Abstract
Primary aldosteronism is the most common form of endocrine hypertension with a prevalence of 6% in the general population with hypertension. The genetic basis of the four familial forms of primary aldosteronism (familial hyperaldosteronism FH types I–IV) and the majority of sporadic unilateral aldosterone-producing adenomas has now been resolved. Familial forms of hyperaldosteronism are, however, rare. The sporadic forms of the disease prevail and these are usually caused by either a unilateral aldosterone-producing adenoma or bilateral adrenal hyperplasia. Aldosterone-producing adenomas frequently carry a causative somatic mutation in either of a number of genes with the KCNJ5 gene, encoding an inwardly rectifying potassium channel, a recurrent target harboring mutations at a prevalence of more than 40% worldwide. Other than genetic variations, gene expression profiling of aldosterone-producing adenomas has shed light on the genes and intracellular signalling pathways that may play a role in the pathogenesis and pathophysiology of these tumors.
Keywords: primary aldosteronism, aldosterone, aldosterone-producing adenoma, transcriptome profiing
1. Introduction
Primary aldosteronism (PA) is the most common potentially curable form of hypertension with a prevalence of 5–10% in patients with hypertension [1,2,3] and is characterized by the excessive production of aldosterone. Aldosterone excess has detrimental effects independent of blood pressure control as demonstrated by the increased risk of cardiovascular and cerebrovascular events and target organ damage in patients with PA relative to matched patients with essential hypertension. PA is mainly caused by either an aldosterone-producing adenoma (APA) or bilateral adrenal hyperplasia (BAH). The diagnosis of an APA is appealing because hypertension can be cured or markedly improved by unilateral adrenalectomy and resolve the aldosterone excess in the majority of cases [4]. In contrast, patients with BAH are usually treated with a mineralocorticoid receptor antagonist but plasma renin levels should be monitored as a therapeutic response (as well as blood pressure) because suppressed renin, independent of blood pressure control, is associated with an increased risk of cardiometabolic events and death relative to patients with essential hypertension [5]. A landmark in PA research was the discovery of germline and somatic mutations that drive the aldosterone overproduction in patients with PA, discoveries that were made possible by the application of next-generation sequencing [6,7,8,9,10,11,12]. The genetic basis of four familial forms of PA has now been described as well as somatic mutations in APAs and these are discussed in more detail below.
Herein, we outline novel contributions and major discoveries that have been made in the field of PA research over the last few years. We describe the genetic basis of familial forms of hyperaldosteronism and the identification of somatic mutations that lead to excess aldosterone production. Differential gene expression profiles between APAs and reference tissues are highlighted, as well as key signalling pathways and molecular mechanisms that may drive cell proliferation and constitutive aldosterone production in APAs. Additionally, the possible influence of genetics and genomics on surgical outcome and the potential application of next-generation sequencing methods and transcriptome profiling as possible prognostic tools are described.
2. Synthesis of Aldosterone
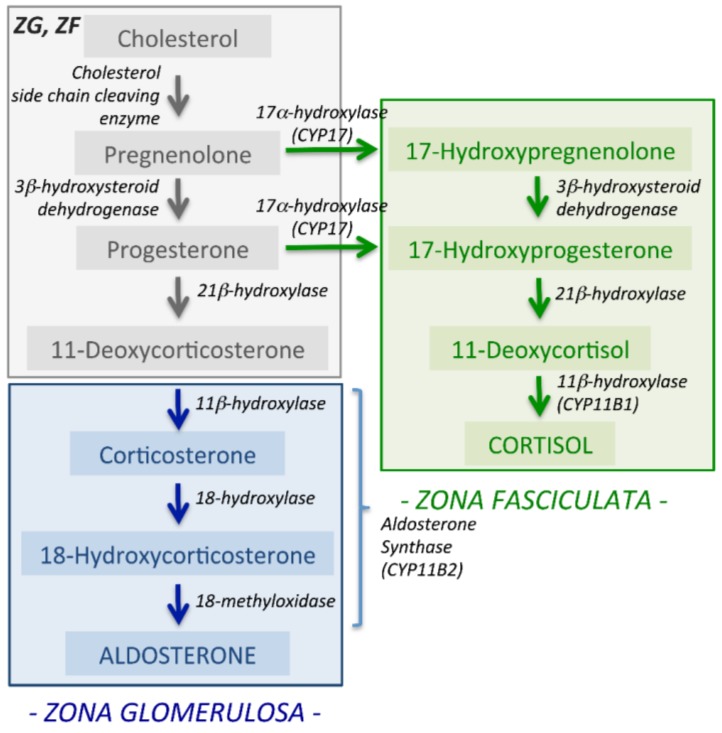
The primary function of aldosterone is to maintain fluid and electrolyte balance for the control of blood pressure. The main physiological regulators of aldosterone synthesis are angiotensin II, potassium and adrenocorticotropic hormone. Aldosterone synthesis is restricted to the zona glomerulosa (ZG), the outer layer of the adrenal cortex (Figure 1) where aldosterone synthase converts deoxycorticosterone to aldosterone by three successive steps of 11β-hydroxylation, 18-hydroxylation and 18-oxidation by a single enzyme, aldosterone synthase (encoded by CYP11B2). CYP11B2 displays a high level of intron and exon sequence homology to the CYP11B1 gene localized in the zona fasciculata (ZF) that encodes 11β-hydroxylase that catalyses the final step in the conversion of 11-deoxycortisol to cortisol (Figure 1). Angiotensin II and potassium regulate aldosterone production via Ca2+ signalling which also plays a key role in the aldosterone excess in PA due to the somatic and germline mutations in ion channels and transporters.
Figure 1.
Aldosterone synthesis in the adrenal cortex. Aldosterone is synthesized in the zona glomerulosa (ZG) distinct from the synthesis of cortisol in the zona fasciculata (ZF). Aldosterone synthase encoded by CYP11B2 performs all three enzymatic steps in the conversion of deoxycorticosterone to aldosterone.
3. Familial Forms of Hyperaldosteronism
There are currently 4 recognised forms of familial hyperaldosteronism (FH types I–IV) and the genetic basis of each type is summarized in Table 1.
Table 1.
Familial forms of hyperaldosteronism.
| Subtype of Primary Aldosteronism | Genetic Variant | Encoded Protein | Brief Description |
|---|---|---|---|
| FH Type I | CYP11B1/CYP11B2 hybrid gene | CYP11B2 | Ectopic expression in ZF; regulated by ACTH |
| FH Type II | CLCN2 mutations | CIC-2 | Chloride voltage-gated channel 2 |
| FH Type III | KCNJ5 mutations | GIRK4 | Potassium Voltage-Gated Channel Subfamily J Member 5 |
| FH Type IV | CACNA1H mutations | Cav3.2 | Calcium Voltage-Gated Channel Subunit α1H |
3.1. Familial Hyperaldosteronism Type I
Familial hyperaldosteronism type I (FH type I or GRA, glucocorticoid remediable aldosteronism) is caused by a hybrid CYP11B1/CYP11B2 gene inherited as an autosomal dominant trait. The hybrid gene results from an asymmetrical crossing over between the highly homologous CYP11B1 (encoding 11β-hydroxylase) and CYP11B2 (encoding aldosterone synthase) genes and comprises 5′ sequences of CYP11B1 (including the promoter region) and 3′ sequences of CYP11B2 (including the coding region of aldosterone synthase). Thus, in FH type I, aldosterone synthase is ectopically expressed in the ZF under the control of adrenocorticotropic hormone (ACTH) rather than restricted to the ZG under the control of angiotensin II [13,14].
3.2. Familial Hyperaldosteronism Type II
Familial hyperaldosteronism type II (FH type II) was first described by Stowasser et al. [15] in a kindred with an autosomal dominant form of PA. Other kindreds were subsequently described and a linkage with a locus on chromosome 7p22 was reported in some but not all families but sequencing the entire linked locus did not identify the genetic cause [16]. In 2018, Scholl et al. [17] identified the genetic variant responsible in the original kindred with FH type II described by Michael Stowasser as a heterozygous variant of the CLCN2 gene that caused early-onset primary aldosteronism and hypertension often with hypokalaemia. CLCN2 encodes CIC-2, a homodimer voltage-gated chloride channel expressed in the adrenal gland predominantly in the ZG [17]. In the original family with FH type II, eight individuals were carriers of the CLCN2 mutation (resulting in the CIC-2 p.Arg172Gln substitution) and of these, seven tested positive with a screening test for primary aldosteronism (elevated aldosterone-to-renin ratio). One carrier for the CIC-2 p.Arg172Gln variant had a normal aldosterone-to-renin ratio, and therefore did not have primary aldosteronism, indicating an incomplete penetrance of the allele. Scholl et al. found the p.Arg172Gln substitution in an additional kindred and two further cases of p.Arg172Gln mutations (1 occurring de novo) in 2 unrelated patients with early-onset PA [17] as well as other CLCN2 variants encoding 4 different mutations in CIC-2 (a de novo p.Met22Lys mutation, p.Tyr26Asn, p.Ser865Arg and p.Lys362del). At the same time, Fernandes-Rosa et al., reported a de novo heterozygous p.Gly24Asp mutation in the CIC-2 chloride channel associated with PA [18]. Electrophysiological recordings showed that the mutated CIC-2 channels display modified gating resulting in increased chloride efflux compared with wild-type CIC-2 channels. The increased chloride efflux leads to depolarization of adrenocortical cells, activation of voltage-dependent Ca2+ channels, Ca2+ influx, increased CYP11B2 gene expression and aldosterone production.
3.3. Familial Hyperaldosteronism Type III
Choi et al. identified the genetic basis of familial hyperaldosteronism type III (FH type III) in 2011 by next-generation sequencing [6]. A gain-of-function mutation in the KCNJ5 gene (encoding the G-protein-coupled inwardly rectifying potassium channel GIRK4) was identified in the male index case and his two daughters. The mutation results in the substitution of a threonine residue (p.Thr158Ala) located just above the selectivity filter of the channel pore which interferes with the Thr158-Pro128 hydrogen bonding [6]. Patch clamp recordings of human embryonic kidney cells expressing the mutated GIRK4 p.Thr158Ala channel showed that the mutation results in a loss of selectivity for K+ and permissively allows the passage of Na+ resulting in membrane depolarization [6]. In adrenal cells, membrane depolarization leads to the opening of voltage gated Ca2+ channels and Ca2+ influx activating the Ca2+ signalling pathway and aldosterone production. Expression of GIRK4 p.Thr158Ala in the human adrenocortical carcinoma cell line (HAC15) caused a marked increase in aldosterone secretion that was dependent on membrane depolarization and Na+ and Ca2+ influx [19]. Until 2017, 22 patients with FH type III were described in the literature from 12 families [20]. Notable is that over half of the patients described with FH type III (14 of 22 cases occurring in 7 of 12 families) carried mutations of the Gly151 residue (p.Gly151Glu or p.Gly151Arg) in the GlyTyrGly motif implicated in K+ selectivity [21].
3.4. Familial Hyperaldosteronism Type IV
Familial hyperaldosteronism type IV (FH type IV) is caused by gain-of-function mutations in Cav3.2, a T type Ca2+ channel encoded by CACNA1H. FH type IV was first identified in 2015 by exome sequencing of 40 unrelated subjects with early-onset hyperaldosteronism and hypertension (<10 years of age) [22]. Scholl et al. identified five subjects with the same heterozygous mutation in CACNA1H encoding the Ca2+ voltage gated channel (Cav3.2) resulting in a Cav3.2 p.Met1549Val substitution [16]. Comparisons of whole cell patch clamp recordings of Cav3.2 p.Met1549Val and wild-type Cav3.2 expressed in human embryonic kidney cells showed that the p.Met1549Val mutation causes an impairment of channel activation and inactivation. The mutant channel displayed slightly slower activation and much slower inactivation time constants compared with the wild-type channel as well as a tail current indicating that a proportion of the mutated channels remain non-inactivated. These properties would lead to an increase in Ca2+ influx in adrenal ZG cells and signal an increase in aldosterone production. Validation of this concept was subsequently demonstrated by the same group by expression of the Cav3.2 p.Met1549Val mutation in human adrenocortical (HAC15) cells which resulted in an increase in CYP11B2 gene transcription and aldosterone secretion relative to cells expressing the wild-type channel [23]. Following the discovery by Scholl, additional mutations in CACNA1H were described involving a substitution of the same Met1549 residue (Met1549Ile) or other amino acid residues (Ser196Leu, Val1951Glu and Pro2083Leu) [24].
4. Somatic Mutations in Aldosterone-Producing Adenomas
The most frequent genetic variation in APA is a somatic mutation of the KCNJ5 gene [25]. First identified by Choi et al. in 2011 by exome sequencing, mutations in KCNJ5 were identified in 8 of 22 APA resulting in GIRK p.Gly151Arg or p.Leu168Arg mutations [6]. Both mutations were demonstrated to interfere with the selectivity filter of the channel pore and result in membrane depolarization causing the opening of voltage gated Ca2+ channels in adrenal glomerulosa cells and Ca2+ influx [6]. Somatic KCNJ5 mutations are found at a prevalence of 40–50% [26,27,28,29,30] although a higher prevalence has been reported in populations from Japan and China [31,32]. Following the description of the KCNJ5 mutations, the application of next generation sequencing rapidly identified additional somatic mutations associated with aldosterone overproduction in sporadic PA. These include heterozygous gain-of-function mutations in Cav1.3 (the α1D subunit of the L-type voltage-dependent calcium channel) encoded by CACNA1D [8,9] and the ion transporters, Na+/K+-ATPase (encoded by ATP1A1) and Ca2+-ATPase (encoded by ATP2B3) [7,8]. These mutations result in an increase in intracellular Ca2+ concentration thereby causing an increase in transcription of the CYP11B2 gene that encodes aldosterone synthase. Activating mutations in exon 3 of CTNNB1 that encodes β-catenin have been identified in APAs as well as in other adrenal tumours [33]. Despite these major advances, the mechanisms underlying the deregulated cell growth of APAs are probably not explained by somatic mutations and the GIRK4 Thr158Ala mutation does not enhance proliferation of adrenal cells in vitro [19]. Herein we discuss the transcriptome studies that have identified genes and signalling pathways that may function in the pathophysiology and pathogenesis of APA.
5. Gene Expression Profiling
Gene expression studies have identified genes with a potential role in the pathogenesis and pathophysiology of APAs (Table 2). Despite inter-study heterogeneity of gene expression data, which may be accounted for by the use of different reference tissues (adjacent cortex or normal adrenal tissue or, in some cases, non-functioning adrenocortical adenomas) and different diagnostic criteria [34,35,36,37,38], such studies have proven valuable in the identification of genes and signalling pathways with a potential role in the pathogenesis and pathophysiology of APAs.
Table 2.
Differentially expressed genes in aldosterone-producing adenomas and their reference tissues used in transcriptome studies.
| Gene | Encoded Protein and Description | Reference Tissue | Ref. |
|---|---|---|---|
| Upregulated Genes | |||
| CYP11B2 | Aldosterone synthase- steroid hydroxylase cytochrome P450 enzyme with 11β-hydroxylase, 18-hydroxylase and 18-oxidase activities | AAC; NLA | [34,39,40,41] |
| Calcium Signaling | |||
| VSNL1 | Visinin-like 1, calcium sensor protein of visinin/recoverin subfamily | NLA | [59] |
| CALN1 | Calneuron 1, calcium-binding protein with high similarity to calmodulin family | NLA | [41,67] |
| CALM2 | Calmodulin 2, calcium-binding protein of calmodulin family. | Adjacent ZG | [42] |
| PCP4 | Purkinje cell protein 4, regulates calmodulin activity by modulating calcium binding by calmodulin | NFA | [68] |
| Nuclear receptor Transcription Factors | |||
| NR4A1 | Nuclear receptor subfamily 4 group A member 1; steroid-thyroid hormone-retinoid receptor superfamily. | WT-KCNJ5-APAs | [56] |
| NR4A2 | Nuclear receptor subfamily 4 group A member 2; steroid-thyroid hormone-retinoid receptor superfamily. | WT-KCNJ5-APAs | [56] |
| NR5A1 | Nuclear receptor subfamily 5 group A member 1 (SF1); transcriptional activator of sex determination. | AAC | [39] |
| NR0B1 | Nuclear receptor subfamily 0 group B member 1 (DAX1); functions in proper formation of adult adrenal gland formation. | AAC | [39] |
| G-protein-coupled Receptors | |||
| LHCGR | Luteinizing hormone/choriogonadotropin receptor | NLA | [60] |
| GNRHR | Gonadotropin releasing hormone receptor | NLA | [60] |
| HTR4 | 5-hydroxytryptamine receptor 4 | NLA; NFA | [60,64] |
| PTGER1 | Prostaglandin E receptor 1 | NFA | [64] |
| MC2R | Melanocortin 2 receptor | NLA | [60] |
| AGTR1 | Angiotensin II receptor type I | NLA | [60] |
| Others | |||
| NEFM | Medium neurofilament protein- biomarker of neuronal damage | KCNJ5-mut APAs; ZF-like APAs | [62,63] |
| TDGF1 | Teratocarcinoma-derived growth factor 1- signaling protein that functions in development and tumor growth | NLA | [41] |
| NPNT | Nephronectin, a secreted matrix protein | NLA | [72] |
| Downregulated Genes | |||
| GSTA1 | Glutathione S-transferase alpha 1- member of a family of enzymes that protect cells from reactive oxygen species | WT-KCNJ5-APAs; NLA | [69] |
| SFPR2 | Secreted frizzled related protein 2- agonist of Wnt signaling | NLA | [72] |
AAC: adjacent adrenal cortex; APAs: aldosterone-producing adenomas; KCNJ5-mut APAs: APAs with KCNJ5 mutations; NFA: non-functioning adrenocortical adenomas; NLA: normal adrenals; WT-KCNJ5 APAs: APAs with wild type KCNJ5 gene; ZF: zona fasciculata; ZG: zona glomerulosa.
Gene expression studies employing microarrays have shown a higher expression of CYP11B2 in APA compared with normal adrenals [39,40,41] and by SAGE (serial analysis of gene expression) in an APA compared with adjacent cortical tissue [42]. However, another study of APA transcriptomes reported two distinct and opposing expression profiles for genes encoding steroidogenic enzymes with CYP11B2 displaying increased or decreased expression levels with respect to normal adrenal tissue [43]. This apparent paradoxical decrease of the gene expressing aldosterone synthase in a tumour that overexpresses aldosterone may be accounted for by sampling areas of the normal adrenal reference tissue. In fact, these may contain aldosterone-producing cell clusters (APCC) that express high levels of CYP11B2 with somatic CACNA1D, ATP1A1 or ATP2B3 mutations [44,45,46]. Conversely large APA with low expression of CYP11B2 that give rise to inappropriate aldosterone production might occur. Another possibility is that non-APA nodules were used in the study due to non-selective diagnostic criteria.
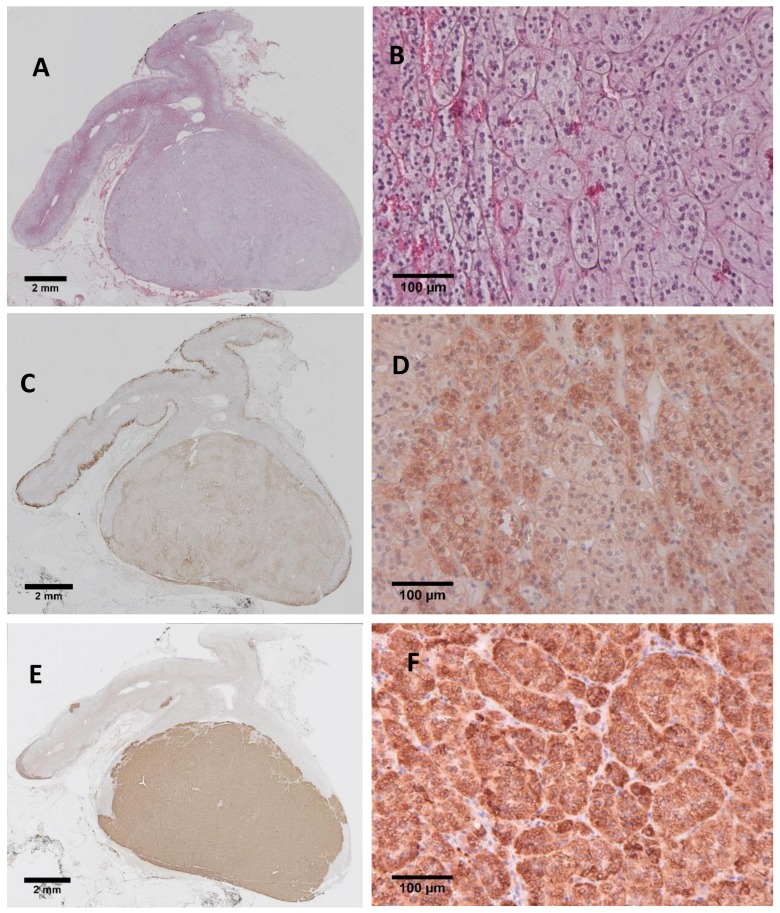
Many studies have described an association of somatic APA mutations with histological phenotype. APAs carrying KCNJ5 mutations have been widely reported to comprise predominantly large lipid-rich ZF-like cells (Figure 2) [8,47,48,49,50]. Some studies have also described a predominance of small compact ZG-like cells in APA harbouring CACNA1D, ATP1A1 or ATP2B3 mutations [8,27,49,51] and somatic APA genotype is associated with plasma steroid profiles [52]. Such genotype-phenotype associations indicate that APA genotype may influence transcriptome signatures. Histological differences between large lipid-rich ZF-like cells and small compact ZG-like cells in APA are shown in Figure 2.
Figure 2.
Histopathological phenotype of aldosterone-producing adenomas. Haematoxylin and eosin staining of an aldosterone-producing adenoma showing large lipid-rich cells of the ZF type (indicated with arrows) (panel A) or a predominance of smaller compact cells of the ZG type (indicated with arrows) (panel B).
No differences in the transcriptome profiles of APA with and without KCNJ5 mutations were initially described [26]. However, later studies reported distinct expression profiles of APA with KCNJ5 mutations compared with APA without KCNJ5 mutations (with higher CYP11B2 expression in the tumours with KCNJ5 mutations) [53]. Different expression profiles were reported in APA with ATP1A1 and ATP2B3 mutations relative to APA with KCNJ5 mutations (with higher CYP11B2 expression in the tumors with ATP1A1 and ATP2B3 mutations) [54]. Azizan et al. [35] demonstrated marked differences in CYP17A1 gene expression from microarrays, validated by real-time PCR, in APA with a ZF phenotype compared to those APA with a ZG phenotype [47]. If CYP17A1 and CYP11B2 are expressed in the same cell then cortisol can be metabolized further to produce the hybrid steroids 18-hydroxycortisol and 18-oxocortisol [55]. Higher levels of these hybrid steroids are associated with FH type I and FH type III (although not in all cases) and in patients with an APA with a KCNJ5 mutation [12,52].
CYP17 expression in APA has been shown to be associated with APA phenotype with marked upregulation in adenomas comprising predominantly ZF-type cells [47]. NURR1 (NR4A2, encoding Nur-related factor 1) and NGFIB (NR4A1, encoding nerve growth factor IB), genes that encode transcription factors playing a key role in the regulation of CYP11B2 gene transcription [56], are upregulated in APA. Also, genes encoding the nuclear receptor transcription factors SF-1 (NR5A1) and DAX1 (NR0B1) that are essential for adrenal development and steroidogenesis, are upregulated in APA [39]. Although low DAX1 expression in adrenocortical tumours is associated with aldosterone production [57]. A target gene of SF-1, VSNL1 [58], is upregulated in APA and VSNL1 in vitro overexpression in the NCI H295R cell line results in an increase in aldosterone production under both basal and angiotensin II-stimulated conditions [59].
Several genes encoding G-protein-coupled receptors are among the genes upregulated in APA, including those encoding the luteinizing hormone receptor (LH-R encoded by LHCGR), gonadotropin releasing hormone receptor (GnRHR encoded by GNRHR), serotonin receptor 4 (HTR4), melanocortin 2 receptor (MC2R), and the angiotensin II type 1 receptor (AGTR1) [60]. Overexpression of LH-R in the adrenocortical carcinoma NCI H295R cell line causes a concentration-dependent increase in CYP11B2 expression after stimulation with luteinizing hormone [40]. Accordingly, the expression of LH-R and GnRHR in APAs has been proposed to be related to increased aldosterone production during pregnancy [61]. Therefore, the presence of activating APA CTNNB1 mutations might contribute to an abnormal receptor activation [60].
NEFM, encoding the medium neurofilament protein, is highly upregulated only in APAs without KCNJ5 mutations and is selectively expressed in the ZG and in APA comprised of predominantly ZG cells [62,63]. Dopamine regulates aldosterone production via activation of its G-protein-coupled receptor (GPCR) subtypes and silencing of NEFM amplified aldosterone stimulation by a DR1 (dopamine receptor subunit 1) agonist and aldosterone secretion in response to the DR1 agonist was greater in primary cultures of APAs composed of primarily ZF cells compared with cultures of APAs with ZG cells. These data indicate a role for NEFM in aldosterone production and cell proliferation [63].
Analysis of the methylome of APAs demonstrated hypomethylation of GPCR genes and a strong association of promoter hypomethylation of the HTR4 and PTGER1 genes with the upregulation of mRNA levels, validated by real-time PCR, was demonstrated in APAs compared with non-functioning adrenocortical adenomas [64]. Methylation of HTR4 and PTGER1 was significantly inversely correlated with their respective mRNA expression levels [64]. The most hypomethylated promoter in APA is the PCP4 (encoding purkinje cell protein 4) promoter with demethylation associated with enhanced gene transcription [65]. CYP11B2 was also extensively hypomethylated in APAs [64] but although hypomethylation was not associated with gene expression levels in this study it could facilitate gene transcription [64]. In contrast, Howard et al., reported hypomethylation of APAs with hypomethylation and overexpression of CYP11B2 [64].
Calcium is a key intracellular messenger for aldosterone production and the intracellular Ca2+ signaling pathway is independent of the renin–angiotensin–aldosterone system in APAs [66]. A number of genes involved in Ca2+ signaling or Ca2+ sequestration have been reported as upregulated in APAs and are described in more detail below. VSNL1 that encodes a Ca2+-sensor protein and a target of the nuclear receptor SF-1 [58] was one of several upregulated genes in APAs by microarray analysis compared with normal adrenals validated by real-time PCR [41]. In NCI H295R adrenal cells, overexpression of VSNL1 resulted in an upregulation of CYP11B2 gene expression under both basal and angiotensin II-stimulated conditions thereby implicating a role for VSNL1 in aldosterone production. Analysis of a larger sample set of tumours showed that VSNL1 was overexpressed in APAs carrying a KCNJ5 mutation compared with those APA without a KCNJ5 mutation. A potential role for the calcium sensor in the protection of cells in an adenoma via Ca2+-related anti-apoptotic cell death mechanisms was hypothesized [59]. The expression of the VSNL1 protein in an APA (carrying a KCNJ5 mutation) that displays strong CYP11B2 immunostaining is shown in Figure 3.
Figure 3.
VSNL1 and CYP11B2 immunohistochemistry. An aldosterone-producing adenoma with a KCNJ5 mutation stained with haematoxylin and eosin panels (A,B); immunostained for VSNL1, panels (C,D); and for CYP11B2 panels (E,F). The VSNL1 antibody was from Merck and the CYP11B2 was a kind gift from Prof Celso Gomez-Sanchez, University of Mississippi, Oxford, MS, USA.
The CALN1 gene, that encodes the Ca2+ binding protein calneuron 1, has been reported as upregulated in APA in two transcriptome studies [41,67]. CALN1 was shown to potentiate aldosterone production and silencing CALN1 led to a decrease in Ca2+ storage in the endoplasmic reticulum and abrogated angiotensin II-mediated aldosterone secretion in an adrenocortical carcinoma cell line [41].
CALM2 encoding calmodulin 2 is a Ca2+-binding protein expressed in a wide-range of tissues involved in signalling, cell cycle progression and proliferation. CALM2 was highly upregulated in a transcriptome comparison of APAs with the adjacent ZG [42]. The increased expression of PCP4 in APA cells is likely to play a role in APA pathophysiology because PCP4 modulates Ca2+-binding by calmodulin and activates the calcium-calmodulin cascade leading to an increased expression of CYP11B2 [68].
GSTA1 (encoding glutathione-S-transferase, an enzyme that protects cells from reactive oxygen species, ROS) gene expression is inversely correlated with the level of aldosterone production in APAs with a KCNJ5 mutation and appears to regulate aldosterone secretion via ROS and Ca2+ signalling [69]. GSTA1 overexpression suppressed aldosterone biosynthesis, while silencing of GSTA1 increased aldosterone production through increasing ROS, superoxide, H2O2 levels, Ca2+ influx and the expression of CAMK1 (encoding Ca2+/calmodulin dependent protein kinase 1) and the transcription factors NR4A1 (also called NGFIB) and NR4A2 that regulate CYP11B2 gene expression [69].
The epidermal growth factor-like teratocarcinoma-derived growth factor-1 gene (TDGF1) was identified as the most highly expressed gene in APAs compared with normal adrenals by microarray analysis [41]. TDGF1 was also identified as upregulated in an APA relative to the paired adjacent cortex by serial analysis of gene expression [41]. Overexpression of TDGF1 in NCI H295R adrenal cells activated the PI3K-Akt signalling pathway and led to an increase in aldosterone production, indicating a potential role in APA pathophysiology [41]. The activation of PI3K/Akt mTOR signalling, a pathway with a known role in cell proliferation, was also reported in patients with PA [41].
Wnt plays a key role in the development of the adrenal cortex and the dysregulation of this signalling pathway is associated with tumorigenesis [70]. The Wnt/β-catenin pathway is constitutively activated in around 70% of APAs [71] with the decreased expression on the Wnt inhibitor SFRP2 (encoding secreted frizzled related protein 2) likely playing a role in the deregulated Wnt/β-catenin signalling [72]. SFRP2 was also four-fold down-regulated in APAs compared with normal adrenals in an oligonucleotide microarray [72]. Mice with an ablation of Sfrp2 display enhanced aldosterone production [72]. β-catenin appears to mediate aldosterone production by increasing the transcription of several genes including AT1R, CYP21 and CYP11B2 as well as upregulating expression of transcription factors NURR1 (NR4A2) and NUR77 (NR4A1) [72].
NPNT (nephronectin), a secreted matrix protein, was most highly expressed in APAs with a ZG phenotype with CTNNB1 mutations. Thereby it may represent a potential biomarker to recognize a subtype of APAs and indicates a further mechanism by which the Wnt/β-catenin signalling pathway may upregulate aldosterone production [72]. These studies show that aberrant Wnt/β-catenin pathway activation is associated with APA development and suggests that the Wnt/β-catenin signalling mediates aldosterone production at multiple levels [71].
6. Single Nucleotide Polymorphisms
Single nucleotide polymorphisms (SNPs) are the most frequent genetic variation in the human genome. A rare nonsynonymous SNP (rs7102584) resulting in a GIRK4.p.Glu282Gln substitution was identified in 12 of 251 patients (5%) with sporadic PA (9 with bilateral and 3 with unilateral PA) compared with a prevalence of 2% in the 1000 genomes cohort [73]. Five common SNPs of the KCNJ5 gene (rs6590357, rs4937391, rs3740835, rs2604204, and rs11221497) were found in patients with sporadic PA and essential hypertension and a significant association of the rs2604204 variant with sporadic PA in Chinese males was found indicating a potential role for this polymorphism in the pathogenesis of sporadic PA in this specific subgroup of patients [74].
7. Influence of Genetics and Genomics on Surgical Outcome
High blood pressure may persist after adrenalectomy due to contributory factors other than PA and the surgical cure rate of patients with APAs varies widely. Comparison of the transcriptomes of APAs with normal adrenals identified two subgroups of APAs based on their expression profiles (low versus high mRNA levels) of genes encoding steroidogenic enzymes. APAs with a low level of CYP11B2 gene transcription are associated with a longer known duration of hypertension and a lower rate of long-term cure [43].
Microarray analysis identified differentially expressed genes in a comparison of the transcriptomes of APAs from patients with persistent hypertension after adrenalectomy with that of patients with APA who were cured by surgery [75]. The differentially expressed genes were associated with five different pathways that included lipid metabolism and cell differentiation and indicate the possibility of using genomic approaches to identify drug targets and prognostic markers [75].
A number of studies have investigated the effect of KCNJ5 mutational status as a marker for surgical outcome. In a prospective study by the TAIPAI (Taiwan Primary Aldosteronsim Investigation study group) of 108 patients that were divided into KCNJ5 mutated and non-mutated groups, patients with an APA carrying a KCNJ5 mutation aged between 37 and 60 years may have an advantage in blood pressure response to surgery but mutation status is not associated with an improvement in arterial stiffness [76].
Cardiovascular complications before and after unilateral adrenalectomy in patients harboring APAs with and without KCNJ5 gene mutations were evaluated in a Japanese population. The KCNJ5-mutated group displayed a significant improvement in left ventricular mass index which was independently associated with the presence of APA KCNJ5 mutations whereas the group without KCNJ5 mutations had no such improvement [77]. A higher left ventricular mass index and plasma aldosterone concentration in patients with APA KCNJ5 mutations relative to those without KCNJ5 mutations has also been reported [35]. Despite the increased cardiac damage, patients with KCNJ5 mutations exhibited a decrease of blood pressure and plasma aldosterone concentrations and a regression of left ventricular mass index similar to the KCNJ5 wild type group after adrenalectomy [35]. Another study reported an association of APA KCNJ5 mutations with lower blood pressure and the higher likelihood of cure of PA by adrenalectomy relative to patients with APA without KCNJ5 mutations [36].
8. Conclusions and Perspectives
Major discoveries have been made in the field of PA research over the last few years mainly due to the application of next-generation sequencing methods. Four familial forms of hyperaldosteronism are now recognized with the genetic basis of three of these uncovered by exome sequencing. Somatic mutations have been identified in ion channels and transporters that alter intracellular ion homeostasis and drive the constitutive aldosterone production in over half of aldosterone-producing adenomas. Differential gene expression studies have further highlighted key signalling pathways and molecular mechanisms that may drive cell proliferation and aldosterone overproduction in aldosterone-producing adenomas. Transcriptome analysis methods may have a future application in the identification of prognostic markers to identify post-operative cardiovascular events.
Acknowledgments
This work was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement No. 694913 to Martin Reincke) and by the Deutsche Forschungsgemeinschaft (DFG) (within the CRC/Transregio 205/1 “The Adrenal: Central Relay in Health and Disease” to Felix Beuschlein, Martin Reincke and Tracy A. Williams; and grants RE 752/20-1 to Martin Reincke and grants BE 2177/13-1 and BE 2177/18-1 to Felix Beuschlein) and the Else Kröner-Fresenius Stiftung in support of the German Conns Registry-Else-Kröner Hyperaldosteronism Registry (2013_A182 and 2015_A171 to Martin Reincke).
Author Contributions
All the authors contributed substantially to the work presented in this manuscript. Tracy A. Williams conceived the work; Felix Beuschlein, Martin Reincke and Isabella Castellano contributed materials; Eva Sušnik performed immunohistochemistry; Lucie S. Meyer, Yuhong Yang and Martina Tetti performed the literature search and prepared art work and tables; Elke Tatjana Aristizabal Prada wrote the first draft of the manuscript; Tracy A. Williams, Felix Beuschlein and Martin Reincke revised the manuscript; all authors critically revised the final version.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Monticone S., D’Ascenzo F., Moretti C., Williams T.A., Veglio F., Gaita F., Mulatero P. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50. doi: 10.1016/S2213-8587(17)30319-4. [DOI] [PubMed] [Google Scholar]
- 2.Kayser S.C., Dekkers T., Groenewoud H.J., van der Wilt G.J., Carel Bakx J., van der Wel M.C., Hermus A.R., Lenders J.W., Deinum J. Study Heterogeneity and Estimation of Prevalence of Primary Aldosteronism: A Systematic Review and Meta-Regression Analysis. J. Clin. Endocrinol. Metab. 2016;101:2826–2835. doi: 10.1210/jc.2016-1472. [DOI] [PubMed] [Google Scholar]
- 3.Monticone S., Burrello J., Tizzani D., Bertello C., Viola A., Buffolo F., Gabetti L., Mengozzi G., Williams T.A., Rabbia F., et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J. Am. Coll. Cardiol. 2017;69:1811–1820. doi: 10.1016/j.jacc.2017.01.052. [DOI] [PubMed] [Google Scholar]
- 4.Williams T.A., Lenders J.W.M., Mulatero P., Burrello J., Rottenkolber M., Adolf C., Satoh F., Amar L., Quinkler M., Deinum J., et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: An international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–699. doi: 10.1016/S2213-8587(17)30135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hundemer G.L., Curhan G.C., Yozamp N., Wang M., Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: A retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–59. doi: 10.1016/S2213-8587(17)30367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi M., Scholl U.I., Yue P., Bjorklund P., Zhao B., Nelson-Williams C., Ji W., Cho Y., Patel A., Men C.J., et al. K+ channel mutations in adrenal aldosterone-producing adenomas and hereditary hypertension. Science. 2011;331:768–772. doi: 10.1126/science.1198785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beuschlein F., Boulkroun S., Osswald A., Wieland T., Nielsen H.N., Lichtenauer U.D., Penton D., Schack V.R., Amar L., Fischer E., et al. Somatic mutations in ATP1A1 and ATP2B3 lead to aldosterone-producing adenomas and secondary hypertension. Nat. Genet. 2013;45:440–444. doi: 10.1038/ng.2550. [DOI] [PubMed] [Google Scholar]
- 8.Azizan E.A., Poulsen H., Tuluc P., Zhou J., Clausen M.V., Lieb A., Maniero C., Garg S., Bochukova E.G., Zhao W., et al. Somatic mutations in ATP1A1 and CACNA1D underlie a common subtype of adrenal hypertension. Nat. Genet. 2013;45:1055–1060. doi: 10.1038/ng.2716. [DOI] [PubMed] [Google Scholar]
- 9.Scholl U.I., Goh G., Stolting G., de Oliveira R.C., Choi M., Overton J.D., Fonseca A.L., Korah R., Starker L.F., Kunstman J.W., et al. Somatic and germline CACNA1D calcium channel mutations in aldosterone-producing adenomas and primary aldosteronism. Nat. Genet. 2013;45:1050–1054. doi: 10.1038/ng.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akerstrom T., Maharjan R., Sven Willenberg H., Cupisti K., Ip J., Moser A., Stalberg P., Robinson B., Alexander Iwen K., Dralle H., et al. Activating mutations in CTNNB1 in aldosterone producing adenomas. Sci. Rep. 2016;6:19546. doi: 10.1038/srep19546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asbach E., Williams T.A., Reincke M. Recent Developments in Primary Aldosteronism. Exp. Clin. Endocrinol. Diabetes. 2016;124:335–341. doi: 10.1055/s-0042-105278. [DOI] [PubMed] [Google Scholar]
- 12.Prada E.T.A., Burrello J., Reincke M., Williams T.A. Old and New Concepts in the Molecular Pathogenesis of Primary Aldosteronism. Hypertension. 2017;70:875–881. doi: 10.1161/HYPERTENSIONAHA.117.10111. [DOI] [PubMed] [Google Scholar]
- 13.Lifton R.P., Dluhy R.G., Powers M., Rich G.M., Cook S., Ulick S., Lalouel J.M. A chimaeric 11 beta-hydroxylase/aldosterone synthase gene causes glucocorticoid-remediable aldosteronism and human hypertension. Nature. 1992;355:262–265. doi: 10.1038/355262a0. [DOI] [PubMed] [Google Scholar]
- 14.Lifton R.P., Dluhy R.G., Powers M., Rich G.M., Gutkin M., Fallo F., Gill J.R., Jr., Feld L., Ganguly A., Laidlaw J.C., et al. Hereditary hypertension caused by chimaeric gene duplications and ectopic expression of aldosterone synthase. Nat. Genet. 1992;2:66–74. doi: 10.1038/ng0992-66. [DOI] [PubMed] [Google Scholar]
- 15.Stowasser M., Gordon R.D., Tunny T.J., Klemm S.A., Finn W.L., Krek A.L. Familial hyperaldosteronism type II: Five families with a new variety of primary aldosteronism. Clin. Exp. Pharmacol. Physiol. 1992;19:319–322. doi: 10.1111/j.1440-1681.1992.tb00462.x. [DOI] [PubMed] [Google Scholar]
- 16.So A., Duffy D.L., Gordon R.D., Jeske Y.W., Lin-Su K., New M.I., Stowasser M. Familial hyperaldosteronism type II is linked to the chromosome 7p22 region but also shows predicted heterogeneity. J. Hypertens. 2005;23:1477–1484. doi: 10.1097/01.hjh.0000174299.66369.26. [DOI] [PubMed] [Google Scholar]
- 17.Scholl U.I., Stolting G., Schewe J., Thiel A., Tan H., Nelson-Williams C., Vichot A.A., Jin S.C., Loring E., Untiet V., et al. CLCN2 chloride channel mutations in familial hyperaldosteronism type II. Nat. Genet. 2018;50:349. doi: 10.1038/s41588-018-0048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandes-Rosa F.L., Daniil G., Orozco I.J., Goppner C., El Zein R., Jain V., Boulkroun S., Jeunemaitre X., Amar L., Lefebvre H., et al. A gain-of-function mutation in the CLCN2 chloride channel gene causes primary aldosteronism. Nat. Genet. 2018;50:355. doi: 10.1038/s41588-018-0053-8. [DOI] [PubMed] [Google Scholar]
- 19.Oki K., Plonczynski M.W., Luis Lam M., Gomez-Sanchez E.P., Gomez-Sanchez C.E. Potassium channel mutant KCNJ5 T158A expression in HAC-15 cells increases aldosterone synthesis. Endocrinology. 2012;153:1774–1782. doi: 10.1210/en.2011-1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monticone S., Tetti M., Burrello J., Buffolo F., De Giovanni R., Veglio F., Williams T.A., Mulatero P. Familial hyperaldosteronism type III. J. Hum. Hypertens. 2017;31:776–781. doi: 10.1038/jhh.2017.34. [DOI] [PubMed] [Google Scholar]
- 21.Dibb K.M., Rose T., Makary S.Y., Claydon T.W., Enkvetchakul D., Leach R., Nichols C.G., Boyett M.R. Molecular basis of ion selectivity, block, and rectification of the inward rectifier Kir3.1/Kir3.4 K(+) channel. J. Biol. Chem. 2003;278:49537–49548. doi: 10.1074/jbc.M307723200. [DOI] [PubMed] [Google Scholar]
- 22.Scholl U.I., Stolting G., Nelson-Williams C., Vichot A.A., Choi M., Loring E., Prasad M.L., Goh G., Carling T., Juhlin C.C., et al. Recurrent gain of function mutation in calcium channel CACNA1H causes early-onset hypertension with primary aldosteronism. eLife. 2015;4:e06315. doi: 10.7554/eLife.06315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reimer E.N., Walenda G., Seidel E., Scholl U.I. CACNA1H(M1549V) Mutant Calcium Channel Causes Autonomous Aldosterone Production in HAC15 Cells and Is Inhibited by Mibefradil. Endocrinology. 2016;157:3016–3022. doi: 10.1210/en.2016-1170. [DOI] [PubMed] [Google Scholar]
- 24.Daniil G., Fernandes-Rosa F.L., Chemin J., Blesneac I., Beltrand J., Polak M., Jeunemaitre X., Boulkroun S., Amar L., Strom T.M., et al. CACNA1H Mutations Are Associated With Different Forms of Primary Aldosteronism. EBioMedicine. 2016;13:225–236. doi: 10.1016/j.ebiom.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams T.A., Monticone S., Mulatero P. KCNJ5 mutations are the most frequent genetic alteration in primary aldosteronism. Hypertension. 2015;65:507–509. doi: 10.1161/HYPERTENSIONAHA.114.04636. [DOI] [PubMed] [Google Scholar]
- 26.Boulkroun S., Beuschlein F., Rossi G.P., Golib-Dzib J.F., Fischer E., Amar L., Mulatero P., Samson-Couterie B., Hahner S., Quinkler M., et al. Prevalence, clinical, and molecular correlates of KCNJ5 mutations in primary aldosteronism. Hypertension. 2012;59:592–598. doi: 10.1161/HYPERTENSIONAHA.111.186478. [DOI] [PubMed] [Google Scholar]
- 27.Akerstrom T., Crona J., Delgado Verdugo A., Starker L.F., Cupisti K., Willenberg H.S., Knoefel W.T., Saeger W., Feller A., Ip J., et al. Comprehensive re-sequencing of adrenal aldosterone producing lesions reveal three somatic mutations near the KCNJ5 potassium channel selectivity filter. PLoS ONE. 2012;7:e41926. doi: 10.1371/journal.pone.0041926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mulatero P., Monticone S., Rainey W.E., Veglio F., Williams T.A. Role of KCNJ5 in familial and sporadic primary aldosteronism. Nat. Rev. Endocrinol. 2013;9:104–112. doi: 10.1038/nrendo.2012.230. [DOI] [PubMed] [Google Scholar]
- 29.Williams T.A., Monticone S., Schack V.R., Stindl J., Burrello J., Buffolo F., Annaratone L., Castellano I., Beuschlein F., Reincke M., et al. Somatic ATP1A1, ATP2B3, and KCNJ5 mutations in aldosterone-producing adenomas. Hypertension. 2014;63:188–195. doi: 10.1161/HYPERTENSIONAHA.113.01733. [DOI] [PubMed] [Google Scholar]
- 30.Fernandes-Rosa F.L., Williams T.A., Riester A., Steichen O., Beuschlein F., Boulkroun S., Strom T.M., Monticone S., Amar L., Meatchi T., et al. Genetic spectrum and clinical correlates of somatic mutations in aldosterone-producing adenoma. Hypertension. 2014;64:354–361. doi: 10.1161/HYPERTENSIONAHA.114.03419. [DOI] [PubMed] [Google Scholar]
- 31.Lenzini L., Rossitto G., Maiolino G., Letizia C., Funder J.W., Rossi G.P. A Meta-Analysis of Somatic KCNJ5 K(+) Channel Mutations In 1636 Patients With an Aldosterone-Producing Adenoma. J. Clin. Endocrinol. Metab. 2015;100:E1089–E1095. doi: 10.1210/jc.2015-2149. [DOI] [PubMed] [Google Scholar]
- 32.Williams T.A., Lenders J.W., Burrello J., Beuschlein F., Reincke M. KCNJ5 Mutations: Sex, Salt and Selection. Horm. Metab. Res. 2015;47:953–958. doi: 10.1055/s-0035-1565090. [DOI] [PubMed] [Google Scholar]
- 33.Tissier F., Cavard C., Groussin L., Perlemoine K., Fumey G., Hagnere A.M., Rene-Corail F., Jullian E., Gicquel C., Bertagna X., et al. Mutations of beta-catenin in adrenocortical tumors: Activation of the Wnt signaling pathway is a frequent event in both benign and malignant adrenocortical tumors. Cancer Res. 2005;65:7622–7627. doi: 10.1158/0008-5472.CAN-05-0593. [DOI] [PubMed] [Google Scholar]
- 34.Lin Y.H., Huang K.H., Lee J.K., Wang S.M., Yen R.F., Wu V.C., Chung S.D., Liu K.L., Chueh S.C., Lin L.Y., et al. Factors influencing left ventricular mass regression in patients with primary aldosteronism post adrenalectomy. J. Renin-Angiotensin-Aldosterone Syst. 2011;12:48–53. doi: 10.1177/1470320310376424. [DOI] [PubMed] [Google Scholar]
- 35.Rossi G.P., Cesari M., Letizia C., Seccia T.M., Cicala M.V., Zinnamosca L., Kuppusamy M., Mareso S., Sciomer S., Iacobone M., et al. KCNJ5 gene somatic mutations affect cardiac remodelling but do not preclude cure of high blood pressure and regression of left ventricular hypertrophy in primary aldosteronism. J. Hypertens. 2014;32:1514–1522. doi: 10.1097/HJH.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 36.Arnesen T., Glomnes N., Stromsoy S., Knappskog S., Heie A., Akslen L.A., Grytaas M., Varhaug J.E., Gimm O., Brauckhoff M. Outcome after surgery for primary hyperaldosteronism may depend on KCNJ5 tumor mutation status: A population-based study from Western Norway. Langenbeck’s Arch. Surg. 2013;398:869–874. doi: 10.1007/s00423-013-1093-2. [DOI] [PubMed] [Google Scholar]
- 37.Rossi G.P., Auchus R.J., Brown M., Lenders J.W., Naruse M., Plouin P.F., Satoh F., Young W.F., Jr. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63:151–160. doi: 10.1161/HYPERTENSIONAHA.113.02097. [DOI] [PubMed] [Google Scholar]
- 38.Monticone S., Viola A., Rossato D., Veglio F., Reincke M., Gomez-Sanchez C., Mulatero P. Adrenal vein sampling in primary aldosteronism: Towards a standardised protocol. Lancet Diabetes Endocrinol. 2015;3:296–303. doi: 10.1016/S2213-8587(14)70069-5. [DOI] [PubMed] [Google Scholar]
- 39.Bassett M.H., Mayhew B., Rehman K., White P.C., Mantero F., Arnaldi G., Stewart P.M., Bujalska I., Rainey W.E. Expression profiles for steroidogenic enzymes in adrenocortical disease. J. Clin. Endocrinol. Metab. 2005;90:5446–5455. doi: 10.1210/jc.2005-0836. [DOI] [PubMed] [Google Scholar]
- 40.Saner-Amigh K., Mayhew B.A., Mantero F., Schiavi F., White P.C., Rao C.V., Rainey W.E. Elevated expression of luteinizing hormone receptor in aldosterone-producing adenomas. J. Clin. Endocrinol. Metab. 2006;91:1136–1142. doi: 10.1210/jc.2005-1298. [DOI] [PubMed] [Google Scholar]
- 41.Williams T.A., Monticone S., Morello F., Liew C.C., Mengozzi G., Pilon C., Asioli S., Sapino A., Veglio F., Mulatero P. Teratocarcinoma-derived growth factor-1 is upregulated in aldosterone-producing adenomas and increases aldosterone secretion and inhibits apoptosis in vitro. Hypertension. 2010;55:1468–1475. doi: 10.1161/HYPERTENSIONAHA.110.150318. [DOI] [PubMed] [Google Scholar]
- 42.Assie G., Auzan C., Gasc J.M., Baviera E., Balaton A., Elalouf J.M., Jeunemaitre X., Plouin P.F., Corvol P., Clauser E. Steroidogenesis in aldosterone-producing adenoma revisited by transcriptome analysis. J. Clin. Endocrinol. Metab. 2005;90:6638–6649. doi: 10.1210/jc.2005-1309. [DOI] [PubMed] [Google Scholar]
- 43.Lenzini L., Seccia T.M., Aldighieri E., Belloni A.S., Bernante P., Giuliani L., Nussdorfer G.G., Pessina A.C., Rossi G.P. Heterogeneity of aldosterone-producing adenomas revealed by a whole transcriptome analysis. Hypertension. 2007;50:1106–1113. doi: 10.1161/HYPERTENSIONAHA.107.100438. [DOI] [PubMed] [Google Scholar]
- 44.Nishimoto K., Tomlins S.A., Kuick R., Cani A.K., Giordano T.J., Hovelson D.H., Liu C.J., Sanjanwala A.R., Edwards M.A., Gomez-Sanchez C.E., et al. Aldosterone-stimulating somatic gene mutations are common in normal adrenal glands. Proc. Natl. Acad. Sci. USA. 2015;112:E4591–E4599. doi: 10.1073/pnas.1505529112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Omata K., Tomlins S.A., Rainey W.E. Aldosterone-Producing Cell Clusters in Normal and Pathological States. Horm. Metab. Res. 2017;49:951–956. doi: 10.1055/s-0043-122394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gomez-Sanchez C.E., Kuppusamy M., Reincke M., Williams T.A. Disordered CYP11B2 Expression in Primary Aldosteronism. Horm. Metab. Res. 2017;49:957–962. doi: 10.1055/s-0043-122238. [DOI] [PubMed] [Google Scholar]
- 47.Azizan E.A., Lam B.Y., Newhouse S.J., Zhou J., Kuc R.E., Clarke J., Happerfield L., Marker A., Hoffman G.J., Brown M.J. Microarray, qPCR, and KCNJ5 sequencing of aldosterone-producing adenomas reveal differences in genotype and phenotype between zona glomerulosa- and zona fasciculata-like tumors. J. Clin. Endocrinol. Metab. 2012;97:E819–E829. doi: 10.1210/jc.2011-2965. [DOI] [PubMed] [Google Scholar]
- 48.Dekkers T., ter Meer M., Lenders J.W., Hermus A.R., Schultze Kool L., Langenhuijsen J.F., Nishimoto K., Ogishima T., Mukai K., Azizan E.A., et al. Adrenal nodularity and somatic mutations in primary aldosteronism: One node is the culprit? J. Clin. Endocrinol. Metab. 2014;99:E1341–E1351. doi: 10.1210/jc.2013-4255. [DOI] [PubMed] [Google Scholar]
- 49.Monticone S., Castellano I., Versace K., Lucatello B., Veglio F., Gomez-Sanchez C.E., Williams T.A., Mulatero P. Immunohistochemical, genetic and clinical characterization of sporadic aldosterone-producing adenomas. Mol. Cell. Endocrinol. 2015;411:146–154. doi: 10.1016/j.mce.2015.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scholl U.I., Healy J.M., Thiel A., Fonseca A.L., Brown T.C., Kunstman J.W., Horne M.J., Dietrich D., Riemer J., Kucukkoylu S., et al. Novel somatic mutations in primary hyperaldosteronism are related to the clinical, radiological and pathological phenotype. Clin. Endocrinol. 2015;83:779–789. doi: 10.1111/cen.12873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kitamoto T., Suematsu S., Yamazaki Y., Nakamura Y., Sasano H., Matsuzawa Y., Saito J., Omura M., Nishikawa T. Clinical and Steroidogenic Characteristics of Aldosterone-Producing Adenomas With ATPase or CACNA1D Gene Mutations. J. Clin. Endocrinol. Metab. 2016;101:494–503. doi: 10.1210/jc.2015-3284. [DOI] [PubMed] [Google Scholar]
- 52.Williams T.A., Peitzsch M., Dietz A.S., Dekkers T., Bidlingmaier M., Riester A., Treitl M., Rhayem Y., Beuschlein F., Lenders J.W., et al. Genotype-Specific Steroid Profiles Associated With Aldosterone-Producing Adenomas. Hypertension. 2016;67:139–145. doi: 10.1161/HYPERTENSIONAHA.115.06186. [DOI] [PubMed] [Google Scholar]
- 53.Monticone S., Hattangady N.G., Nishimoto K., Mantero F., Rubin B., Cicala M.V., Pezzani R., Auchus R.J., Ghayee H.K., Shibata H., et al. Effect of KCNJ5 mutations on gene expression in aldosterone-producing adenomas and adrenocortical cells. J. Clin. Endocrinol. Metab. 2012;97:E1567–E1572. doi: 10.1210/jc.2011-3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Akerstrom T., Willenberg H.S., Cupisti K., Ip J., Backman S., Moser A., Maharjan R., Robinson B., Iwen K.A., Dralle H., et al. Novel somatic mutations and distinct molecular signature in aldosterone-producing adenomas. Endocr. Relat. Cancer. 2015;22:735–744. doi: 10.1530/ERC-15-0321. [DOI] [PubMed] [Google Scholar]
- 55.Lenders J.W.M., Williams T.A., Reincke M., Gomez-Sanchez C.E. DIAGNOSIS OF ENDOCRINE DISEASE: 18-Oxocortisol and 18-hydroxycortisol: Is there clinical utility of these steroids? Eur. J. Endocrinol. 2018;178:R1–R9. doi: 10.1530/EJE-17-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bassett M.H., Suzuki T., Sasano H., De Vries C.J., Jimenez P.T., Carr B.R., Rainey W.E. The orphan nuclear receptor NGFIB regulates transcription of 3beta-hydroxysteroid dehydrogenase. implications for the control of adrenal functional zonation. J. Biol. Chem. 2004;279:37622–37630. doi: 10.1074/jbc.M405431200. [DOI] [PubMed] [Google Scholar]
- 57.Reincke M., Beuschlein F., Lalli E., Arlt W., Vay S., Sassone-Corsi P., Allolio B. DAX-1 expression in human adrenocortical neoplasms: Implications for steroidogenesis. J. Clin. Endocrinol. Metab. 1998;83:2597–2600. doi: 10.1210/jcem.83.7.5095. [DOI] [PubMed] [Google Scholar]
- 58.Ferraz-de-Souza B., Hudson-Davies R.E., Lin L., Parnaik R., Hubank M., Dattani M.T., Achermann J.C. Sterol O-acyltransferase 1 (SOAT1, ACAT) is a novel target of steroidogenic factor-1 (SF-1, NR5A1, Ad4BP) in the human adrenal. J. Clin. Endocrinol. Metab. 2011;96:E663–E668. doi: 10.1210/jc.2010-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams T.A., Monticone S., Crudo V., Warth R., Veglio F., Mulatero P. Visinin-like 1 is upregulated in aldosterone-producing adenomas with KCNJ5 mutations and protects from calcium-induced apoptosis. Hypertension. 2012;59:833–839. doi: 10.1161/HYPERTENSIONAHA.111.188532. [DOI] [PubMed] [Google Scholar]
- 60.Ye P., Mariniello B., Mantero F., Shibata H., Rainey W.E. G-protein-coupled receptors in aldosterone-producing adenomas: A potential cause of hyperaldosteronism. J. Endocrinol. 2007;195:39–48. doi: 10.1677/JOE-07-0037. [DOI] [PubMed] [Google Scholar]
- 61.Albiger N.M., Sartorato P., Mariniello B., Iacobone M., Finco I., Fassina A., Mantero F. A case of primary aldosteronism in pregnancy: Do LH and GNRH receptors have a potential role in regulating aldosterone secretion? Eur. J. Endocrinol. 2011;164:405–412. doi: 10.1530/EJE-10-0879. [DOI] [PubMed] [Google Scholar]
- 62.Zhou J., Lam B., Neogi S.G., Yeo G.S., Azizan E.A., Brown M.J. Transcriptome Pathway Analysis of Pathological and Physiological Aldosterone-Producing Human Tissues. Hypertension. 2016;68:1424–1431. doi: 10.1161/HYPERTENSIONAHA.116.08033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maniero C., Garg S., Zhao W., Johnson T.I., Zhou J., Gurnell M., Brown M.J. NEFM (Neurofilament Medium) Polypeptide, a Marker for Zona Glomerulosa Cells in Human Adrenal, Inhibits D1R (Dopamine D1 Receptor)-Mediated Secretion of Aldosterone. Hypertension. 2017;70:357–364. doi: 10.1161/HYPERTENSIONAHA.117.09231. [DOI] [PubMed] [Google Scholar]
- 64.Itcho K., Oki K., Kobuke K., Yoshii Y., Ohno H., Yoneda M., Hattori N. Aberrant G protein-receptor expression is associated with DNA methylation in aldosterone-producing adenoma. Mol. Cell. Endocrinol. 2018;461:100–104. doi: 10.1016/j.mce.2017.08.019. [DOI] [PubMed] [Google Scholar]
- 65.Kobuke K., Oki K., Gomez-Sanchez C.E., Ohno H., Itcho K., Yoshii Y., Yoneda M., Hattori N. Purkinje cell protein 4 expression is associated with DNA methylation status in aldosterone-producing adenoma. J. Clin. Endocrinol. Metab. 2017 doi: 10.1210/jc.2017-01996. [DOI] [PubMed] [Google Scholar]
- 66.Rasmussen H., Isales C.M., Calle R., Throckmorton D., Anderson M., Gasalla-Herraiz J., McCarthy R. Diacylglycerol production, Ca2+ influx, and protein kinase C activation in sustained cellular responses. Endocr. Rev. 1995;16:649–681. doi: 10.1210/er.16.5.649. [DOI] [PubMed] [Google Scholar]
- 67.Kobuke K., Oki K., Gomez-Sanchez C.E., Gomez-Sanchez E.P., Ohno H., Itcho K., Yoshii Y., Yoneda M., Hattori N. Calneuron 1 Increased Ca(2+) in the Endoplasmic Reticulum and Aldosterone Production in Aldosterone-Producing Adenoma. Hypertension. 2018;71:125–133. doi: 10.1161/HYPERTENSIONAHA.117.10205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang T., Satoh F., Morimoto R., Nakamura Y., Sasano H., Auchus R.J., Edwards M.A., Rainey W.E. Gene expression profiles in aldosterone-producing adenomas and adjacent adrenal glands. Eur. J. Endocrinol. 2011;164:613–619. doi: 10.1530/EJE-10-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li X., Wang B., Tang L., Zhang Y., Chen L., Gu L., Zhang F., Ouyang J., Zhang X. GSTA1 expression is correlated with aldosterone level in KCNJ5-mutated adrenal aldosterone-producing adenoma. J. Clin. Endocrinol. Metab. 2017 doi: 10.1210/jc.2017-00950. [DOI] [PubMed] [Google Scholar]
- 70.El Wakil A., Lalli E. The Wnt/beta-catenin pathway in adrenocortical development and cancer. Mol. Cell. Endocrinol. 2011;332:32–37. doi: 10.1016/j.mce.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 71.Berthon A., Drelon C., Ragazzon B., Boulkroun S., Tissier F., Amar L., Samson-Couterie B., Zennaro M.C., Plouin P.F., Skah S., et al. WNT/beta-catenin signalling is activated in aldosterone-producing adenomas and controls aldosterone production. Hum. Mol. Genet. 2014;23:889–905. doi: 10.1093/hmg/ddt484. [DOI] [PubMed] [Google Scholar]
- 72.Teo A.E., Garg S., Johnson T.I., Zhao W., Zhou J., Gomez-Sanchez C.E., Gurnell M., Brown M.J. Physiological and Pathological Roles in Human Adrenal of the Glomeruli-Defining Matrix Protein NPNT (Nephronectin) Hypertension. 2017;69:1207–1216. doi: 10.1161/HYPERTENSIONAHA.117.09156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murthy M., Xu S., Massimo G., Wolley M., Gordon R.D., Stowasser M., O’Shaughnessy K.M. Role for germline mutations and a rare coding single nucleotide polymorphism within the KCNJ5 potassium channel in a large cohort of sporadic cases of primary aldosteronism. Hypertension. 2014;63:783–789. doi: 10.1161/HYPERTENSIONAHA.113.02234. [DOI] [PubMed] [Google Scholar]
- 74.Li N.F., Li H.J., Zhang D.L., Zhang J.H., Yao X.G., Wang H.M., Abulikemu S., Zhou K.M., Zhang X.Y. Genetic variations in the KCNJ5 gene in primary aldosteronism patients from Xinjiang, China. PLoS ONE. 2013;8:e54051. doi: 10.1371/journal.pone.0054051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xie L.F., Ouyang J.Z., Wang A.P., Wang W.B., Li X.T., Wang B.J., Mu Y.M. Gene Expression Profile of Persistent Postoperative Hypertension Patients with Aldosterone-producing Adenomas. Chin. Med. J. 2015;128:1618–1626. doi: 10.4103/0366-6999.158318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chang C.H., Hu Y.H., Tsai Y.C., Wu C.H., Wang S.M., Lin L.Y., Lin Y.H., Satoh F., Wu K.D., Wu V.C. Arterial stiffness and blood pressure improvement in aldosterone-producing adenoma harboring KCNJ5 mutations after adrenalectomy. Oncotarget. 2017;8:29984–29995. doi: 10.18632/oncotarget.16269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kitamoto T., Suematsu S., Matsuzawa Y., Saito J., Omura M., Nishikawa T. Comparison of cardiovascular complications in patients with and without KCNJ5 gene mutations harboring aldosterone-producing adenomas. J. Atheroscler. Thromb. 2015;22:191–200. doi: 10.5551/jat.24455. [DOI] [PubMed] [Google Scholar]