Summary
The purpose of this study is to develop a reliable and valid tool for measuring the dynamic sitting balance of wheelchair users with spinal cord injury. The balance tests were performed in nine patients with chronic spinal cord injury (average of 17.2 years postinjury) between levels C6 and L1, while they were sitting in their wheelchairs and on a standardized stool (unsupported sitting), twice, 7 days apart. Limits of stability (LOS) and sequential weight shifting (SWS) were designed in this study. The balance tests measured participants' volitional weight shifting in multiple directions within their base of support. Their mobility scores on the Spinal Cord Independence Measure III were correlated with the balance test results. The LOS results showed moderate to excellent test–retest reliability (intraclass correlation coefficients ranged from 0.673 to 0.990) for both the wheelchair and the unsupported sitting. The SWS results showed moderate to excellent reliability (intraclass correlation coefficients ranged from 0.688 to 0.952). The LOS results correlated significantly with the Spinal Cord Independence Measure III mobility scores only in case of unsupported sitting, but the SWS test results showed significant correlations in both sitting conditions. To sum up, the sitting LOS and SWS tests are reliable and valid tools for assessing the dynamic sitting balance control of patients with spinal cord injury.
Keywords: mobility, reliability, sitting balance, spinal cord injury, validity
Introduction
Approximately 70–80% of people with spinal cord injury (SCI) are dependent for life on a wheelchair for mobility [1]. Good sitting balance control is essential for such people because they are often confined to the sitting position when performing the activities of daily living (ADLs). Activities that require sitting quietly (such as feeding, grooming, and bathing), dynamic activities (such as propelling their wheelchair up or down ramps) as well as the ADLs require different degrees of sitting balance control. When ascending a ramp, people with SCI lean forward as far as possible to prevent the wheelchair from tipping backwards. When descending, they lean back as far as possible to prevent falling [2]. These techniques require maximal postural excursions. That is why investigators studying balance control in an SCI population employ maximal postural sway as an outcome measure.
Sitting balance control directly affects transfer performance [3]. An appropriate sitting position is fundamental to providing a stable base of support for transfer activities. A sense of position in space is another crucial factor when attempting a transfer. In addition, the ability to precisely and accurately control intentional movements of the centre of gravity in different directions is important. Better directional control provides more accurate control in performing a variety of transfer activities. When individuals transfer from short sitting (with the hips and knees at approximately 90°) to an unsupported position, they require good directional control. Transfer from a wheelchair to a bathtub is a common example.
Falls are a major problem for SCI sufferers. In a prospective study of 659 community-dwelling wheelchair users who suffered from SCI (age 54.8 ± 12.6 years), 31% reported a total of 553 fall events [4]. In a retrospective study by the same group, a review of 45 individuals with SCI showed that 24 (53%) of them had experienced a total of 27 fall episodes. The major factor contributing to falls was found to be loss of balance during functional activities [5]. Falls most often occurred during transfer (44%), reaching (11%), propelling a wheelchair (15%), moving in bed (22%), transferring to or riding in a vehicle (30%), and taking a shower (8%). Wheelchair users with SCI have been found to have decreased or absent trunk control, leading to poor sitting balance and stability, which in turn may cause falls during transfer [6].
A supported or unsupported short sitting position is commonly adopted by people with SCI when performing the ADLs. However, most previous studies assessing sitting balance control have focused on the maximum displacement of the centre of pressure (COP) when sitting with knees straight, which are relatively less functional. In addition, the assessment of sitting balance control should include the diagonal movements commonly required in transfer. The time and movement control required to achieve different excursions have not been investigated in previous studies, but they are important factors in dynamic sitting balance control. When performing transfer activities, people with SCI usually lean the trunk forward to lift their buttocks off the initial surface and quickly pivot the buttocks to the target surface using a twisting motion [7]. Moreover, the functional activities do not end in a single direction, but in a sequence of movements. The present study was therefore designed to develop laboratory-based tests for use in a clinical setting to assess the dynamic sitting balance control of wheelchair users with SCI.
Materials and methods
Nine persons with SCI participated in this study—six females and three males (refer to Table 1). The participants were aged 35–63 years (mean ± standard deviation, 50.6 ± 10.7 years). Time since injury averaged 17.2 years (from 2 years to 48 years). Their level of injury ranged from C6 to L1, according to the International Standards for Neurological and Functional Classification of SCI. One year postinjury is commonly classified as the chronic stage because neural recovery plateaus at approximately 12 months postinjury [8]. The inclusion criteria for the study were as follows: able to sit unsupported; at least 1 year postinjury; incomplete injury according to the American Spinal Injury Association Impairment Scale; aged ≥18 years; and able to communicate and follow instructions. The exclusion criteria were the following: unstable cardiopulmonary disease; serious complications related to the SCI, such as pressure ulcers; contracture or marked hypertonicity of the muscles; poorly controlled hypertension; and metastatic cancer. Written consent was obtained from all participants prior to the start of the study. The study was approved by the Ethics Committee of the Hong Kong Polytechnic University, Hung Hom, Hong Kong (HSEARS09902245R). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Table 1.
Characteristics of the participants.
| Participant | Age (y) | Time since injury (y) | Injury level | ASIA grade |
|---|---|---|---|---|
| 1 | 35 | 22 | T1 | B |
| 2 | 36 | 10 | T1 | B |
| 3 | 57 | 11 | T1 | B |
| 4 | 63 | 48 | T1 | C |
| 5 | 61 | 2 | T1 | C |
| 6 | 58 | 13 | L1 | D |
| 7 | 55 | 10 | C7 | D |
| 8 | 48 | 10 | T12 | D |
| 9 | 42 | 29 | C6 | B |
ASIA = American Spinal Injury Association.
Testing procedure
Two dynamic sitting balance control tests were conducted—limits of stability (LOS) test and sequential weight shifting test. The two tests were performed in patients either in supported or unsupported sitting conditions.
Instrumentation
The setup consisted of a tailor-made force platform (90 cm × 90 cm) and an adjustable-height screen placed 1.5 m in front of the participants on which the COP was continuously displayed. Participants' COP was measured by four load cells (SBDEG; Measurement Specialties Inc., Schaevitz, VA, USA) mounted on the platform. The measurement range of the load cells was 40–400 pound force. All movement data from the force platform were sampled and digitized via a multifunction data acquisition USB (NI USB-6009; National Instruments, Austin, Texas, USA) with an eight-channel analog-to-digital converter at a sample rate of 1000 Hz. It was connected to a computer that was programmed using tailored LabView software (version 8.6; National Instruments) to display and store in real time the motion of the COP during the sitting balance tests.
Limits of stability
Supported sitting was defined as being seated in the patient's own wheelchair without resting on the back support in case of paraplegia or on both the back and the head supports in case of tetraplegia at the beginning of the balance tests. Patients might get support from the wheelchair when they moved their centre of gravity close to the LOS. Unsupported sitting was defined as sitting on a standardized stool without any support but with an adjustable seat height. Each participant's hips, knees, and ankles were kept at approximately 90° of flexion, with the feet shoulder-width apart while resting on the platform. A cushion was placed on the stool for comfort and to reduce the risk of generating pressure sores during testing. Each participant underwent practice trials for familiarization prior to the actual balance test.
For the LOS test in sitting condition, the traditional standing protocol, which has widely been used in both research and clinical studies [9], was adopted. The test measured the intentional weight shifting ability in multiple directions within their base of support. The initial COP was displayed at the centre of the screen, together with eight target positions in front, right front, right, right back, back, left back, left, and left front. The participants were required to move the COP trace on the screen towards one of eight selected target positions by shifting their weight within their LOS as quickly and as smoothly as possible when one of the visual targets appeared. There was a 20-second rest period between trials to minimize fatigue that might affect performance. The participants wore a safety harness, which was connected to an overhead suspension frame, during the unsupported sitting tests. The investigator was beside the participant for safety. There was a 2-second baseline measurement of COP sway prior to the appearance of the visual target. Each direction was repeated three times, and the results were averaged.
A computer program was developed to record the following parameters: (1) reaction time—the time from the appearance of a target to the onset of the voluntary shifting of the COP; (2) maximum excursion—the maximum displacement of the COP in the target direction; (3) directional control—a comparison of the amount of movement of the COP in the on-target direction with the amount of off-target displacement.
In the supported trials, the data from both the eight directions and the “combined forward” direction, which consisted of data of forward, right forward, and left forward targets only, were captured for data analysis. The “combined forward” direction was analysed because the other five directions could, to some extent, be affected by the wheelchair's arm rests and back support.
Sequential weight shifting
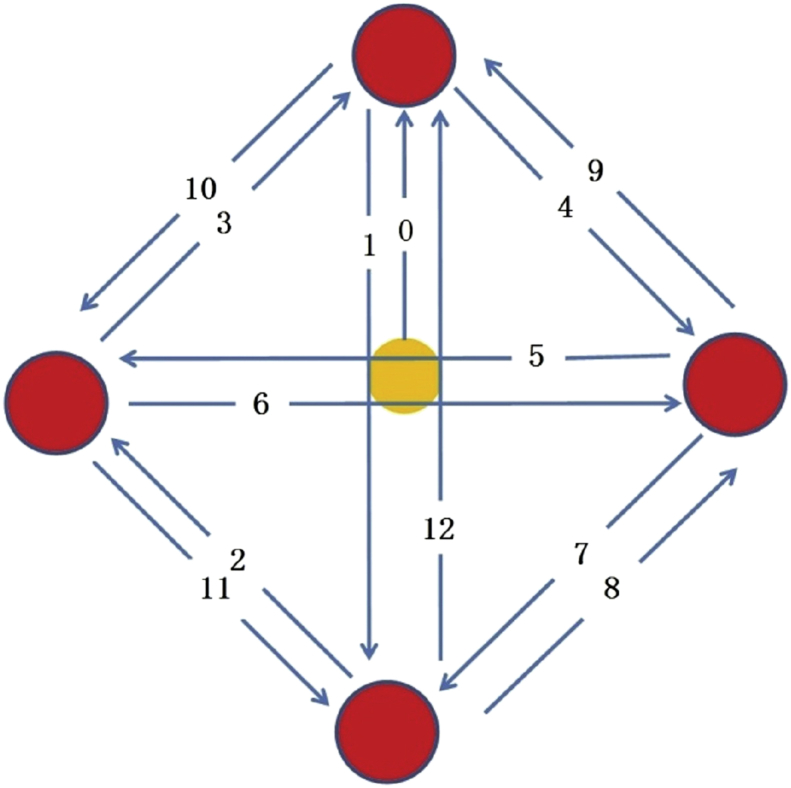
The sitting positions were the same as those used in the LOS test. As soon as a target appeared, participants were asked to shift their COP to move the screen trace to the target as quickly as possible without losing their balance. Twelve targets appeared sequentially. When each target was hit, it disappeared and another appeared. The 12 targets appeared above, left, below, and right of the centre (Fig. 1). The distance from the centre to each target was 75% of that patient's maximal excursion, as determined in the LOS test. The trajectory is shown in Fig. 1. The participants had continuous visual feedback about the position of their COP from the screen as they performed the weight shifts. The total time and directional control for participants to hit the 12 targets sequentially were computed.
Fig. 1.
Trajectory of the targets in SWS. The filled yellow circle denotes the centre, filled red circles denote the target locations and the arrows denote the trajectory. SWS = sequential weight shifting.
Modified functional reach test
The modified functional reach test used [10] has been shown to have excellent test–retest reliability [intraclass correlation coefficient (ICC) 0.85–0.94]. The participants were seated in their own wheelchairs. A ruler was placed across the participant's shoulder at the level of the acromion. Their hips, knees, and ankles were positioned at approximately 90° of flexion. There was a clearance of 5 cm between the popliteal fossa and the wheelchair. Participants were instructed to sit erect initially with both arms flexed to 90°. The anatomical landmark used to measure functional reach was the ulnar styloid process. This landmark was used in this study instead of the third metacarpal with a fist because the ulnar styloid process is a prominent protrusion not affected by the wrist angle, which varies from patient to patient. The participants were instructed to reach forward as far as possible without losing their balance. They were allowed to use the nonreaching arm for counterbalance, but not for weight bearing or for holding on to surrounding objects. The difference between the starting position and the maximum distance reached was recorded. An average of three trials was performed for data analysis.
Functional assessment
The Spinal Cord Independence Measure III (SCIM III) has been used for rating the comprehensive ability of those with SCI in performing basic everyday tasks. It is an efficient and objective instrument for functional assessment devised by Catz and Itzkovich [11] group at the Loewenstein Rehabilitation Hospital, Ra'anana, Israel. This version has been shown to be highly reliable (ICC = 0.94) and sensitive to changes in function for people with SCI [12], [13]. The Chinese version has also been found to have good internal consistency and reliability [14]. The scale consists of three subscales: “self-care” with four items and scores ranging from 0 to 20; “respiration and sphincter management” with four items and scores ranging from 0 to 40; and “mobility” involving nine items relevant to indoor and outdoor transfers, with scores ranging from 0 to 40. The total score therefore ranges from 0 to 100, with a higher score indicating greater independence in functional activity. Each SCIM III item, except bathing, bladder, and bowel management, is scored through direct observation by a physiotherapist. These three items are self-reported.
Statistical analysis
Intraclass correlation coefficients (ICC3,k) were employed to assess the test–retest reliability of the sitting LOS test and the sequential weight shifting test. An ICC3 model was used for assessing intra-rater reliability, with “k” denoting the number of trials used in the different tests [15]. The ICC values were interpreted according to a rating system suggested by Shrout and Fleiss [16] (<0.40, poor reliability; 0.40–0.75, fair to good reliability; and >0.75, excellent reliability). Correlations between the sitting balance test results and SCIM III mobility scores were analysed using Pearson's product–moment coefficient of correlation. A significance level (α) of 0.05 was chosen for statistical comparisons.
Results
Test–retest reliability of the LOS and sequential weight shifting tests
For the nine participants, the sitting balance tests were repeated in the same order with the same examiner 7 days apart. The LOS test showed excellent reliability (ICCs ranging from 0.751 to 0.990) in terms of reaction time, maximum excursion, and directional control in supported sitting (Table 2), and moderate to excellent reliability (ICCs 0.673–0.955) in the combined forward directions (average of the forward, left forward, and right forward directions). Only seven participants could complete the unsupported sitting trials, but their results also showed excellent reliability (ICCs 0.817–0.947). The SWS results in supported sitting also exhibited moderate to excellent test–retest reliability (ICCs ranging from 0.688 to 0.952). The unsupported sitting trials showed excellent test–retest reliability (ICCs 0.788–0.846).
Table 2.
Test–retest reliability for the limits of stability and sequential weight shifting tests in patients with spinal cord injury.
| Combined forward in supported sitting (n = 9) | Supported sitting (n = 9) | Unsupported sitting (n = 7) | |
|---|---|---|---|
| Limits of stability | |||
| Reaction time | 0.818 | 0.751 | 0.885 |
| Maximum excursion | 0.955 | 0.990 | 0.817 |
| Directional control | 0.673 | 0.863 | 0.947 |
| Sequential weight shifting | |||
| Movement time | 0.688 | 0.788 | |
| Directional control | 0.952 | 0.846 | |
Correlation between sitting balance control results and SCIM III
In supported sitting, neither the results of the modified reach test nor the results of the LOS test (reaction times, maximum excursions, and directional control) correlated with the SCIM III scores (Table 3). In unsupported sitting, instead, the three aforementioned measures from the LOS test showed significant correlations with the SCIM III scores. Finally, the total time and directional control in the SWS test in both supported and unsupported sitting were significantly correlated with the SCIM III scores (Table 3).
Table 3.
Correlations between the sitting balance tests and SCIM III mobility scores.
| Correlation with mobility score of SCIM III (p) | |
|---|---|
| Modified functional reach test | 0.459 (0.252) |
| Combined forward in supported sitting | |
| Limits of stability—reaction time | −0.489 (0.219) |
| Limits of stability—maximum excursion | 0.311 (0.453) |
| Limits of stability—directional control | 0.250 (0.550) |
| Supported sitting | |
| Limits of stability—reaction time | −0.433 (0.284) |
| Limits of stability—maximum excursion | 0.278 (0.505) |
| Limits of stability—directional control | 0.313 (0.451) |
| Sequential weight shifting—movement time | −0.829 (0.011*) |
| Sequential weight shifting—directional control | 0.849 (0.033*) |
| Unsupported sitting | |
| Limits of stability—reaction time | −0.852 (0.015*) |
| Limits of stability—maximum excursion | 0.813 (0.026*) |
| Limits of stability—directional control | 0.889 (0.007*) |
| Sequential weight shifting—movement time | −0.823 (0.044*) |
| Sequential weight shifting—directional control | 0.927 (0.024*) |
*A statistically significant difference at the p < 0.05 confidence level.
SCIM III = Spinal Cord Independence Measure III.
Discussion
The LOS and SWS tests in sitting were developed to measure both the supported and the unsupported dynamic sitting balance control of wheelchair users with chronic SCI. The tests encompass temporal and spatial domains and involve both diagonal and orthogonal displacements. Fast reaction, maximal weight shifting, and accurate movement control are required for the functional aspects of daily living.
Reliability of the tests
These dynamic sitting balance tests were found to have moderate to excellent test–retest reliability. The maximum excursions determined in these tests were similar to those of the modified functional reach test, as reported by Lynch's group in forward reach (average ICC = 0.91) [10]. These tests, however, also include diagonal displacements (right forward, right backward, left forward, and left backward) along with the forward, rightward, backward, and leftward directions. The ability to shift their weight forward and backward is essential for wheelchair users when propelling their wheelchairs up or down ramps [2], but the diagonal pathways are also required for good transfer performance. Apart from measuring the maximum weight shifting, the test requires the wheelchair users with SCI to lean as quickly and as smoothly as possible towards the eight targets; the reaction time and the smoothness of the trajectory are also taken into consideration in the two tests.
In the sequential weight shifting test, the distance from the centre to each target was set at 75% of the LOS. This provided sufficient challenge to avoid any ceiling effect, but it allowed the participants to complete the test, as 100% of the LOS might not be achieved, especially in the diagonal directions. The 75% distance was also suitable for avoiding excessive fatigue.
Correlation of the sitting balance control results with functional assessments
The modified functional reach test results were not correlated with the results on the mobility scale of the SCIM III functional assessment (Table 3). The reason may be that the movements required during the performance of the ADLs are multidirectional, so the forward body movement alone cannot reflect the ADL ability properly.
Although eight directions of movement were tested in supported sitting, the results still did not correlate significantly with the results on the mobility scale of the SCIM III. By contrast, the unsupported sitting measurements correlated well with the functional assessment scores (Table 3). The reaction times had a negative correlation with the mobility scale (r = −0.852), so patients able to react more quickly also had better mobility scores in the functional assessment. Similarly, the participants who could lean more and had better directional control performed better in functional mobility testing. The question arises as to why only the unsupported sitting results show these correlations. In the mobility assessment of the SCIM III, the tests involve lots of transfer activities [11], such as from a wheelchair to a tub or a car and vice versa. These transfers involve lots of unsupported sitting. This may explain why the unsupported sitting results show better correlations.
The sequential weight shifting results, both supported and unsupported, correlated well with the mobility scores of the SCIM III (Table 3). In the ADLs, shifting the body's centre of mass controllably in all directions is often important. In transfer and mobility particularly, wheelchair users have to control the acceleration and deceleration of the trunk in diagonal directions with the right timing. The traditional sitting balance test, like the modified functional reach test, and even the LOS test are not able to assess such functional-related performances. All these may contribute to the high correlation between the sitting balance test results and functional ability, as reflected in the mobility scores of the SCIM III.
The cushion used for the sitting balance test might alter the residual somatosensory input to the participants and affect their motor performance. Further investigation on the sensorimotor interaction is warranted in patients with SCI. In daily activities such as during transfer, the sitting balance also involves the vertical dimension. However, the present sitting balance test was restricted to a two-dimensional perspective only; investigation of multiplanar motion will certainly yield meaningful information regarding sitting balance control of patients with SCI.
This study mainly focused on the reliability and validity of the dynamic sitting balance tests for the general population of wheelchair users with SCI. A future study might profitably amplify these findings by looking into more homogenous groups—men and women, older and younger [17], subacute and chronic, higher and lower injury level [10], [18]—and with a larger sample size.
Conflicts of interest
This research received no specific grant from any other funding agency in the public, commercial, or not-for-profit sectors. No commercial party having a direct financial interest in the research findings reported here has or will confer a benefit upon the authors or upon any organization with which the authors are associated. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Acknowledgements
The authors thank The Hong Kong Polytechnic University for financial support of this study. They also thank the participants and Mr Bill Purves for his English editorial advice.
References
- 1.Post M.W.M., vanAsbeck F.W.A., vanDijk A.J., Schrijvers A.J.P. Services for spinal cord injured: availability and satisfaction. Spinal Cord. 1997;35:109–115. doi: 10.1038/sj.sc.3100362. [DOI] [PubMed] [Google Scholar]
- 2.Sisto S.A., Druin E., Sliwinski M.M. Mosby; St Louis, MO: 2009. Spinal cord injuries management and rehabilitation; pp. 351–379. [Google Scholar]
- 3.Bolin I., Bodin P., Kreuter M. Sitting position: posture and performance in C5–C6 tetraplegia. Spinal Cord. 2000;38:425–434. doi: 10.1038/sj.sc.3101031. [DOI] [PubMed] [Google Scholar]
- 4.Nelson A.L., Groer S., Palacios P., Mitchell D., Sabharwal S., Kirby R.L. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil. 2010;91:1166–1173. doi: 10.1016/j.apmr.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Nelson A.L., Ahmed S., Harrow J., Fitzger S., Sanchez-Anguiano A., Gavin-Dreschnack D. Fall-related fractures in persons with spinal cord impairment: a descriptive analysis. SCI Nurs. 2003;20:30–37. [PubMed] [Google Scholar]
- 6.Bernard P.L., Peruchon E., Micallef J.P., Hertog C., Rabischong P. Balance and stabilization capability of paraplegic wheelchair athletes. J Rehabil Res Dev. 1994;31:287–296. [PubMed] [Google Scholar]
- 7.Gagnon D., Nadeau S., Noreau L., Eng J., Gravel D. Trunk and upper extremity kinematics during sitting pivot transfers performed by individuals with spinal cord injury. Clin Biomech. 2008;23:279–290. doi: 10.1016/j.clinbiomech.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 8.Burns A.S., Ditunno J.F. Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine. 2001;26:S137–S145. doi: 10.1097/00007632-200112151-00023. [DOI] [PubMed] [Google Scholar]
- 9.Tsang W.W.N., Hui-Chan C.W.Y. Effects of Tai Chi on joint proprioception and stability limits in elderly subjects. Med Sci Sports Exerc. 2003;35:1962–1971. doi: 10.1249/01.MSS.0000099110.17311.A2. [DOI] [PubMed] [Google Scholar]
- 10.Lynch S.M., Leahy P., Barker S.P. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–133. doi: 10.1093/ptj/78.2.128. [DOI] [PubMed] [Google Scholar]
- 11.Catz A., Itzkovich M. Spinal Cord Independence Measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res Dev. 2007;44:65–68. doi: 10.1682/jrrd.2005.07.0123. [DOI] [PubMed] [Google Scholar]
- 12.Itzkovich M., Gelernter I., Biering-Sorensen F., Weeks C., Laramee M.T., Craven B. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–1933. doi: 10.1080/09638280601046302. [DOI] [PubMed] [Google Scholar]
- 13.Zhang X., Wang C.H., Liang Q. Comparison of sensitivity of SCIM vs FIM in patient with spinal cord injury. Chin J Rehabil. 2009;24:315–317. [Google Scholar]
- 14.Wang Y.L., Liang Q., Huang D.F. Reliability and validity of the Chinese version of Spinal Cord Independence Measure II. Chin J Rehabil Med. 2007;22:714–717. [Google Scholar]
- 15.Portney L.G., Watkins M.P. Foundations of clinical research. 3rd ed. Pearson Education Inc; Upper Saddle River, New Jersey: 2009. Validity in experimental design. [Google Scholar]
- 16.Shrout P., Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 17.Curtis K.A., Roach K.E., Applegate E.B., Amar T., Benbow C.S., Genecco T.D. Reliability and validity of the wheelchair user's Shoulder Pain Index (SUSPI) Paraplegia. 1995;33:595–601. doi: 10.1038/sc.1995.126. [DOI] [PubMed] [Google Scholar]
- 18.Chen C.L., Yeung K.T., Bih L.I., Wang C.H., Chen M.I., Chien J.C. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84:1276–1281. doi: 10.1016/s0003-9993(03)00200-4. [DOI] [PubMed] [Google Scholar]