Abstract
This study aimed to compare the psychopathological profiles of children at familial high risk of schizophrenia spectrum psychosis (FHR‐SZ) or bipolar disorder (FHR‐BP) with population‐based controls. We used Danish nationwide registers to retrieve a cohort of 522 seven‐year‐old children of parents with schizophrenia spectrum psychosis (N=202), bipolar disorder (N=120) or none of these disorders (N=200). Psychopathology was assessed by reports from multiple informants, including children, parents and teachers. Lifetime DSM‐IV diagnoses were ascertained by blinded raters through the Schedule for Affective Disorders and Schizophrenia for School‐Age Children. The dimensional assessment of psychopathology was performed by the Child Behavior Checklist, the Teacher's Report Form, a modified version of the ADHD‐Rating Scale, the Test Observation Form, and the State‐Trait Anxiety Inventory for Children. Current level of functioning was evaluated using the Children's Global Assessment Scale (CGAS). The prevalence of lifetime psychiatric diagnoses was significantly higher in both FHR‐SZ children (38.7%, odds ratio, OR=3.5, 95% confidence interval, CI: 2.2‐5.7, p < 0.001) and FHR‐BP children (35.6%, OR=3.1, 95% CI: 1.8‐5.3, p < 0.001) compared with controls (15.2%). FHR‐SZ children displayed significantly more dimensional psychopathology on all scales and subscales compared with controls except for the Anxious subscale of the Test Observation Form. FHR‐BP children showed higher levels of dimensional psychopathology on several scales and subscales compared with controls, but lower levels compared with FHR‐SZ children. Level of functioning was lower in both FHR‐SZ children (CGAS mean score = 68.2; 95% CI: 66.3‐70.2, p < 0.0001) and FHR‐BP children (73.7; 95% CI: 71.2‐76.3, p < 0.05) compared with controls (77.9; 95% CI: 75.9‐79.9). In conclusion, already at the age of seven, FHR‐SZ and FHR‐BP children show a higher prevalence of a broad spectrum of categorical and dimensional psychopathology compared with controls. These results emphasize the need for developing early intervention strategies towards this vulnerable group of children.
Keywords: Schizophrenia spectrum psychosis, bipolar disorder, children at familial high risk, psychiatric diagnoses, dimensional psychopathology, level of functioning, early intervention strategies
The importance of early detection and intervention for the outcome of schizophrenia has received increasing attention during the last two decades. Efforts have moved from studying treatment in first‐episode psychosis towards evaluating intervention before the onset of psychosis1. Moreover, studies on intervention in individuals with ultra‐high‐risk states have provided promising results2. Evidence also confirms that schizophrenia is a neurodevelopmental disorder with subtle signs long before psychosis onset3, 4. These findings suggest that intervention should begin already in the premorbid phase.
Identifying early antecedents in children and adolescents is necessary in the effort to develop primary intervention strategies for severe mental illness like schizophrenia and bipolar disorder. Additionally, differentiation between shared and distinct antecedents and risk factors in the two disorders is a prerequisite in determining whether preventive interventions should or not be illness specific5.
Since schizophrenia and bipolar disorder are rare events in the general population, familial high risk studies of children born to parents with schizophrenia (FHR‐SZ) or bipolar disorder (FHR‐BP) are useful in studying trajectories towards these conditions. The offspring of parents with severe mental disorders have been reported to have elevated rates of not only the disorder of their parents but also a wide range of other mental disorders6, 7.
Studies on psychopathology in child offspring of parents with schizophrenia and bipolar disorder, as opposed to adult offspring, are vital because they provide knowledge on early developmental psychopathology long before onset of the full‐blown disorders. Indeed, earlier studies have found a high prevalence of a broad spectrum of Axis I disorders and dimensional psychopathology in FHR‐SZ children8, 9, 10, 11, 12, 13, 14, 15 as well as FHR‐BP children12, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30. However, many previous clinical studies have weaknesses, such as small sample sizes, use of convenience samples, inclusion of children from different age groups, or lack of a proper control group. Furthermore, studies of FHR‐SZ children using comprehensive semi‐structured diagnostic interviews and clinical rating scales are rare.
To investigate whether FHR‐SZ and FHR‐BP children are at risk of developing disorders that are specific to their respective risk profiles, or if they simply share a general proneness to psychopathology, it is necessary to study children with different familial risk profiles simultaneously. This has only been done in very few studies12, 31.
In the present study, we aimed to characterize and compare psychopathological profiles in children born to parents with schizophrenia or bipolar disorder and population‐based controls.
METHODS
Data presented are part of the Danish High Risk and Resilience Study ‐ VIA 7, a nationwide population‐based cohort study of 522 seven‐year‐old FHR‐SZ children, FHR‐BP children and controls32.
Participants
A cohort of 522 seven‐year‐old (age range 6.9‐8.4 years) children, born and living in Denmark, with no, one or two biological parents diagnosed with schizophrenia spectrum psychosis (defined as ICD‐10 codes F20, F22 and F25, or ICD‐8 codes 295, 297, 298.29, 298.39, 298.89 and 298.99) or bipolar disorder (defined as ICD‐10 codes F30 and F31, or ICD‐8 codes 296.19 and 296.39) was identified using the Danish Civil Registration System33 and the Danish Psychiatric Central Research Register34, including both inpatient and outpatient contacts.
Families in which at least one parent had been diagnosed with schizophrenia spectrum psychosis (the index parent) were matched to control families on gender, age and municipality of the child. Parents from the control group could be registered with any other psychiatric diagnoses except for schizophrenia spectrum psychosis or bipolar disorder.
Families where a parent had been diagnosed with bipolar disorder were a non‐matched sample, but they were comparable to the other two groups in terms of age and gender of the children.
Procedures
The study was approved by the Danish Data Protection Agency. The Danish Ministry of Health granted permission to retrieve data from the Danish registers. The study protocol was sent to the Danish Committee on Health Research Ethics, which decided that ethical approval was not needed due to the observational nature of the study. Written informed consent was obtained from all adult participants and from the legal guardians of participating children.
A group of psychologists, medical doctors and nurses carried out the assessments after being trained in the use of all instruments. The investigators who examined the children were blinded to the illness status of the parents. The caregiver who at the present time point knew the child best was asked to provide information on the child's psychopathology.
Children's psychiatric diagnoses and level of functioning
Children's psychiatric diagnoses were ascertained through the Schedule for Affective Disorders and Schizophrenia for School‐Age Children ‐ Present and Lifetime Version (K‐SADS‐PL)35. The interview was firstly carried out with the caregiver, then with the child. Best‐estimate lifetime DSM‐IV‐diagnoses were made based on K‐SADS‐PL and all other available data on the child (e.g., results of cognitive tests and psychopathology scales). Consensus diagnoses were made at conferences with a child and adolescent psychiatrist (AT). In the vast majority of cases, the K‐SADS‐PL interviews were video‐recorded, enabling the researchers to watch parts of them if there was uncertainty regarding scores.
In K‐SADS‐PL, probable diagnoses are made if criteria for the core symptoms are met, all but one (or a minimum of 75%) of the remaining criteria are met, and the symptoms are causing functional impairment35. Both definite and probable diagnoses were included in the analysis. We excluded elimination disorders, because of their questionable clinical significance.
Current level of functioning of the child was evaluated using the Children's Global Assessment Scale (CGAS)36, as a part of the K‐SADS‐PL interview.
Dimensional assessment of the children's psychopathology
The Child Behavior Checklist school‐age version (CBCL) was completed by the primary caregiver37. The scale includes 118 problem behavior items rated on a Likert scale from zero (not true) to two (very true or often true). We used the two broad‐band subscales (Internalizing and Externalizing) and the six DSM‐IV oriented subscales (Affective Problems, Anxiety Problems, Somatic Problems, Attention Deficit/Hyperactivity Problems, Oppositional Defiant Problems and Conduct Problems).
The Teacher's Report Form (TRF) was completed by the child's teacher37. In most aspects this instrument corresponds to the CBCL and most of its items have counterparts in the CBCL.
We used a modified version of the ADHD‐Rating Scale (mADHD‐RS)38, 39, 40 to assess symptoms of attention‐deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD), rated by primary caregivers and teachers. The original ADHD‐Rating Scale consists of two nine‐item subscales related to the core symptomatology of ADHD: Inattention and Hyperactivity/Impulsivity. The mADHD‐RS includes an additional eight‐item subscale for problems related to oppositional defiant disorder38, 40. The items are rated on a four‐point Likert scale from zero (never or rarely) to three (very often).
The Test Observation Form (TOF) was used to assess behavioral and emotional problems observed during a test session41. It consists of 125 items, scored on a four‐point Likert scale. It was completed by the child examiner after testing. The TOF is subdivided into the two broad‐band Internalizing and Externalizing subscales and into five empirically based subscales. We excluded the open‐ended item 125, where problems not covered by the other items can be rated.
The State‐Trait Anxiety Inventory for Children (STAI‐CH) was used to measure the children's self‐reported level of anxiety42. This instrument consists of two 20‐item scales including both direct and reversed statements. The State‐Anxiety scale was used to measure current level of anxiety at the examination, and the Trait‐Anxiety scale to measure the general level of anxiety. Since the STAI‐CH is constructed to be used with nine‐ to twelve‐year‐old children, it was administered verbally, and the meaning of the questions was explained if needed. The scores of each subscale range from 20 (indicating a low level of anxiety) to 60 (indicating a high level of anxiety). To make the differences in percentages comparable to the other scales, 20 points were subtracted to each score before analysis, so that the potential scores ranged from 0 to 40.
Interrater reliability
All raters attended formal courses on the use of K‐SADS‐PL prior to data collection. Reliability ratings were held regularly during data collection. Interrater reliability was estimated based on ten video‐recorded K‐SADS‐PL interviews using Krippendorff's alpha with 95% bootstrap confidence intervals (CIs)43. The combined observed agreement of K‐SADS‐PL skip‐out criteria across sections in the screening interview was 90.3%. Krippendorff's alpha was 0.74 (95% CI: 0.63‐0.82). Because of an insufficient number of cases, it was not possible to estimate Krippendorff's alpha of skip‐out criteria separately for each section of the screening interview. Observed agreement ranged from 80 to 100%, except for the post‐traumatic stress disorder section, where observed agreement was 20%.
Krippendorff's alpha of CGAS was 0.87 (95% Cl: 0.70‐0.92).
Statistical analyses
Differences in demographic and clinical characteristics between the three groups were analyzed by one‐way analysis of variance or chi‐square test, as appropriate.
Between‐group differences in diagnoses were evaluated using logistic regression adjusting for the children's gender. Differences in dimensional psychopathology between the groups were analyzed using generalized linear model (GLM) with Tweedie distribution and log link function, due to non‐normally distributed data. Differences in CGAS scores were analyzed using GLM with normal distribution and log link function. Analyses were adjusted for children's gender.
RESULTS
Background characteristics
A final cohort of 522 children from 506 families was retrieved from Danish national registers (Figure 1). Of these, 200 FHR‐SZ children, 119 FHR‐BP children and 200 controls participated with some data on psychopathology.
Figure 1.
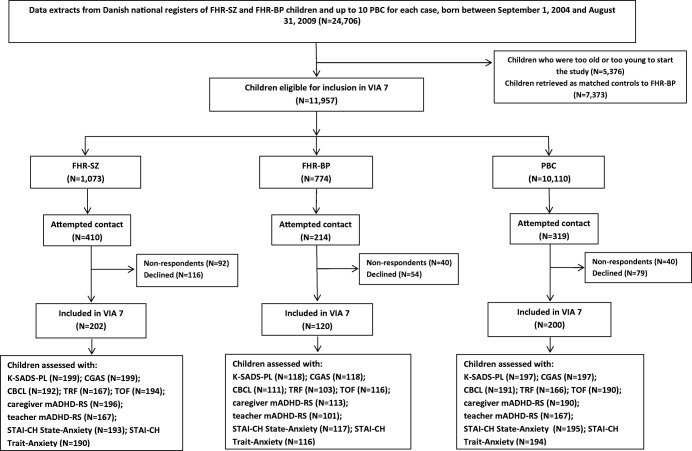
Flow chart of the recruitment of children in the Danish High Risk and Resilience Study ‐ VIA 7. FHR‐SZ – children of parents with schizophrenia spectrum psychosis, FHR‐BP – children of parents with bipolar disorder, PBC – population‐based control children of parents with no diagnoses of schizophrenia spectrum psychosis or bipolar disorder, K‐SADS‐PL – Schedule for Affective Disorder and Schizophrenia for School‐Age Children ‐ Present and Lifetime Version, CGAS – Children's Global Assessment Scale, CBCL – Child Behavior Checklist school‐age version, TRF – Teacher's Report Form, TOF – Test Observation Form, mADHD‐RS – ADHD‐Rating Scale, modified version, STAI‐CH – State‐Trait Anxiety Inventory for Children
We found several significant differences in family characteristics and home environment between the three groups (Table 1).
Table 1.
Characteristics of children participating with data on psychopathology in the Danish High Risk and Resilience Study ‐ VIA 7 and their biological parents
| FHR‐SZ | FHR‐BP | PBC | p | Pairwise comparisons | |||
|---|---|---|---|---|---|---|---|
| FHR‐SZ vs. PBC | FHR‐BP vs. PBC | FHR‐BP vs. FHR‐SZ | |||||
| Children (N=519) | (N=200) | (N=119) | (N=200) | ‐ | ‐ | ‐ | ‐ |
| Female, N (%) | 92 (46.0) | 55 (46.2) | 93 (46.5) | 0.995 | ‐ | ‐ | ‐ |
| Age at inclusion, years, mean±SD | 7.8 ± 0.2 | 7.9 ± 0.2 | 7.8 ± 0.2 | 0.096 | ‐ | ‐ | ‐ |
| Two ill parents, N (%) | 8 (4.0) | 1 (0.8) | ‐ | ‐ | ‐ | ‐ | ‐ |
| Child's home environment | |||||||
| Living with both biological parents, N (%) | 80 (40.0) | 62 (52.1) | 169 (84.5) | <0.0001 | <0.0001 | <0.0001 | 0.035 |
| Living out of home, N (%) | 11 (5.5) | 0 (0.0) | 1 (0.5) | <0.001 | 0.003 | 0.440 | 0.009 |
| Living with index parent, N (%) | 122 (61.0) | 83 (69.7) | 189 (94.5) | <0.0001 | <0.0001 | <0.0001 | 0.115 |
| Living with a single parent, N (%) | 75 (37.5) | 39 (32.8) | 21 (10.6) | <0.0001 | <0.0001 | <0.0001 | 0.394 |
| PSP primary caregiver, mean±SD | 73.1 ± 14.0 | 74.5 ± 14.1 | 84.4 ± 9.1 | <0.0001 | <0.0001 | <0.0001 | 0.346 |
| Index parents (N=517) | (N=198) | (N=115) | (N=204) | ‐ | ‐ | ‐ | ‐ |
| Female, N (%) | 110 (55.6) | 63 (54.8) | 115 (56.4) | 0.962 | ‐ | ‐ | ‐ |
| Age at child's birth, years, mean±SD | 30.1 ± 6.0 | 33.1 ± 7.0 | 32.8 ± 4.8 | <0.0001 | <0.0001 | 0.673 | <0.0001 |
| PSP, mean±SD | 66.3 ± 15.6 | 68.9 ± 14.1 | 84.3 ± 9.9 | <0.0001 | <0.0001 | <0.0001 | 0.115 |
| Employed or studying, N (%) | 92 (49.5) | 60 (55.6) | 185 (92.0) | <0.0001 | <0.0001 | <0.0001 | 0.313 |
| Education | |||||||
| Primary/lower secondary, N (%) | 54 (30.5) | 10 (9.3) | 8 (4.1) | ||||
| Upper secondary, vocational, short‐cycle tertiary, N (%) | 75 (42.4) | 44 (40.7) | 95 (48.2) | <0.0001 | <0.0001 | 0.930 | <0.0001 |
| Bachelor degree, equivalent or higher, N (%) | 48 (27.1) | 54 (50.0) | 94 (47.7) | ||||
| Biological non‐index parents (N=489) | (N=184) | (N=113) | (N=192) | ||||
| Female, N (%) | 81 (44.0) | 51 (45.1) | 83 (43.2) | 0.949 | ‐ | ‐ | ‐ |
| Age at child's birth, years, mean±SD | 30.9 ± 6.4 | 33.1 ± 5.4 | 33.0 ± 4.3 | <0.001 | <0.001 | 0.856 | <0.001 |
| PSP, mean±SD | 76.4 ± 14.3 | 81.8 ± 13.1 | 85.5 ± 8.4 | <0.0001 | <0.0001 | 0.013 | <0.001 |
| Employed or studying, N (%) | 133 (75.6) | 93 (86.1) | 179 (95.2) | <0.0001 | <0.0001 | 0.006 | 0.032 |
| Education | |||||||
| Primary/lower secondary, N (%) | 30 (17.1) | 5 (4.8) | 10 (5.3) | ||||
| Upper secondary, vocational, short‐cycle tertiary, N (%) | 86 (49.1) | 44 (41.9) | 89 (47.6) | 0.002 | 0.002 | 0.310 | <0.001 |
| Bachelor degree, equivalent or higher, N (%) | 59 (33.7) | 56 (53.3) | 88 (47.1) | ||||
Index parents refer to the biological parents with a diagnosis of schizophrenia spectrum psychosis or bipolar disorder. FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder, PBC – population‐based controls, PSP – Personal and Social Performance Scale
Children's psychiatric diagnoses
A total of 514 children were assessed with K‐SADS‐PL (Table 2). The prevalence of any lifetime DSM‐IV Axis I psychiatric diagnoses (excluding elimination disorders) was significantly higher in both FHR‐SZ children (38.7%, odds ratio, OR=3.5, 95% CI: 2.2‐5.7, p < 0.001) and FHR‐BP children (35.6%, OR=3.1, 95% CI: 1.8‐5.3, p < 0.001) compared with controls (15.2%).
Table 2.
Lifetime prevalence of DSM‐IV Axis I disorders in offspring of parents with schizophrenia or bipolar disorder compared with population‐based controls
| FHR‐SZ (N=199) | FHR‐BP (N=118) | PBC (N=197) | ||||
|---|---|---|---|---|---|---|
| N (%) | OR (95% CI) | N (%) | OR (95% CI) | N (%) | ||
| Any Axis I disorder | 108 (54.3%) | 2.0 (1.4‐3.1)*** | 64 (54.2%) | 2.0 (1.3‐3.3)** | 73 (37.1%) | |
| Any Axis I disorder, excluding elimination disorders | 77 (38.7%) | 3.5 (2.2‐5.7)*** | 42 (35.6%) | 3.1 (1.8‐5.3)*** | 30 (15.2%) | |
| Two or more Axis I disorder, excluding elimination disorders | 28 (14.1%) | 4.4 (1.9‐10.4)*** | 17 (14.4%) | 4.6 (1.8‐11.4)** | 7 (3.6%) | |
| Affective disorders | 3 (1.5%) | ‐ | 5 (4.2%) | ‐ | 2 (1.0%) | |
| Psychotic disorder NOS | 2 (1.0%) | ‐ | 0 | ‐ | 0 | |
| Anxiety disorders | 23 (11.6%) | 2.8 (1.2‐6.1) * | 14 (11.9%) | 2.8 (1.2‐6.8) * | 9 (4.6%) | |
| Disruptive behavior disorders | 12 (6.0%) | 6.4 (1.4‐29.2) * | 4 (3.4%) | 3.5 (0.6‐19.5) | 2 (1.0%) | |
| ADHD | 41 (20.6%) | 3.5 (1.8‐6.6) *** | 11 (9.3%) | 1.4 (0.6‐3.1) | 14 (7.1%) | |
| Pervasive developmental disorders | 12 (6.0%) | 2.5 (0.9‐7.2) | 9 (7.6%) | 3.2 (1.0‐9.9) * | 5 (2.5%) | |
| Post‐traumatic stress disorder | 4 (2.0%) | ‐ | 3 (2.5%) | ‐ | 0 | |
| Stress and adjustment disorders | 11 (5.5%) | 3.8 (1.0‐13.8) * | 10 (8.5%) | 6.0 (1.6‐22.2)** | 3 (1.5%) | |
| Tic disorders | 7 (3.5%) | ‐ | 2 (1.7%) | ‐ | 3 (1.5%) | |
| Elimination disorders | 53 (26.6%) | 1.0 (0.6‐1.5) | 38 (32.2%) | 1.3 (0.8‐2.1) | 54 (27.4%) | |
FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder, PBC – population‐based controls, OR – odds ratio, CI – confidence interval, NOS – not otherwise specified, ADHD – attention‐deficit/hyperactivity disorder
*p < 0.05, **p < 0.01,***p < 0.001
Both familial risk groups had a higher prevalence of several psychiatric diagnoses compared with controls. However, due to the small number of children with some diagnoses, it was not possible to estimate ORs for all categories. FHR‐SZ children had significantly higher ORs of anxiety disorders (OR=2.8, 95% CI: 1.2‐6.1, p < 0.05), disruptive behavior disorders (OR=6.4, 95% CI: 1.4‐29.2, p < 0.05), ADHD (OR=3.5, 95% CI: 1.8‐6.6, p < 0.001), and stress and adjustment disorders (OR=3.8, 95% CI: 1.0‐13.8, p < 0.05), compared with controls. FHR‐BP children had significantly higher ORs of anxiety disorders (OR=2.8, 95% CI: 1.2‐6.8, p < 0.05), pervasive developmental disorders (OR=3.2, 95% CI: 1.0‐9.9, p < 0.05), and stress and adjustment disorders (OR=6.0, 95% CI: 1.6‐22.2, p < 0.01), compared with controls.
Among cases with ADHD, FHR‐BP children most often presented the predominantly inattentive type of the disorder (N=8, 72.7%), while FHR‐SZ children and controls most often presented the combined or predominantly hyperactive‐impulsive type (N=24, 58.5%, and N=8, 57.1%, respectively). The small number of children with ADHD did not allow calculations of the significance of these findings.
Children's level of functioning and dimensional psychopathology
FHR‐SZ children had a significantly lower level of functioning (CGAS mean score=68.2, 95% CI: 66.3‐70.2) compared with controls (77.9, 95% CI: 75.9‐79.9, p < 0.0001) and with FHR‐BP children (73.7, 95% CI: 71.2‐76.3, p=0.0009) (Table 3). FHR‐BP children had significantly lower levels of functioning compared with controls (p=0.0126).
Table 3.
Estimated means and percentage differences adjusted for child's gender between familial high risk groups on CBCL, TRF, TOF, STAI‐CH and CGAS total and broad‐band scores
| FHR‐SZ | FHR‐BP | PBC | Estimated differences in percentage (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Test (informant) | N | Mean (95% CI) | N | Mean (95% CI) | N | Mean (95% CI) | FHR‐SZ vs. PBC | FHR‐BP vs. PBC | FHR‐SZ vs. FHR‐BP |
| CBCL (caregiver) | |||||||||
| Total | 192 | 27.2 (24.4‐30.3) | 111 | 23.4 (20.2‐27.0) | 191 | 17.0 (15.1‐19.1) | 59.9% (36.4‐87.5)**** | 37.6% (14.2‐65.8)*** | 16.2% (– 3.0 to 39.2) |
| Internalizing | 194 | 6.6 (5.9‐7.4) | 110 | 6.6 (5.7‐7.7) | 191 | 4.9 (4.3‐5.5) | 35.4% (13.8‐61.2)*** | 36.0% (11.2‐66.3)** | −0.4% (– 17.9 to 20.9) |
| Externalizing | 193 | 7.8 (6.8‐8.8) | 111 | 6.1 (5.1‐7.3) | 191 | 4.1 (3.5‐4.8) | 90.4% (56.1‐132.3)**** | 50.9% (19.3‐90.9)*** | 26.2% (1.5‐56.9) * |
| TRF (teacher) | |||||||||
| Total | 167 | 26.2 (22.7‐30.2) | 103 | 20.0 (16.5‐24.2) | 166 | 14.7 (12.5‐17.2) | 78.3% (43.9‐120.9)**** | 36.2% (6.2‐74.7) * | 30.9% (3.2‐66.1) * |
| Internalizing | 168 | 5.7 (4.9‐6.6) | 103 | 5.5 (4.6‐6.7) | 167 | 3.7 (3.1‐4.3) | 56.0% (25.1‐94.7)**** | 50.6% (17.1‐93.6)** | 3.6% (– 18.3 to 31.5) |
| Externalizing | 168 | 6.5 (5.3‐7.9) | 103 | 4.5 (3.4‐5.9) | 167 | 3.0 (2.4‐3.8) | 113.3% (56.2‐191.4)**** | 47.3% (1.9‐112.8) * | 44.9% (2.7‐104.3) * |
| TOF (tester) | |||||||||
| Total | 194 | 34.9 (30.7‐39.7) | 116 | 24.9 (20.9‐29.8) | 190 | 25.0 (21.8‐28.7) | 39.4% (15.6‐68.1)*** | −0.4% (–20.3 to 24.5) | 39.9% (12.6‐73.8)** |
| Internalizing | 194 | 7.6 (6.5‐8.9) | 116 | 5.7 (4.6‐7.1) | 190 | 4.9 (4.1‐5.9) | 53.7% (21.8‐93.9)*** | 15.3% (–12.7 to 52.1) | 33.4% (2.5‐73.6) * |
| Externalizing | 194 | 13.2 (11.2‐15.6) | 116 | 8.0 (6.3‐10.1) | 190 | 9.0 (7.5‐10.9) | 46.4% (14.5‐87.0)** | −12.0% (–34.9 to 19.0) | 66.2% (24.3‐122.4)*** |
| STAI‐CH (child) | |||||||||
| State‐Anxiety | 193 | 8.1 (7.5‐8.8) | 117 | 7.2 (6.5‐7.9) | 195 | 6.9 (6.4‐7.5) | 17.2% (5.2‐30.6)** | 3.2% (– 9.2 to 17.3) | 13.6% (0.2‐28.7) * |
| Trait‐Anxiety | 190 | 12.6 (11.5‐13.7) | 116 | 12.2 (10.9‐13.6) | 194 | 10.4 (9.5‐11.4) | 20.9% (6.9‐36.6)** | 17.4% (2.0‐35.1) * | 3.0% (– 10.3 to 18.2) |
| CGAS | 199 | 68.2 (66.3‐70.2) | 118 | 73.7 (71.2‐76.3) | 197 | 77.9 (75.9‐79.9) | −12.4% (–15.7 to −8.9)**** | −5.4% (–9.4 to – 1.2) * | −7.4% (–11.5 to – 3.1)*** |
FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder, PBC – population‐based controls, CI – confidence interval, CBCL – Child Behavior Checklist school‐age version, TRF – Teacher's Report Form, TOF – Test Observation Form, STAI‐CH – State‐Trait Anxiety Inventory for Children, CGAS – Children's Global Assessment Scale
*p < 0.05, **p < 0.01,***p < 0.001,****p < 0.0001
FHR‐SZ children scored significantly higher than controls on all psychopathology scales and subscales except for the TOF Anxious subscale (Table 3; Figures 2 and 3). FHR‐BP children scored significantly higher compared with controls on several psychopathology scales and subscales. However, there were no significant differences in mean scores between FHR‐BP children and controls on any of the TOF subscales (Table 3; Figures 2 and 3).
Figure 2.
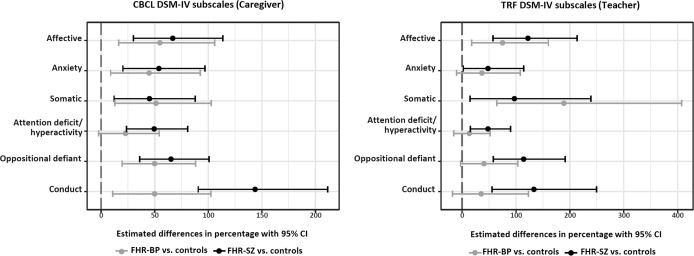
Percentage differences in mean scores of subscales of the Child Behavior Checklist (CBCL) and the Teacher's Report Form (TRF). The population‐based control group is set as reference (the vertical dashed line). FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder
Figure 3.
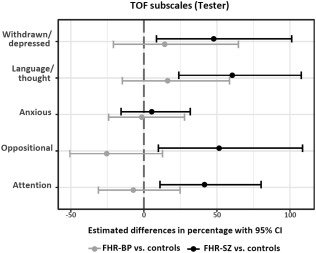
Percentage differences in mean scores of subscales of the Test Observation Form (TOF). The population‐based control group is set as reference (the vertical dashed line). FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder
FHR‐SZ children had significantly higher mean scores on all the subscales of both the caregiver and teacher version of mADHD‐RS compared with controls, reflecting higher levels of ADHD and oppositional defiant symptoms (Figure 4). FHR‐BP children had significantly higher mean scores compared with controls on all subscales of the caregiver version of mADHD‐RS except for the Hyperactivity/Impulsivity subscale. FHR‐BP children and controls did not differ on the subscales of the teacher version of mADHD‐RS, although the difference on the Inattention subscale and the subscale of oppositional defiant disorder problems showed a trend towards significance (Figure 4).
Figure 4.
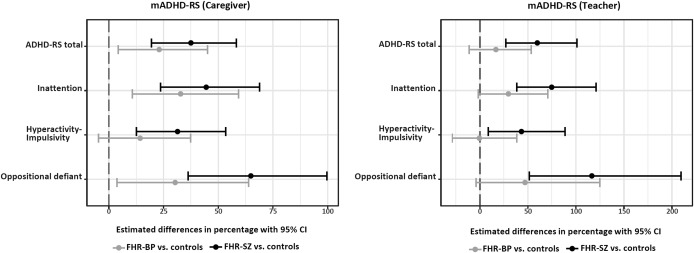
Percentage differences in mean scores of subscales of the modified version of the ADHD‐Rating Scale (mADHD‐RS). The population‐based control group is set as reference (the vertical dashed line). ADHD‐RS total – sum score of the Inattention and the Hyperactivity‐Impulsivity subscales, FHR‐SZ – children with familial high risk for schizophrenia spectrum psychosis, FHR‐BP – children with familial high risk for bipolar disorder
DISCUSSION
Main findings
The Danish High Risk and Resilience Study ‐ VIA 7 is a nationwide cohort study of 522 seven‐year‐old children. It is the only population‐based, representative familial high risk study, and it is the largest clinical study to date assessing psychopathology in children of parents with schizophrenia and bipolar disorder compared with controls.
We found that FHR‐SZ and FHR‐BP children have an equally higher prevalence of a broad spectrum of lifetime DSM‐IV psychiatric diagnoses – e.g., anxiety disorders, and stress and adjustment disorders – compared with controls. Further, we found a gradient in levels of unspecific dimensional psychopathology and daily functioning between the groups, with FHR‐SZ children being the most affected and controls being the least affected, whereas FHR‐BP children displayed intermediate levels of psychopathology and functioning.
Specificity of psychopathology in familial high risk children
Our findings of an elevated prevalence of psychiatric diagnoses and dimensional psychopathology in FHR‐SZ and FHR‐BP children are consistent with the results of earlier familial high risk studies7, 8, 9, 10, 12, 16, 17, 19, 29, 30. Overall, both familial high risk groups in our study presented with a broad range, i.e. unspecific, categorical and dimensional psychopathology at this young age. Depressive disorders were rare in both groups, mania was absent, and only two FHR‐SZ children were diagnosed with psychotic disorder not otherwise specified.
We found elevated rates of anxiety disorders as well as stress and adjustment disorders in both familial high risk groups. This is in accordance with earlier reports of anxiety disorders being common in FHR‐BP children44. The findings support the first step of the clinical staging model suggested by Duffy et al29, implying that anxiety and sleep disorders in childhood, as well as adjustment, mood and substance use disorders in adolescence, could represent early precursors of bipolar disorder in the offspring of parents with that disorder.
Rates of psychopathology in FHR‐BP children have varied substantially in previous studies. This may be attributed to differences in parents' severity of illness, procedures for assessing offspring diagnoses, and age of the offspring23, 45. Parents with bipolar disorder have often been recruited through inpatient and outpatient clinics, whereas they were identified through Danish registers in this study. Therefore, the group of parents in our study was likely to be more heterogeneous in terms of severity of the disorders, which may explain the lower levels of psychopathology in FHR‐BP children compared with other familial high risk studies of bipolar disorder. Indeed, our findings are in line with the Dutch Bipolar Offspring Study, where most parents were recruited through a patient advocacy group23.
Differences in psychopathological presentation between the two high risk groups
Even though evidence of the shared genetic risk factors for schizophrenia and bipolar disorder is robust, knowledge concerning common or distinct developmental psychopathology is still lacking5. Our findings showed that FHR‐SZ and FHR‐BP children both present an elevated prevalence of unspecific categorical and dimensional psychopathology, even though FHR‐BP children differed less from controls than did FHR‐SZ children.
Also, FHR‐SZ children consistently displayed elevated levels of behavioral problems across settings, namely at home, at school and during the test session, as rated by several informants. In contrast, even though parents of FHR‐BP children reported a high prevalence of behavioral and emotional problems compared with controls, teachers reported less deviation from controls and the investigators observed levels of problems equal to those of controls.
Both high risk groups had an elevated prevalence of anxiety as well as stress and adjustment disorders. FHR‐BP children displayed a significantly elevated prevalence of pervasive developmental disorders compared with controls, whereas the elevated prevalence in FHR‐SZ children did not reach significance. Only FHR‐SZ children had an elevated prevalence of ADHD and disruptive behavior disorders compared with controls. Thus, even though both high risk groups show elevated levels of unspecific psychopathology, there are also differences between their psychopathological profiles.
ADHD and disruptive behavior disorders in familial high risk children
We found significantly higher levels of ADHD and disruptive behavior disorders in FHR‐SZ children compared with controls, which is in line with findings of impaired attention and disruptive behaviors in previous studies8, 9, 10, 12, 46. However, earlier studies have reported conflicting results on ADHD and disruptive behavior disorders in FHR‐BP children19, 47. In particular, Duffy et al29 suggested that ADHD only precedes bipolar disorder in offspring of bipolar parents who do not respond to lithium treatment.
We did not find a higher prevalence of diagnoses of ADHD and disruptive behavior disorders in FHR‐BP children at this early age compared with controls. Further, among children with a diagnosis of ADHD, those from the FHR‐BP group most often had the predominantly inattentive type, whereas children from the FHR‐SZ and control groups most often had the combined or predominantly hyperactive‐impulsive type. Likewise, in the dimensional measures, we only found some evidence of elevated symptoms of ADHD and disruptive behavior disorders in FHR‐BP children, in the form of elevated scores on the Inattention subscale and the subscale of oppositional defiant disorder problems of the caregiver version of mADHD‐RS. Detection of inattention in a classroom setting may be more challenging than the observation of hyperactivity and impulsivity, which may explain why the difference between the FHR‐BP group and controls only showed a trend towards significance in teachers' ratings of inattention.
Strengths and limitations
An important strength of this study is the use of Danish national registers to recruit the families, which contributes to the high representativeness of this large nationwide cohort.
The narrow age range of the children is also a major strength of the study, since the prevalence and nature of psychopathological disorders and symptoms are highly age‐dependent. The prevalence of psychopathology could be compared between the study groups with higher precision and power.
Psychopathology was evaluated both categorically and dimensionally with state‐of‐the‐art assessment instruments through multiple informants in different settings. This provided a comprehensive understanding of the children's psychopathology in different contexts.
Another major strength of the study is the inclusion of FHR‐SZ and FHR‐BP children in the same study, which allowed to explore possible shared and different antecedents between these groups.
This study also has some limitations. The FHR‐BP group consisted of only 120 children. Some of the non‐significant differences between FHR‐BP and controls may thus be due to an insufficient statistical power. However, the FHR‐BP group scored lower than the FHR‐SZ group on most psychopathology scales, which is more likely the reason why the latter group differed significantly from controls on more scales than did the former one.
Some studies have suggested that parental mood influences the parental reports on children's psychopathology, although results have been conflicting48. This could potentially explain why parents from the FHR‐BP group reported more dimensional psychopathology than teachers and investigators.
As these results are from the first wave of assessments, we cannot determine whether the high rates of psychopathology found in these children are a transient phenomenon or rather a part of different trajectories towards more severe illnesses. We need to monitor the prevalence of psychopathological symptoms in the familial high risk groups over time, and explore if they may predict schizophrenia or bipolar disorder later in life. Also, follow‐up studies are needed to identify resilience factors that can protect children with psychopathology from developing severe mental illness.
Implications
Children from the familial high risk groups displayed significantly more dimensional psychopathology and psychiatric disorders compared with controls. The finding of high levels of psychopathology at this early age in FHR‐SZ and FHR‐BP children could have implications for school performance, peer relations and other important developmental aspects. A preventive strategy could be to offer these children and their families special and enhanced attention and support from teachers and health care professionals. Also, our findings highlight the need to strengthen the collaboration between adult and child psychiatry in the treatment of these families.
Furthermore, longitudinal familial high risk studies are needed to identify which psychopathological symptoms predict conversion to severe mental disorders in FHR‐SZ and FHR‐BP children and which resilience factors help these children compensate and protect them from conversion. The next wave of assessment of this cohort at age 11 began in March 2017 and is called the Danish High Risk and Resilience Study ‐ VIA 11.
Finally, our findings emphasize the need for clinical trials of primary interventions towards this vulnerable group of children to prevent their unspecific psychopathological symptoms from converting into severe mental disorders and to increase their daily level of functioning.
At this stage, we cannot determine whether the signs and symptoms of psychopathology found in these children at familial high risk represent transitory states that they will eventually grow out of or antecedents of more severe disorders. However, we can assert that some of these children have symptoms which impair their current level of functioning and call for interventions to support their healthy development.
ACKNOWLEDGEMENTS
This work was supported by the Mental Health Services of the Capital Region of Denmark, the Lundbeck Foundation Initiative for Integrative Psychiatric Research (iPSYCH), Aarhus University, the Tryg Foundation and the Beatrice Surovell Haskell Fund for Child Mental Health Research of Copenhagen. The authors would like to express their gratitude to the dedicated families participating in the study; to M. Skjærbæk, A. Ranning, H. Jensen, M. Melau, C. Gregersen, H. Stadsgaard, K. Kold Zahle and M. Toft Henriksen for contributing to data collection; to C. Bøcker Pedersen and M. Giørtz Pedersen for retrieving the register extract; to M. Chaine and J. Ohland for help with data management; and to P.B. Mortensen, T. Werge, D. Hougaard and A. Børglum for collaboration in iPSYCH.
REFERENCES
- 1. Fusar‐Poli P, McGorry PD, Kane JM. Improving outcomes of first‐episode psychosis: an overview. World Psychiatry 2017;16:251‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yung AR. Treatment of people at ultra‐high risk for psychosis. World Psychiatry 2017;16:207‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rapoport JL, Giedd JN, Gogtay N. Neurodevelopmental model of schizophrenia: update 2012. Mol Psychiatry 2012;17:1228‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Owen MJ, O'Donovan MC. Schizophrenia and the neurodevelopmental continuum: evidence from genomics. World Psychiatry 2017;16:227‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Laurens KR, Luo L, Matheson SL et al. Common or distinct pathways to psychosis? A systematic review of evidence from prospective studies for developmental risk factors and antecedents of the schizophrenia spectrum disorders and affective psychoses. BMC Psychiatry 2015;15:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dean K, Stevens H, Mortensen PB et al. Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Arch Gen Psychiatry 2010;67:822‐9. [DOI] [PubMed] [Google Scholar]
- 7. Rasic D, Hajek T, Alda M et al. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta‐analysis of family high‐risk studies. Schizophr Bull 2014;40:28‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. de la Serna E, Baeza I, Andrés S et al. Comparison between young siblings and offspring of subjects with schizophrenia: clinical and neuropsychological characteristics. Schizophr Res 2011;131:35‐42. [DOI] [PubMed] [Google Scholar]
- 9. Keshavan M, Montrose DM, Rajarethinam R et al. Psychopathology among offspring of parents with schizophrenia: relationship to premorbid impairments. Schizophr Res 2008;103:114‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ross RG, Compagnon N. Diagnosis and treatment of psychiatric disorders in children with a schizophrenic parent. Schizophr Res 2001;50:121‐9. [DOI] [PubMed] [Google Scholar]
- 11. Hans SL, Auerbach JG, Styr B et al. Offspring of parents with schizophrenia: mental disorders during childhood and adolescence. Schizophr Bull 2004;30:303‐15. [DOI] [PubMed] [Google Scholar]
- 12. Sanchez‐Gistau V, Romero S, Moreno D et al. Psychiatric disorders in child and adolescent offspring of patients with schizophrenia and bipolar disorder: a controlled study. Schizophr Res 2015;168:197‐203. [DOI] [PubMed] [Google Scholar]
- 13. Donatelli JA, Seidman LJ, Goldstein JM et al. Children of parents with affective and nonaffective psychoses: a longitudinal study of behavior problems. Am J Psychiatry 2010;167:1331‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dworkin RH, Green SR, Small NE et al. Positive and negative symptoms and social competence in adolescents at risk for schizophrenia and affective disorder. Am J Psychiatry 1990;147:1234‐6. [DOI] [PubMed] [Google Scholar]
- 15. Niemi LT, Suvisaari JM, Tuulio‐Henriksson A et al. Childhood developmental abnormalities in schizophrenia: evidence from high‐risk studies. Schizophr Res 2003;60:239‐58. [DOI] [PubMed] [Google Scholar]
- 16. Birmaher B, Axelson D, Monk K et al. Lifetime psychiatric disorders in school‐aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Arch Gen Psychiatry 2009;66:287‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chang K, Steiner H, Ketter T. Studies of offspring of parents with bipolar disorder. Am J Med Genet 2003;123C:26‐35. [DOI] [PubMed] [Google Scholar]
- 18. Henin A, Biederman J, Mick E et al. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry 2005;58:554‐61. [DOI] [PubMed] [Google Scholar]
- 19. Vandeleur C, Rothen S, Gholam‐Rezaee M et al. Mental disorders in offspring of parents with bipolar and major depressive disorders. Bipolar Disord 2012;14:641‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Frías Á, Palma C, Farriols N et al. Characterizing offspring of bipolar parents: a review of the literature. Actas Esp Psiquiatr 2015;43:221‐34. [PubMed] [Google Scholar]
- 21. Singh MK, DelBello MP, Stanford KE et al. Psychopathology in children of bipolar parents. J Affect Disord 2007;102:131‐6. [DOI] [PubMed] [Google Scholar]
- 22. Morón‐Nozaleda MG, Díaz‐Caneja CM, Rodríguez‐Toscano E et al. A developmental approach to dimensional expression of psychopathology in child and adolescent offspring of parents with bipolar disorder. Eur Child Adolesc Psychiatry 2017;26:1165‐75. [DOI] [PubMed] [Google Scholar]
- 23. Mesman E, Birmaher BB, Goldstein BI et al. Categorical and dimensional psychopathology in Dutch and US offspring of parents with bipolar disorder: a preliminary cross‐national comparison. J Affect Disord 2016;205:95‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Diler RS, Birmaher B, Axelson D et al. Dimensional psychopathology in offspring of parents with bipolar disorder. Bipolar Disord 2011;13:670‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Giles LL, DelBello MP, Stanford KE et al. Child behavior checklist profiles of children and adolescents with and at high risk for developing bipolar disorder. Child Psychiatry Hum Dev 2007;38:47‐55. [DOI] [PubMed] [Google Scholar]
- 26. Dienes KA, Chang KD, Blasey CM et al. Characterization of children of bipolar parents by parent report CBCL. J Psychiatr Res 2002;36:337‐45. [DOI] [PubMed] [Google Scholar]
- 27. Egeland JA, Shaw JA, Endicott J et al. Prospective study of prodromal features for bipolarity in well Amish children. J Am Acad Child Adolesc Psychiatry 2003;42:786‐96. [DOI] [PubMed] [Google Scholar]
- 28. Maoz H, Goldstein T, Axelson DA et al. Dimensional psychopathology in preschool offspring of parents with bipolar disorder. J Child Psychol Psychiatry 2014;55:144‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Duffy A, Horrocks J, Doucette S et al. The developmental trajectory of bipolar disorder. Br J Psychiatry 2014;204:122‐8. [DOI] [PubMed] [Google Scholar]
- 30. Goetz M, Sebela A, Mohaplova M et al. Psychiatric disorders and quality of life in the offspring of parents with bipolar disorder. J Child Adolesc Psychopharmacol 2017;27:483‐93. [DOI] [PubMed] [Google Scholar]
- 31. Maziade M, Gingras N, Rouleau N et al. Clinical diagnoses in young offspring from eastern Québec multigenerational families densely affected by schizophrenia or bipolar disorder. Acta Psychiatr Scand 2008;117:118‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Thorup AAE, Jepsen JR, Ellersgaard DV et al. The Danish High Risk and Resilience Study ‐ VIA 7 ‐ a cohort study of 520 7‐year‐old children born of parents diagnosed with either schizophrenia, bipolar disorder or neither of these two mental disorders. BMC Psychiatry 2015;15:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pedersen CB. The Danish Civil Registration System. Scand J Publ Health 2011;39(Suppl. 7):22‐5. [DOI] [PubMed] [Google Scholar]
- 34. Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Publ Health 2011;39(Suppl. 7):54‐7. [DOI] [PubMed] [Google Scholar]
- 35. Kaufman J, Birmaher B, Brent D et al. Schedule for Affective Disorders and Schizophrenia for School‐Age Children ‐ Present and Lifetime Version (K‐SADS‐PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980‐8. [DOI] [PubMed] [Google Scholar]
- 36. Shaffer D. A Children's Global Assessment Scale (CGAS). Arch Gen Psychiatry 1983;40:1228. [DOI] [PubMed] [Google Scholar]
- 37. Achenbach TM, Rescorla LA. Manual for the ASEBA School‐Age Forms & Profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families, 2001. [Google Scholar]
- 38. Makransky G, Bilenberg N. Psychometric properties of the parent and teacher ADHD Rating Scale (ADHD‐RS): measurement invariance across gender, age, and informant. Assessment 2014;21:694‐705. [DOI] [PubMed] [Google Scholar]
- 39. DuPaul G, Power TJ, Anastopoulos A et al. ADHD Rating Scale‐IV. New York: Guilford, 1998. [Google Scholar]
- 40. Barkley R, Gwenyth EH, Arthur LR. Defiant teens. A clinician's manual for assessment and family intervention. New York: Guilford, 1999. [Google Scholar]
- 41. McConaughy SH, Achenbach TM. Manual for the Test Observation Form for ages 2‐18. Burlington: University of Vermont, Center for Children, Youth, & Families, 2004. [Google Scholar]
- 42. Spielberger CD, Edwards CD, Lushene R et al. State‐Trait Anxiety Inventory for Children: sampler set, manual, test booklet, scoring key. Palo Alto: Mind Garden, 1973. [Google Scholar]
- 43. Zapf A, Castell S, Morawietz L et al. Measuring inter‐rater reliability for nominal data ‐ which coefficients and confidence intervals are appropriate? BMC Med Res Methodol 2016;16:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Duffy A, Horrocks J, Doucette S et al. Childhood anxiety: an early predictor of mood disorders in offspring of bipolar parents. J Affect Disord 2013;150:363‐9. [DOI] [PubMed] [Google Scholar]
- 45. Duffy A, Doucette S, Lewitzka U et al. Findings from bipolar offspring studies: methodology matters. Early Interv Psychiatry 2011;5:181‐91. [DOI] [PubMed] [Google Scholar]
- 46. Keshavan MS, Sujata M, Mehra A et al. Psychosis proneness and ADHD in young relatives of schizophrenia patients. Schizophr Res 2003;59:85‐92. [DOI] [PubMed] [Google Scholar]
- 47. Duffy A. The nature of the association between childhood ADHD and the development of bipolar disorder: a review of prospective high‐risk studies. Am J Psychiatry 2012;169:1247‐55. [DOI] [PubMed] [Google Scholar]
- 48. Maoz H, Goldstein T, Goldstein BI et al. The effects of parental mood on reports of their children's psychopathology. J Am Acad Child Adolesc Psychiatry 2014;53:1111‐22.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]


