Abstract
Rates of venous thromboembolism have increased in the adolescent population over the last two decades, likely due to advanced diagnostics, increased use of central venous catheters, chronic medical conditions, obesity, and oral contraceptive use [1]. Of these factors, a modifiable risk factor for adolescents is obesity. Sedentary lifestyle and prolonged immobilization are additional prothrombotic risk factors that are often associated with obesity. With ever-increasing screen time, sedentary behavior has risen accordingly, especially among gamers. We present four cases of adolescents who developed life-threatening venous thromboembolic events in the setting of obesity, sedentary lifestyle and/or immobilization, and prolonged video game use.
Keywords: Adolescents, thrombosis, obesity, sedentary, video games, electronics
INTRODUCTION
Pediatric venous thromboembolism (VTE) is rare with an incidence rate of 0.7–4.9 per 100,000 person-years[1–5]. Two peaks in incidence are noted: one in infants <1 year and the second in adolescents. Over the last two decades, there has been an increase in pediatric VTE, attributable to improved diagnostics, clinical awareness, and increasing risk factors—higher complexity of care, central venous catheters, obesity, and increased use of oral contraceptive pills[1].
Notably, between 1980–2012 obesity has more than doubled in children aged 6–11 (7% to 18%) and quadrupled in adolescents aged 12–19 (5% to 21%)[6]. Among other lifestyle factors, sedentary behavior is a risk factor for obesity as well as thrombosis. Children and adolescents spend 8 hours/day on average engaging in sedentary behavior including watching television, playing videogames, and participating in other electronic activities[7]. Given the pediatric VTE direct mortality rate of 2% and risk for post-thrombotic syndrome of 26%[8,9], it is important to understand underlying modifiable risk factors so that we can work towards prevention of thrombotic events in this population. We present a case series of four adolescent obese males who developed VTEs in the setting of excessive sedentary behavior, specifically prolonged video game use, among other risk factors. This observation raises concern about the contribution of increasing screen time and obesity rates on the risk for VTE, especially in the adolescent population.
RESULTS
Case 1
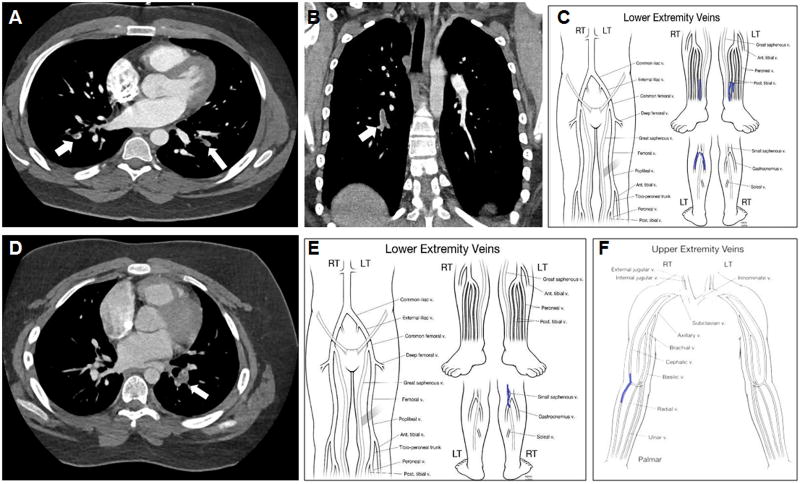
An 18-year-old obese male (BMI 37 kg/m2) presented with bilateral pulmonary emboli (PE) and an associated right lower lobe infarction (Figure 1A). He had a very sedentary lifestyle, spending up to 12 consecutive hours playing video games per day. No other risk factors or significant family history were identified. Thrombophilia testing revealed factor V Leiden (FVL) heterozygosity, but no other abnormalities. This patient received 6 months of anticoagulation. Lifestyle modification counseling addressed healthy diet, exercise, hydration, and avoidance of tobacco products. At 17 months from his diagnosis, he has lost 36 kg (BMI 25 kg/m2), which he has sustained for 6 months, and he has remained VTE recurrence-free.
FIGURE 1.
(A) Chest CT, axial view, revealing a pulmonary embolism (arrows) in case 1. (B) Chest CT scan, coronal view, revealing an acute right pulmonary artery embolism (arrow) in case 2. (C) Lower extremity mapping computed from ultrasound revealing thromboses in bilateral posterior tibial veins and left upper calf gastrocnemius vein (case 2). (D) Pulmonary embolism on chest CT scan in case 3 (arrow). (E) Lower extremity mapping computed from ultrasound revealing a right saphenous vein thrombus in case 3. (F) Upper extremity mapping demonstrating bilateral cephalic vein thromboses in case 3.
Case 2
A 15-year-old obese male (BMI 50 kg/m2) presented with autoimmune hemolytic anemia with a hemoglobin of 4.0 g/dL, and was started on high-dose corticosteroids. On hospital day 3 he developed acute occlusive thrombi in the bilateral posterior tibial veins and in the gastrocnemius vein in the left upper calf. A chest CT was performed and revealed an acute PE in the descending branch of the right pulmonary artery (Figure 1B–C). Prior to his VTE, he endorsed a sedentary lifestyle, playing video games 4–12 hours/day. Due to his symptomatic anemia, his physical activity was further limited preceding the VTE. Given his critical illness, obesity, and immobility, his VTE was considered provoked, and no further thrombophilia testing was pursued. He received anticoagulation for 6 months and participated in a weight management program which encouraged increased physical activity. Though he has been unable to sustain weight loss, he has remained recurrence free for 12 months with improved physical activity.
Case 3
A 13-year-old obese male (BMI 56 kg/m2) developed a left lower lobe PE (Figure 1D) in the setting of 3-week immobility secondary to Guillain-Barre syndrome. He also had occlusive thromboses in bilateral cephalic veins and in the right saphenous vein (Figure 1E–F). In addition to his immobility secondary to Guillain-Barre syndrome, he also had a sedentary lifestyle at baseline, playing video games for several consecutive hours/day. His family history was positive for father developing a line-associated thrombus. Thrombophilia testing was recommended, but declined. This patient received 3 months of anticoagulation and 6 months of physical therapy which promoted a more active lifestyle.
Case 4
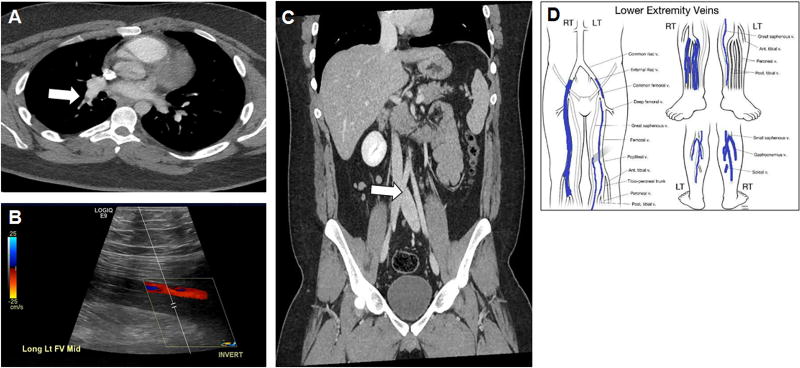
A 17-year-old obese male (BMI 39 kg/m2) developed bilateral basilar PE (Figure 2A) and pulmonary infarctions in the setting of a left proximal femoral DVT (Figure 2B). Prior to the VTE, he was sedentary for several hours playing video games. Comprehensive thrombophilia testing identified FVL heterozygosity. Given the location of the DVT, he underwent a CT venogram, which revealed mild compression of the left common iliac vein as it passed under the right common iliac artery (Figure 2C), consistent with May-Thurner syndrome. He received 6 months of anticoagulation. Lifestyle modifications were discussed though he was unable to lose weight, and in fact, gained weight with no improvement in sedentary behavior. Eight months after completion of therapy, he developed a new occlusive DVT in the contralateral (right) lower extremity extending from the common femoral vein down to his calf veins (Figure 2D). He was then placed on life-long anticoagulation.
FIGURE 2.
Case 4 (A) Pulmonary embolism on chest CT (arrow); (B) Initial deep venous thrombosis on ultrasound; (C) Mild compression of the left common iliac vein as it passes under the right common iliac artery (arrow); (D) Lower extremity mapping computed from ultrasound revealing an extensive right LE deep venous thrombosis (second event).
DISCUSSION
With the rising incidence of thromboembolism in adolescents, it is important to identify modifiable risk factors associated with this increase[1,8,9]. In a recent study of adolescent thromboembolism, associated risk factors for developing a thromboembolic event included obesity in 47%, central venous catheters in 27%, infection in 27%, surgery in 27%, immobility in 22%, autoimmune disease in 19%, and other medical conditions in 11% of patients[10]. Pediatric VTE is often a result of a combination of at least two prothrombotic risk factors[11]. Certainly, our four patients had risk factors beyond obesity, sedentary lifestyle, and prolonged video game use, however, the contribution of these prothrombotic risk factors in addition to others (i.e., FVL heterozygosity, immobilization due to illness, autoimmune and inflammatory conditions), possibly resulted in major VTEs. However, it should be noted that FVL heterozygosity is only a minor risk factor for VTE.
The combination of sedentary lifestyle and the growing popularity of electronic gaming in adolescents, especially “extreme gamers” playing up to 48.5 hours/week[12], may pose excessive VTE risk, especially in the setting of obesity. More routine gamers spend 13 hours/week playing video games, and up to 97% of adolescents report playing any electronic games[12,13]. While gaming, most players are sedentary, often in seated or cross-legged positions. Since prolonged seated immobility is a well-established risk factor for developing VTE in the setting of travel[14], one could hypothesize that immobility in the setting of gaming confers a similar risk.
A case-control study that evaluated prolonged work- and computer-related seated immobility demonstrated an increased risk of VTE in adults that were seated for at least 10 hours/day including at least 2 consecutive hours without getting up[15]. Additionally, prolonged television viewing is a documented risk factor for mortality from PE in adults[16]. Many case reports link prolonged gaming (3 to 80 continuous hours) to thromboses, often termed “eThrombosis”[12,17–20].
Identifying prolonged video game use and immobility in the setting of obesity may be essential in risk assessment and counseling. With further investigation of prolonged gaming as a pro-thrombotic risk factor, it is conceivable that these VTEs could be considered “provoked”. Of note, gaming may be a surrogate marker for sedentary lifestyle instead of an independent risk factor; however, inquiring about gaming time may be an important window into understanding the degree of sedentary behavior. Encouraging patients to have a more active lifestyle and to minimize screen time may reduce the risk of VTE in adolescents. Providers could recommend taking breaks hourly to stretch/walk while gaming. Furthermore, combining weight management clinics or exercise programs with thrombosis clinics may reduce VTE risk. Though observational, this case series highlights prolonged video game use as an important potential VTE risk factor that should be studied further in larger, prospective cohorts.
Acknowledgments
Research reported in this publication was supported, in part, by the Mayo Clinic-National Institutes of Health Clinical Pharmacology Training Grant T32 GM08685. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ABBREVIATIONS KEY
- VTE
Venous thromboembolism
- DVT
Deep venous thrombosis
- CT
Computed tomography
- OCP
Oral contraceptive pills
- PE
Pulmonary embolism
- FVL
Factor V Leiden
Footnotes
CONFLICTS OF INTEREST
None
References
- 1.Tuckuviene R, Christensen AL, Helgestad J, et al. Pediatric venous and arterial noncerebral thromboembolism in Denmark: a nationwide population-based study. J Pediatr. 2011;159(4):663–669. doi: 10.1016/j.jpeds.2011.03.052. [DOI] [PubMed] [Google Scholar]
- 2.Stein PD, Kayali F, Olson RE. Incidence of venous thromboembolism in infants and children: data from the National Hospital Discharge Survey. J Pediatr. 2004;145(4):563–565. doi: 10.1016/j.jpeds.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 3.Andrew M, David M, Adams M, et al. Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 1994;83(5):1251–1257. [PubMed] [Google Scholar]
- 4.van Ommen CH, Heijboer H, Buller HR, et al. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 2001;139(5):676–681. doi: 10.1067/mpd.2001.118192. [DOI] [PubMed] [Google Scholar]
- 5.Sabapathy CA, Djouonang TN, Kahn SR, et al. Incidence Trends and Mortality from Childhood Venous Thromboembolism: A Population-Based Cohort Study. J Pediatr. 2016;172:175–180 e171. doi: 10.1016/j.jpeds.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Fryar CD, et al. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. [PubMed] [Google Scholar]
- 7.Roberts JD, Rodkey L, Ray R, et al. Electronic media time and sedentary behaviors in children: Findings from the Built Environment and Active Play Study in the Washington DC area. Prev Med Rep. 2017;6:149–156. doi: 10.1016/j.pmedr.2017.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Estepp JH, Smeltzer M, Reiss UM. The impact of quality and duration of enoxaparin therapy on recurrent venous thrombosis in children. Pediatr Blood Cancer. 2012;59(1):105–109. doi: 10.1002/pbc.23396. [DOI] [PubMed] [Google Scholar]
- 9.Chalmers EA. Epidemiology of venous thromboembolism in neonates and children. Thromb Res. 2006;118(1):3–12. doi: 10.1016/j.thromres.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Ishola T, Kirk SE, Guffey D, et al. Risk factors and co-morbidities in adolescent thromboembolism are different than those in younger children. Thromb Res. 2016;141:178–182. doi: 10.1016/j.thromres.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 11.Gerotziafas GT. Risk factors for venous thromboembolism in children. Int Angiol. 2004;23(3):195–205. [PubMed] [Google Scholar]
- 12.Chang HC, Burbridge H, Wong C. Extensive deep vein thrombosis following prolonged gaming ('gamer's thrombosis'): a case report. J Med Case Rep. 2013;7:235. doi: 10.1186/1752-1947-7-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lenhart AKJ, Middaugh E, Rankin Macgill A, Evans C, Vitak J. Teens’ gaming experiences are diverse and include significant social interaction and civic engagement. 2008 [Google Scholar]
- 14.Beasley R, Heuser P, Raymond N. SIT (seated immobility thromboembolism) syndrome: a 21st century lifestyle hazard. N Z Med J. 2005;118(1212):U1376. [PubMed] [Google Scholar]
- 15.Healy B, Levin E, Perrin K, et al. Prolonged work- and computer-related seated immobility and risk of venous thromboembolism. J R Soc Med. 2010;103(11):447–454. doi: 10.1258/jrsm.2010.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shirakawa T, Iso H, Yamagishi K, et al. Watching Television and Risk of Mortality From Pulmonary Embolism Among Japanese Men and Women: The JACC Study (Japan Collaborative Cohort) Circulation. 2016;134(4):355–357. doi: 10.1161/CIRCULATIONAHA.116.023671. [DOI] [PubMed] [Google Scholar]
- 17.Phipps C, Ng HJ. Upper limb deep vein thrombosis and portable computer games. Am J Med. 2008;121(6):e3. doi: 10.1016/j.amjmed.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 18.Chew HC. Shortness of breath in a computer gamer. Am J Emerg Med. 2006;24(7):892–894. doi: 10.1016/j.ajem.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 19.Lee H. A new case of fatal pulmonary thromboembolism associated with prolonged sitting at computer in Korea. Yonsei Med J. 2004;45(2):349–351. doi: 10.3349/ymj.2004.45.2.349. [DOI] [PubMed] [Google Scholar]
- 20.Beasley R, Raymond N, Hill S, et al. eThrombosis: the 21st century variant of venous thromboembolism associated with immobility. Eur Respir J. 2003;21(2):374–376. doi: 10.1183/09031936.03.00039403. [DOI] [PubMed] [Google Scholar]