Abstract
Objective:
The Melanoma Screening Day Campaign started in the Russian Federation in 2006. In the present study, we analyzed the 2015-2016 survey questionnaire data acquired from screened individuals in the city of Krasnoyarsk in eastern Siberia, which has a population of one million, in order to understand the level of awareness regarding melanoma/skin cancer prevention and early diagnosis.
Methods:
Individuals were enrolled in the screening campaign by mass media advertising. Free whole-body examinations were provided by the doctors, and the standardized questionnaire forms (n=444) were completed to obtain relevant demographic, epidemiological, and clinical data. Descriptive and univariate analyses were conducted to elucidate the main characteristics of the screened population. Percentage frequency was used to characterize the population.
Result:
A substantial proportion of the screened individuals were female (80%). The most common reasons for participating in the screening were a high number of moles, or a change in the appearance of the moles. Internet recourses were the main channel for obtaining the information about the Melanoma Day Screening Campaign. 5% of screened individuals had a family history of melanoma/skin cancer. The mean age of the participants was 36.63±16.31 years. The percentage of screened individuals who took part in this program increased in 2016 (18%) versus 2015 (8%). In total, 5 individuals with suspected melanoma/skin cancer were identified during the two-year Campaign, all of whom were referred to the regional oncology center.
Conclusion:
The analysis of data from the Melanoma Screening Day Campaign in Krasnoyarsk Krai revealed the necessity to use the media to attract older subjects with potential melanoma/skin cancer risk to undergo screening. Individuals with suspected malignancies should be monitored up until the time when a final diagnosis is determined. Moreover, such events are an appropriate way to inform and educate the public about cutaneous cancer prevention.
Keywords: Melanoma, nevi, screening, Siberia-Russian Federation
Introduction
Melanoma incidence rates are rising in the Russian Federation, as shown by the 17.27% increase between 2004 and 2014, reaching a incidence of 4.14 cases per 100,000 individuals in 2014. Although melanoma incidence rates in the Russian Federation are lower than those in western European countries, the mortality rates continue to grow, highlighting the importance of prevention and early diagnosis of this disease. In the Russian Federation, standardized melanoma mortality rates increased from 1.3 to 1.51 per 100,000 individuals between 2004 and 2014 (Kaprin et al., 2015). Melanoma survival rates are dependent on the disease stage, which corresponds to primary tumor thickness. Therefore, early diagnosis is crucial for patient prognosis.
In 1999 the Euromelanoma Screening Day Campaign was established by dermatological societies to draw public attention to skin cancer and the early symptoms of melanoma, and to increase diagnoses of melanoma/skin cancer in the early stages (van der Leest et al., 2011). The Russian Federation joined this project in 2006 under supervision of the National Alliance of Dermatologists and Cosmetologists. Information about the campaign is usually announced through various media outlets and poster advertisements in public areas.
Krasnoyarsk is a city with a population of one million people, predominantly of Caucasian origin, and is located in eastern Siberia in the Russian Federation. The Melanoma Screening Day Campaign has been carried out here since 2007. To evaluate the results of this screening campaign in 2015-2016, we analyzed the responses from the questionnaire-based survey obtained from the screened individuals.
Materials and Methods
Subjects
The Melanoma Screening Day Campaign was carried out in accordance with the ethical standards of the Krasnoyarsk State Medical University (the local ethics committee on human experimentation), and with the Helsinki Declaration.
The screening was performed in the outpatient departments of regional dermatovenereology and oncology hospitals, and private clinics. Free-of-charge consultations were provided by dermatologists or oncologists, since skin cancer patients in Russia are treated by oncologists in specialized regional oncology centers. The public was informed in advance about the campaign and any individual willing to undergo skin examination by the specialist was free to book the appointment with a doctor via the websites of the Melanoma Screening Day Campaign or the relevant hospital.
During their visit to the doctor on the day of screening, the patients were required to complete the first part of the questionnaire, where their birthdate, gender, and education were indicated. They were also asked about how they obtained information about the project, their sunbathing habits, and any previous personal or family history of melanoma/skin cancer. The doctor then performed a skin examination and completed the remainder of the screening for with information regarding nevus count, presence of lentigo, dysplastic nevi, seborrheic keratomas, skin cancer, etc. The patients with lesions suspected of being skin cancer were referred to oncologists, and special information was provided in the questionnaire (name of oncologist and medical center for referral).
Copies of the questionnaires were analyzed and the data were statistically processed using Statistica software version 7.0 (Statsoft, Moscow, Russia). Percentage frequency was used to characterize the population. Quantitative data were expressed as mean values ± standard deviation (SD). Categorical variables described as percentages were compared using Chi-Square analysis. P-values less than 0.05 were considered to be significant.
Results
In total, 199 individuals visited doctors during the Melanoma Screening Day Campaign in 2015, while 245 participants were recorded in 2016. Females accounted for 78% of all the participants in 2015, and 83% in 2016. The mean age of the participants was 36.63±16.31 years, with a range of 0.2-78 years. Most of the screened individuals were 20-49 years old, both in 2015 and 2016 (63% and 64%, respectively) (Table 1), and were holders of higher educational qualifications (68% and 65% respectively). The percentage of participants aged ≥65 years increased from 3.0% in 2015 to 7.3% in 2016. The most common reasons for participating in the screening were a large number of moles (58%), and changes in mole appearance or appearance of new moles (42% in 2015 and 37% in 2016). In addition, 15% of participants indicated the need for general skin examinations as the reason to attend the screening in both years. In 2015, 8% of the respondents indicated their previous participation in the Melanoma Screening Day Campaign, whereas the number of such individuals increased to 18% in 2016. Internet resources were specified by respondents as the most frequent route of acquiring information about the campaign (46% in 2015 and 41% in 2016), although the number of individuals who were advised by doctors to participate in the screening was more than doubled in 2016 as compared with 2015 (Table 2). Although the number of doctors who participated in the program decreased in 2016, the number of individuals screened per doctor increased (Figure 1).
Table 1.
Data of Individuals Examined During the Melanoma Day Screening Campaign.
| 2015, | 2016, | Total, | P-value† | ||
|---|---|---|---|---|---|
| n = 199 (100%) | n = 245 (100%) | n = 444 (100%) | 2015 vs 2016 | ||
| Gender | Male | 38 (19.1%) | 37 (15.1%) | 75 (16.9%) | 0.16 |
| Female | 156 (78.4%) | 204 (83.3%) | 360 (81.1%) | 0.12 | |
| Not mentioned | 5 (2.5%) | 4 (1.6%) | 9 (2.0%) | 0.37 | |
| Age | 0-19 | 29 (14.6%) | 32 (13.1%) | 61 (13.7%) | 0.37 |
| 20-34 | 63 (31.7%) | 82 (33.4%) | 145 (32.7%) | 0.38 | |
| 35-49 | 62 (31.2%) | 75 (30.6%) | 137 (30.9%) | 0.49 | |
| 50-64 | 37 (18.6%) | 38 (15.5%) | 75 (16.9%) | 0.23 | |
| 65+ | 6 (3.0%) | 18 (7.3%) | 24 (5.4%) | 0.03 | |
| Not mentioned | 2 (1.0%) | 0% (0.0) | 2 (0.5%) | 0.2 | |
| Skin phototype | I | 22 (11.0%) | 10 (4.1%) | 32 (7.2%) | 0.004 |
| II | 25 (12.6%) | 46 (18.8%) | 71 (16.0%) | 0.049 | |
| III | 68 (34.2%) | 99 (40.4%) | 167 (37.6%) | 0.12 | |
| IV | 74 (37.2%) | 73 (29.8%) | 147 (33.1%) | 0.04 | |
| Not mentioned | 10 (5.0%) | 17 (7.0%) | 27 (6.1%) | 0.26 |
Compared using Chi-Square analysis; P<0.05 was considered significant.
Table 2.
Sources of Information on the Melanoma Day Screening Campaign, the Individuals’ Reasons for Attending Screening, and Previous Participation in Similar Campaigns
| 2015, | 2016, | Total, | P-value† | ||
|---|---|---|---|---|---|
| n = 199 (100%) | n = 245 (100%) | n = 444 (100%) | 2015 vs 2016 | ||
| Distributions of sources of information on Melanoma Day Screening Campaign | Drugstore | 39 (19.6%) | 24 (9.8%) | 63 (14.2%) | 0.003 |
| Doctor | 21 (10.6%) | 61 (24.9%) | 82 (18.5%) | 0.0001 | |
| Internet | 91 (45.7%) | 100 (40.8%) | 191 (43%) | 0.19 | |
| Press | 5 (2.5%) | 3 (1.2%) | 8 (1.8%) | 0.26 | |
| Other | 40 (20.1%) | 52 (21.2%) | 92 (20.7%) | 0.43 | |
| Not mentioned | 3 (1.5%) | 5 (2.0%) | 8 (1.8%) | 0.48 | |
| Reasons for attending | High amount of moles | 144 (57.3%) | 142 (58%) | 156 (57.7%) | 0.48 |
| Change in mole | 84 (42.2%) | 91 (37.1%) | 175 (39.4%) | 0.16 | |
| Personal history of melanoma/skin cancer | 3 (1.5%) | 3 (1.2%) | 6 (1.4%) | 0.56 | |
| Family history of melanoma/skin cancer | 6 (3%) | 7 (2.9%) | 13 (2.9%) | 0.57 | |
| General skin examination | 29 (14.6%) | 38 (15.5%) | 67 (15.1%) | 0.45 | |
| Not mentioned | 1 (0.5%) | 1 (0.4%) | 2 (0.5%) | 0.7 | |
| Previous skin cancer screening | None | 180 (90.5%) | 200 (81.6%) | 380 (85.6%) | 0.01 |
| Yes | 16 (8.0%) | 44 (18.0%) | 60 (13.5%) | 0.002 | |
| Unknown | 3 (1.5%) | 1 (0.4%) | 4 (0.9%) | 0.24 |
Compared using Chi-Square analysis; P<0.05 was considered significant.
Figure 1.
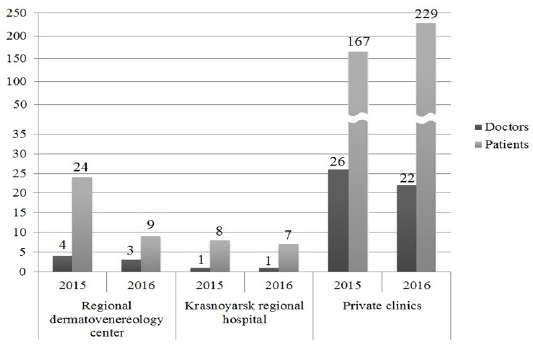
Number of Participating Hospitals and Centers, Number of Doctors and Individuals per Center who Took Part in the Melanoma Day Screening Campaign.
The occupation or common leisure interests of the vast majority of screened individuals were not related to outdoor activities (Table 3). In 2015 and 2016, 37% and 30% of individuals were of skin phototype IV, respectively, 34% and 40% of individuals were of skin phototype III, and 12.6% and 18.8% of individuals were of skin phototype II, respectively; the percentage of participants with skin phototype I decreased in 2016 compared with 2015, accounting for 4.1% of participants. Some of the respondents (47%) mentioned a history of severe sunburns when they were <18 years of age. Only 6% of the individuals never went sunbathing, while >80% of participants never used solariums. In addition, 13.6% of respondents in 2015 and 11.4% in 2016 never used sunscreens during sunbathing. In total, 5% of screened individuals had a family history of melanoma/skin cancer, and 3% had themselves been diagnosed with melanoma/skin cancer. In 2016, 4% of the respondents did not answer whether or not they had been diagnosed with melanoma/skin cancer previously.
Table 3.
Sun Exposure Habits and Melanoma Risk Factors of Screened Individuals
| 2015, | 2016, | Total, | P-value† | ||
|---|---|---|---|---|---|
| n = 199 (100%) | n = 245 (100%) | n = 444 (100%) | 2015 vs 2016 | ||
| Outdoor occupation or frequent outdoor activities | Not related | 162 (81.4%) | 214 (87.3%) | 376 (84.7%) | 0.06 |
| Yes, but duration not mentioned | 5 (2.5%) | 1 (0.4%) | 6 (1.4%) | 0.07 | |
| Yes, within 1 year or less | 3 (1.5%) | 3 (1.2%) | 6 (1.4%) | 0.56 | |
| Yes, more than 1 year but less than 5 years | 10 (5.0%) | 7 (2.9%) | 17 (3.8%) | 0.17 | |
| Yes, more than 5 year but less than 10 years | 7 (3.5%) | 5 (2.0%) | 12 (2.7%) | 0.25 | |
| Yes, more than 10 years | 11 (5.5%) | 9 (3.7%) | 20 (4.5%) | 0.24 | |
| Not mentioned | 1 (0.5%) | 6 (2.4%) | 7 (1.6%) | 0.1 | |
| Use of sunscreens | Never | 27 (13.6%) | 28 (11.4%) | 55 (12.4%) | 0.29 |
| Sometimes | 102 (51.3%) | 155 (63.3%) | 257 (57.9%) | 0.01 | |
| Always | 48 (24.1%) | 43 (17.6%) | 91 (20.5%) | 0.06 | |
| Never go sunbathing | 13 (6.5%) | 13 (5.3%) | 26 (5.90%) | 0.36 | |
| Not mentioned | 9 (4.5%) | 6 (2.5%) | 15 (3.4%) | 0.17 | |
| Painful sunburn erythema (2 days or longer) before 18 years old | None | 76 (38.2%) | 82 (33.5%) | 158 (35.6%) | 0.18 |
| Yes | 88 (44.2%) | 119 (48.6%) | 207 (46.6%) | 0.21 | |
| Don’t remember | 29 (14.6%) | 40 (16.3%) | 69 (15.5%) | 0.29 | |
| Not mentioned | 6 (3%) | 4 (1,6%) | 10 (2.3%) | 0.26 | |
| Use of solarium | None | 176 (88.4%) | 210 (85.7%) | 386 (86.9%) | 0.24 |
| Yes, less than 20 times per year | 17 (8.5%) | 22 (9.0%) | 39 (8.8%) | 0.5 | |
| Yes, more than 20 times per year | 3 (1.5%) | 4 (1.6%) | 7 (1.6%) | 0.61 | |
| Not mentioned | 3 (1.5%) | 9 (3.7%) | 12 (2.7%) | 0.13 | |
| Family history of melanoma | None | 178 (89.4%) | 212 (86.5%) | 390 (87.8%) | 0.22 |
| Yes, one of the relatives | 12 (6.0%) | 10 (4.1%) | 22 (5.0%) | 0.23 | |
| Yes, more than two relatives | 0 (0.0%) | 1 (0.4%) | 1 (0.2%) | 0.55 | |
| Unknown | 5 (2.5%) | 14 (5.7%) | 19 (4.3%) | 0.08 | |
| Not mentioned | 4 (2.0%) | 8 (3.3%) | 12 (2.7%) | 0.31 | |
| Personal history of skin cancer | None | 189 (95%) | 216 (88.2%) | 405 (91.2) | 0.01 |
| Melanoma | 2 (1.0%) | 4 (1.6%) | 6 (1.4%) | 0.44 | |
| Non-melanoma skin cancer | 2 (1.0%) | 5 (2.0%) | 7 (1.6%) | 0.32 | |
| Unknown | 0 (0.0%) | 10 (4.1%) | 10 (2.3%) | 0.003 | |
| Non-cutaneous malignancies | 4 (2.0%) | 2 (0.8%) | 6 (1.4%) | 0.25 | |
| Not mentioned | 2 (1.0%) | 8 (3.3%) | 10 (2.3%) | 0.1 |
Compared Using Chi-Square Analysis; P<0.05, Was Considered Significant.
In 2015 and 2016, 83% and 90.6% of individuals, respectively, were examined with the use of a dermatoscope. The total nevus count in 87% of the screened individuals was <50. Lesions that were designated as dysplastic nevi were found in 18% of the screened participants. 27% of patients were diagnosed as having seborrheic keratosis. Altogether, within the 2-year survey, non-melanoma skin cancer and melanoma were suspected in 5 patients, who were subsequently referred to the regional oncology center for further examination and appropriate treatment (Table 4).
Table 4.
Clinical Findings in Screened Individuals
| 2015, | 2016, | Total, | P-value†, | ||
|---|---|---|---|---|---|
| n = 199 (100%) | n = 245 (100%) | n = 444 (100%) | 2015 vs 2016 | ||
| Number of melanocytic nevi | <25 | 136 (68.3%) | 160 (65.3%) | 296 (66.7%) | 0.28 |
| 25-50 | 44 (22.1%) | 48 (19.6%) | 92 (20.7%) | 0.3 | |
| 50-100 | 9 (4.5%) | 16 (6.5%) | 25 (5.6%) | 0.24 | |
| >100 | 2 (1.0%) | 4 (1.6%) | 6 (1.4%) | 0.44 | |
| Not mentioned | 8 (4.0%) | 17 (6.9%) | 25 (5.0%) | 0.13 | |
| Dysplastic nevi | Yes | 33 (16.6 %) | 45 (18.4%) | 78 (17.6%) | 0.36 |
| None | 159 (79.9%) | 176 (71.8%) | 335 (75.5%) | 0.03 | |
| Not mentioned | 7 (3.5%) | 24 (9.8%) | 31 (7.0%) | 0.007 | |
| Seborrheic keratosis | Yes | 53 (26.6%) | 66 (26.9%) | 119 (26.8%) | 0.51 |
| None | 139 (69.8%) | 165 (67.3%) | 304 (68.5%) | 0.32 | |
| Not mentioned | 7 (3.5%) | 14 (5.7%) | 22 (5.0%) | 0.2 | |
| Melanoma | 0 (0%) | 1 (0.4%) | 1 (0.2%) | 0.55 | |
| Basal cell carcinoma | 2 (1.0%) | 2 (0.8%) | 4 (0.9%) | 0.61 | |
| Squamous cell carcinoma | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | _ |
Compared using Chi-Square analysis; P<0.05, was considered significant.
Discussion
In the present study, we analyzed the data obtained from the melanoma prevention campaign in city with a population of one million in eastern Siberia. We observed a decrease in the number of participants who presented to regional dermatovenereology centers for melanoma screening in 2016, and an increase in the number of participants who were screened in private clinics. This tendency may be due to more intensive advertising by private clinics, or to the distribution of such clinics throughout the city that makes access to the doctor and possibility of obtaining free medical consultation easier. Most participants of the 2015-2016 campaign belonged to an urban population and constituted >90% of screened individuals.
Females were found to account for the majority of participants examined in the two-year period, which is in line with other reports; this may be explained by the greater concern about appearance and cancer risk among women (Stratigos et al., 2007). In the 2015-2016 screening campaign, 77% of individuals were aged <50 years, although the mean age of melanoma patients in the Russian Federation is 60.9 years (Kaprin et al., 2015). This tendency was also observed in the Euromelanoma Campaign in Greece (Stratigos et al., 2007). The results of this campaign in Sweden revealed that 58% of screened individuals were aged >50 years (Paoli et al., 2009). This may be due to the focus of the advertisement campaign on individuals in the higher risk group in terms of age, as well as the compulsory payment for examination, which attracted subjects with a more objective need for screening.
The majority of patients had no family history of melanoma or skin cancer, which indicates that better targeting of individuals in higher risk groups is required. It should be mentioned, nevertheless, that the individuals who attended the screening demonstrated a higher level of melanoma risk factors. In 2016, we observed seborrheic keratosis in 30% of participants, although some data show that this comprises only 3% of cases in dermatology clinics (Kiellberg and Sand, 2005). 20% of participants had lentigo on the back; by contrast, a previous study showed that this was present in 8% of 334 individuals resident in our city who were assessed (Motorina et al., 2016). It is notable that a relatively high number of cases of dysplastic nevi were identified among the screened individuals. We suggest that this may be due to an unclear definition of this type of lesion, rather than due to a real number of patients that came to be examined, as discordant clinical criteria have been proposed to define this type of nevus. Kelly et al., (1997) proposed that dysplastic nevi should be defined as melanocytic lesions with a macular component and the presence of ≥3 of the following features: irregular pigmentation, ill-defined border, irregular border, erythema and size ≥5 mm. Tucker et al., (1997) proposed that dysplastic nevi should be defined as lesions ≥5 mm in diameter that are flat or contain a flat component and have at least two additional hallmarks from the following: irregular borders, indistinct borders or inconstant pigmentation. The Consensus Development Conference in 1992 recommended the definition of atypical moles rather than dysplastic nevi, but no compliance between dermatologists, pathologists, oncologists and other clinicians has been reached on this matter (Goldstein and Tucker, 2013).
The data indicated an increased frequency in the use of dermoscopy (83.4% of screened individuals in 2015 and 90.6% in 2016). However the frequency of examination by dermoscopy could be further increased.
Apart from the necessity for more focused selection of individuals for melanoma/skin cancer screening, it is important to obtain data from dermatologists concerning the final diagnosis after histological examination of patients who were referred to an oncology center with suspected melanoma/skin cancer. All patients suspected of having melanoma/skin cancer were referred to a regional oncological dispensary. It should be noted that doctors were not further informed about the final diagnosis, although this is an important point in terms of assessment of the effectiveness of the program. However, despite this significant drawback, the campaign helps to identify patients with an elevated risk of melanoma/skin cancer development.
Funding Statement
The database collection was not funded. Melanoma Screening Day campaign sponsors list is possible to obtain from the corresponding author. Database analysis was supported by a grant from the Russian Science Foundation (project №14-15-00074).
Statement of human rights
All the procedures of the studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement conflict of Interest
The authors declare no conflicts of interest.
Acknowledgements
None.
References
- Goldstein AM, Tucker MA. Dysplastic nevi and melanoma. Cancer Epidemiol Biomarkers Prev. 2013;22:528–32. doi: 10.1158/1055-9965.EPI-12-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaprin AD, Starinskiy VV, Petrova GV. Malignancies in Russia in 2014 (morbidity and mortality) Moscow: RIIS FIAN; 2015. p. 249. (in Russian) [Google Scholar]
- Kelly JW, Yeatman JM, Regalia C, et al. A high incidence of melanoma found in patients with multiple dysplastic naevi using photographic surveillance. Med J Aust. 1997;167:191–4. doi: 10.5694/j.1326-5377.1997.tb138843.x. [DOI] [PubMed] [Google Scholar]
- Kiellberg LH, Sand C. Referral pattern of skin diseases in an acute outpatient dermatological clinic in Copenhagen. Acta Derm Venereol. 2005;85:509–11. doi: 10.1080/00015550510034957. [DOI] [PubMed] [Google Scholar]
- Levano W, Miller JW, Leonard B, et al. Public education and targeted outreach to underserved women through the national breast and cervical cancer early detection program. Cancer. 2014;120:2591–6. doi: 10.1002/cncr.28819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motorina AV, Palkina NV, Komina AV, et al. Genetic analysis of melanocortin 1 receptor red hair color variants in Russian population of Eastern Siberia. Eur J Cancer Prev. 2016;13 doi: 10.1097/CEJ.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoli J, Danielsson M, Wennberg AM. Results of the 'Euromelanoma Day'screening campaign in Sweden 2008. JEADV. 2009;23:1304–10. doi: 10.1111/j.1468-3083.2009.03316.x. [DOI] [PubMed] [Google Scholar]
- Stratigos A, Nikolaou V, Kedicoglou S, et al. Melanoma/skin cancer screening in a Mediterranean country:results of the Euromelanoma screening day campaign in Greece. JEADV. 2007;21:56–62. doi: 10.1111/j.1468-3083.2006.01865.x. [DOI] [PubMed] [Google Scholar]
- Tucker MA, Halpern A, Holly EA, et al. Clinically recognized dysplastic nevi. A central risk factor for cutaneous melanoma. JAMA. 1997;277:1439–44. [PubMed] [Google Scholar]
- van der Leest RJT, de Vries E, Bulliard J-L, et al. The Euromelanoma skin cancer prevention campaign in Europe:characteristics and results of 2009 and 2010. JEADV. 2011;25:1455–65. doi: 10.1111/j.1468-3083.2011.04228.x. [DOI] [PubMed] [Google Scholar]
- Wolff T, Tai E, Miller T. Screening for skin cancer:an update of the evidence for the U.S. preventive services task force. Ann Intern Med. 2009;150:194–8. doi: 10.7326/0003-4819-150-3-200902030-00009. [DOI] [PubMed] [Google Scholar]


