Abstract
Aims
The aim of this study was to examine prescribing trends for benzodiazepines and Z‐drugs to General Medical Services (GMS) patients in Ireland.
Methods
A repeated cross‐sectional analysis of the national pharmacy claims database was conducted for GMS patients aged ≥16 years from 2005 to 2015. Prescribing rates per 1000 eligible GMS population were calculated with 95% confidence intervals (CIs). Negative binomial regression was used to determine longitudinal trends and compare prescribing rates across years, gender and age groups. Duration of supply and rates of concomitant benzodiazepine and Z‐drug prescribing were determined. Age (16–44, 45–64, ≥65 years) and gender trends were investigated.
Results
Benzodiazepine prescribing rates decreased significantly from 225.92/1000 population (95% CI 224.94–226.89) in 2005 to 166.07/1000 population (95% CI 165.38–166.75) in 2015 (P < 0.0001). Z‐drug prescribing rates increased significantly from 95.36/1000 population (95% CI 94.73–96.00) in 2005 to 109.11/1000 population (95% CI 108.56–109.67) in 2015 (P = 0.048). Approximately one‐third of individuals dispensed either benzodiazepines or Z‐drugs were receiving long‐term prescriptions (>90 days). The proportion of those receiving >1 benzodiazepine and/or Z‐drug concomitantly increased from 11.9% in 2005 to 15.3% in 2015. Benzodiazepine and Z‐drug prescribing rates were highest for older women (≥65 years) throughout the study period.
Conclusions
Benzodiazepine prescribing to the GMS population in Ireland decreased significantly from 2005 to 2015, and was coupled with significant increases in Z‐drug prescribing. The study shows that benzodiazepine and Z‐drug prescribing is common in this population, with high proportions of individuals receiving long‐term prescriptions. Targeted interventions are needed to reduce potentially inappropriate long‐term prescribing and use of these medications in Ireland.
Keywords: benzodiazepines, potentially inappropriate prescribing, primary care, Z‐drugs
What is Already Known about this Subject
Prescribing guidelines advocate that benzodiazepine and Z‐drug prescriptions should be limited to short‐term use (i.e. ≤4 weeks) to minimize the risk of adverse outcomes (e.g. dependence, withdrawal symptoms).
Guidelines are often not adhered to as long‐term prescribing and use of benzodiazepines and Z‐drugs persist across healthcare settings worldwide.
What this Study Adds
Benzodiazepine prescribing to the GMS eligible population aged ≥16 years in Ireland decreased significantly from 2005 to 2015 while Z‐drug prescribing increased significantly.
Prescribing of benzodiazepines and Z‐drugs is common in Ireland, with approximately one‐third of those dispensed these drugs receiving them for extended periods (>3 months).
Introduction
Benzodiazepines have multiple clinical indications, including anxiety and insomnia. Guidelines advocate that benzodiazepine prescriptions should be limited to short‐term use (i.e. ≤4 weeks) to minimize the risk of adverse outcomes (e.g. dependence, withdrawal symptoms) 1, 2. However, guidelines are often not adhered to as long‐term use persists worldwide 3. An estimated 3% of the general population use benzodiazepines for extended periods (>6 months) 4. Long‐term benzodiazepine use is potentially inappropriate and can give rise to a range of adverse effects including cognitive and psychomotor impairment, particularly in older people (≥65 years) 5. Benzodiazepine use has also been linked to numerous adverse events, including an increase of more than 50% in the likelihood of falls in older people 6.
Despite recognition of issues with benzodiazepines for decades, many countries have reported limited or no significant reduction in prescribing levels in recent years 7, 8, 9. For example, retrospective analysis of 133.3 million ambulatory care visits in the US, found no significant change in benzodiazepine prescribing in older adults from 2001 to 2010 7. In some instances, changes in benzodiazepine prescribing appear to have been offset by increases in Z‐drug hypnotic prescribing (e.g. http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=7430, http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=4348) 9, 10. Z‐drugs were originally promoted as favourable alternatives to benzodiazepines for insomnia because of their more selective hypnotic profile and shorter elimination half‐life values 11. Consequently, more favourable perceptions of Z‐drugs' associated benefits and potential for harms have been identified amongst prescribers compared to benzodiazepines 12, 13. However, there is a lack of compelling evidence of any clinically useful differences between both drug classes in terms of effectiveness, potential for adverse effects, dependence or abuse 14. Moreover, problems such as dependence have also been reported by individuals using Z‐drugs 15, 16. Hence, current evidence does not support prescribing Z‐drugs to reduce benzodiazepine prescribing.
In Ireland, concerns over long‐term benzodiazepine prescribing and the potential for dependence and misuse led to the Benzodiazepine Committee being established in 2000 17. This national, multidisciplinary committee was tasked with examining existing benzodiazepine prescribing in Ireland and making recommendations to foster rational prescribing practices and reduce inappropriate use. In addition to prescribing guidelines, numerous explicit criteria have been developed as indicators of prescribing appropriateness [e.g. PROMPT (PRescribing Optimally in Middle‐aged People's Treatments) criteria for middle‐aged people (45–64 years) 18, Beers criteria 19 and STOPP/START (Screening Tool of Older Person's Prescriptions/Screening Tool to Alert doctors to Right Treatment) criteria 20 for older people]. However, evidence to date suggests that the Committee's prescribing guidelines, as well as subsequent prescribing criteria have had little effect in improving benzodiazepine prescribing and use in Ireland 21, 22, 23, 24, 25. For example, a cross‐sectional analysis of Irish prescribing data for 338 801 older people in 2007, identified long‐term prescribing (defined as >4 weeks) of long‐acting benzodiazepines (half‐life >24 h) as one of the most common indicators of potentially inappropriate prescribing among the study population with a prevalence of 5% 24.
Most previous evaluations of benzodiazepine and Z‐drug prescribing practices in Ireland have focused on older people, involved the application of STOPP and only included long‐acting benzodiazepines 21, 22, 23, 24, 25. Given evidence linking benzodiazepine use to adverse outcomes in different population groups in Ireland (e.g. falls in older populations 26, mortality in polysubstance misusers 27, cases of deliberate self‐harm 28, 29), it is important to examine prescribing patterns of all benzodiazepines and Z‐drugs across the adult population to determine if prescribing practices have improved and to identify populations where targeted interventions are required to improve safe and rational use.
This study aimed to examine the prescribing of benzodiazepines and Z‐drugs in Ireland over an 11‐year period using a national administrative pharmacy claims database. The objectives were to establish the prescribing rates and secular trends for benzodiazepines and Z‐drugs, including changes in individual medications prescribed, duration of supply, therapeutic duplication (i.e. concomitant prescribing of >1 benzodiazepine or Z‐drug, or concomitant prescribing of both drug classes). Prescribing rates and secular trends were also investigated across years based on individual drugs and drug categories (i.e. hypnotics versus anxiolytics, short‐acting versus long‐acting benzodiazepines), individuals' gender and age profiles.
Methods
Study design and study population
A repeated cross‐sectional analysis was conducted using individual‐level dispensing data obtained from the Irish General Medical Services (GMS) pharmacy claims database. The GMS scheme is administered by the Health Service Executive (HSE) – Primary Care Reimbursement Services (PCRS), which is responsible for reimbursement to community pharmacies of all claims made by GMS‐eligible individuals. The GMS pharmacy claims database represents the single largest pharmacy claims dataset in Ireland. Detailed information on the GMS scheme has previously been published (see 30) and key summary information is provided below.
Data were included on all GMS‐eligible individuals aged ≥16 years in Ireland over the study period (1 January 2005–31 December 2015). Individuals aged ≥16 years were included because pre‐defined age bands are used to categorize individuals within the database (i.e. 16–44, 45–64, ≥65 years).
The GMS scheme provides free health services based on means testing and age (those >70 years have higher means thresholds) 30. For prescription medications, a monthly co‐payment (€0.50 per item) was introduced in October 2010. This co‐payment increased over time to €2.50 per item (subject to a limit of €25 per family per month) as of December 2013, and this fee structure applied for the remainder of the study period. As of 2015, the scheme covered 37.8% of the general Irish population 31. However, as the scheme is means‐tested, it over‐represents socially‐deprived populations. Previously, all adults aged ≥70 years were automatically eligible for the scheme. However, since January 2009, a higher income threshold has applied to this cohort compared to the general population. The scheme currently covers 78.2% of the population aged 70 years and over 31, 32. The pharmacy claims database contains basic demographic information and details on monthly dispensed medications, coded using the World Health Organisation Anatomical Therapeutic Chemical (ATC) classification system, for each individual within the scheme 33. As the data were anonymized and analysed at group level, ethical approval was not required.
Data analysis
For this analysis, all benzodiazepine and Z‐drug prescriptions were identified using relevant ATC codes [i.e. antiepileptics (N03AE), anxiolytics (N05BA), hypnotics/sedatives (N05CD, N05CF)] 33 and subsequently extracted from the database. All benzodiazepines and Z‐drugs licensed for use during the study period were included in the analysis (Supporting Information, Table S1). Benzodiazepines were further subcategorized according to their plasma half‐life (t 1/2) as long‐acting (t 1/2 > 24 h) or short‐acting (t 1/2 ≤ 24 h) 34, 35.
Prescribing rates were calculated per 1000 GMS population per year and associated 95% confidence intervals (CIs) for all GMS‐eligible individuals aged ≥16 years, as identified from annual HSE‐PCRS reports across all study years (2005–2015) (available from: https://www.sspcrs.ie). Prescribing rates were interpreted as the rate of individuals receiving at least one benzodiazepine or Z‐drug prescription per 1000 GMS population. Therapeutic duplication, whereby patients were prescribed >1 benzodiazepine and/or Z‐drug concomitantly in the same calendar month, was identified using ATC codes 33.
The average number of defined daily doses (DDDs) per prescription was calculated. DDDs were calculated for oral formulations of all benzodiazepines and Z‐drugs that were extracted from the database using standard reference values 33. The average number of DDDs per prescription per study year was calculated by dividing the total DDD quantity by the number of claims dispensed for all included drugs.
Duration of supply for each individual was defined as the maximum length of any consecutive benzodiazepine or Z‐drug use over the study period with the maximum duration as the variable of interest. The relationship between duration of benzodiazepine/Z‐drug use and both age and gender was investigated using Chi‐square tests. New users were identified as individuals without any benzodiazepine or Z‐drug dispensing in the previous 12 months. The GMS dataset had 100% eligibility coverage for the year before the incidence cases, where information on coverage of eligibility was available (97% of cases).
Trends in prescribing rates were examined using a negative binomial regression model. The log of the GMS population was used as the offset term and year, age group, gender and all possible interactions between these variables were included as fixed‐effects in the model. Tests for trends in proportions over time were examined using logistic regression with year as a continuous variable. P‐values < 0.05 were deemed significant. Data analyses were performed using SAS statistical software v.9.4 (SAS Institute, Inc., Cary, NC, USA).
Nomenclature of targets and ligands
Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY 36, and are permanently archived in the Concise Guide to PHARMACOLOGY 2017/18.
Results
Population sample
During the study period, the number of GMS‐registered individuals aged ≥16 years in Ireland ranged from 914 505 to 1 427 880. The proportion of women declined from 57.2% in 2005 to 54.3% in 2015. There was an overall decline in the proportion of individuals aged ≥65 years and increases in the proportions aged 16–44 years and 45–64 years. A detailed overview of the sample population's demographic profile is provided in Supporting Information, Table S2.
Prescribing trends
Benzodiazepine prescribing rates decreased significantly by 26.5% between 2005 and 2015 (P < 0.0001), with consistent decreases in prescribing rates during the study period except for 2008 and 2014 (Figure 1a). The percentage change in Z‐drug prescribing rates increased by 14.4% from 2005 to 2015 (P = 0.048). Prescribing rates increased steadily from 2005 to 2011 and then stabilized following a reduction in 2012.
Figure 1.
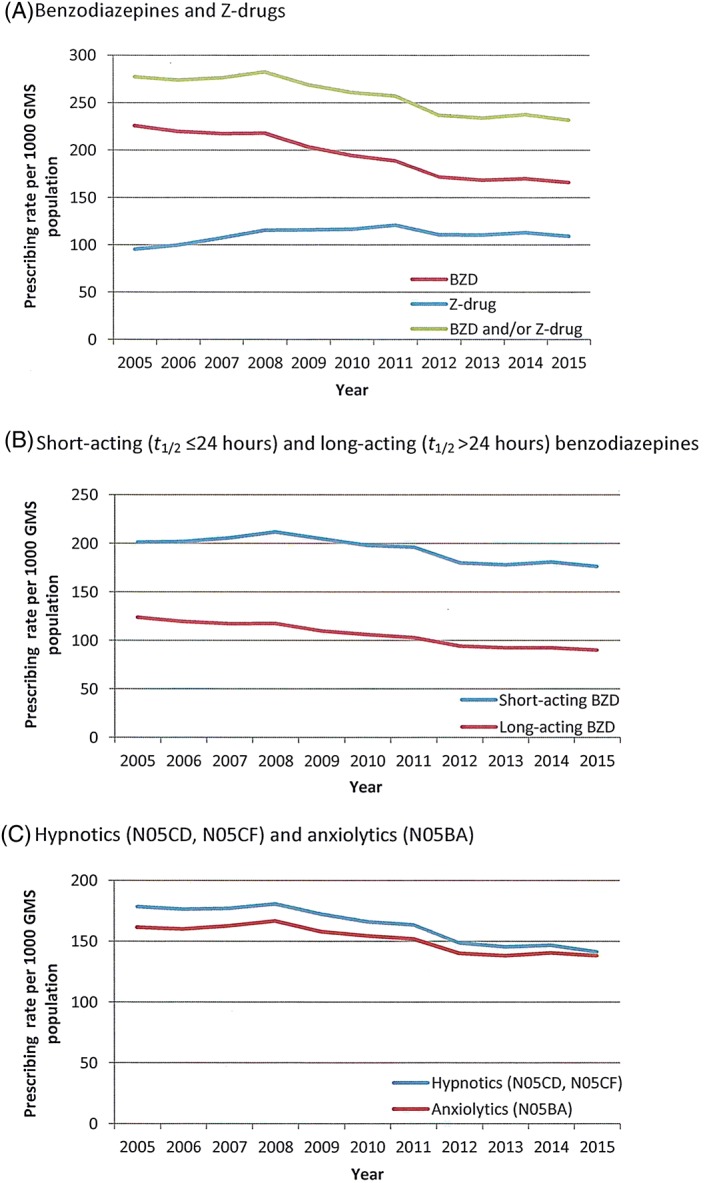
Prescribing rates for (A) benzodiazepines and Z‐drugs, (B) short‐acting and long‐acting benzodiazepines [BZDs] and (C) hypnotics and anxiolytics issued to GMS‐eligible individuals aged ≥16 years from 2005 to 2015
The five most commonly dispensed drugs between 2005 and 2015 were http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=3364, http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=7111, http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=7300, zopiclone and zolpidem (Figure 2). The total proportion of all benzodiazepine and Z‐drug items dispensed for which these drugs accounted increased each year over the study period (range 65.5–77.52%). Of these drugs, temazepam was the only drug with consistent decreases in prescribing rates. There was an overall increase in the prescribing rates of alprazolam, zopiclone and zolpidem, while the prescribing rate of diazepam decreased slightly. Detailed prescribing trend data for individual drugs is provided in Supporting Information, Table S3.
Figure 2.
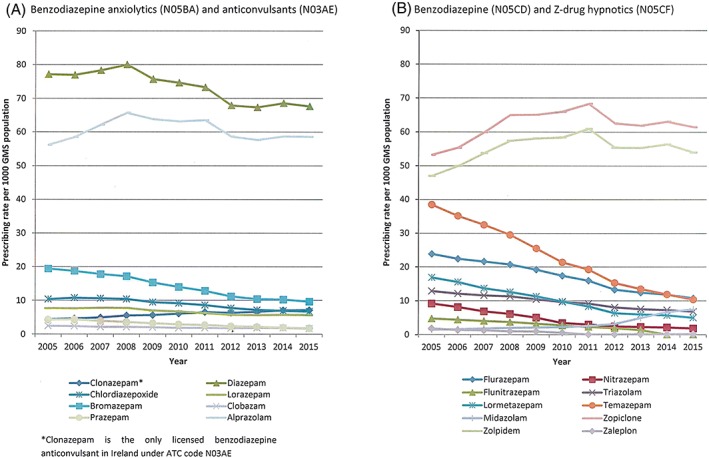
Prescribing rates for individual (A) benzodiazepine anxiolytics and anticonvulsants and (B) benzodiazepine and Z‐drug hypnotics issued to GMS‐eligible individuals aged ≥16 years from 2005 to 2015
Prescribing rates for short‐acting benzodiazepines remained consistently higher than long‐acting benzodiazepines across the study period (Figure 1b). Prescribing rates for long‐acting benzodiazepines showed consistent decreases during the study period. The overall decrease in prescribing rates was larger for long‐acting benzodiazepines (decreased by 27.1% from 123.8 per 1000 GMS population in 2005 to 90.2 per 1000 GMS population in 2015) compared to short‐acting benzodiazepines (decreased by 12.4% from 200.9 per 1000 GMS population in 2005 to 175.9 per 1000 GMS population in 2015). Similar trends were observed when the medications were grouped as anxiolytics (N05BA) and hypnotics (N05CD, N05CF) [Figure 1c].
The proportion of individuals receiving duplicate benzodiazepine prescriptions significantly decreased from 18.1% in 2005 to 13% in 2015 (test for trend, P < 0.001; Figure 3). The proportion of individuals receiving duplicate Z‐drug prescriptions remained largely stable (2.7% in 2015), while the proportion of individuals receiving combinations of benzodiazepines and Z‐drugs significantly increased from 11.9% in 2005 to 15.3% in 2015 (time trend, P < 0.001).
Figure 3.
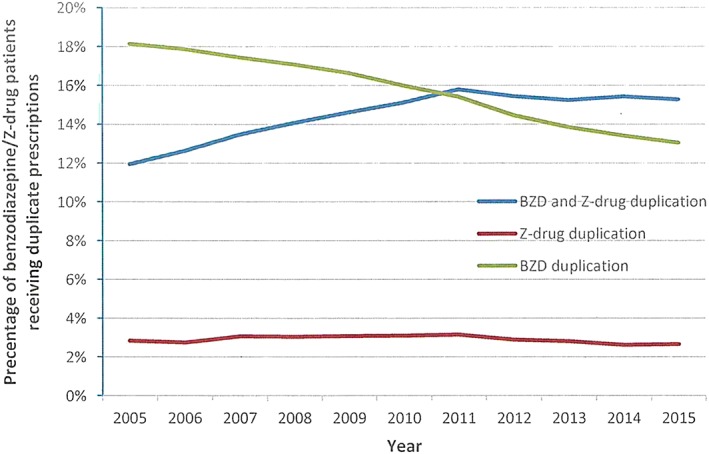
Proportion of GMS‐eligible individuals aged ≥16 years receiving duplicate prescriptions involving combinations of benzodiazepines and/or Z‐drugs from 2005 to 2015
Quantity of supply
The average number of DDDs dispensed per benzodiazepine prescription (monthly prescriptions) to individuals per year decreased during the study period from 20.7 DDDs (standard deviation [SD] ±15.2) in 2005 to 18 DDDs (SD ±15.7) per month in 2015. The average number of DDDs dispensed per Z‐drug prescription to individuals per year remained largely stable over time [26.1 DDDs (SD ±11.9) in 2005; 25.6 DDDs (SD ±12.2) in 2015]. The majority of benzodiazepine and Z‐drug prescriptions dispensed each month were for periods of greater than 3 weeks (83.7–90.8% of benzodiazepine prescriptions, 84.4–89.3% of Z‐drug prescriptions).
New users
Incidence rates for new benzodiazepine and Z‐drug prescriptions decreased throughout the study period and were consistently higher for women than men (Figure 4). The decrease in incidence rate for benzodiazepine prescriptions was greatest in those aged 45–64 years (decreased by 58.0%) compared to other age groups (decreased by 49.2% in individuals aged 16–44 years and by 50.5% in individuals aged ≥65 years). Similar trends were observed with the incidence rate of new Z‐drug prescriptions, however, the magnitude of these changes was smaller for each age category (decreased by 46.5% in individuals aged 16–44 years, by 49.2% in individuals aged 45–64 years, by 39.6% in individuals aged ≥65 years).
Figure 4.
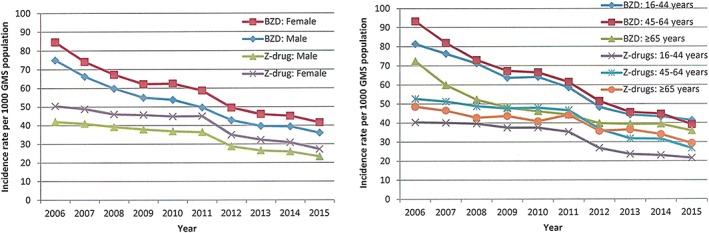
Incidence rates for new benzodiazepine (BZD) and Z‐drug prescriptions issued to GMS‐eligible patients aged ≥16 years from 2006 to 2015 according to gender and age
Long‐term use
Approximately one‐third of individuals dispensed these medications were receiving benzodiazepine (30.2%) and Z‐drug prescriptions (34.3%) on a consecutive basis for >3 months (Figure 5).
Figure 5.

Duration of consecutive benzodiazepine and Z‐drug use for GMS‐eligible individuals aged ≥16 years during study period
Gender and age
Benzodiazepine prescribing rates decreased significantly over time for both men and women (P < 0.0001). The interaction between age and year was only significant in women (P = 0.007) and appeared to indicate a slower decline in prescribing rates for women aged 16–44 years and ≥65 years compared to women aged 45–64 years (Supporting Information, Figure S1).
Z‐drug prescribing rates decreased significantly in men over time (P < 0.0001). The increase in prescribing rates in women was not statistically significant (P = 0.08). The interaction between age and year was significant in both men and women (P < 0.001) with the largest increases occurring in individuals aged ≥65 years across both genders (Supporting Information, Figure S1).
Significantly higher proportions of women were receiving benzodiazepine prescriptions for more than 6 months compared to men (P < 0.0001) (Supporting Information, Figure S2). A significantly higher proportion of older individuals (≥65 years) were receiving benzodiazepine prescriptions for periods exceeding 21 days compared to younger cohorts (P < 0.0001).
Similar trends were observed with Z‐drugs based on individuals' gender (Supporting Information, Figure S2). A significantly higher proportion of older individuals were receiving Z‐drug prescriptions for periods exceeding 60 days compared to younger cohorts (P < 0.0001).
Discussion
This study examined prescribing trends for benzodiazepines and Z‐drugs in Ireland from 2005 to 2015 using national pharmacy claims data for the GMS population aged ≥16 years. An overall significant reduction in benzodiazepine prescribing was observed, coupled with significant increases in Z‐drug prescribing, which mirrors trends observed in other countries 9, 10. However, it is difficult to make direct comparisons between the observed prescribing rates and those reported in other countries because of differences in the nature of the dataset, sample population and time periods examined 7, 8, 9. This is a challenge with pharmacoepidemiological studies as, even where consistent methods have been applied to multiple European databases, benzodiazepine and Z‐drug prescribing rates have varied considerably and this has been attributed to the characteristics of individual datasets, as well as clinical and policy factors related to the medications examined 37. Compared to other population database studies, prescribing rates from 2005 to 2015 for benzodiazepines and Z‐drugs in the GMS‐eligible population appear to be comparable to, if not higher than, most recently published data from various countries across Europe 37, 38, 39, Asia 40 and the US 10. The demographics of those receiving benzodiazepines and Z‐drugs in Ireland are consistent with the literature, whereby long‐term use was most common in older women 3.
The findings may suggest evidence of progress in reducing benzodiazepine prescribing in Ireland with an absolute reduction of 6% in the proportion of individuals on the GMS dispensed these medications between 2005 and 2015. However, any observed progress in reducing benzodiazepine prescribing levels in Ireland has, to date, been slow, and offset by increased Z‐drug prescribing, despite reports highlighting problems with both drug classes, such as falls 41. As data were only available from 2005, it was not possible to establish a true picture of national baseline prescribing amongst the GMS population prior to the Benzodiazepine Committee's report and guidelines, or assess their immediate impact 1, 17. Previous reports have, however, indicated that these publications had little, if no, immediate impact on national prescribing practices 42, 43. Very little change was observed in benzodiazepine prescribing between 2005 and 2008. It is beyond the scope of the data to establish the main reasons for more sizeable decreases observed between 2008 and 2011. It may be attributable to changes in GMS scheme eligibility and the reduction in the number of older people registered on the scheme, as this cohort is frequently identified as the largest consumers of benzodiazepines 44. Therapeutic switching to Z‐drugs may also have occurred. These factors may also have contributed to the small fluctuations in prescribing rates observed for individual drugs during the study period. Interestingly, the observed reduction between 2011 and 2012 preceded the introduction of a national auditing system 45.
Despite the overall decrease in benzodiazepine prescribing, the data do not indicate any substantial improvement in prescribing practices. Long‐term prescribing remains common with almost one‐third of individuals receiving prescriptions for more than 3 months. This is comparable to recent data from the UK 46 and US 47. In addition, the most common quantities dispensed were for 4‐week periods, despite guidelines recommending that individuals receiving these medications on a long‐term basis only be issued with small medication quantities at a time (≤7‐day supply) 1. Moreover, prescribing levels have stabilized in recent years, indicating that any progress has stalled and that clear scope exists for further reductions. This is consistent with data from other countries and further highlights the need for targeted interventions to improve the prescribing and use of these medications 7, 8, 9.
Incidence rates for new benzodiazepine and Z‐drug prescriptions decreased over time and could be interpreted as an indication that prescribers are more cautious in initiating patients on these medications. However, as the study was unable to differentiate between continuous users and patients who had significant periods without a prescription after initial exposure, this observation could be misleading. New and existing prescribing practice needs to be carefully monitored, as inappropriate use of these medications and dependence has also been identified among younger and middle‐aged populations 16, 48, 49. Therefore, without targeted interventions aimed at curtailing initiation; restricting duration of prescriptions to recommended periods; and weaning patients off these medicines, inappropriate long‐term use of benzodiazepines and Z‐drugs could persist for many generations to come. Identifying the most effective intervention approaches to achieve these aims remains challenging. Numerous interventions have been conducted to date aimed at increasing appropriate prescribing and reducing long‐term use of benzodiazepines and Z‐drugs, including education of patients and healthcare professionals, audit and feedback, computerized alerts, as well as psychological and pharmacological interventions 50, 51. However, heterogeneity in study design and intervention approaches, as well as poor descriptions of interventions in published studies has limited the pooling of outcome data and generation of pooled effect estimates to determine the most effective interventions and allow replication in other clinical settings 47, 48.
The apparent shift towards increased Z‐drug prescribing is not a favourable development. Z‐drug prescribing appears to be following a pattern previously observed with benzodiazepines, with a large proportion of patients receiving a month's supply on each prescription and prescriptions for durations in excess of 30 days, contrary to prescribing guideline recommendations 14. This also suggests a lack of awareness among prescribers and patients of the lack of evidence to support Z‐drug use in place of benzodiazepines as in other countries 12, 13, 15.
This study was completed as new legislation was implemented in Ireland in 2017 that introduced additional prescribing requirements for benzodiazepines and Z‐drugs (e.g. total quantity prescribed must now be specified in words and figures) 52. Possession of these medications without a prescription is also now a criminal offence 52. It is unclear to what extent, if any, this will impact on current practice. The findings show that temazepam prescribing was comparatively higher than other benzodiazepines until recent years, despite more stringent legal restrictions on temazepam prescribing since 1993 53. It is also important to note, that previous legislative restrictions on benzodiazepine prescribing have been associated with increased prescribing of less favourable alternatives (e.g. phenobarbital) and this needs to be avoided 54.
The study's main strength is that it provides the first detailed analysis of benzodiazepine and Z‐drug prescribing trends on a national scale using a large, high‐quality, valid and accurate data source for measuring benzodiazepine and Z‐drug use amongst the GMS population aged ≥16 years in Ireland 30. Previous reports have been restricted to specific subgroups (e.g. GMS patients aged <15 years) 55 or geographical regions in Ireland 42, 43. The study demonstrates how the Benzodiazepine Committee's recommendation that national prescribing data be reviewed and reported at regular intervals can be fulfilled 17. The study also highlights guideline recommendations that are not being adhered to, with large proportions of patients receiving long‐term prescriptions, and a month's supply of medication at a time 1. These findings could help in developing targeted interventions to improve prescribing practices.
In terms of study limitations, it must be noted that the GMS database represents approximately one‐third of the Irish population and is over‐representative of individuals with a lower socioeconomic status, women and older age 30. It is difficult to determine the impact of this on the reported prescribing rates. On one hand, benzodiazepine prescribing is more common in individuals with a lower socioeconomic status, which could lead to an overestimation of true prescribing rates 56. However, the demographic shifts observed between 2005 and 2015 show that older individuals appear to be under‐represented. As benzodiazepine use is more common in older patients 44, this could equally support the claim that prescribing rates have been underestimated. It must also be noted that complete data on prescriptions issued to patients attending private doctors in Ireland are not available and, therefore, it is not possible to determine the impact of the economic challenges encountered in Ireland between 2008 and 2012 and the consequent increase the number of GMS‐eligible individuals on prescribing trends for these medications. Decreases in benzodiazepine prescribing on public health schemes in Australia were previously coupled with increased prescribing on private prescriptions 57. Until electronic health records are available for all patients, it will not be possible to determine the overall prescribing rates for benzodiazepines and Z‐drugs in Ireland. An additional study limitation is that the GMS database does not contain any information about patients' clinical indications or the setting in which prescriptions were issued. Consequently, prescribing rates could not be adjusted for clinical conditions in which long‐term benzodiazepine exposure could be entirely appropriate (e.g. epilepsy). This prevents a more detailed investigation into factors associated with prescribing of these medications, as well as a true determination of clinical appropriateness and assessment of prescribing outcomes.
Although the data indicate that reductions in benzodiazepine prescribing have been offset to an extent by increases in Z‐drug prescribing, it is not known whether these changes have led to prescribing changes for other psychotropic medications. This requires a more detailed follow‐up study. The study utilized primary care dispensing data from a national pharmacy claims database, which allows for medicine use at patient level to be explored. Unlike prescribing databases, dispensing data is more likely to reflect actual medicine use by patients. However, the data does not tell us if patients actually took the medicines dispensed. Nevertheless, the data show that considerable quantities of these medications are circulating among the general population with potential for diversion and a range of adverse consequences. For example, the number of cases presenting to drug treatment centres in Ireland with benzodiazepines or Z‐drugs as the main problem substance has increased continually in recent years 58. Similar problems have also been observed regarding accumulation of unused and undisposed of opioids prescribed postoperatively 59.
Conclusions
This study found an overall decrease in benzodiazepine prescribing in Ireland over an 11‐year period coupled with an increase in Z‐drug prescribing. Long‐term prescribing of benzodiazepines and Z‐drugs remains common and is not limited to older people with the potential to perpetuate continued long‐term use for future generations. The findings highlight the need to revisit existing guidelines and conduct more detailed evaluations regarding their implementation to reduce potentially inappropriate long‐term use of benzodiazepines and Z‐drugs in Ireland.
Competing Interests
The authors have stated explicitly that there are no conflicts of interest in connection with this article. This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors. K.B. and C.C. are funded by the Health Research Board (HRB) in Ireland (grant code RL‐15‐1579) but the funder had no role in the conduct of the study.
The authors thank the HSE‐PCRS for supplying the data on which the study was based.
Contributors
C.A.C. conceived and designed the study and led the writing of the paper. C.R. conceived and designed the study, contributed to the interpretation of data and reviewed and critiqued draft manuscripts of the paper. C.C. and C.P.B. contributed to the interpretation of data and reviewed and critiqued draft manuscripts of the paper. K. Bennett conceived and designed the study, provided data and carried out the statistical analysis, and acted as joint lead for the writing of the paper. All authors approved the final submission.
Supporting information
Table S1 Benzodiazepines and Z‐drugs classified according to ATC code and half‐life value
Table S2 Proportions of GMS eligible individuals during study period categorized according to gender and age
Table S3 Prescribing rates per 1000 GMS population for individual benzodiazepine and Z‐drugs
Figure S1 Prescribing rates for (a) benzodiazepines (BZDs) and (b) Z‐drugs issued to GMS eligible patients aged ≥16 years from 2005 to 2015 according to gender and age
Figure S2 Duration of consecutive (a) benzodiazepine and (b) Z‐drug use among patients during study period according to gender and age
Cadogan, C. A. , Ryan, C. , Cahir, C. , Bradley, C. P. , and Bennett, K. (2018) Benzodiazepine and Z‐drug prescribing in Ireland: analysis of national prescribing trends from 2005 to 2015. Br J Clin Pharmacol, 84: 1354–1363. doi: 10.1111/bcp.13570.
References
- 1. Benzodiazepine Committee . Benzodiazepines: good practice guidelines for clinicians. Dublin: Department of Health and Children, 2002. Available at http://www.drugsandalcohol.ie/5349 (last accessed 8 August 2017).
- 2. The Royal Australian College of General Practitioners . Prescribing drugs of dependence in general practice, Part B – benzodiazepines. Victoria, Australia, 2015. Available at http://www.drugsandalcohol.ie/24380 (last accessed 8 August 2017).
- 3. Donoghue J, Lader M. Usage of benzodiazepines: a review. Int J Psychiatry Clin Pract 2010; 14: 78–87. [DOI] [PubMed] [Google Scholar]
- 4. Kurko TA, Saastamoinen LK, Tahkapaa S, Tuulio‐Henriksson A, Taiminen T, Tiihonen J, et al Long‐term use of benzodiazepines: Definitions, prevalence and usage patterns – a systematic review of register‐based studies. Eur Psychiatry 2015; 30: 1037–1047. [DOI] [PubMed] [Google Scholar]
- 5. Lader M. Benzodiazepine harm: how can it be reduced? Br J Clin Pharmacol 2014; 77: 295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al Meta‐analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009; 169: 1952–1960. [DOI] [PubMed] [Google Scholar]
- 7. Marra EM, Mazer‐Amirshahi M, Brooks G, van den Anker J, May L, Pines JM. Benzodiazepine prescribing in older adults in U.S. ambulatory clinics and emergency departments (2001–10). J Am Geriatr Soc 2015; 63: 2074–2081. [DOI] [PubMed] [Google Scholar]
- 8. Benard‐Laribiere A, Noize P, Pambrun E, Bazin F, Verdoux H, Tournier M, et al Trends in incident use of benzodiazepines and Z‐drugs in France from 2006 to 2012: a population‐based study. Pharmacoepidemiol Drug Saf 2017; 26: 162–166. [DOI] [PubMed] [Google Scholar]
- 9. Alessi‐Severini S, Bolton JM, Enns MW, Dahl M, Collins DM, Chateau D, et al Use of benzodiazepines and related drugs in Manitoba: a population‐based study. CMAJ Open 2014; 2: E208–E216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaufmann CN, Spira AP, Alexander GC, Rutkow L, Mojtabai R. Trends in prescribing of sedative‐hypnotic medications in the USA: 1993–2010. Pharmacoepidemiol Drug Saf 2016; 25: 637–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Drover DR. Comparative pharmacokinetics and pharmacodynamics of short‐acting hypnosedatives: zaleplon, zolpidem and zopiclone. Clin Pharmacokinet 2004; 43: 227–238. [DOI] [PubMed] [Google Scholar]
- 12. Siriwardena AN, Qureshi Z, Gibson S, Collier S, Latham M. GPs' attitudes to benzodiazepine and 'Z‐drug' prescribing: a barrier to implementation of evidence and guidance on hypnotics. Br J Gen Pract 2006; 56: 964–967. [PMC free article] [PubMed] [Google Scholar]
- 13. Hoffmann F. Perceptions of German GPs on benefits and risks of benzodiazepines and Z‐drugs. Swiss Med Wkly 2013; 143: w13745. [DOI] [PubMed] [Google Scholar]
- 14. National Institute for Health and Clinical Excellence . Guidance on the use of zaleplon, zolpidem and zopiclone for the short‐term management of insomnia. London: National Institute for Health and Care Excellence, 2004. Available at https://www.nice.org.uk/guidance/ta77 (last accessed 8 August 2017).
- 15. Siriwardena AN, Qureshi MZ, Dyas JV, Middleton H, Orner R. Magic bullets for insomnia? Patients' use and experiences of newer (Z drugs) versus older (benzodiazepine) hypnotics for sleep problems in primary care. Br J Gen Pract 2008; 58: 417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guerlais M, Grall‐Bronnec M, Feuillet F, Gerardin M, Jolliet P, Victorri‐Vigneau C. Dependence on prescription benzodiazepines and Z‐drugs among young to middle‐aged patients in France. Subst Use Misuse 2015; 50: 320–327. [DOI] [PubMed] [Google Scholar]
- 17. Benzodiazepine Committee . Report of the Benzodiazepine Committee Dublin, Ireland: Department of Health and Children, 2002. Available at http://www.drugsandalcohol.ie/5348 (last accessed 8 August 2017)
- 18. Cooper JA, Ryan C, Smith SM, Wallace E, Bennett K, Cahir C, et al The development of the PROMPT (PRescribing Optimally in Middle‐aged People's Treatments) criteria. BMC Health Serv Res 2014; 14: 484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. American Geriatrics Society . American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2015; 63: 2227–2246. [DOI] [PubMed] [Google Scholar]
- 20. Gallagher P, Ryan C, Byrne S, Kennedy J, O'Mahony D. STOPP (Screening Tool of Older Person's Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46: 72–83. [DOI] [PubMed] [Google Scholar]
- 21. Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross‐sectional study. BMJ Open 2015; 5: e008656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ryan C, O'Mahony D, Kennedy J, Weedle P, Byrne S. Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol 2009; 68: 936–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ryan C, O'Mahony D, Kennedy J, Weedle P, Cottrell E, Heffernan M, et al Potentially inappropriate prescribing in older residents in Irish nursing homes. Age Ageing 2013; 42: 116–120. [DOI] [PubMed] [Google Scholar]
- 24. Cahir C, Fahey T, Teeling M, Teljeur C, Feely J, Bennett K. Potentially inappropriate prescribing and cost outcomes for older people: a national population study. Br J Clin Pharmacol 2010; 69: 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cahir C, Fahey T, Teljeur C, Bennett K. Prescriber variation in potentially inappropriate prescribing in older populations in Ireland. BMC Fam Pract 2014; 15: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McMahon CG, Cahir CA, Kenny RA, Bennett K. Inappropriate prescribing in older fallers presenting to an Irish emergency department. Age Ageing 2014; 43: 44–50. [DOI] [PubMed] [Google Scholar]
- 27. Bellerose D, Lyons S, Carew AM, Walsh S, Long J. Problem benzodiazepine use in Ireland: treatment (2003 to 2008) and deaths (1998 to 2007). HRB Trends Series 9. 2010; Dublin, Ireland: Health Research Board. Available at http://www.drugsandalcohol.ie/14287 (last accessed 8 August 2017).
- 28. National Suicide Research Foundation . National Registry of Deliberate Self Harm Annual Report 2011. Cork, Ireland: National Suicide Research Foundation, 2012. Available at http://www.nsrf.ie/publications/reports (last accessed 8 August 2017).
- 29. National Suicide Research Foundation . National Registry of Deliberate Self Harm Annual Report 2010. Cork, Ireland: National Suicide Research Foundation, 2011. Available at http://www.nsrf.ie/publications/reports (last accessed 8 August 2017).
- 30. Sinnott SJ, Bennett K, Cahir C. Pharmacoepidemiology resources in Ireland – an introduction to pharmacy claims data. Eur J Clin Pharmacol 2017; 73: 1449–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Health Service Executive . Primary Care Reimbursement Service: Statistical Analysis of Claims and Payments 2015. Dublin, Ireland: Health Service Executive, 2015. Available at http://www.hse.ie/eng/staff/PCRS/PCRS_Publications/PCRS-statistical-analysis-of-claims-and-payments-2015.pdf (last accessed 8 August 2017).
- 32. Central Statistics Office . Census of Population 2016 – Profile 3 An Age Profile of Ireland. Dublin, Ireland, 2017. Available at http://www.cso.ie/en/statistics (last accessed 22 August 2017).
- 33. WHO Collaborating Centre for Drug Statistics Methodology . Guidelines for ATC classification and DDD assignment 2012; Oslo, Norway. Available at https://www.whocc.no/filearchive/publications/2017_guidelines_web.pdf (last accessed 8 August 2017).
- 34. Ashton H. Benzodiazepines: how they work and how to withdraw (also known as The Ashton Manual). Secondary Benzodiazepines: how they work and how to withdraw (also known as The Ashton Manual) 2002. Available at http://www.benzo.org.uk/manual/index.htm (last accessed 8 August 2017).
- 35. Passaro A, Volpato S, Romagnoni F, Manzoli N, Zuliani G, Fellin R. Benzodiazepines with different half‐life and falling in a hospitalized population: The GIFA study. Gruppo Italiano di Farmacovigilanza nell'Anziano. J Clin Epidemiol 2000; 53: 1222–1229. [DOI] [PubMed] [Google Scholar]
- 36. Harding SD, Sharman JL, Faccenda E, Southan C, Pawson AJ, et al The IUPHAR/BPS guide to PHARMACOLOGY in 2018: updates and expansion to encompass the new guide to IMMUNOPHARMACOLOGY. Nucl Acids Res 2018; 46: D1091–D1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Huerta C, Abbing‐Karahagopian V, Requena G, Oliva B, Alvarez Y, Gardarsdottir H, et al Exposure to benzodiazepines (anxiolytics, hypnotics and related drugs) in seven European electronic healthcare databases: a cross‐national descriptive study from the PROTECT‐EU Project. Pharmacoepidemiol Drug Saf 2016; 25 (S1): 56–65. [DOI] [PubMed] [Google Scholar]
- 38. Sakshaug S, Handal M, Hjellvik V, Berg C, Ripel A, Gustavsen I, et al Long‐term use of Z‐hypnotics and co‐medication with benzodiazepines and opioids. Basic Clin Pharmacol Toxicol 2017; 120: 292–298. [DOI] [PubMed] [Google Scholar]
- 39. Cloos JM, Bocquet V, Rolland‐Portal I, Koch P, Chouinard G. Hypnotics and triazolobenzodiazepines – best predictors of high‐dose benzodiazepine use: results from the Luxembourg National Health Insurance Registry. Psychother Psychosom 2015; 84: 273–283. [DOI] [PubMed] [Google Scholar]
- 40. Takeshima N, Ogawa Y, Hayasaka Y, Furukawa TA. Continuation and discontinuation of benzodiazepine prescriptions: a cohort study based on a large claims database in Japan. Psychiatry Res 2016; 237: 201–207. [DOI] [PubMed] [Google Scholar]
- 41. Richardson K, Bennett K, Kenny RA. Polypharmacy including falls risk‐increasing medications and subsequent falls in community‐dwelling middle‐aged and older adults. Age Ageing 2015; 44: 90–96. [DOI] [PubMed] [Google Scholar]
- 42. Flynn K. Minor tranquillisers and sedatives: use and misuse in the West of Ireland. Galway, Ireland: Western Region Drugs Task Force, 2009. Available at http://www.drugsandalcohol.ie/11506 (last accessed 8 August 2017).
- 43. Henman M, Vivero L, Gustafsson A, Mulvenna K. Benzodiazepine usage in the North Eastern Health Board region of the Republic of Ireland. Trinity College Dublin, 2004. Available at http://www.drugsandalcohol.ie/12669 (last accessed 8 August 2017).
- 44. Rosman S, Le Vaillant M, Pelletier‐Fleury N. Gaining insight into benzodiazepine prescribing in general practice in France: a data‐based study. BMC Fam Pract 2011; 12: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shannon J. HSE benzodiazepine letters to encourage quality prescribing. Medical Independent website, 2012. Available at http://www.drugs.ie/news/article/hse_benzodiazepine_letters_to_encourage_quality_prescribing (last accessed 8 August 2017).
- 46. Davies J, Rae TC, Montagu L. Long‐term benzodiazepine and Z‐drugs use in the UK: a survey of general practice. Br J Gen Pract 2017; 67: 609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiat 2015; 72: 136–142. [DOI] [PubMed] [Google Scholar]
- 48. Cooper JA, Moriarty F, Ryan C, Smith SM, Bennett K, Fahey T, et al Potentially inappropriate prescribing in two populations with differing socio‐economic profiles: a cross‐sectional database study using the PROMPT criteria. Eur J Clin Pharmacol 2016; 72: 583–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Weymann D, Gladstone EJ, Smolina K, Morgan SG. Long‐term sedative use among community‐dwelling adults: a population‐based analysis. CMAJ Open 2017; 5: E52–E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Smith AJ, Tett SE. Improving the use of benzodiazepines – is it possible? A non‐systematic review of interventions tried in the last 20 years. BMC Health Serv Res 2010; 10: 321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pollmann AS, Murphy AL, Bergman JC, Gardner DM. Deprescribing benzodiazepines and Z‐drugs in community‐dwelling adults: a scoping review. BMC Pharmacol Toxicol 2015; 16: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Irish Medical Council, Pharmaceutical Society of Ireland . Irish Medical Council/Pharmaceutical Society of Ireland Joint Guidance: Safe Prescribing and Dispensing of Controlled Drugs. Ireland, 2017.
- 53. S.I. No. 342/1993 — Misuse of Drugs (Amendment) Regulations, 1993. Ireland, 1993.
- 54. Fisher J, Sanyal C, Frail D, Sketris I. The intended and unintended consequences of benzodiazepine monitoring programmes: a review of the literature. J Clin Pharm Ther 2012; 37: 7–21. [DOI] [PubMed] [Google Scholar]
- 55. O'Sullivan K, Reulbach U, Boland F, Motterlini N, Kelly D, Bennett K, et al Benzodiazepine prescribing in children under 15 years of age receiving free medical care on the General Medical Services scheme in Ireland. BMJ Open 2015; 5: e007070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Quigley P, Usher C, Bennett K, Feely J. Socioeconomic influences on benzodiazepine consumption in an Irish region. Eur Addict Res 2006; 12: 145–150. [DOI] [PubMed] [Google Scholar]
- 57. Islam MM, Conigrave KM, Day CA, Nguyen Y, Haber PS. Twenty‐year trends in benzodiazepine dispensing in the Australian population. Intern Med J 2014; 44: 57–64. [DOI] [PubMed] [Google Scholar]
- 58. Health Research Board . Drug Treatment in Ireland NDTRS 2009 to 2015. Health Research Board, Ireland, 2017. Available at http://www.drugsandalcohol.ie/27023 (last accessed 31 July 2017).
- 59. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg 2017; 152: 1066–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Benzodiazepines and Z‐drugs classified according to ATC code and half‐life value
Table S2 Proportions of GMS eligible individuals during study period categorized according to gender and age
Table S3 Prescribing rates per 1000 GMS population for individual benzodiazepine and Z‐drugs
Figure S1 Prescribing rates for (a) benzodiazepines (BZDs) and (b) Z‐drugs issued to GMS eligible patients aged ≥16 years from 2005 to 2015 according to gender and age
Figure S2 Duration of consecutive (a) benzodiazepine and (b) Z‐drug use among patients during study period according to gender and age


