinking | < .001 | |||
|
| ||||
| No | 836 (71.4) | 372 (65.0) | 464 (77.5) | |
| Yes | 335 (28.6) | 200 (35.0) | 135 (22.5) | |
|
| ||||
| Work Indoor Air Restrictions | 1.000 | |||
|
| ||||
| Never Allowed | 543 (89.3) | 320 (91.4) | 223 (86.4) | |
| Sometimes Allowed | 46 (7.6) | 21 (6.0) | 25 (9.7) | |
| Always Allowed | 19 (3.1) | 9 (2.6) | 10 (3.9) | |
Note.
Bonferroni-adjusted
p-value based on a log transformation
Cessation interest was measured on a scale of 0 (least likely) to 10 (most likely)
Several differences were apparent when the data were compared by region of residence. Compared to rural participants, urban participants were less likely to use tobacco daily (urban, 90.4% vs rural, 97.7%; p < .001), first tried (urban, 14.5 vs rural, 13.3 years; p < .001) and began using tobacco regularly later in life (urban, 18.2 vs rural, 17.3 years; p = .043), and used any tobacco product for a shorter amount of time [urban, 29.0 years vs rural, 34.1 years; p < .001 (results were similar when the current tobacco product type was considered, p < .001)]. Participants’ cessation interest was significantly higher among urban participants (urban, 6.6 vs rural, 5.7; p =.016). Although urban participants were more likely to be in the contemplation or preparation stage of change than rural participants, and were more likely to have attempted to quit in the last year, these findings were not statistically significant with a Bonferroni correction applied.
Table 4 and Supplemental Table 3 show the distributions of participants’ tobacco-related characteristics by tobacco product used. Participants did not differ regarding their daily use of each tobacco product category (p > .99) or age at first regular use (p > .99); however, there were differences for ages that participants first tried tobacco (p < .03). The duration of tobacco use differed by product type, with SLT (33.3 years) and combustible users (32.5 years) having used any tobacco the longest, and ENDS (29.1 years) or dual users (27.4 years; p = .008) the shortest. Similarly, use of current tobacco product types also differed significantly. Over half of participants used their respective tobacco products within 30 minutes of waking, with the exception of SLT users (39.9%, p < .001). Although mean cessation interest and stage of change did not differ significantly by product type, there were significant differences for numbers of quit attempts, with ENDS users the least likely to have attempted to quit (94.7% made no quit attempts; vs Combustible, 68.5%; SLT, 72.6%; and Dual, 54.5%; p < .001). Approximately 40% of combustible and dual users had other tobacco users in the household, whereas this was reported in a much smaller proportion of ENDS (24.8%) and SLT users (13.9%; p < .001).
Table 4.
Baseline Tobacco-related Behaviors among Adult Tobacco Users in Ohio, Stratified by Tobacco Product Category (N = 1210)
| Tobacco Product, N (%)
|
|||||
|---|---|---|---|---|---|
| Combustible (N = 724) | SLT (N = 208) | ENDS (N = 133) | Dual (N = 145) | p-valuea | |
| Daily User | 1.000 | ||||
|
| |||||
| No | 40 (5.5) | 10 (4.8) | 13 (9.7) | 8 (5.5) | |
| Yes | 683 (94.5) | 198 (95.2) | 120 (90.2) | 137 (94.5) | |
|
| |||||
| Age First Tried Tobaccob [mean (SD)] | 14.2 (5.4) | 12.7 (4.6) | 14.3 (4.3) | 13.7 (5.9) | .030 |
| Age Began Regular Useb [mean (SD)] | 17.9 (5.6) | 17.1 (5.9) | 18.2 (5.6) | 17.4 (5.8) | 1.000 |
| Years Consumed Tobacco [mean (SD)] | 32.5 (14.5) | 33.3 (17.1) | 29.1 (16.1) | 27.4 (15.9) | .009 |
| Years Consumed Productc [mean (SD)] | 32.4 (14.5) | 27.0 (15.7) | 2.4 (1.6) | 27.4 (15.9) | < .001 |
| Time to First Use, Minutes | < .001 | ||||
|
| |||||
| >30 | 254 (35.3) | 125 (60.1) | 60 (45.8) | 51 (35.2) | |
| ≤0 | 466 (64.7) | 83 (39.9) | 71 (54.2) | 94 (64.8) | |
|
| |||||
| Cessation Interestd [mean (SD)] | 6.2 (3.1) | 5.4 (3.0) | 5.9 (3.2) | 6.8 (3.0) | 1.000 |
| Stage of Change | .179 | ||||
|
| |||||
| Pre-Contemplation | 371 (59.0) | 127 (73.0) | 83 (69.8) | 67 (54.0) | |
| Contemplation | 222 (35.3) | 43 (24.7) | 30 (25.2) | 50 (40.3) | |
| Preparation | 36 (5.7) | 4 (2.3) | 6 (5.0) | 7 (5.7) | |
|
| |||||
| Previous Quit Attempts in Past Year | < .001 | ||||
|
| |||||
| one | 496 (68.5) | 151 (72.6) | 126 (94.7) | 79 (54.5) | |
| 1–4 | 180 (24.9) | 51 (24.5) | 6 (4.5) | 52 (35.9) | |
| ≥5 | 48 (6.6) | 6 (2.9) | 1 (0.8) | 14 (9.7) | |
|
| |||||
| Other Household Tobacco Users | < .001 | ||||
|
| |||||
| No | 434 (59.9) | 179 (86.1) | 100 (75.2) | 87 (60.0) | |
| Yes | 290 (40.1) | 29 (13.9) | 33 (24.8) | 58 (40.0) | |
|
| |||||
| Binge Drinking | .003 | ||||
|
| |||||
| No | 525 (75.0) | 120 (58.5) | 94 (73.4) | 97 (70.3) | |
| Yes | 175 (25.0) | 85 (41.5) | 34 (26.6) | 41 (29.7) | |
|
| |||||
| Work Indoor Air Restrictions | 1.000 | ||||
|
| |||||
| Never Allowed | 312 (88.9) | 101 (89.4) | 73 (94.8) | 57 (85.1) | |
| Sometimes allowed | 27 (7.7) | 10 (8.9) | 1 (1.3) | 8 (11.9) | |
| Always allowed | 12 (3.4) | 2 (1.8) | 3 (3.9) | 2 (3.0) | |
Note.
Bonferroni-adjusted
p-value is based on a log transformation
The reported p-value excludes ENDS users (3 separate tests comparing ENDS users to each of the other products all result in p-values < .001)
Cessation interest was measured on a scale of 0 (least likely) to 10 (most likely)
DISCUSSION
In this paper, we outline the baseline characteristics of participants recruited into a new and ongoing prospective cohort of adult tobacco users in urban and rural Appalachian Ohio. Participants in this study differed in regard to a number of baseline tobacco-related behaviors and characteristics by region of residence as well as by type of tobacco products used.
In this study, racial differences in the geographic samples were pronounced. Appalachian participants were almost exclusively Caucasian, whereas a much larger proportion of non-white (predominantly African-American) participants were recruited from urban residents. Indeed, our recruitment of 2.4% African-American participants in the 6 Appalachian counties closely approximates the 2.6% proportion of African Americans in the same counties, according to US Census estimates.47 Similarly, 23.4% of our urban participants were African-American, which somewhat exceeds the census estimates of 21.2%.47 However, in the urban Franklin county, Asian/Pacific Islanders constitute 4.9% of residents, which is notably higher than the 0.7% that we recruited.47
We also observed significant differences in education and income among recruitment regions. Urban participants tended to have higher education and higher household incomes than rural participants. These differences, too, reflect those of the source populations. In the 6 Appalachian counties, 11.4% to 16.6% of residents hold a Bachelor’s degree and the median household incomes ranged between $37,000 and $45,000.47 This is in stark contrast to Census estimates for Franklin County, among which 36.7% hold a Bachelor’s degree and the median household income is approximately $52,000.47 The reasons behind these differences, broadly include that Franklin County boasts a strong economy and includes several colleges and OSU, which attract and maintain a diverse student body; whereas the Appalachian region is in economic distress and does not include many institutes of higher learning.48
We found that ENDS and dual users were younger than users of SLT or combustible tobacco products, that SLT users were almost exclusively male, and that users of combustible tobacco products were more likely to be non-white than users of SLT, ENDS, or dual products. The distributions of these characteristics in the current study are consistent with tobacco control literature. For instance, in the National Adult Tobacco Survey (NATS), ENDS users were 167% more likely to be <45 years of age (versus ≥45), whereas users of combustible tobacco products were only 54% more likely to be in the <45 year age group.49 In agreement with our results, SLT users were 16 times more likely to be male than female,50,51 and the prevalence of use of combustible tobacco products, SLT, and ENDS was 23.5%, 2.1%, and 1.1%, respectively, among African Americans (estimates were similar for His-panics and ‘Other non-Hispanic’ racial groups).49
Given the recruitment criteria, nearly all participants in our study used tobacco products daily. On average, tobacco product use began at 17 years and most used tobacco within 30 minutes of waking. The high prevalence of daily tobacco use (>94%) in this study is higher than the 75.4% cigarette smoking prevalence among adults who reported tobacco use at least some days in the NATS.52 The discrepancy between our study and the NATS may be explained in part by geography. For instance, the prevalence of daily use of cigarettes among individuals living in Ohio who smoked at least some days each week was 88.2% using 2011 United States Census-Tobacco Use Supplement.53 In further contrast to national studies, the mean age at initiation among tobacco users was older (eg, average age at initiation among current tobacco users ≥ some days is 15.6 years in the NATS).52 In agreement with national data, in this study 59% used tobacco within 30 minutes of waking; this estimate is similar (58%) to that found in the NATS.52
We also observed differences in tobacco-related characteristics by study region. Urban participants were less likely to use tobacco daily, began using tobacco later in life, and used tobacco for a shorter amount of time. However, comparisons to existing data are challenging as most studies have not examined differences in tobacco-related characteristics by region and none have examined these characteristics contrasting Appalachian and urban areas. The finding that urban participants were less likely to use tobacco products daily is similar to those from the 2011 US Census-Tobacco Use Supplement. Among Ohio smokers who smoked at least some days each week, the proportion of daily smokers was lower among those living in metropolitan areas (85.6%) versus non-metropolitan areas (93.10%).53
In this study, 54%–65% of users of combustible, ENDS, and dual products used tobacco within 30 minutes of waking. These findings are like another report in a multiethnic online national survey,54 in which 56% of combustible users and 64.8% of dual (combustible plus ENDS) users reported tobacco use within 30 minutes of waking. Importantly, 95% of exclusive ENDS users had no quit attempts in the past year. This prevalence (5%) of quit attempts appears low, but comparisons to prior reports are difficult as others have examined quit attempts among dual tobacco product users where the ENDS product was considered a cessation aid for other tobacco.54,55 In the multiethnic online survey, Pulvers et al54 report 66.7% of dual combustible/ENDS users made attempts to quit in the last year. In a separate national survey, Rutten et al,55 report 82% of dual combustible/ ENDS users had made quit attempts.
The strengths of this study include the creation and maintenance of a large cohort of adult tobacco users that will provide crucial data on tobacco use over time. Importantly, follow-up data will allow us to examine associations of baseline cognitive, affective and purchasing factors related to tobacco product preferences with uptake of novel products and cessation interest, attempts and successful quitting. The inclusion of urban and rural community residents will allow for characterization of these factors within their regional context. This feature is critical to understanding use in a state with a high prevalence of consumption and tobacco-attributable diseases. This cohort study has demonstrated success in enrolling participants from both rural Appalachian and urban Ohio populations, as well as with users of several tobacco product types. Our goal of 21% response rate was reached, and we have further achieved, and thus far, maintained an excellent participation rate (93% at 18 months). We owe the success of our enrollment strategy to the utilization of local interviewers (particularly for Appalachian participants) and the use of financial incentives that were used in the initial mailings and for completion of the baseline interview. A potential limitation of this research is the lack of generalizability to a nationally representative population. It is our intent to continue to compare our findings to those of other national samples, including the PATH study.13 It should be acknowledged that we defined current users of tobacco products at baseline to be those who used tobacco at least some days each week; therefore, comparisons to other studies that defined current use differently may be challenging.
Other future plans include the expansion and continued surveillance of the established cohort. As an important next step, we have added a subsample of the cohort to provide non-invasive biomarkers of nicotine dependence (ie, nicotine metabolite ratio), tobacco-specific carcinogens (ie, NNAL) and respiratory-related disease, such as asthma (ie, fractional exhaled nitric oxide). Quantification of these biomarkers in each of the 4 groups of current tobacco users will inform a discussion of the potential risks and benefits of specific product use. We are especially interested in the adoption of new products, such as the transition from combustible products to exclusive ENDS use. We also anticipate learning whether this type of transition assists the participant to permanently quit using tobacco. Also, to improve understanding of how marketing of tobacco products influences purchasing behavior, we have initiated another sub-study that collects cognitive and behavioral information during participant’s actual tobacco product purchases, via ecological momentary assessment. Here, all 4 tobacco product user types will be enrolled in a 3-year longitudinal study.
In conclusion, the establishment of this cohort of adult current combustible, SLT, dual, and ENDS users has allowed us to identify and compare factors associated with tobacco product preferences and the use of new and emerging products. Future studies will focus on the associations of cognitive and affective, and purchasing factors with the use of specific products. We have provided information to ascertain whether the magnitude of these associations differ by urban versus rural regions in the state of Ohio. Importantly, the inclusion of rural Appalachia, a region with a high prevalence of consumption and disease burden, may provide additional insights into the implementation of tobacco control interventions among a special population of tobacco product users.
IMPLICATIONS FOR TOBACCO REGULATION
Surveillance of the diversity of tobacco products used may assist in determining: (1) additional products derived from tobacco over which FDA may choose to exert (deem) its jurisdiction; (2) regulations and other restrictions to be applied to the marketing of such newly-deemed tobacco products; and, (3) sales and marketing regulations to be applied to tobacco products currently subject to FDA jurisdiction under § 906d and § 907 of the Tobacco Control Act.
Supplementary Material
Acknowledgments
This research is supported by grant P50CA180908 from the National Cancer Institute of the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) Center for Tobacco Products. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Footnotes
Human Subjects Statement
All participants gave informed consent to participate in the Tobacco User Adult Cohort. All study protocols were approved by the Institutional Review Board of The Ohio State University (2014C0029).
Conflict of Interest Statement
Dr Brasky has served as a statistical consultant for the plaintiffs in class-action lawsuits against tobacco companies. Dr Shields has served as an expert witness for the plaintiffs in class-action lawsuits against tobacco companies.
Contributor Information
Theodore M. Brasky, Assistant Professor, Division of Cancer Prevention and Control, The Ohio State University College of Medicine, Columbus, OH.
Alice Hinton, Clinical Research Data Manager, The Ohio State University Center of Excellence in Regulatory Tobacco Science, Columbus, OH.
Nathan J. Doogan, Post-doctoral Fellow, The Ohio State University Center of Excellence in Regulatory Tobacco Science, Columbus, OH.
Sarah E. Cooper, Program Manager, The Ohio State University Center of Excellence in Regulatory Tobacco Science, Columbus, OH.
Haikady N. Nagaraja, Professor, Division of Biostatistics, The Ohio State University College of Public Health, Columbus, OH.
Wenna Xi, Research Associate, Division of Biostatistics, The Ohio State University College of Public Health, Columbus, OH.
Peter G. Shields, Professor, The Ohio State University Center of Excellence in Regulatory Tobacco Science, Columbus, OH.
Mary Ellen Wewers, Professor, The Ohio State University Center of Excellence in Regulatory Tobacco Science, Columbus, OH.
References
- 1.Herzog B, Gerberi J, Scott A. [Accessed September 18, 2017];Tobacco-Nielsen C-store data-e-cig $ sales decline moderates. 2014 Available at: http://www.c-storecanada.com/attachments/article/153/Nielsen%20C-Stores%20-%20Tobacco.pdf.
- 2.McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U.S. adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17(10):1195–1202. doi: 10.1093/ntr/ntu213. [DOI] [PubMed] [Google Scholar]
- 3.Cullen J, Mowery P, Delnevo C, et al. Seven-year patterns in US cigar use epidemiology among young adults aged 18–25 years: a focus on race/ethnicity and brand. Am J Public Health. 2011;101(10):1955–1962. doi: 10.2105/AJPH.2011.300209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson A, Xiao H, Vallone DM. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob Res. 2012;14(8):927–932. doi: 10.1093/ntr/ntr306. [DOI] [PubMed] [Google Scholar]
- 5.Backinger CL, Fagan P, O’Connell ME, et al. Use of other tobacco products among U.S. adult cigarette smokers: prevalence, trends and correlates. Addict Behav. 2008;33(3):472–489. doi: 10.1016/j.addbeh.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bombard JM, Pederson LL, Koval JJ, et al. How are lifetime polytobacco users different than current cigarette-only users? Results from a Canadian young adult population. Addict Behav. 2009;34(12):1069–1072. doi: 10.1016/j.addbeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: findings from national surveys. Tob Control. 2010;19(2):104–109. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Connor RJ. Postmarketing surveillance for “modified-risk” tobacco products. Nicotine Tob Res. 2012;14(1):29–42. doi: 10.1093/ntr/ntq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mejia AB, Ling PM. Tobacco industry consumer research on smokeless tobacco users and product development. Am J Public Health. 2010;100(1):78–87. doi: 10.2105/AJPH.2008.152603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hajek P, Etter JF, Benowitz N, et al. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–1810. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatsukami DK, Ebbert JO, Feuer RM, et al. Changing smokeless tobacco products new tobacco-delivery systems. Am J Prev Med. 2007;33(6 Suppl):S368–S378. doi: 10.1016/j.amepre.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Zeller M, Hatsukami D. The strategic dialogue on tobacco harm reduction: a vision and blueprint for action in the US. Tob Control. 2009;18(4):324–332. doi: 10.1136/tc.2008.027318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):371–378. doi: 10.1136/tobaccocontrol-2016-052934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. doi: 10.1056/NEJMsa1607538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ayers JW, Leas EC, Allem JP, et al. Why do people use electronic nicotine delivery systems (electronic cigarettes)? A content analysis of Twitter, 2012–2015. PLoS One. 2017;12(3):e0170702. doi: 10.1371/journal.pone.0170702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernat JK, Ferrer RA, Margolis KA, et al. US adult tobacco users’ absolute harm perceptions of traditional and alternative tobacco products, information-seeking behaviors, and (mis)beliefs about chemicals in tobacco products. Addict Behav. 2017;71:38–45. doi: 10.1016/j.addbeh.2017.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hershberger AR, Karyadi KA, VanderVeen JD, et al. Beliefs about the direct comparison of e-cigarettes and cigarettes. Subst Use Misuse. 2017;52(8):982–991. doi: 10.1080/10826084.2016.1268628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel D, Davis KC, Cox S, et al. Reasons for current e-cigarette use among U.S. adults. Prev Med. 2016;93:14–20. doi: 10.1016/j.ypmed.2016.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kram Y, Klesges RC, Ebbert JO, et al. Dual tobacco user subtypes in the U.S. Air Force: dependence, attitudes, and other correlates of use. Nicotine Tob Res. 2014;16(9):1216–1223. doi: 10.1093/ntr/ntu056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee YO, Hebert CJ, Nonnemaker JM, et al. Multiple tobacco product use among adults in the United States: cigarettes, cigars, electronic cigarettes, hookah, smokeless tobacco, and snus. Prev Med. 2014;62:14–19. doi: 10.1016/j.ypmed.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 21.Sung HY, Wang Y, Yao T, et al. Polytobacco use of cigarettes, cigars, chewing tobacco, and snuff among US adults. Nicotine Tob Res. 2016;18(5):817–826. doi: 10.1093/ntr/ntv147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen K, Marshall L, Hu S, et al. State-specific prevalence of current cigarette smoking and smokeless tobacco use among adults aged >/=18 years - United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2015;64(19):532–536. [PMC free article] [PubMed] [Google Scholar]
- 23.Roberts ME, Doogan NJ, Kurti AN, et al. Rural tobacco use across the United States: how rural and urban areas differ, broken down by census regions and divisions. Health Place. 2016;39:153–159. doi: 10.1016/j.healthplace.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doogan NJ, Roberts ME, Wewers ME, et al. A growing geographic disparity: rural and urban cigarette smoking trends in the United States. Prev Med. 2017 Mar 16; doi: 10.1016/j.ypmed.2017.03.011. pii: S0091-7435(17)30106-8 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu L, Edland S, Myers MG, et al. Smoking prevalence in urban and rural populations: findings from California between 2001 and 2012. Am J Drug Alcohol Abuse. 2016;42(2):152–161. doi: 10.3109/00952990.2015.1125494. [DOI] [PubMed] [Google Scholar]
- 26.Holt JB, Zhang X, Presley-Cantrell L, et al. Geographic disparities in chronic obstructive pulmonary disease (COPD) hospitalization among Medicare beneficiaries in the United States. Int J Chron Obstruct Pulmon Dis. 2011;6:321–328. doi: 10.2147/COPD.S19945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ohio Cancer Incidence Surveillance System – Ohio Department of Health. Lung & bronchus cancer in Ohio, 2008–2013. Ohio Department of Health and The Ohio State University; 2016. [Accessed September 18, 2017]. Available at: https://www.odh.ohio.gov/-/media/ODH/ASSETS/Files/health/OCISS/LungBronchProfile_Final.pdf?la=en. [Google Scholar]
- 28.Ohio Colleges of Medicine Government Resource Center. [Accessed September 18, 2017];The 2010 Ohio Family Health Survey: final data set. 2010 Available at: http://grc.osu.edu/OMAS/2010Survey.
- 29.United States Census Bureau. [Accessed September 18, 2017];2010 census urban and rural classification and urban area criteria. 2010 Available at: https://www.census.gov/geo/reference/ua/urban-rural-2010.html.
- 30.Brick JM, Williams D, Montaquila JM. Address-based sampling for subpopulation surveys. Public Opin Q. 2011;75(3):409–428. [Google Scholar]
- 31.United States Postal Service. [Accessed September 18, 2017];CDS user guide. 2016 Available at: https://ribbs.usps.gov/cds/documents/tech_guides/CDS_USER_GUIDE.PDF.
- 32.United States Institute of Medicine Committee on the Assessment of Asthma and Indoor Air. [Accessed September 18, 2017];Clearing the air: asthma and indoor air exposures. 2000 Available at: https://www.nap.edu/catalog/9610/clearing-the-air-asthma-and-indoor-air-exposures.
- 33.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heatherton TF, Kozlowski LT, Frecker RC, et al. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 35.Ferketich AK, Wee AG, Shultz J, et al. A measure of nicotine dependence for smokeless tobacco users. Addict Behav. 2007;32(9):1970–1975. doi: 10.1016/j.addbeh.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prochaska JO, Velicer WF. The Transtheoretical Model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 37.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 38.Abrams DB, Niaura R, Brown RA, et al. The Tobacco Dependence Treatment Handbook: A Guide to Best Practices. New York, NY: The Guilford Press; 2003. [Google Scholar]
- 39.United States Department of Labor, Bureau of Labor Statistics. Current Population Survey. [Accessed September 18, 2017];Design and Methodology (Technical Paper 63RV) 2002 Available at: https://www.census.gov/prod/2002pubs/tp63rv.pdf.
- 40.Dillard AJ, McCaul KD, Klein WM. Unrealistic optimism in smokers: implications for smoking myth endorsement and self-protective motivation. J Health Commun. 2006;11(Suppl 1):93–102. doi: 10.1080/10810730600637343. [DOI] [PubMed] [Google Scholar]
- 41.Haddock CK, Lando H, Klesges RC, et al. Modified tobacco use and lifestyle change in risk-reducing beliefs about smoking. Am J Prev Med. 2004;27(1):35–41. doi: 10.1016/j.amepre.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 42.Liu ST, Nemeth JM, Klein EG, et al. Adolescent and adult perceptions of traditional and novel smokeless tobacco products and packaging in rural Ohio. Tob Control. 2014;23(3):209–214. doi: 10.1136/tobaccocontrol-2012-050470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martino SC, Scharf DM, Setodji CM, et al. Measuring exposure to protobacco marketing and media: a field study using ecological momentary assessment. Nicotine Tob Res. 2012;14(4):398–406. doi: 10.1093/ntr/ntr223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Naimi TS, Brewer RD, Mokdad A, et al. Binge drinking among US adults. JAMA. 2003;289(1):70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 45.Wechsler H, Nelson TF. Binge drinking and the American college student: what’s five drinks? Psychol Addict Behav. 2001;15(4):287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- 46.American Association for Public Opinion Research. [Accessed September 18, 2017];Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. (9). 2016 Available at: http://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf.
- 47.United States Census Bureau. [Accessed September 18, 2017];QuickFacts 2015. 2015 Available at: http://www.census.gov/quickfacts.
- 48.Ohio Department of Higher Education. [Accessed September 18, 2017];Ohio public institutions - map and school profiles. 2017 Available at: https://www.ohiohighered.org/campuses/map.
- 49.Hu SS, Neff L, Agaku IT, et al. Tobacco product use among adults - United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65(27):685–691. doi: 10.15585/mmwr.mm6527a1. [DOI] [PubMed] [Google Scholar]
- 50.King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. doi: 10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults--United States, 2012–2013. MMWR Morb Mortal Wkly Rep. 2014;63(25):542–547. [PMC free article] [PubMed] [Google Scholar]
- 52.US Centers for Disease Control and Prevention. [Accessed September 18, 2017];National Adult Tobacco Survey 2013–2014. 2017 Available at: http://www.cdc.gov/tobacco/data_statistics/surveys/nats/
- 53.The Interuniversity Consortium for Political and Social Research. [Accessed September 18, 2017];Current Population Survey Tobacco Use Supplement (TUS), 2010–2011 Wave: Online Analysis Tool. 2017 Available at: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/36434/datasets/0001/sdaxml.
- 54.Pulvers K, Hayes RB, Scheuermann TS, et al. Tobacco use, quitting behavior, and health characteristics among current electronic cigarette users in a national tri-ethnic adult stable smoker sample. Nicotine Tob Res. 2015;17(9):1085–1095. doi: 10.1093/ntr/ntu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rutten LJ, Blake KD, Agunwamba AA, et al. Use of e-cigarettes among current smokers: associations among reasons for use, quit intentions, and current tobacco use. Nicotine Tob Res. 2015;17(10):1228–1234. doi: 10.1093/ntr/ntv003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.