Abstract
Background
Cannabis legalization in Colorado resulted in increased cannabis-associated health care utilization. Our objective was to examine cooccurrence of cannabis and mental health diagnostic coding in Colorado emergency department (ED) discharges and replicate the study in a subpopulation of ED visits where cannabis involvement and psychiatric diagnosis were confirmed through medical review.
Methods
We collected statewide ED International Classification of Diseases, 9th Revision, Clinical Modification diagnoses from the Colorado Hospital Association and a subpopulation of ED visits from a large, academic hospital from 2012 to 2014. Diagnosis codes identified visits associated with mental health and cannabis. Codes for mental health conditions and cannabis were confirmed by manual records review in the academic hospital subpopulation. Prevalence ratios (PRs) of mental health ED discharges were calculated to compare cannabis-associated visits to those without cannabis. Rates of mental health and cannabis-associated ED discharges were examined over time.
Results
Statewide data demonstrated a fivefold higher prevalence of mental health diagnoses in cannabis-associated ED visits (PR = 5.35, 95% confidence interval [CI], 5.27–5.43) compared to visits without cannabis. The hospital subpopulation supported this finding with a fourfold higher prevalence of psychiatric complaints in cannabis attributable ED visits (PR = 4.87, 95% CI = 4.36–5.44) compared to visits not attributable to cannabis. Statewide rates of ED visits associated with both cannabis and mental health significantly increased from 2012 to 2014 from 224.5 to 268.4 per 100,000 (p < 0.0001).
Conclusions
In Colorado, the prevalence of mental health conditions in ED visits with cannabis-associated diagnostic codes is higher than in those without cannabis. There is a need for further research determining if these findings are truly attributed to cannabis or merely coincident with concurrent increased use and availability.
Medical cannabis liberalization in 2009 resulted in a rapid increase of the social acceptability of marijuana use in Colorado. In November 2012, Colorado voters approved state constitutional amendment 64, making recreational marijuana legal and further increasing the accessibility of cannabis use in the state.1 Fully legal state sales of cannabis to the general public began on January 1, 2014. The legalization of medical cannabis in 2001 and the development of a fully commercialized medical cannabis industry in 2009 led to normalized and destigmatized use preceding full legalization. Increased patient reporting and increased provider surveillance occurred during this period, prior to full legalization, thus providing a unique setting to examine health-related associations with cannabis use that minimizes reporting and surveillance bias. Questioning cannabis use patterns has become standard practice in Colorado emergency departments (EDs) since 2010.2 Thus, Colorado provides the optimal environment to study health outcomes associated with cannabis use.
Emergency department data provide a unique perspective on emerging disease trends. This perspective is especially important when new exposures, such as increased cannabis utilization, become more common. Emergency physician observations have yielded increased understanding of the health impact of cannabis, such as tourist ED visits related to marijuana3, butane hash oil associated burns4, cannabinoid hyper-emesis5, and many other conditions.6 Similarly, Colorado emergency physicians have noted an increase in cannabis associated psychiatric visits to local EDs.7 However, it is unclear if this association is due to increased use in the general population or if there is a disproportionate rise in cannabis associated psychiatric visits.
Cannabis use is known to exacerbate some mental health disorders like schizophrenia, personality, mood, and anxiety disorders.8–22 Cannabis use can result in development of psychotic symptoms and early onset of psychosis.23–25 Additionally, early cannabis use is a potential risk factor for diagnosis of psychotic disorders.8,11,12,26 Use of cannabis with high delta-9-tetrahy-drocannabinol (Δ9-THC), which is common in Colorado, has been shown to increase the risk of a first episode of psychosis, and daily use exacerbated this risk.23–26 Acute high doses of Δ9-THC and cumulative lifetime cannabis use may result in anxiety attacks or panic disorders.13,27–30 In an environment where high Δ9-THC cannabis is the norm, additional examination of mental health conditions among cannabis users is warranted.
Survey data demonstrate that past month cannabis use has remained constant in Colorado residents since legalization in 2014.31 However, increased health care utilization associated with acute and chronic cannabis use has been observed.3,32–34 According to the Colorado 2014–2016 Behavioral Risk Factors Surveillance System, the prevalence of current mental health distress (14 or more poor mental health days) was 10.1% and a prior diagnosis of depression was present in 18.4% of Colorado residents. The estimates were significantly higher in those who reported using cannabis regularly over the past 30 days; 17.9% of regular cannabis users had current mental health distress and 29.9% reported a prior diagnosis of depression.35 Taken together, these findings prompted us to examine the relationship between mental health care utilization and cannabis use in Colorado.
Our primary objective was to determine the prevalence ratios (PRs) of mental health diagnoses among ED visits with cannabis-associated diagnostic codes compared to those without cannabis-associated diagnostic codes in Colorado. Our secondary objective was to provide supportive findings in a cohort with case confirmation through medical chart review, adjudicating cannabis attribution and psychiatric diagnoses in a subpopulation of ED discharges at a large urban academic hospital.
METHODS
Study Design
This was a cross-sectional study of Colorado Hospital Association ED (CHAED) discharge data with an additional analysis of a subpopulation of discharges from the University of Colorado Hospital ED (UCHED) that included chart reviews. Additionally we completed a retrospective analysis of both populations to examine rates over time. Data were analyzed from 2012 to 2014, a period chosen to minimize bias when all CHA member hospitals were reporting their ED discharges and all data were coded consistently in International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). This study period also minimizes reporting and surveillance biases since cannabis policy liberalization occurred in 2009 allowing patients and providers to become comfortable with discussion of marijuana use patterns in the health care setting. This study protocol was approved by the Colorado Multiple Institution Review Board.
Study Setting and Population
CHAED Visits
Analysis of the statewide CHAED discharges was conducted from January 1, 2012, to December 31, 2014.36 There were 69 member hospitals of the Colorado Hospital Association at the time of this analysis. These hospitals were representative of rural, urban, academic, and private hospitals in Colorado. However, the database did not include inpatient mental health facilities, ambulatory surgical centers, long-term care facilities, military hospitals, or other outpatient treatment settings. ED visits for both Colorado residents and nonresidents were included in this analysis. The unit of analysis was defined as each incident ED visit due to the lack of unique patient identifiers to follow individual patients within the data set.
UCHED Chart Review
A sample of the larger statewide CHAED visits was selected from UCHED from January 1, 2012, through December 31, 2014. UCHED data were included in the aggregate CHAED data though these data sets were analyzed separately. The UCHED data augment the CHAED data by determination if cannabis contributed to the incident visit since ICD-9-CM diagnostic codes may also capture distant or unrelated cannabis use, potentially overestimating the association in the CHAED data set.
Study Protocol
All CHAED visits from 2012 to 2014 were simultaneously coded as 0 or 1 for presence of a cannabis-associated ICD-9-CM diagnostic code (the exposure), the presence of a mental health–related diagnostic code (the outcome) in the primary diagnosis. All CHAED visits in the data set were coded as having marijuana and/or psychiatric ICD-9-CM codes. Those with a cannabis-associated ICD-9-CM code in the CHAED data set were excluded since inclusion of this group may falsely bias results by including transient cannabis-induced intoxication symptoms, such as intoxication induced panic, rather than a true underlying psychiatric diagnosis. However, all UCHED visits were reviewed to determine presences of at least one cannabis-associated ICD-9-CM diagnostic code; the visits were then manually abstracted and simultaneously determined to be attributed to cannabis (0 or 1) and determined if there was a psychiatric diagnosis (0 or 1) associated with the visit. After ED discharges were categorized as associated with cannabis (CHAED) or attributed to cannabis (UCHED), rates of ED visits associated or attributed to cannabis were calculated for each year and examined across years 2012, 2013, and 2014 independently and in conjunction with mental health or psychiatric diagnoses.
Measurements
Cannabis Exposure
In both CHAED and UCHED, cannabis-associated ED visits were identified by the presence of at least one ICD-9-CM cannabis diagnostic code. These codes included accidental poisoning by psychodysleptics (E854.1),37 poisoning by psychodysleptics (969.6),38 nondependent cannabis abuse (codes 305.20–305.23),39 and cannabis dependence (codes 304.30–304.33).40
Verification of Cannabis Attribution
University of Colorado Hospital ED visits with cannabis-associated ICD-9-CM codes were abstracted by three trained research assistants blinded to the study hypothesis. Each visit was considered at least partially attributable to cannabis if one or more of the following criteria were met: 1) the ED physician identified cannabis as likely precipitating or contributing to the condition bringing the patient to the ED, 2) the patient was admitted to the hospital and the inpatient physician identified cannabis as likely precipitating or contributing to the condition, and/or 3) the urine toxicology screen was positive and there was a documented temporal relationship between cannabis exposure and a condition or event known to be associated with cannabis use (for example, motor vehicle collisions41–44 or acute panic attack27,28). Assessment of cannabis use is included in the drug use section of the standard nursing assessment questionnaire performed on every patient seen in the UCHED. In criteria 3, both urine toxicology screening and temporal use were necessary otherwise the visit was considered not attributable to cannabis. For abstraction training, 300 UCHED charts with cannabis-associated ICD-9-CM codes were abstracted by both a medical toxicologist and one of the research assistants. The research assistants were retrained on the discrepancies identified. Visits where cannabis attribution was questionable were arbitrated by a single medical toxicologist (AAM). The same medical toxicologist abstracted a random sample amounting to 20% of all charts reviewed by the research assistants and the kappa statistic was calculated to determine inter-rater reliability.
Identification of Mental Health Diagnoses CHAED
The Healthcare Cost and Utilization Project’s (HCUP) multiple-level Clinical Classification Software (CCS) was applied to the primary diagnoses of all CHAED visits to identify visits with primary diagnoses of mental health conditions.45 These visits were identified as a group (“mental health conditions”). This group was divided into 13 mental health diagnosis categories, such as mood disorders, anxiety disorders, schizophrenia, and other psychotic disorders (Table 1).
Table 1.
ED Visits* With Cannabis-related Codes† and Mental Health Diagnoses in Colorado 2012–2014 (N = 4,693,173).
| Mental Health Primary Diagnoses | ED Visits With Cannabis Codes,† n = 38,301 | ED Visits Without Cannabis Codes,† n = 4,654,872 | PR (95% CI) | |||
|---|---|---|---|---|---|---|
| Schizophrenia and other psychotic disorders | 1,136 | (2.96) | 15,028 | (0.32) | 9.18 | (8.66–9.75) |
| Suicide and intentional self-inflicted injury | 1,069 | (2.79) | 16,315 | (0.35) | 7.96 | (7.49–8.46) |
| Mood disorders | 2,597 | (6.78) | 42,652 | (0.92) | 7.40 | (7.12–7.69) |
| Personality disorders | 50 | (0.13) | 849 | (0.02) | 7.16 | (5.38–9.52) |
| Impulse control disorders | 16 | (0.04) | 278 | (0.006) | 6.99 | (4.23–11.58) |
| Adjustment disorders | 178 | (0.46) | 3,404 | (0.07) | 6.35 | (5.47–7.39) |
| Developmental disorders | 99 | (0.26) | 1,915 | (0.04) | 6.28 | (5.13–7.69) |
| Attention deficit, conduct, and disruptive behavior disorders | 184 | (0.48) | 3,783 | (0.08) | 5.91 | (5.10–6.85) |
| Screening and history of mental health and substance abuse codes | 114 | (0.30) | 2,924 | (0.06) | 4.74 | (3.93–5.71) |
| Anxiety disorders | 1,465 | (3.82) | 45,220 | (0.97) | 3.94 | (3.74–4.14) |
| Miscellaneous mental disorders | 109 | (0.28) | 5,199 | (0.11) | 2.55 | (2.11–3.08) |
| Disorders usually diagnosed in infancy, childhood, or adolescence | 9 | (0.02) | 613 | (0.01) | 1.78 | (0.92–3.44) |
| Delirium, dementia, and amnestic and other cognitive disorders | 54 | (0.14) | 7,888 | (0.17) | 0.83 | (0.64–1.09) |
PR = prevalence ratio.
An individual can be represented more than once in the data.
Data are reported as n (%). International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes of accidental poisoning by psychodysleptics (E854.1), poisoning by psychodysleptics (969.6), nondependent cannabis abuse (codes 305.20–305.23), and cannabis dependence (codes 304.30–304.33).
Verification of Acute Psychiatric Visits UCHED
Visits were confirmed as acute psychiatric visits through chart review and a final diagnosis of the acute incidence or exacerbation of depression, anxiety, panic attacks, psychosis, suicidal ideation, suicide attempts, bipolar, or other mood disorders.
Data Analysis
This study included all ED visits from both populations (CHAED and UCHED) where the cannabis exposure and mental health diagnoses could be classified. Within the statewide CHAED visits, crude PRs, and 95% confidence intervals (CI) were calculated for ED visits with cooccurring mental health primary diagnoses and cannabis-associated diagnostic codes compared to ED visits with mental health primary diagnoses and no cooccurring cannabis-associated diagnostic codes. Within the evaluated UCHED visits, the PR and 95% CI was examined for ED visits with psychiatric diagnosis confirmed through chart review and were attributed to cannabis compared to ED visits with psychiatric diagnosis but not attributed to cannabis. PRs are the appropriate epidemiologic summary statistic to characterize outcome in relation to exposure in this cross-sectional cohort because exposure and outcome were assessed simultaneously and they account for changing visit denominators and thus this was the primary analytic method for these longitudinal data.46 Additionally, the rates of ED visits associated or attributed to cannabis were calculated and compared to examine trends across time. Trends across years were tested using univariate logistic regression and significance was determined by the Wald chi-square test p value of <0.05. Time (years) was treated as a continuous variable. A sensitivity analysis was performed in a random 1% of UCHED visits not containing a cannabis or psychiatric ICD-9-CM code to ensure no cases were missed. The SAS version 9.4 (SAS Institute Inc.) statistical software package was used for all statistical analyses.
RESULTS
CHAED Visits
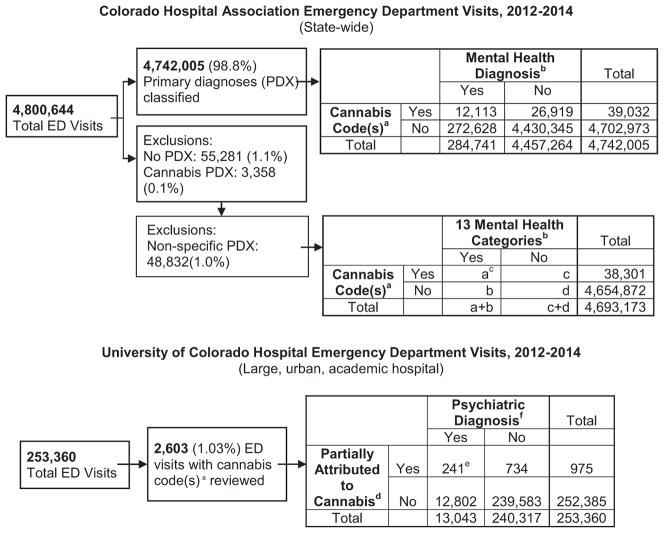
There were 4,800,644 ED visits from 2012 to 2014 and 42,390 (0.8%) of these had cannabis-associated diagnostic codes (Figure 1). Among those, 55,281 (1.1%) ED visits did not have a primary diagnosis and 3,358 (0.1%) had a cannabis-associated code in the primary diagnosis and were excluded. This left 4,742,005 (98.8%) ED visits with primary diagnosis codes and 39,032 (0.8%) with a cannabis-associated diagnostic code. When examining all mental health conditions, there were 284,741 (6.0%) ED visits having a mental health condition and 12,113 (0.2%) having a mental health condition with cooccurring cannabis diagnostic code(s) (Figure 1). When examining the 13 mental health categories, there were an additional 48,832 (1.0%) ED visits excluded from the denominator because the primary diagnosis was not specific enough for further classification; none of these codes were mental health conditions. There were 102,506 (36.0%) ED visits with primary diagnosis of alcohol-related disorders and 29,087 (10.2%) ED visit with primary diagnosis of substance-related disorders. Both of these categories were not further examined. Final analysis of the 13 mental health categories included 4,693,173 (97.8%) ED visits, and 38,301 (0.8%) had cannabis-associated diagnostic codes (Figure 1).
Figure 1.
Data extraction algorithms for statewide and urban academic hospital ED, Colorado 2012–2014. aICD-9-CM codes of accidental poisoning by psychodysleptics (E854.1), poisoning by psychodysleptics (969.6), nondependent cannabis abuse (codes 305.20–305.23), and cannabis dependence (codes 304.30–304.33). bMental health–related ICD-9-CM code in the primary diagnosis specific for schizophrenia and other psychotic disorders; suicide and intentional self-infiicted injury; mood disorders; personality disorders; impulse control disorders; adjustment disorders; developmental disorders; attention deficit, conduct, and disruptive behavior disorders; screening and history of mental health and substance abuse codes; anxiety disorders; miscellaneous mental disorders; disorders usually diagnosed in infancy, childhood, or adolescence; and delirium, dementia, and amnestic and other cognitive disorders. cSee Table 1 for numbers. dMental health–related ICD-9-CM code in the primary diagnosis, excluding substance use– and alcohol use–related codes. eCannabis involvement was determined by chart review for participating or contributing to the condition bringing the patient to the ED. fPsychiatric visits were determined by manual chart review and included acute depression, anxiety, panic attacks, psychosis, suicidal ideation, suicide attempts, bipolar and other mood disorders. ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification.
UCHED
From 2012 to 2014 there were 253,360 total ED visits at the UCHED. There were 13,043 (5.15%) visits due to psychiatric primary diagnosis over this time period and there were 2,603 (1.03%) visits with a cannabis-associated diagnostic code(s). Among those with a cannabis-associated diagnostic code, 975 (37.50%) were deemed partially attributed to cannabis by individual chart review and 241 (24.72%) were confirmed psychiatric visits (Figure 1). The sensitivity analysis did not reveal any additional cannabis associated visits or psychiatric diagnoses missed by the ICD-9-CM data extraction indicating near perfect sensitivity of the diagnoses coding. The Cohen’s kappa statistic was 0.91 (95% CI = 0.87–0.95), indicating excellent inter-rater agreement.47
Main Results
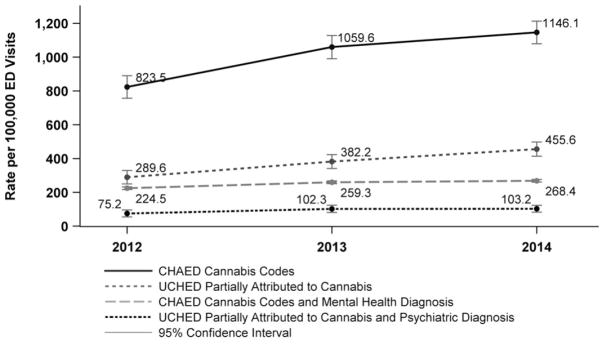
There was a fivefold greater prevalence of mental health primary diagnoses among statewide CHAED visits with cannabis-associated diagnostic codes compared to ED visits without cannabis-associated diagnostic codes (PR = 5.35, 95% CI = 5.27–5.43). Visits with mental health primary diagnoses comprised 31.0% of ED visits with cannabis-associated diagnostic codes. Other prominent categories included injuries and poisonings (12.7%), diseases of the nervous system (7.6%), diseases of the respiratory system (6.4%), and diseases of the digestive system (6.3%). Examination of the 13 mental health diagnosis categories revealed greater prevalence of 12 of the mental health diagnosis categories when cannabis-associated diagnostic codes were present compared to ED visits without cannabis-associated diagnostic codes (Table 1). The rates of statewide CHAED visits with cannabis-associated diagnostic codes significantly increased from 2012 to 2014 from 823.5 (95% CI = 756.7–890.2) to 1,146.1 per 100,000 (95% CI = 1,079.4–1,212.8, p < 0.0001). The rates of CHAED visits with both a cannabis-associated diagnostic code and a mental health primary diagnosis also significantly increased from 2012 to 2014 from 224.5 (95% CI = 216.8–232.3) to 268.4 per 100,000 (95% CI = 260.7–276.0, p < 0.0001; Figure 2).
Figure 2.
Rates of ED discharges involving cannabis per 100,000, 2012–2014. Involving cannabis was determined by ICD-9-CM codes of accidental poisoning by psychodysleptics (E854.1), poisoning by psychodysleptics (969.6), nondependent cannabis abuse (codes 305.20–305.23), and cannabis dependence (codes 304.30–304.33) in the CHAED discharges and by chart review for cannabis participating or contributing to the condition bringing the patient to the UCHED discharges. Mental health diagnosis was determined by mental health–related ICD-9-CM code in the primary diagnosis, excluding substance use– and alcohol use–related codes in CHAED discharges and psychiatric diagnosis was determined through records review in UCHED discharges. CHAED = Colorado Hospital Association ED discharges (statewide); ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification; UCHED = University of Colorado Hospital ED discharges (large, urban, academic hospital).
The UCHED data support the CHAED findings with a fourfold greater prevalence of psychiatric related ED visits in ED visits partially attributed to cannabis compared to ED visits not attributable to cannabis (PR = 4.87, 95% CI = 4.36–5.44; Table 2). The rates of UCHED visits attributed to cannabis have significantly increased from 2012 to 2014 from 289.6 (95% CI = 249.9–329.3) to 455.6 per 100,000 (95% CI = 413.34–497.8, p < 0.0001). The rates of UCHED visits attributable to cannabis in confirmed psychiatric visits increased from 2012 to 2014 from 75.2 (95% CI = 55.0–95.5) to 103.2 per 100,000 (95% CI = 83.0–123.3, p = 0.0815; Figure 2).
Table 2.
University of Colorado Hospital ED Visits, January 1, 2012, to December 31, 2014 (N = 253,360)
| Clinical Variable | Total ED visits, (N = 253,360) | ED Visits With Cannabis Codes* (n = 2,603) | ED Visits Partially Attributed to Cannabis (n = 975) | ED Visits Partially Attributed to Cannabis and Psychiatric† (n = 241) |
|---|---|---|---|---|
| Age (years), median (IQR) | 52 (26–79) | 34 (25–47) | 30 (23–40) | 28 (22–39) |
| Male sex | 107,569 (42.46) | 1,701 (65.35) | 631 (64.72) | 188 (78.01) |
| Race | ||||
| AI and AN | 1,415 (0.56) | 9 (0.35) | 1 (0.10) | 0 (0.00) |
| Asian | 6,785 (2.68) | 23 (0.88) | 13 (1.33) | 3 (1.24) |
| African American | 69,916 (27.60) | 1,002 (38.49) | 364 (37.33) | 76 (31.54) |
| NH and Other PI | 642 (0.25) | 7 (0.27) | 4 (0.41) | 1 (0.41) |
| White | 116,523 (45.99) | 1,187 (45.60) | 421 (43.18) | 120 (49.79) |
| Mixed race | 56,851 (22.39) | 369 (14.18) | 169 (17.33) | 40 (16.60) |
| Unknown | 1,228 (0.48) | 6 (0.23) | 3 (0.31) | 1 (0.41) |
| Hispanic | 55,868 (22.05) | 387 (14.87) | 177 (18.15) | 44 (18.26) |
| Disposition | ||||
| Admit/transfer | 46,167 (18.22) | 1,362 (52.32) | 221 (22.67) | 60 (24.90) |
| Discharge/ED observation/expired | 200,221 (79.03) | 1,128 (43.33) | 703 (72.10) | 180 (74.69) |
| AMA/left before visit complete | 6,972 (2.75) | 19 (0.73) | 11 (1.13) | 1 (0.41) |
Data are reported as n (%).
AI = American Indian; AMA = against medical advice; AN = Alaska native; IQR = interquartile range; NH = Native Hawaiian; PI = Pacific Islander.
International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes: accidental poisoning by psychodysleptics (E854.1), poisoning by psychodysleptics (969.6), nondependent cannabis abuse (codes 305.20–305.23), and cannabis dependence (codes 304.30–304.33).
Psychiatric visits were determined by manual chart review and included acute depression, anxiety, panic attacks, psychosis, suicidal ideation, suicide attempts, and bipolar and other mood disorders.
DISCUSSION
Colorado experienced a fivefold greater prevalence of mental health diagnoses in ED visits with cannabis-related diagnostic codes compared to ED visits without cannabis-related diagnostic codes. This finding was replicated in a subpopulation of ED visits at a large urban hospital where cannabis involvement and psychiatric diagnoses were verified. Furthermore, our findings showed state-level increases over time in the rate of ED visits with cannabis-associated diagnostic codes, which was also supported by the subpopulation analysis. We are aware that the study design and data sources generating these findings are limited. ED data are often used to identify emerging health concerns in public health at the population level.48–51 For example, ED documentation of opioid overdoses was critical is describing the national opioid epidemic.52,53 These findings describe and document patterns in mental health ED visits and cannabis coding. They are intended to be hypothesis-generating and support future studies especially in vulnerable populations such as individuals diagnosed with mental health conditions.
As more states legalize cannabis across the country it is critical that the impacts of legalization are well described so that legislatures and voters make informed decisions related to public health policy and practice. It is especially critical to describe any effects among vulnerable populations like those with mental illnesses. Increased ED psychiatric visits in states with poor psychiatric resources can result in significantly longer ED visits and poorer mental health outcomes.54 The UCHED study showed a 30% (increase from 75 to 103/100,000 visits) increase over the time period, which can have direct impact on hospital systems if they can be prevented. While this increase was not statistically significant in the UCHED data set, likely due to the smaller population, a significantly increased rate was identified in the larger, CHAED data set. This 30% increase is clinically significant given longer ED length of stay and limited psychiatric inpatient bed availability in Colorado.55,56 While not implying causation, these paired findings suggest that EDs and other health care facilities in cannabis-legalized states may experience increased numbers of mental health visits associated with cannabis use.
These findings highlight the need for prospective cohort studies that can parse out the relationship between cannabis use and mental health within a legalized environment. In 2015, an estimated 70.4% (8.1 million) of U.S. adults 18 and older with past-year substance use disorders also reported mental illness conditions.57 This high burden combined with strong associations between cannabis use and mental health disorders highlight the need to develop research cohorts, in a legalized environment, for follow-up of clinical, behavioral, social, and demographic data to determine the effect of legalized environments on mental health conditions.8–30 These studies can also distinguish the degree to which people with mental health illnesses self-medicate using cannabis. This is a necessary data element to capture given that the prevalence of mental health ED visits, among ED visits with cannabis-associated diagnostic codes, is greater than any other disease category in Colorado, and it is unclear how many patients are using cannabis to treat their disease. Colorado has preceded other states in cannabis policy liberalization with significant increases in cannabis availability. This paired with relatively poor access to mental health resources may increase this effect size in Colorado. A prospective cohort study that captures these regional variations in both cannabis policy and mental health treatment access may help delineate the contributing factors that have resulted in this rise of cannabis associated emergency mental health visits.
LIMITATIONS
These data are limited due to the retrospective nature and the inability to determine causality. There are several possibilities for the findings in this study. It is possible we are capturing increases in reporting cannabis use from patients or increases in surveillance protocols of cannabis use from health care providers due to policy liberalization. However, there is a long cannabis history in Colorado that contributed to the product becoming legalized. We saw a major increase in patient reporting and provider surveillance after medical liberalization in 2009. Thus, reporting of use in patients and increased surveillance was present for over 2 years prior to this study period. We believe that this history makes Colorado the optimal setting for reducing, though admittedly not eliminating, the surveillance and reporting bias. We acknowledge that it remains opaque whether the rates prior to legalization were lower due to decreased reporting and decreased surveillance of cannabis use because the product was illicit; however, more years of data in a legalized environment may elucidate this limitation. Unfortunately, other states, even with similar marijuana policy have combinations of varied timing between medical and recreational legalization, differences in cannabis availability and differences in mental health care access making a reasonable comparator impossible. Additional biases resulting from extending these analyses outside of the Colorado region complicate the findings further. Nevertheless, these findings show a new normal in Colorado with rates of cannabis use and mental health care ED visits at 268.4 visits per 100,000 ED visits.
It is likely that patients with mental health evaluations and diagnoses have more thorough questioning around substance abuse habits than other ED complaints. Therefore, asymmetric drug screening in mental health patients compared to the general patient population may overestimate the association in mental health-related ED visits compared to other conditions. We address these limitations in the subpopulation analysis with direct chart review that conservatively required both temporally related cannabis use confirmed with urine toxicology screening. Furthermore, patients with substance abuse disorders, a common cooccurring diagnosis with mental health disorders that may be documented below the primary diagnosis, may be directly admitted to detoxification programs and thus would not be captured in the ED discharges.58 Additionally, lower access to mental health resources in Colorado compared with other states may result in more ED visits in those with mental health conditions thus artificially inflating the association rates.
There are limitations in the ICD-9-CM coding system in identifying both cannabis use and mental health conditions within the statewide data. The use of only primary diagnoses for state mental health CHAED visits misses ED visits with mental health-related complaints documented in secondary or tertiary diagnostic codes. However, this misclassification would underestimate the amount of statewide ED visits with mental health diagnoses and cannabis-associated diagnostic codes and bias the findings toward the null hypothesis. Additionally, measuring cannabis use with cannabis ICD-9-CM coding within the statewide ED visits may be capturing regular marijuana use much like screening for tobacco use. Also, it is possible that we captured medical cannabis use that patients may be using to treat a mental health condition. Conversely, it is possible we misclassified mental health conditions as not involving cannabis use when in fact cannabis use was involved but not documented.
The statewide CHAED data provides a larger, more geographically diverse cohort of visits with a cannabis diagnostic code; however, a major limitation with a large secondary dataset is the inability to determine the role cannabis played in the visit. To mitigate these limitations, we included a subpopulation analysis of UCHED visits, a large urban hospital with medical record review for visit attribution to cannabis. The findings among the UCHED subpopulation analysis support the statewide findings. However, in the UCHED subpopulation it was possible that a visit met criteria 3 (being positive for a urine drug screen and having temporally documented cannabis use in a condition known to be association with cannabis) and, for example, a patient used medical cannabis and was involved in a motor vehicle accident but was not at fault. This may overattribute cases to cannabis exposures, although we would expect this to have a small effect. Adversely, if there was no documentation of the timing of use or if there was not urine toxicology screen, a visit that was truly attributed cannabis use would not be coded as such. This limitation would underestimate cannabis attribution. We believe that it was more likely that we underestimated cannabis attribution and our approach was conservative in minimizing the risk of overattribution within the hospital level data. Neither the statewide data nor the UCHED data are able to accurately quantify the amount of cannabis utilized and therefore we are not able to determine if there is a dose effect of this exposure by these data.
It is possible that our findings in the statewide data are overestimated due to multiple visits by the same individuals who have mental health conditions and are cannabis users. One would expect to see repeat ED visits among noncannabis users and non–mental health patients as well. It is unlikely that duplicate patients would account for all these findings, but repeat visits may be disproportionate among those with mental health conditions. Patients with mental health disorders are more likely to have multiple ED visits within a year which may be less likely in other emergency conditions, such as trauma.59 The UCHED data demonstrate that only seven individuals had two visits and two patients had three visits supporting our assertion that this was a minor contributing factor. Unfortunately, with the available statewide data ED visits cannot be matched with high probability at the patient level at this time.
It is possible that with cannabis liberalization more people are using recreational cannabis to self-medicate. This could lead to inappropriate administration and adverse health outcomes. The number of registered medical marijuana patients spiked in 2010 at 116,198 patients and has slightly declined to 113,745 patients in 2014 after recreational legalization.60 The plateau of the number of medical marijuana patients could indicate that people are using the legalized market to self-medicate without direction from a physician. However, there is incentive to become a registered medical marijuana patient because medical cannabis has a lower tax and the THC concentration in cannabis-infused products is regulated differently than recreational cannabis.1 It is unlikely that this would account for all of the observed increase in rate.
The final and most concerning possibility is that these findings are due to legalization and increased utilization of cannabis. Although there is no baseline prevalence data of mental health conditions among regular cannabis user prior to legalization, there was an increase in mental health distress among regular cannabis users in Colorado from 15.4% (95% CI = 12.1%–18.7%) in 2014 to 19.9% (95% CI = 17.0%–22.9%) in 2016 with no changes in mental health distress among the general population at this time (10.0%).35 Clearly many factors are associated with increased mental health distress and cannabis use is only one potential contributing factor. Past 30-day and regular cannabis use remains flat in the state at 13.5%. It is possible that the established users are using more or exploring new products, which could lead to increases in adverse health outcomes. Sales data are the closest proxy to the prevalence of cannabis use in Colorado. Cannabis flower, edibles, and nonedible sales have increased 126.4%, 77.6%, and 36.8% from 2014 to 2016 with the highest gross sales documented in 2016.61 Thus, sales of cannabis continue to increase but the rate of use is unchanged suggesting higher use by the same individuals. Concurrent with this, we have observed an increased rate of cannabis-associated emergency mental health visits.
It is possible that all of these limitations, added together, account for these measured increases and there is no true increase in cannabis attributed emergency mental health disease. However, we believe that these data suggest an increase in cannabis-attributed mental health visits with the acknowledged limitations taken into account. It is unclear what the true increase in this rate is due to these limitations. The current study is only generalizable to EDs in Colorado but are more representative of the Denver-metro area in Colorado, which has one of the highest prevalence of cannabis users (16.8%) and highest number of hospitals reporting to the CHA.62 These findings may be validated with research conducted at the patient level or a prospective cohort study. Additionally, the ICD-10-CM coding system allows for diagnostic coding of cannabis intoxication, use, abuse, dependence, and poisonings. More work should be done to identify the reasons for these increases. If these observations do represent an increase of disease due to increased cannabis use, then cannabis legalization may burden an already vulnerable mental health population.
CONCLUSIONS
In summary, in Colorado, the prevalence of mental health conditions in ED visits with cannabis use diagnostic codes is higher than in ED visits without cannabis use diagnostic codes. Further research should focus on determining if these findings are truly attributed to cannabis or merely coincident with concurrent increased use and availability. Examination in other regions with variable cannabis policy, varied cannabis availability, and variable access to mental health treatment may allow for more precise quantification of each factors’ contribution to these observations.
Acknowledgments
AAM received support from NIH K23 GM110516, NIH CTSI UL1 TR001082, and CDPHE 17 FHHA 96950. The contents of this work are the sole responsibility of the authors and do not necessarily represents the views of the National Institutes of Health (NIH).
Footnotes
The authors have no potential conflicts to disclose.
References
- 1.CO Const. amend. 64 art. XVIII §16.
- 2.Wenzel J. Weed Goes Wide: The Subtle Mainstreaming of Cannabis in Colorado [Internet] Denver Post; 2015. [Accessed May 20, 2017]. Available from: http://www.denverpost.com/2015/12/28/weed-goes-wide-the-subtle-mainstreaming-of-cannabis-in-colorado/ [Google Scholar]
- 3.Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA. Marijuana tourism and emergency department visits in Colorado. N Engl J Med. 2016;37:797–8. doi: 10.1056/NEJMc1515009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell C, Slim J, Flaten HK, Lindberg G, Arek W, Monte AA. Butane hash oil burns associated with marijuana liberalization in Colorado. J Med Toxicol. 2015;11:422–5. doi: 10.1007/s13181-015-0501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim HS, Anderson JD, Saghafi O, Heard KJ, Monte AA. Cyclic vomiting presentations following marijuana liberalization in Colorado. Acad Emerg Med. 2015;22:694–9. doi: 10.1111/acem.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim HS, Monte AA. Colorado cannabis legalization and its effect on emergency care. Ann Emerg Med. 2016;68:71–5. doi: 10.1016/j.annemergmed.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M. Marijuana and acute health care contacts in Colorado. Prev Med. 2017;104:24–30. doi: 10.1016/j.ypmed.2017.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ. 2002;325:1212–3. doi: 10.1136/bmj.325.7374.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. Am J Psychiatry. 2001;158:2033–7. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- 10.Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry. 2002;59:1039–44. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- 11.Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ. 2005;330:11. doi: 10.1136/bmj.38267.664086.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Os J, Bak M, Hanssen M, Bijl RV, de Graaf R, Verdoux H. Cannabis use and psychosis: a longitudinal population-based study. Am J Epidemiol. 2002;156:319–27. doi: 10.1093/aje/kwf043. [DOI] [PubMed] [Google Scholar]
- 13.Kedzior KK, Laeber LT. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population- a meta-analysis of 31 studies. BMC Psychiatry. 2014;14:136. doi: 10.1186/1471-244X-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lev-Ran S, Le Foll B, McKenzie K, George TP, Rehm J. Bipolar disorder and co-occurring cannabis use disorders: characteristics, co-morbidities and clinical correlates. Psychiatry Res. 2013;209:459–65. doi: 10.1016/j.psychres.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Feingold D, Weiser M, Rehm J, Lev-Ran S. The association between cannabis use and anxiety disorders: results from a population-based representative sample. Eur Neuropsychopharmacol. 2016;26:493–505. doi: 10.1016/j.euroneuro.2015.12.037. [DOI] [PubMed] [Google Scholar]
- 16.Shalit N, Shoval G, Shlosberg D, Feingold D, Lev-Ran S. The association between cannabis use and suicidality among men and women: a population-based longitudinal study. J Affect Disord. 2016;205:216–24. doi: 10.1016/j.jad.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Andréasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet. 1987;2:1483–6. doi: 10.1016/s0140-6736(87)92620-1. [DOI] [PubMed] [Google Scholar]
- 18.Zammit S, Allebeck P, Andreasson S, Lundberg I, Lewis G. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ. 2002;325:1199. doi: 10.1136/bmj.325.7374.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Allebeck P. Cannabis use and depression: a longitudinal study of a national cohort of Swedish conscripts. BMC Psychiatry. 2012;12:112. doi: 10.1186/1471-244X-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Andreasson S, Allebeck P. Cannabis, schizophrenia and other non-affective psychoses: 35 years of follow-up of a population-based cohort. Psychol Med. 2012;42:1321–8. doi: 10.1017/S0033291711002078. [DOI] [PubMed] [Google Scholar]
- 21.Hickman M, Vickerman P, MacLeod J, Kirkbride J, Jones PB. Cannabis and schizophrenia: model projections of the impact of the rise in cannabis use on historical and future trends in schizophrenia in England and Wales. Addiction. 2007;102:597–606. doi: 10.1111/j.1360-0443.2006.01710.x. [DOI] [PubMed] [Google Scholar]
- 22.Veen ND, Selten JP, van der Tweel I, Feller WG, Hoek HW, Kahn RS. Cannabis use and age at onset of schizophrenia. Am J Psychiatry. 2004;161:501–6. doi: 10.1176/appi.ajp.161.3.501. [DOI] [PubMed] [Google Scholar]
- 23.Di Forti M, Sallis H, Allegri F, et al. Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull. 2014;40:1509–17. doi: 10.1093/schbul/sbt181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tosato S, Lasalvia A, Bonetto C, et al. The impact of cannabis use on age of onset and clinical characteristics in first-episode psychotic patients. Data from the Psychosis Incident Cohort Outcome Study (PICOS) J Psychiatr Res. 2013;47:438–44. doi: 10.1016/j.jpsychires.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Di Forti M, Marconi A, Carra E, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2:233–8. doi: 10.1016/S2215-0366(14)00117-5. [DOI] [PubMed] [Google Scholar]
- 26.Di Forti M, Morgan C, Dazzan P, et al. High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009;195:488–91. doi: 10.1192/bjp.bp.109.064220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dannon PN, Lowengrub K, Amiaz R, Grunhaus L, Kotler M. Comorbid cannabis use and panic disorder: short term and long term follow-up study. Hum Psychopharmacol. 2004;19:97–101. doi: 10.1002/hup.560. [DOI] [PubMed] [Google Scholar]
- 28.Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Lifetime associations between cannabis, use, abuse, and dependence and panic attacks in a representative sample. J Psychiatr Res. 2006;40:477–86. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Tournier M, Sorbara F, Gindre C, Swendsen JD, Verdoux H. Cannabis use and anxiety in daily life: a naturalistic investigation in a non-clinical population. Psychiatry Res. 2003;118:1–8. doi: 10.1016/s0165-1781(03)00052-0. [DOI] [PubMed] [Google Scholar]
- 30.Ilan AB, Gevins A, Coleman M, ElSohly MA, de Wit H. Neurophysiological and subjective profile of marijuana with varying concentrations of cannabinoids. Behav Pharmacol. 2005;16:487–96. doi: 10.1097/00008877-200509000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Vigil DI, Hall KE, Contreras E, et al. Monitoring Changes in Marijuana Use Patterns: Chapter 1. Behavioral Risk Factor Surveillance System (BRFSS) 2014–2015 Survey Results [Internet] Denver: 2017. [Accessed May 20, 2017]. Available from: https://drive.google.com/file/d/0B0tmPQ67k3NVR2ZNZWtPYk9IN0k/view. [Google Scholar]
- 32.Davis JM, Mendelson B, Berkes JJ, Suleta K, Corsi KF, Booth RE. Public health effects of medical marijuana legalization in Colorado. Am J Prev Med. 2016;50:373–9. doi: 10.1016/j.amepre.2015.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Monte AA, Zane RD, Heard KJ. The implications of marijuana legalizaiton in Colorado. JAMA. 2015;313:241–2. doi: 10.1001/jama.2014.17057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–27. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colorado Health and Environmental Data (CHED) [Accessed Sep 19, 2015];Behavioral Risk Factors Surveillance System. Available from: http://www.chd.dphe.state.co.us/topics.aspx?q=Adult_Health_Data.
- 36.CHA Databank. [Accessed Sep 9, 2016];2015 Available from: http://www.cha.com/Member-Services/CHA-DATABANK.aspx.
- 37.International Classification of Diseases 9th Revision Clinical Modification. Los Angeles: Practice Management Information Corporation [PMIC]; 2015. p. 827. [Google Scholar]
- 38.International Classification of Diseases 9th Revision Clinical Modification. Los Angeles: Practice Management Information Corporation [PMIC]; 2015. p. 725. [Google Scholar]
- 39.International Classification of Diseases 9th Revision Clinical Modification. Los Angeles: Practice Management Information Corporation [PMIC]; 2015. p. 314. [Google Scholar]
- 40.International Classification of Diseases 9th Revision Clinical Modification. Los Angeles: Practice Management Information Corporation [PMIC]; 2015. pp. 313–4. [Google Scholar]
- 41.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59:478–92. doi: 10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lowenstein SR, Koziol-McLain J. Drugs and traffic crash responsibility: a study of injured motorists in Colorado. J Trauma. 2001;50:313–20. doi: 10.1097/00005373-200102000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised. Addiction. 2016;111:1348–59. doi: 10.1111/add.13347. [DOI] [PubMed] [Google Scholar]
- 45.HCUP CCS. Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Accessed May 20, 2017]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 46.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 47.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Int Biometric Soc. 1977;33:159–74. [PubMed] [Google Scholar]
- 48.Consensus Recommendations for National and State Poisoning Surveillance: Report from the Injury Surveillance Workgroup (ISW7) Atlanta: Safe States; 2012. [Accessed May 20, 2017]. Available from: http://c.ymcdn.com/sites/www.safestates.org/resource/resmgr/imported/ISW7. [Google Scholar]
- 49.Xiang Y, Zhao W, Xiang H, Smith GA. ED visits for drug-related poisoning in the United States, 2007. Am J Emerg Med. 2012;2012:293–301. doi: 10.1016/j.ajem.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 50.Slavova S, Bunn TL, Talbert J. Drug overdose surveillance using hospital discharge data. Public Health Rep. 2014;129:437–45. doi: 10.1177/003335491412900507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chretien JP, Tomich NE, Gaydos JC, Kelley PW. Real-time public health surveillance for emergency preparedness. Am J Public Health. 2009;99:1360–3. doi: 10.2105/AJPH.2008.133926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reardon JM, Harmon KJ, Schult GC, Staton CA, Waller AE. Use of diagnosis codes for detection of clinically significant opioid poisoning in the emergency department: a retrospective analysis of a surveillance case definition. BMC Emerg Med. 2016;16:11. doi: 10.1186/s12873-016-0075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L. HCUP Statistical Brief #219. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [Accessed Dec 28, 2017]. Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009–2014. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.pdf. [Google Scholar]
- 54.Pearlmutter MD, Dwyer KH, Burke LG, Rathlev N, Maranda L, Volturo G. Analysis of emergency department length of stay for mental health patients at ten Massachusetts emergency departments. Ann Emerg Med. 2017;70(193–202):e16. doi: 10.1016/j.annemergmed.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 55.Blumstein H, Singleton AH, Suttenfield CW, Hiestand BC. Weekday psychiatry faculty rounds on emergency department psychiatric patients reduces length of stay. Acad Emerg Med. 2013;20:498–502. doi: 10.1111/acem.12131. [DOI] [PubMed] [Google Scholar]
- 56.Zhu JM, Singhal A, Hsia RY. Emergency department length-of-stay for psychiatric visits was significantly longer than for nonpsychiatric visits, 2002–11. Health Aff (Millwood) 2016;35:1698–706. doi: 10.1377/hlthaff.2016.0344. [DOI] [PubMed] [Google Scholar]
- 57.Center for Behavioral Health Statistics and Quality. [Accessed May 20, 2017];Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51) 2016 Available from: http://www.samhsa.gov/data/
- 58.Mark T, Vandivort-Warren R, Stocks C, et al. Treatment for Substance Use Disorders in Community Hospitals. 2010 Available from: http://www.hcup-us.ahrq.gov/reports.jspJan 27, 2017.
- 59.Coffey R, Houchens R, Chu B, et al. [Accessed Dec 21, 2016];Emergency Department Use for Mental and Substance Use Disorders. 2010 Available from: http://www.hcup-us.ahrq.gov/reports.jsp.
- 60.Colorado Department of Public Health and Environment. [Accessed Dec 28, 2017];Medical Marijuana Registry. Available from: https://www.colorado.gov/pacific/cdphe/medicalmarijuana.
- 61.Brohl B, Humphreys H, Kammerzell R, Burack J. [Accessed Aug 2, 2017];Marijuana Enforcement Division 2016 Annual Report. 2017 Available from: https://www.colorado.gov/pacific/sites/default/files/2016 MED Annual Report_Final.pdf.
- 62.Hall KE, Vigil DI, Contreras E, Van Dyke M. [Accessed Sep 15, 2017];Monitoring Trends in Adult Marijuana Use. 2017 Available from: https://www.colorado.gov/pacific/cdphe/adult-marijuana-use-trends.