Abstract
Objective:
Ultrasonography (US) and parathyroid scintigraphy (PS) with 99mTc-MIBI are common methods for preoperative localization of parathyroid adenomas but there discrepancies exist with regard to diagnostic accuracy. The aim of the study was to compare PS and US for localization of parathyroid adenoma with a systematic review and meta-analysis of the literature.
Methods:
Pub Med, Scopus (EMbase), Web of Science and the reference lists of all included studies were searched up to 1st January 2016. The search strategy was according PICO characteristics. Heterogeneity between the studies was accounted by P < 0.1. Point estimates were pooled estimate of sensitivity, specificity and positive predictive value of SPECT and ultrasonography with 99% confidence intervals (CIs) by pooling available data. Data analysis was performed using Meta-DiSc software (version 1.4).
Results:
Among 188 studies and after deletion of duplicated studies (75), a total of 113 titles and abstracts were studied. From these, 12 studies were selected. The meta-analysis determined a pooled sensitivity for scintigraphy of 83% [99% confidence interval (CI) 96.358 -97.412] and for ultra-sonography of 80% [99% confidence interval (CI) 76-83]. Similar results for specificity were also obtained for both approache.
Conclusion:
According this meta- analysis, there were no significant differences between the two methods in terms of sensitivity and specificity. There were overlaps in 99% confidence intervals. Also features of the two methods are similar.
Keywords: Parathyroid neoplasms, ultrasonography, radionuclide imaging, sensitivity and specificity
Introduction
Primary hyperparathyroidism is 3rd most common neuroendocrine disorder (Johnston et al., 1996; Mazzeo et al., 1996; Tukagi et al., 1985; Ruda et al., 2006). Parathyroid adenoma is the most common pathology for hyperparathyroidism (Wong et al., 2015; Lumachi et al., 2000; Bahansali et al.,2006; Cakal et al., 2012; Perie et al., 2005). It is more prevalent in women. Hyperparathyroidism is characterized by parathyroid hormone (PTH) increase and hypercalcemia since PTH is the key calcium hemostasis regulator (Mahmoudi et al., 2015; Gupta et al., 2013). Bilateral neck exploration was the traditional surgical treatment (Shafieia et al., 2012). But recently, minimally invasive parathyroidectomy (MIP) is most important key treatment in parathyroid adenoma as a standard care for hyperparathyroidism. It needs locoregional anesthesia, minor cervical exploration and smaller incisions in comparison with conventional bilateral neck exploration (Shafieia et al., 2012).
Exact preoperative localization of parathyroid adenoma is very important for MIP (Gooding 1993). The radiological and nuclear imaging methods are suggested for preoperative planning. The 99mTc-MIBI parathyroid scintigraphy (PS) and ultrasonography (US) are acceptable imaging modalities to detect parathyroid adenoma prior to operation. But in literature there is a discrepancy between accuracy of these two methods. Clinicians should be aware of essential factors in choice of an appropriate plan such as diagnostic accuracy, radiation dose, cost benefit and availability (Patel et al., 2010; Frilling et al., 2000; Nabriski et al.,1992).
PS make available incremental diagnostic value in localization parathyroid adenoma and guide the surgeon. US is a simple, non-expensive and available imaging modality for parathyroid adenoma localization (Lumachi et al., 2000; Cakal et al., 2012; Patel et al., 2010; Lumachi et al., 2001; Arici et at., 2001; Berri et al., 2006; Kim et al., 2012; Tublin et al., 2009; Freudenburg et al., 2006; Kebapci et al., 2004; Grosso et al., 2007; Hajioff et al., 2004; Gergel et al., 2014; Lo et al., 2007; Berczi et al., 2002; Barczynski et al., 2006).
We designed a systematic review and meta-analysis to determine the diagnostic accuracy of parathyroid scintigraphy and ultrasonography for preoperative localization of parathyroid adenoma.
Materials and Methods
We conducted a systematic search of electronic database (MEDLINE, Scopus (EMbase), Web of Science) and MEDLINE non-indexed databases up to 1january 2016. The last updated search was done on 12 February 2017. The reference lists of all included studies were searched for further studies.
Search strategy
The search strategy was according PICO characteristics, Mesh term and key word are including: Patients/problem: Parathyroid Adenomas, Neoplasm, Parathyroid, Parathyroid Neoplasm, Neoplasms Parathyroid, Cancer of Parathyroid, Parathyroid Cancers, Cancer of the Parathyroid, Parathyroid Adenoma, Adenoma, Parathyroid, Adenomas, Parathyroid,” “primary hyperparathyroidism,” “parathyroid adenoma as population.
Index
Ultrasound Imaging, Imaging, Ultrasound Imagings, Ultrasound, Ultrasound Imagings, Sonography, Medical, Medical Sonography, Ultrasonic Imaging, Imaging, Ultrasonic, Diagnosis, Ultrasonic, Diagnoses, Ultrasonic, Ultrasonic Diagnoses, Ultrasonic Diagnosis
Comparison
Imaging, Radionuclide, Radioisotope Scanning, Scintigraphy, Gamma Camera Imaging, Gamma Camera, Scanning, Radioisotope, Scintiphotography, radionuclide imaging,’’ ‘‘SPECT,’’ ‘‘sestamibi,,’’ ‘‘computed tomography.
Outcome
Specificity and Sensitivity, Sensitivity, Specificity, Diagnostic accuracy
The literature search was performed by two independent reviewers (NN and SKRR). After reviewed Titles study and abstracts relevant studies were selected. Selection criteria are included 1) studies of patients with suspected parathyroid adenoma 2) undergoing ultrasound, parathyroid scintigraphy and surgery as gold standard. 3) Tc-99m sestamibi with early and delayed images was considered as Sestamibi-scintigraphy techniques.
Letters to the editor, review articles, case reports, and paper with not enough information of sensitivity and predictive value were excluded. Studies quality was assessed using the modified QUADAS criteria (Quality Assessment of Diagnostic Accuracy Studies).
Extraction of study characteristics
A standard template worksheet were used for data extraction including paper’s code, reviewer code, Bibliographic information, study date (year), sample size, Study design , Sensitivity, specificity and ROC of ultrasonography as well as Sensitivity, specificity and ROC of scintigraphy. Sensitivity and specificity of ultrasonography and scintigraphy were calculated if were not reported.
Data analysis was performed using Meta-DiSc software (version 1.4). Der Simonian-Laired, random-effect model was used to pool the extraction data. Forest plots and pooled effect size of the extraction data was used with 99% confidence intervals (CI). Studies Heterogeneity was evaluated using visual inspection of the forest plots for (i) degree of deviation of sensitivity and specificity of each study from the vertical line corresponding with the pooled estimates, (ii) inconsistence index and (iii) Chi-square p-values.
Results
All articles were reviewed by two reviewers. The 188 were included after 75 duplicate articles removal. 113 title and abstracts were reviewed and 40 non relevance articles were excluded. Then 73 full text studies were appraised. Finally 12 original articles with eligibility criteria were selected for meta-analysis (Figure 1). The quality assessment of included studies according modified QUADAS score 2 is presented in Figure 2. Table 1 shows the included studies characteristics. The pooled estimates of sensitivity, specificity and Receiver Operating Characteristics (ROC) are described in Table 2.
Figure 1.
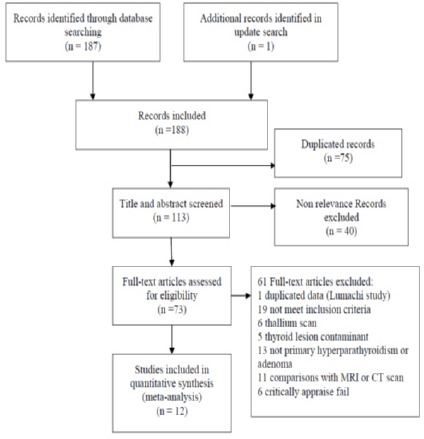
Flow Diagram of Article Selection Process
Figure 2.
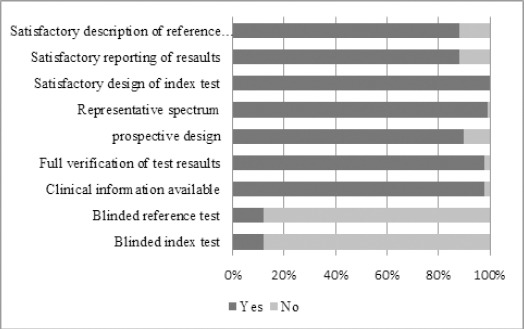
The Quality Assessment of Included Studies According Modified QUADAS Score 2
Table 1.
The Basic Study Characteristics
| First author | Publication year | Sample size Female Male | Type of study | Country | Mean age of participants |
|---|---|---|---|---|---|
| Arici | 2001 | 338 | Retrospective | USA | 60 |
| 242 | |||||
| 96 | |||||
| Barczynski | 2006 | 121 | Retrospective | Poland | 56.1 |
| 106 | |||||
| 15 | |||||
| Berczi | 2002 | 63 | Prospective | Hungary | 54 |
| 50 | |||||
| 13 | |||||
| Bhansali | 2006 | 46 | Prospective | India | 37.1 |
| 33 | |||||
| 13 | |||||
| Cakal | 2012 | 39 | Prospective | Turkey | 53.2 |
| 29 | |||||
| 10 | |||||
| Freudenburg | 2006 | 84 | Prospective | Germany | 54 |
| 46 | |||||
| 38 | |||||
| D.Hajioff | 2004 | 48 | Prospective | UK | 60 |
| 36 | |||||
| 12 | |||||
| Lo | 2007 | 100 | Prospective | China | 55.5 |
| 70 | |||||
| 30 | |||||
| Lumachi | 2000 | 91 | Prospective | Italy | 59 |
| 65 | |||||
| 26 | |||||
| Patel | 2010 | 63 | Retrospective | UK | 59 |
| 42 | |||||
| 21 | |||||
| Tubline | 2009 | 144 | Prospective | USA | 63.2 |
| 117 | |||||
| 27 |
Table 2.
The Pooled Estimate of Sensitivity, Specificity and AUC of Tc-99m Sestamibi and Ultrasound Studies
| Pooled estimate | Ultrasound (99%CI) |
Tc-99m sestamibi (99%CI) |
|---|---|---|
| sensitivity | 80 %( 77-83%) | 84% (80-87%) |
| specificity | 77% (71-82%) | 87% (83-91%) |
| AUC(± standard error) | 0.87 (0.042) | 0.94 (0.033) |
The forest plot of pooled US sensitivity, SP sensitivity and SROC are presented in Figures 3-6.
Figure 3.
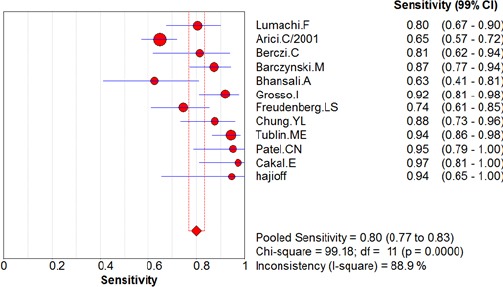
The Forest Plot of Pooled US Sensitivity
Figure 4.
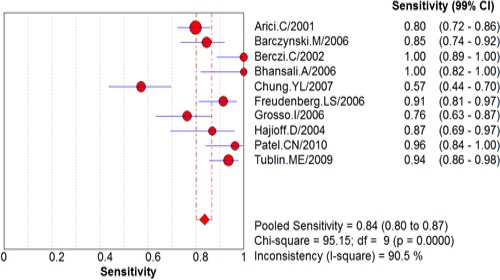
The Forest Plot of Pooled SP Sensitivity
Figure 5.
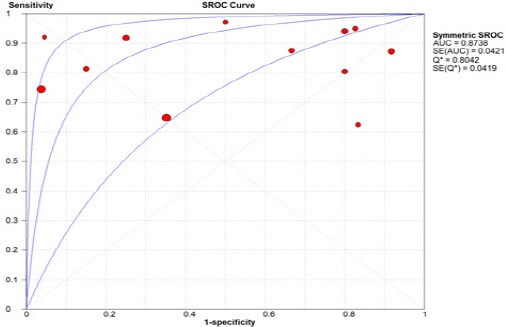
The Forest Plot of Pooled US SROC
Figure 6.
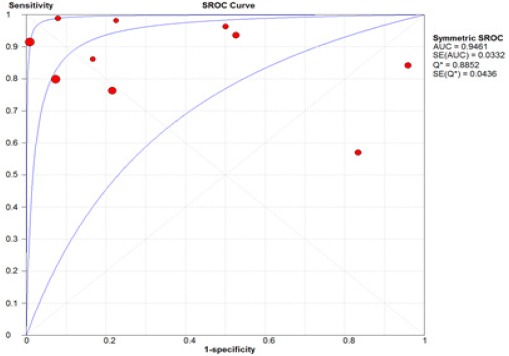
The Forest Plot of Pooled PS SROC
Discussion
Various diagnostic modalities are suggested to preoperative localization of parathyroid Adenoma (Lumachi et al., 2001; Arici et at., 2001; Berri et al., 2006; Kim et al., 2012; Tublin et al., 2009; Freudenburg et al., 2006). 99m Tc-sestamibi parathyroid scintigraphy and ultrasonography are common diagnostic methods for parathyroid adenoma localization (Carlson et al., 1990; Li et al., 2012; Carlier et al., 2008). Most key benefit of precise preoperative localization is minimally invasive parathyroid surgery. Accuracy of imaging methods is dissimilar (Li et al., 2012; Carlier et al., 2008; Maka et al., 1997; Haciyanli et al., 2003; Yip et al., 2008; Mihai et al., 2008). A wide range of sensitivity and specificity was informed in literature for PS and US. The operator dependence of US is known. Also several aspects may influence the accuracy of PS were identified (Shafieia et al., 2012; Gooding 1993).
Our study findings showed the pooled sensitivity of two methods are not statistically different but the pooled estimate of PS specificity is significantly higher than US specificity. Our research has directly compared PS and US, and we selected studies that PS and US were performed for each patient. According to individual studies, the findings are conflicting. As some studies, support these findings and some refer to the superiority of US.
Most of diagnostic studies report the positive predictive value (PPV) of test instead of specificity because of no true negative cases. PPV shows the number of true positive cases among total positive result. In real situation (not study) PPV is more affected by disease prevalence which is neglected in diagnostic studies. In this systematic review and meta-analysis we restricted the inclusion criteria to studies with adequate findings to calculate the specificity.
In a meta-analysis and systematic review study of nuclear imaging in the diagnosis of parathyroid adenoma, the results have mentioned using nuclear imaging as the most common parathyroid adenoma detection method. In this study only nuclear imaging method is studied. Cumulative sensitivity of nuclear imaging in diagnose of parathyroid glands in this meta-analysis obtained 86% with 81-90% confidence interval, which is quite consistent with the results of our recent study (Wong et al., 2015).
Another Meta-analysis and systematic review study on all type of diagnostic methods for preoperative localization techniques in primary hyperparathyroidism the sensitivity of two methods were not statistically different. Because of different inclusion criteria the specificity and positive predictive value of two studies were not comparable. The results of recent meta-analysis and systematic review study are provided acceptable sensitivity and specificity of this method.
In this systematic review only studies that have been done by SPECT imaging method has entered, because thallium studies did not earn enough score to enter the study. For this reason, in this study subgroup analyzes and comparison of the diagnostic accuracy of different methods of nuclear imaging was not possible.
One of the very significant limitations in diagnostic studies are performing diagnostic tests in patient groups, in this study all studies that clearly indicated this point were excluded.
The many initial studies were case-reports with no gold standard comparison (surgical outcomes) were expressed, and these studies did not enter the data extraction process.
Also a significant number of studies because of limitation entry criteria in terms of language study were published did not enter in meta-analysis and systematic review study.
The strengths of the study include the high quality of input studies, pointed out in a critical appraisal phase. All input studies obtained full score of key questions of critical appraisal check list.
Depending on the type of input studies that were diagnostic, accomplishment of famous tests and drawing funnel plot to explore the publication bias was not possible, So all studies were further investigated after critical appraisal, that are listed in the Table.
As another limitation, the diagnosis of parathyroid is affected by position, size, functional characteristics of hyper-functioning, thyroid nodule and goiter. In our study only the thyroid nodule and goiter were controlled. The individual studies did not control this aspect of disease. It should be noticed that gray literatures were not included.
In most studies, the time interval between diagnostic tests and surgical procedures was not stated that could affect results. As a conclusion, sensitivity in nuclear imaging technique is similar to ultrasound, but the specificity of nuclear imaging is higher than US. Also features of two methods are close together.
Funding statements
There were no sources of funding for the article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Arici C, Cheah WK, Ituarte PH, et al. Can localization studies be used to direct focused parathyroid operation s? Surg J (N Y) 2001;129:720–9. doi: 10.1067/msy.2001.114556. [DOI] [PubMed] [Google Scholar]
- Barczynski M, Golkowski F, Konturek A, et al. Technetium-99m-sestamibi subtraction scintigraphy vs. ultrasonography combined with a rapid parathyroid hormone assay in parathyroid aspirates in preoperative localization of parathyroid adenomas and in directing surgical approach. Clin Endocrinol. 2006;65:106–13. doi: 10.1111/j.1365-2265.2006.02556.x. [DOI] [PubMed] [Google Scholar]
- Berczi C, Mezosi E, Galuska L, et al. Technetium-99m-sestamibi/pertechnetate subtraction scintigraphy vs ultrasonography for preoperative localization in primary hyperparathyroidism. Eur Radiol. 2002;12:605–9. doi: 10.1007/s003300101045. [DOI] [PubMed] [Google Scholar]
- Berri RN, Lloyd LR. Detection of parathyroid adenoma in patients with primary hyperparathyroidism:the use of office-based ultrasound in preoperative localization. Am J Surg. 2006;191:311–4. doi: 10.1016/j.amjsurg.2005.10.027. [DOI] [PubMed] [Google Scholar]
- Bhansali A, Masoodi S, Bhadada S, et al. Ultrasonography in detection of single and multiple abnormal parathyroid glands in primary hyperparathyroidism:comparison with radionuclide scintigraphy and surgery. Clin Endocrinol. 2006;65:340–5. doi: 10.1111/j.1365-2265.2006.02601.x. [DOI] [PubMed] [Google Scholar]
- Cakal E, Cakir E, Dilli A, et al. Parathyroid adenoma screening efficacies of different imaging tools and factors affecting the success rates. Clin Imaging. 2012;36:688–94. doi: 10.1016/j.clinimag.2012.01.038. [DOI] [PubMed] [Google Scholar]
- Carlier T, Oudoux A, Mirallié E, et al. 99mTc-MIBI pinhole SPECT in primary hyperparathyroidism:comparison with conventional SPECT, planar scintigraphy and ultrasonography. Eur J Nucl Med Mol Imaging. 2008;35:637–43. doi: 10.1007/s00259-007-0625-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson GL, Farndon JR, Clayton B, Rose PG. Thallium isotope scintigraphy and ultrasonography:comparative studies of localization techniques in primary hyperparathyroidism. Br J Surg. 1990;77:327–9. doi: 10.1002/bjs.1800770330. [DOI] [PubMed] [Google Scholar]
- Freudenberg LS, Frilling A, Sheu S-Y, Görges R. Optimizing preoperative imaging in primary hyperparathyroidism. Langenbecks Arch Surg. 2006;391:551–6. doi: 10.1007/s00423-006-0076-y. [DOI] [PubMed] [Google Scholar]
- Frilling A, Görges R, Clauer U, Tecklenborg K, Broelsch CE. Minimally invasive parathyroidectomy under local anesthesia in connection with ultrasonography, sestamibi scintigraphy and intra-operative parathormone measurement. Chirurg. 2000;71:1474–9. doi: 10.1007/s001040051246. [DOI] [PubMed] [Google Scholar]
- Gergel M, Brychta I, Vician M, Olejnik J. Primary hyperparathyreosis:is concordant sonography and scintigraphy really so important? Bratisl Lek Listy. 2014;115:649–52. doi: 10.4149/bll_2014_125. [DOI] [PubMed] [Google Scholar]
- Gooding G. Sonography of the thyroid and parathyroid. Radiol Clin North Am. 1993;31:967–89. [PubMed] [Google Scholar]
- Grosso I, Sargiotto A, D'Amelio P, et al. Preoperative localization of parathyroid adenoma with sonography and 99mTc-sestamibi scintigraphy in primary hyperparathyroidism. J Clin Ultrasound. 2007;35:186–9. doi: 10.1002/jcu.20319. [DOI] [PubMed] [Google Scholar]
- Gupta S, Mittal A, Sathian B. Significance of HCG to distinguish parathyroid carcinoma from benign disease and in adding prognostic information:A hospital based study from Nepal. Asian Pac J Cancer Prev. 2013;14:325–7. doi: 10.7314/apjcp.2013.14.1.325. [DOI] [PubMed] [Google Scholar]
- Haciyanli M, Lal G, Morita E, et al. Accuracy of preoperative localization studies and intraoperative parathyroid hormone assay in patients with primary hyperparathyroidism and double adenoma. J Am Coll Surg. 2003;197:739–46. doi: 10.1016/S1072-7515(03)00676-8. [DOI] [PubMed] [Google Scholar]
- Hajioff D, Iyngkaran T, Panagamuwa C, Hill D, Stearns M. Preoperative localization of parathyroid adenomas:ultrasonography, sestamibi scintigraphy, or both? Clin Otolaryngol Allied Sci. 2004;29:549–52. doi: 10.1111/j.1365-2273.2004.00858.x. [DOI] [PubMed] [Google Scholar]
- Johnston L, Carroll M, Britton K, et al. The accuracy of parathyroid gland localization in primary hyperparathyroidism using sestamibi radionuclide imaging. J Clin Endocrinol Metab. 1996;81:346–5. doi: 10.1210/jcem.81.1.8550776. [DOI] [PubMed] [Google Scholar]
- Kebapci M, Entok E, Kebapci N, Adapinar B. Preoperative evaluation of parathyroid lesions in patients with concomitant thyroid disease:role of high resolution ultrasonography and dual phase technetium 99m sestamibi scintigraphy. J Endocrinol Invest. 2004;27:24–3. doi: 10.1007/BF03350906. [DOI] [PubMed] [Google Scholar]
- Kim YI, Jung YH, Hwang KT, Lee HY. Efficacy of (99)mTc-sestamibi SPECT/CT for minimally invasive parathyroidectomy:comparative study with (99)mTc-sestamibi scintigraphy, SPECT, US and CT. Ann Nucl Med. 2012;26:804–10. doi: 10.1007/s12149-012-0641-0. [DOI] [PubMed] [Google Scholar]
- Li CC, Yang C, Wang S, et al. A 10-year retrospective study of primary hyperparathyroidism in children. Exp Clin Endocrinol Diabetes. 2012;120:229–33. doi: 10.1055/s-0032-1301895. [DOI] [PubMed] [Google Scholar]
- Lo C-Y, Lang BH, Chan W, Kung AW, Lam KS. A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg. 2007;193:155–9. doi: 10.1016/j.amjsurg.2006.04.020. [DOI] [PubMed] [Google Scholar]
- Lumachi F, Zucchetta P, Marzola M, et al. Advantages of combined technetium-99m-sestamibi scintigraphy and high-resolution ultrasonography in parathyroid localization:comparative study in 91 patients with primary hyperparathyroidism. Eur J Endocrinol. 2000;143:755–60. doi: 10.1530/eje.0.1430755. [DOI] [PubMed] [Google Scholar]
- Lumachi F, Ermani M, Basso S, et al. Localization of parathyroid tumours in the minimally invasive era:which technique should be chosen? Population-based analysis of 253 patients undergoing parathyroidectomy and factors affecting parathyroid gland detection. Endocr Relat Cancer. 2001;8:63–9. doi: 10.1677/erc.0.0080063. [DOI] [PubMed] [Google Scholar]
- Mahmoudi T, Karimi Kh, Arkani M, et al. Parathyroid hormone gene rs6256 and calcium sensing receptor gene rs1801725 variants are not associated with susceptibility to colorectal cancer in Iran. Asian Pac J Cancer Prev. 2015;15:6035–39. doi: 10.7314/apjcp.2014.15.15.6035. [DOI] [PubMed] [Google Scholar]
- Mazzeo S, Caramella D, Lencioni R, et al. Comparison among sonography, double-tracer subtraction scintigraphy, and double-phase scintigraphy in the detection of parathyroid lesions. AJR Am J Roentgenol. 1996;166:1465–70. doi: 10.2214/ajr.166.6.8633466. [DOI] [PubMed] [Google Scholar]
- Mihai R, Weisters M, Stechman MJ, Gleeson F, Sadler G. Cost-effectiveness of scan-directed parathyroidectomy. Langenbecks Arch Surg. 2008;393:739–43. doi: 10.1007/s00423-008-0383-6. [DOI] [PubMed] [Google Scholar]
- Moka D, Voth E, Larena-Avellaneda A, Schicha H. 99mTc-MIBI-SPECT for the location of small parathyroid adenoma. Nuklearmedizin. 1997;36:240–4. [PubMed] [Google Scholar]
- Nabriski D, Bendahan J, Shapiro MS, Freund U, Lidor C. Sarcoidosis masquerading as a parathyroid adenoma. Head Neck. 1992;14:384–6. doi: 10.1002/hed.2880140508. [DOI] [PubMed] [Google Scholar]
- Patel C, Salahudeen H, Lansdown M, Scarsbrook A. Clinical utility of ultrasound and 99m Tc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol. 2010;65:278–87. doi: 10.1016/j.crad.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Perie S, Fessi H, Tassart M, et al. Usefulness of combination of high-resolution ultrasonography and dual-phase dual-isotope iodine 123/technetium Tc 99m sestamibi scintigraphy for the preoperative localization of hyperplastic parathyroid glands in renal hyperparathyroidism. Am J Kidney Dis. 2005;45:344–52. doi: 10.1053/j.ajkd.2004.10.021. [DOI] [PubMed] [Google Scholar]
- Ruda JM, Stack BC, Hollenbeak CS. The cost-effectiveness of additional preoperative ultrasonography or sestamibi–SPECT in patients with primary hyperparathyroidism and negative findings on sestamibi scans. Arch Otolaryngol Head Neck Surg. 2006;132:46–53. doi: 10.1001/archotol.132.1.46. [DOI] [PubMed] [Google Scholar]
- Shafieia B, Hoseinzadeh S, Fotouhia F, et al. Preoperative 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism and concomitant nodular goiter:comparison of SPECT-CT, SPECT, and planar imaging. Nucl Med Commun. 2012;33:1070–6. doi: 10.1097/MNM.0b013e32835710b6. [DOI] [PubMed] [Google Scholar]
- Takagi H, Tominaga Y, Uchida K, et al. Comparison of imaging methods for diagnosing enlarged parathyroid glands in chronic renal failure. J Comput Assist Tomogr. 1985;9:733–7. doi: 10.1097/00004728-198507010-00014. [DOI] [PubMed] [Google Scholar]
- Tublin ME, Pryma DA, Yim JH, et al. Localization of parathyroid adenomas by sonography and technetium tc 99m sestamibi single-photon emission computed tomography before minimally invasive parathyroidectomy:are both studies really needed? J Ultrasound Med. 2009;28:183–90. doi: 10.7863/jum.2009.28.2.183. [DOI] [PubMed] [Google Scholar]
- Wong KK, Fig LM, Gross MD, Dwamena BA. Parathyroid adenoma localization with 99mTc-sestamibi SPECT/CT:a meta-analysis. Nucl Med Commun. 2015;36:363–75. doi: 10.1097/MNM.0000000000000262. [DOI] [PubMed] [Google Scholar]
- Yip L, Pryma DA, Yim JH, et al. Can a lightbulb sestamibi SPECT accurately predict single-gland disease in sporadic primary hyperparathyroidism? World J Surg. 2008;32:784–92. doi: 10.1007/s00268-008-9532-x. [DOI] [PubMed] [Google Scholar]


