Abstract
Isolated hemimegalencephaly (iHME) is a rare form of congenital malformation of cortical development characterized by enlargement of all or part of one cerebral hemisphere. It typically presents with intractable seizures, developmental delay, contralateral hemiparesis, and hemianopia. We report a case of an 18-month-old girl who presented first with focal seizures at tenth day of life, with no other physical or behavioral abnormality. Initial EEG showed excessive sharp EEG transients more over the right hemisphere; repeated EEG showed spikes, polyspikes, sharps, and slow wave discharges predominately over the right hemisphere. MRI of the brain showed asymmetric enlargement of the right cerebral hemisphere, suggestive of hemimegalencephaly. Initial treatment with antiepileptic drugs (AEDs) was successful in controlling her seizures, but later on the seizures became intractable even on polytherapy of AEDs; finally, functional hemispherectomy was performed and she became seizure free. Identification of this and similar cases of iHME can help us to better understand this disorder and eventually to provide better treatment options for it.
Keywords: Hemimegalencephaly, hemiparesis, hemispherectomy, intractable epilepsy
INTRODUCTION
Hemimegalencephaly (HME) is a rare congenital malformation of cortical development characterized by enlargement of all or part of one cerebral hemisphere.[1] It may occur as an isolated disease or as a part of different syndromes such as Proteus syndrome, neurofibromatosis, linear nevus sebaceous syndrome, tuberous sclerosis complex, or Klippel–Weber–Trenaunay syndrome.[2] The typical characteristics of isolated hemimegalencephaly (iHME) include ipsilateral severe cortical dysplasia or dysgenesis, white matter hypertrophy, and a dilated and dysmorphic lateral ventricle.[3] This asymmetric and enlarged brain tissue is associated with intractable seizures, developmental delay, contralateral hemiparesis, and hemianopia.[4] As there is no cure for iHME, the principal aim of the treatment of this disease is to control seizures, which is done by using a variety of antiepileptic drugs (AEDs).[4] However, in majority of patients, the seizures remain intractable and hemispherectomy is the treatment of choice.[4] Even though this surgical procedure has been shown to be successful in reducing the frequency of seizures. The purpose of hemispherectomy is to functionally isolate and eradicate the epileptogenic zone, which is widely diffused to an entire hemisphere, but the risks of morbidity, which include hydrocephalus, intracranial hematomas, and infections, remain high.[3]
Cases of iHME present as sporadic cases and do not show familial inheritance or sex preference.[2] This fact makes it very difficult to identify a particular genetic etiology for iHME. Nevertheless, different studies have shown an association between iHME and mutations in AKT3, PIK3CA, and MTOR genes.[2] It has also been reported that Pitx2, lefty-1, lefty-2, and Zic3 genes play a role in asymmetric growth pattern of brain hemisphere.[5] Therefore, it is important that more cases of iHME are identified and reported so that further research can be conducted to understand this disorder and develop better treatment strategy. Only a few cases of iHME have been reported from Pakistan, but this is first case report in which functional hemispherectomy was performed.
CASE REPORT
An 18-month-old girl presented to the Aga Khan University Hospital, Karachi, Pakistan, with a history of focal seizures at tenth day of life. Her seizures consisted of jerky movements localized to the left side of the body with uprolling of eyes and excessive crying. No other symptoms were noted. The child was born via spontaneous vaginal delivery at term. On examination at the time of birth, the child had a visible right-sided cephalhematoma. The head circumference was 34 cm and birth weight was 2.8kg. She was the only child of nonconsanguineous parents. There was no history of miscarriage or syndromic baby in either parent's family.
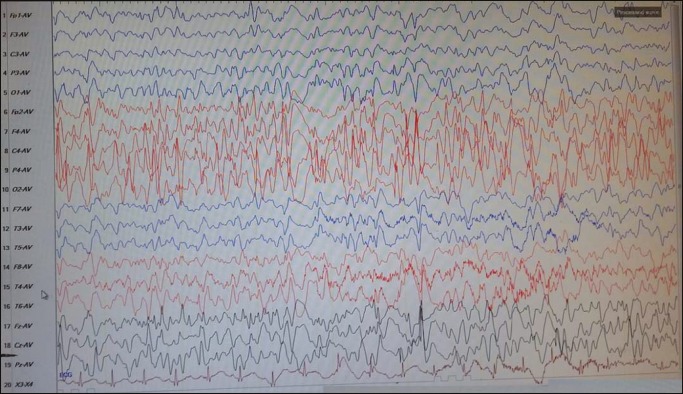
Initial workup included EEG, which showed excessive sharp EEG transients more over the right hemisphere, and MRI of the brain, which showed asymmetric enlargement of the right cerebral hemisphere and diffuse thickening of cortical gray matter with increased myelination over right hemisphere, suggestive of right-sided HME [Figure 1]. Initially, her seizures were well controlled with phenobarbital.
Figure 1.
MRI showing transverse view of the brain. Hemimegalencephaly of the right side of the brain can be easily identified. A cephalhematoma can also be seen on the right
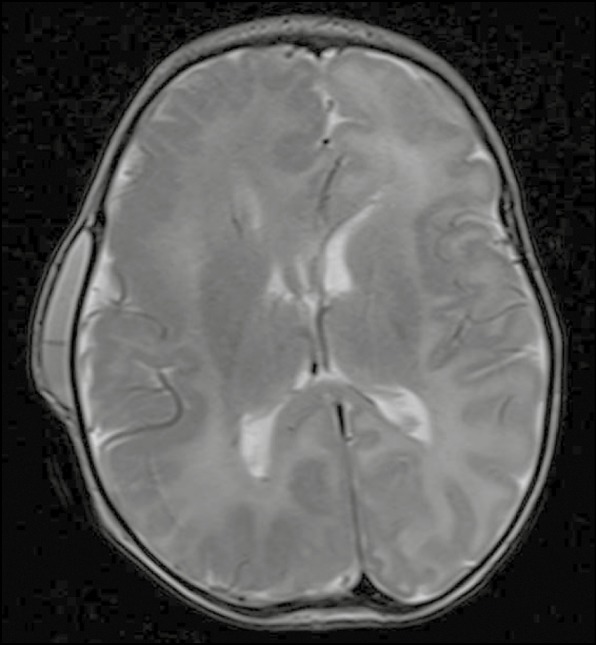
At the age of five and a half months, the child presented to the emergency room with multiple left-sided focal seizures. This time a paucity of movement over left-sided body was also noted. The head circumference was 37.5 cm, weight 5.5 kg, and height 58 cm. She had partial neck holding, could reach out objects, and coos. No dysmorphic features or skin manifestation were noted and she did not present with any syndromic features. Another EEG was conducted that showed right-sided dominant spikes, polyspikes, sharps, and slow wave discharges [Figure 2]. Her seizures were intractable with polytherapy of AEDs. At the age of 14 months, the child was referred for possible surgical intervention to “Regional University Hospital (CHRU) in Lille, France,” where right functional hemispherectomy was performed successfully. After the surgery, the toddler came back to Pakistan and remained 100% seizure free, and we are tapering off the medicine. There were no immediate or long-term postsurgical complications seen. Currently, her seizures are controlled on low-dose Levetiracetam.
Figure 2.
EEG recording shows predominantly right-sided spike, polyspikes, and wave discharges
DISCUSSION
Malformations of cortical development arise due to disruption in the proliferation, migration, or postmigration stages during the development of cortex.[6] Disruption in any of these processes can cause seizures and neurodevelopmental delay in children.[6] HME, characterized by the hamartomatous growth of a cerebral hemisphere, has been categorized under the term “cortical dysgenesis” owing to disorders of proliferation.[7]
HME is categorized into three types: isolated, syndromic, and total.[8] iHME has no associated hemicorporal hypertrophy or cutaneous or systemic involvement. Syndromic HME (for example, epidermal nevus syndrome and Proteus syndrome) is associated with other features, which include hemicorporal hypertrophy of the ipsilateral part of the body. Total HME, which is the least common form, also involves enlargement of the brain stem and cerebellum. Cases of syndromic HME have been reported from Pakistan previously;[9] however, here we report the first case of iHME from our institute after receiving consent from the parents.
Previous studies have shown that mutations in AKT3, PIK3CA, and mTOR genes are associated with iHME2. In particular, the association of the modulation of mTOR signaling cascade and iHME has been the focus of many studies.[10] Some studies suggest that mTOR activation itself can produce nerve cell excitability and this can be helpful in explaining why patients with iHME have seizures.[10] These findings show that further research needs to be conducted on iHME, not only to better understand this disorder but also to develop better treatment options for these patients.
CONCLUSION
Functional hemispherectomy is a very good treatment option in iHME with intractable seizures. But expertise needs to be developed to provide this option to more patients in a local setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Santos AC, Escorsi-Rosset S, Simao GN, Terra VC, Velasco T, Neder L, et al. Hemispheric dysplasia and hemimegalencephaly: Imaging definitions. Childs Nerv Syst. 2014;30:1813–21. doi: 10.1007/s00381-014-2476-6. [DOI] [PubMed] [Google Scholar]
- 2.Baek ST, Gibbs EM, Gleeson JG, Mathern G W. Hemimegalencephaly, a paradigm for somatic postzygotic neurodevelopmental disorders. Curr Opin Neurol. 2013;26:122–7. doi: 10.1097/WCO.0b013e32835ef373. [DOI] [PubMed] [Google Scholar]
- 3.Mirzaa GM, Poduri A. Megalencephaly and hemimegalencephaly: breakthroughs in molecular etiology. Am J Med Genet C Semin Med Genet. 2014;166C:156–72. doi: 10.1002/ajmg.c.31401. [DOI] [PubMed] [Google Scholar]
- 4.Tinkle BT, Schorry EK, Franz DN, Crone KR, Saal HM. Epidemiology of hemimegalencephaly: A case series and review. Am J Med Genet A. 2005;139:204–11. doi: 10.1002/ajmg.a.31024. [DOI] [PubMed] [Google Scholar]
- 5.Geschwind DH, Miller BL. Molecular approaches to cerebral laterality: Development and neurodegeneration. Am J Med Genet. 2001;101:370–81. [PubMed] [Google Scholar]
- 6.Jamuar SS, Walsh CA. Genomic variants and variations in malformations of cortical development. Pediatr Clin North Am. 2015;62:571–85. doi: 10.1016/j.pcl.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns W B. A developmental and genetic classification for malformations of cortical development: Update 2012. Brain. 2012;135:1348–69. doi: 10.1093/brain/aws019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flores-Sarnat L. Hemimegalencephaly: Part 1. Genetic, clinical, and imaging aspects. J Child Neurol. 2002;17:373–84. doi: 10.1177/088307380201700512. [DOI] [PubMed] [Google Scholar]
- 9.Rafique MZ, Ahmad MN, Yaqoob N, Ahsan H. Diffuse bilateral thalamic astrocytoma. J Coll Physicians Surg Pak. 2007;17:170–2. [PubMed] [Google Scholar]
- 10.Crino PB. mTOR signaling in epilepsy: insights from malformations of cortical development. Cold Spring Harb Perspect Med. 2015;5(4):1–17. doi: 10.1101/cshperspect.a022442. [DOI] [PMC free article] [PubMed] [Google Scholar]