Abstract
Objective
To investigate the potential spillover effects of the Hospital Readmissions Reduction Program (HRRP) on readmissions for nontargeted conditions and patient populations. We examine HRRP effects on nontargeted conditions separately and on non‐Medicare populations in Florida and California.
Data Sources
From 2007–2013, 100 percent Medicare inpatient claims data, 2007–2013 State Inpatient Database (SID) for Florida, and 2007–2011 SID for California.
Study Design
We conducted an interrupted time series analysis to estimate the change in 30‐day all‐cause unplanned readmission trends after the start of HRRP using logistic regression.
Principal Findings
Hospitals with the largest reductions in targeted Medicare readmissions experienced higher reductions in nontargeted Medicare readmissions. Among nontargeted conditions, reductions were higher for neurology and surgery conditions than for the cardiovascular and cardiorespiratory conditions, which are clinically similar to the targeted conditions. For non‐Medicare patients, readmission trends for targeted conditions in Florida and California did not change after HRRP.
Conclusions
Our findings are consistent with positive spillover benefits associated with HRRP. The extent of these benefits, however, varies across condition and patient groups. The observed patterns suggest a complex response, including a role of nonfinancial factors, in driving lower readmissions.
Keywords: Hospital Readmissions Reduction Program, spillover effects, interrupted time series
Preventing avoidable readmissions in Medicare represents a significant opportunity to increase the value of health care services by improving patient outcomes and reducing spending (MedPAC 2007; Jencks, Williams, and Coleman 2009). The Hospital Readmissions Reduction Program (HRRP), established by the Affordable Care Act (ACA), imposes financial penalties on hospitals with higher than expected 30‐day readmission rates. The program started penalizing hospitals with excess readmission rates for acute myocardial infarction (AMI), heart failure, and pneumonia on October 1, 2012. The targeted conditions were expanded to include chronic obstructive pulmonary disease (COPD) and total knee and hip replacement in FY 2015. In the third year of the program (FY 2015), 78 percent of hospitals received penalties, totaling $428 million (Boccuti and Casillas 2015).
Recent studies have found broad reductions in Medicare readmission rates during the HRRP implementation period for targeted and nontargeted conditions (Carey and Lin 2015; Zuckerman et al. 2016). Based on an analysis of data from New York State, Carey and Lin found that Medicare readmissions for nontargeted conditions fell by about 1 percentage point between 2008 and 2012. Using Medicare claims data, Zuckerman et al. reported a 2.2 percentage point reduction in nontargeted readmissions nationwide between 2007 and 2015. While these findings suggest there may be spillover benefits associated with the HRRP, more research is needed to better understand the extent of such spillovers and thus assess the full impact of the HRRP.
Our study contributes to prior literature on the effects of HRRP in several ways. First, we examine whether hospitals that experienced reduced readmission rates for targeted conditions are the ones that experienced lower readmission rates for nontargeted conditions. While prior studies found reductions in nontargeted readmissions in the HRRP implementation period (Carey and Lin 2015; Zuckerman et al. 2016), the relationship between these reductions and readmission reductions for the targeted conditions is unclear. Establishing this connection would provide stronger evidence on the existence of HRRP spillover effects. Second, in contrast to prior literature that has either focused on select nontargeted conditions (Carey and Lin 2015) or pooled all nontargeted conditions in their analysis (Zuckerman et al. 2016), we examine readmission changes across nontargeted conditions separately. Our approach allows us to uncover any variation in HRRP effects across different nontargeted conditions that may be masked in analyzing nontargeted readmissions as a whole. Third, while prior literature has investigated the effect of the HRRP on the non‐Medicare population in New York State (Carey and Lin 2015), our study expands on this work by focusing on two large states with different health care delivery systems, California and Florida.
The HRRP may lead to different types of spillover effects depending on the role that financial and nonfinancial factors play in hospitals’ decision‐making. On one hand, hospitals’ responses may be driven by financial incentives (penalties for higher than average targeted readmissions) and disincentives (cost of administering readmission reduction initiatives and lost revenue associated with reduced readmissions) associated with the HRRP. As there are no financial penalties associated with excess readmissions for nontargeted conditions, hospitals may not have an incentive to engage in efforts to reduce readmissions for nontargeted populations. In fact, within this economic framework, hospitals may shift resources away from nontargeted conditions or may cover lost revenue by increasing readmissions for nontargeted conditions or populations. This would imply that hospitals with the largest reductions in Medicare readmission rates for targeted conditions would have smaller reductions in readmissions for nontargeted conditions when compared to other hospitals.
On the other hand, nonpecuniary factors, such as patient satisfaction and overall quality of care, may determine how a hospital responds to the HRRP. The spotlight on a hospital's readmissions brought on by the HRRP may cause a hospital to implement hospital‐wide readmission reduction initiatives, such as improved discharge planning for all conditions. Hospitals may take into account both financial and nonfinancial factors in responding to the HRRP incentives, finding it optimal to focus their efforts on a limited set of nontargeted conditions and leading to variations in spillover benefits across conditions.
In this study, we use Medicare and non‐Medicare data to investigate the extent to which readmission reductions observed in nontargeted conditions and populations may reflect spillover benefits of the HRRP. In particular, we address the following research questions: (1) Did Medicare readmission trends in targeted and nontargeted conditions change after HRRP implementation? (2) Were reductions in nontargeted readmissions larger in hospitals that had the greatest readmission reduction in targeted conditions? (3) Were reductions in readmissions larger for nontargeted conditions that are related to the targeted conditions? and (4) Did readmission trends in targeted conditions for non‐Medicare patients change after the start of the HRRP implementation?
Methods
Overview of Study Design
We conduct an interrupted time series analysis to compare the time trends in 30‐day all‐cause readmission rates before and after HRRP implementation. The interrupted time series analysis has been widely applied in health services research (Gillings, Makuc, and Siegel 1981; Soumerai et al. 1987; Brufsky et al. 1998; Andersson et al. 2006; Feldstein et al. 2006). The method accounts for underlying secular trends in readmission rates during the pre‐policy period to more accurately assess the impact of HRRP.
We conduct the analysis at the discharge level on a quarterly basis. We use the passage of the ACA in March 2010, which established the HRRP, as the start of the HRRP implementation. The targeted conditions examined in this study are the three conditions covered by the HRRP at the beginning of the program: AMI, heart failure, and pneumonia. We estimate the pre‐ and post‐HRRP implementation change in readmission trends for targeted and nontargeted conditions among the national Medicare population and for targeted conditions among the non‐Medicare population in California and Florida.
Data Sources
The primary data sources for the Medicare population are the Medicare Provider Analysis and Review (MedPAR) Inpatient Research Identifiable Files (RIFs) for 2007–2008 and the 100 percent Inpatient Limited Data Set (LDS) Standard Analytic Files for 2009–2013. These databases include 100 percent Medicare FFS claims for all acute care hospitals with discharges between January 1, 2007, and December 31, 2013. Patient's age, Medicare enrollment status, date of death, and county of residence for the Medicare population are pulled from the MedPAR Master Beneficiary Summary Files for 2007–2008 and the denominator files for 2009–2013. The primary data source for the non‐Medicare population is the 2007–2013 State Inpatient Database (SID) for Florida and the 2007–2011 SID for California, which contain all inpatient discharge abstracts for each state. Additional covariates are constructed using the FY 2014 Inpatient Prospective Payment System Impact File, the 2015 Hospital Compare database, the 2014–2015 Area Health Resource File, and the FY 2009 American Hospital Association (AHA) Annual Survey Database. Variables obtained from each source are listed in Appendix Table S1.
Populations Studied
We conduct analyses on both the Medicare patient population and the non‐Medicare patient population, which includes patients with an expected payer of Medicaid or private insurance. The Medicare population consists of Medicare FFS beneficiaries who had an index stay in a short‐term acute care hospital between February 2007 and November 2013. Following CMS methodology, an index hospitalization for the condition‐specific readmission measures is one that is not within 30 days of the discharge date of a prior index stay for the same condition. Therefore, hospitalizations cannot be counted as both a readmission and an index admission within the same condition‐specific measure. We include hospitalizations in short‐term acute care hospitals that participate in Medicare's inpatient prospective payment system (IPPS). Because our data cover 2007 to 2013, we exclude admissions occurring in January 2007 as they do not have a 30‐day look‐back period needed to identify index admissions. Similarly, we exclude discharges occurring in December 2013 as we cannot observe their 30‐day look‐forward period that is needed to identify the 30‐day readmissions. The 2008 Inpatient RIF does not link to the 2009 Inpatient LDS file; therefore, we also exclude December 2008 discharges in the 2008 Inpatient RIF and admissions before February 2009 in the 2009 Inpatient LDS file from our analysis.
In analyzing targeted readmissions, we create separate cohorts for beneficiaries who were hospitalized with one of the three targeted conditions (AMI, heart failure, and pneumonia) based on the primary ICD‐9 diagnosis code associated with the index stay.1 For nontargeted conditions, we follow CMS’s hospital‐wide all‐cause unplanned readmission measure and divide the beneficiaries into five cohorts: cardiorespiratory, cardiovascular, neurology, surgery, and medicine (Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation [YNHHSC/CORE] 2015b).2 We exclude beneficiaries who were hospitalized for AMI, heart failure, and pneumonia from the nontargeted condition cohorts.
We apply CMS’s inclusion and exclusion criteria for the condition‐specific and hospital‐wide 30‐day readmission measures in constructing the cohorts for targeted and nontargeted conditions, respectively. These restrictions include but are not limited to excluding admissions that resulted in death in the hospital, discharged against medical advice, and transferred to another inpatient facility (Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation [YNHHSC/CORE] 2015a,b). Following CMS, we also exclude AMI stays that are admitted and discharged on the same day. We deviate from CMS’s restrictions regarding Medicare coverage. Because we construct patient comorbid risk factors and illness severity indicators based only on the index hospital claim, we require that the patient be enrolled in Part A Medicare during the inpatient stay in addition to the 30‐day period after discharge. In contrast, CMS requires the patient also be enrolled in Parts A and B Medicare for the 12 months prior to admission.
We include all hospitals regardless of their total number of discharges in the analysis. Hospitals with few discharges make up only a small portion of our study cohort. For example, hospitals with fewer than 25 discharges in a given condition consist of less than 0.3 percent of our sample. Finally, we exclude cases with missing data for any covariate, which represents around 4 percent of cases.3 Of all the covariates, missing data on the concentration of hospitals in a Hospital Referral Region, obtained from the FY 2009 AHA Annual Survey Database, led to the largest number of cases excluded (<2 percent). Overall, our inclusion and exclusion criteria resulted in sample sizes ranging from 1,184,677 cases in 2,777 hospitals for the AMI cohort to 19,493,873 cases in 2,908 hospitals for the Medicine cohort.
For the non‐Medicare population, we conduct analyses on three cohorts of index stays with a primary diagnosis of AMI, heart failure, or pneumonia in California and Florida. We limit the study population to patients aged 18 and over who had an expected source of payment from Medicaid or a private payer for the index hospital stay. While Florida's SID data allow researchers to track 30‐day readmissions via variables that track days between admissions and the length of stay, the data only include information on the discharge quarter, so we exclude discharges during the first quarter of 2007 and the last quarter of 2013 from the analysis. California's SID data are only available through 2011. In constructing the non‐Medicare cohort, the percent of cases excluded with a missing value for any cohort ranged from a low of 4.1 percent of cases (1,968 of 47,759 cases) for the AMI cohort in Florida to a high of 6.8 percent of cases (3,546 of 52,133 cases) for the AMI cohort in California. Overall, our inclusion and exclusion criteria resulted in sample sizes ranging from 37,283 cases in 155 hospitals for the heart failure cohort in Florida to 62,446 cases in 264 hospitals for the pneumonia cohort in California.
Outcome and Explanatory Variables
The outcome variable is an indicator for being readmitted to a short‐term acute care hospital for any reason (all‐cause) within 30 days of discharge from a short‐term acute care hospital. We exclude planned readmissions from the outcome definition based on CMS’s risk‐standardized readmission measure definitions.
Our key explanatory variables are a dummy variable indicating the post‐intervention period, a continuous trend variable that is zero at the period of intervention and gives the number of quarters from the intervention during both the pre and post‐intervention periods (e.g., −3, −2, −1, 0, 1, 2, 3, 4, …), and the interaction between the post‐intervention indicator variable and the trend variable.
Defining the intervention period has been one of the main challenges in evaluating the effects of the HRRP. The HRRP was established during a period of heightened focus on hospital readmissions. CMS started public reporting of hospital readmissions for AMI, heart failure, and pneumonia in July 2009, and the period between 2008 and 2011 contained numerous stages of rulemaking related to public reporting and the HRRP. Similar to Zuckerman et al. (2016), we use the quarter after the passage of the ACA in March 2010, which established the HRRP, as the start of the HRRP. While there are other milestones in the initiation of the HRRP, the passage of the ACA was the earliest point at which hospitals had sufficient information to respond to the HRRP.
In our expanded models for nontargeted conditions, we use a categorical variable to indicate whether the index admission was in a hospital in the top 25 percentile, middle 50 percentile, or bottom 25 percentile in terms of its reduction in readmission rates for targeted conditions (see Appendix). To construct this hospital group variable, we estimate each hospital's reduction in readmission rates accounting for the hospital's performance, characteristics, and changes in case mix over time. Specifically, we divide each hospital's actual readmission rate by the hospital's predicted rate, which is based on its case mix and characteristics. Then, we estimate the linear trend in the hospital‐level ratio of the actual to predicted readmission rate before and after the HRRP. We use the change in the slope of this ratio's trend after the HRRP as the estimate of the hospital's reduction in readmission rate.
To test whether spillover effects vary across nontargeted conditions, we create a dummy variable, indicating whether the index is an admission for the nontargeted cardiorespiratory or cardiovascular conditions. We use the cardiovascular/cardiorespiratory condition category to define conditions most related to the targeted conditions because CMS includes the targeted conditions in these two condition categories when constructing their hospital‐wide all‐cause unplanned readmission measure. We use the neurology and surgery groups to define other nontargeted conditions because hospitals generally organize care for these groups separately from the targeted conditions. We do not include the medicine group in the other nontargeted conditions as it spans a diverse set of conditions, some of which may be related to the targeted conditions (e.g., other lower and upper respiratory diseases).
To control for patient‐level severity and clinical complexity, we use a different set of risk variables for each condition, following CMS’s Risk‐Standardized Readmission Measure definitions (Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation [YNHHSC/CORE] 2015a,b). We identify the risk variables based on the index stay, which is different than the CMS methodology that considers the 12‐month period prior to and including the index stay in determining the risk variables. Furthermore, CMS methodology has identified a set of conditions that may reflect complications of care rather than comorbid conditions if they occur only in the index stay and not the 12‐month period prior to the index stay. As we base all indicators of patient severity and clinical complexity on the index stay, we exclude these conditions from our list of risk adjustment variables. Additional patient‐ and hospital‐level characteristics that are included in our models are discussed in the Appendix.
Statistical Analysis
We use logistic regressions to model the probability of being readmitted to a short‐term acute care hospital within 30 days of discharge from an index stay. We first estimate the change in readmissions after the HRRP using a baseline specification given in Equation (1). We estimate the baseline model separately for condition‐specific cohorts in Medicare and non‐Medicare populations.
| (1) |
where R is an indicator variable for 30‐day readmission, X is a vector of control variables, t is the continuous trend, and HRRP is the indicator for the postACA period. The coefficient on HRRP*t, β 4, captures the change in readmission trend slope after the ACA.
We also use an expanded model to assess the extent to which potential spillover effects varied across hospital and condition groups. We estimate the expanded model, presented in Equation (2), using pooled data that includes nontargeted hospitalizations for cardiovascular, cardiorespiratory, neurology, and surgery cohorts.
| (2) |
where X is a vector of control variables, t is the time trend variable, HRRP is the indicator variable for post‐ACA period, Group 2 and Group 3 are indicator variables for hospitals in the middle 50 percent and bottom 25 percent in targeted readmission reductions, respectively, and Cardio is an indicator variable for an index hospitalization in the cardiovascular/cardiorespiratory nontargeted condition group. Hospitals in the top 25 percent in targeted readmission reductions and other nontargeted conditions serve as the reference groups. We focus on how the changes in slope of the readmission trend (coefficient on t) in the post‐HRRP period varies for different hospital and condition categories. Based on our model, β 19 + β 24 and and β 19 reflect the difference in slope changes after the ACA between hospitals with the largest and smallest reductions in targeted readmissions for the cardiovascular/cardiorespiratory and other nontargeted conditions, respectively. Similarly, β 20 and β 20 + β 24 reflect the difference in slope changes after the ACA between cardiovascular/cardiorespiratory and other nontargeted readmissions for the top and bottom 25 percent of hospitals in targeted readmission reductions, respectively. We estimate standard errors clustered at the hospital level in all regressions.
Results
Overall HRRP Effects
We find that the HRRP is associated with reductions in readmission rates for the targeted conditions (AMI, heart failure, and pneumonia) and nontargeted conditions (cardiorespiratory, cardiovascular, neurology, surgery, and medicine). Before the HRRP, readmission rates were increasing for the heart failure, pneumonia, neurology, and surgery cohorts (odds ratio > 1 with a p‐value <.01) (Table 1). Readmission rates for the AMI, cardiorespiratory, and cardiovascular cohorts were steady before the passage of the ACA (p‐value >.1), and readmission rates for the medicine cohort were decreasing (odds ratio < 1 with a p‐value <.01). After the HRRP, the slopes of the readmission rate trends decreased for all cohorts, indicating readmission rates started falling or continued to fall at a greater rate after the ACA (odds ratio < 1 with a p‐value <.01). These reductions represent sizable decreases in readmission rates during the study period. From the quarter before the HRRP (2010 Q1) to the end of our study period (2013 Q4), risk‐adjusted rates of readmission decreased by a low of 2.1 percentage points for the surgery and cardiovascular cohorts to a high of 4.5 percentage points for the AMI cohort (Table 1).
Table 1.
Estimates from Logistic Regressions of Readmission Rates for the Medicare Population, 2007–2013 (Odds Ratios)
| Targeted Conditions | Nontargeted Conditions | |||||||
|---|---|---|---|---|---|---|---|---|
| AMI | Heart Failure | Pneumonia | Cardiorespiratory | Cardiovascular | Neurology | Surgery | Medicine | |
| Pre‐HRRP slope | 0.999 | 1.003*** | 1.002*** | 1.000 | 0.999 | 1.003*** | 1.004*** | 0.999*** |
| (0.997, 1.001) | (1.001, 1.004) | (1.001, 1.004) | (0.999, 1.002) | (0.998, 1.000) | (1.001, 1.004) | (1.003, 1.005) | (0.998, 1.000) | |
| Post‐HRRP slope | 0.977*** | 0.984*** | 0.987*** | 0.984*** | 0.988*** | 0.984*** | 0.984*** | 0.984*** |
| (0.976, 0.979) | (0.983, 0.985) | (0.985, 0.988) | (0.983, 0.985) | (0.987, 0.989) | (0.983, 0.985) | (0.983, 0.985) | (0.983, 0.984) | |
| Difference in slopes, post‐HRRP minus pre‐HRRP | 0.979*** | 0.982*** | 0.984*** | 0.984*** | 0.988*** | 0.981*** | 0.980*** | 0.985*** |
| (0.976, 0.981) | (0.980, 0.983) | (0.983, 0.986) | (0.982, 0.985) | (0.987, 0.990) | (0.979, 0.983) | (0.979, 0.981) | (0.984, 0.986) | |
| Number of index admissions | 1,184,677 | 2,630,397 | 2,161,482 | 3,287,316 | 5,160,353 | 2,958,644 | 11,660,645 | 19,493,873 |
| Number of hospitals | 2,777 | 2,892 | 2,896 | 2,907 | 2,901 | 2,901 | 2,868 | 2,907 |
| Difference in risk‐adjusted readmission rates (percentage point difference between 2013Q4 and 2010Q1 presented) | −0.045 | −0.039 | −0.026 | −0.036 | −0.021 | −0.027 | −0.021 | −0.033 |
The 95 percent confidence intervals are reported in parentheses under the odds ratios; * p < .1, ** p < .05, *** p < .01; models include patient‐level variables for risk adjustments including comorbidities and hospital‐level control variables.
Source: Authors’ analysis of 2007–2008 MedPAR Inpatient Research Identifiable Files and 2009–2013 100 percent Inpatient Standard Analytic Files.
Relationship between Reductions in Targeted and Nontargeted Conditions
Figure 1 presents trends in unadjusted readmission rates for the nontargeted conditions. We divide hospitals into three groups based on their response to the HRRP for the targeted conditions. The top performing hospitals include the top 25 percent of hospitals in terms of their reductions in readmission rates for the targeted conditions, and the bottom performing hospitals are the bottom 25 percent of hospitals. The figure shows that top performing hospitals reduced readmission rates for the nontargeted conditions the most. On the other hand, readmission rates for the nontargeted conditions in the bottom performing hospitals were declining even before the ACA. The reductions continued after the HRRP, but the change in slope was smaller than the top performers.
Figure 1.
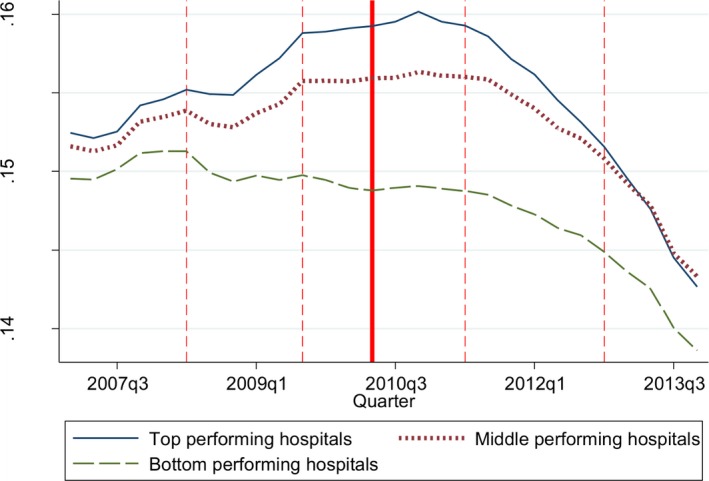
- Notes. Our analysis includes 43,954,459 index admissions in 3,156 hospitals. To adjust for seasonal patterns in readmission rates, we plot the moving average readmission rates. For each quarter, we calculate the average of the readmission rates for two quarters before the present quarter, and one quarter after. The solid vertical line represents the second quarter of 2010, after passage of the Affordable Care Act. The dashed vertical lines represent (1) Q2 of 2008—proposed rule before CMS’s public reporting of readmission rates; (2) Q3 of 2009—start of CMS’s public reporting; (3) Q2 of 2011—proposed rule identifying the targeted conditions subject to financial penalties; and (4) Q4 of 2012—start of financial penalties. We divide hospitals into groups based on their slope change in the ratio of observed to predicted readmission rates for targeted conditions before and after the HRRP. The top performing hospitals include the top 25 percentile of hospitals in terms of their slope reductions in readmission rates for the targeted conditions before and after the HRRP. The middle performing hospitals are the middle 50 percentile of hospitals and the bottom performing hospitals are the bottom 25 percentile. Source: Authors’ analysis of 2007–2008 MedPAR Inpatient Research Identifiable Files and 2009–2013 100 percent Inpatient Standard Analytic Files.
Our expanded logistic regression model results show that these relationships between hospital group and readmission rate trends observed in unadjusted readmissions remain even after controlling for patient and hospital‐level characteristics (Table 2 and Figure S1). The difference between pre‐ and post‐ACA readmission trend slopes, presented in Table 2, is our estimate of the effect of the HRRP. We find that the reduction in slope of the readmission trend is larger for top performing hospitals relative to bottom performing hospitals in both cardiovascular/cardiorespiratory and neurology/surgery condition cohorts (cardiovascular/cardiorespiratory: OR = 1.013, p‐value <.01; neurology/surgery: OR: 1.011, p‐value <.01). We find similar results when we estimate the model using data on all nontargeted conditions, including the medicine cohort (results shown in the Table S2).
Table 2.
Estimates from Logistic Regressions of Readmission Rates Comparing Related and Other Nontargeted Conditions, 2007–2013 (Odds Ratios)
| Nontargeted Conditions Related to Targeted Conditions (Cardiorespiratory, Cardiovascular) | Other Nontargeted Conditions (Neurology, Surgery) | Difference, Related Conditions—Other Conditions | |
|---|---|---|---|
| Difference in slopes between post‐HRRP and pre‐HRRP periods for top performing hospitals | 0.981*** | 0.975*** | 1.005*** |
| (0.978, 0.983) | (0.973, 0.978) | (1.002, 1.009) | |
| Difference in slopes between post‐HRRP and pre‐HRRP periods for bottom performing hospitals | 0.993*** | 0.986*** | 1.007*** |
| (0.990, 0.996) | (0.983, 0.989) | (1.004, 1.011) | |
| Difference in slope changes, bottom—top | 1.013*** | 1.011*** | 1.002 |
| (1.009, 1.017) | (1.008, 1.013) | (0.997, 1.007) | |
| Number of index admissions | 23,038,413 | ||
| Number of hospitals | 2,904 |
Estimates presented in this table are from a logistic regression model that includes patient‐level variables for risk adjustments including comorbidities and hospital‐level control variables. We divide hospitals into groups based on their slope change in the ratio of observed to predicted readmission rates for targeted conditions before and after the HRRP. The top performing hospitals include the top 25 percentile of hospitals in terms of their slope reductions in readmission rates for the targeted conditions before and after the HRRP. The bottom performing hospitals are the bottom 25 percentile. *p < 0.1, **p < 0.05, ***p < 0.01.
Source: Authors’ analysis of 2007–2008 MedPAR Inpatient Research Identifiable Files and 2009–2013 100 percent Inpatient Standard Analytic Files.
Comparing Spillover Effects across Nontargeted Conditions
Table 2 also shows the results of our analysis comparing spillover effects in the cardiorespiratory/cardiovascular conditions with spillover effects in the other conditions. We find that readmission trend slopes decreased for both nontargeted condition cohorts among top performing and bottom performing hospitals. However, the slope of the readmission trend decreased by a larger magnitude for the neurology/surgery cohort compared to the cardiovascular/cardiorespiratory cohort (among top performing hospitals: OR = 1.005, p‐value <.01; among bottom performing hospitals: OR = 1.007, p‐value <.01). The differences in readmission slope reductions between cardiovascular/cardiorespiratory and neurology/surgery cohorts were similar between top performing and bottom performing hospitals (OR = 1.002, p‐value >.1).
HRRP Effects for Non‐Medicare Population
We find that the HRRP is not associated with changes in readmission rates for the targeted conditions in the non‐Medicare population in California and Florida. Our logistic regression model in Table 3 shows that while the odds ratios for the difference in slopes for the Medicare populations in California and Florida were all statistically significant and less than 1 (p‐value <.01 for all targeted conditions in Florida and AMI in California; p‐value <.05 for heart failure in California; p‐value <.1 for pneumonia in California), there are no statistically significant changes in slopes in the post‐ACA period in the non‐Medicare population. When we examined the Medicare FFS population using SID data (not shown), our results were directionally similar to the ones based on Medicare claims data but statistically insignificant. Some of this difference may be due to the difference between the two samples as the Medicare FFS population in SID data is identified through the “expected primary payer” data, which may be a noisy indicator of the actual payer.
Table 3.
Estimates from Logistic Regressions of Readmission Rates for the California and Florida Medicare and Non‐Medicare Populations (Odds Ratios)
| Targeted Conditions, Medicare | Targeted Conditions, Non‐Medicare | |||||
|---|---|---|---|---|---|---|
| AMI | Heart Failure | Pneumonia | AMI | Heart Failure | Pneumonia | |
| California (2007–2011) | ||||||
| Pre‐HRRP slope | 0.999 | 1.002 | 0.998 | 1.004 | 0.997 | 0.993* |
| (0.991,1.007) | (0.997,1.007) | (0.993,1.003) | (0.994,1.014) | (0.990,1.005) | (0.986,1.001) | |
| Post‐HRRP slope | 0.960*** | 0.987** | 0.983** | 1.004 | 0.984 | 1.002 |
| (0.940,0.980) | (0.975,0.998) | (0.969,0.997) | (0.974,1.036) | (0.965,1.004) | (0.979,1.025) | |
| Difference in slopes, post‐HRRP minus pre‐HRRP | 0.960*** | 0.984** | 0.985* | 1.001 | 0.987 | 1.009 |
| (0.939,0.982) | (0.972,0.997) | (0.970,1.000) | (0.970,1.032) | (0.966,1.008) | (0.986,1.032) | |
| Number of index admissions | 53,283 | 125,111 | 108,928 | 48,587 | 52,687 | 62,446 |
| Number of hospitals | 260 | 269 | 269 | 253 | 267 | 264 |
| Florida (2007–2013) | ||||||
| Pre‐HRRP slope | 1.003 | 1.009*** | 1.007** | 0.985** | 1.002 | 1.001 |
| (0.996,1.010) | (1.005,1.014) | (1.001,1.014) | (0.973,0.998) | (0.989,1.014) | (0.990,1.013) | |
| Post‐HRRP slope | 0.983*** | 0.990*** | 0.989*** | 1.001 | 0.993* | 0.998 |
| (0.977,0.990) | (0.986,0.994) | (0.984,0.994) | (0.989,1.013) | (0.984,1.001) | (0.990,1.006) | |
| Difference in slopes, post‐HRRP minus pre‐HRRP | 0.980*** | 0.981*** | 0.982*** | 1.016 | 0.991 | 0.996 |
| (0.971,0.990) | (0.975,0.987) | (0.974,0.991) | (0.997,1.035) | (0.975,1.008) | (0.983,1.010) | |
| Number of index admissions | 86,439 | 194,295 | 133,381 | 45,791 | 37,283 | 57,400 |
| Number of hospitals | 155 | 156 | 157 | 152 | 155 | 156 |
The 95 percent confidence intervals are reported in parentheses under the odds ratios; *p < .1, **p < .05, ***p < .01; models include patient‐level variables for risk adjustments including comorbidities and hospital‐level control variables.
Source: Authors’ analysis of 2007–2008 MedPAR Inpatient Research Identifiable Files and 2009–2013 100 percent Inpatient Standard Analytic Files for the California and Florida Medicare populations, 2007–2011 California State Inpatient Database for the California non‐Medicare population, and 2007–2013 Florida State Inpatient Database for the Florida non‐Medicare population.
Discussion
Our analyses yield four main results that both confirm and expand previous literature. First, consistent with prior research (Carey and Lin 2015; Zuckerman et al. 2016), we find that hospitals, on average, experienced reductions in Medicare readmission rates for both targeted and nontargeted conditions after HRRP implementation. We observe reductions in readmissions in all three targeted conditions and the five nontargeted condition categories. Second, we find that hospitals that experienced the largest reductions in targeted readmissions experienced larger reductions in nontargeted readmissions relative to other hospitals. This result holds after controlling for the hospital's average pre‐ACA readmission rate in our analysis, providing support that this result is not likely driven by hospitals with high readmission rates having greater opportunities to reduce readmissions. This finding expands on previous work by drawing a direct link between the effects of hospital readmission reduction efforts for targeted conditions and nontargeted conditions. Third, readmission reductions were not larger for nontargeted conditions that are more clinically related to the targeted conditions. Finally, we find that readmissions for non‐Medicare patients treated for the targeted conditions in Florida and California did not change during the HRRP period.
Our findings suggest that hospitals implemented readmission reduction initiatives that extended to a wider set of conditions beyond the ones targeted by the HRRP. At a minimum, the results allow us to dismiss concerns that the HRRP could result in hospitals shifting resources away from nontargeted conditions or increasing readmissions for nontargeted conditions in response to the HRRP. Beyond this conclusion, the effects of the HRRP initiative on readmissions for nontargeted conditions may reflect two different (but not necessarily mutually exclusive) potential factors influencing hospital behavior: (1) hospitals may find it easier to broadly implement readmission reduction efforts rather than target specific conditions; (2) hospitals may be motivated by factors beyond the HRRP penalties to reduce Medicare readmissions.
Explaining the Effects of HRRP Implementation on Nontargeted Conditions: Broad‐Based Interventions
The policy focus on reducing readmissions, through programs including the HRRP, has increased efforts among hospital managers to develop and implement strategies aimed to prevent avoidable readmissions (Bradley et al. 2012, 2013, 2014; Kripalani et al. 2014; Hanes 2015; Krishnan et al. 2015). Some of these strategies, such as improved discharge planning, better care coordination, and enhanced patient education may be applied generally (noncondition‐specific) and scaled across condition categories with relative ease. Others are condition‐specific and involve technology or care specific to the condition, such as the use of remote monitoring of vital signs for heart failure patients.
In recent years, much of the emphasis has been on readmission reduction programs that include an array of noncondition‐specific strategies, programs such as the Society of Hospital Medicine's (SHM) Project Better Outcomes through Optimizing Safe Transitions (BOOST), Project Re‐Engineering Discharge (RED), Care Transitions Intervention, and the Transitional Care Model (Krishnan et al. 2015). For such programs, it may be difficult to implement for select conditions or patient populations, particularly if the same hospital staff are implementing these programs. If so, efforts to reduce readmissions for targeted conditions may not be separable from care processes for patients with nontargeted conditions.
Explaining the Effects of HRRP Implementation on Nontargeted Conditions: Nonpecuniary Incentives
Because reductions in readmissions have the potential to reduce hospital revenue, hospitals driven by financial interests will be incentivized to limit the impact of readmission reduction efforts to targeted conditions. Thus, the observed reductions in readmissions for nontargeted conditions suggest that factors other than the HRRP penalties, such as patient satisfaction and overall quality of care, may be affecting hospital behavior. In fact, we found that hospitals achieved larger readmission reductions for neurology and surgery relative to cardiorespiratory/cardiovascular conditions that are more clinically similar to the targeted conditions. This result is counterintuitive from a narrow spillover effects perspective, which would predict greater opportunities for spillover among clinically related conditions.
Policies and programs other than HRRP penalties may have contributed to the reductions in readmissions observed in our analysis. For example, the public reporting of readmissions for the three targeted conditions, which started in 2009, may have had lagged effects on readmissions that materialized during our study period. Similarly, the public reporting of the hospital‐wide readmission measure that started in 2013 may have affected hospitals’ behavior with respect to nontargeted conditions. As a result, the effects of public reporting on hospital reputation and ability to compete in its market may have contributed to efforts to reduce readmissions.
In assessing potential factors driving our results, it is interesting to note that we did not find evidence for spillover effects in the non‐Medicare patient populations in Florida and California. This is consistent with Carey and Lin who found no change in unadjusted readmissions among the non‐Medicare population in New York State. Collectively, our findings, based on non‐Medicare populations in three large states with differing healthcare patterns, provide evidence on the limits to the spillover effects of HRRP. It supports the notion that financial considerations may play a role in determining the hospitals’ response to the HRRP, but also suggests that interventions to reduce readmissions may be separable by patient populations. Even though hospitals may aim to achieve higher quality and patient satisfaction, they do so against cost constraints, which may lead them to identify the optimal size and scope of the readmission reduction initiatives to be implemented. More research is needed to fully understand the effects of the HRRP on non‐Medicare populations and validate our findings for other states.
Our study has certain limitations. First, potential lag time involved in policy response and the existence of other policies and programs implemented around the passage of the ACA may confound the relationship between the timing of the observed readmission reductions and the implementation of the HRRP. Second, patient comorbid conditions and illness severity may be partially captured in the analysis as they are based only on the index hospital claim. Finally, our results on the non‐Medicare population based on data from Florida and California may not be generalizable to the rest of the country.
This study presents empirical evidence that is consistent with the spillover benefits associated with the HRRP. We find that the potential spillover effects vary across condition and patient groups. Future research should explore the determinants of this variation to better understand how hospitals responded to incentives created by the HRRP. Specifically, more research is needed to better understand the different types of initiatives hospitals implement in response to the HRRP as well as hospitals’ decision‐making process that determines the size, scope, and content of these readmission reduction initiatives.
Supporting information
Appendix SA1: Author Matrix.
Table S1. List of Covariates.
Table S2. Estimates from Logistic Regressions of Readmission Probability for Non‐Targeted Conditions, 2007–2013.
Figure S1. Trends in Adjusted Readmission Rates for Nontargeted Conditions by Groups of Hospitals (Based on Reduction in Readmission Rates for Targeted Conditions), 2007–2013.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was supported by The Commonwealth Fund, a national, private foundation based in New York City that supports independent research on health care issues and makes grants to improve health care practice and policy. The views presented here are those of the authors and not necessarily those of The Commonwealth Fund, its directors, officers, or staff. KNG Health Consulting, the company with which all three authors are affiliated, has conducted prior work on hospital readmissions and the Hospital Readmissions Reduction Program for American Hospital Association, America's Essential Hospitals, and Association of American Medical Colleges. The authors wish to thank Eric C. Schneider for his valuable input on earlier drafts of this paper.
Disclosures: None.
Disclaimer: None.
Notes
AMI: 410.x0, 410.x1, heart failure: 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.xx, pneumonia: 480.0, 480.1, 480.2, 480.3, 480.8, 480.9, 481, 482.0, 482.1, 482.2, 482.30, 482.31, 482.32, 482.39, 482.40, 484.41, 482.42, 482.49, 482.81, 482.82, 482.83, 482.84, 482.89, 482.9, 483.0, 483.1, 483.8, 485, 486, 487.0, 488.11.
CMS’ hospital‐wide all‐cause unplanned readmission measure includes AMI in the cardiovascular condition group and heart failure and pneumonia in the cardiorespiratory condition group. While CMS includes these targeted conditions in constructing the cardiorespiratory and cardiovascular cohorts, we do not.
We conducted a sensitivity analysis by adding indicator variables for missing values to the model. The results are nearly identical to the results presented.
References
- Andersson, K. , Petzold M. G., Sonesson C., Lonnroth K., and Carlsten A.. 2006. “Do Policy Changes in the Pharmaceutical Reimbursement Schedule Affect Drug Expenditures? Interrupted Time Series Analysis of Cost, Volume and Cost per Volume Trends in Sweden 1986–2002.” Health Policy 79 (2): 231–43. [DOI] [PubMed] [Google Scholar]
- Boccuti, C. , and Casillas G.. 2015. “Aiming for Fewer Hospital U‐Turns: The Medicare Hospital Readmission Reduction Program” [accessed on July 1, 2017]. The Henry J. Kaiser Family Foundation. Available at http://kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/
- Bradley, E. H. , Curry L., Horwitz L. I., Sipsma H., Thompson J. W., Elma M., Walsh M. A., and Krumholz H. M.. 2012. “Contemporary Evidence about Hospital Strategies for Reducing 30‐day Readmissions: A National Study.” Journal of the American College of Cardiology 60 (7): 607–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley, E. H. , Curry L., Horwitz L. I., Sipsma H., Wang Y., Walsh M. N., Goldman D., White N., Pi I. L., and Krumholz H. M.. 2013. “Hospital Strategies Associated with 30‐Day Readmission Rates for Patients with Heart Failure. Circulation.” Cardiovascular Quality and Outcomes 6 (4): 444–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley, E. H. , Sipsma H., Horwitz L. I., Curry L., and Krumholz H. M.. 2014. “Contemporary Data about Hospital Strategies to Reduce Unplanned Readmissions: What Has Changed?” Journal of the American Medical Association Internal Medicine 174 (1): 154–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brufsky, J. W. , Ross‐Degnan D., Calabrese D., Gao X., and Soumerai S. B.. 1998. “Shifting Physician Prescribing to a Preferred Histamine‐2‐Receptor Antagonist: Effects of a Multifactorial Intervention in a Mixed‐Model Health Maintenance Organization.” Medical Care 36 (3): 321–32. [DOI] [PubMed] [Google Scholar]
- Carey, K. , and Lin M. Y.. 2015. “Readmissions to New York Hospitals Fell for Three Target Conditions from 2008 to 2012, Consistent with Medicare Goals.” Health Affairs 34 (6): 978–85. [DOI] [PubMed] [Google Scholar]
- Feldstein, A. C. , Smith D. H., Perrin N., Yang X., Simon S. R., Krall M., and Soumerai S. B.. 2006. “Reducing Warfarin Medication Interactions: An Interrupted Time Series Evaluation.” Archives of Internal Medicine 166 (9): 1009–15. [DOI] [PubMed] [Google Scholar]
- Gillings, D. , Makuc D., and Siegel E.. 1981. “Analysis of Interrupted Time Series Mortality Trends: An Example to Evaluate Regionalized Perinatal Care.” American Journal of Public Health 71 (1): 38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanes, E . 2015. “Emerging Heart Failure Strategies Improve Outcomes and Reduce Readmissions” [accessed on October 28, 2016]. Available at http://www.modernhealthcare.com/article/20150501/SPONSORED/150509999
- Jencks, S. F. , Williams M. V., and Coleman E. A.. 2009. “Rehospitalizations among Patients in the Medicare Fee‐for‐Service Program.” New England Journal of Medicine 360 (14): 1418–28. [DOI] [PubMed] [Google Scholar]
- Kripalani, S. , Theobald C. N., Anctil B., and Vasilevskis E. E.. 2014. “Reducing Hospital Readmission: Current Strategies and Future Directions.” Annual Review of Medicine 65: 471–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan, J. A. , Gussin H. A., Prieto‐Centurion V., Sullivan J. L., Zaidi F., and Thomashow B. M.. 2015. Integrating COPD Into Patient‐Centered Hospital Readmissions Reduction Programs. Chronic Obstructive Pulmonary Diseases (Miami, Fla.) 2 (1): 70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MedPAC . 2007. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington, DC: MedPAC. [Google Scholar]
- Soumerai, S. B. , Avorn J., Ross‐Degnan D., and Gortmaker S.. 1987. “Payment Restrictions for Prescription Drugs under Medicaid.” New England Journal of Medicine 317 (9): 550–6. [DOI] [PubMed] [Google Scholar]
- Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE) . 2015a. “2015 Condition‐Specific Measures Updates and Specifications Report: Hospital‐Level 30‐Day Risk‐Standardized Readmission Measures” [accessed on July 1, 2016]. Available at https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774371008
- Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE) . 2015b. “2015 Measure Updates and Specifications Report: Hospital‐Wide All‐Cause Unplanned Readmission Measure – Version 4.0” [accessed on July 1, 2016]. Available at https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774371008
- Zuckerman, R. B. , Sheingold S. H., Orav E. J., Ruhter J., and Epstein A. M.. 2016. “Readmissions, Observation, and the Hospital Readmissions Reduction Program.” New England Journal of Medicine 374 (16): 1543–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. List of Covariates.
Table S2. Estimates from Logistic Regressions of Readmission Probability for Non‐Targeted Conditions, 2007–2013.
Figure S1. Trends in Adjusted Readmission Rates for Nontargeted Conditions by Groups of Hospitals (Based on Reduction in Readmission Rates for Targeted Conditions), 2007–2013.


