Abstract
Objective
To find out the knowledge, attitude, practice, and barriers of cervical cancer screening in mid-western rural, Nepal.
Methods
A hospital-based cross-sectional study was conducted. Women aged 20 or more were interviewed using a structured questionnaire regarding the socio-demographic information, knowledge, attitude, practice, and barriers to the cervical cancer screening.
Results
Total of 360 participants were recruited for this study, mean age was 30.13±10.4 years. More than 87% of participants had inadequate knowledge, but around 72% had a favorable attitude towards cervical cancer screening. There was a significant portion of women (86.4%) had never done any cervical cancer screening test. Despite being higher literacy rate of Brahmin and Chhetri ethnic group, they were less likely to attend the cervical cancer screening than Dalit and Janajati (p<0.001); and those who had a positive family history of cancer were more likely to attend the cervical cancer screening (p<0.001). Similarly, married women, who had adequate knowledge and or favorable attitude, were more likely to practice cervical cancer screening, though statistically not significant. Factors such as “No symptoms,” “Lack of awareness,” “Embarrassment,” etc. were the most common barriers for the cervical cancer screening.
Conclusion
The adequate knowledge and practice of cervical cancer screening were meager among rural Nepalese women, but most of them had a favorable attitude. There is an imperative need for related awareness programs to promote the uptake of cervical cancer screening tests.
Keywords: Cervical Cancer, Early Detection of Cancer, Diagnosis, Awareness, Nepal
INTRODUCTION
Cervical cancer is the fourth most common cancer among women in the World. About 266,000 women die from this disease every year in the world and among them, 87% mortality occurs in the less developed regions only [1]. Therefore, it is one of the most common malignancies and the leading cause of cancer deaths in women in developing countries. The highest incidence and mortality rates are observed in sub-Saharan Africa, Latin America, and South Asia. Cervical cancer is the number one cancer among women in Nepal. The age-standardized incidence and mortality rate of cervical cancer in Nepal is 19 and 12 (per 100,000 per annum), respectively. In comparison to more developed countries, the incidence rate of cervical cancer is 2 times higher while the mortality is almost four times higher in Nepal [2]. The study conducted in Nepal reported that 80.9% of cervical cancer cases were diagnosed at late stage, and 86% of those patients have never heard of cervical Pap smear test before [3]. These figures indicate that there are problems regarding screening and prevention of this disease. It is estimated that 95% of women have never been screened for cervical cancer in low-income countries due to the limited access to the screening program [4].
National Guideline for Cervical Cancer Screening and Prevention program in 2010 in Nepal had the objective to screen at least 50% of women aged 30 to 60 years to reduce 10% cervical cancer burden within 5 years [5]. Unfortunately, the majority (about 95%) of women still never have done cervical cancer screening according to the report by Ranjit et al., [6] in 2016. Moreover, the proportion of unscreened women for cervical cancer is much higher among the illiterate women and living in the rural region.
The most common challenges in cervical cancer prevention programs in developing countries are, increasing women's awareness, increasing provider knowledge and skills, and effective monitoring and evaluation approach [7,8]. Generally, reports from many developing countries indicated that women had an inadequate understanding of causes, risks, and prevention of cervical cancer [9,10]. Cervical cancer screening is an effective method for reducing the incidence and mortality of cervical cancer, but the screening attendance rate in Nepal is far away from satisfactory level. Currently, there are few published data regarding knowledge, attitude, and practice of cervical cancer screening in urban region of Nepal. But decidedly fewer studies are there to identify the barriers to women primarily living in rural part. In order to increase the cervical cancer screening uptake, it is essential to know knowledge, attitude and possible obstacles and address such problems by the policymakers. The objective of this study is to determine the level of knowledge and attitude and to investigate the barriers of the screening programs among women living in the rural region.
MATERIALS AND METHODS
1. Study setting and ethical approval
This study was approved by the ethical review board of the Nepal Health Research Council, Nepal. Informed consent was taken from each participant. It was a hospital-based cross-sectional study. Participants were recruited from the visitors in the clinic of Karnali Academy of Health Sciences, Jumla. Participants were interviewed with a structured questionnaire by the Medical Assistant from June to September 2017.
2. Inclusion and exclusion criteria
Women from Jumla district aged 20 or more and agreed to participate in the survey were included. Women with significant morbidity, psychiatric disorder and suffering from cancer were excluded.
3. Data collection
The sample size was calculated based on 35% of prevalence of adequate knowledge using Cochrane formula (n=z2pq/d2) [10]. The sample size of 350 was obtained after calculation with 5% allowable error at 95% confidence interval (CI). The questionnaire consisted of 5 parts: socio-demographic information, knowledge, attitude, practice (KAP) and possible barriers to cervical cancer screening.
The first part, the socio-demographic questionnaire included 8 questions about socio-demographic characteristics of the respondents: age, sex, marital status, education, ethnicity, and religion, etc. This section provided the baseline data of the respondents.
The second part included 11 questions about knowledge on cervical cancer; it is risk factors, symptoms, preventive measures, and its screening, which are shown in Table 1. Some items had multiple answers, so the scoring was ‘1’ for each correct response and ‘0’ for the wrong answer with a total score of 30. The analysis of knowledge score was ranked as adequate knowledge if the total score equals to or higher than 15 (≥50%) and inadequate knowledge if the total score is less than 14 (<50%) [11].
Table 1. Knowledge on cervical cancer and screening (n=357).
| Items | Values | |
|---|---|---|
| Definition of cervical cancer | 87 (24.4) | |
| Signs and symptoms | ||
| No symptoms in early-stage | 43 (13.2) | |
| Post-coital bleeding | 93 (25.4) | |
| Post-menopausal bleeding | 86 (26.4) | |
| Dyspareunia | 99 (30.2) | |
| Increased vaginal discharge | 146 (44.2) | |
| Risk factors | ||
| Multiple sexual partners | 147 (41.5) | |
| Multiple pregnancies | 168 (47.5) | |
| Early marriage | 199 (56.1) | |
| Tobacco smoking | 39 (11.0) | |
| Low socioeconomic status | 34 (9.6) | |
| Long-term OCP use | 54 (15.2) | |
| HPV infection | 60 (16.9) | |
| Prevention of cervical cancer | ||
| No multiple sexual partners | 150 (42.3) | |
| Avoiding multiple pregnancies | 159 (44.9) | |
| Use of condom instead of long-term OCP | 58 (16.3) | |
| Avoiding early marriage/early sexual debut | 135 (37.9) | |
| HPV immunization | 74 (20.7) | |
| Maintaining good personal hygiene | 114 (32.1) | |
| Regular cervical screening | 93 (26.3) | |
| Proper treatment of sexually transmitted infections | 64 (18.0) | |
| Cervical cancer is treatable if detected early | 178 (49.9) | |
| Ideal time to start cervical cancer screening | 76 (21.4) | |
| Screening interval | 35 (9.8) | |
| When to stop cervical cancer screening | 57 (17.2) | |
| Available screening tests | ||
| Pap smear | 72 (21.8) | |
| HPV test | 31 (9.4) | |
| VIA | 3 (0.9) | |
Values are presented as correct response (%).
HPV, human papillomavirus; OCP, oral contraceptive pill; VIA, Visual Inspection with Acetic Acid.
The third part was related to attitude consisted of 10 statements regarding the attitude of participant toward the cervical cancer screening. The statements were: cervical cancer is highly prevalent in our country, cervical cancer is the leading cause of death in women among all malignancy in Nepal, any adult women can acquire cervical cancer, cervical cancer cannot be transmitted from one person to another, cervical cancer can be detected early through various screening method, Screening helps in prevention of cervical cancer etc. The Likert scale was used with a range from 1 (strongly disagree), 2 (disagree), 3 (don't know), 4 (agree), and 5 (strongly agree). The highest possible score was 50, and the neutral score was 30. If the respondent's score was above the neutral score it was considered as a favorable attitude, and if the score was below neutral score it was considered as an unfavorable attitude [10].
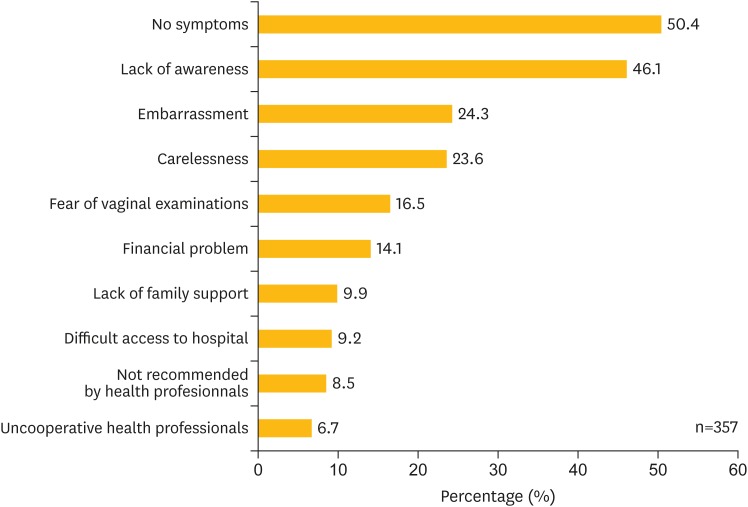
The fourth part was related to the question about cervical cancer screening practice with ‘Yes’ or ‘No’ answer and the fifth part was related with the possible barriers, there were 10 options with multiple choices, which is demonstrated in Fig. 1.
Fig. 1.
Barriers to participation in cervical cancer screening.
4. Validity and reliability
Content validity was established by extensive literature review, consulting with the research advisor, subject experts, and peer review. The tool was forward and backward translated into English and Nepali to retain the same concept. The reliability was maintained by pretesting in 35 women in the same setting. The internal consistency of the questionnaires was accomplished by estimating the Cronbach's α value based on the recommendation of >0.70. The Cronbach's α value calculated was 0.90.
5. Statistical analysis
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS version 16.0; IBM Corp., Armonk, NY, USA). Descriptive statistics were used to describe the women's socio-demographic characteristics and KAP scores. Cross-tabulations were used to describe the association of age, marital status, education, ethnicity and family history of cancer with knowledge, attitude and practice of cervical cancer screening. Binary logistic regression analysis was done for factors predictive towards likely to attend the screening. The χ2 test was used for statistical significance. Odds ratio (OR) was calculated at 95% CI, p<0.05 was considered as significant.
RESULTS
Total of 360 participants was recruited for this study. The majority (62.2%) of participants were from the age group of 20–29 years. Mean age of the participants was 30.13±10.4. Married women were 86.9%, and illiterate were 45.6%. Among the literate women, 77.5% of the women's education level was secondary or more. Brahmin and Chhetri ethnic groups occupied 67.5% followed by Dalit 21.1%. Maximum number (93.1%) of people were Hindu followed by Buddhism 3.3%. Around 8.1% of women had a positive family history of cancer (Table 2).
Table 2. Socio-demographic characteristics of the participants (n=360).
| Characteristics | Values | |
|---|---|---|
| Age | ||
| 20–29 | 224 (62.2) | |
| 30–39 | 70 (19.4) | |
| 40–49 | 36 (10.0) | |
| 50–59 | 22 (6.1) | |
| Above 60 | 8 (2.2) | |
| Mean age | 30.13±10.4 | |
| Marital status | ||
| Unmarried | 47 (13.1) | |
| Married | 313 (86.9) | |
| Education | ||
| Illiterate | 164 (45.6) | |
| Literate | 196 (54.4) | |
| Education level (n=196) | ||
| Informal education | 13 (6.6) | |
| Primary level | 32 (15.3) | |
| Secondary level | 82 (41.8) | |
| Higher secondary and above | 69 (35.7) | |
| Ethnicity | ||
| Chhetri | 172 (47.8) | |
| Brahmin | 71 (19.7) | |
| Dalit | 76 (21.1) | |
| Janajati | 22 (6.1) | |
| Don't want to answer | 19 (5.3) | |
| Religion | ||
| Hinduism | 335 (93.1) | |
| Buddhism | 12 (3.3) | |
| Christianity | 9 (2.5) | |
| Islam | 4 (1.1) | |
| Family history of cancer | ||
| Positive | 29 (8.1) | |
| Negative | 285 (79.2) | |
| Don't know | 46 (12.8) | |
Values are presented as frequency (%) or mean±standard deviation.
Table 3 demonstrates the different level of scores of the knowledge, attitude, and practice of cervical cancer screening of the study participants. More than 87% of participants had inadequate level of knowledge with the mean score 8.04±5.13 (maximum score was 30 and range of the score obtained by the participants was from 0 to 23) but 71.7% had favorable attitude towards cervical cancer screening with mean score 32.44±11.53 (maximum score was 50, and the range of the score obtained by participants was from 0–47). There was a significant portion of women (86.4%) who had never done any cervical cancer screening test. The proportion of adequate vs. inadequate knowledge, favorable vs. unfavorable attitude and screening (practice) vs. not screening scores of the participants were all statistically significant (p<0.001).
Table 3. Knowledge, attitude, and practice score of the participants.
| Items | Values | p-value | |
|---|---|---|---|
| Knowledge score (n=357) | <0.001 | ||
| Adequate | 45 (12.6) | ||
| Inadequate | 312 (87.4) | ||
| Mean score | 8.04±5.13 | ||
| Range of score | 0–23 | ||
| Attitude score (n=357) | <0.001 | ||
| Favorable | 256 (71.7) | ||
| Unfavorable | 101 (28.3) | ||
| Mean score | 32.44±11.53 | ||
| Range of score | 0–47 | ||
| Practice (n=360) | <0.001 | ||
| Yes | 49 (13.6) | ||
| No | 311 (86.4) | ||
Values are presented as frequency (%) or mean±standard deviation.
Table 1 shows the items on the question and correct response of the participants regarding the knowledge of cervical cancer and screening which included the definition, sign and symptoms, possible risk factors, preventive steps, screening, and treatment. Majority of the participants did not have an adequate, correct response to different questions. Surprisingly only 0.9% of the participants correctly know that Visual Inspection with Acetic Acid (VIA) is also a cervical cancer screening method.
Table 4 presents the association in between knowledge, attitude and practice with different characteristics of the participants such as age, marital status, education, ethnicity, and family history of cancer. Though age ≤30 vs. ≥31 was not significantly associated with attitude (p=0.101; OR=1.53; 95% CI=0.91–2.57), elder women had a favorable attitude towards cervical cancer screening. Marital status, unmarried vs. married was significantly associated with knowledge (p=0.004; OR=0.34; 95% CI=0.16–0.73) and attitude (p<0.001; OR=4.3; 95% CI=2.28–8.12) showing married women had 2.9 times more inadequate knowledge but had a more favorable attitude. The illiterate vs. literate group was significantly associated with attitude (p=0.013; OR=0.54; 95% CI=0.33–0.88) and practice (p=0.007; OR=0.43; 95% CI=0.23–0.80) which means illiterate women were more likely to have a favorable attitude and go for cervical cancer screening. Similarly, the ethnic group of Brahmin and Chhetri vs. others (p=0.000; OR=4.68; 95% CI=2.49–8.80) and family history of cancer positive vs. negative (p=0.000; OR=0.17; 95% CI=0.07–0.39) were significantly associated with the practice of cervical cancer screening, indicating Brahmin and Chhetri had 4.7 times less likely to do the screening and positive family history of cancer group had 5.9 times more chances to go for cervical cancer screening.
Table 4. Association of different variables with knowledge (n=357), attitude (n=357), and practice (n=360).
| Characteristics | Knowledge | Attitude | Practice | ||||
|---|---|---|---|---|---|---|---|
| Inadequate | Adequate | Unfavorable | Favorable | No | Yes | ||
| Age | |||||||
| ≤30 | 207 (58.0) | 35 (9.8) | 75 (21.0) | 167 (46.8) | 208 (57.8) | 34 (9.4) | |
| ≥31 | 105 (29.4) | 10 (2.8) | 26 (7.3) | 89 (24.9) | 103 (28.6) | 15 (4.2) | |
| OR (95% CI) | 0.56 (0.26–1.18) | 1.53 (0.91–2.57) | 0.89 (0.46–1.71) | ||||
| p-value | 0.125 | 0.101 | 0.728 | ||||
| Marital status | |||||||
| Unmarried | 35 (9.8) | 12 (3.4) | 27 (7.6) | 20 (5.6) | 43 (11.9) | 4 (1.0) | |
| Married | 277 (77.6) | 33 (9.2) | 74 (20.7) | 236 (66.1) | 268 (74.4) | 45 (12.5) | |
| OR (95% CI) | 0.34 (0.16–0.73) | 4.30 (2.28–8.12) | 1.80 (0.61–5.27) | ||||
| p-value | 0.004 | 0.000 | 0.274 | ||||
| Education | |||||||
| Illiterate | 144 (40.3) | 17 (4.8) | 35 (9.8) | 126 (35.3) | 133 (36.9) | 31 (8.6) | |
| Literate | 168 (47.1) | 28 (7.8) | 66 (18.5) | 130 (36.4) | 178 (49.4) | 18 (5.0) | |
| OR (95% CI) | 0.70 (0.37–1.34) | 0.54 (0.33–0.88) | 0.43 (0.23–0.80) | ||||
| p-value | 0.291 | 0.013 | 0.007 | ||||
| Ethnicity* | |||||||
| Brahmin & Chhetri | 213 (63.0) | 27 (8.0) | 70 (20.7) | 170 (50.3) | 223 (65.4) | 20 (5.9) | |
| Others | 83 (24.3) | 15 (4.4) | 24 (7.1) | 74 (21.9) | 69 (20.2) | 29 (8.5) | |
| OR (95% CI) | 1.42 (0.72–2.81) | 1.27 (0.74–2.17) | 4.68 (2.49–8.80) | ||||
| p-value | 0.305 | 0.384 | 0.000 | ||||
| Family history of cancer | |||||||
| Positive | 27 (8.7) | 2 (0.6) | 8 (2.6) | 21 (6.8) | 17 (5.4) | 12 (3.8) | |
| Negative | 242 (77.8) | 40 (12.9) | 74 (23.8) | 208 (66.9) | 254 (80.9) | 31 (9.9) | |
| OR (95% CI) | 2.23 (0.51–9.75) | 1.07 (0.45–2.52) | 0.17 (0.07–0.39) | ||||
| p-value | 0.274 | 0.876 | 0.000 | ||||
Values are presented as number (%).
CI, confidence interval; OR, odds ratio.
*Ethnicity-19 participants who did not want to answer their ethnicity were excluded; Others-Dalit and Janajati.
Fig. 1 demonstrates the top 10 possible barriers to participate in cervical cancer screening (n=357). More than 50% of the participant answered that screening was not needful without any symptoms. There were 46.1% women who did not go for screening due to lack of awareness. There was a significant number of women who thought screening was embarrassing (24.3%) and some answered they were too busy or careless (23.6%) to go for screening. Similarly, other barriers were fear of vaginal examination (16.5%), the financial problem (14.1%), lack of family support (9.9%), difficult access to the hospital (9.2%), not recommended by health professionals (8.5%) or uncooperative health professionals (6.7%).
Table 5 shows the factors predictive towards cervical cancer screening practice by the use of binary logistic regression analysis. Factors ethnicity (other ethnic group vs. Brahmin and Chhetri) and family history of cancer (positive vs. negative) were significantly associated with cervical cancer screening practice. Other ethnic groups such as Dalit and Janajati, those who had a positive family history of cancer were more likely to attend the cervical cancer screening. Similarly, married women, those who had adequate knowledge and or favorable attitude were more likely to practice cervical cancer screening, though statistically not significant.
Table 5. Factors predictive towards likely to attend cervical cancer screening.
| Variables | p-value | Exp (B) | 95% CI |
|---|---|---|---|
| Age (>30 vs. <30 yr) | 0.178 | 0.55 | 0.23–1.30 |
| Marital status (married vs. unmarried) | 0.295 | 2.29 | 0.48–10.83 |
| Education (literate vs. illiterate) | 0.922 | 0.95 | 0.41–2.22 |
| Ethnicity (others* vs. Brahmin & Chhetri) | 0.001 | 3.66 | 1.72–7.79 |
| Family history of cancer (positive vs. negative) | 0.000 | 6.08 | 2.36–15.64 |
| Knowledge score (adequate vs. inadequate) | 0.634 | 1.29 | 0.45–3.69 |
| Attitude (favorable vs. unfavorable) | 0.311 | 1.63 | 0.63–4.26 |
| Constant | 0.000 | 0.29 |
CI, confidence interval.
*Others: Dalit and Janajati.
DISCUSSION
This study was conducted in typical rural site- a mid-western very remote district of Nepal. Jumla is known as one of the most backward areas with the total population of 108,921, economically underdeveloped, medically underserved in comparison to the other parts of the country. Half of the people in this region are living below the poverty line [12,13]. Human Development Index (HDI) of Jumla is 0.409 which is one of the lowest in the country, representing the poor indicator in terms of health, literacy, and income [14]. It takes around 30–36 hours risky travel by bus to reach Bharatpur Cancer Hospital [15] or capital city, Kathmandu for diagnosis or treatment of any cancer due to the poor condition road. People need to walk several hours to visit the only hospital situated in district headquarter of Jumla. Despite being the most common cancer of women in Nepal, a systematic screening program is out of reach to the women residing in a remote location. A few months prior to this study we had conducted cervical cancer screening program using cytology and visual tests in the same region. The participation of the women was not encouraging despite being free of cost. There is a significant number of studies done regarding knowledge, attitude and the factors that affect the cervical cancer screening behavior among the health professional as well as in general population in different countries in different settings. However, to the best of our knowledge, this is a first comprehensive study regarding the knowledge, attitude, practice and possible barriers to cervical cancer screening in such a poor resource setting.
We found that majority of the participants (87.4%) had inadequate knowledge and almost equal number of women (86.4%) had never done cervical cancer screening practice, but interestingly 71.7% of the women had a favorable attitude towards cervical cancer screening. These findings of knowledge and practice are almost consistent with the other studies as well, but the positive attitude was higher in this study [10,16,17]. A similar study by Shrestha et al. [18], 2014, reported that 53% had inadequate knowledge, but only 38% had adequate attitude and only 13% had sufficient practice regarding Pap smear test among 100 women in the urban region of Nepal. The author also stated that higher education had significant relation with adequate knowledge, attitude, and practice regarding Pap smear test. Furthermore, literate women were found to have significantly higher cervical cancer screening behavior than illiterate women [19]. But interestingly we found that more proportion of literate women had adequate knowledge, but they had lower favorable attitude and lower practice of screening than the illiterate women, which was statistically significant (p<0.050). As expected, we found that unmarried young women had the higher adequate knowledge, but married women had a higher favorable attitude (p<0.000). Education only might not be enough to motivate the women for screening in a rural region. Therefore, special education program such as school health program and or community health program which not only give one-way education but also to create awareness via discussion among the students (both boys and girls) in school and husband and wife in the community. During such program, the pros and cons of cervical cancer screening, the burden of cervical cancer in person, family, society, and country should be well discussed. Knowledge is basically gained by an educational program which is considered to be a precursor for behavior, but it is not in direct relation, other factors such as attitude also play a role in formulating behavior [20]. Therefore, awareness program should be conducted in such a way that to promote the screening uptake. At the same time, women empowerment, cultural sensitivity of shyness and implementation of such programs should also be addressed. Women health professional and Female Community Health Volunteer (FCHV) can play significant role to overcome with some socio-cultural issue, because women usually feel embarrassed to talk or examined by the male health professional.
One of the striking findings of this study was KAP regarding cervical cancer of the different ethnic group. There are several ethnicities in Nepal, Brahmin and Chhetri are regarded to be higher caste and Janajati and Dalit to be lower. Usually, literacy and education level is also higher among Brahmin and Chhetri ethnic group [21]. But we found that women of Brahmin and Chhetri had the higher inadequate knowledge and unfavorable attitude regarding cervical cancer in comparison to other ethnic groups (Dalit and Janajati) though statistically not significant. Moreover, the practice of cervical cancer screening was significantly higher among the other ethnic group (Dalit and Janajati) than Brahmin and Chhetri (p<0.000). More than two-thirds of the participants in this study belonged to an upper caste ethnic group — Brahmin and Chhetri, but their cervical cancer screening uptake was disappointing despite having higher literacy and education level. So, this finding was very peculiar in this setting and not comparable with other similar studies within the country [10,18]. The possible reasons for less practice of cervical cancer screening by relatively higher educated ethnic group (also known as ‘more advantageous ethnic group’ in Nepal) might be the socio-cultural factor such as cultural sensitivity for shyness, lack of women empowerment or lack of family support and lack of awareness in health-seeking behavior [22]. But in the less advantageous group, despite their poor financial status, women are more empowered, they can decide on their own; these group of women seems to be relatively easy to convince for health-seeking behavior. We tried to find out the possible barriers in between those ethnic groups which showed that “lack of awareness” was significantly common among Brahmin and Chhetri whereas “embarrassment” was more common among others ethnic group (Dalit and Janajati).
Jia et al. [9] in 2013 assessed the knowledge and barriers among women in Wufeng county, a high incidence region of cervical cancer in China, reported that those who had positive history of cancer were more likely to attend cervical cancer screening; in the same way we also found that those women who had positive family history of cancer were almost 6 times more likely to do cervical cancer screening practice (p<0.000) probably because they perceived more susceptibility towards cancer.
It is imperative to address the factors, which are playing as obstacles for successful screening program in a particular region or the entire country. Barrier factors might be different in priority from a separate area or different ethnic group or culture. There were several studies done in Nepal and developing countries around the world with respect to the barriers of cervical cancer screening uptake. Common obstacles found were an embarrassment, fear of pain, no symptoms, lack of counseling, not recommended by a health professional, anxious feeling once the disease was diagnosed, do not know the benefit of screening, not feeling at risk and no apparent reason [3,9,10,23,24,25]. Similarly, most of the barriers in our study were almost same except financial problem, lack of family support, limited or inaccessible access to health care facility and uncooperative health professional in different order of priority. Most of those barriers were related to the knowledge and awareness of client; some were hospital and health professional related; some were family and financial problem-related. Therefore, it is imperative to overcome these barriers; awareness program about cervical cancer is very crucial. Some facts should be counseled such as cervical cancer is initially symptomless, which is preventable to the large extent if periodically screened; in every opportunity, health professional should recommend or co-operate doing screening, and it should also be focused that cervical cancer screening such as VIA is not painful procedure and free of cost according to the national screening guideline [5]. A study conducted in far western rural Nepal among 261 women reported that self-sampling method for cervical cancer screening by human papillomavirus (HPV) DNA test is a viable method in rural areas with limited access to health services and the author suggests further research on this [26]. Nevertheless, it seems not practical at present condition in rural set up for at least 2 reasons — financial and logistics. First, HPV DNA test is not free of cost in Nepal, so it may not be affordable. Second, HPV DNA analysis demands high skilled human resource and advanced setting which is available only on few centers in capital city Kathmandu, and moreover, such cervicovaginal samples should be analyzed within a certain time (normally within 2 weeks) to ensure the good quality of the result. Unfortunately, there is lack of a system to transport this sample to the laboratory of Kathmandu and get a report on time. Therefore, self-sampling might be an option in future provided this test is free and easily available.
Limitation of this study was sampling method since we used the convenience sampling so the result may not be generalized. Moreover, it was a cross-sectional study hence KAP of cervical cancer screening could not be explored in depth because knowledge, attitude and practice are inter-related and many factors play a role [27,28]. There might be some bias regarding practice, a few months prior we had conducted a screening camp so the practice of women might have seemed to be higher than their actual behavior. Despite the randomization, the order of the questions might have had an impact on the result. In spite of these limitations our significant strength was, for the first time, we explored the KAP and barrier factors of the cervical cancer screening among typical rural and more impoverished women.
In conclusion, the adequate knowledge and practice of cervical cancer screening were meager among rural Nepalese women, but most of them had a favorable attitude. There is a need for related awareness programs to promote the uptake of cervical cancer screening test. This study gives insight into the formulation of strategies to overcome with barriers for optimal utilization of screening test in a rural region.
ACKNOWLEDGMENTS
We would like to thank the hospital staffs of Karnali Academy of Health Sciences for assistance during data collection. We also thank all the participants in the study.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this study was reported.
- Conceptualization: T.N., M.M., C.H.
- Data curation: T.N., M.M., M.N., S.N.
- Formal analysis: M.M., S.N.
- Investigation: T.N., M.M., S.R., S.S., M.N.
- Methodology: T.N., M.M., C.H.
- Project administration: T.N., M.M.
- Resources: T.N., M.M., S.R., S.S., C.H.
- Supervision: T.N., C.H.
- Validation: P.M.A., C.H.
- Visualization: T.N.
- Writing - original draft: T.N., M.M.
- Writing - review & editing: T.N., M.M., P.M.A., C.H.
References
- 1.ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre) Human papillomavirus and related diseases in the world. Barcelona: ICO/IARC HPV Information Centre; 2017. [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012 v1.0 [Internet] Lyon: International Agency for Research on Cancer; 2013. [cited 2016 Jan 10]. Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. [Google Scholar]
- 3.Gyenwali D, Pariyar J, Onta SR. Factors associated with late diagnosis of cervical cancer in Nepal. Asian Pac J Cancer Prev. 2013;14:4373–4377. doi: 10.7314/apjcp.2013.14.7.4373. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Comprehensive cervical cancer control: a guide to essential practice. 2nd ed [Internet] Geneva: World Health Organization; 2014. [cited 2016 Dec 3]. Available from: http://www.who.int/reproductivehealth/publications/cancers/cervical-cancer-guide/en/ [PubMed] [Google Scholar]
- 5.Family Health Division (NP) National guideline for cervical cancer screening and prevention in Nepal. Kathmandu: Government of Nepal Ministry of Health & Population; 2010. [Google Scholar]
- 6.Ranjit A, Gupta S, Shrestha R, Kushner AL, Nwomeh BC, Groen RS. Awareness and prevalence of cervical cancer screening among women in Nepal. Int J Gynaecol Obstet. 2016;134:37–40. doi: 10.1016/j.ijgo.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Wellensiek N, Moodley M, Moodley J, Nkwanyana N. Knowledge of cervical cancer screening and use of cervical screening facilities among women from various socioeconomic backgrounds in Durban, Kwazulu Natal, South africa. Int J Gynecol Cancer. 2002;12:376–382. doi: 10.1046/j.1525-1438.2002.01114.x. [DOI] [PubMed] [Google Scholar]
- 8.Gichangi P, Estambale B, Bwayo J, Rogo K, Ojwang S, Opiyo A, et al. Knowledge and practice about cervical cancer and Pap smear testing among patients at Kenyatta National Hospital, Nairobi, Kenya. Int J Gynecol Cancer. 2003;13:827–833. doi: 10.1111/j.1525-1438.2003.13612.x. [DOI] [PubMed] [Google Scholar]
- 9.Jia Y, Li S, Yang R, Zhou H, Xiang Q, Hu T, et al. Knowledge about cervical cancer and barriers of screening program among women in Wufeng county, a high-incidence region of cervical cancer in China. PLoS One. 2013;8:e67005. doi: 10.1371/journal.pone.0067005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shrestha S, Dhakal P. Knowledge, attitude and practice regarding cervical cancer screening among women attending a teaching hospital, Bharatpur, Chitwan. J Family Reprod Health. 2017;11:18–23. [PMC free article] [PubMed] [Google Scholar]
- 11.Oche MO, Kaoje AU, Gana G, Ango JT. Cancer of the cervix and cervical screening: current knowledge, attitude and practices of female health workers in Sokoto, Nigeria. Int J Med Med Sci. 2013;5:184–190. [Google Scholar]
- 12.Central Bureau of Statistics (NP) National population and housing census 2011 (national report) Kathmandu: Government of Nepal National Planning Commission Secretariat; 2012. [Google Scholar]
- 13.Government of Nepal National Planning Commission; Oxford Poverty and Human Development Initiative. Nepal's multidimensional poverty index: analysis towards action. Kathmandu: Government of Nepal National Planning Commission; 2018. [Google Scholar]
- 14.Government of Nepal National Planning Commission; United Nations Development Programme. Nepal human development report 2014: beyond geography, unlocking human potential. Kathmandu: Government of Nepal National Planning Commission; 2014. [Google Scholar]
- 15.Gyenwali D, Khanal G, Paudel R, Amatya A, Pariyar J, Onta SR. Estimates of delays in diagnosis of cervical cancer in Nepal. BMC Womens Health. 2014;14:29. doi: 10.1186/1472-6874-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhendup T, Tshering P. Cervical cancer knowledge and screening behaviors among female university graduates of year 2012 attending national graduate orientation program, Bhutan. BMC Womens Health. 2014;14:44. doi: 10.1186/1472-6874-14-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aweke YH, Ayanto SY, Ersado TL. Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: community-based cross-sectional study. PLoS One. 2017;12:e0181415. doi: 10.1371/journal.pone.0181415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shrestha P. Knowledge, attitude, and practice regarding Pap smear test among women in Ward no. 14, Dharan [master's thesis] Tromsø: UiT The Arctic University of Norway; 2014. [Google Scholar]
- 19.Acharya Pandey R, Karmacharya E. Cervical cancer screening behavior and associated factors among women of Ugrachandi Nala, Kavre, Nepal. Eur J Med Res. 2017;22:32. doi: 10.1186/s40001-017-0274-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Waller J, McCaffery K, Wardle J. Measuring cancer knowledge: comparing prompted and unprompted recall. Br J Psychol. 2004;95:219–234. doi: 10.1348/000712604773952430. [DOI] [PubMed] [Google Scholar]
- 21.Bista DB. People of Nepal. 6th ed. Kathmandu: Ratna Pustak Bhandar; 1996. [Google Scholar]
- 22.Gurung DD, Bisht S International Centre for Integrated Mountain Development. Women's empowerment at the frontline of adaptation: emerging issues, adaptive practices, and priorities in Nepal. Kathmandu: International Centre for Integrated Mountain Development; 2014. [Google Scholar]
- 23.Thippeveeranna C, Mohan SS, Singh LR, Singh NN. Knowledge, attitude and practice of the Pap smear as a screening procedure among nurses in a tertiary hospital in north eastern India. Asian Pac J Cancer Prev. 2013;14:849–852. doi: 10.7314/apjcp.2013.14.2.849. [DOI] [PubMed] [Google Scholar]
- 24.Singh E, Seth S, Rani V, Srivastava DK. Awareness of cervical cancer screening among nursing staff in a tertiary institution of rural India. J Gynecol Oncol. 2012;23:141–146. doi: 10.3802/jgo.2012.23.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tran NT, Taylor R, Choe SI, Pyo HS, Kim OS, So HC. Knowledge, attitude and practice (KAP) concerning cervical cancer and screening among rural and urban female healthcare practitioners in the Democratic People’s Republic of Korea. Asian Pac J Cancer Prev. 2011;12:3023–3028. [PubMed] [Google Scholar]
- 26.Johnson DC, Bhatta MP, Smith JS, Kempf MC, Broker TR, Vermund SH, et al. Assessment of high-risk human papillomavirus infections using clinician- and self-collected cervical sampling methods in rural women from far western Nepal. PLoS One. 2014;9:e101255. doi: 10.1371/journal.pone.0101255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ranabhat S, Tiwari M, Dhungana G, Shrestha R. Association of knowledge, attitude and demographic variables with cervical Pap smear practice in Nepal. Asian Pac J Cancer Prev. 2014;15:8905–8910. doi: 10.7314/apjcp.2014.15.20.8905. [DOI] [PubMed] [Google Scholar]
- 28.Shekhar S, Sharma C, Thakur S, Raina N. Cervical cancer screening: knowledge, attitude and practices among nursing staff in a tertiary level teaching institution of rural India. Asian Pac J Cancer Prev. 2013;14:3641–3645. doi: 10.7314/apjcp.2013.14.6.3641. [DOI] [PubMed] [Google Scholar]