Abstract
Background:
Neck circumference (NC) is an index of subcutaneous adipose tissue distribution in an area of the upper part of the body. The aim of this study was to assess whether NC can be used as an indicator of central obesity and to determine the prevalence of central obesity in apparently healthy Bosnian young adults.
Methods:
Participants for this cross-sectional study were recruited using the snowball method. NC was measured in horizontal straight position by placing the top edge of a plastic tape only below the laryngeal prominence and perpendicular to the longitudinal axis of the neck, with the head positioned in the Frankfort horizontal plane. Body mass index, waist circumference (WC), and waist-to-hip ratio were taken following the WHO guidelines.
Results:
The study included 111 second year University of Sarajevo Dentistry students (49 students of male gender and 62 students of the female gender). Determined the optimal cutoff value of NC in the detection of central obesity based on WC values in healthy young participants of male gender was ≥37.45 cm (P < 0.001), while in healthy young participants of the female gender, it was ≥32.75 cm (P < 0.001). Based on the WHO guidelines for WC, central obesity was determined in 24.49% (n = 12) of male patients, and in 29.03% (n = 18) of female participants included in our investigation (P < 0.05).
Conclusions:
The results of the present study indicate that NC may be used as a screening tool for central obesity in healthy young adults. Prevalence of central obesity observed among student population suggests that there is a justified need for an implementation of healthy lifestyle programs in this population that would have preventive purposes.
Keywords: Anthropometry, central obesity, gender difference, metabolic syndrome, young adults
Introduction
Neck circumference (NC) is an index of subcutaneous adipose tissue distribution in an area of the upper part of the body.[1] Results of current, yet still limited, investigations have shown that NC represents simple, fast, and easily accessible method in identification of individuals with obesity. NC plays an independent contribution to predicting the cardio-metabolic abnormalities beyond the classical anthropometric indices of body mass index (BMI), waist circumference (WC), and waist-hip-ratio (WHR) and may be used as an optimal screening method in other obesity-related chronic diseases.[2]
In an assessment of central obesity most frequently used anthropometric methods are WC and WHR. Studies have shown they have not only numerous advantages but also important disadvantages.[3] Novel studies suggest that NC can also be used as an index of central obesity.[4] Framingham heart study that included middle-aged population demonstrated that NC was independently associated with visceral adiposity and BMI.[5] Studies that evaluated the possible use of NC as an indicator of central obesity in healthy young adults are scarce.
Majority of studies conducted to date have evaluated the prevalence of overweight and obesity in middle-aged and elderly population or in children and adolescents.[6,7,8] According to WHO data, the prevalence of obesity in adults of Bosnia and Herzegovina in 2008 was 26.5% (23.8% in men and 28.9% in women).[9] Obesity in childhood and young adulthood is not a benign problem. It is often associated with the presence of the metabolic syndrome and asymptomatic cardiovascular disease. Young adults with obesity who had elevated glycosylated hemoglobin of >8% have an increased likelihood of having atheromata in the aorta and coronary arteries. Childhood obesity strongly predicts the risk for obesity and metabolic syndrome in later adulthood.[10]
Therefore, the aim of the present study was to assess whether NC can be used as an indicator of central obesity and to determine the prevalence of central obesity in apparently healthy Bosnian young adults.
Methods
This cross-sectional study included the second year University of Sarajevo Dentistry students. The study participants were recruited using the snowball method.[11] The research was undertaken during human physiology course practical exercises between April and June 2016. Inclusion criteria were that the study participants should be apparently healthy persons between 19 and 24 years of age of both genders. We excluded the individuals with goiter and other neck masses and deformity. Furthermore, subjects with a history of thyroid disease, diabetes, dyslipidemia, hypertension, or any other disease were excluded from the study. All patients included in the study signed informed consent and the study protocol was approved by the Local Ethics Committee. Individual questionnaires were especially designed for the study and data such as general characteristics, lifestyle characteristics (smoking, alcohol consumption, and physical activity), anthropometric characteristics, values of blood pressure (BP), data on family history of cardiovascular diseases, and diabetes mellitus were recorded.
Measurements were obtained in light clothes, fasting, and standing, without shoes and at the end of expiration. NC was measured with regular plastic tape to the nearest 0.5 mm. The participants were standing erect with the arms hanging loosely at sides and head positioned in a horizontal straight position. The top edge of a plastic tape was placed only below the laryngeal prominence and perpendicular to the longitudinal axis of the neck, with the head positioned in the Frankfort horizontal plane.[12] Weight was measured using a digital scale to the nearest 0.1 kg with only undergarments, and height was determined using a portable stadiometer to the nearest 1 mm barefoot. WC was taken horizontally to the nearest 1 mm, using a plastic tape measure at the midpoint between the costal margin and iliac crest in the midaxillary line. According to the International Diabetes Federation guidelines values of WC >94 cm for men and >80 cm for women of European descent define central obesity.[13] BMI was calculated as weight (kilogram) divided by the square of height (meter). WHR ratio was calculated by dividing the WC (cm) by the hip circumference (cm). Optimal values of WHR according to the current WHO guidelines are up to 0.90 for men and up to 0.85 for women.[13]
Blood pressure (BP) was measured using trained personnel in the morning hours (8:30–11:30 am). The patients were advised to avoid tea, coffee, energy drinks, and physical exercises in the morning of the examination day until the measurements were taken. Before the BP measurement, the participants were asked to sit still for 10 min. BP was measured 3-times with a 5-min rest interval between the measurements, with the participant being in a sitting position. BP was measured using a standard mercury-column sphygmomanometer. The average of three BP measurements was calculated. Essential hypertension was defined as average systolic blood pressure (SBP) ≥140 mmHg and/or average diastolic blood pressure (DBP) ≥90 mmHg, and/or currently receiving treatment for hypertension with antihypertensive medicine. We defined prehypertension as SBP between 120 and 139 mmHg or DBP between 80 and 89 mmHg according to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High BP (JNC-7).[14]
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) software version 20.0 (IBM, Chicago, Illinois, USA) was used for the statistical analysis of data. The Kolmogorov–Smirnov test was used to test the normality of distribution of variables. For the parametric comparisons between two independent groups, a student t-test was used. Receiver operating characteristic (ROC) curves were constructed by calculating the sensitivities and specificities of NC at several cutoff points. Chi-square test was used to assess the difference between categorical variables. P < 0.05 was considered statistically significant.
Results
The total sample comprised 111 participants (49 students of male gender and 62 students of female gender). In the total sample of participants, mean age was 21.83 ± 1.43 years.
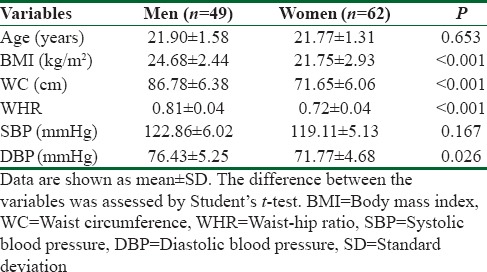
Table 1 shows that there was no significant difference in age between male and female participants included in the study. Significant difference was observed in values of BMI, WC, and WHR between the genders. Significant difference between the genders was not determined in values of SBP. However, significant difference in values of DBP based on gender was established.
Table 1.
Baseline characteristics of study participants
As shown in Figure 1, optimal cutoff value of NC as an indicator of central obesity determined by ROC curve in healthy young participants of male gender was ≥37.45 cm. Area under the curve (AUC) for determined cutoff value was 0.862 with 95% confidence interval (95% CI) of 0.763–0.961 (P < 0.001). For calculated optimal NC cutoff value of ≥37.45 cm, maximal specificity was 83.33%, and maximal sensitivity was 68.00%.
Figure 1.
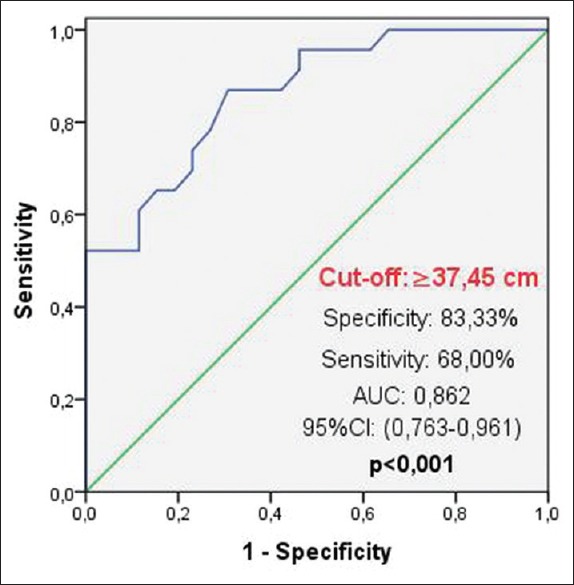
Optimal cutoff value of neck circumference determined by receiver operating characteristic curve for the detection of central obesity defined by waist circumference values in healthy young participants of male gender
Figure 2 shows that optimal cutoff value of NC as an indicator of central obesity determined by ROC curve in healthy young participants of female gender was ≥32.75 cm. AUC for determined cutoff value was 0.811 with 95% CI of 0.695–0.962 (P < 0.001). For calculated optimal NC cutoff value of ≥32.75 cm, maximal specificity was 85.00%, and maximal sensitivity was 63.63%.
Figure 2.
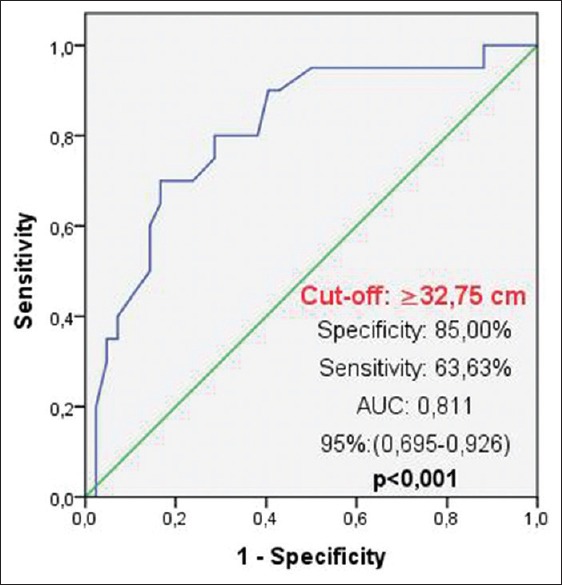
Optimal cutoff value of neck circumference determined by receiver operating characteristic curve for the detection of central obesity defined by waist circumference values in healthy young participants of female gender
Based on the WHO guidelines for WC, central obesity was determined in 24.49% (n = 12) of male participants, and in 29.03% (n = 18) of female participants included in our investigation. Observed difference in the prevalence of central obesity between genders was statistically significant (P < 0.05).
Discussion
To the best of our knowledge, we are the first to report possible use of NC as an indicator of central obesity defined by WC values in apparently healthy Bosnian young adults. In a recent study, Hingorjo et al.[15] reported that NC is a potentially useful initial screening tool for overweight and general type of obesity based on BMI values in Pakistani student population.
It is important to emphasize that use of NC as a parameter of adiposity has just recently been introduced. Its usage is not widely accepted and only of late, the importance of its possible measurement is explored. The study represents a contribution in encouragement of NC measurement in everyday clinical practice. However, confounding factors such as cigarette smoking, alcohol intake, and physical activity were collected but not assessed within the present study, and this may represent a potential source of bias for obtained findings. The similar future study should take into consideration these factors.
Obtained results suggest that NC can be used in the detection of central obesity. As an indicator of upper body/visceral obesity, NC has been shown to be associated with diverse metabolic abnormalities. Although the explanation for the strong association between visceral fat and metabolic abnormalities is not known, according to recent hypothesis, visceral fat represent “ectopic fat depot” which is associated with greater infiltration of adipose tissue with inflammatory cells, excess release of potentially harmful cytokines, and reduced release of beneficial adipokines.[16]
In an assessment of central obesity, WC is most frequently used the method. Based on WHO guidelines for WC, results of the present study have shown that central obesity was more prevalent in female gender and are in accordance with observations made by other authors.[17] Results of a study conducted among Turkish students of both genders have determined the prevalence of central obesity similar to the one observed in our research.[18] However, it should be noted that WC measurement in an assessment of central obesity is associated with numerous disadvantages such as dependence of WC from the constitution of individuals, their muscle mass, gut content, respiratory movements, and clothing. Standard protocol for WC measurement still does not exist. In comparison with WC, NC has important advantages. Studies to date have shown good reliability of NC measurement in an assessment of adiposity that does not require multiple measurements for obtaining the precision. Furthermore, NC does not depend on the time of measurement (exp. preprandial and postprandial period), and its assessment is especially practical in winter, as well as in the frequent healthcare institutions.[19]
The strengths of the present study are that it represents the first study that evaluated the potential use of NC as an indicator of central obesity based on WC values in young participants of Bosnian descent. We have also determined gender-specific cut-off values for NC in the detection of central obesity, which is of importance since studies have shown that ethnic background and gender affect values of anthropometric parameters.[2] Furthermore, since central obesity is one of the components of the metabolic syndrome, results of the present study have shown that screening and prevention of the metabolic syndrome should start from a young age.
In interpreting the findings of the current study, several limitations should be acknowledged. First, the sample size was small consisting of healthy young adults from a select population, and therefore, the results cannot be generalized over the whole population. Second, the cross-sectional design of the study prevents us from deducing any causal relations between our findings. Third, NC is used to represent upper-body subcutaneous fat. We did not perform radiographic measures to quantify this depot of fat directly. Considering the limitations of our study, further large prospective population-based studies are still needed to validate our findings.
Conclusions
The results of the present study indicate that NC may be used as a screening tool for central obesity. If obtained findings are confirmed in large prospective population-based studies then NC measurement should be included in everyday clinical practice as a simple, practical, and reliable method of central obesity assessment in healthy young adults. Prevalence of central obesity observed among student population included in our investigation suggests that there is a justified need for an implementation of healthy lifestyle programs in this population that would have preventive purposes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ferretti Rde L, Cintra Ide P, Passos MA, de Moraes Ferrari GL, Fisberg M. Elevated neck circumference and associated factors in adolescents. BMC Public Health. 2015;15:208. doi: 10.1186/s12889-015-1517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou JY, Ge H, Zhu MF, Wang LJ, Chen L, Tan YZ, et al. Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovasc Diabetol. 2013;12:76. doi: 10.1186/1475-2840-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taheri M, Kajbaf TZ, Taheri MR, Aminzadeh M. Neck circumference as a useful marker for screening overweight and obesity in children and adolescents. Oman Med J. 2016;31:170–5. doi: 10.5001/omj.2016.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saka M, Türker P, Ercan A, Kiziltan G, Baş M. Is neck circumference measurement an indicator for abdominal obesity? A pilot study on Turkish adults. Afr Health Sci. 2014;14:570–5. doi: 10.4314/ahs.v14i3.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preis SR, Massaro JM, Hoffmann U, D'Agostino RB, Sr, Levy D, Robins SJ. Neck circumference as a novel measure of cardiometabolic risk: The Framingham Heart Study. J Clin Endocrinol Metab. 2010;95:3701–10. doi: 10.1210/jc.2009-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khabazkhoob M, Emamian MH, Hashemi H, Shariati M, Fotouhi A. Prevalence of overweight and obesity in the middle-age population: A Priority for the health system. Iran J Public Health. 2017;46:827–34. [PMC free article] [PubMed] [Google Scholar]
- 7.Binu J, Harnagle R. A Study on the prevalence of overweight and obesity and its influencing factors among rural geriatric population in Kerala. Int J Curr Microbiol Appl Sci. 2014;3:284–93. [Google Scholar]
- 8.Zhou Y, Zhang Q, Wang T, Zhang Y, Xu B. Prevalence of overweight and obesity in Chinese children and adolescents from 2015. Ann Hum Biol. 2017;44:642–3. doi: 10.1080/03014460.2017.1371224. [DOI] [PubMed] [Google Scholar]
- 9.WHO Noncommunicable diseases country profiles. 2014. [Last accessed on 2017 Sep 09]. Available from: http://www.who.int/nmh/countries/en .
- 10.Baalwa J, Byarugaba BB, Kabagambe EK, Otim AM. Prevalence of overweight and obesity in young adults in Uganda. Afr Health Sci. 2010;10:367–73. [PMC free article] [PubMed] [Google Scholar]
- 11.Gyarmathy VA, Johnston LG, Caplinskiene I, Caplinskas S, Latkin CA. A simulative comparison of respondent driven sampling with incentivized snowball sampling – The “strudel effect”. Drug Alcohol Depend. 2014;135:71–7. doi: 10.1016/j.drugalcdep.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papandreou D, Noor ZT, Rashed M, Jaberi HA. Association of neck circumference with obesity in female college students. Open Access Maced J Med Sci. 2015;3:578–81. doi: 10.3889/oamjms.2015.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation. Geneva: World Health Organization; 2008. [Last accessed on 2017 Sep 09]. Available from: http://www.whqlibdoc.who.int/publications/2011/9789241501491_eng.pdf . [Google Scholar]
- 14.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: New challenges of the old problem. Arch Intern Med. 2004;164:2126–34. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- 15.Hingorjo MR, Qureshi MA, Mehdi A. Neck circumference as a useful marker of obesity: A comparison with body mass index and waist circumference. J Pak Med Assoc. 2012;62:36–40. [PubMed] [Google Scholar]
- 16.Jensen MD. Role of body fat distribution and the metabolic complications of obesity. J Clin Endocrinol Metab. 2008;93:S57–63. doi: 10.1210/jc.2008-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beigh SH, Jain S. Prevalence of metabolic syndrome and gender differences. Bioinformation. 2012;8:613–6. doi: 10.6026/97320630008613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karakaş P, Bozkır MG. Anthropometric indices in relation to overweight and obesity among Turkish medical students. Arch Med Sci. 2012;8:209–13. doi: 10.5114/aoms.2012.28546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo X, Li Y, Sun G, Yang Y, Zheng L, Zhang X, et al. Prehypertension in children and adolescents: Association with body weight and neck circumference. Intern Med. 2012;51:23–7. doi: 10.2169/internalmedicine.51.6347. [DOI] [PubMed] [Google Scholar]


