Abstract
Introduction:
Cervical cancer rates vary across the world, being highest in Eastern Africa (including Zimbabwe) and lowest in Western Asia. It is the second most common type of cancer in women in the South East Asia region and a major cause of cancer deaths among women of low and middle income countries (LMICs) like Nepal. This review is an attempt to make a comprehensive report of prevalence, incidence and mortality of cervical cancer in LMICs.
Methods:
The review was conducted applying a computerized search with the Medical Subject Heading (MeSH) major topics “Cervical Cancer”, “Cervical neoplasm” “Epidemiology”, (“prevalence” OR “incidence” OR “mortality”) and “HPV” OR “Human papillomavirus” as MeSH subheading. The search limits were: language (“English”), LMICs, dates (articles published from “1st January 2000 to 31st December 2015”), and species (“Humans”). The search was supplemented by cross-referencing. Publications that met the inclusion criteria were included in the synthesis.
Results:
Among the 20 studies reviewed; seven were from Africa, seven from Asia, three from South America, and one each from North America, Europe and Oceania. The review found the highest reported age standardized incidence rate as 17.9/100,000/year in Zimbabwe in 2000 and the lowest as 0.11/100,000/year in China in 2006. One study of Nigeria revealed a cervical cancer prevalence of 5.0 per 1,000 in 2012 in the 25-64 year age group. Further, the highest reported age standardized mortality rate was 16/100,000/year in India in 2015 and the lowest 1.8/100,000/year in Colombia in 2013. In addition, coitarche, tobacco smoking, number of sexual partners and family history of cervical cancer were reported as significant risk factors.
Conclusion:
The study provides a review of reported prevalence, incidence and mortality of cervical cancer in LMICs from 1st January 2000 to 31st December 2015. The scarcity of information reveals a substantial need for further studies on cervical cancer prevalence, incidence and mortality with associated risk factors in LMICs.
Keywords: Cervical cancer, epidemiology, low and middle income countries
Introduction
Cervical cancer occurs in the lower part of the uterus that connects to the vagina; in the cells of the cervix (Fritz et al., 2000). Recent global figures estimate 527,624 new cases and 265,672 deaths due to cervical cancer annually. Cervical cancer rates are highest in Eastern Africa (including Zimbabwe) and lowest in Western Asia. However, it is the second most common type of cancer in women in the South East Asia region and the major cause of cancer deaths among women of low and middle income countries (LMICs) like Nepal. International Agency for Research on Cancer (IARC, 2012) estimated age standardized incidence rate of cervical cancer as 19.0 per 100,000 and age standardized mortality rate as 12.0 per 100,000 in Nepal (Ferlay et al., 2013).
Studies have shown that sexual behavior at an early age and increasing incidence of human papillomavirus (HPV) infection cause cervical cancer incidence to increase among younger women (Bosch et al., 1995). Studies have estimated that over 80% of sexually active women will be infected with genital HPV at some point in their lifetime (Syrjanen et al., 1990). Oncogenic HPV infection is the major etiological agent of cervical cancer of which70% are caused by HPV-16 and HPV-18 type (Munoz et al., 2004; Schiffman et al., 2007).
In spite of the high disease burden, there are limited numbers of studies conducted on prevalence, incidence and mortality of cervical cancer in LMICs and no systematic review exists in this field. Our aim is to investigate the prevalence, incidence, mortality and major risk factors of cervical cancer reported by articles published in the period from 1st Jan 2000 to 31st Dec 2015 in LMICs. We believe this systematic review will constitute valuable reference materials for epidemiologists, health policy makers and researchers on cervical cancer.
Materials and Methods
Design
We conducted the review applying a computerized systematic search to identify the prevalence, incidence and mortality of cervical cancer in LMICs. The inclusion criteria of articles were: original article, studies reporting prevalence, incidence, and mortality rates, articles in English and studies conducted on humans. Figure 1 describes the inclusion and exclusion criteria as well as extraction process.
Figure 1.
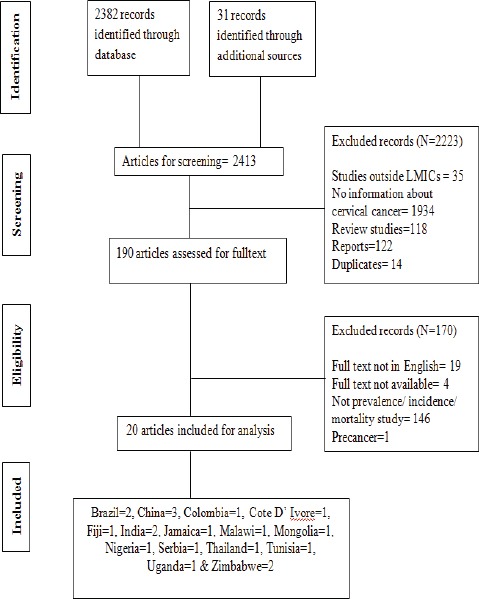
Flow Diagram of the Study
Data extraction
We performed a three-stage selection for data extraction. In the first stage, a search of the online Medical Literature Analysis and Retrieval System (MEDLINE) database was performed with a combination of Medical Subject Heading (MeSH) terms: “Cervical Cancer” and “Cervical Neoplasm” as major topics and “Epidemiology”, (“prevalence” OR “incidence” OR “mortality”) and “HPV” OR “Human papillomavirus” as subheadings. A similar search was also performed in Scopus and CINAHL. The search limits were: language (“English”), dates (articles published from “1st January 2000 to 31st December 2015”), and species (“Humans”). A total of 21,444 articles were obtained from these searches.
Furthermore, the result was narrowed down by adding the name of each LMIC as defined by the World Bank. According to the latest revision of World Bank, a total of 135 countries are listed as LMICs (The World Bank, 2016). Thus at the end of first stage, we obtained 2413 specific articles.
In the second stage we reviewed titles and abstracts using predefined screening criteria. Exclusion criteria were: studies outside of LMICs, studies with no information about cervical cancer, reviews, reports, and duplicates. If the required information was not available in the abstract, we stopped reviewing further. Studies not satisfying the inclusion criteria were excluded at this stage.
In the third stage, we used the following exclusion criteria for further filtering the 190 papers from stage two: full text not in English, full text not available, not prevalence/ incidence/ mortality study, study reporting pre-cancer. Finally, we obtained 20 papers which were selected for further review and analysis (Figure 1). The characteristics recorded for each study included: country of origin, author’s name and year of publication, study duration, age group, cervical cancer prevalence per 1000 per year, crude incidence, age standardized incidence rate, crude mortality, age standardized mortality rate per 100,000 per year and classification of cancer.
Ethical consideration
This article is based on published data, and hence ethical approval is not required.
Result
Characteristics of the studies
Detailed characteristics of the articles are presented in Table 1. The 20 articles that were included in the analysis were from 15 countries: Brazil (N=2) (Kalakun and Bozzetti, 2005; Gonzaga et al., 2013), China (N=3) (Chen, 2006; Du et al., 2015; Wang, 2015), Colombia (N=1) (Pineros et al., 2013), Cote D’ Ivore (N=1) (Echimane et al., 2000), Fiji (N=1) (Kuehn et al., 2012), India (N=2) (Dhillon et al., 2011; Dikshit et al., 2012), Jamaica (N=1) (Gibson et al., 2008), Malawi (N=1) (Banda et al., 2001), Mongolia (N=1) (Sandagdorj et al., 2010), Nigeria (N=1) (Durowade et al., 2012), Serbia (N=1) (Naumovic et al., 2015), Thailand (N=1) (Sriamporn et al., 2003), Tunisia (N=1) (Missaoui et al., 2010), Uganda (N=1) (Wabinga, 2002) and Zimbabwe (N=2) (Chokunonga et al., 2000; Chokunonga et al., 2013).
Table 1.
Study Characteristics
| Country | Study ID | Titles | Study duration | Age group (years) | CC prevalence per 1000 | CC crude Incidence per 100,000/ year | CC ASR Incidence per 100,000/ year | CC crude Mortality per 100,000/ year | CC ASR Mortality per 100,000/ year | Classification of cancer |
|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | Gonzaga CMR (2013) | Cervical cancer mortality trends in Brazil: 1980-2009 | 2005-09 | >20 | NR | NR | NR | NR | 4.8 | NR |
| Brazil | Kalakun L (2005) | Evolution of uterine cervical cancer mortality from 1979 to 1998 in the State of Rio Grande do Sul, Brazil | 1979-98 | 15-74 | NR | NR | NR | 7.58 | NR | NR |
| China | Du PL (2015) | Cervical Cancer Mortality Trends in China, 1991-2013, and Predictions for the Future | 1991-2000 | 15-85 | NR | 13.4 | 10.4 | NR | 2.59 | ICD-10 |
| China | Chen JG (2006) | Trends in the incidence of cancer in Qidong, China, 1978–2002 | 5 yrs 1998-2002 | NR | NR | 0.14 | 0.11 | NR | NR | ICD-10 |
| China | Wang T (2015) | A Populationbased Study of Invasive Cervical Cancer Patients in Beijing: 1993–2008 | 1 year 2008 | 0-70+ | NR | 0.65 | NR | 0.1 | NR | ICD-10 |
| Colombia | Pineros M (2013) | Patterns and trends in cancer mortality in Colombia 1984–2008 | 1984-2008 | NR | NR | NR | NR | NR | 1.8 | NR |
| Cote D’ Ivore | Echimane AK (2000) | Cancer Incidence in Abidjan, Ivory Coast | 1995–97 | 15-75+ | NR | 2.75 | NR | NR | NR | ICD-10 |
| Fiji | Kuehn R (2012) | Cervical cancer incidence and mortality in Fiji 2003–2009 | 2003-2009 | 0-65+ | NR | NR | 3.94 | NR | 3.98 | NR |
| India | Dhillon PK (2011) | Trends in breast, ovarian and cervical cancer incidence in Mumbai, India over a 30-year period, 1976–2005: an age–period–cohort analysis | 5 yrs 2001-05 | 30–64 | NR | NR | 5.32 | NR | NR | ICD-10 |
| India | Dikshit R (2015) | Cancer mortality in India: a nationally representative survey | 2001-03 | 30-69 | NR | NR | NR | NR | 16 | ICD-10 |
| Jamaica | Gibson TN (2010) | Age-Specific Incidence of Cancer in Kingston and St Andrew, Jamaica, 2003 – 2007 | 5 yrs 2003-07 | 0-85+ | NR | 3.48 | 3.48 | NR | NR | ICD-9 |
| Malawi | Banda LT (2001) | Cancer incidence in Blantyre, Malawi 1994-1998 | 5 yrs 1994-98 | 0-65+ | NR | 2.76 | 5.24 | NR | NR | ICD-10 |
| Mongolia | Sandagdorj T (2010) | Cancer Incidence and Mortality in Mongolia - National Registry Data | 2003-07 | 0-65 | NR | 4.36 | 5.08 | 1.45 | 1.89 | NR |
| Nigeria | Durowade KA (2012) | Prevalence and risk factors of cervical cancer among women in an urban community of Kwara State, North Central Nigeria | NR | 25-64 | 5 | NR | NR | NR | NR | ICD-10 |
| Serbia | Naumovic T (2015) | Mortality from cervical cancer in Serbia in the period 1991-2011 | 1991-2011 | 35-75+ | NR | NR | NR | 12.71 | 6.92 | NR |
| Thailand | Sriamporn S (2003) | Cervix Cancer in Khon Kaen, Northeast Thailand, 1985-1999 | 5 yrs 1995-99 | 0-75+ | NR | 3.2 | 3.24 | NR | NR | NR |
| Tunisia | Missaoui N (2010) | Cervical Adenocarcinoma and Squamous Cell Carcinoma Incidence Trends among Tunisian Women | 14 yrs 1996-2003 | 23-85 | NR | 0.41 | 0.49 | NR | NR | ICD 10 |
| Uganda | Wabinga HR (2010) | Trends in the incidence of cancer in Kampala, Uganda | 5 yrs 2006-10 | 0-65+ | NR | NR | 10.04 | NR | NR | ICD-10 |
| Zimbabwe | Chokunonga E (2000) | Cancer incidence in the African population of Harahare, Zimbabwe: second results from the cancer registry 1993-1995 | 3 yrs 1993-95 | 0-65+ | NR | 6.07 | 17.93 | NR | NR | ICD-10 |
| Zimbabwe | Chokunonga E (2013) | Trends in the incidence of cancer in the black population of Harare, Zimbabwe 1991–2010 | 1991-2010 | 0-75+ | NR | NR | 15.74 | NR | NR | ICD-10 |
NR, Not Reported
Cervical cancer prevalence and risk factor
Only one study reported prevalence as 5.0 per 1000 in 2012 (Durowade et al., 2012) in Nigeria. In addition, the study reported coitarche, tobacco smoking, number of sexual partners and family history of cervical cancer as significant risk factors (Durowade et al., 2012).
Cervical cancer incidence
Ten studies reported cervical cancer crude incidence (Chokunonga et al., 2000; Echimane et al., 2000; Banda et al., 2001; Sriamporn et al., 2003; Chen, 2006; Gibson et al., 2008; Missaoui et al., 2010; Sandagdorj et al., 2010; Du et al., 2015; Wang, 2015) whereas 12 studies reported age standardized incidence rate (Chokunonga et al., 2000; Banda et al., 2001; Wabinga, 2002; Sriamporn et al., 2003; Chen, 2006; Gibson et al., 2008; Missaoui et al., 2010; Sandagdorj et al., 2010; Dhillon et al., 2011; Kuehn et al., 2012; Chokunonga et al., 2013; Du et al., 2015). The crude incidence rate was reported highest as 13.4/100,000/year in 2015 (Du et al., 2015) and lowest as 0.14/100,000/year in 2006 (Chen, 2006) in China (Figure 2). Age standardized incidence rate was reported highest as 17.93/100,000/year in Zimbabwe in 2000 (Chokunonga et al., 2000) and lowest as 0.11/100,000/year in China in 2006 (Chen, 2006).
Figure 2.
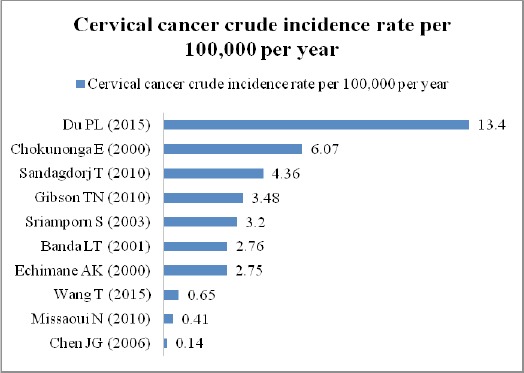
Cervical Cancer Crude Incidence Rate Per 100,000 Per Year.
Cervical cancer mortality
Four studies reported cervical cancer crude mortality rate (Kalakun and Bozzetti, 2005; Sandagdorj et al., 2010; Naumovic et al., 2015; Wang, 2015) whereas seven studies reported age standardized mortality rate (Sandagdorj et al., 2010; Dikshit et al., 2012; Kuehn et al., 2012; Gonzaga et al., 2013; Pineros et al., 2013; Du et al., 2015; Naumovic et al., 2015). The crude mortality rate was reported highest as 12.71/100,000/year in 2015 in Serbia (Naumovic et al., 2015) and lowest as 0.1/100,000/year in 2015 in China (Wang, 2015) (Figure 3). Age standardized mortality rate was reported highest as 16/100,000/year in India in 2015 (Dikshit et al., 2012) and lowest as 1.8/100,000/year in Colombia in 2013 (Pineros et al., 2013).
Figure 3.
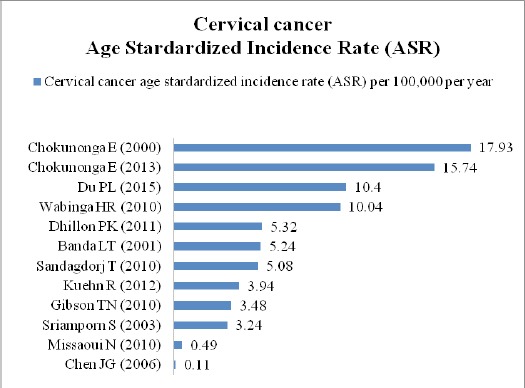
Cervical Cancer Age Standardized Incidence Rate Per 100,000 Per Year.
Figure 4.
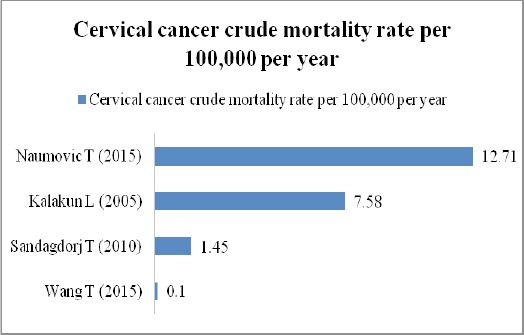
Cervical Cancer Crude Mortality Rate Per 100,000 Per Year.
Figure 5.
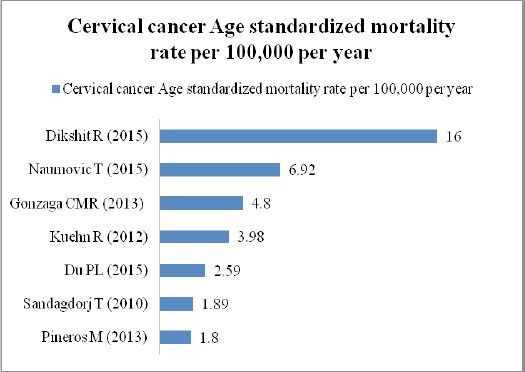
Cervical Cancer Age Standardized Mortality Rate Per 100,000 Per Year.
Discussion
This review is the first comprehensive report of prevalence, incidence and mortality of cervical cancer in LMICs. Among the 20 studies reviewed; seven studies were from Africa (Chokunonga et al., 2000; Echimane et al., 2000; Banda et al., 2001; Wabinga, 2002; Gibson et al., 2008; Missaoui et al., 2010; Durowade et al., 2012; Chokunonga et al., 2013), seven from Asia (Sriamporn et al., 2003; Chen, 2006; Sandagdorj et al., 2010; Dhillon et al., 2011; Dikshit et al., 2012; Du et al., 2015; Wang, 2015), three studies were from South America (Kalakun and Bozzetti, 2005; Gonzaga et al., 2013); (Pineros et al., 2013) one study from North America (Gibson et al., 2008) one from Europe (Naumovic et al., 2015) and one from Oceania (Kuehn et al., 2012). The findings of the review give a strong imperative for further studies on cervical cancer prevalence, incidence and mortality in LMICs, where the disease burden is substantial.
Only one study, one from Nigeria reported prevalence as 5.0 per 1,000 in 2012 in age group 25-64 (Durowade et al., 2012). Whereas, the IARC country specific estimate for cervical cancer prevalence for Nigeria was 15.6 per 1,000 per year (Bray et al., 2013). Further, the study from Nigeria reported coitarche, tobacco smoking, number of sexual partners and family history of cervical cancer as significant risk factors (Durowade et al., 2012). There is strong epidemiologic evidence indicating that HPV is the major etiology of cervical cancer (Bosch et al., 1995; Chichareon et al., 1998). In addition, the onset of sexual intercourse at an early age and a greater number of lifetime sexual partners raises the risk of cervical cancer (Brinton et al., 1987). Furthermore, long-term use of oral contraceptives may be a cofactor that increases risk of cervical cancer by up to four-fold in women who are positive for cervical HPV DNA (Moreno et al., 2002). Another of the reviewed studies reported that high parity and poor genital hygiene conditions were the main co-factors for cervical cancer in the population with prevalent HPV infections (Bayo et al., 2002). Therefore, the role of persistent infection with oncogenic types of HPV in the etiology of cervical cancer has encouraged the evaluation of HPV testing as a screening tool (IARC, 1995; Bosch et al., 2002; Franco, 2003). Cigarette smoking is the only nonsexual behavior consistently and strongly correlated with cervical cancer, independently increasing risk two- to four fold (Winkelstein, 1990).
In the absence of a nationwide screening program, there are disparities in screening, treatment, and ultimately survival. The variation in study population, sample size and time frame have shown variation in the reported incidence in our review (Chokunonga et al., 2000; Banda et al., 2001; Wabinga, 2002; Sriamporn et al., 2003; Chen, 2006; Gibson et al., 2008; Missaoui et al., 2010; Sandagdorj et al., 2010; Dhillon et al., 2011; Kuehn et al., 2012; Chokunonga et al., 2013; Du et al., 2015) and the IARC country specific estimates of cervical cancer (Ferlay et al., 2013). The highest age standardized incidence rate is 17.93/100,000/year in Zimbabwe in 2000 which is one of the countries in East Africa having the highest cervical cancer incidence rates.
The age standardized mortality rate was reported highest as 16/100,000/year in India in 2015 among the other LMICs (Pineros et al., 2013). Also, India has the highest age standardized mortality rates in South-East Asia followed by Myanmar and Nepal (Ferlay et al., 2013). An analysis of population-based surveys indicates that coverage of cervical cancer screening in developing countries is 19% compared to 63% in developed countries and ranges from 1% in Bangladesh to 73% in Brazil (Gakidou E, 2009). Studies have shown that population based screening programs may be an effective method to prevent cervical cancer deaths also in developing countries (Sankaranarayanan et al., 2007). According to the WHO, 80% to 100% coverage of the target population with Pap smear screening, adequate diagnosis and treatment would allow a 60% to 90% reduction in cervical cancer (Boyle and Levin, 2008). A large cluster randomized trial from India shows that a single round of HPV screening can significantly reduce the numbers of advanced cervical cancers and deaths from cervical cancer in a low resource setting (Sankaranarayanan et al., 2009). In addition, studies confirm that vaccination programs containing the seven most common HPV types would prevent about 87% of cervical cancer worldwide (Munoz et al., 2004).
Unfortunately, the majority of women in developing countries still do not have access to cervical cancer prevention programmes which is resulting in increased cervical cancer disease burden (Ferlay et al., 2013). Furthermore, low adherence among women regarding screening and diagnosis of chronic non-communicable diseases has been one of the most important factor to be considered for cervical cancer screening and diagnosis in LMICs (Hodgkins and Orbell, 1998; Floyd et al., 2000), (Shrestha et al., 2013).
Limitations
Our study is limited to MEDLINE, CINAHL and Scopus database searches. Thus, it may not cover all the studies conducted in this field; particularly those published in non-indexed local journals, non-English publications, and open access platforms not covered by MEDLINE, CINAHL and Scopus. Moreover, we did not assess the publication bias of the articles, as it is not relevant in context of prevalence, incidence and mortality studies. There are chances of considerable under reporting in the prevalence or incidence or mortality rates in our study particularly since the capacity for cancer diagnosis and data capture is limited in LMICs.
In conclusion, the review reported prevalence of cervical cancer as 5.0 per 1,000 in 2012 in Nigeria among the age group 25-64 years and the highest age standardized incidence rate as 17.93/100,000/year in Zimbabwe in 2,000 and lowest as 0.11/100,000/year in China in 2006. Further, the age standardized mortality rate was reported highest as 16/100,000/year in India in 2015 and lowest as 1.8/100,000/year in Colombia in 2013. This review provides useful information for the future prevention and clinical management guidelines on cervical cancer in LMICs, but more importantly reveals the substantial need for further studies on cervical cancer prevalence, incidence and mortality with associated risk factors in LMICs.
Conflict of Interest
The authors have no conflict of interest.
References
- Banda LT, Parkin DM, Dzamalala CP, et al. Cancer incidence in Blantyre, Malawi 1994-1998. Trop Med Int Health. 2001;6:296–304. doi: 10.1046/j.1365-3156.2001.00707.x. [DOI] [PubMed] [Google Scholar]
- Bayo S, Bosch X, Sanjose SD, et al. Risk factos of invasive cervical cancer in Mali International. J Epidemiol. 2002;31:202–9. doi: 10.1093/ije/31.1.202. [DOI] [PubMed] [Google Scholar]
- Bosch FX, Lorincz A, Munoz N, et al. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55:244–65. doi: 10.1136/jcp.55.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch FX, Manos MM, Muñoz N, et al. Prevalence of human papillomavirus in cervical cancer:a worldwide perspective. J Natl Cancer Inst. 1995;87:796–802. doi: 10.1093/jnci/87.11.796. [DOI] [PubMed] [Google Scholar]
- Boyle P, Levin B. World cancer report 2008. International agency for research on cancer. 2008:288–90. [Google Scholar]
- Bray F, Ren JS, Masuyer E, et al. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer. 2013;132:1133–45. doi: 10.1002/ijc.27711. [DOI] [PubMed] [Google Scholar]
- Brinton LA, Hamman RF, Huggins GR, et al. Sexual and reproductive risk factors for invasive squamous cell cervical cancer. J Natl Cancer Inst. 1987;79:23–30. [PubMed] [Google Scholar]
- Chen JG. Trends in the incidence of cancer in Qidong, China, 1978–2002. Int J Cancer. 2006;119:1447–54. doi: 10.1002/ijc.21952. [DOI] [PubMed] [Google Scholar]
- Chichareon S, Herrero R, Munoz N, et al. Risk factors for cervical cancer in Thailand:a Case–control study. J Nat Cancer Inst. 1998;90:50–7. doi: 10.1093/jnci/90.1.50. [DOI] [PubMed] [Google Scholar]
- Chokunonga E, Borok MZ, Chirenje ZM, et al. Trends in the incidence of cancer in the black population of Harare, Zimbabwe 1991-2010. Int J Cancer. 2013;133:721–9. doi: 10.1002/ijc.28063. [DOI] [PubMed] [Google Scholar]
- Chokunonga E, Levy LM, Bassett MT, et al. Cancer incidence in the African population of Harare, Zimbabwe:second results from the cancer registry 1993-1995. Int J Cancer. 2000;85:54–9. doi: 10.1002/(sici)1097-0215(20000101)85:1<54::aid-ijc10>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Dhillon PK, Yeole BB, Dikshit R, et al. Trends in breast, ovarian and cervical cancer incidence in Mumbai, India over a 30-year period, 1976-2005:an age-period-cohort analysis. Br J Cancer. 2011;105:723–30. doi: 10.1038/bjc.2011.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dikshit R, Gupta PC, Ramasundarahettige C, et al. Cancer mortality in India:a nationally representative survey. Lancet. 2012;379:1807–16. doi: 10.1016/S0140-6736(12)60358-4. [DOI] [PubMed] [Google Scholar]
- Du PL, Wu KS, Fang JY, et al. Cervical cancer mortality trends in China, 1991-2013, and predictions for the future. Asian Pac J Cancer Prev. 2015;16:6391–6. doi: 10.7314/apjcp.2015.16.15.6391. [DOI] [PubMed] [Google Scholar]
- Durowade KA, Osagbemi GK, Salaudeen AG, et al. Prevalence and risk factors of cervical cancer among women in an urban community of Kwara State, north central Nigeria. J Prev Med Hyg. 2012;53:213–9. [PubMed] [Google Scholar]
- Echimane AK, Ahnoux AA, Adoubi I, et al. Cancer incidence in Abidjan, Ivory Coast:first results from the cancer registry, 1995-1997. Cancer. 2000;89:653–63. doi: 10.1002/1097-0142(20000801)89:3<653::aid-cncr22>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Soerjomataram I, Ervik M, et al. 'Globocan 2012 v1.0, cancer incidence and mortality worldwide:IARC cancerbase No. 11 [Internet].'. Lyon: International agency for research on cancer; 2013. [accessed on 29/05/2016]. Available from: http://globocan.iarc.fr . [Google Scholar]
- Floyd DL, Prentice-Dunn S, Rogers RW. A meta-analysis of research on protection motivation theory. J Appl Soc Psychol. 2000;30:407–29. [Google Scholar]
- Franco EL. Primary screening of cervical cancer with human papillomavirus tests. J Natl Cancer Inst Monogr. 2003;31:89–96. doi: 10.1093/oxfordjournals.jncimonographs.a003488. [DOI] [PubMed] [Google Scholar]
- Fritz PA, Percy C, Jack A, et al. International classification of diseases for oncology. third edition. Geneva: World Health Organization; 2000. pp. 58–9. [Google Scholar]
- Gakidou E SN, Ziad O. Coverage of cervical cancer screening in 57 countries:low average levels and large inequalities. PloS Med. 2009;5:e132. doi: 10.1371/journal.pmed.0050132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson TN, Blake G, Hanchard B, et al. Age-specific incidence of cancer in Kingston and St Andrew, Jamaica, 1998-2002. West Indian Med J. 2008;57:81–9. [PubMed] [Google Scholar]
- Gonzaga CM, Freitas-Junior R, Barbaresco AA, et al. Cervical cancer mortality trends in Brazil 1980-2009. Cad Saude Publica. 2013;29:599–608. doi: 10.1590/s0102-311x2013000300017. [DOI] [PubMed] [Google Scholar]
- Hodgkins S, Orbell S. Can protection motivation theory predict behavior? A longitudinal test exploring the role of previous behaviour. Psychol Health. 1998;13:237–50. [Google Scholar]
- IARC. IARC monographs on the evaluation of carcinogenic risks to humans, Human papillomaviruses. IARC Monographs, 64. Lyon: IARC Press; 1995. pp. 88–89. [PMC free article] [PubMed] [Google Scholar]
- Kalakun L, Bozzetti MC. Evolution of uterine cervical cancer mortality from 1979 to 1998 in the State of Rio Grande do Sul, Brazil. Cad Saude Publica. 2005;21:299–309. doi: 10.1590/s0102-311x2005000100033. [DOI] [PubMed] [Google Scholar]
- Kuehn R, Fong J, Taylor R, et al. Cervical cancer incidence and mortality in Fiji 2003-2009. Aust N Z J Obstet Gynaecol. 2012;52:380–6. doi: 10.1111/j.1479-828X.2012.01461.x. [DOI] [PubMed] [Google Scholar]
- Missaoui N, Trabelsi A, Landolsi H, et al. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among Tunisian women. Asian Pac J Cancer Prev. 2010;11:777–80. [PubMed] [Google Scholar]
- Moreno V, Bosch FX, Muñoz N, et al. Effect of oral contraceptives on risk of cervical cancer in women with human papillomavirus infection:the IARC multicentric casecontrol study. Lancet Oncol. 2002;359:1085–192. doi: 10.1016/S0140-6736(02)08150-3. [DOI] [PubMed] [Google Scholar]
- Munoz N, Bosch FX, Castellsague X, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer. 2004;111:278–85. doi: 10.1002/ijc.20244. [DOI] [PubMed] [Google Scholar]
- Naumovic T, Miljus D, Djoric M, et al. Mortality from cervical cancer in Serbia in the period 1991-2011. J BUON. 2015;20:231–4. [PubMed] [Google Scholar]
- Pineros M, Gamboa O, Hernandez-Suarez G, et al. Patterns and trends in cancer mortality in Colombia 1984-2008. Cancer Epidemiol. 2013;37:233–9. doi: 10.1016/j.canep.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Sandagdorj T, Sanjaajamts E, Tudev U, et al. Cancer incidence and mortality in Mongolia - National Registry Data. Asian Pac J Cancer Prev. 2010;11:1509–14. [PubMed] [Google Scholar]
- Sankaranarayanan R, Esmy PO, Rajkumar R, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India:a cluster-randomised trial. Lancet. 2007;370:398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385–94. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- Schiffman M, Castle PE, Jeronimo J, et al. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- Shrestha AD, Kosalram K, Gopichandran V. Gender difference in care of type 2 diabetes. J Nepal Med Assoc. 2013;52:245–50. [PubMed] [Google Scholar]
- Sriamporn S, Pengsaa P, Hakama M, et al. Cervix cancer in Khon Kaen, northeast Thailand, 1985-1999. Asian Pac J Cancer Prev. 2003;4:312–8. [PubMed] [Google Scholar]
- Syrjanen K, Hakama M, Saarikoski S, et al. Prevalence, incidence, and estimated life-time risk of cervical human papillomavirus infections in a nonselected Finnish female population. Sex Transm Dis. 1990;17:15–9. [PubMed] [Google Scholar]
- The World Bank. World bank country and lending groups, country classification. 2016. [accessed 29/05/2016]. Available from: http://data.worldbank.org/about/country-and-lending-groups .
- Wabinga HR. Pattern of cancer in Mbarara, Uganda. East Afr Med J. 2002;79:193–7. doi: 10.4314/eamj.v79i4.8877. [DOI] [PubMed] [Google Scholar]
- Wang T. A population-based study of invasive cervical cancer patients in Beijing 1993–2008. Chin Med J. 2015;128:3298–3304. doi: 10.4103/0366-6999.171420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelstein W. Smoking and cervical cancer - current status:a review. Am J Epidemiol. 1990;131:945–57. doi: 10.1093/oxfordjournals.aje.a115614. [DOI] [PubMed] [Google Scholar]


