Abstract
We examined beliefs about genetically targeted care (GTC) among African American men and women in a hospital-based sample and identified sociodemographic, cultural, and clinical factors having significant independent associations with these beliefs. Specifically, beliefs about GTC were evaluated after respondents were randomly primed with a racial or non-racial cue about race and genetics. Despite priming with a racial or non-racial cue, many respondents had positive beliefs about GTC. But, 49% believed that GTC would limit access to medical treatment, 46% believed that people will not trust GTC, and 20% believed that people like them would not benefit from GTC. Racial and non-racial priming did not have significant associations with negative beliefs about GTC. However, cultural beliefs related to temporal orientation were associated significantly with believing that genetically targeted care will limit access to medical treatment. Greater levels of future temporal orientation were associated with a reduced likelihood of endorsing this belief (OR = 0.70, 95% CI = 0.49, 1.01, p = 0.05). Respondents who had a chronic medical condition had an almost three-fold greater likelihood of believing that they would not benefit from GTC (OR = 2.90, 95% CI = 1.00, 8.37, p = 0.05). Greater exposure to information about genetic testing for chronic conditions was also associated with a reduced likelihood of believing that they would not benefit from GTC (OR = 0.40, 95% CI = 0.64, 0.91, p = 0.02). African Americans have diverse beliefs about GTC that should be considered as genetic and genomic services are offered.
Keywords: African American, Beliefs, Genetically targeted, Medical care
INTRODUCTION
Since the completion of the Human Genome Project, efforts have been directed towards developing strategies to translate and integrate genomic information into clinical practice and population health.1 One of the best examples of this is genetic counseling and testing for BRCA1 and BRCA2 (BRCA1/2) mutations, which are associated with breast cancer. It is now possible for women to learn if they have a deleterious BRCA1/2 mutation and to use this information to make informed decisions about risk reduction and management strategies.2–7 To date, many women have had genetic counseling and testing for BRCA1/2 mutations and these services are now the standard of care for women who have a personal or family history of breast cancer that is suggestive of hereditary disease. However, many unanswered questions remain about genetic factors involving other chronic diseases and research is being conducted to understand the contribution of these factors to conditions such as cardiovascular disease, diabetes, and obesity.8–10 It is anticipated that these discoveries will be translated into clinical practices and be used to develop personalized approaches for treatment and management of disease.11 Reducing racial and ethnic disparities in morbidity and mortality from chronic diseases is an expected outcome of personalized approaches for disease treatment and management. However, racial and ethnic minorities may have concerns about personalized approaches; less than one-third of African American women at increased risk for hereditary breast cancer received BRCA1/2 test results.3
Attempts to develop a better understanding of barriers and facilitators to utilization of personalized approaches to medical care and disease prevention among African Americans have explored beliefs and attitudes about race-based medicine. For instance, African Americans were concerned that use of genetic technologies in medical care would result in racial discrimination and a permanent genetic underclass that would further exacerbate unequal access to medical care.12 In another study, Bevan and colleagues found that African Americans were significantly more concerned about race-based prescription drugs in comparison to whites, and African Americans also expressed concerns that race-based medicine is akin to racial profiling, which may increase medical distrust.13 But, beliefs and attitudes about genetically targeted care may differ from those about race-based medicine. Studies have shown that African Americans have favorable attitudes about genetic testing for inherited breast cancer risk14,15 and qualitative research has shown that some African Americans believe that individualized genetic testing will result in the best quality of care.13 However, quantitative data are not available on how these beliefs might differ among African Americans and whether or not beliefs vary as a function of an individual’s cultural values, health care experiences, and socioeconomic background. Attitudes about race-based medicine, and potential predictors of these beliefs, have been explored primarily in qualitative studies that were interested in racial differences between African Americans and whites.12,13
To extend these studies, we completed a hospital-based survey with adult African American men and women to evaluate their beliefs about genetically targeted medical care. In this report, we describe the extent to which African Americans believed that genetically targeted care would result in positive (e.g., improved medical care) and negative (e.g., distrust, limited access) outcomes. Since prior reports have shown that African Americans and whites differ in their belief about race-based medicine,12,13 we sought to determine if beliefs about genetically targeted care differed based on whether respondents were primed with a racial or non-racial cue about race and genetics and examined the relationship between these beliefs and cultural values, clinical factors, and sociodemographic characteristics to identify factors that have a significant independent association with beliefs about genetically targeted care. Since qualitative studies have shown that individuals use religious frameworks to understand disease and these frameworks are important to beliefs about the roles that genetics play in health outcomes,16,17 we were particularly interested in the relationship between religious and spiritual values and beliefs about genetically targeted care. We predicted that individuals with greater religious values would be most likely to expect negative outcomes of genetically targeted medical care. We also evaluated the relationship between future temporal orientation and beliefs about genetically targeted care. Temporal orientation, or preferences to focus on past, present, and future implications and consequences, is one of the primary contexts through which individuals understand and give meaning to their experiences. Previous research has shown that future temporal orientation is positively associated with acceptance of genetic counseling for inherited cancer risk18; we hypothesized that future temporal orientation would be associated significantly with positive expectations about genetically targeted care.
MATERIALS AND METHODS
Sample characteristics
The study was approved by the Institutional Review Boards at the University of Pennsylvania and the Medical University of South Carolina. Respondents were African American men and women who had seen a primary care provider at the University of Pennsylvania. We identified a random sample of 2062 patients from a billing database managed by the Office of Research and of these, 298 were screened for eligibility. Of the 298 who were screened, 206 (69%) were eligible and completed the survey. To be included in the study, individuals had to be at least age 18 years and be able to speak English. We excluded individuals who were currently participating in a research study. Respondents who were missing data on beliefs about genetically targeted care were also excluded from the analysis; thus the final sample included 152 respondents.
Procedures
Patients were invited to participate in the study using a mailed invitation that described the purpose of the study and the procedures involved in participation. A self-addressed reply card was included in the invitation letter for individuals to return if they did not want to be contacted. Individuals who did not opt out at this point were contacted to complete a 40-min structured telephone survey. Following provision of verbal consent, a screening interview was completed and those who were eligible completed the telephone survey to obtain sociodemographic information and clinical experiences and to evaluate exposure to information about genetics, cultural factors, and beliefs about genetically targeted care. Patients who completed the survey were mailed a $20 gift certificate.
MEASURES
Sociodemographic factors
We obtained race, gender, marital status, education level, employment status, and income level by self-report during the interview. Respondents were also asked to indicate their usual source of health care (e.g., doctor’s office or some other type of place).
Clinical factors
We obtained personal history of cancer and family history of disease using items from our previous research.19 Specifically, respondents were asked if they had ever been diagnosed with cancer (yes or no). We used a similar item to determine if respondents had a first-degree relative who had been diagnosed with cancer. Lastly, respondents were asked if they had ever been diagnosed with diabetes, hypertension, heart problems, or arthritis. Those who reported yes to any of these conditions were categorized as having a chronic condition and those who reported no for all of these conditions were categorized as not having a chronic condition.
Exposure to information about genetics
We adapted items from previous research14 to evaluate exposure to information about genetic factors involved in chronic disease. Specifically, respondents were asked, “Before this survey, how much they had heard or read about genes involved in cancer, heart disease, hypertension, and diabetes (1 = almost nothing, 2 = a little bit, 3 = a fair amount, 4 = a lot).” We summed these items to create an exposure to genetics scale; higher scores reflected greater exposure. This scale had good internal consistency (Cronbach’s alpha = 0.83).
Cultural factors
We used the temporal orientation and religiosity scales developed by Lukwago and colleagues to evaluate future temporal orientation and religious and spiritual values.20 The religiosity scale asked respondents to indicate how much they agree (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree) with items such as: that they have a personal relationship with God, pray for healing when ill, and their spiritual beliefs are the foundation to their whole approach to life. Items for future temporal orientation asked respondents to indicate how much they agree that: “the choices I have made in life clearly show that I think about the future, I often think about how my actions today will affect my health when I am older, and I have a plan for what I want to do in the next 5 years of my life.” Higher scores indicated greater endorsement of religiosity and future temporal orientation. These instruments had acceptable internal consistency in our sample (Cronbach’s alpha = 0.68 for future temporal orientation and 0.89 for religiosity).
Beliefs about genetically targeted medical care
We used Likert-style items to evaluate beliefs about genetic targeted care. These items were developed by investigators at the Annenberg School for Communication at the University of Pennsylvania and asked respondents about positive and negative outcomes of genetically targeted care. First, respondents were read a brief statement to describe how genetic information may be used in health care: “Doctors are using genetics as the basis for screening, diagnosis, and prescribing medication. This practice is called genetically targeted care. Because of their genetics, people respond better or worse than others to certain medications and medical treatments. Some say that genetically targeted care will discriminate against people that are less responsive to medications and limit their access to medical treatment. Others say that using genetics to personalize medicine is a good way to tailor treatment to individuals and improve their overall medical care.” Then respondents were asked to select one of the following statements that come closest to their view: (1) genetically targeted care will improve people’s overall medical care and (2) genetically targeted care will discriminate against people that are less responsive to medical treatment.
Respondents were then asked about their beliefs about genetically targeted care using five Likert-style items. Specifically, respondents were asked the following questions: (1) genetically targeted care is a good way to personalize medicine, (2) genetically targeted care will limit some people’s access to medical treatment, (3) people like me will not benefit from genetically targeted care, (4) people will not trust genetically targeted care, (5) it is a good idea to get a genetic test to find out how a person will respond to medical treatment (1 = strongly disagree, 2 = somewhat disagree, 3 = neither agree nor disagree, 4 = somewhat agree, 5 = strongly agree). These items had acceptable face validity and were included in this study based on expected outcomes of genetically targeted medical care11 and beliefs and attitudes about different approaches for integrating genomics into medical care.13–15 Items on genetically targeted care were administered after respondents were randomly assigned to be primed for a racial or non-racial cue. The racial cue read as: “Some doctors are using race as a substitute for individual genetic profiles because it is too costly and difficult to obtain genetic profiles for each of their patients. In the absence of genetic testing, race is an alternate way to provide patients with genetically targeted care because people of the same racial group tend to share many of the same genes.” The non-racial cue read as: “Some doctors are using individual genetic profiles to customize medical care to each of their patients. Although genetic testing may be costly and difficult to obtain, it is a valuable way to provide each patient with genetically targeted care because everyone has a unique genetic makeup.” The priming statements and description of genetically targeted care were also developed by investigators at the Annenberg School for Communication.
Data analysis
First, we generated descriptive statistics to characterize respondents in terms of sociodemographic factors and beliefs about genetically targeted care. Next, we used Chi Square Tests of Association and t-tests to evaluate the bivariate relationship between beliefs about genetically targeted care and sociodemographic factors, clinical experiences, exposure to information about genetics, and cultural factors. We then used multivariate logistic regression analysis to identify factors having significant independent associations with beliefs about genetically targeted care. Variables that had a p < 0.10 association with beliefs about genetically targeted care in the bivariate analyses were included in the regression model.
RESULTS
Table 1 shows the characteristics of our sample. Most respondents were female (56%), were not married (64%), had some college education or were college graduates (59%), and were not employed (51%). Forty-one percent of respondents had a family history of cancer and 68% had a personal history of a chronic disease (68%). The mean (SD) age of respondents was 48.6 (14.4). When given a choice to select a statement that most closely reflected their views on how genetic information may be used in health care, 68% of respondents chose “genetically targeted care will improve people’s overall medical care” and 32% chose “genetically targeted care will discriminate against people who are less responsive to medical treatment.” Consistent with this, respondents were most likely to endorse items that measured positive outcomes of genetically targeted care. As shown in Fig. 1, 78% of respondents agreed or strongly agreed that it is a good idea to have a genetic test to determine how a person will respond to medical treatment and 68% agreed or strongly agreed that genetically targeted care is a good way to personalize medicine. At the same time, however, a substantial minority of respondents agreed that genetically targeted care will limit access to medical treatment (49% agreed or strongly agreed) and that people will not trust genetically targeted care (46% agreed or strongly agreed). Twenty percent of respondents agreed or strongly agreed that people similar to them would not benefit from genetically targeted care. Since there was limited variability in responses to items that asked about positive beliefs about genetically targeted care, our subsequent analyses focused on items that asked about negative beliefs about how genetic information may be used in health care. We re-coded these items into dichotomous variables (strongly agree/agree versus strongly disagree/disagree/neutral) for these analyses.
Table 1.
Sample characteristics (n = 152).
| Variable | Level | n(%) |
|---|---|---|
| Gender | Female | 85 (56%) |
| Male | 67 (44%) | |
|
| ||
| Marital status | Not married | 98 (64%) |
| Married | 54 (36%) | |
|
| ||
| Education level | ≥Some college | 90 (59%) |
| ≤High school | 62 (41%) | |
|
| ||
| Employment status | Employed | 74 (49%) |
| Not employed | 77 (51%) | |
|
| ||
| Income levela | >$35,000 | 72 (53%) |
| ≤$35,000 | 65 (47%) | |
|
| ||
| Personal cancer history | Yes | 14 (9%) |
| No | 138 (91%) | |
|
| ||
| Family history of cancera | Yes | 62 (41%) |
| No | 90 (59%) | |
|
| ||
| Personal history of chronic disease | Yes | 102 (68%) |
| No | 49 (32%) | |
|
| ||
| Health insurance | Yes | 139 (91%) |
| No | 13 (9%) | |
|
| ||
| Setting for usual source of health care | Doctor’s office | 138 (91%) |
| Other type of facility | 14 (9%) | |
|
| ||
| Previous research participation | Yes | 58 (38%) |
| No/don’t know | 94 (62%) | |
|
| ||
| Priming cue | Racial | 73 (48%) |
| Non-racial | 79 (52%) | |
|
| ||
| Age | Mean (SD) | 48.6 (14.4) |
|
| ||
| Exposure to information about genetics | Mean (SD) | 13.8 (4.2) |
|
| ||
| Religiosity | Mean (SD) | 27.7 (4.9) |
|
| ||
| Future temporal orientation | Mean (SD) | 15.5 (2.4) |
|
| ||
| Present temporal orientation | Mean (SD) | 9.1 (2.5) |
15 respondents refused to provide income; 1 refused to provide employment status; 1 refused to provide information on chronic diseases.
Figure 1.
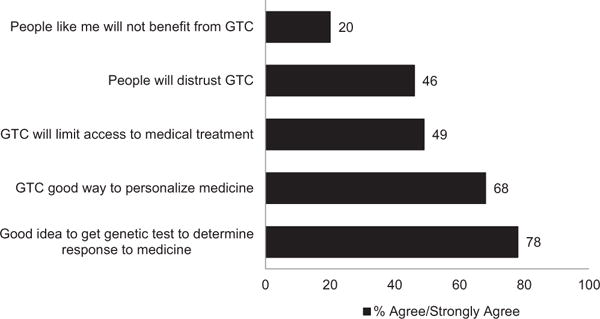
Descriptive information on beliefs about genetically targeted care (GTC).
Table 2 shows the results of the bivariate analysis of items that measured negative beliefs about genetically targeted care. There were no differences in responses to any of these items after priming using the racial and non-racial cues. However, respondents who had some college education or were college graduates were significantly more likely than those with fewer years of formal education to agree that genetically targeted care will limit access to medical treatment (p = 0.03). Respondents who were employed and those who usually received medical care at a doctor’s office were also likely to endorse this belief, but these associations were marginally significant (p = 0.06). Respondents who endorsed this belief also had lower levels of future temporal orientation compared to those who disagreed (Table 3) (p = 0.10). Different variables were associated significantly with beliefs about benefitting from genetically targeted care. Specifically, men were more likely than women to believe that people like them would not benefit from genetically targeted care (p = 0.05). In addition, respondents who had a chronic condition were more likely than those who did not have a chronic disease to report this belief (Table 2) (p = 0.05). Respondents who agreed that they would not benefit from genetically targeted care had significantly less exposure to information about genetic testing for chronic diseases compared to those who did not hold this belief (p = 0.02). None of the sociodemographic, clinical, or cultural factors were associated significantly with distrust of genetically targeted care (Tables 2 and 3).
Table 2.
Bivariate analysis of beliefs about genetically targeted care.
| Variable | Level | Beliefs about limited access to treatmenta | Beliefs about reduced benefitsb | ||
|---|---|---|---|---|---|
| % agree | Chi square | % agree | Chi square | ||
| Gender | Female Male |
48% 51% |
0.09 | 14% 27% |
3.84† |
|
| |||||
| Marital status | Not married Married |
48% 52% |
0.21 | 26% 16% |
2.02 |
|
| |||||
| Education level | ≥Some college ≤High school |
57% 39% |
4.74* | 17% 24% |
1.31 |
|
| |||||
| Employment status | Employed Not employed |
57% 42% |
3.48† | 20% 19% |
0.01 |
|
| |||||
| Income level† | >$35,000 ≤$35,000 |
51% 49% |
0.06 | 19% 18% |
0.02 |
|
| |||||
| Personal cancer history | Yes No |
57% 48% |
0.38 | 21% 20% |
0.02 |
|
| |||||
| Family history of cancel† | Yes No |
47% 51% |
0.28 | 24% 17% |
1.31 |
|
| |||||
| Chronic disease | Yes No |
50% 47% |
0.12 | 24% 10% |
3.79* |
|
| |||||
| Health insurance | Yes No |
49% 54% |
0.12 | 22% 0% |
3.59† |
|
| |||||
| Setting for usual source of health care | Doctor’s office Other facility |
51% 28% |
2.66† | 21% 7% |
1.54 |
|
| |||||
| Previous research participation | Yes No/don’t know |
55% 46% |
1.28 | 26% 16% |
2.22 |
|
| |||||
| Priming cue | Racial Non-racial |
54% 44% |
1.70 | 24% 15% |
1.93 |
p < 0.05;
p < 0.10.
Genetically targeted care will limit some people’s access to medical treatment.
People like me will not benefit from genetically targeted care.
Table 3.
Bivariate analysis of beliefs about genetically targeted care by cultural factors and exposure.
| Variable | Beliefs about limited access to treatmenta | t-Value | Beliefs about reduced benefitsb | t-Value | ||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||
| Agree | Disagree | Agree | Disagree | |||
| Religiosity | 27.1 (5.3) | 28.3 (4.4) | 1.48 | 28.5 (4.7) | 27.5 (5.0) | −1.00 |
|
| ||||||
| Future temporal orientation | 15.2 (2.4) | 15.8 (2.3) | 1.66† | 15.4 (2.2) | 15.5 (2.4) | 0.34 |
|
| ||||||
| Present temporal orientation | 9.0 (2.5) | 9.1 (2.6) | 0.07 | 9.2 (2.8) | 9.0 (2.5) | −0.38 |
|
| ||||||
| Exposure to genetic information | 14.2 (4.0) | 13.4 (4.4) | −1.22 | 12.2 (4.2) | 14.2 (4.1) | 2.33* |
p < 0.05;
p < 0.10.
Genetically targeted care will limit some people’s access to medical treatment.
People like me will not benefit from genetically targeted care.
The results of the multivariate logistic regression analysis of beliefs about not benefitting from genetically targeted care and the potential for genetically targeted care to limit access to treatment are reported in Table 4. Only future temporal orientation had an independent association with believing that genetically targeted care will limit access to medical treatment. Greater levels of future temporal orientation were associated with a reduced likelihood of endorsing this belief (OR = 0.70, 95% CI = 0.49, 1.01, p = 0.05). In the model of beliefs about the reduced benefits of genetically targeted care, respondents who had a chronic medical condition had an almost three-fold greater likelihood of believing that they would not benefit from this type of care (OR = 2.90, 95% CI = 1.00, 8.37, p = 0.05). Greater exposure to information about genetic testing for chronic conditions was also associated with a reduced likelihood of believing that they would not benefit from genetically targeted care (OR = 0.40, 95% CI = 0.64, 0.91, p = 0.02).
Table 4.
Multivariate regression analysis of beliefs about genetically targeted care.
| Variable | Level | OR | 95% CI | p-Value |
|---|---|---|---|---|
| Genetically targeted care will limit access to treatment | ||||
|
| ||||
| Education | ≥Some college ≤High school |
1.82 | 0.91, 3.63 | 0.09 |
|
| ||||
| Employment status | Employed Not employed |
1.75 | 0.89, 3.44 | 0.11 |
|
| ||||
| Health care | Doctor’s office Other facility |
2.81 | 0.80, 9.83 | 0.11 |
|
| ||||
| Future temporal orientation | a | 0.70 | 0.49, 1.01 | 0.05 |
|
| ||||
| People will not benefit from genetically targeted care | ||||
|
| ||||
| Gender | Male Female |
0.45 | 0.19, 1.06 | 0.07 |
|
| ||||
| Chronic condition | Yes No |
2.90 | 1.00, 8.37 | 0.05 |
|
| ||||
| Exposure to genetic information | a | 0.60 | 0.40, 0.91 | 0.02 |
Continuous variable; ORs for continuous variable reflect the OR for a 1-unit change in the covariate.
DISCUSSION
The purpose of this study was to examine beliefs about genetically targeted health care among African American men and women. Overall, respondents in this study reported positive beliefs about genetically targeted care; when given a choice, 68% indicated that genetically targeted care will improve a person’s overall medical care and only about one-third indicated that genetically targeted care would discriminate against people who are less responsive to medical treatment when given a choice between these two statements. Further, 79% of respondents agreed genetic testing is useful to determine how a person would respond to medical treatment and close to 70% agreed that genetic testing is a good strategy for personalizing medical treatment. These findings are consistent with the results of previous studies that evaluated beliefs about the benefits, limitations, and risks of specific types of genetic testing between African American and white women14 and research that examined these beliefs among African American women at increased risk for hereditary disease.15 At the same time, however, a substantial minority of respondents in this study held negative beliefs about genetically targeted care. Almost one-half of respondents agreed that genetically targeted care will limit some people’s access to medical treatment and 46% agreed that people would not trust genetically targeted care. Surprisingly, beliefs about genetically targeted care were not associated significantly with being primed with a racial or non-racial cue. This could be because African Americans already have beliefs about how race will be used in medical care from their personal experiences. Previous research has shown that non-Hispanic Blacks and Hispanics are more likely than whites to have negative perceptions about the health care system and believe that minorities receive lower quality care.21 We did not evaluate the association between negative beliefs about genetically targeted care and acceptance of genetic testing or other types of genomic medicine; this is an important issue to evaluate as part of future studies. Despite this, our research provides novel insight on African Americans who are most likely to have negative beliefs about genetically targeted care.
We found that respondents who had a chronic medical condition were about three times more likely than those who were unaffected to report that people like them will not benefit from genetically targeted care. This may be because these individuals, having already been diagnosed with a medical condition, may view genetic information as having less value. Notably, this viewpoint is an accurate understanding of susceptibility testing, where the goal is to identify one’s risk of developing a disease. For instance, individuals who had a personal history of a chronic condition were excluded from the Family Healthware Trial (FHT) because the goal of the trial was to predict one’s risk of developing diseases such as hypertension, diabetes, and cancer.22 However, the ultimate goal of genetically targeted strategies such as family health history assessment is to increase a patient’s engagement and activation in their health and health care. Excluding individuals who have a personal history of chronic diseases is inconsistent with the nature of primary care and public health practice; individuals who have a personal history of diabetes, hypertension, and other chronic diseases are not more likely than those who are unaffected to meet the guidelines for health behaviors that are recommended for disease management.23–25 To the extent that the likelihood of experiencing a negative clinical outcome (e.g., heart attack, stroke) is associated with one’s family health history, then it may be useful to consider alternate ways in which this information could be used to promote healthy behavior change among those with a personal history of chronic disease. Family health history is the most basic form of genetic information26; information about clinical outcomes among family members after they have been diagnosed with diseases such as diabetes or hypertension could be more beneficial than susceptibility to chronic conditions among populations that have high rates of chronic diseases. In our sample, 68% of respondents had a chronic disease; national data show that about one-third of African Americans have hypertension.27 Hypertension is one of the leading risk factors for adverse cardiovascular events and stroke27; family health history of heart attack and stroke after being diagnosed with hypertension and/or diabetes could encourage individuals who have chronic conditions to engage in preventive health behaviors. Genetic information may also be relevant to inform treatment decisions among individuals who have a personal history of chronic disease. Previous studies have shown that African Americans have difficulty understanding basic genetic and medical genetic terminology28; therefore, efforts are needed to develop and evaluate new strategies for educating diverse clinical populations about genetic and genomic concepts. Educational approaches, especially if they are delivered in formats and venues that are likely to be acceptable and accessible, could enhance exposure to information about genetically targeted care and address negative beliefs about the potential to benefit from this type of care.
We also found that future temporal orientation was associated significantly with beliefs about the potential for genetically targeted care to limit access to treatment. Greater levels of future temporal orientation were associated with a reduced likelihood of endorsing this belief. Future temporal orientation reflects the extent to which individuals are concerned about and consider future consequences29; previous studies have shown that future temporal orientation is positively associated with acceptance of genetic counseling for BRCA1 and BRCA2 mutations.18,30 Genetic testing for inherited cancer risk and disease susceptibility is generally used for planning and prevention; individuals with greater future temporal orientation may view access to medical treatment and the ability to plan treatment and prevention options within the context of future outcomes. Additional research is needed to examine the association between future temporal orientation and acceptance of different types of genetically targeted care. In contrast to our hypotheses, religiosity was not associated significantly with the beliefs about genetically targeted care that we measured. Possible explanations for this include our modest sample size and limited variability in religiosity. It is also possible that the aspects of religiosity we measured (e.g., praying for health) are not relevant to beliefs about the impact that genetically targeted care may have on access to health care and possible benefits of this type of medicine. Future studies should evaluate the association between other domains of religiosity and beliefs about other applications of genetics in medical care.
In considering the results of this study, some limitations should be noted. First, our sample of 152 respondents was made up of patients from a single health care institution in an urban area and we were only able to contact about 14% of patients who were identified from billing records to screen them for eligibility. However, our health care system has a geographically diverse patient population that is drawn from the Philadelphia, PA metropolitan area and 69% of those who were screened and eligible completed the survey. An additional limitation may be that the items we used to evaluate beliefs about genetically targeted care were newly developed. While these items had acceptable face validity, psychometric research is needed to determine the correlation between items and to characterize their reliability and validity, especially with respect to predicting acceptance of genetically targeted care. We also did not evaluate the association between beliefs about genetically targeted care and acceptance of testing or intentions to use health care that is informed by genetic information. This is an important area for future research, especially among African Americans and other racial and ethnic minority groups. Our previous research has shown African Americans have low uptake of genetic testing,3 despite having positive attitudes about BRCA1 and BRCA2 testing.15 Lastly, future studies should evaluate the association between beliefs about genetically targeted care and experiences with racial discrimination. Individuals who have more experiences with racial discrimination may be more likely to have negative expectations about genetically targeted care, but we did not evaluate discrimination in our study.
CONCLUSION
Our study sheds new light on beliefs about genetically targeted care among African American men and women. Our findings show that African Americans have diverse, and in some ways conflicting, beliefs about genetically targeted care. Studies that determine whether positive or negative beliefs are most important to acceptance of genetically targeted care, and long-term outcomes from these approaches, could be used to develop pre-test education and counseling strategies that are effective at informing patients about the benefits, limitations, and risks of this type of care to ensure that patients make decisions that are consistent with their individual preferences.
Acknowledgments
This research was supported by National Human Genome Research Institute grant #R01HG004346 and grant #U54MD010706 from the National Institute on Minority Health and Health Disparities. We would like to acknowledge Benita Weathers, Aliya Collier, and Brandon Mahler for assistance with data collection and management. We are very appreciative to all the men and women who participated in this research.
Footnotes
Conflict of interest: None disclosed.
Compliance with ethics guidelines: This research was conducted in compliance with the regulations for human subjects protections in the United States.
Contributor Information
Chanita Hughes Halbert, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC, USA; Health Equity and Rural Outreach Center, Ralph H. Johnson Department of Medical Affairs, Charleston, SC, USA
Jasmine A. McDonald, Department of Epidemiology, Columbia University, Mailman School of Public Health, New York, NY, USA
Gayenell Magwood, College of Nursing, Medical University of South Carolina, Charleston, SC, USA
Melanie Jefferson, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC, USA
References
- 1.Collins FS, Green ED, Guttmacher AE, Guyer MS. A vision for the future of genomics research. Nature. 2003;422:835–847. doi: 10.1038/nature01626. [DOI] [PubMed] [Google Scholar]
- 2.Graves KD, Vegella P, Poggi EA, et al. Long-term psychosocial outcomes of BRCA1/BRCA2 testing: differences across affected status and risk-reducing surgery choice. Cancer Epidemiol Biomarkers Prev. 2012;21:445–455. doi: 10.1158/1055-9965.EPI-11-0991. http://dx.doi.org/10.1158/1055-9965.epi-11-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halbert CH, Kessler L, Stopfer JE, Domchek S, Wileyto EP. Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genet Med. 2006;8:576–582. doi: 10.1097/01.gim.0000237719.37908.54. http://dx.doi.org/10.109701.gim.0000237719.37908.54. [DOI] [PubMed] [Google Scholar]
- 4.Halbert CH, Stopfer JE, McDonald J, et al. Long-term reactions to genetic testing for BRCA1 and BRCA2 mutations: does time heal women’s concerns? J Clin Oncol. 2011;29:4302–4306. doi: 10.1200/JCO.2010.33.1561. http://dx.doi.org/10.1200/jco.2010.33.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Neill SC, Valdimarsdottir HB, Demarco TA, et al. BRCA1/2 test results impact risk management attitudes, intentions, and uptake. Breast Cancer Res Treat. 2010;124:755–764. doi: 10.1007/s10549-010-0881-4. http://dx.doi.org/10.1007/s10549-010-0881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz MD, Hughes C, Roth J, et al. Spiritual faith and genetic testing decisions among high-risk breast cancer probands. Cancer Epidemiol Biomarkers Prev. 2000;9:381–385. [PubMed] [Google Scholar]
- 7.Schwartz MD, Lerman C, Brogan B, et al. Utilization of BRCA1/BRCA2 mutation testing in newly diagnosed breast cancer patients. Cancer Epidemiol Biomarkers Prev. 2005;14:1003–1007. doi: 10.1158/1055-9965.EPI-03-0545. http://dx.doi.org/10.1158/1055-9965.epi-03-0545. [DOI] [PubMed] [Google Scholar]
- 8.Adeyemo A, Rotimi C. Genetic variants associated with complex human diseases show wide variation across multiple populations. Public Health Genomics. 2010;13:72–79. doi: 10.1159/000218711. http://dx.doi.org/10.1159/000218711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frazer KA, Ballinger DG, Cox DR, et al. A second generation human haplotype map of over 3.1 million SNPs. Nature. 2007;449:851–861. doi: 10.1038/nature06258. http://dx.doi.org/10.1038/nature06258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The International HapMap, C. A haplotype map of the human genome. Nature. 2005;437:1299–1320. doi: 10.1038/nature04226. http://dx.doi.org/10.1038/nature04226. http://www.nature.com/nature/journal/v437/n7063/suppinfo/nature04226_S1.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green ED, Guyer MS. Charting a course for genomic medicine from base pairs to bedside. Nature. 2011;470:204–213. doi: 10.1038/nature09764. http://dx.doi.org/10.1038/nature09764. [DOI] [PubMed] [Google Scholar]
- 12.Bates BR, Poirot K, Harris TM, Condit CM, Achter PJ. Evaluating direct-to-consumer marketing of race-based pharmacogenomics: a focus group study of public understandings of applied genomic medication. J Health Commun. 2004;9:541–559. doi: 10.1080/10810730490882720. http://dx.doi.org/10.1080/10810730490882720. [DOI] [PubMed] [Google Scholar]
- 13.Bevan JL, Lynch JA, Dubriwny TN, et al. Informed lay preferences for delivery of racially varied pharmacogenomics. Genet Med. 2003;5:393–399. doi: 10.1097/01.gim.0000087989.12317.3f. http://dx.doi.org/10.109701.GIM.0000087989.12317.3F. [DOI] [PubMed] [Google Scholar]
- 14.Hughes C, Gomez-Caminero A, Benkendorf J, et al. Ethnic differences in knowledge and attitudes about BRCA1 testing in women at increased risk. Patient Educ Couns. 1997;32:51–62. doi: 10.1016/s0738-3991(97)00064-5. [DOI] [PubMed] [Google Scholar]
- 15.Kessler L, Collier A, Brewster K, et al. Attitudes about genetic testing and genetic testing intentions in African American women at increased risk for hereditary breast cancer. Genet Med. 2005;7:230–238. doi: 10.1097/01.gim.0000159901.98315.fe. http://dx.doi.org/10.109701.GIM.0000159901.98315.FE. [DOI] [PubMed] [Google Scholar]
- 16.Harris TM, Keeley B, Barrientos S, et al. A religious framework as a lens for understanding the intersection of genetics, health, and disease. Am J Med Genet C Semin Med Genet. 2009;151C:22–30. doi: 10.1002/ajmg.c.30192. http://dx.doi.org/10.1002/ajmg.c.30192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris TM, Parrott R, Dorgan KA. Talking about human genetics within religious frameworks. Health Commun. 2004;16:105–116. doi: 10.1207/S15327027HC1601_7. http://dx.doi.org/10.1207/S15327027HC1601_7. [DOI] [PubMed] [Google Scholar]
- 18.Gurmankin Levy A, Micco E, Putt M, Armstrong K. Value for the future and breast cancer-preventive health behavior. Cancer Epidemiol Biomarkers Prev. 2006;15:955–960. doi: 10.1158/1055-9965.EPI-05-0169. http://dx.doi.org/10.1158/1055-9965.epi-05-0169. [DOI] [PubMed] [Google Scholar]
- 19.Halbert CH, Brewster K, Collier A, et al. Recruiting African American women to participate in hereditary breast cancer research. J Clin Oncol. 2005;23:7967–7973. doi: 10.1200/JCO.2004.00.4952. http://dx.doi.org/10.1200/jco.2004.00.4952. [DOI] [PubMed] [Google Scholar]
- 20.Lukwago SN, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Fam Commun Health. 2001;24:63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M. Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev. 2000;57:218–235. doi: 10.1177/1077558700057001S10. [DOI] [PubMed] [Google Scholar]
- 22.O’Neill SM, Rubinstein WS, Wang C, et al. Familial risk for common diseases in primary care: the Family Health-ware Impact Trial. Am J Prev Med. 2009;36:506–514. doi: 10.1016/j.amepre.2009.03.002. http://dx.doi.org/10.1016/j.amepre.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez S, Tobin JN, Cassells A, Diaz-Gloster M, Kalida C, Ogedegbe G. The counseling African Americans to Control Hypertension (CAATCH) trial: baseline demographic, clinical, psychosocial, and behavioral characteristics. Implement Sci. 2011;6:100. doi: 10.1186/1748-5908-6-100. http://dx.doi.org/10.1186/1748-5908-6-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orzech KM, Vivian J, Huebner Torres C, Armin J, Shaw SJ. Diet and exercise adherence and practices among medically underserved patients with chronic disease: variation across four ethnic groups. Health Educ Behav. 2013;40:56–66. doi: 10.1177/1090198112436970. http://dx.doi.org/10.1177/1090198112436970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiu SH, Sun ZL, Cai X, Liu L, Yang B. Improving patients’ adherence to physical activity in diabetes mellitus: a review. Diabetes Metabolism J. 2012;36:1–5. doi: 10.4093/dmj.2012.36.1.1. http://dx.doi.org/10.4093/dmj.2012.36.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Valdez R, Yoon PW, Qureshi N, Green RF, Khoury MJ. Family history in public health practice: a genomic tool for disease prevention and health promotion. Annu Rev Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. http://dx.doi.org/10.1146/annurev.publ-health.012809.103621. [DOI] [PubMed] [Google Scholar]
- 27.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roc-cella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. http://dx.doi.org/10.1161/hypertensionaha.108.113357. [DOI] [PubMed] [Google Scholar]
- 28.Kessler L, Collier A, Halbert CH. Knowledge about genetics among African Americans. J Genet Couns. 2007;16:191–200. doi: 10.1007/s10897-006-9054-3. http://dx.doi.org/10.1007/s10897-006-9054-3. [DOI] [PubMed] [Google Scholar]
- 29.McGrath JE. The Social Psychology of Time: New perspectives. Newbury Park, California: Sage Publications; 1988. [Google Scholar]
- 30.Hughes C, Fasaye GA, LaSalle VH, Finch C. Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns. 2003;51:107–114. doi: 10.1016/s0738-3991(02)00179-9. [DOI] [PubMed] [Google Scholar]


