Summary
Background/Objective
Standing radiograph with Cobb's method is routinely used to diagnose scoliosis, a medical condition defined as a lateral spine curvature > 10° with concordant vertebral rotation. However, radiation hazard and two-dimensional (2-D) viewing of 3-D anatomy restrict the application of radiograph in scoliosis examination.
Methods
In this study, a freehand 3-D ultrasound system was developed for the radiation-free assessment of scoliosis. Bony landmarks of the spine were manually extracted from a series of ultrasound images with their spatial information recorded to form a 3-D spine model for measuring its curvature. To validate its feasibility, in vivo measurements were conducted in 28 volunteers (age: 28.0 ± 13.0 years, 9 males and 19 females). A significant linear correlation (R2 = 0.86; p < 0.001) was found between the spine curvatures as measured by Cobb's method and the 3-D ultrasound imaging with transverse process and superior articular process as landmarks. The intra- and interobserver tests indicated that the proposed method is repeatable.
Results
The 3-D ultrasound method using bony landmarks tended to underestimate the deformity, and a proper scaling is required. Nevertheless, this study demonstrated the feasibility of the freehand 3-D ultrasound system to assess scoliosis in the standing posture with the proposed methods and 3-D spine profile.
Conclusion
Further studies are required to understand the variations that exist between the ultrasound and radiograph results with a larger number of volunteers, and to demonstrate its potential clinical applications for monitoring of scoliosis patients. Through further clinical trials and development, the reported 3-D ultrasound imaging system can potentially be used for scoliosis mass screening and frequent monitoring of progress and treatment outcome because of its radiation-free and easy accessibility feature.
Keywords: Cobb angle, freehand 3-D ultrasound, scoliosis, spine deformity
Introduction
Scoliosis is a three-dimensional (3-D) spine deformation, characterised by a lateral spine curvature > 10° [1], frequently accompanied with vertebral rotation [2]. Sixty-five percent of cases are estimated to be idiopathic [3]. Treatments for scoliosis including bracing and surgery are essential when the spine curvatures exceed 20° for skeleton immature patients [4]. This is particularly true with the risk of curve progression for teenage patients as significant curve progressions are often observed among children during their rapid growth period. It has been suggested that the prevalence of scoliosis in the population after puberty is higher than that in the population prior to puberty [5], [6], [7]. Therefore, early screening and frequent monitoring of scoliosis can apparently mitigate the curve progression and treatments intervention.
The standing radiograph has been widely exploited to evaluate the spine deformity and identify the type of scoliosis through Cobb's method [8], which is currently considered the gold standard in scoliosis diagnosis. The degree of spine curvature obtained with Cobb's method is named the Cobb angle, which provides vital information for delineating spine curvature and developing treatment plans for curve progression. Patients with scoliosis should regularly undergo X-ray examination of the spine to monitor curve progression and treatment outcome [4], [9]. However, the measurement accuracy of the Cobb angle is influenced by the awareness and practice of the observer, the position of the patient, and the position of the radiography tube [10]. The intra- and interobserver variation of measuring Cobb angle can be 3–5° and 6–9°, respectively [10], [11], [12]. Moreover, frequent X-ray diagnosis gradually builds up harmful effects in the human body, especially for children. Levy et al [13] reported that the considerable amount of X-ray radiation received by growing children with adolescent idiopathic scoliosis raised the risk of cancer by 2.4/1000. Furthermore, vertebral rotation of the spine is one of the essential parameters for assessing scoliosis as a 3-D deformity, predicting the curvature prognosis, and monitoring the progression [14], [15], [16]. However, vertebra rotation information in the traverse plane could not be directly obtained on standing posterior–anterior radiographs [15], resulting in failure to obtain an accurate degree of rotation on the radiograph. Apparently, a radiation-free system that can assess spine deformity on coronal, sagittal, and traverse planes is necessary for the mass screening, diagnosis, and follow-up observation for scoliosis.
Various nonradiation systems based on the skin surface contour of trunk have been developed for assessing scoliosis. Most of them are based on surface topography or optical techniques. Quantec spinal image system (Quantec Image Processing, Warrington, Cheshire, UK) applies Moire topography [17] to obtain surface topography of the patient with fringe pattern projection, in which a Q angle is used as a quantitative parameter for measuring the degree of asymmetry in the coronal plane. However, there is a considerable difference between the Q angle and the Cobb angle, with the maximum difference between Q and Cobb angles of 6° when the Cobb angle is < 21° [18]. Recently, the electromagnetic topographical technique was developed for scoliosis screening. Using this principle, the Ortelius 800 system (Orthoscan Technologies, Inc., Sherborn, MA, USA) records the position of the tip of the spinous process by palpating the patient's back with a position sensor attached on the examiner finger and builds a spine representative model for examining spinal deformities. However, the assessment is slightly subjective (ascribed to manual palpation) and vulnerable to spinous process deviation and traumatic damage. It was reported that the Orthoscan did not accurately measure the scoliosis curve [19]. Similarly, measurements using optical techniques are also inaccurate, which is ascribed to the indirect assessment of the spine deformity from trunk asymmetry indices, although the optical systems used for scoliosis examination provide noninvasive and noncontact measurements [9]. These radiation-free systems are less accurate than radiographs because they assess spine deformity indirectly from the body surface.
Radiation-free imaging modalities including ultrasound and magnetic resonance imaging (MRI) can also be used to measure spine curvature. MRI can provide adequate 3-D information for assessing the spine curvature. However, examination is routinely conducted with the patient placed in a supine position. It was revealed that the Cobb angle obtained in the standing posture is more accurate than the measurements performed in the supine posture [15]. MRI in the upright position has recently become commercially available, but it has yet to gain widespread acceptance. In addition, MRI examination is time consuming and expensive. Therefore, it is not feasible to use MRI in mass screening and longitudinal observation for scoliosis. By contrast, ultrasound imaging is a low-cost, widely available, and radiation-free imaging modality. It has been reported that the vertebra rotation can be derived with ultrasound imaging [20]. The feasibility of using landmarks in cross-sectional B-mode ultrasound images acquired with continuous scanning approach, including laminae and transverse process (TP) as the landmarks, to assess spine curvature has been demonstrated in in vitro experiments [21], [22], [23]. A number of 3-D ultrasound systems have been advanced to overcome the limitations of 2-D viewing of 3-D anatomy [22], [23], [24], [25], [26], [27], [28], [29], [30], [31]. Purnama et al [29] showed that imaging of the human spine using freehand 3-D ultrasound was feasible, but no measurement of spine curvature angle was conducted. Ungi et al [30] reported about using ultrasound images collected along the sagittal direction with position information for spine curvature measurement. The TPs in ultrasound images acquired using the single snap approach were manually marked to devise the spatial information and calculate the TP angle for measuring vertebra orientation. Cheung et al [22], [28] reported a method to form a 3-D spine profile by using spinous processes and TPs detected in 3-D ultrasound images of spine phantoms. Koo et al [23] compared different methods for measuring spinal curvature of spine phantoms using data collected with 3-D ultrasound imaging. The performance and accuracy of the aforementioned methods with freehand 3-D ultrasound have not been evaluated in vivo, and the effect of the patient posture was not taken into account in above studies. It has been reported that the muscle balance and standing stability can be significantly influenced by body postures [32], [33]. Chen et al [34] reported a preliminary study with four scoliosis patients to demonstrate the feasibility of measuring spine curvature based on a coronal view image formed using 3-D ultrasound imaging. Recently, Cheung et al [35] reported a volume projection imaging method for scoliosis assessment based on 3-D ultrasound imaging, and 36 participants with different Cobb angles were tested. Although these methods, which are based on coronal view images, have been demonstrated to be feasible in vivo and can provide rapid image formation, they were not able to provide a 3-D profile of spinal deformity.
In this study, we report the development of a freehand 3-D ultrasound system and a method to measure lateral deformity by establishing a 3-D profile of spine, with the consideration of the influence of body posture. A frame structure was designed and developed to support the patients so they could maintain a stable standing posture. Two methods using different bony features in the 3-D profile of the spine were proposed to measure the angle of spine curvature. The performance of the new system was examined for the individuals with different spine curvature angles.
Materials and methods
Freehand 3-D ultrasound system
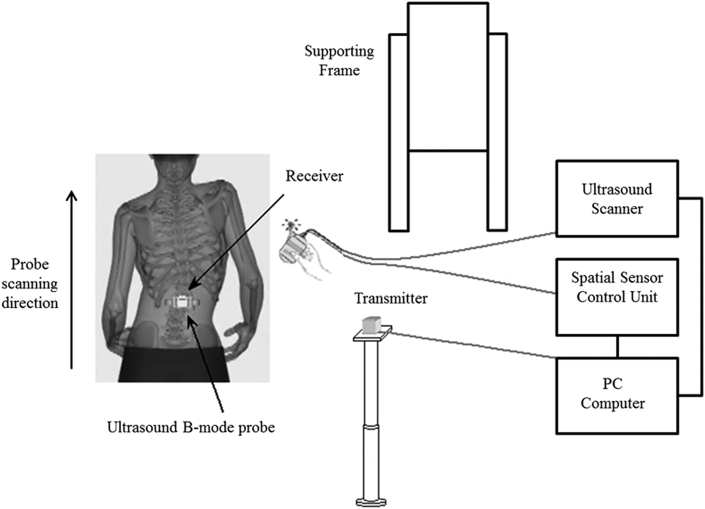
The freehand 3-D ultrasound system for assessing scoliosis (Figure 1) consisted of a custom-designed supporting frame structure, ultrasound scanner EUB-8500 (Hitachi Ltd., Tokyo, Japan), compact electromagnetic spatial sensing device MiniBird Model 130 (MiniBird Ascension Technology Corporation, Burlington, VT, USA), and high-performance desktop computer with video capture card NIIMAQ PCI/PXI-1411 (National Instruments Corporation, Austin, TX, USA). Custom-designed software with user-friendly interface programmed by Visual C++ (Microsoft Corporation, Redmond, WA, USA) was developed for data acquisition, visualisation, and measurement.
Figure 1.
Freehand three-dimensional ultrasound system for scoliosis assessment.
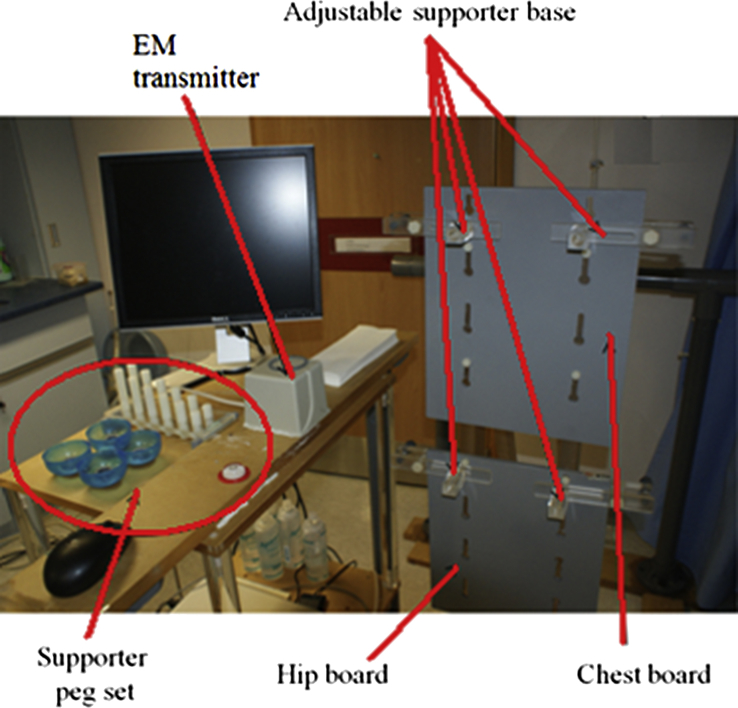
Scoliosis can cause standing instability [36], [37], [38], resulting in postural changes in body attitude [32], [33]. A custom-designed supporting frame structure was therefore developed to improve the standing stability of the patients during scanning. As shown in Figure 2, this frame structure consisted of two vertically movable chest and hip boards and four adjustable and movable posture supporting pegs. Four posture supporting pegs mounted on boards could be adjusted to locate and fix the position of acromion and pelvis, thus allowing the participants to maintain their natural standing posture during scanning. Although the standing stability of the participants was enhanced with the developed frame structure, the whole scanning procedure should be performed as quickly as possible. It was found that a linear ultrasound probe with a width of 92 mm (EUP-L65/6-14MHz, Hitachi, Ltd., Tokyo, Japan) can cover each pair of TP tips of all vertebras of spine in a single ultrasound B-mode image. The entire spine of an individual could then be examined by only one sweep of scan using this probe, thus reducing the total scanning time, with an average time of < 2 minutes.
Figure 2.
Supporting frame structure and electromagnetic (EM) transmitter used in the freehand three-dimensional ultrasound system.
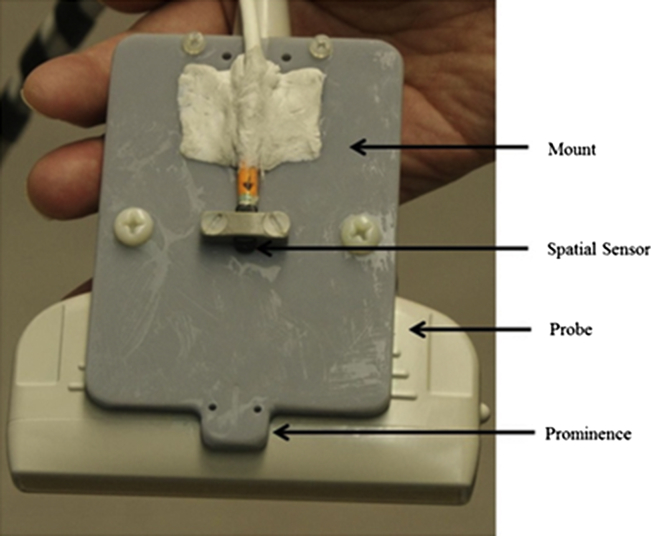
According to the information provided by the manufacturer, the position and orientation resolution of the system within a working range of approximately of 50 cm is 1.4 mm and 0.5°, respectively (medSAFE manual, Ascension Technology Corporation, Burlington, VT, USA). The position sensor was attached onto the ultrasound probe with a fixation device for collecting position and orientation information (Figure 3). The prominence of the mounting plate was used to make probe steering more convenient to follow the shape of the spine during scanning. The spatial offsets between the position sensor and the ultrasound probe were calibrated using a crosswire phantom [39], [40]. A recent study using the same position sensor system demonstrated that it has very high accuracy for both position and angle measurements [41].
Figure 3.
Ultrasound probe attached with position sensor using a fixation mount.
Figure 4 shows the scanning of a patient using this freehand 3-D ultrasound system. Prior to scanning, the participants were requested to remove any metallic items. Then the four posture supporting pegs were adjusted for facilitating the maintenance of a natural standing posture. An adequate amount of ultrasound gel was applied onto the patient's back to assure ultrasound image quality. The scanning was guided by spinous processes or furrows using the prominence of the custom-made mount (Figure 3), enabling the TPs being captured in view of ultrasound images. Images of the spine were steadily scanned along the spine from the fifth lumbar vertebra (L5) up towards the first thoracic vertebra (T1), during which the individual was instructed to stand still and breathe shallowly. During the data acquisition, ultrasound B-mode images with corresponding position and orientation information of the ultrasound probe were recorded and transmitted to a personal computer at a frame rate of 23 frame/s.
Figure 4.
Experimental setup and a typical test for a participant.
Spine curvature measurement
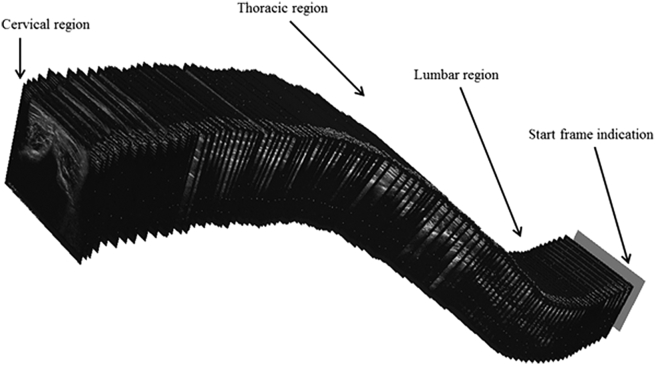
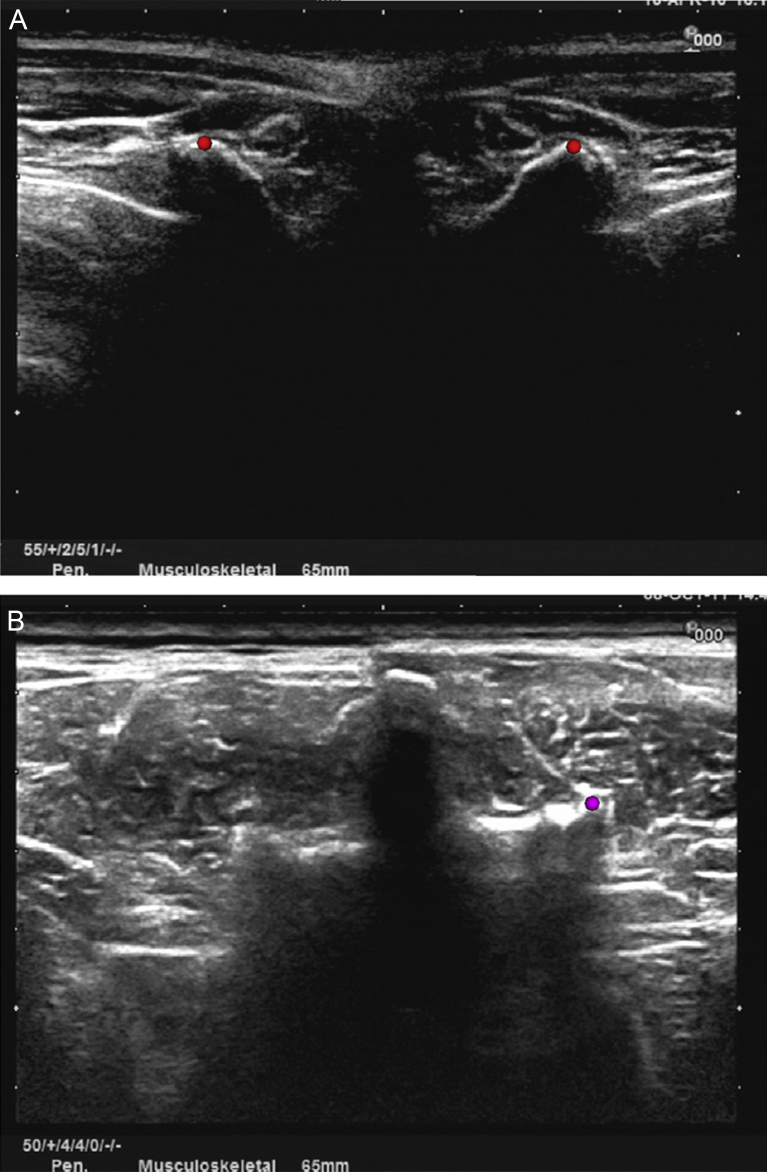
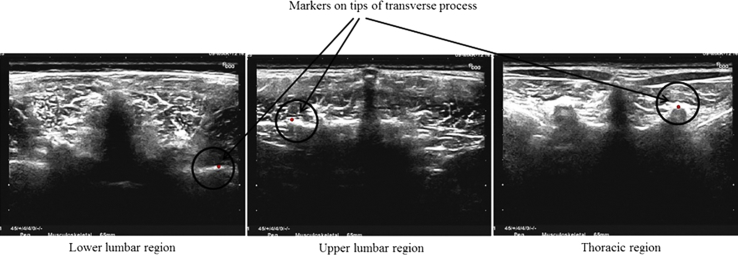
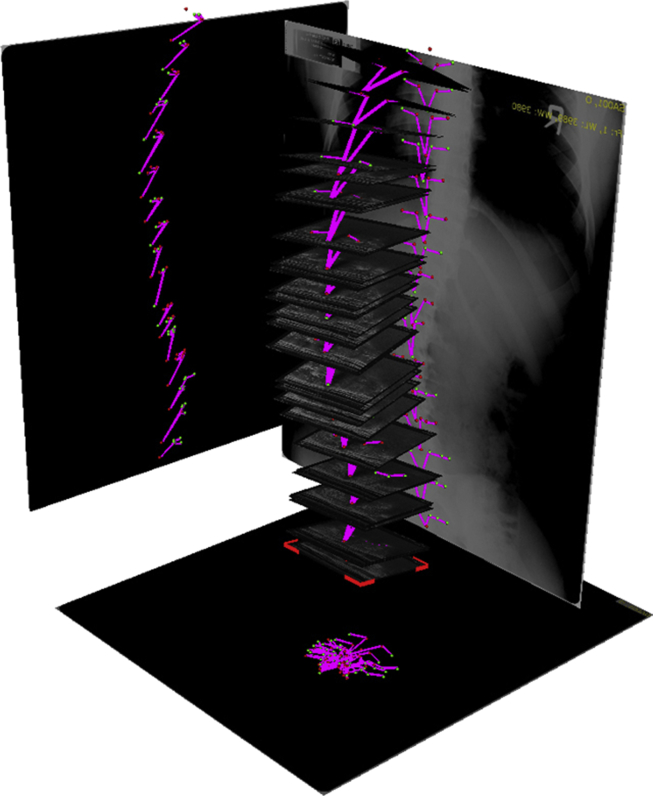
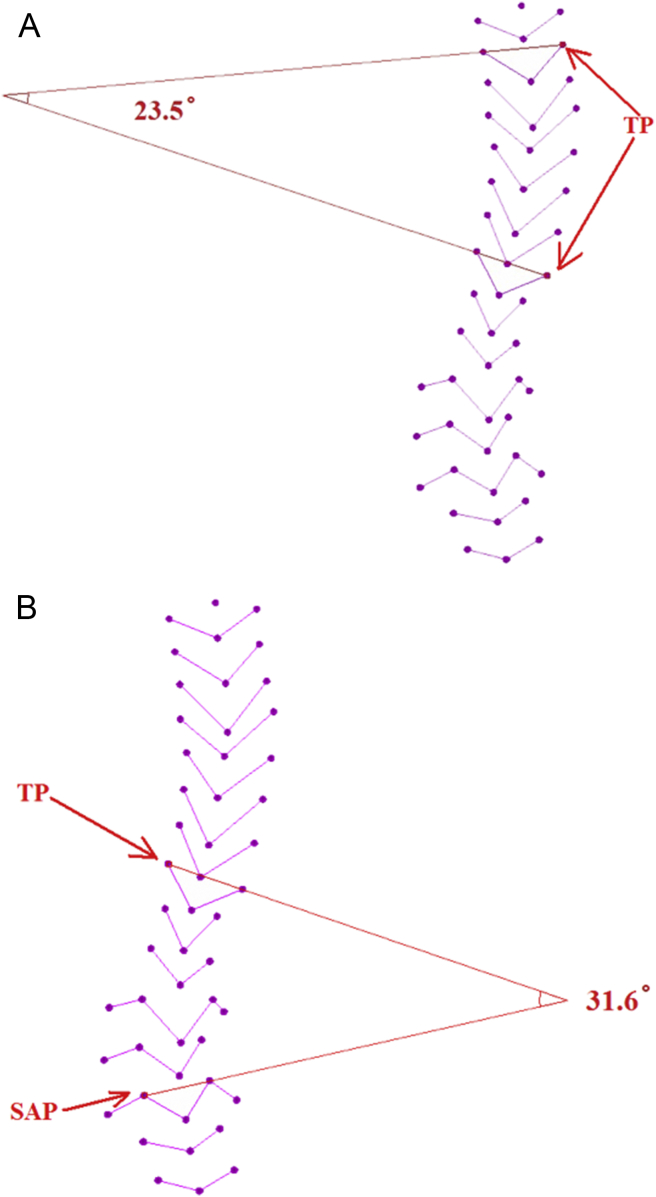
The collected B-mode images were displayed in 3-D space in the custom-designed interface according to their corresponding spatial information (Figure 5). The tips of different bony processes were used as the bony features to form a virtual spine model for the curvature measurement. The image set was then reviewed by an operator to manually identify the images with the sharpest tip of process among their neighbouring images. And the recognised process tip was marked with a spherical marker in the corresponding image using the custom-designed software. As shown in Figure 6A, the peak of the convex shape closest to the skin surface displaying as a bright ridge in the B-mode ultrasound image was defined as the tip of the TP. Figure 7 shows typical images with TP collected from different locations of the spine. It was found that in some patients with thick spinal muscle or subcutaneous fat the tips of the TP were obscured, thus influencing the marking process, particularly when searching for TP in the lumbar region of individuals with a high body mass index (BMI). The tips of the superior articular process (SAP) were then used as alternative bony features to determine the vertebrae in the lumbar region (Figure 6B). After all tips had been marked, a virtual 3-D model of a patient's spine was formed using these tips with their 3-D spatial positions, and it was then projected into a 2-D plane to form an image analog to the posterior–anterior X-ray (Figure 8). Moreover, the X-ray images could be displayed together with the 3-D model of the spine and its projection to facilitate the visualisation effect for the comparison with radiograph (Figure 8). The angle of the spine curvature was measured in the projection plane according to the definition of the Cobb angle, i.e., the angle between the most tilted pairs of vertebrae. The pair of vertebrae was marked in the projected virtual 3-D model of the spine for the corresponding measurement. The orientation of vertebrae was determined by the lines drawn along the markers of TP or SAP of the vertebrae in the projection plane. In this study, the results were obtained for both using TP only (TP–TP) as well as using the TP and SAP combination (TP–SAP, where TP–TP was adopted if a measurement was conducted for vertebra without SAP). Figures 9A and 9B show the typical measurements of the spine curvature using the 3-D images with TP–TP and TP–SAP references in the projection plane, respectively.
Figure 5.
Stack of B-mode images displayed in three-dimensional space according to the spatial information of each image.
Figure 6.
Marks placed at the tips of the processes in B-mode image. (A) Two marks were placed at the transverse processes in a typical ultrasound image. (B) A mark was placed at the superior articular process in a typical ultrasound image where the transverse processes could not be identified.
Figure 7.
Markers at the tip of transverse processes at various regions of the spine.
Figure 8.
A virtual spine model formed using the detected spine processes in B-mode images with projections in the three orthogonal planes.
Figure 9.
Measurement of spine curvature using 3-D ultrasound imaging. (A) 3-D ultrasound measurement using the TP–TP method. (B) 3-D ultrasound measurement using the TP–SAP method. 3-D = three-dimensional; TP = transverse process; SAP = superior articular process.
Experiments
A total of 28 participants (age 28.0 ± 13.0 years, 9 males and 19 females) were recruited in this study to investigate the relationship between the X-ray Cobb angle and the spine curvature measured using the 3-D ultrasound method. This study was approved by the institutional ethics committee of the Hong Kong Polytechnic University, and all participants gave written informed consent prior to participation in the study. The exclusion criteria for the study included any neuromuscular diseases, ferromagnetic implantation, pacemaker implantation, or a traumatic injury. The radiographs of 28 participants were also supplied by their clinicians for comparison.
All participants were scanned by the same operator. The spine curvature was measured twice using the proposed method for each scan by two observers. The two measurements of each observer were used to evaluate the intraobserver repeatability, and the mean value of each observer was applied in the interobserver repeatability test. The results obtained by the 3-D ultrasound method were compared with the Cobb angle measured on the radiograph. Using the software SDV free edition version 1.3 (Santesoft Ltd., Athens, Greece), the Cobb angle was measured from the radiographs by a rater who was experienced in handling X-ray spine images and was blind to the results of the 3-D ultrasound measurements.
Statistical analysis
Linear regressions analysis was used to study the relationship between the spine curvatures measured using 3-D ultrasound method and Cobb's method. Bland and Altman's [42] method of differences was used to evaluate the agreement of the assessment between the two methods. The level of significance was set at p < 0.05. An intraclass correlation coefficient (ICC) was applied to test the intraobserver and interobserver repeatability with one-way random-effects model.
Results
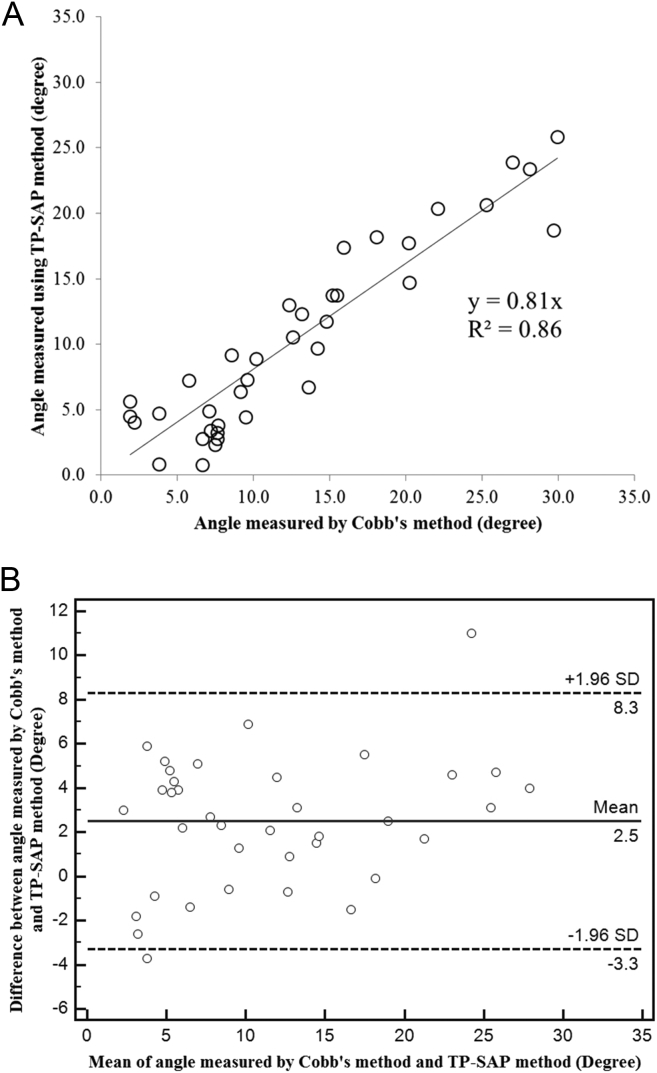
A total of 37 curvatures were measured on the radiographs of the 28 participants, ranging from 1.9° to 29.9°, whereas the participants' spine curvatures obtained with 3-D ultrasound imaging using the TP–SAP method ranged from 0.8° to 25.9°. The results demonstrated a significant linear correlation between the spine curvatures measured using Cobb's method and the 3-D ultrasound method with the TP–SAP method (R2 = 0.86; p < 0.001; Figure 10A). The Bland–Altman plot (Figure 10B) showed a low mean difference (d = 2.5°), and the differences were symmetrically distributed around the mean difference. For the reproducibility of measurement, both intra- and interobserver tests showed very good repeatability, with ICC values being 0.93 (p < 0.001) and 0.89 (p < 0.001), respectively.
Figure 10.
Comparison between Cobb's method and 3-D ultrasound imaging with the TP–SAP approach for the subject test. (A) Correlation between the spine curvature angles measured using Cobb's method and 3-D ultrasound imaging. (B) Bland–Altman plot between the results obtained by the two methods. 3-D = three-dimensional; TP = transverse process; SAP = superior articular process.
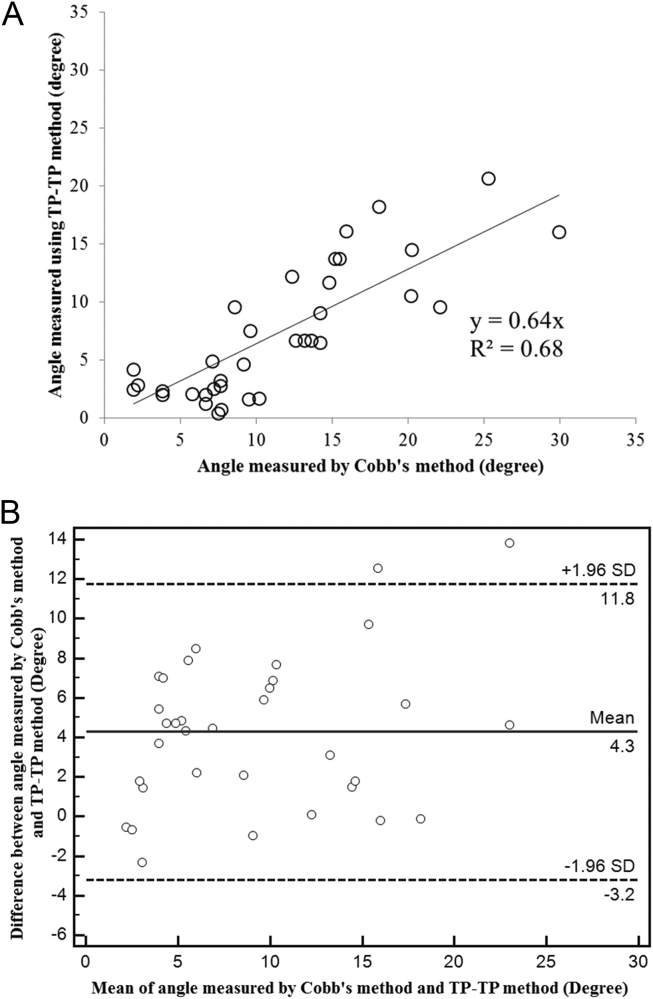
One patient's TP in the lower lumbar region could not be found; thus, only 27 participants were included in the analysis of using the TP–TP method. The spine curvatures obtained with the TP–TP method ranged from 0.48° to 20.7°, and the corresponding Cobb angle ranged from 1.9° to 29.9° for the 34 curvatures identified. A good linear correlation was also demonstrated between the results obtained with Cobb's method and the 3-D ultrasound method (R2 = 0.68; p < 0.001; Figure 11A), although it is poorer in comparison with that using the TP–SAP method. The Bland–Altman plot (Figure 11B) also showed a relatively poorer agreement between the two results in comparison with the TP–SAP method. For the reproducibility of in vivo measurement, both intra- and interobserver tests showed relatively poorer repeatability in comparison with that using the TP–SAP method, with the ICC value being 0.57 (p = 0.0045) and 0.75 (p < 0.001), respectively.
Figure 11.
Comparison between the results of Cobb's method and 3-D ultrasound imaging with the TP–TP approach. (A) Correlation between the spine curvature angles measured by Cobb's method and 3-D ultrasound imaging. (B) Bland–Altman plot between the results obtained by the two methods. 3-D = three-dimensional; TP = transverse process; SAP = superior articular process.
Discussion
In this study, a freehand 3-D ultrasound system was successfully developed for the radiation-free assessment of scoliosis together with two curvature measurement methods on the spine 3-D profile, based on the earlier feasibility study on spine phantoms [22]. In addition to using TP as landmarks for measurement [29], it was also proposed to use TP–SAP landmarks for the measurement of spine curvature. It was demonstrated that the TP–SAP method performed much better in comparison with the method using TP only (the TP–TP method). There was a better correlation between the Cobb angle and the result obtained using 3-D ultrasound imaging with the TP–SAP method (R2 = 0.86, p < 0.001) in comparison with that obtained using the TP–TP method (R2 = 0.68, p < 0.001). The measurement using the TP–SAP method also showed higher intra- and interobserver repeatability (ICC = 0.93 and ICC = 0.89, respectively) in comparison with that using the TP–TP method (ICC = 0.57 and ICC = 0.75, respectively). However, it was noted that the results of both TP–TP and TP–SAP methods appeared to underestimate the spine curvature in comparison with X-ray Cobb's method. Hence, this study demonstrated that it is feasible to use the 3-D profile of the spine obtained using the radiation-free 3-D ultrasound imaging to assess spine deformity, but more efforts are required to understand the potential reasons for the underestimation of the spine curvature.
According to Denis [43] classification, ultrasound images obtained in the transverse plane covered the majority of the posterior column of the spine and part of the middle column of the spine. It was found that vertebra processes, consisting of four articular processes, two TPs, and one spinous process, were more easily identified than other spinal landmarks because of its sharp delineation in the ultrasound images. Herzenberg et al [14] measured spine curvature by using spinous process tip as the landmark and reported that the angle using spinous process underestimated the degree of spine curvature in comparison with Cobb's method. This could be explained by the vertebral axial rotation with vertebral lateral deviation, one of the abnormalities observed in idiopathic scoliosis. The spinous processes increasingly deviated to the concave side when the vertebral bodies rotate [44]. It was also suggested that the magnitude of vertebral axial rotation correlated with the lateral deviation of vertebrae from the spinal axis [45]. In fact, the spinous process deviations caused by vertebral rotation might result in the inaccuracy of interpretation on the vertebral body alignment on the radiographs of the spine [46], [47]. Unlike the deviations of spinous process, it was reported that deviations of TP were mainly induced by injury or elongation [43], [48], [49], [50]. In this study, TPs were used as references for the 3-D ultrasound method for the measurement of spine curvature. It was found in this study that the measurement using TPs as reference also underestimated the Cobb angle, for both the TP–SAP and TP–TP methods. The feasibility of using vertebra's TPs as the landmarks has been demonstrated in a number of earlier studies [21], [22], [30]. In Ungi et al's [30] method, every single measurement on an individual vertebra involved two B-mode images captured at different moments so as to capture the important bony features from two sides of the vertebra. This method could work well with spine phantoms. However, the vertebra's physical position between the B-mode images could probably be changed by various factors including breathing, balance shift, posture change, and different pressures exerted from the probe during in vivo examinations. By contrast, the continuous capturing technique used in the current study enables bony features to be captured from both sides of the vertebra simultaneously, overcoming the hurdles in the study reported by Ungi et al [30]. In addition, marking bony features from different images and connecting the bony features have to involve the vertebra identification process. In human volunteers, particularly those with severe scoliosis, the bony features are unevenly distributed. The packed bony features in B-mode ultrasound images at certain locations of the spine might lead to misconnection of the bony feature of different vertebras, whereas the continuous capturing technique could follow the turning of spine, enabling all the bony features from both sides of the same vertebra to be captured more conveniently.
It was found that locating the tip of TP in the lumbar region for individuals with high BMI is still a challenging task, which is ascribed to the poor image quality of ultrasound induced by the large attenuation of signals passing through the thick muscle and fat layers. In this study, one participant's TP of vertebrae in the lumbar region could not be identified, resulting in the removal of this participant from the analysis of using the TP–TP method. Therefore, for the lumbar region, the use of SAP as landmarks was also studied as they are located closer to the vertebra body than TP and also easier to be detected in ultrasound images particularly for participants with high BMI. Contrary to TPs, the deviation of SAPs was not widely reported. Furthermore, the distance between a pair of SAPs is shorter than that between a pair of TPs, making it easier to be captured by B-mode images in a single sweep. With the smaller distance, the potential effect of vertebra rotation is also lessened. These factors indicate that using SAPs as bony landmarks in the lumber region may lead to a more reliable measurement of spine deformity using ultrasound imaging. The SAP of all participants recruited was successfully located in this study. The correlation and repeatability of the method using TP–SAP were found to be substantially better than those of the method using TP alone. The results clearly indicated that using SAP as landmarks was superior to using TP in the lumbar region. Further studies with a larger number of participants and a wider range of spine curvature should be conducted to confirm this observation.
The virtual 3-D model of the spine was established with the selected bony landmarks obtained from ultrasound images, which could provide the deformity information of the spine in the coronal, sagittal, and transverse planes. Scoliosis is increasingly considered as a 3-D complex spine deformity problem. Yazici et al [15] suggested that adolescent idiopathic scoliosis be evaluated on the coronal, sagittal, and transverse planes in the upright position. Although computed tomography and MRI can provide high-resolution 3-D images, the patients are usually examined in the supine position, which is inappropriate for spine deformity assessment. By contrast, the freehand 3-D ultrasound system can assess spine deformity in the upright position. It has been previously reported that there was a correlation between the Cobb angle and the vertebra rotation according to a relatively simple ultrasound measurement [20]. The virtual 3-D model of the spine established in this study also revealed that vertebra rotation and spinal deformity can be measured in three orthogonal planes. Vertebra rotation was excluded in this study, because there is no available computed tomography or MRI data for validation. Future studies need to be conducted along this direction to demonstrate the potential of 3-D ultrasound imaging and 3-D spine model for the assessment of kyphosis and vertebra rotation.
In spite of the encouraging results demonstrated in the study, several limitations of the current system were identified. It was found that the identification of bony landmarks could be influenced by the quality of ultrasound images. It was reported that image quality of ultrasound would be degraded under thick subcutaneous fat tissue [51]. The poor ultrasound image quality at different anatomical locations was reported to be associated with obesity and adiposity [52], [53], [54]. Therefore, it remains a challenging task to locate the tip of process, particularly for participants with high BMI values. Furthermore, the manual marking procedure for the tips of process was time-consuming and subjective. Image enhancement, and automatic or semiautomatic tip identification methods should be developed to enhance the manual efforts in placing markers in the future. In addition, ultrasound probes with other frequencies may also be studied to find the optimal level. In this study, only 28 participants with different spinal curvatures were tested; a much larger patient group is needed to establish a reliable equation to transfer the curvature measured using the freehand 3-D ultrasound system to the Cobb angle, and to fully demonstrate the potential of this new imaging modality for the assessment of scoliosis.
Conclusion
A 3-D ultrasound imaging system was successfully developed for the radiation-free assessment of scoliosis, wherein examination was conducted with the patient placed in a standing posture supported by a custom-designed frame structure. The results of the in vivo test demonstrated that it is feasible to use the new system to quantitatively assess scoliosis. The repeatability of the test was affected by the manual identification of process tips in ultrasound images, which was time-consuming and influenced by the B-mode image quality. The system should be improved by enhancing the image quality, developing methods for automatic or semiautomatic approaches for tip of process identification. Nevertheless, it was also revealed that the virtual 3-D model of the spine formed by the bony landmarks extracted from ultrasound images could provide information on spine deformity on different planes as well as vertebrae rotation information. Therefore, it is worthwhile to continue these efforts to improve the system to fully demonstrate its clinical value. If it is successful, significant numbers of radiograph examination can be avoided by using 3-D ultrasound imaging for monitoring curve progression and treatment outcomes of scoliosis.
Conflicts of interest
Some of authors have been inventors of a number of patents related to the technique and may benefit from their implementation or licensing.
Funding/support
This study was supported by the Research Grant Council of Hong Kong (PolyU5332/07E) and the Hong Kong Innovation and Technology Fund (UIM213).
Acknowledgements
The authors thank Mr Meng Sing Wong and Wong Meng Sing Clinics for their generous support in the recruitment of participants, and Ms Sally Ding for editing the manuscript.
References
- 1.Bunnell W.P. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986;11:773–776. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Stokes I.A.F. 3-Dimensional terminology of spinal deformity: a report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine. 1994;19:236–248. [PubMed] [Google Scholar]
- 3.Agabegi S.S., Agabegi E. 2nd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2008. Step-up to medicine. [Google Scholar]
- 4.Kim H., Kim H.S., Moon E.S., Yoon C.S., Chung T.S., Song H.T. Scoliosis imaging: what radiologists should know. Radiographics. 2010;30:1823–1842. doi: 10.1148/rg.307105061. [DOI] [PubMed] [Google Scholar]
- 5.Daruwalla J., Balasubramaniam P., Chay S., Rajan U., Lee H. Idiopathic scoliosis. Prevalence and ethnic distribution in Singapore schoolchildren. J Bone Joint Surg Br Vol. 1985;67-B:182–184. doi: 10.1302/0301-620X.67B2.3980521. [DOI] [PubMed] [Google Scholar]
- 6.Neinstein L.S., Gordon C., Katzman D., Rosen D., Woods E. 5th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2007. Adolescent health care: a practical guide. [Google Scholar]
- 7.Konieczny M., Senyurt H., Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Childrens Orthop. 2013;7:3–9. doi: 10.1007/s11832-012-0457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobb J. Outline for the study of scoliosis. Am Acad Orthop Surg Instruct Course Lect. 1948;5:15. [Google Scholar]
- 9.Thomsen M., Abel R. Imaging in scoliosis from the orthopaedic surgeon's point of view. Eur J Radiol. 2006;58:41–47. doi: 10.1016/j.ejrad.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Morrissy R.T., Goldsmith G.S., Hall E.C., Kehl D., Cowie G.H. Measurement of the Cobb angle on radiographs of patients who have scoliosis: evaluation of intrinsic error. J Bone Joint Surg Am Vol. 1990;72A:320–327. [PubMed] [Google Scholar]
- 11.Carman D.L., Browne R.H., Birch J.G. Measurement of scoliosis and kyphosis radiographs — intraobserver and interobserver variation. J Bone Joint Surg Am Vol. 1990;72A:328–333. [PubMed] [Google Scholar]
- 12.Pruijs J., Hageman M., Keessen W., van der Meer R., van Wieringen J. Variation in Cobb angle measurements in scoliosis. Skeletal Radiol. 1994;23:4. doi: 10.1007/BF00223081. [DOI] [PubMed] [Google Scholar]
- 13.Levy A.R., Goldberg M.S., Mayo N.E., Hanley J.A., Poitras B. Reducing the lifetime risk of cancer from spinal radiographs among people with adolescent idiopathic scoliosis. Spine. 1996;21:1540–1547. doi: 10.1097/00007632-199607010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Herzenberg J.E., Waanders N.A., Closkey R.F., Schultz A.B., Hensinger R.N. Cobb angle versus spinous process angle in adolescent idiopathic scoliosis: the relationship of the anterior and posterior deformities. Spine. 1990;15:874–879. doi: 10.1097/00007632-199009000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Yazici M., Acaroglu E.R., Alanay A., Deviren V., Cila A., Surat A. Measurement of vertebral rotation in standing versus supine position in adolescent idiopathic scoliosis. J Pediatr Orthop. 2001;21:252–256. [PubMed] [Google Scholar]
- 16.Pinheiro A.P., Tanure M.C., Oliveira A.S. Validity and reliability of a computer method to estimate vertebral axial rotation from digital radiographs. Eur Spine J. 2010;19:415–420. doi: 10.1007/s00586-009-1186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Idesawa M., Yatagai T., Soma T. Scanning moire method and automatic measurement of 3-D shapes. Appl Opt. 1977;16:2152–2162. doi: 10.1364/AO.16.002152. [DOI] [PubMed] [Google Scholar]
- 18.Thometz J.G., Lamdan R., Liu X.C., Lyon R. Relationship between Quantec measurement and Cobb angle in patients with idiopathic scoliosis. J Pediatr Orthop. 2000;20:512–516. [PubMed] [Google Scholar]
- 19.Knott P., Mardjetko S., Nance D., Dunn M. Electromagnetic topographical technique of curve evaluation for adolescent idiopathic scoliosis. Spine. 2006;31:E911–E915. doi: 10.1097/01.brs.0000245924.82359.ab. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki S., Yamamuro T., Shikata J., Shimizu K., Iida H. Ultrasound measurement of vertebral rotation in idiopathic scoliosis. J Bone Joint Surg Br Vol. 1989;71:252–255. doi: 10.1302/0301-620X.71B2.2647754. [DOI] [PubMed] [Google Scholar]
- 21.Chen W., Lou E.H.M., Le L.H. 33rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBS) 2011. Using ultrasound imaging to identify landmarks in vertebra models to assess spinal deformity; pp. 8495–8498. Boston, MA. [DOI] [PubMed] [Google Scholar]
- 22.Cheung C.W.J., Law S.Y., Zheng Y.P. Presented at the Engineering in Medicine and Biology Society (EMBC), 35th Annual International Conference of the IEEE, Osaka, Japan. 2013. Development of 3-D ultrasound system for assessment of adolescent idiopathic scoliosis (AIS) and system validation. [DOI] [PubMed] [Google Scholar]
- 23.Koo T.K., Guo J.Y., Ippolito C., Bedle J.C. Assessment of scoliotic deformity using spinous processes: comparison of different analysis methods of an ultrasonographic system. J Manipulative Physiol Ther. 2014;37:667–677. doi: 10.1016/j.jmpt.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Nelson T.R., Pretorius D.H. Three-dimensional ultrasound imaging. Ultrasound Med Biol. 1998;24:1243–1270. doi: 10.1016/s0301-5629(98)00043-x. [DOI] [PubMed] [Google Scholar]
- 25.Fenster A., Downey D.B., Cardinal H.N. Three-dimensional ultrasound imaging. Phys Med Biol. 2001;46:R67–R99. doi: 10.1088/0031-9155/46/5/201. [DOI] [PubMed] [Google Scholar]
- 26.Gee A., Prager R., Treece G., Berman L. Engineering a freehand 3D ultrasound system. Pattern Recogn Lett. 2003;24:757–777. [Google Scholar]
- 27.Huang Q.H., Zheng Y.P., Lu M.H., Chi Z.R. Development of a portable 3D ultrasound imaging system for musculoskeletal tissues. Ultrasonics. 2005;43:153–163. doi: 10.1016/j.ultras.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Cheung C.W.J., Zheng Y.P. Development of 3-D ultrasound system for assessment of adolescent idiopathic scoliosis (AIS) In: Lim C.T., Goh J.C.H., editors. 6th World Congress of Biomechanics. Springer; New York: 2010. pp. 584–587. [Google Scholar]
- 29.Purnama K.E., Wilkinson M.H.F., Veldhuizen A.G., van Ooijen P.M.A., Lubbers J., Burgerhof J.G.M. A framework for human spine imaging using a freehand 3D ultrasound system. Technol Health Care. 2010;18:1–17. doi: 10.3233/THC-2010-0565. [DOI] [PubMed] [Google Scholar]
- 30.Ungi T., King F., Kempston M., Keri Z., Lasso A., Mousavi P. Spinal curvature measurement by tracked ultrasound snapshots. Ultrasound Med Biol. 2014;40:447–454. doi: 10.1016/j.ultrasmedbio.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 31.Jiang W.W., Li C., Li A.H., Zheng Y.P. A novel breast ultrasound system for providing coronal images: system development and feasibility study. Ultrasonics. 2015;56:427–434. doi: 10.1016/j.ultras.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 32.Nault M.L., Allard P., Hinse S., Le Blanc R., Caron O., Labelle H. Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine. 2002;27:1911–1917. doi: 10.1097/00007632-200209010-00018. [DOI] [PubMed] [Google Scholar]
- 33.Fortin C., Feldman D.E., Cheriet F., Labelle H. Differences in standing and sitting postures of youth with idiopathic scoliosis from quantitative analysis of digital photographs. Phys Occup Ther Pediatr. 2013;33:313–326. doi: 10.3109/01942638.2012.747582. [DOI] [PubMed] [Google Scholar]
- 34.Chen W., Lou E.H.M., Zhang P.Q., Le L.H., Doug H. Reliability of assessing the coronal curvature of children with scoliosis by using ultrasound images. J Childrens Orthop. 2013;7:521–529. doi: 10.1007/s11832-013-0539-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheung C.W.J., Zhou G.Q., Law S.Y., Mak T.M., Lai K.L., Zheng Y.P. Ultrasound volume projection imaging for assessment of scoliosis. IEEE Trans Med Imaging. 2015;99 doi: 10.1109/TMI.2015.2390233. [published online on Jan 12 2015] [DOI] [PubMed] [Google Scholar]
- 36.Sahlstrand T., Ortengren R., Nachemson A. Postural equilibrium in adolescent idiopathic scoliosis. Acta Orthop Scand. 1978;49:354–365. doi: 10.3109/17453677809050088. [DOI] [PubMed] [Google Scholar]
- 37.Herman R., Mixon J., Fisher A., Maulucci R., Stuyck J. Idiopathic scoliosis and the central nervous system: a motor control problem. Spine. 1985;10:1–14. doi: 10.1097/00007632-198501000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Byl N.N., Gray J.M. Complex balance reactions in different sensory conditions: adolescents with and without idiopathic scoliosis. J Orthop Res. 1993;11:215–227. doi: 10.1002/jor.1100110209. [DOI] [PubMed] [Google Scholar]
- 39.Prager R.W., Rohling R.N., Gee A.H., Berman L. Rapid calibration for 3-D freehand ultrasound. Ultrasound Med Biol. 1998;24:855–869. doi: 10.1016/s0301-5629(98)00044-1. [DOI] [PubMed] [Google Scholar]
- 40.Detmer P.R., Bashein G., Hodges T., Beach K.W., Filer E.P., Burns D.H. 3D ultrasonic image feature localization based on magnetic scanhead tracking: in vitro calibration and validation. Ultrasound Med Biol. 1994;20:923–936. doi: 10.1016/0301-5629(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 41.Jiang W.W., Li A.H., Zheng Y.P. A semi-automated 3-D annotation method for breast ultrasound imaging: system development and feasibility study on phantoms. Ultrasound Med Biol. 2014;40:434–446. doi: 10.1016/j.ultrasmedbio.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 42.Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 43.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Middleditch A., Oliver J. 2nd ed. Butterworth-Heinemann; Oxford: 2002. Functional anatomy of the spine. [Google Scholar]
- 45.Stokes I.A.F., Gardnermorse M. Analysis of the interaction between vertebral lateral deviation and axial rotation in rotation in scoliosis. J Biomech. 1991;24:753–759. doi: 10.1016/0021-9290(91)90339-o. [DOI] [PubMed] [Google Scholar]
- 46.Mellado J.M., Larrosa R., Martin J., Yanguas N., Solanas S., Cozcolluela M.R. MDCT of variations and anomalies of the neural arch and its processes: part 2. Articular processes, transverse processes, and high cervical spine. Am Jo Roentgenol. 2011;197:W114–W121. doi: 10.2214/AJR.10.5811. [DOI] [PubMed] [Google Scholar]
- 47.Mellado J.M., Larrosa R., Martin J., Yanguas N., Solanas S., Cozcolluela M.R. MDCT of variations and anomalies of the neural arch and its processes: part 1. Pedicles, pars interarticularis, laminae, and spinous process. Am J Roentgenol. 2011;197:W104–W113. doi: 10.2214/AJR.10.5803. [DOI] [PubMed] [Google Scholar]
- 48.Brewin A., Hill M., Ellis H. The prevalence of cervical ribs in a London population. Clin Anat. 2009;22:331–336. doi: 10.1002/ca.20774. [DOI] [PubMed] [Google Scholar]
- 49.Eom K.S., Kim T.Y., Moon S.K. Extreme elongation of the transverse processes of the fifth lumbar vertebra: an unusual variant. Turk Neurosurg. 2011;21:648–650. [PubMed] [Google Scholar]
- 50.Thawait G.K., Chhabra A., Carrino J.A. Spine segmentation and enumeration and normal variants. Radiol Clin North Am. 2012;50:587–592. doi: 10.1016/j.rcl.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 51.Carpenter D.A., Kossoff G., Griffiths K.A. Correction of distortion in US images caused by subcutaneous tissues: results in tissue phantoms and human subjects. Radiology. 1995;195:563–567. doi: 10.1148/radiology.195.2.7724784. [DOI] [PubMed] [Google Scholar]
- 52.Shmulewitz A., Teefey S.A., Robinson B.S. Factors affecting image quality and diagnostic efficacy in abdominal sonography: a prospective study of 140 patients. J Clin Ultrasound. 1993;21:623–630. doi: 10.1002/jcu.1870210909. [DOI] [PubMed] [Google Scholar]
- 53.Almeida A.D., Cotrim H.P., Barbosa D.B.V., de Athayde L.G.M., Santos A.S., Bitencourt A.G.V. Fatty liver disease in severe obese patients: diagnostic value of abdominal ultrasound. World J Gastroenterol. 2008;14:1415–1418. doi: 10.3748/wjg.14.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Magnussen C.G., Thomson R., Juonala M., Viikari J.S.A., Dwyer T., Raitakari O.T. Use of B-mode ultrasound to examine preclinical markers of atherosclerosis image quality may bias associations between adiposity and measures of vascular structure and function. 2011;30:363–369. doi: 10.7863/jum.2011.30.3.363. [DOI] [PubMed] [Google Scholar]