Abstract
A 15-month retrospective study of 1,000 outpatients was conducted to determine the exact cause of general dizziness. The most common diagnosis in all analyzed cases was cervicogenic general dizziness (89%). The majority of the patients who underwent magnetic resonance imaging of the cervical spine had narrow spinal canals. Measuring the anteroposterior diameter of the spinal canal in each case was critical to obtain an accurate diagnosis in line with the diagnostic criteria used. General dizziness may develop because of inappropriate neck posture over long periods of time in individuals with some form of underlying cervical disease. The causes of general dizziness were different between male and female patients and between patients of different age groups. Triggers leading to general dizziness included engaging in farming, gardening, or weeding activities for long periods of time, particularly in elderly women. Selection of the appropriate muscle relaxant type and dosage is important in the treatment of patients with cervicogenic general dizziness who also experience a stiff neck and shoulders. Following treatment, 90% of patients no longer experienced general dizziness or exhibited clear improvements in their symptoms within 1 week. The results of this study emphasize the importance of cervicogenic general dizziness, which is due to cervical vertebral lesions and is exacerbated by excessive stress on the cervical spine.
Keywords: general dizziness, cervicogenic, narrow spinal canal, muscle relaxants
Introduction
General dizziness is a symptom frequently encountered in everyday clinical practice. However, the causes of this symptom are highly varied and can often be difficult to treat. In addition, reaching a definitive diagnosis in patients with general dizziness can prove difficult. At our hospital, patients who complain of general dizziness despite having no intracranial disease presentation and no clear signs of inner ear dysfunction or systemic conditions, patients complaining of severe dizziness for which treatments attempted by multiple medical facilities have failed to achieve adequate results, and patients with refractory dizziness and those with dizziness of an unknown cause are frequently treated.
This study was a retrospective analysis of the patients who visited our hospital with a chief complaint of general dizziness. Herein, I primarily consider cervicogenic general dizziness, which was the most common cause of our patients’ symptoms.
Patients and Methods
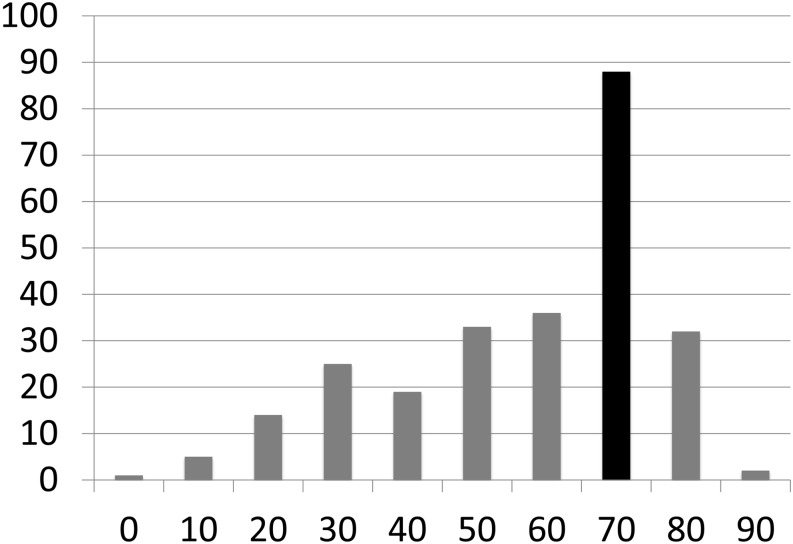
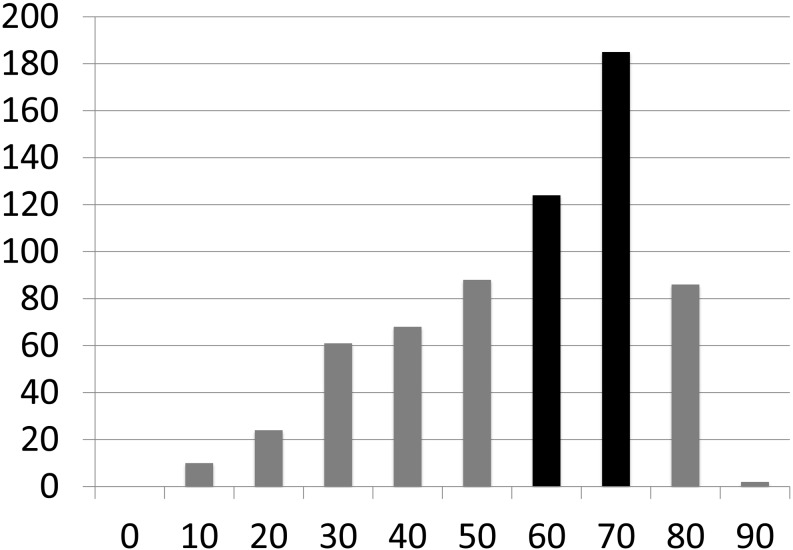
This study included 1,000 patients (299 men and 701 women) who visited our hospital during a 15-month period between June 2013 and September 2014 with a chief complaint of general dizziness. The patients’ ages ranged from 9 to 91 years, and the mean age was 62.0 years. All study participants provided informed consent, and the study design was approved by the appropriate ethics review board. Men in their 70s were the most prominent group of patients. The women in the study exhibited a trend of increasing prevalence of general dizziness with increasing age up to their 70s (Figures 1 and 2).
Figure 1.
Number of male patients with general dizziness in each age group.
Figure 2.
Number of female patients with general dizziness in each age group.
I used the various definitions established by the Japan Foundation for Equilibrium Research (1987) to diagnose cervicogenic general dizziness. These definitions are as follows: “In many cases, the cause of vertigo lies in the cervical region, as a result of events such as rotation or extension of the neck, or abnormalities of the equilibrium sensation”; “repeatedly occurring vertigo”; “symptoms affecting the neck, particularly cervical neuralgia, sympathetic tenderness, and vertigo accompanied by autonomic nervous symptoms”; “vertigo, dizziness, or imbalance caused by abnormal afferent input from the neck, in cases in which no organic vestibular impairment is observed”; and “a lack of disorders leading to vertigo involving areas other than the cervical region”1,2,3).
Patients with no cerebral, systemic, or other non-cervical disorders were treated for cervicogenic general dizziness even if cochlear symptoms such as hearing loss could not be excluded. Of these patients, those meeting the following criteria were diagnosed with cervicogenic general dizziness:
a) Abnormal cervical findings on magnetic resonance imaging (MRI) and neck stress
b) No abnormal cranial MRI findings, and neck stress
Lesions such as cervical spinal canal stenosis (defined as an anterior-posterior diameter of the spinal canal less than 12 mm at the levels of several vertebral bodies), degenerative cervical spondylosis, cervical disc herniation, ossification of the posterior longitudinal ligament (OPLL), and syringomyelia were assessed using cervical MRI in order to aid in the diagnosis of cervical spinal disorders.
No systemic symptoms, such as hypertension, diabetes, or anemia, or cochlear symptoms were observed, although no cause of general dizziness was identified on cranial MRI. Although the patients’ conditions were well controlled, many experienced general dizziness. Many of these patients had cervicogenic symptoms, such as hypertonia of the neck and scapular muscle group, and met the above criterion listed under a) (patients who placed stress on their necks prior to the manifestation of dizziness).
The following section describes the diagnostic imaging procedures, causation, treatment methods, and prognoses of the general dizziness cases treated at our hospital in this retrospective study.
Results
Pathological causes of dizziness disorder
Most of the 1,000 patients with general dizziness in this study had cervicogenic general dizziness (n = 899; 90%), followed by drug-induced general dizziness (27 patients, pregabalin: 8, antihypertensive drugs: 9, other causative drugs), cerebrovascular infarction (13 patients), orthostatic hypotension (10 patients), concussion (5 patients), overwork (5 patients), benign seizure-induced general dizziness (3 patients), vasovagal reflex (3 patients), anemia (3 patients), psychogenic disorders (2 patients), and 1 patient each with cerebral hemorrhage, cerebellar atrophy, hypertensive emergency, and the common cold. Three patients had general dizziness due to other causes, and 23 had general dizziness due to unknown causes (2%).
Symptoms and imaging findings in patients with cervicogenic general dizziness
Of the patients diagnosed with cervicogenic general dizziness, 744 (83%) presented with lightheadedness, and 155 patients (17%) exhibited rotatory vertigo. Seven-hundred and six patients (79%) presented with stiff shoulders, 416 (46%) had a sensation of a heavy head or headache (tension-type headache), 198 (22%) had numbness of the hands/upper extremities, 104 (12%) had scapular pain, and 46 (5%) had tinnitus. It was believed that the tinnitus was the result of tension applied to the neck and scapular muscle group, which also affected the ossicular muscles. Therefore, tinnitus in the patients in this study was determined not to be a cochlear symptom (these symptoms disappeared in all cases following treatment with a muscle relaxant). It is not unusual for nystagmus to occur in patients with cervicogenic general dizziness as a result of lightheadedness, rotatory vertigo, or anterior or posterior flexion of the neck. However, no distinct characteristics were observed during the diagnosis. This symptom was thus deemed to have little value in diagnostic confirmation. Eighty-four of the 193 patients who did not experience stiff shoulders complained of a headache or a heavy head sensation believed to be indicative of a tension-type headache. Based on these observations, 790 patients (88%) diagnosed with cervicogenic general dizziness were determined to have hyperflexion of the neck, scapular muscles, or temporalis muscle.
Cervical MRI was performed in 600 of 899 patients diagnosed with cervicogenic general dizziness (67%). Cervical spinal canal stenosis was diagnosed in 544 of these patients (91%), degenerative cervical spondylosis was found in 40 patients, herniated cervical spinal discs were found in 11 patients, and 1 patient each was diagnosed with OPLL, cervical scoliosis, and syringomyelia. The anteroposterior spinal canal diameters in patients diagnosed with cervicogenic general dizziness with underlying spinal canal stenosis ranged from 4.0 mm to 11.6 mm (mean: 9.0 mm). Cranial MRI was performed in all 299 patients who did not undergo cervical MRI. We confirmed that no causal factors for general dizziness were present within these patients’ skulls.
Causes of cervicogenic general dizziness
Patient interviews revealed that the etiology of general dizziness symptoms differed depending on patient sex and age. Of all patients with cervicogenic general dizziness, 712 (79%) were able to recall episodes in which an excessive load was placed on the neck, which was then considered to cause their symptoms. The incidence of cervicogenic general dizziness by season was also examined in the 186 men and 489 women who visited our hospital between June 2013 and May 2014.
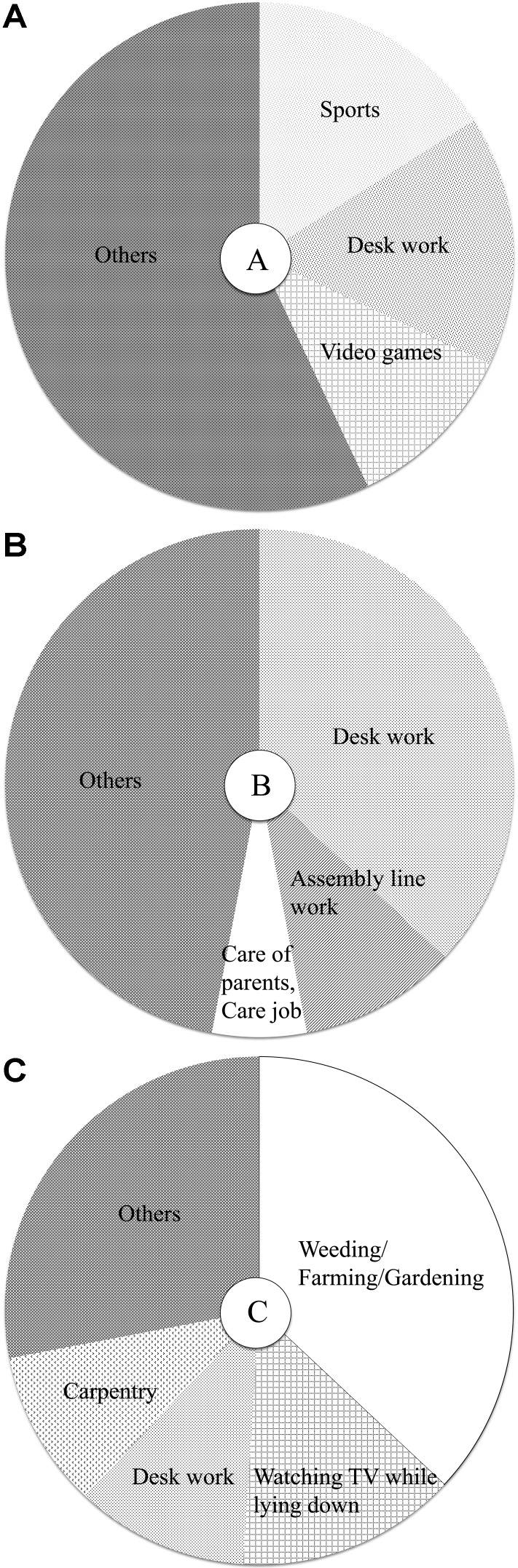
The symptoms of male patients in their teens up to their 50s were often associated with their occupations. Specifically, desk work, such as operating a personal computer (PC) for long periods of time, was often a symptom trigger in these patients (Figures 3A and 3B). In elderly male patients, gardening activities, such as landscaping and tree planting, were the most common triggers, although long periods of viewing television in an awkward posture, such as when lying on one’s side, was also a frequent trigger (Figure 3C).
Figure 3.
A: Causes of general dizziness in male patients between the age of 10 and 29 years (n = 19). B: Causes of general dizziness in male patients between the age of 30 and 59 years (n = 68). C: Causes of general dizziness in male patients over the age of 60 years (n = 115).
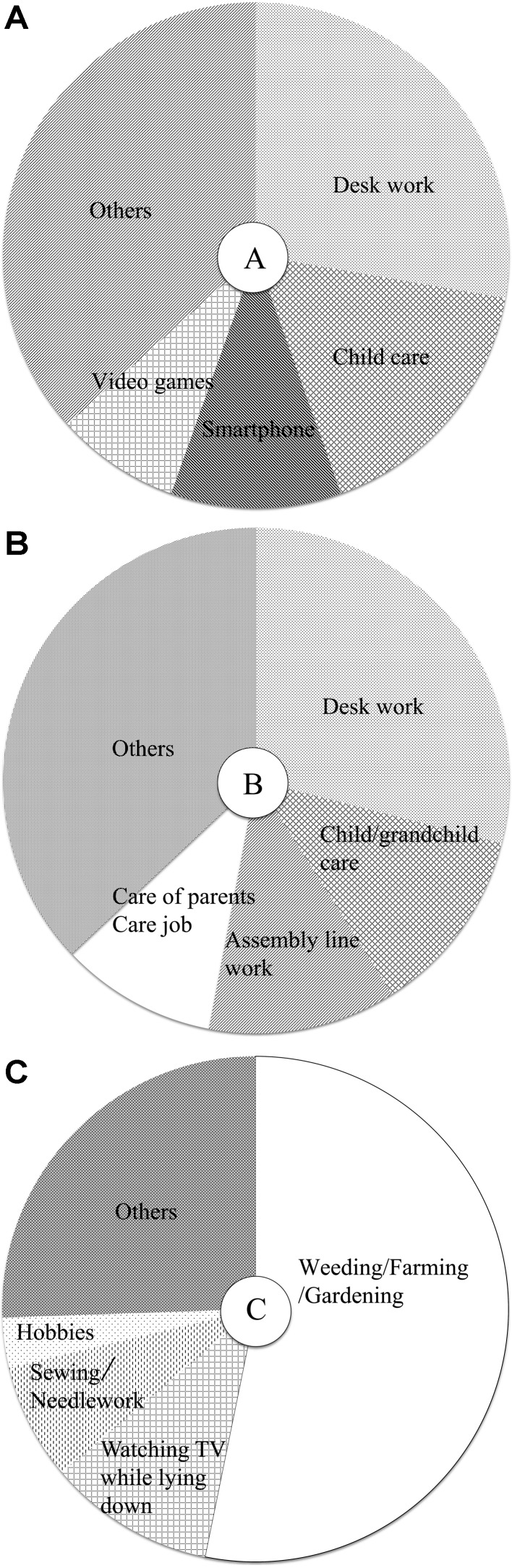
In female patients in their teens up to their 50s, long periods of desk work, including PC operation, childcare activities such as piggybacking and hugging, or caring for grandchildren were the most frequent symptom triggers (Figures 4A and B). In young women, maintaining a forward leaning posture for long periods during activities such as smartphone use, playing video games, and studying were also common symptom triggers (Figure 4A). In female patients aged 60 and older, gardening activities, such as landscaping and weeding, triggered symptoms much more frequently during the spring (March to May 2014) and fall seasons (September to November 2013) (Figures 4C and 5B). In addition, lying down on one’s side for a long period of time with a straining neck posture during activities such as watching TV or reading was found to be a frequent symptom trigger during the winter months (December 2013 to February 2014) (Figure 4C).
Figure 4.
A: Causes of general dizziness in female patients between the ages of 10 and 29 years (n = 36). B: Causes of general dizziness in female patients between the ages of 30 and 59 years (n = 185). C: Causes of general dizziness in female patients over the age of 60 years (n = 289).
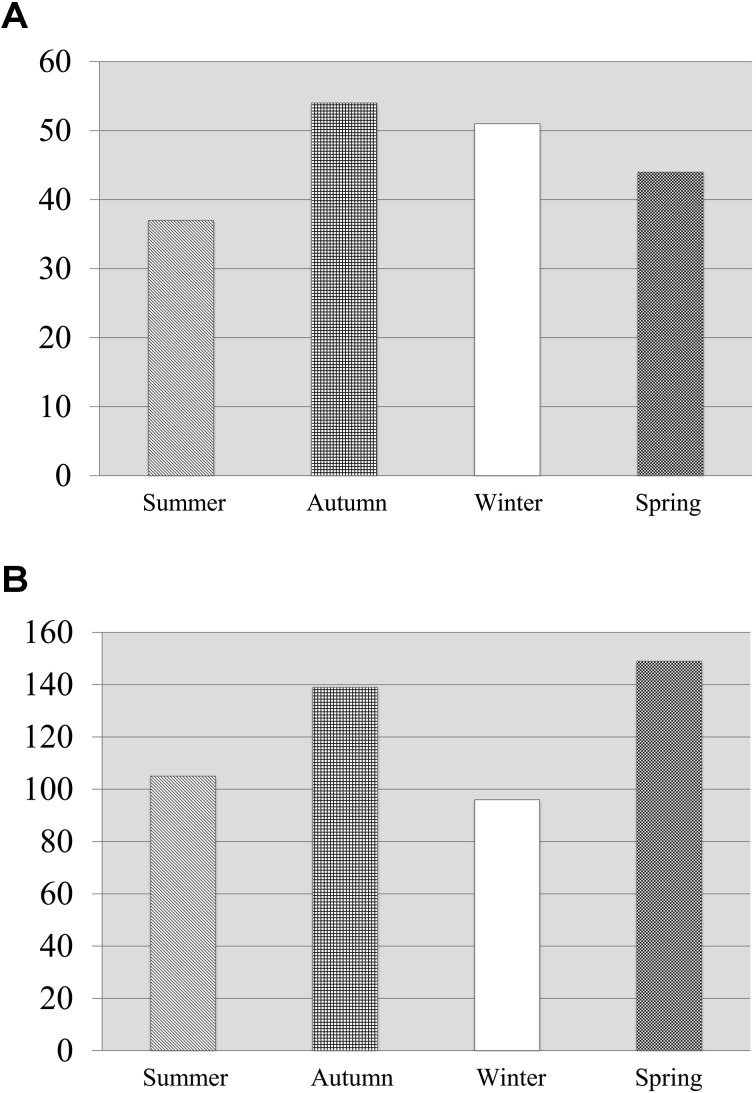
Although the number of male patients with general dizziness increased slightly in the autumn when harvesting chores are common, there were few changes in symptom prevalence throughout the year (Figure 5A). In contrast, the number of female patients with general dizziness tended to increase in the spring when patients began engaging in long periods of agricultural and gardening activities (Figure 5B). In addition, the number of male and female patients decreased slightly during the summer months (June to August 2013) when outdoor activities are more common, while the number of male patients increased slightly, and the number of female patients decreased slightly during the winter months (Figures 5A and 5B).
Figure 5.
A: Number of patients with general dizziness by season (men). B: Number of patients with general dizziness by season (women).
Drug therapy for cervicogenic general dizziness
Correction is most important when symptoms are accompanied by excessive tension of the neck and scapular muscles or a tension-type headache. Muscle relaxants and opioid drugs were used in all 790 cases determined to be caused by tension-type headaches or excessive tension of the neck, scapular muscles, or temporalis muscle. Muscle relaxants with stronger effects were selected in the majority of the cases. Doses of 1–6 mg per day of tizanidine were generally administered to non-elderly patients, and milder drug regimens, such as 40–60 mg per day of afloqualone, were prescribed for elderly patients. Another commonly prescribed drug was eperisone, which was prescribed at doses of 100–150 mg per day. Dantrolene may also be effective in intractable cases. The above findings indicate that the selection of muscle relaxant drug type and dose were made on a patient-by-patient basis to ensure that the underlying causes of the symptoms were addressed appropriately and effectively. When the effects of typical muscle relaxants were inadequate, a dibenzodiazepine-class or benzodiazepine-class anxiolytic drug with muscle relaxant effects was used in combination with Chinese herbal medicines, such as peony and licorice decoctions (Shakuyakukanzoto), which is a neurotropin used as a therapeutic agent. This medicine is used to suppress pain affecting the lower body and to improve blood circulation in the upper body. Non-steroidal anti-inflammatory drugs were also used, as appropriate, to address upper body pain symptoms, including headache, as such symptoms can create a vicious circle that exacerbates tension on the neck and scapular muscles. Tocopherol nicotinate and opioid drugs were used in combination in patients without stress on the neck and scapular muscles. These patients were also provided with comprehensive lifestyle guidance to help them avoid excessive stress on the neck.
Cervicogenic general dizziness prognosis
General dizziness improved in all cases within a short period, provided that a suitable drug therapy was selected, and patients were able to adjust their trigger behaviors. General dizziness symptoms disappeared or exhibited clear evidence of improvement within 1 week in 806 patients (90%) and within 2 weeks in another 33 patients (4%). Improvement first appeared after 1 month in 18 patients (2%) and after 2 months in 3 patients (0.3%). No improvement was observed in 39 patients (4%). The subsequent clinical course for these patients is unknown. In cases wherein general dizziness improved, understanding the causal condition and reducing the amount of stress placed on the neck resulted in no recurrences during the shortest observation period of 3 months. General dizziness symptoms only recurred repeatedly when patients resumed placing excessive stress on the neck.
Actual case examples
Case 1: 54-year-old female patient
Chief complaint: Recurrent lightheadedness and rotatory vertigo
History of present disease: The patient works as a cook and began experiencing recurrent lightheadedness and rotatory vertigo several years earlier, with episodes lasting for 1–2 days. These episodes were occasionally accompanied by occipital pain. The patient’s condition was often exacerbated when she moved her head. Two days before examination, the patient experienced a rotative vertigo episode lasting for 1 day and took time off from work. She visited our hospital when her symptoms did not improve. The patient had never sought medical attention regarding her dizziness symptoms in the past.
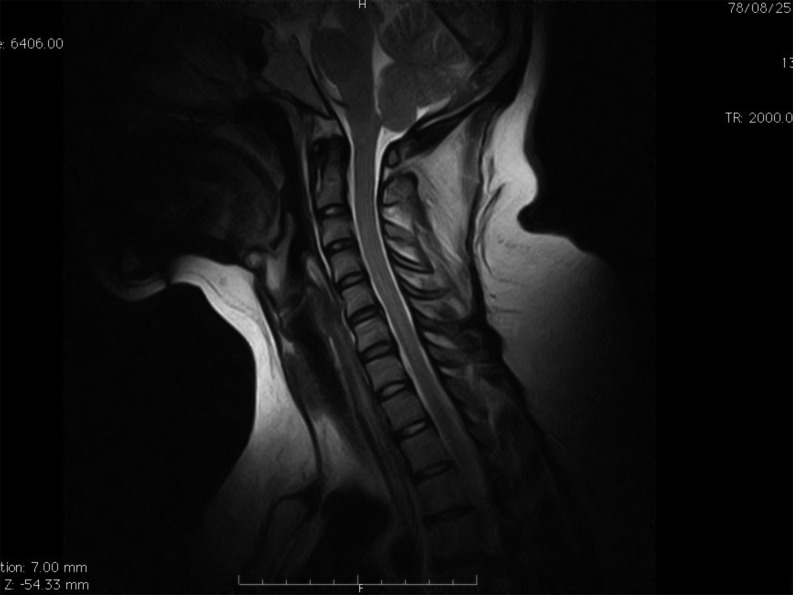
Diagnosis and clinical course: Based on the patient interview, the patient was suspected of having cervicogenic general dizziness, as she complained of severe shoulder stiffness occasionally becoming pronounced at the right upper extremity. Cervical MRI revealed spinal canal stenosis and mild cervical spondylotic lesions (Figure 6). In addition to drug therapy (tizanidine, diphenidol, and sodium loxoprofen), the patient was advised to avoid straining her neck as much as possible and to take breaks as needed. General dizziness symptoms and headache disappeared almost completely by the time she returned to work 1 week later, during which time the patient continued drug therapy. The patient has had no recurrence of general dizziness symptoms for over 1 year.
Figure 6.
Case 1: Sagittal MRI (0.3-T), cervical cross-section, T2-weighted image.
Case 2: 83-year-old female patient
Chief complaint: Recurrent rotatory vertigo
Current medical history: The patient began experiencing repeated rotatory vertigo episodes starting 2 years prior to the visit. Treatment received from multiple medical facilities proved ineffective. The physicians whom the patient had previously visited were unable to identify the cause of the patient’s symptoms.
Diagnosis and clinical course: The patient often engages in typical gardening activities, such as weeding, and experiences repeated, momentary back pain episodes (greater occipital neuralgia). The patient’s subjective symptoms other than general dizziness included mild shoulder stiffness, numbness of the right hand, and right shoulder pain. Cervical MRI revealed spinal canal stenosis and degenerative cervical spondylosis (Figure 7). Drug therapy was prescribed (eperisone, betahistine mesylate, and celecoxib) in addition to lifestyle guidance, instructing the patient to refrain from long periods of weeding and similar activities. As a result, the patient’s general dizziness symptoms disappeared within 1 week, and her subsequent course has been favorable.
Figure 7.
Case 2: Sagittal MRI (0.3-T), cervical cross-section, T2-weighted image.
Case 3: 89-year-old female patient
Chief complaint: Recurrent rotatory vertigo and lightheadedness
Current medical history: The patient began experiencing repeated rotatory vertigo and lightheadedness episodes starting 4–5 years ago. Despite receiving treatment from several medical institutions, her symptoms did not improve.
Diagnosis and clinical course: The patient often does farm work in the fields and experienced general dizziness, a heavy head sensation, and shoulder stiffness when turning her head upwards. Cervical MRI revealed spinal canal stenosis and degenerative cervical spondylosis (Figure 8). The patient was started on drug therapy (afloqualone, difenidol, and Ryokyojutsukanto [tuckahoe, cassia twig, largehead atractylodes, and licorice decoction, a Chinese herbal medicine]) and was prescribed lifestyle guidance instructing her to refrain from long periods of field work and to occasionally take breaks as needed. As a result, the patient’s symptoms disappeared within 1 week.
Figure 8.
Case 3: Sagittal MRI (0.3-T), cervical cross-section, T2-weighted image.
Case 4: 78-year-old female patient
Chief complaint: Recurrent rotatory vertigo and lightheadedness
Current medical history: The patient had experienced repeated episodes of rotatory vertigo and lightheadedness since entering her 50s. Although she had visited several medical facilities, the cause of her condition remained unclear. The patient had no improvement in her general dizziness episodes.
Diagnosis and clinical course: The patient engages in gardening activities such as weeding, generally for long periods of time. She often feels that her head is weighted down and that her shoulders have become stiff. A cervical MRI revealed spinal canal stenosis and degenerative cervical spondylosis (Figure 9). In addition to drug therapy (afloqualone and sulpiride), the patient was provided with lifestyle guidance, including the recommendation to avoid long periods of gardening. The patient’s dizziness symptoms disappeared 1 week after initiating treatment. Subsequently, the patient had no recurrence of general dizziness symptoms for 2 years.
Figure 9.
Case 4: Sagittal MRI (0.3-T), cervical cross-section, T2-weighted image.
Discussion
Although “general dizziness” is commonly encountered in routine practice, reaching an accurate diagnosis remains challenging even with modern medical techniques. The condition is thus still a frequent subject of debate.
In Kaetsu area of Niigata Prefecture, it is estimated that sudden cases of severe rotatory vertigo and cases complicated by cochlear symptoms are often first admitted to an emergency outpatient facility at a hospital in a neighboring city or are referred to an otorhinolaryngology practitioner. As such, when diagnosing patients presenting with general dizziness symptoms, it is important to consider that typical otorhinolaryngological conditions are likely to have already been eliminated during prior examinations. When considering the majority of the patients with general dizziness admitted to our hospital, I presume that the causal illness was not discovered by the patient’s previous physicians or was intractable. Alternatively, the patient may have visited our hospital for examination after repeated symptom episodes raised concerns regarding intracranial conditions. The population of patients with general dizziness visiting our hospital is highly likely to differ from that seen by otorhinolaryngologists, neurologists, internal medicine physicians, or general practitioners. Nevertheless, in this study of patients with significant general dizziness symptoms admitted to our hospital, the primary causal disorder in patients without typical otorhinolaryngological diseases was cervicogenic general dizziness. I also found that the most common causal disorder varied by patient age and sex. I discuss the causes of cervicogenic general dizziness, its mechanism of onset, and treatment options in the following sections.
Importance of distinguishing cervicogenic general dizziness from benign paroxysmal positioning vertigo
Benign paroxysmal positioning vertigo (BPPV) is a condition that has recently come to be considered the most common cause of general dizziness in Japan, with some reports stating that the condition accounts for approximately 40% of all cases of peripheral vertigo4). BPPV is a benign disorder that causes dizziness due to stimulation of the semicircular canal interior after otoliths are unintentionally detached from the equilibrium plaque of the utricular macula when the head is tilted in certain directions. In actual clinical practice, BPPV can be diagnosed under a broad definition including many instances wherein a BPPV diagnosis is reached when nystagmus or vertigo alone is observed when the head or neck is moved, even when no dizziness appears. BPPV diagnoses are also believed to be frequently made in many cases wherein dizziness or nystagmus appear only when a specific head position is adopted. This condition is also believed to be common in patients with cervicogenic general dizziness. Although our hospital did not perform detailed evaluations of each of the patients included in this study using otorhinolaryngological tests, only 0.3% of the 1,000 patients had the potential to be diagnosed with BPPV under our stringent diagnostic criteria. As the treatment methods for the two conditions are completely different, providing differential treatment regimens for patients with cervicogenic general dizziness and for those with BPPV is of high clinical importance.
Recognition of cervicogenic general dizziness
Cervicogenic dizziness was first described in a 1926 paper by Barre as a type of general dizziness induced by cervical arthritis. This condition is also referred to as Barre-Lieou Syndrome today5). Ryan and Cope later published a report in 1955 describing general dizziness caused by cervical spinal abnormalities, particularly spondylosis. In this paper, the condition was referred to as “cervicogenic vertigo”, a term that others have continued to use6, 7). Numerous reports on cervicogenic general dizziness have been published in Europe and the United States. Currently, the more clinically oriented name “cervicogenic vertigo (general dizziness, imbalance)” is used to describe the condition. This condition is regarded as important in both Europe and the United States1, 4, 8,9,10,11,12,13), although it has a surprisingly low level of recognition in Japan3). It is important to recognize that general dizziness is frequently triggered by excessive stress placed on the cervical spine. In patients presenting with cervicogenic general dizziness, the presence of an underlying cervical spine condition can be confirmed using cervical MRI examination. In addition, the attending physicians can easily determine whether the patient engages in activities that cause him/her to place excessive stress on the neck prior to the manifestation of general dizziness symptoms. In this study, spinal canal stenosis was found to be a complicating condition in approximately 90% of patients in whom cervical MRI was performed. In addition, although the causes of general dizziness symptoms differed depending on patient age and sex, it was confirmed that patients in all cases adopted postures that placed excessive stress on the neck.
Mechanism of onset for general dizziness arising from vertebral disorders
Lightheadedness was used to describe approximately 80% of the general dizziness findings in this study. However, estimating the site of injury or the causative disorder based only on differences in presentation between rotatory vertigo and lightheadedness proved difficult.
Discussion of the pathways involved in cervicogenic general dizziness often begins with the neural pathways of the vestibular system. There is also a peripheral vestibular system serving as a descending nerve tract. The brainstem and cerebellum are also involved, as they comprise the central vestibular system. The vestibulospinal tract is located in the cervical spinal cord. The lateral vestibulospinal tract communicates with the otolith input (linear acceleration and gravity) and supplies all cervical, thoracic, and lumbar spinal cord segments, while the medial vestibulospinal tract transmits semicircular canal input (angular acceleration) and supplies the cervical spinal cord only. In addition, the cerebellar spinal cord tract, which is an ascending nerve tract that sends sensory information from the lower body and trunk to the cerebellum, can become a source of general dizziness following neck injury.
When shoulder stiffness persists because of cervical spinal disorders, the cervical sympathetic nerves can become tense. This may cause general dizziness as a result of an autonomic imbalance. Symptoms, including headache, general dizziness, tinnitus, stiffness of the neck and scapular muscles, retrobulbar pain, general malaise, and palpitations caused by Barre-Lieou syndrome5, 15), may appear as a result of whiplash accidents or cervical spondylosis and are encountered relatively frequently.
Although the number of related cases may be small, insufficient circulation to the cerebellum and the brainstem due to osteophytes narrowing the vertebral artery (observed in patients with cervical spondylosis) is believed to cause general dizziness symptoms. Physical pressure on the vertebral artery or vertebral nerves accompanying the cervical vertebrae or resulting from lateral punctures will cause bending and narrowing of the vertebral artery during neck movements. This would, in turn, lead to so-called vertebrobasilar artery insufficiency (Power’s syndrome)14). Although evaluation of the vertebrobasilar artery using MRA was not performed during this study, MRA is believed to be necessary to eliminate this and similar potential causal disorders during diagnosis.
Spinal canal stenosis and cervicogenic general dizziness
Although diagnostic criteria for cervical vertebral canal stenosis exist, severe symptoms that would necessitate surgery in actual clinical cases often do not appear in mild cases where the anteroposterior diameter of the spinal canal is approximately 10–12 mm. However, it is important to recognize regarding long-term stresses on the neck that even mild cases of spinal canal stenosis can induce general dizziness.
Treatment and prognosis of cervicogenic general dizziness
Continued placement of excessive stress on the neck during neck and scapular muscle group flexion can prolong or exacerbate cervicogenic general dizziness symptoms. Of the patients with cervicogenic general dizziness examined in this study, 90% had remission of their symptoms within 1 week of initiating appropriate treatment. Relieving excessive tension on the neck and scapular muscle groups is the most important therapeutic factor in achieving rapid improvement in cervicogenic general dizziness symptoms3, 11, 16). In the patients examined during this study, drug therapies with weak muscle relaxant effects, such as afloqualone and tolperisone, had sufficient effects, while drugs with stronger effects, such as tizanidine, often required extremely high dosages of 6 mg per day and required the concomitant use of several types of muscle relaxants. When these muscle relaxants did not achieve sufficient results, tranquilizers and Chinese herbal medicines such as peony and licorice decoctions (Shakuyakukanzoto) and arrowroot decoctions (Kakkonto), were used concomitantly. Tranquilizers such as thienodiazepine and benzodiazepine were similarly used to relieve muscle tension if necessary. Gaining a thorough understanding of the particular characteristics of each patient and knowledge regarding the actions and side effects of different drug therapies are necessary when selecting muscle relaxants or other drugs and determining appropriate dosages.
Patients must be provided with adequate information to convince them to adjust their behaviors related to their neck condition based on an accurate diagnosis in order to achieve timely improvement and to prevent the recurrence of general dizziness. It is also important to provide lifestyle guidance to patients to help them avoid placing excessive stress on the neck. This includes avoiding the maintenance of stressful neck postures for long periods of time. Based on the cases involving general dizziness in this study, it appears that not only appropriate drug therapy but also well-planned lifestyle guidance can contribute to high rates of successful treatment outcomes.
Conclusion
General dizziness may be induced following engagement in repetitive activity patterns that are common in modern life and that place excessive stress on the neck in the presence of underlying cervical spinal conditions. Treatment of excessive tension placed on the cervical/scapular muscle group or the temporal muscle can result in improvements in general dizziness symptoms within 1 week. It is also extremely important to advise patients to monitor their own cervical condition and to adjust lifestyle habits that place too much stress on the neck for extended periods. It should also be emphasized that cervicogenic general dizziness is an important contemporary lifestyle disorder that can be treated.
A nearly identical version of this paper was published in the Journal of the Japanese Association of Rural Medicine in the Japanese language in 201617).
Conflicts of Interest
The author has no conflicts to disclose regarding the publication of this paper.
Acknowledgements
I would like to offer my deepest gratitude to Dr. Masafumi Fukuda of the Department of Neurosurgery, Brain Research Institute, Niigata University for his invaluable support and guidance regarding the execution of this study.
References
- 1.Komatsuzaki A. Cervicogenic dizziness. Materials for the standardization of the vertigo diagnostic criteria – Report of the Vertigo Diagnostic Standardization Committee. “Keiseimemai. Memai shindan kijun-ka no tame no shiryō — 1987-nen memai shindan kijun-ka iinkai tōshin-sho. Equilibrium Res (Suppl.) 1995; 11: 54.(in Japanese). [Google Scholar]
- 2.Kondo A.Cervicogenic dizziness. Diagnosis and treatment. Neurosurgery Bulletin Keiseimemai-shindan to chiryo. Noshinkei geka shokuho 2009; 19: 203––207. (in Japanese). [Google Scholar]
- 3.Futaki T. Vertigo: Diagnosis and treatment approaches. Memai no mi-kata kangae-kata Igaku Shoin, 2001. (in Japanese).
- 4.Barnsley L, Lord S, Bogduk N. Whiplash injury. Pain 1994; 58: 283–307. doi: 10.1016/0304-3959(94)90123-6 [DOI] [PubMed] [Google Scholar]
- 5.Barre JA. Surun syndrome symphathique cervical posterieure et sa cause frequente: I’arthrite cervicale. Rev Neurol 1926; 45: 1246–1248. [Google Scholar]
- 6.Cope S, Ryan GMS. Cervical and otolith vertigo. J Laryngol Otol 1959; 73: 113–120. doi: 10.1017/S0022215100055018 [DOI] [PubMed] [Google Scholar]
- 7.Ryan GMS, Cope S. Cervical vertigo. Lancet 1955; 269: 1355–1358. doi: 10.1016/S0140-6736(55)93159-7 [DOI] [PubMed] [Google Scholar]
- 8.Brandt T, Bronstein AM. Cervical vertigo. J Neurol Neurosurg Psychiatry 2001; 71: 8–12. doi: 10.1136/jnnp.71.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown JJ. Cervical contributions to balance. Cervical vertigo. In: The Head Neck Sensory Motor System. Berthoz A, Vidal PP, Graf W, Eds. Oxford University Press 1992; 644-647.
- 10.Galm R, Rittmeister M, Schmitt E. Vertigo in patients with cervical spine dysfunction. Eur Spine J 1998; 7: 55–58. doi: 10.1007/s005860050028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karlberg M, Magnusson M, Malmström EM, et al. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil 1996; 77: 874–882. doi: 10.1016/S0003-9993(96)90273-7 [DOI] [PubMed] [Google Scholar]
- 12.Norré ME. Cervical vertigo. Diagnostic and semiological problem with special emphasis upon cervical nystagmus. Acta Otorhinolaryngol Belg 1987; 41: 436–452. [PubMed] [Google Scholar]
- 13.Scherer H. Neck-induced vertigo. Arch Otorhinolaryngol Suppl 1985; 2: 107–124 (in German). [PubMed] [Google Scholar]
- 14.Powers SR, Jr, Drislane TM, Nevins S. Intermittent vertebral artery compression; a new syndrome. Surgery 1961; 49: 257–264. [PubMed] [Google Scholar]
- 15.Nagashima M. Autonomic neurosurgery: Pathophysiology and clinical practice of syndrome sympathique cervicale posterieur-Barre-Lieou (Special edition: Recent progress in Neurosurgery). Surgical Therapy 1971; 24: 307–322 (in Japanese). [PubMed] [Google Scholar]
- 16.Furman JM, Whitney SL. Central causes of dizziness. Phys Ther 2000; 80: 179–187. [PubMed] [Google Scholar]
- 17.Takahashi S. Importance of cervicogenic dizziness. “Keisei memai no jyuyosei”. J J Rural Med 2016; 65: 15–24 (in Japanese, Abstract in English). [Google Scholar]