Abstract
Objective
This study examined differences in clinical presentation of men and women with binge-eating disorder (BED) who participated in treatment research at a medical-school based program.
Methods
Participants were 682 adults (n=182 men, n=500 women) with DSM-IV-defined BED. Doctoral-level research clinicians assessed eating-disorder psychopathology, including BED diagnosis, using the Structured Clinical Interview for DSM-IV Disorders (SCID) and Eating Disorder Examination (EDE) interview. Research clinicians measured height and weight and participants completed a battery of established self-report measures.
Results
Men had significantly higher body mass index (BMI) than women; women had significantly higher eating-disorder psychopathology (EDE scales and global score) and depression than men. Differences in eating-disorder psychopathology and depression remained higher for women than men after adjusting for race/ethnicity and BMI. Frequency of binge-eating episodes, subjective binge-eating episodes, and overeating episodes did not differ significantly by sex. Women had younger ages of onset for dieting and binge-eating behaviors than men but ages of onset for obesity and BED did not significantly differ between men and women.
Conclusion
There are some sex differences in clinical presentation and age-of-onset timeline of adults with BED. Men and women develop obesity and BED (at diagnostic threshold) around the same age but women begin dieting and binge-eating behaviors earlier than men. At presentation for treatment for BED, men and women did not differ in binge-eating frequency and although men and women differed significantly on BMI and eating-disorder psychopathology, the magnitude of these differences was quite modest.
Keywords: binge-eating disorder, obesity, gender, sex, treatment, depression
Introduction
Binge-eating disorder (BED) has an estimated 12-month prevalence of 0.8–1.2%, which is higher than other eating disorders (Hudson, Hiripi, Pope, & Kessler, 2007; Kessler et al., 2013). The female-to-male ratio of individuals with BED of approximately 2:1 is less discrepant than for other eating disorders (Cossrow et al., 2016; Hudson et al., 2007; Kessler et al., 2013; Marques et al., 2011). Although community research has found that men and women who binge eat experience similar levels of clinical impairment (Marques et al., 2011; Striegel, Bedrosian, Wang, & Schwartz, 2012), men are underrepresented in treatment studies for BED (Shingleton, Thompson-Brenner, Thompson, Pratt, & Franko, 2015; Thompson-Brenner et al., 2013) and epidemiological studies have documented that men with BED seek treatment less often than women (Hudson et al., 2007; Marques et al., 2011).
Few studies have explored potential sex differences between men and women seeking treatment for BED (Barry, Grilo, & Masheb, 2002; Guerdjikova, McElroy, Kotwal, & Keck, 2007; Tanofsky, Wilfley, Spurrell, Welch, & Brownell, 1997). These preliminary studies, which were limited in power to detect differences given the small number of men (ns ranged only from 21 to 44), reported mostly non-significant differences between men and women in terms of binge-eating frequency and associated eating-disorder psychopathology. To examine sex differences more adequately among adults with BED, Shingleton et al. (2015) pooled data from nine research sites that enrolled patients in 11 treatment studies of psychosocial treatments to yield two study groups: men (n=208; 15.7%) and women (n=1117; 84.3%). This study found that men had a higher average BMI than women, women had higher eating-disorder psychopathology than men, but men and women did not differ on binge eating frequency. Findings from the Shingleton et al. (2015) study require extension for several reasons, including: (a) Shingleton et al. (2015) pooled data obtained with similar, but methodologically different, assessment measures for determining BED diagnoses and characterizing eating-disorder psychopathology (i.e., 9 studies used an investigator-based interview and 2 studies used a self-report questionnaire); (b) different sites contributing data had markedly different rates of men/women participants perhaps reflecting – to varying degrees – different recruitment strategies, inclusion and exclusion criteria, screening methods, and assessment procedures; and (c) participants were seeking psychosocial treatments. Thus, additional research is needed to characterize potential sex differences more definitively in adults with BED, including those who may seek pharmacological treatments.
The current study aimed to examine sex differences in adults’ clinical presentation in a large sample of adults with BED who sought treatment in the context of a research study; all research was conducted at one location that used consistent recruitment strategies, inclusion criteria, and assessment protocols. All participants were evaluated using a consistent, interview-based assessment of eating-disorder variables including binge-eating episodes and BED diagnosis. Based on earlier research using smaller samples of individuals with BED, we hypothesized that men would have heavier BMIs, lower eating-disorder psychopathology and lower depression than women.
Methods
Participants
Participants (N=682) responded to advertisements for pharmacological and psychosocial BED treatment studies that are reflective of the emerging literature on psychological treatments (Grilo, 2017b) and pharmacological treatments (McElroy, 2017). Treatment studies took place at an urban, medical-school based program located in the northeastern United States. Participants were between 18 and 65 years old and met full DSM-IV (American Psychiatric Association, 2004) criteria for BED1. All treatment studies required, in addition to BED, co-existing overweight or obesity (Grilo, 2017a; Grilo, Masheb, & Salant, 2005; Grilo et al., 2014; Grilo, Masheb, Wilson, Gueorguieva, & White, 2011; Grilo, White, Gueorguieva, Barnes, & Masheb, 2013). Participants were excluded if they were receiving outside treatment for eating/weight concerns, had medical conditions that influenced eating/weight (e.g., uncontrolled diabetes), were taking medications that could influence eating/weight (e.g., steroids), had a severe mental illness that could interfere with clinical assessment (e.g., psychosis), or were pregnant.
Men (n=182) and women (n=500) were included in the current analyses. Overall, participants had a mean age of 46.02 (SD=9.83). The mean BMI was 38.29 kg/m2 (SD=6.29). Participants self-identified as White (n=485, 71.3%), Black (n=114, 16.8%), Hispanic (n=53, 7.8%), or other race/ethnicity (n=28, 4.1%); 2 participants did not report race/ethnicity. Participants had varying levels of education: high school or less (n=134, 19.8%), some college (n=232, 34.9%), or a college degree or more (n=310, 45.9%); 6 participants did not report their education level.
This study received ethical approval from the Yale Human Investigations Committee; all participants provided written informed consent prior to study assessments.
Measures
Trained doctoral-level research clinicians, monitored to maintain reliability, evaluated participants. Research clinicians measured participants’ height and weight and calculated BMI (kg/m2). Research clinicians administered the Structured Clinical Interview for DSM-IV Axis I Disorders (First, Spitzer, Gibbon, & Williams, 1997) to determine DSM-IV-based BED diagnosis and age of onset, and the semi-structured Eating Disorder Examination (Fairburn & Cooper, 1993) to confirm BED diagnosis and characterize eating-disorder psychopathology.
Eating Disorder Examination (EDE)
The EDE (Fairburn & Cooper, 1993) is an investigator-based interview that evaluates eating-disorder psychopathology in the past 28 days, and over longer intervals corresponding to diagnostic criteria. The EDE also assesses three types of eating episodes: objective binge-eating episodes (OBEs, eating an unusually large amount of food while perceiving a loss of control over eating; this corresponds to the DSM-IV and DSM-5 definitions of binge-eating episodes), subjective binge-eating episodes (SBEs, eating a small or typical amount of food while perceiving a loss of control) and objective overeating episodes (OOEs, eating an unusually large amount of food without perceiving a loss of control). Four subscales (Restraint, Eating Concern, Shape Concern, and Weight Concern) and a Global severity score reflect eating-disorder psychopathology. Additionally, two items on the EDE assess overvaluation of weight and overvaluation of shape; the overvaluation construct involves an individual’s undue emphasis of weight or shape in his or her self-evaluation, and is thought to be a core cognitive feature of eating disorders including BED (Grilo, 2013). Ratings reflect the modal severity for the past 28 days and 4 is considered to be the clinical cut-point (Fairburn & Cooper, 1993; Goldschmidt et al., 2010). The EDE is a well-established interview for assessing eating disorders with good inter-rater and test-retest reliability in BED (Grilo, Masheb, Lozano-Blanco, & Barry, 2004). EDE items in the current study were internally consistent, α=.81, with excellent inter-rater reliability2.
Self-report Questionnaires
The Beck Depression Inventory (BDI) is a well-established measure of depression (Beck & Steer, 1987) that captures a broad range of negative affect. The BDI has excellent psychometric properties (Beck, Steer, & Carbin, 1988). In the current study, internal consistency was excellent, α=.89. The Questionnaire for Eating and Weight Patterns, Revised (QEWP-R), used in DSM-IV field trials, assesses the current and historical aspects (onset of obesity, dieting, binge-eating behaviors, as well as recent participation in a weight control program) of BED and obesity (Yanovski, 1993) that were used in this study.
Statistical Analyses
To evaluate sex differences, chi-square tests (categorical variables) and analyses of variance (ANOVAs; continuous variables) compared men and women. OBE, SBE, and OOE variables were transformed by square-root prior to analyses to meet the assumption of normality. Analyses of covariance (ANCOVAs) adjusted for race/ethnicity and BMI. Additionally, partial eta-squared (ηp2), an effect-size measure that describes the proportion of the total variance attributable to each independent variable, was calculated. Partial eta squared (ηp2) values are considered small at .01, medium at .06, and large at .14 (Cohen, 1988).
Results
Sex Differences in Demographic Characteristics
Table 1 summarizes demographic variables and statistical tests of differences between men (n=182) and women (n=500) included in this study. A comparison of proportions revealed a significant sex difference in distribution of race/ethnicity (a greater proportion of men were White and a greater proportion of women were Black). Additionally, women (n=137, 28.4%) were more likely to have participated in a weight control program in the 6 months prior to the treatment study compared with men (n=21, 11.6%). Age and education did not differ significantly between men and women.
Table 1.
Demographic and clinical variables by sex.
| Men n=182 |
Women n=500 |
χ2 | N | p | φ | |
|---|---|---|---|---|---|---|
| Race/Ethnicity | 5.69 | 680 | .128 | .092 | ||
| White | 77.8%* | 69.0% | ||||
| Black | 11.7%* | 18.6% | ||||
| Hispanic | 7.2% | 8.0% | ||||
| Other | 3.3% | 4.4% | ||||
| Education | 0.59 | 676 | .744 | .030 | ||
| High School | 21.8% | 19.1% | ||||
| Some College | 33.5% | 34.6% | ||||
| College Degree | 44.7% | 46.3% | ||||
| Treatment in Past 6 months | 11.6%* | 28.4% | 20.40 | 664 | <.001 | .175 |
| M (SD) | M (SD) | F | Total df | p | ηp2 | |
|
|
||||||
| Age | 47.08 (9.30) | 45.63 (9.99) | 2.92 | 682 | .088 | .004 |
Note. Percentages reflect the proportion of participants from one sex (column) in the demographic category (row).
Specific contrasts were performed within race/ethnicity and education and significant differences between women and men (p<.05) are starred.
Sex Differences in Clinical Characteristics
Table 2 summarizes the clinical characteristics along with statistical tests comparing men and women, as well as parallel statistical tests after adjusting for race/ethnicity and BMI. BMI was significantly higher for men than women. Eating-disorder psychopathology (all EDE scales, global score, and mean of overvaluation of weight and shape) was significantly higher for women than for men; these differences generally maintained their significance after adjusting for BMI and race/ethnicity. Depression was also higher among women than men, and this also remained significant after adjusting for BMI and race/ethnicity. OBE, SBE, and OOE frequencies did not differ significantly between men and women. Inspection of overvaluation of weight or shape categorically (i.e., “moderate” or higher overvaluation of weight or shape) revealed that despite statistically differences in the continuous variable, similar proportions of men (61.5%) and women (66.6%) had clinical levels of overvaluation of weight or shape, χ2(1, N = 682) = 1.51, p = .220, φ = .047.
Table 2.
Analyses of variance and pairwise comparisons comparing men and women.
| Men n=182 |
Women n=500 |
ANOVA | ANCOVA (adj. race, BMI) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| M (SD) | M (SD) | F | N | p | ηp2 | p | ηp2 | |
| BMI | 39.14 (6.12) | 37.98 (6.32) | 4.58 | 679 | .033 | .007 | n/a | n/a |
| Episodes | ||||||||
| OBE | 18.68 (15.04) | 17.55 (11.85) | 0.42 | 682 | .516 | .001 | .200 | .007 |
| SBE | 9.05 (14.29) | 8.24 (13.22) | 1.21 | 681 | .272 | .002 | .618 | .003 |
| OOE | 3.73 (7.53) | 3.05 (6.39) | 0.34 | 682 | .559 | .001 | .388 | .004 |
| EDE Global Score | 2.35 (0.86) | 2.82 (0.88) | 38.94 | 682 | <.001 | .054 | <.001 | .052 |
| Restraint | 1.63 (1.26) | 1.90 (1.32) | 5.75 | 682 | .017 | .008 | .015 | .015 |
| Eating | 1.64 (1.28) | 2.21 (1.30) | 25.99 | 682 | <.001 | .037 | <.001 | .042 |
| Shape | 3.26 (1.14) | 3.80 (1.10) | 31.85 | 682 | <.001 | .045 | <.001 | .044 |
| Weight | 2.85 (0.98) | 3.36 (1.01) | 34.48 | 682 | <.001 | .048 | <.001 | .048 |
| Overvaluation | 3.32 (1.72) | 3.72 (1.75) | 7.13 | 682 | .008 | .010 | .05 | .011 |
| BDI | 13.84 (8.39) | 16.54 (9.04) | 12.34 | 677 | <.001 | .018 | <.001 | .027 |
| Age of Onset | ||||||||
| Obesity | 18.32 (11.43) | 17.32 (10.20) | 1.06 | 616 | .303 | .002 | .092 | .005 |
| Dieting | 26.21 (10.66) | 21.13 (8.86) | 31.16 | 560 | <.001 | .053 | <.001 | .064 |
| Binge Eating | 26.83 (12.97) | 22.77 (12.18) | 12.34 | 599 | <.001 | .020 | <.001 | .022 |
| BED | 28.04 (13.96) | 27.20 (13.38) | 0.47 | 635 | .491 | .001 | .463 | .001 |
Note. Partial eta squared (ηp2) values are considered small at .01, medium at .06, and large at .14 (Cohen, 1988). OBE, SBE, and OOE variables were square root-transformed to meet assumptions of normality. However, we report non-transformed means here to facilitate interpretation. BMI=Body Mass Index; OBE=Objective binge episode; SBE=Subjective binge episode; OOE=Objective overeating episode; EDE=Eating Disorder Examination; BDI=Beck Depression Inventory; BED=Binge eating disorder.
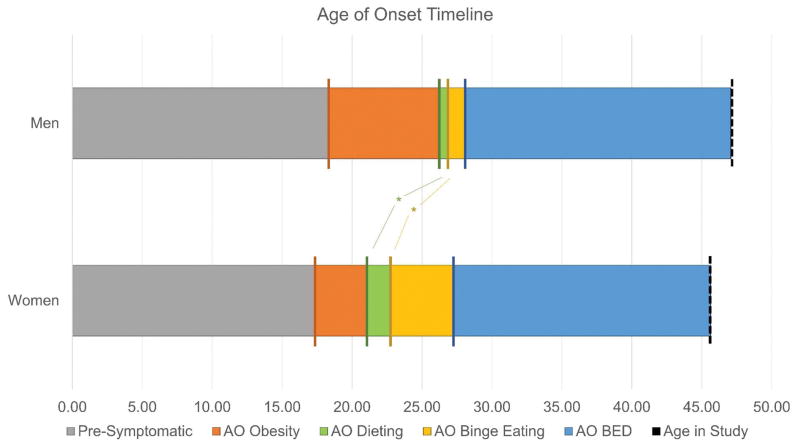
Exploratory Analyses of Age-of-Onset Timelines
Figure 1 depicts the age-of-onset timelines of obesity, dieting, binge-eating behaviors, and BED as reported by participants at the time of the study. ANCOVAs adjusted for race/ethnicity and BMI. Dieting and binge-eating behavior onset was younger for women than for men; this maintained significance after adjusting for race/ethnicity and BMI. Age of obesity and BED onset did not significantly differ between men and women. Men were significantly older than women at the time of the study.
Figure 1.
BED age-of-onset timeline for men and women in BED treatment studies.
Note. This figure depicts the mean ages of onset (AO) for obesity, dieting, binge eating, and binge-eating disorder (BED) as reported by participants at the time of the study.
* Significant differences at the p<.05 level between men and women. Omitted asterisks indicate nonsignificant differences.
Discussion
The current study examined sex differences in the clinical presentation of adults with BED who participated in treatment studies for BED. Our aim was to extend earlier research (Shingleton et al., 2015) by using a large study group of adults who participated in treatment studies at one location and were assessed using a consistent, interview-based protocol, to provide a definitive examination of sex differences in men and women with BED. Our findings indicate that men have a higher BMI and lower eating-disorder psychopathology and depression than women when they present for treatment, but similar frequencies of binge-eating episodes. Notably, the differences between women and men do not have a large magnitude. This suggests that although there are some statistically-significant sex differences among men and women with BED, those differences may not warrant different approaches to assessment or treatment formulation.
Our study also provided new data and findings regarding potential sex differences in the developmental aspects of BED and excess weight. Men and women develop obesity and full-threshold BED around the same ages, but women begin dieting and binge-eating behaviors earlier than men. This suggests that women may experience eating problems for a longer time than men, who appear to develop BED more rapidly once they begin dieting. The longer duration of eating problems for women may account for some of the sex differences observed in eating-disorder psychopathology.
Our findings are consistent with those of Shingleton et al. (2015), which were based on pooled psychosocial trial data: men have higher BMI and lower psychopathology than women, yet there is no sex difference in binge-eating episode frequency. One primary difference between our findings and those of Shingleton et al. (2015) was in dietary restraint. Our study found that women were statistically significantly higher than men on dietary restraint whereas Shingleton et al. (2015) found no sex differences; we note that our significant difference had a small magnitude. The current study also provided new evidence of sex differences in the age-of-onset timeline among individuals with BED. Men and women both developed obesity first, at similar ages, followed by dieting (significantly younger for women), followed by binge-eating behavior (significantly younger for women), followed by full-threshold BED at similar ages.
These results suggest that women had eating problems for a longer duration than men, who appear to develop BED more rapidly after dieting begins. These exploratory findings, which were based on retrospective data, warrant prospective investigation. If this timeline were confirmed by prospective studies, it is possible that different targets for prevention programs may apply to women (who could have an intervention earlier on to prevent the development of full-threshold BED) and men (who may need to be captured at the onset of the disorder since its development is more rapid).
Findings have implications for clinical practice. Men had higher BMIs than women, albeit less than 2 kg/m2 different; this may put them at a marginally greater risk for obesity-related health problems that require additional medical monitoring. Women, on the other hand, had higher eating-disorder psychopathology. Sex differences in eating-disorder psychopathology may be a true indicator of more problematic eating-disorder thoughts and behaviors among women, but may also be reflective of the relevance of some questions to men. The magnitude of differences between men and women across subscales suggest that these differences are clinically minimal. Such findings are important in that they strongly challenge clinical lore that men with BED are characterized by lower levels of cognitive and affective aspects of eating-disorder psychopathology than women. Thus, clinicians should assess specifically for the full range of eating-disorder psychopathology, including for example, shape and weight concerns, when evaluating men seeking treatment for BED.
Results from our study pertain to men and women from the urban northeastern United States and our findings regarding similarities and differences apply to adults with BED who chose to participate in treatment studies for BED. Generalizability to individuals who seek treatment in different clinical settings (Marques et al., 2011), those who do not seek treatment, or those who do not wish to participate in treatment research is uncertain. It is not known whether there may be different sex differences among individuals with BED who do not seek treatment, those who choose not to participate in treatment research studies, or those who seek treatment in different setting. The study design allowed us to complement the findings of Shingleton et al. (2015) aggregated data that may have systematic error variance due to geographical or site-specific differences. Data from trials included in the current study used consistent study protocols, including recruitment, assessment protocols, inclusion and exclusion criteria, and supervision procedures.
As well as the study strengths, it is important to interpret findings in the context of study limitations. We analyzed sex differences and although sex is in many ways similar to the social construct of gender, we did not assess the extent to which participants identified with female or male genders. Gender identity may yield more nuanced information about adults seeking BED treatment. Additionally, our sample was comprised of adults with BED who enrolled in treatment studies at a university-based medical school in a specialist eating-disorder clinic, and we had some safety-based exclusion criteria. Most participants were White, well-educated, and had a BMI in the overweight or obesity range. Examination of how sex differences may intersect with race/ethnicity and education may yield important findings. Moreover, generalizability to patients with BED who do not have co-morbid overweight or obesity, and those who seek treatment for co-existing medical problems (e.g., uncontrolled diabetes) is also uncertain. Of note, nearly 75% of individuals with BED have a BMI in the overweight or obese range (Kessler et al., 2013). Yet, because clinical characteristics may be associated with BMI, future research should examine potential sex differences across weight categories. Finally, although our primary outcomes (BMI and eating-disorder psychopathology) were measured by independent, doctoral-level research clinicians, the age-of-onset variables were self-reported. Retrospective data can be inaccurate or biased, so our findings should be considered exploratory until the hypotheses they generate can be tested using prospective research designs.
Sex differences in the clinical presentation of individuals with BED are important for clinicians and clinical researchers to understand, and may help guide clinical evaluation and treatment formulation and perhaps may inform refinement of treatment and prevention efforts. Additional research, including research on men’s and women’s experiences of treatment and whether sex predicts or moderates treatment outcomes, can help advance this work further. The Shingleton et al. (2015) study found minimal sex differences in treatment outcomes with psychosocial interventions. Those findings warrant replication and extension to additional treatment approaches. Our findings here about the age-of-onset timeline (i.e., younger dieting and binge-eating behavior for women; more rapid onset of BED after men begin dieting) should also be replicated to determine if the timing of prevention or early intervention work may differ for men and women.
Acknowledgments
Dr. Grilo reports research grants from the National Institutes of Health (K24 DK070052, R01 DK49587, R01 DK073542) that supported this research; this paper does not reflect the view of the Public Health Service nor the NIH and they played no role in the content of this paper.
Funding: This research was supported, in part, by National Institutes of Health grants K24 DK070052, R01 DK49587, and R01 DK073542.
Footnotes
DSM-IV (APA, 2004) BED research criteria include binge eating at least twice weekly (eating an objectively large amount of food while experiencing a subjective loss of control) for six months, without weight compensatory behaviors (e.g., purging). These criteria are more stringent than the newly published DSM-5 BED diagnostic criteria, which require binge eating at least once weekly for three months. All participants who met DSM-IV criteria would also meet DSM-5 criteria for BED.
In the data for the present study, inter-rater reliability of the EDE was examined in 113 cases. The intraclass correlation coefficient for OBEs was 0.94, Global severity score was 0.92, Restraint was 0.92, Eating Concern was 0.78, Weight Concern was 0.91, and Shape Concern was 0.94.
Dr. Grilo reports several broader interests which did not influence this research or paper. Dr. Grilo’s broader interests include: Consultant and advisory board to Shire and Sunovion; Honoraria for lectures and CME activities from Physician’s Postgraduate Press CME Institute, Physicians Education Resources CME Institute; Global Medical Education CME Institure; Vindico CME, Medscape Medical Education, Honoraria for lectures and presentations at scientific conferences and grand rounds, Honoraria from American Psychological Association for editorial roles; and Royalties from Guilford Press and Taylor & Francis Publishers for academic books.
Potential conflicts of interest: Dr. Lydecker reports no conflicts of interest. Dr. Grilo reports no relevant conflicts of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: Author; 2004. Text Revision ed. [Google Scholar]
- Barry DT, Grilo CM, Masheb RM. Gender differences in patients with binge eating disorder. Int J Eat Disord. 2002;31:63–70. doi: 10.1002/eat.1112. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer R. Manual for revised Beck Depression Inventory. New York: Psychological Corporation; 1987. [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cossrow N, Pawaskar M, Witt EA, Ming EE, Victor TW, Herman BK, … Erder MH. Estimating the prevalence of binge eating disorder in a community sample from the United States: Comparing DSM-IV-TR and DSM-5 criteria. J Clin Psychiatry. 2016;77:e968–974. doi: 10.4088/JCP.15m10059. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. New York: Guilford Press; 1993. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), Clinician Version. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Goldschmidt AB, Hilbert A, Manwaring JL, Wilfley DE, Pike KM, Fairburn CG, … Striegel-Moore RH. The significance of overvaluation of shape and weight in binge eating disorder. Behav Res Ther. 2010;48:187–193. doi: 10.1016/j.brat.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM. Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? Int J Eat Disord. 2013;46:208–211. doi: 10.1002/eat.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM. Behavioral weight loss vs stepped multi-modal treatment for binge eating disorder: Acute and longer-term 18-month outcomes. Ann Behav Med. 2017a;51:S752–S753. [Google Scholar]
- Grilo CM. Psychological and Behavioral Treatments for Binge-Eating Disorder. J Clin Psychiatry. 2017b;78(Suppl 1):20–24. doi: 10.4088/JCP.sh16003su1c.04. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int J Eat Disord. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Salant SL. Cognitive behavioral therapy guided self-help and orlistat for the treatment of binge eating disorder: A randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2005;57:1193–1201. doi: 10.1016/j.biopsych.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, White MA, Gueorguieva R, Barnes RD, Walsh BT, … Garcia R. Treatment of binge eating disorder in racially and ethnically diverse obese patients in primary care: Randomized placebo-controlled clinical trial of self-help and medication. Behav Res Ther. 2014;58:1–9. doi: 10.1016/j.brat.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, White MA. Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. J Consult Clin Psychol. 2011;79:675–685. doi: 10.1037/a0025049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, White MA, Gueorguieva R, Barnes RD, Masheb RM. Self-help for binge eating disorder in primary care: A randomized controlled trial with ethnically and racially diverse obese patients. Behav Res Ther. 2013;51:855–861. doi: 10.1016/j.brat.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerdjikova AI, McElroy SL, Kotwal R, Keck PE., Jr Comparison of obese men and women with binge eating disorder seeking weight management. Eat Weight Disord. 2007;12:e19–23. doi: 10.1007/BF03327777. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, … Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73:904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, Diniz JB. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44:412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy SL. Pharmacologic Treatments for Binge-Eating Disorder. J Clin Psychiatry. 2017;78(Suppl 1):14–19. doi: 10.4088/JCP.sh16003su1c.03. [DOI] [PubMed] [Google Scholar]
- Shingleton RM, Thompson-Brenner H, Thompson DR, Pratt EM, Franko DL. Gender differences in clinical trials of binge eating disorder: An analysis of aggregated data. J Consult Clin Psychol. 2015;83:382–386. doi: 10.1037/a0038849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel RH, Bedrosian R, Wang C, Schwartz S. Why men should be included in research on binge eating: Results from a comparison of psychosocial impairment in men and women. Int J Eat Disord. 2012;45:233–240. doi: 10.1002/eat.20962. [DOI] [PubMed] [Google Scholar]
- Tanofsky MB, Wilfley DE, Spurrell EB, Welch R, Brownell KD. Comparison of men and women with binge eating disorder. Int J Eat Disord. 1997;21:49–54. doi: 10.1002/(sici)1098-108x(199701)21:1<49::aid-eat6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, Franko DL, Thompson DR, Grilo CM, Boisseau CL, Roehrig JP, … Wilson GT. Race/ethnicity, education, and treatment parameters as moderators and predictors of outcome in binge eating disorder. J Consult Clin Psychol. 2013;81:710–721. doi: 10.1037/a0032946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanovski SZ. Binge eating disorder: Current knowledge and future directions. Obes Res. 1993;1:306–324. doi: 10.1002/j.1550-8528.1993.tb00626.x. [DOI] [PubMed] [Google Scholar]