Abstract
Objective
To analyze the changes in the pharmacotherapy and glycemic control trends in elderly patients with type 2 diabetes mellitus (T2DM) in Japan.
Methods
We extracted the data of 7,590 patients (5,396 men and 2,194 women; median year of birth: 1945) with T2DM registered in the National Center Diabetes Database for the years 2005 to 2013, and conducted age-stratified (<65, 65-74, and ≥75 years of age) analyses.
Results
The hemoglobin A1c (HbA1c) levels declined from 2005 to 2013, and for those who received antihyperglycemic drug prescription, the HbA1c levels were lower in the older age group than in the younger age group. In the ≥75 age group, dipeptidyl peptidase-4 inhibitors (DPP4i) became the most frequently prescribed drug (49.1%) in 2013, and sulfonylureas remained the second-most frequently prescribed drug (37.8%) with decreased prescribed doses. The prescription ratio of oral drugs associated with a risk of hypoglycemia was higher in patients ≥75 years of age than in those <75 years of age (40.5% and 26.4%, respectively in 2013), although it showed a downward trend. The prescription rates of insulin for patients ≥75 years of age increased during the study period.
Conclusion
The pharmacotherapy trends for elderly patients with T2DM changed dramatically in Japan with the launch of DPP4i in 2009. Glycemic control in a considerable portion of the ≥75 age group in Japan was maintained at the expense of potential hypoglycemia by the frequent, although cautious, use of sulfonylureas, glinides and insulin.
Keywords: antidiabetic drugs, elderly, type 2 diabetes
Introduction
Diabetes mellitus is associated with an increased risk of cardiovascular diseases, cancer and dementia, all of which can cause significant impairment of the quality of life of the patients and a significant increase in the financial burden of health care systems (1).
The proportion of people strongly suspected of having diabetes has not increased since 2006 in Japan [Ministry of Health, Labour and Welfare of Japan. Status of diabetes. In: Outline of Results from 2015 National Health and Nutrition Survey, 2015. (In Japanese); URL http://www.mhlw.go.jp/file/04-Houdouhappyou-10904750-Kenkoukyoku-Gantaisakukenkouzoushinka/kekkagaiyou.pdf]. However, the number of elderly patients with diabetes mellitus is on the rise due to the improved prognosis of patients with diabetes mellitus (2) and increase in population of the elderly in Japan. With regard to the targets for glycemic control in elderly patients with diabetes mellitus, the “Japan Diabetes Society (JDS)/Japan Geriatrics Society (JGS) Joint Committee on Improving Care for Elderly Patients with Diabetes” issued a statement entitled, “Glycemic control in elderly patients with diabetes mellitus,” in 2016 (3).
Two relatively recent events brought about significant changes in the trends of the use of antidiabetic drugs in Japan; one was the introduction of dipeptidyl peptidase-4 inhibitors (DPP4is) to the Japanese market in 2009, and the other was the increase in the daily permissible prescription dose of metformin from 750 to 2,250 mg in 2010.
We previously established the National Center Diabetes Database with financial support from the National Center for Global Health and Medicine and the Ministry of Health, Labour and Welfare of Japan to examine the current status of diabetes management and to keep track of diabetic patients in Japan (4). For this study, we extracted the antidiabetic drug prescription and hemoglobin A1c (HbA1c) data from 2005 to 2013 for patients with type 2 diabetes mellitus registered in the database and conducted age-stratified analyses of the data.
In the present study, we evaluated the situation of elderly diabetic patients in Japan before the issuance of the “Glycemic control in elderly patients with diabetes mellitus” statement in 2016 (3).
Materials and Methods
Population included in the analysis
The structure of the National Center Diabetes Database has been described in detail previously (4). This database contains the medical records of 8,647 diabetic patients receiving outpatient treatment at 8 medical institutions in Japan. The criteria proposed by the Japan Diabetes Society (5-7), which are almost identical to the criteria of the World Health Organization [World Health Organization (eds). Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Report of a WHO/IDF consultation 2006; URL http://whqlibdoc.who.int/publications/2006/9241594934_eng.pdf], were used for the diagnosis of diabetes. From the National Center Diabetes Database, we selected the data of 7,590 outpatients ≥20 years of age who had been diagnosed with type 2 diabetes mellitus. This research was conducted in conformity with the “Ethical Guidelines for Medical and Health Research involving Human Subjects” issued by the Ministry of Health, Labour and Welfare of Japan, and with the approval of the National Center for Global Health and Medicine Research Ethics Committee.
Statistical analysis
From the database, we extracted the following information about each patient: year and month of birth, sex, height, body weight, HbA1c level, and the names and doses of drugs prescribed to reduce the blood glucose levels. The patients' ages were determined based on the dates of the prescriptions. Weight (in kilograms) was divided by the square of height (in meters) to calculate the body mass index (BMI), and the values were rounded to three significant digits. For patients for whom multiple data points were available in a single year, the final data for the year were considered.
The antidiabetic drugs prescribed were categorized by their mechanism of action. The treatment strategies adopted were classified into three categories: “not prescribed any antidiabetic drugs,” (category A) “prescribed antidiabetic drugs other than insulin” (category B) and “prescribed insulin” (category C). Treatment category B was further subdivided into categories B-1 [“prescribed antidiabetic drugs other than those potentially associated with severe hypoglycemia-namely sulfonylureas and glinides (3)”] and B-2 (“prescribed sulfonylureas or glinides”). The subjects were also categorized into 3 age groups: <65, 65-74 and ≥75 years of age, for each year of data acquisition, in accordance with the statement, “Glycemic control in elderly patients with diabetes mellitus,” issued by the “JDS/JGS Joint Committee on Improving Care for Elderly Patients with Diabetes” (3).
The daily dose of sulfonylureas was categorized into two groups: the “lower-dose sulfonylurea therapy” (any dose of tolbutamide, ≤2 mg of glimepiride, ≤40 mg of gliclazide or ≤1.25 mg of glibenclamide), recommended for use with DPP4is by “the Committee for Proper use of Incretin-based Therapy” [https://www.nittokyo.or.jp/modules/information/index.php?content_id=19 (in Japanese)] and “higher-dose sulfonylurea therapy” (sulfonylurea doses higher than those categorized in the “lower-dose sulfonylurea therapy” group). According to a post hoc analysis of the Veterans Affairs Diabetes Trial (VDAT), intensive blood glucose-lowering therapy was associated with a reduced risk of death in patients with diabetes of <15 years' duration, but with an increased risk of death in patients with diabetes of ≥20 years' duration (8); therefore, we conducted a sub-analysis in patients ≥75 years of age (as of 2013) divided into the following three groups: patients diagnosed with diabetes for <15 years, 15-20 years or ≥20 years.
The data analyses were performed using R, version 3.2.1 (R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2015; URL http://www.R-project.org/). Continuous variables were expressed as the means ± standard deviations or medians with the 25th-75th percentiles, and differences in these values were examined by Student's t-test and Wilcoxon's signed-rank test, respectively. Differences in the frequencies among the three age groups and the long-term trends in the annual frequencies were examined by a chi-squared test for trends in proportions. Differences in the values among the three age groups and long-term trends of annual summary statistics were examined using a Jonckheere-Terpstra test for trends. p values of less than 0.05 were considered to indicate statistical significance.
Results
Characteristics of the patients included in the analyses
The number of patients analyzed and their characteristics are shown in Table 1. During the study period, the BMI increased (p for trend <0.001), the HbA1c value decreased (p for trend <0.001), the duration of diabetes from the diagnosis increased (p for trend <0.001), and the proportion of older patients increased (p for trend <0.001). In 2013, the percentages of patients who were 65-74 and those who were ≥75 years of age were 56.8% and 24.8%, respectively.
Table 1.
Baseline Characteristics of the Patients.
| Year | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Total number of patients | 3,599 | 4,375 | 4,907 | 5,505 | 6,079 | 6,042 | 5,835 | 5,426 | 5,065 |
| Men | 2,452 | 3,015 | 3,411 | 3,871 | 4,286 | 4,276 | 4,126 | 3,854 | 3,622 |
| Women | 1,147 | 1,360 | 1,496 | 1,634 | 1,793 | 1,766 | 1,709 | 1,572 | 1,443 |
| <65 years | 1,984 | 2,400 | 2,650 | 2,943 | 3,150 | 3,041 | 2,857 | 2,507 | 2,188 |
| 65-74 years | 1,140 | 1,330 | 1,452 | 1,588 | 1,758 | 1,758 | 1,713 | 1,666 | 1,619 |
| ≥ 75 years | 475 | 645 | 805 | 974 | 1,171 | 1,243 | 1,265 | 1,253 | 1,258 |
| Years after diagnosis of diabetes* | 9(4-16) | 8(4-16) | 9(4-16) | 9(4-16) | 9(4-16) | 10(4-17) | 10(5-17) | 11(6-18) | 12(7-19) |
| BMI (kg/m2)** (number of patients) |
24.2±4.0 (2,581) |
24.3±3.9 (3,179) |
24.3±4.0 (3,613) |
24.5±4.1 (4,177) |
24.6±4.3 (4,840) |
24.8±4.4 (4,636) |
24.8±4.4 (4,769) |
24.7±4.3 (4,738) |
24.7±4.3 (4,201) |
| HbA1c (%)* (number of patients) |
7.6(6.9-8.4) (3,524) |
7.4(6.8-8.3) (4,265) |
7.2(6.7-8.0) (4,782) |
7.1(6.6-7.9) (5,359) |
7.1(6.5-7.8) (5,960) |
7.1(6.6-7.8) (5,875) |
7.1(6.6-7.8) (5,680) |
7.0(6.5-7.6) (5,225) |
6.9(6.5-7.5) (4,927) |
* median with the 25-75th percentiles, ** means±standard deviations
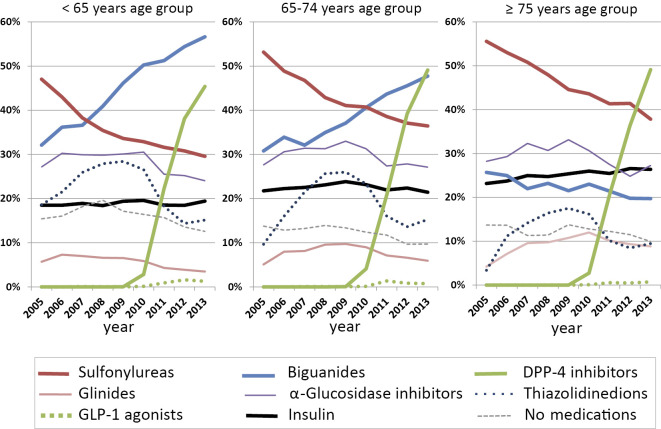
Changes in cumulative total antidiabetic drug prescription trends in elderly patients
The cumulative total antidiabetic drug prescription rates during the defined period are shown, stratified by the age group, in Fig. 1. In 2013, DPP4i was the most frequently prescribed drug in the 65-74 and ≥75 age groups (49.1% and 49.1%, respectively) and the second-most frequently prescribed drug in the <65 age group (45.4%). Although the frequency of prescription of sulfonylureas steadily decreased from 2005 to 2013 in all age groups (p for trend <0.001), sulfonylureas remained the second-most frequently prescribed drug in the ≥75 age group in 2013 (37.8%). The proportion of patients prescribed biguanides in the ≥75 age group decreased from 2005 (25.7%) to 2013 (19.7%, p for trend <0.001), in contrast to the increase in the prescription rates of biguanides in the <65 age group and 65-74 age group from 2005 (32.1% and 30.8%, respectively) to 2013 (56.6%, p for trend <0.001 and 47.7%, p for trend <0.001, respectively). Biguanides were used less frequently in older age groups than in younger age groups throughout the observation period (p for trend with age group, <0.001). The proportions of patients prescribed glinides, thiazolidinediones or alpha-glucosidase inhibitors peaked around 2009, the year in which DPP4i was launched in Japan, and decreased gradually thereafter. In 2013, the prescription frequency of glinides and alpha-glucosidase inhibitors was higher (p for trend with age group in 2013, <0.001 and <0.023, respectively), while that of the thiazolidinediones was lower (p for trend with age group in 2013, <0.001) in the older age group than in the younger age group.
Figure 1.
Cumulative total antidiabetic drug prescription rates stratified by age group from 2005-2013.
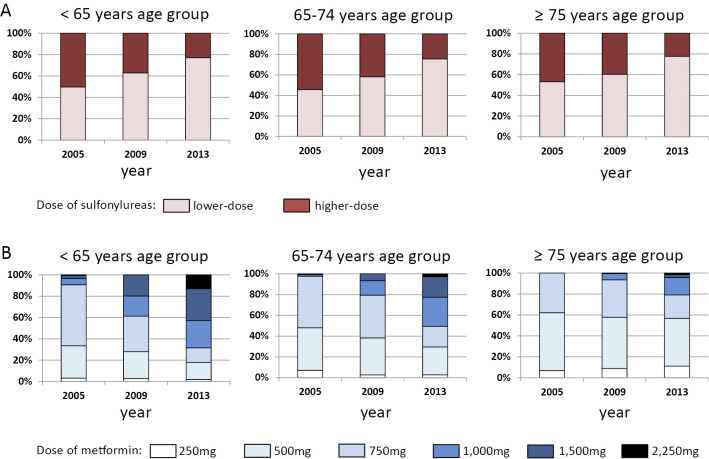
Changes in the dosages of sulfonylureas and metformin in elderly patients
We next examined the changes in the dosages of the sulfonylureas and metformin over time in the study participants (Fig. 2). Compared to that in 2005, the prescription rate of lower-dose sulfonylurea therapy was higher in all age groups in 2013 (Fig. 2A, p <0.001), and there were no significant differences in the prescription rates of lower-dose sulfonylurea therapy among the three age groups (Fig. 2A, p for trend with age group in 2013, 0.84).
Figure 2.
Changes in the dosages of sulfonylureas and metformin. A: Prescription rates of lower-dose sulfonylurea therapy, stratified by age group in 2005, 2009 and 2013. For the present analysis, “lower-dose sulfonylurea therapy” was defined as follows: any dose of tolbutamide, ≤2 mg of glimepiride, ≤40 mg of gliclazide or ≤1.25 mg of glibenclamide. B: Dosage of metformin in the subjects stratified by age group in 2005, 2009 and 2013.
Compared to that in 2005, the prescription rate of metformin at more than 750 mg/day was higher in all age groups in 2013 (Fig. 2B, p <0.001). However, there were significant differences in the prescription rates of metformin at more than 750 mg/day among the three age groups in 2013: namely, in the ≥75 age group, the rate was 20.9%, whereas in the 65-74 and <65 age groups, the rates were 50.5% and 68.4%, respectively (Fig. 2B, p for trend with age group in 2013, 0.001).
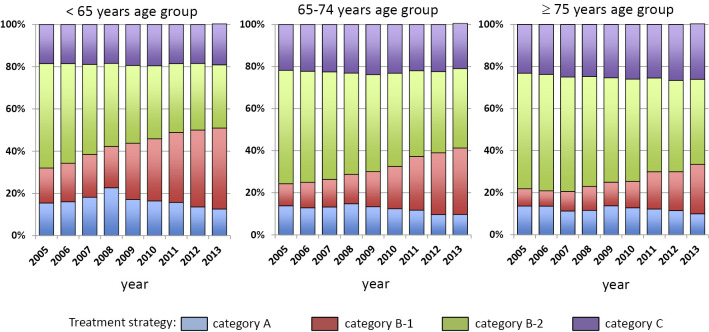
Changing trends in the treatment strategies adopted for hyperglycemia in elderly patients
We next performed an age-stratified analysis of the treatment strategy adopted for hyperglycemia during the defined study period. As shown in Fig. 3, the proportion of patients in treatment category A was smaller in the older age group than in the younger age group in 2013 (p for trend with age group in 2013, <0.009). The proportion of patients in treatment category B-1 increased during the defined study period, but to a lesser degree in the older age group than in the younger age group (p for trend with age group in 2013, <0.001). The proportion of patients in treatment category B-2 decreased during the defined study period, with the proportion of patients in this treatment category being larger in the older age group than in the younger age group in 2013 (p for trend with age group in 2013, <0.001). In 2013, 40.5% of those in the ≥75 age group were treated under the strategy of this category. Insulin was used more frequently in the older age group than in the younger age group (p for trend with age group in 2013, <0.001). The frequency of using insulin in the ≥75 age group showed a gradual annual increase from 2005 (23.2%) to 2013 (27.3%, p for trend <0.05), while no trend was apparent in the frequency of using insulin in the <65 and 65-74 age groups (p for trend <0.50 and <0.71, respectively). In 2013, the prescription rate of insulin in the ≥75 age group was 26.4%.
Figure 3.
Treatment strategy for hyperglycemia stratified by age group from 2005-2013. Category A: not prescribed any antidiabetic drugs, category B-1: prescribed antidiabetic drugs other than those potentially associated with severe hypoglycemia, category B-2: prescribed sulfonylureas or glinides, category C: prescribed insulin
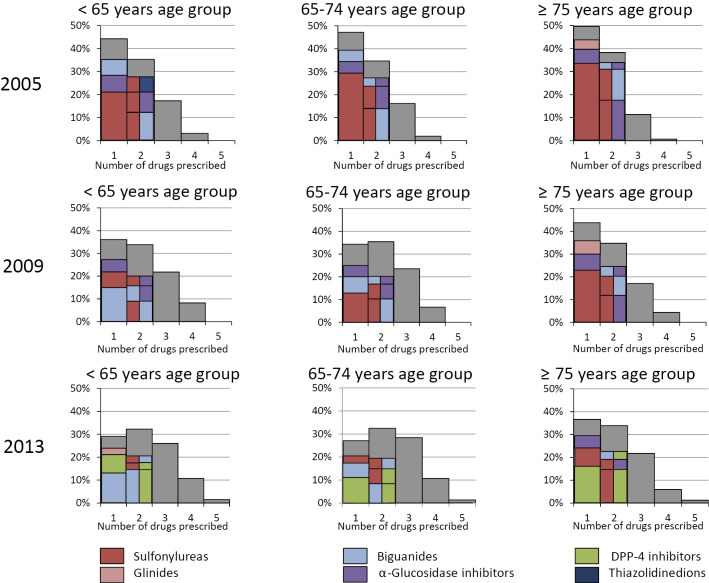
Number of antidiabetic drugs prescribed and the choice of drug class in elderly patients
As shown in Fig. 4, the number of antidiabetic drugs prescribed to the category B patients (patients receiving antidiabetic drugs other than insulin) showed a gradual increase from 2005 to 2013 (p for trend <0.001), and this trend was less often observed in the older age group than in the younger age group in 2013 (Fig. 4, p for trend with age group in 2013, <0.001). When we examined the choice of drug class in the category B patients, DPP4i emerged as the most frequently prescribed drug for monotherapy in 2013 in the 65-74 and ≥75 age groups, in contrast to the trend observed in 2005, when sulfonylureas were the most frequently prescribed drugs for monotherapy in all three age groups. The most common two-drug combination in 2005 was sulfonylureas plus α-glucosidase inhibitor in the ≥75 age group and sulfonylureas plus biguanides in the two <75 age groups, changing to sulfonylureas plus DPP4i in the ≥75 age group and biguanides plus DPP4i in the two <75 age groups in 2013.
Figure 4.
Number of drugs prescribed for glycemic control in patients receiving antidiabetic drugs other than insulin, stratified by age group in 2005, 2009 and 2013. Drug classes ranked first, second and third used as monotherapy or in two-drug combinations are also presented as insets (for two-drug combinations, the two drug classes are displayed side by side). Drug classes ranked from fourth and lower are indicated in gray.
Glycemic control
As shown in Table 2 and Table 3, the median HbA1c level was the highest and the proportion of patients with HbA1c values of less than 7.0% or 8.0% was the lowest in treatment category C, followed, in order, by treatment categories B-2, B-1 and A. The median HbA1c levels showed a declining trend, and the proportion of patients with HbA1c values <8.0% showed an inclining trend from 2005 to 2013 in all three age groups, irrespective of the treatment strategy used. No significant trend from 2005 to 2013 was observed with regard to the proportion of patients ≥75 years of age with HbA1c values <7.0% in treatment category C (Table 3).
Table 2.
The Median (25-75th Percentile) of HbA1c Levels (%).
| Years | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | p for trend |
|---|---|---|---|---|---|---|---|---|---|---|
| Age group | ||||||||||
| <65 | ||||||||||
| All category | 7.7(7.0-8.6) | 7.5(6.8-8.4) | 7.2(6.7-8.0) | 7.2(6.6-7.9) | 7.1(6.5-7.9) | 7.2(6.6-7.8) | 7.1(6.6-7.8) | 7.0(6.5-7.6) | 7.0(6.5-7.7) | <0.001 |
| Category A | 6.8(6.4-7.4) | 6.8(6.4-7.4) | 6.7(6.3-7.3) | 6.7(6.3-7.1) | 6.6(6.2-7.0) | 6.7(6.3-7.1) | 6.6(6.2-7.0) | 6.5(6.0-6.8) | 6.4(6.1-6.8) | <0.001 |
| Category B-1 | 7.4(6.9-8.4) | 7.2(6.7-8.0) | 7.0(6.5-7.7) | 7.0(6.6-7.7) | 6.9(6.5-7.5) | 7.0(6.6-7.5) | 7.0(6.5-7.5) | 6.8(6.5-7.4) | 6.8(6.4-7.4) | <0.001 |
| Category B-2 | 7.8(7.2-8.5) | 7.6(7.0-8.4) | 7.4(6.8-8.2) | 7.3(6.8-8.1) | 7.3(6.7-8.1) | 7.4(6.8-8.0) | 7.4(6.8-8.0) | 7.2(6.7-7.9) | 7.2(6.7-7.9) | <0.001 |
| Category C | 8.3(7.4-9.5) | 8.2(7.6-9.6) | 7.9(7.0-9.0) | 7.7(6.9-8.8) | 7.7(6.9-8.7) | 7.7(7.0-8.6) | 7.7(7.0-8.8) | 7.5(6.8-8.6) | 7.6(6.9-8.6) | <0.001 |
| 65-75 | ||||||||||
| All category | 7.5(6.9-8.3) | 7.4(6.8-8.1) | 7.2(6.7-7.9) | 7.1(6.6-7.9) | 7.1(6.6-7.7) | 7.1(6.7-7.7) | 7.1(6.7-7.7) | 7.0(6.5-7.5) | 6.9(6.5-7.5) | <0.001 |
| Category A | 6.9(6.4-7.4) | 6.9(6.4-7.3) | 6.8(6.3-7.1) | 6.8(6.4-7.2) | 6.7(6.3-7.1) | 6.7(6.3-7.1) | 6.7(6.3-7.1) | 6.3(6.0-6.7) | 6.4(6.1-6.8) | <0.001 |
| Category B-1 | 7.1(6.6-7.6) | 7.1(6.5-7.5) | 6.9(6.5-7.5) | 6.8(6.4-7.3) | 6.8(6.4-7.3) | 6.9(6.5-7.3) | 6.9(6.5-7.4) | 6.8(6.4-7.1) | 6.7(6.4-7.1) | <0.001 |
| Category B-2 | 7.6(7.0-8.2) | 7.5(6.9-8.2) | 7.3(6.8-8.0) | 7.2(6.7-7.9) | 7.2(6.7-7.7) | 7.2(6.8-7.8) | 7.3(6.8-7.8) | 7.1(6.7-7.6) | 7.0(6.6-7.5) | <0.001 |
| Category C | 8.0(7.3-8.9) | 7.9(7.0-8.5) | 7.6(7.0-8.5) | 7.6(6.9-8.5) | 7.4(6.8-8.3) | 7.6(6.9-8.1) | 7.6(6.9-8.2) | 7.4(6.8-8.1) | 7.3(6.8-7.9) | <0.001 |
| ≥ 75 | ||||||||||
| All category | 7.4(6.9-8.3) | 7.3(6.7-8.1) | 7.2(6.6-7.9) | 7.1(6.5-7.8) | 7.0(6.5-7.6) | 7.1(6.6-7.6) | 7.1(6.6-7.7) | 7.0(6.5-7.7) | 6.9(6.5-7.5) | <0.001 |
| Category A | 6.9(6.5-7.5) | 6.7(6.4-7.3) | 6.8(6.3-7.1) | 6.7(6.3-7.3) | 6.8(6.4-7.1) | 6.7(6.3-7.1) | 6.7(6.3-7.1) | 6.6(6.2-7.0) | 6.4(6.1-6.8) | <0.001 |
| Category B-1 | 6.9(6.5-7.5) | 7.0(6.6-8.4) | 6.8(6.4-7.4) | 6.8(6.4-7.2) | 6.7(6.2-7.5) | 6.8(6.5-7.2) | 6.8(6.5-7.2) | 6.8(6.4-7.3) | 6.6(6.3-7.1) | <0.001 |
| Category B-2 | 7.6(7.0-8.3) | 7.5(6.9-8.1) | 7.3(6.7-8.0) | 7.1(6.6-7.8) | 7.1(6.5-7.7) | 7.2(6.8-7.9) | 7.2(6.8-7.9) | 7.1(6.6-7.7) | 7.1(6.6-7.5) | <0.001 |
| Category C | 7.7(7.0-8.6) | 7.6(6.8-8.8) | 7.4(6.8-8.4) | 7.4(6.7-8.6) | 7.3(6.7-8.1) | 7.4(6.8-8.1) | 7.4(6.8-8.1) | 7.4(6.8-8.2) | 7.3(6.8-7.9) | <0.001 |
Category A; not prescribed any antidiabetic drugs, category B-1; prescribed antidiabetic drugs other than sulfonylureas or glinides, category B-2; prescribed sulfonylureas or glinides, category C; prescribed insulin
Table 3.
The Percentage of Patients with HbA1c Value Less than 7.0%/Less than 8.0%.
| Years | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | p for trend |
|---|---|---|---|---|---|---|---|---|---|---|
| Age group | ||||||||||
| <65 | ||||||||||
| All category | 24.0%/58.8% | 28.9%/65.0% | 38.5%/71.2% | 42.1%/74.2% | 44.0%/76.3% | 39.8%/77.5% | 41.4%/77.7% | 48.5%/80.2% | 48.3%/81.2% | <0.001/<0.001 |
| Category A | 56.0%/88.7% | 54.9%/88.8% | 63.4%/88.4% | 67.2%/91.4% | 68.7%/92.7% | 67.8%/94.6% | 70.7%/95.0% | 80.5%/96.6% | 81.0%/98.8% | <0.001/<0.001 |
| Category B-1 | 28.5%/66.6% | 38.5%/74.4% | 48.3%/81.4% | 47.9%/79.0% | 51.5%/86.3% | 46.4%/85.6% | 47.7%/84.7% | 55.6%/87.4% | 58.0%/88.9% | <0.001/<0.001 |
| Category B-2 | 18.0%/56.5% | 22.4%/62.6% | 30.4%/68.2% | 33.7%/70.8% | 35.3%/71.7% | 41.4%/80.7% | 31.6%/72.9% | 38.3%/75.6% | 36.2%/77.1% | <0.001/<0.001 |
| Category C | 13.0%/39.5% | 14.3%/41.6% | 22.8%/50.6% | 26.4%/57.2% | 28.3%/56.6% | 41.9%/82.2% | 22.4%/58.7% | 29.2%/62.2% | 27.3%/61.0% | <0.001/<0.001 |
| 65-75 | ||||||||||
| All category | 27.3%/67.4% | 32.2%/69.8% | 36.2%/75.2% | 40.0%/76.8% | 43.4%/80.4% | 40.1%/81.3% | 41.1%/81.2% | 49.8%/85.2% | 54.2%/86.9% | <0.001/<0.001 |
| Category A | 48.6%/86.3% | 52.1%/93.3% | 60.2%/93.4% | 60.2%/93.0% | 65.5%/92.4% | 62.6%/94.8% | 67.5%/94.8% | 81.8%/97.4% | 79.5%/98.0% | <0.001/0.007 |
| Category B-1 | 40.3%/81.5% | 44.7%/83.0% | 50.5%/87.2% | 58.1%/86.9% | 60.5%/91.0% | 54.3%/92.7% | 53.5%/89.6% | 62.4%/60.6% | 68.2%/94.7% | <0.001/<0.001 |
| Category B-2 | 23.0%/66.9% | 27.9%/68.0% | 31.4%/73.4% | 34.8%/77.0% | 37.7%/80.2% | 41.8%/80.0% | 33.6%/80.4% | 43.6%/83.8% | 45.2%/85.0% | <0.001/<0.001 |
| Category C | 17.6%/48.8% | 23.4%/53.4% | 24.7%/61.7% | 27.4%/60.5% | 30.4%/66.7% | 39.2%/79.6% | 26.5%/65.7% | 30.8%/69.8% | 38.2%/74.3% | <0.001/<0.001 |
| ≥ 75 | ||||||||||
| All category | 31.5%/70.2% | 35.7%/70.7% | 39.5%/76.8% | 43.4%/78.7% | 47.8%/83.4% | 40.3%/82.4% | 42.2%/80.5% | 46.1%/83.7% | 50.7%/86.0% | <0.001/<0.001 |
| Category A | 49.2%/86.4% | 61.9%/90.5% | 62.9%/95.5% | 59.8%/91.6% | 64.2%/96.7% | 63.0%/95.2% | 71.9%/91.1% | 71.3%/97.1% | 82.5%/95.8% | <0.001/0.023 |
| Category B-1 | 51.3%/86.5% | 46.7%/82.2% | 55.4%/90.5% | 57.1%/93.8% | 68.2%/95.3% | 60.3%/90.4% | 56.5%/92.5% | 60.6%/95.3% | 67.0%/94.2% | 0.013/0.011 |
| Category B-2 | 28.5%/68.4% | 31.1%/69.5% | 35.8%/75.2% | 41.3%/78.2% | 44.3%/82.8% | 37.3%/80.3% | 35.3%/77.8% | 43.0%/83.7% | 45.2%/85.3% | <0.001/<0.001 |
| Category C | 21.5%/59.8% | 28.0%/58.7% | 30.4%/66.5% | 33.8%/66.2% | 36.7%/72.3% | 41.2%/84.2% | 30.4%/72.2% | 30.8%/70.4% | 33.2%/76.0% | 0.19/<0.001 |
Category A: not prescribed any antidiabetic drugs, category B-1: prescribed antidiabetic drugs other than sulfonylureas or glinides, category B-2: prescribed sulfonylureas or glinides, category C: prescribed insulin
In 2013, the median HbA1c values were lower and the proportion of patients with HbA1c values <8.0% higher in the older age groups than in the younger age groups in treatment categories B-1, B-2 and C (Table 2, p for trend with age group in 2013, <0.001 in categories B-1, B-2 and C, and Table 3, p for trend with age group in 2013, <0.001 in categories B-1, B-2 and C). The proportion of patients with HbA1c values <7.0% was significantly higher in the older age group than in the younger age group in category B-1 (p for trend with age group in 2013, <0.001) and category B-2 (p for trend with age group in 2013, 0.0013), but did not exhibit a significant trend with the age groups in “prescribed insulin” group (p for trend with age group in 2013, 0.062). We then analyzed the glycemic control status in the ≥75 age group in 2013 according to the duration after the diagnosis of diabetes.
Discussion
In the present report, we aggregated the prescription trends for elderly diabetic patients before and after the prescription trend for type 2 diabetes changed dramatically around the world with the launch of DPP4is (9-16). The prescription pattern for elderly people with diabetes in other countries is very different from that in Japan. The most commonly prescribed oral antidiabetic drugs for the elderly in the US (15) and Canada (17) are metformin, sulfonylureas and DPP4id, in that order; similarly, in Thailand, the most commonly prescribed drug is metformin, followed in frequency by sulfonylureas and DPP4i, which are prescribed at equivalent rates (18). In contrast, in China (19), as in Japan, higher prescription rates of sulfonylureas are noted for the elderly. In our present analysis, stratification of the prescription rates by the cumulative prescription and monotherapy prescription of choice revealed that drugs that promote insulin secretion (such as sulfonylureas and DPP4is) were used more frequently than biguanides in the older age groups during the observation period. In 2013, DPP4is ranked first as the most frequently prescribed drug class in the 65-74 and ≥75 age groups.
Among drugs that promote insulin secretion, the high prescription rate of DPP4i for elderly patients appears to be unique to Japan. There are several reasons why DPP4is are preferred over metformin and sulfonylureas in elderly Japanese patients. First, this class of drugs has been shown to exhibit excellent glucose-lowering efficacy in East Asians (20). Second, DPP4is improve glycemic control while not being associated with an elevated risk of hypoglycemia and cause weight gain at a lower frequency than sulfonylureas. Third, in many countries, including the US, metformin is preferred as the initial pharmacologic agent for the treatment of type 2 diabetes, if it is tolerated and not contraindicated (21). In contrast, the guidelines in Japan recommend the selection of glucose-lowering agents based on the disease condition of each individual patient while considering the pharmacological and safety profile of each glucose-lowering agent (22). Fourth, as reflected by the health insurance program in Japan for people over 75 years of age, the self-payment for medical examinations and medication in Japan is relatively low compared to most other countries. Under this circumstance, DPP4is are often chosen, even though drugs of this class are more expensive than sulfonylureas or metformin.
There are also several reasons why sulfonylureas are preferred over biguanides in elderly Japanese patients. First, sulfonylureas, which promote insulin secretion, are preferably prescribed for patients with decreased insulin secretion, which is more often observed in patients with smaller BMI values (23-25). The BMI values of type 2 diabetic patients in the East Asian population are lower than those in the Caucasian population (23), and elderly type 2 diabetic patients are leaner than younger type 2 diabetic patients in Japan (4). A sub-analysis of the treatment categories in the ≥75 age group in 2013 according to the duration of diabetes revealed smaller numbers of patients in treatment categories A and B-1 and larger numbers in treatment categories B-2 and C in the subgroup of patients with a longer duration of diabetes (supplementary material). The larger proportion of patients with a longer duration of diabetes and a lower insulin reserve might also be among the reasons for the preferential prescription of sulfonylureas in the older age group in Japan. Second, small additional doses of sulfonylureas are often effective in Japanese type 2 diabetic patients in whom adequate glycemic control is not achieved with DPP4i monotherapy (26, 27), with a lower frequency of severe hypoglycemia episodes than in patients receiving high-dose sulfonylurea therapy [https://www.nittokyo.or.jp/modules/information/index.php?content_id=19 (in Japanese)]. Third, a Committee statement issued in 2012 concerning the proper use of biguanides in Japan recommended that special caution be exercised when prescribing biguanides to elderly patients over 75 years of age who have declined functional reserves and an elevated risk of lactic acidosis. Accordingly, the prescription of sulfonylureas decreased, but these agents remain the second-most frequently prescribed drug with decreased prescribed doses, and biguanides are prescribed at a lower frequency and in smaller doses in elderly patients in Japan than in other countries (Fig. 1, 2).
In the ≥75 age group, the prescription rate of insulin showed a gradual annual increase from 2005 to 2013, while no trend was apparent with respect to the frequency of insulin use in the <65 and 65-74 age groups. As with sulfonylureas, the existence of a larger proportion of patients with a longer duration of diabetes and a lower insulin reserve (supplementary material) might explain the more frequent prescription of insulin in the older age group. In addition, compared to prescribing a larger number of antidiabetic drugs in combination, including larger doses of metformin, in younger age groups, glycemic control using fewer oral antidiabetic drugs in combination without metformin might be insufficient in older patients.
According to previous studies, glycemic control improved each year during the specified study period in Japan (9, 10). The results of the present study (Table 2, 3) are consistent with these previous reports. In the present analysis of type 2 diabetic patients, the HbA1c values were lower in the older age group than in the younger age group for those who received antihyperglycemic pharmacotherapy. This tendency was very similar to that reported recently by the GUIDANCE study conducted in Europe (28). It has been reported that good glycemic control can prevent the development and progression of microvascular complications in patients with type 2 diabetes mellitus (29-31). In elderly patients as well, good glycemic control has been reported to prevent the development and progression of microvascular complications (32) and to reduce the risk of developing acute complications, such as infections (33, 34), which is the third leading cause of death in elderly diabetic patients in Japan (2). The medical institutions included in the present analysis may have prescribed antidiabetic drugs with reference to the above reports for many elderly patients with the objective of achieving a level of glycemic control similar to that in younger diabetic patients.
Can the intensive glycemic control recommended for younger patients improve the quality of life and longevity of elderly patients with type 2 diabetes mellitus? Observational studies on the risk factors for death in diabetic patients have reported that mortality increases with increasing HbA1c levels (35-37) and that there is a U-shaped curvilinear relationship between the HbA1c and mortality (38, 39). In a sub-analysis of the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trial, no excess mortality was observed in the group of type 2 diabetes mellitus patients ≥65 years of age who were given intensive blood glucose-lowering therapy (32). A post hoc analysis of data from the VDAT showed that, with intensive blood glucose-lowering therapy, the risk of death decreased in patients with diabetes of <15 years' duration, while it increased in patients with diabetes of ≥20 years' duration (8). Our present sub-analysis in the ≥75 age group in 2013 showed that treatment strategies potentially associated with hypoglycemia were prescribed more frequently in patients with a longer duration of diabetes (supplementary material). Given the present results, as well as those of the VDAT trial, patients in this age group were given less intensive glucose-lowering therapy. As a result, the proportion of patients with HbA1c values <7.0% was lower in the patient subgroup with a longer duration after the diagnosis of diabetes than in other subgroups of diabetes duration.
With regard to the risk of cardiovascular complications, a sub-analysis of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial showed no marked difference in the risk of cardiovascular death between the normal and intensive treatment groups among patients ≥65 years of age (40). According to the results of a post hoc analysis of the Japanese Elderly Diabetes Intervention Trial (J-EDIT), the incidence of cerebrovascular disorders was significantly higher in the groups with HbA1c values in the highest quartile (HbA1c ≥8.8%) and lowest quartile (HbA1c <7.3%) than in other groups (41). With regard to the risk of the development of dementia, both hyperglycemia (34, 42) and hypoglycemia (43, 44) in diabetic patients have been reported to be associated with an increased risk. Based on these reports, it has been recommended in recent years, with respect to pharmacotherapy for elderly patients with type 2 diabetes mellitus, that glycemic targets be defined after considering the patient's general condition, including the history of the use of drugs that may cause severe hypoglycemia (45). In Japan, the statement, “Glycemic control in elderly patients with diabetes mellitus,” was issued in 2016 by the JDS/JGS Joint Committee on Improving Care for Elderly Patients with Diabetes (3). The statement recommends that, when considering the use of drugs that can cause severe hypoglycemia to treat diabetes mellitus, such as insulin, sulfonylureas and glinides, the HbA1c target be set at 7.0% to <8.0% for patients ≥75 years of age who have a normal cognitive function and no issues with their activities of daily living (ADL). In the present analysis, the proportion of patients with HbA1c <7.0% was lower in treatment categories B-2 and C than in treatment category B-1, and the proportion of patients with HbA1c <7.0% in treatment category C among those ≥75 years of age did not exhibit an increasing trend from 2005 to 2013 (Table 3). These trends might reflect an attitude towards the avoidance of harmful hypoglycemia in the elderly before the publication of the guideline, “Glycemic control in elderly patients with diabetes mellitus.”
There were some limitations associated with this study, so caution should be practiced when interpreting the results. First, the study population consisted of type 2 diabetic patients who were receiving outpatient treatment and did not include patients requiring prolonged hospitalization or long-term facility care for complications; therefore, the treatment/glycemic control trends reflected by the present results may not apply to the latter subset of patients. Second, most of the patients included in the present analysis were treated by a diabetes specialist. The choice of hypoglycemic drugs used by a family doctor might differ from that used by a diabetologist, which may have influenced the present results. Third, the doses of the drugs recorded were those based on the physicians' prescriptions and may therefore have been higher than those actually taken by the patients. Fourth, since the database provided no information on the ADL profiles of the patients, we were unable to take this variable into account while performing the analyses. Finally, the cost effectiveness of the changes in the prescription trends cannot be discussed in this study, as we did not record the treatment costs incurred by the patients in our database.
Japanese society is continuing to age. As such, we should continue to monitor the trends in the treatment of type 2 diabetes mellitus in elderly Japanese patients.
Author's disclosure of potential Conflicts of Interest (COI).
Mitsuhiko Noda: Honoraria, Novo Nordisk Pharma, Taisho Toyama Pharmaceutical and Merck Sharp and Dohme.
Financial Support
This work was funded by Grants-in-Aid from the National Center for Global Health and Medicine (21-119 and 24-104) and from the Ministry of Health, Labour and Welfare, Japan (Grant numbers: Comprehensive Research on Life-Style Related Diseases including Cardiovascular Disease and Diabetes H22-019 and H25-016), and from the Japan Agency for Medical Research and Development (Grant: Practical Research Project for Lifestyle-related Diseases, including Cardiovascular Disease and Diabetes).
Supplementary Material
Sub-analysis in patients ≥75 years of age (as of the year 2013) stratified by years after diagnosis of diabetes.
Acknowledgement
The authors thank Miyako Kishimoto (Sanno Hospital), Hiroshi Noto (St Luke's International Hospital), Hiroji Kitazato (Omori Red Cross Hospital), Kazuo Izumi (National Center for Global Health and Medicine) and Hirohito Sone (Niigata University) for their expert advice and suggestions for the construction of the database. We would also like to acknowledge the skillful data acquisition and invaluable assistance in the registration process provided by Fumie Takano, Masako Ushiyama, Tomoko Umetani, Kumiko Kimura, Hiroko Imanari, Kahoru Kono, Chika Sasaki, Reiko Iwai, Yumiko Watanabe, Chikako Kanehira, Tami Kurishita, Akiko Inoue, Moe Nakanishi, Chika Takahashi, Miki Someya, Ryuji Mitsui, Masako Ooga, Mari Hamada, Miho Yasue, Yuka Uotani, Kayuri Fijiwara, Junko Kudo, Rie Furui, Yoshimi Ishibashi and Chieko Kohno.
References
- 1. Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301: 2129-2140, 2009. [DOI] [PubMed] [Google Scholar]
- 2. Namakura J, Kamiya H, Haneda M, et al. Causes of death in Japanese patients with diabetes based on the results of a survey of 45,708 cases during 2001-2010. -Report from the Committee on the Causes of Death in Diabetes Mellitus. J Diabetes Int 8: 397-410, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Haneda M, Ito H; Japan Diabetes Society (JDS)/Japan Geriatrics Society (JGS) Joint Committee on Improving Care for Elderly Patients with Diabetes.. Committee report: glycemic targets for elderly patients with diabetes. Diabetol Int 7: 331-333, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yamamoto-Honda R, Takahashi Y, Yamashita S, et al. Constructing the National Center Diabetes Database. Diabetol Int 5: 234-243, 2014. [Google Scholar]
- 5. Kosaka K. Diagnostic criteria for diabetes mellitus in Japan-from a report of the Japan Diabetes Society (JDS) Committee on the Diagnosis of Diabetes Mellitus, 1982. Diabetes Res Clin Pract 24: S59-S62, 1994. [DOI] [PubMed] [Google Scholar]
- 6. Kuzuya T, Nakagawa S, Satoh J, et al. ;. Committee of the Japan Diabetes Society on the diagnostic criteria of diabetes mellitus.. Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. Diabetes Res Clin Pract 55: 65-85, 2002. [DOI] [PubMed] [Google Scholar]
- 7. Seino Y, Nanjo N, Tajima N, et al. Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. The Committee of the Japan Diabetes Society on the diagnostic criteria of diabetes mellitus. Diabetol Int 1: 2-20, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Duckworth WC, Abraira C, Moritz TE, et al. ;. Investigators of the VADT.. The duration of diabetes affects the response to intensive glucose control in type 2 subjects: The VA Diabetes Trial. J Diabetes Complications 25: 355-361, 2011. [DOI] [PubMed] [Google Scholar]
- 9. Oishi M, Yamazaki K, Okuguchi F, Sugimoto H, Kanatsuka A, Kashiwagi A. Changes in oral antidiabetic prescriptions and improved glycemic control during the years 2002-2011 in Japan (JDDM32). J Diabetes Invest 5: 581-587, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kohoro T, Yamazaki T, Sato H, et al. Trends in antidiabetic prescription patterns in Japan from 2005 to 2011. Int Heart J 54: 93-97, 2013. [DOI] [PubMed] [Google Scholar]
- 11. Hampp C, Borders-Hemphill V, Money DG, Wysowski DK. Use of antidiabetic drugs in the U.S., 2003-2012. Diabetes Care 34: 1367-1374, 2014. [DOI] [PubMed] [Google Scholar]
- 12. Chiristensen DH, Rungby J, Thomsen RW. Nationwide trends in glucose-lowering drug use, Denmark, 1999-2014. Clin Epidemiol 8: 381-387, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mata-Cases M, Franch-Nadal J, Real J, Maurico D. Glycemic control and antidiabetic treatment trends in primary care centers in patients with type 2 diabetes mellitus during 2007-2013 in Catalonia: a population-based study. BMJ Open 6: e012463, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ko SH, Kim DJ, Park CY, et al. ;. Task Force Team for Diabetes Fact Sheet of the Korean Diabetes Association.. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002-2013: Nationwide population-based cohort study. Medicine (Baltimore) 95: e4018, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lipska KJ, Yao X, Herrin J, et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006-2013. Diabetes Care 40: 468-475, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Turner LW, Nartey D, Stafford RS, Singh S, Alexander GC. Ambulatory treatment of type 2 diabetes in the U.S., 1997-2012. Diabetes Care 37: 985-992, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Clemens KK, Shariff S, Liu K, et al. Trends in antihyperglycemic medication prescriptions and hypoglycemia in older adults: 2002-2013. PLoS One 10: e0137596, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yotsapon T, Sirinate K, Ekgaluck W, et al. Clinical characteristics and outcomes of the oldest old people with type 2 diabetes - perspective from a tertiary diabetes center in Thailand. BMC Endocr Disord 16: 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang L, Ji L, Guo L, et al. Treatment patterns and glycemic control in older adults with type 2 diabetes mellitus receiving only oral antidiabetes drugs in China. Diabetes Technol Ther 17: 816-824, 2015. [DOI] [PubMed] [Google Scholar]
- 20. Kim YG, Hahn S, Oh TJ, Kwak SH, Park KS, Cho YM. Differences in the glucose-lowering efficacy of dipeptidase-4 inhibitors between Asians and non-Asians: a systematic review and meta-analysis. Diabetologia 56: 696-708, 2013. [DOI] [PubMed] [Google Scholar]
- 21. The American Diabetes Association (eds.) Standards of medical care in diabetes-2017. . Pharmacologic approaches to glycemic treatment. Diabetes Care 40 (Supple 1): S64-S74, 2017. [DOI] [PubMed] [Google Scholar]
- 22. Tajima N, Noda M, Origasa H, et al. Evidence-based practice guideline for the treatment for diabetes in Japan 2013. Diabetol Int 6: 151-187, 2015. [Google Scholar]
- 23. Moller JB, Pedersen M, Tanaka H, et al. Body composition is the main determinant for the difference in type 2 diabetes pathophysiology between Japanese and Caucasians. Diabetes Care 37: 796-804, 2014. [DOI] [PubMed] [Google Scholar]
- 24. Yoshinaga H, Kosaka K. Heterogenous relationship of early insulin response and fasting insulin level with development of non-insulin-dependent diabetes mellitus in non-diabetic Japanese subjects with or without obesity. Diabetes Res Clin Pract 44: 129-136, 1999. [DOI] [PubMed] [Google Scholar]
- 25. Yamamoto-Honda R, Osame K, Kitazato H, et al. Insulin secretion and insulin sensitivity in Japanese patients with Type 2 diabetes: a cross-sectional study comparing the homeostasis model assessment-2 (HOMA-2) indexes derived from the oral glucose tolerance test. Diabetology Int 2: 72-78, 2011. [Google Scholar]
- 26. Harashima SI, Ogura M, Tanaka D, et al. Sitagliptin add-on low dosage sulphonylureas: efficacy and safety of combination therapy on glycemic control and insulin secretion capacity in type 2 diabetes. Int J Clin Pract 66: 465-476, 2012. [DOI] [PubMed] [Google Scholar]
- 27. Umahaya R, Yonemoto T, Kyou C, et al. Low-dose glimepiride with sitagliptin improves glycemic control without dose-dependency in patients with type 2 diabetes inadequately controlled on high-dose glimepiride. Endocr J 61: 1163-1170, 2014. [DOI] [PubMed] [Google Scholar]
- 28. Muller N, Khunti K, Kuss O, et al. Is there evidence of potential overtreatment of glycemia in elderly people with type 2 diabetes? Data from the GUIDANCE study. Acta Diabetol 54: 209-214, 2017. [DOI] [PubMed] [Google Scholar]
- 29. Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 28: 103-117, 1995. [DOI] [PubMed] [Google Scholar]
- 30. UK Prospective Diabetes Study (UKPDS) Group. . Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352: 837-853, 1998. [PubMed] [Google Scholar]
- 31. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359: 1577-1589, 2008. [DOI] [PubMed] [Google Scholar]
- 32. ADVANCE Collaborative Group. . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358: 2560-2572, 2008. [DOI] [PubMed] [Google Scholar]
- 33. Pearson-Stuttard J, Blundell S, Harris T, Cook DG, Critchley J. Diabetes and infection: assessing the association with glycemic control in population-based studies. Lancet Diabetes Endocrinol 4: 148-158, 2016. [DOI] [PubMed] [Google Scholar]
- 34. McGovern AP, Hine J, de Lusingnan S. Infection risk in elderly people with reduced glycemic control. Lancet Diabetes Endocrinol 4: 303-304, 2016. [DOI] [PubMed] [Google Scholar]
- 35. Eeg-Olofsson K, Cederholm J, Nilsson PM, et al. New aspects of HbA1c as a risk factor for cardiovascular diseases in type 2 diabetes: an observational study from the Swedish National Diabetes Register (NDR). J Intern Med 268: 471-482, 2010. [DOI] [PubMed] [Google Scholar]
- 36. Landman GW, van Hateren KJ, Kleefstra N, Groenier KH, Gans RO, Bilo HJ. The relationship between glycaemic control and mortality in patients with type 2 diabetes in general practice (ZODIAC-11). Br J Gen Pract 60: 172-175, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sluik D, Boeing H, Montonen J, et al. HbA1c measured in stored erythrocytes is positively linearly associated with mortality in individuals with diabetes mellitus. PLoS one 7: e38877, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet 2010: 375, 481-489, 2010. [DOI] [PubMed] [Google Scholar]
- 39. Huang ES, Liu JY, Moffet HH, John PM, Karter AJ. Glycemic control, complications, and death in older diabetic patients: the diabetes and aging study. Diabetes Care 34: 1329-1336, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Miller ME, Bonds DE, Gerstein HC, et al. ;. ACCORD Investigators.. The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: Post hoc epidemiological analysis of the ACCORD study. BMJ 340: b5444, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Araki A, Iimuro S, Sakurai T, et al. ; Japanese Elderly Intervention Trial Research Group. . Non-high-density lipoprotein cholesterol: an important predictor of stroke and diabetes-related mortality in Japanese elderly diabetic patients. Geriatr Gerontol Int 12 (Suppl 1): 18-28, 2012. [DOI] [PubMed] [Google Scholar]
- 42. Cukierman-Yaffe T, Gerstein HC, Williamson JD, et al. Relationship between baseline glycemic control and cognitive function in individuals with type 2 diabetes and other cardiovascular risk factors: the action to control cardiovascular risk in diabetes-memory in diabetes (ACCORD-MIND) trial. Diabetes Care 32: 221-226, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP Jr, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA 301: 1565-1572, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lin CH, Sheu WH. Hypoglycemic episodes and risk of dementia in diabetes mellitus: 7-year follow-up study. J Intern Med 273: 102-110, 2013. [DOI] [PubMed] [Google Scholar]
- 45. Kirkman MS, Briscoe VJ, Clark N, et al. ; Consensus development conference on diabetes and older adults.. Diabetes in older adults: a consensus report. J Am Geriat Soc 60: 2342-2356, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sub-analysis in patients ≥75 years of age (as of the year 2013) stratified by years after diagnosis of diabetes.