To
The Editor
Sir,
Medulloblastoma constitutes one of the most commonly occurring intracranial tumors in the pediatric age group. It involves the posterior fossa with the site of predilection being the cerebellar vermis.[1] Rarely, medulloblastoma may be located in the cerebellar hemisphere, which is commonly noticed in the adult. A medulloblastoma with epicenter in the cerebellopontine angle[1,2,3,4,5,6] in extra-axial space is extremely uncommon and exact management remains debatable due to paucity of published literature. Till date about 27 cases of cerebellopontine medulloblastoma have been reported but mostly in the adult age group as isolated case reports and only few case reports are available referring to the pediatric age group. The authors did an extensive search on Pubmed and Medline and could manage to collect only seven pediatric cases of cerebellopontine angle medulloblastoma and authors add another interesting case from their experience, so a total of eight cases form the cohort of the current study. There were 50% males (n = 4), with mean age at diagnosis being 10 years (ranging from 3 to 17 years), and the commonest histopathological type of pediatric cerebellopontine medulloblastoma was of the classic variety (43%).
A 16-year-old female student presented to our emergency neurosurgical services with a complaint of progressive worsening headache associated with repeated episodes of projectile vomiting over last 2 months and diminution of hearing in the right ear with mild facial symmetry for the last one month. She developed altered sensorium since early morning on the day of admission. Examination at admission revealed irritation and drowsiness with stable vitals. Neurological examination revealed the presence of bilateral papilledema on fundi evaluation and bilateral six nerve paresis. She also had lower motor neurone seventh cranial nerve paresis and right-sided gross cerebellar signs.
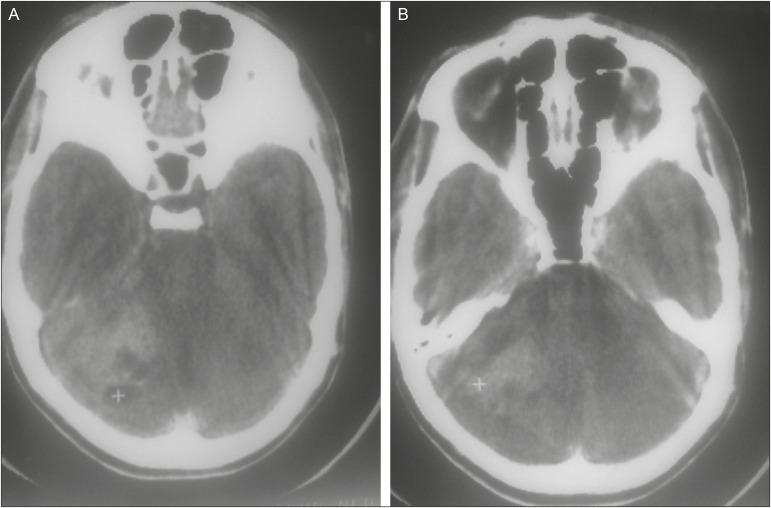
An emergency cranial computed tomography scan revealed the presence of a large heterogeneous hyperdense mass lesion located in the right cerebellopontine angle causing distortion and displacement of brainstem and right cerebellar hemisphere and obliterating fourth ventricles producing marked obstructive hydrocephalus with periventricular ooze. An intravenous contrast study showed heterogeneous enhancement with multiple hypodense areas [Figure 1A, B]. Although magnetic resonance imaging scan study of the brain was planned, the patient neurologically worsened rapidly due to aggravations of obstructive hydrocephalus and an emergency surgery was performed instead of ventriculo-peritoneal shunt under general anesthesia.
Figure 1.
(A) Computed tomography scan of head showing heterogeneous mass lesion in cerebello-pontine angle with distortion of brainstem and obliteration of fourth ventricle associated with small cyst. (B) Noncontrast cranial computed tomography scan showing heterogeneous mass lesion located in cerebello-pontine angle
She underwent right retromastoid craniectomy in the sitting position. After first making a small incision over the dura in the inferno-medial quadrant and releasing CSF from cisternal magna, posterior fossa became lax and further dura was opened and cerebellum was retracted using a retractor and CSF was released from the cerebellopontine angle cistern; a well-circumscribed mass lesion became evident. It was soft in consistency with areas of firmness, highly vascular, suckable, and greyish pink in color, and near total excision of mass was done with anatomical preservation of the seventh and eight cranial nerve complexes and after securing hemostasis wound was closed in layers.
In the immediate postoperative period, she was electively ventilated overnight. The next morning, she was extubated. Postoperative period was uneventful except that there was no improvement of the right seventh and eighth nerve deficit. She was discharged from the hospital on the 12th day. Histopathological examination of the specimen revealed a highly cellular tumor with arrangement of lobular patterns, and reticulum stain showed a dense network of reticulin fibers. Immunohistochemical study revealed the diagnosis of the desmoplastic variant of medulloblastoma. She received radiotherapy after 2 months following surgery. At the last follow-up, 6 months after the radiotherapy, she was doing well although mild facial paresis was persisting.
Medulloblastoma represents one of the commonest pediatric intracranial tumors and is located in the posterior fossa with preferred site of predilection being the cerebellar vermis. It usually presents with rapidly progressing clinical course along with the feature of the raised intracranial tension and cerebellar dysfunction.[1,2] Rarely, medulloblastoma may be located in the cerebellar hemisphere and commonly in the adult.[3,4,5,7]. Extra-axially, the medulloblastoma may get localized in two typical areas: the tentorial region and the cerebellopontine angle.[6]
Development of medulloblastoma in the cerebellopontine angle is regarded as an extremely uncommon entity and typically represents the desmoplastic variant of medulloblastoma, occurring in the age group of 19–46 years. Only a few isolated cases are reported in the pediatric age group.[8,9,10,11,12,13]
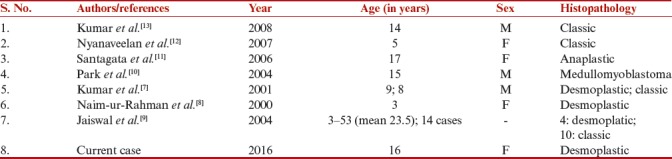
Pediatric cerebellopontine angle medulloblastoma tends to occur equally in males and females, with mean age of 10 years (range 3–17 years) at the time of diagnosis [Table 1]. Our case is interesting and probably the third in the pediatric age group, where desmoplastic medulloblastoma was entirely located in the cerebellopontine angle.[7,8]
Table 1.
Summary of published pediatric cerebello-pontine angle medulloblastoma
Clinically, pediatric cerebellopontine angle medulloblastoma presents with symptoms of raised intracranial pressure and cerebellar dysfunction along with features of the seventh and eighth cranial nerve dysfunction. Due to the lack of definite and characteristic clinical features, audiometry examination or even computed tomography and magnetic resonance imaging study may not be able to clearly establish the diagnosis in the preoperative stage and differentiate it from other common regional lesions including acoustic schwannoma, meningioma, cholesteatoma, and schwannoma of lower cranial nerves. Kumar et al.[7] observed that diminution of hearing or involvement of the seventh cranial nerve is uncommon and may help to differentiate pediatric cerebellopontine angle medulloblastoma from acoustic schwannoma. Even few cerebellopontine angle medulloblastoma cases may develop acute labyrinthine failure,[4] and these cases with acute onset with evidence of the early cerebellar signs and ataxic gait may indicate an axial origin of tumor, but the presence of positional nystagmus, may be an early sign suggestive of cerebellopontine angle medulloblastoma than comparing to other mass lesions such as schwannoma and meningioma.[7]
The site of origin of medulloblastomas occurring in the cerebellopontine angle is still debatable. It is postulated that pediatric cerebellopontine angle medulloblastoma may originate from external granular layer remnants in the cerebellar hemisphere, mostly from the flocullus or proliferating residue of the lateral medullary vellum and further projecting into the cerebellopontine cistern.[5,6]
The commonest histopathological type of pediatric cerebellopontine angle medulloblastoma is classic (43%), followed by anaplastic and medullomyoblastoma[8,9,10,11,12,13] [Table 1].
The mainstay of therapy for pediatric cerebellopontine angle medulloblastoma is multimodality combination therapy, which includes primary craniotomy and gross total surgical excision followed by adjuvant therapy, comprising radiotherapy and chemotherapy.[14,15] Mehta et al.[4] observed 30% 5-year survival in cases who underwent surgery followed by radiotherapy. In pediatric cerebellopontine angle medulloblastoma, the lesion is usually approached with retromastoid craniectomy and maximum decompression of lesions is achieved with careful preservation of cranial nerves and brainstem. Cordon et al.[14] advocated chemotherapy as it helps in prolonging disease-free survival.
To summarize the cerebellopontine angle medulloblastoma represents an extremely rare group of lesions, typically reported to occur in the adult but can also occur in the pediatric age group. All cases of cerebellopontine angle mass lesions presenting with atypical clinical signs and symptoms merit a consideration for possibility of the existence of pediatric cerebellopontine angle medulloblastoma, which must be kept as one of the differentials, although incidence remains extremely uncommon, and patients should be also explained about the possible need of adjuvant therapy if histopathological examination reveals presence of medulloblastoma.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- 1.Spina A, Boari N, Gagliardi F, Franzin A, Terreni MR, Mortini P. Review of cerebellopontine angle medulloblastoma. Br J Neurosurg. 2013;27:316–20. doi: 10.3109/02688697.2012.741733. [DOI] [PubMed] [Google Scholar]
- 2.Hubbard JL, Scheithauer BW, Kispert DB, Carpenter SM, Wick MR, Laws ER., Jr Adult cerebellar medulloblastomas: the pathological, radiographic, and clinical disease spectrum. J Neurosurg. 1989;70:536–44. doi: 10.3171/jns.1989.70.4.0536. [DOI] [PubMed] [Google Scholar]
- 3.Fallah A, Banglawala SM, Provias J, Jha NK. Extra-axial medulloblastoma in the cerebellopontine angle. Can J Surg. 2009;52:E101–2. [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta JS, Sharr MM. An unusual cause of acute labyrinthine failure. J Laryngol Otol. 1998;112:193–5. doi: 10.1017/s0022215100140290. [DOI] [PubMed] [Google Scholar]
- 5.Yamada S, Aiba T, Hara M. Cerebellopontine angle medulloblastoma: case report and literature review. Br J Neurosurg. 1993;7:91–4. doi: 10.3109/02688699308995062. [DOI] [PubMed] [Google Scholar]
- 6.Giangaspero F, Chieco P, Ceccarelli C, Lisignoli G, Pozzuoli R, Gambacorta M, et al. “Desmoplastic” versus “classic” medulloblastoma: comparison of DNA content, histopathology and differentiation. Virchows Arch A Pathol Anat Histopathol. 1991;418:207–14. doi: 10.1007/BF01606058. [DOI] [PubMed] [Google Scholar]
- 7.Kumar R, Achari G, Mishra A, Chhabra DK. Medulloblastomas of the cerebellopontine angle. Neurol India. 2001;49:380–3. [PubMed] [Google Scholar]
- 8.Naim-ur-Rahman, Jamjoom A, al-Rayess M, Jamjoom ZA. Cerebellopontine angle medulloblastoma. Br J Neurosurg. 2000;14:262–3. doi: 10.1080/026886900408504. [DOI] [PubMed] [Google Scholar]
- 9.Jaiswal AK, Mahapatra AK, Sharma MC. Cerebellopontine angle medulloblastoma. J Clin Neurosci. 2004;11:42–5. doi: 10.1016/j.jocn.2003.02.005. [DOI] [PubMed] [Google Scholar]
- 10.Park SY, Kim JH, Kim KT, Kim YJ, Kim TH, Hwang K, et al. A case of medullomyoblastoma of cerebellopontine angle mimicking acoustic neuroma. Yonsei Med J. 2004;45:719–22. doi: 10.3349/ymj.2004.45.4.719. [DOI] [PubMed] [Google Scholar]
- 11.Santagata S, Kesari S, Black PM, Chan JA. Anaplastic variant of medulloblastoma mimicking a vestibular schwannoma. J Neurooncol. 2007;81:49–51. doi: 10.1007/s11060-006-9235-9. [DOI] [PubMed] [Google Scholar]
- 12.Nyanaveelan M, Azmi A, Saffari M, Banu SK, Suryati MY, Jeyaledchumy M. Cerebellopontine angle medulloblastoma. Med J Malaysia. 2007;62:173–4. [PubMed] [Google Scholar]
- 13.Kumar R, Bhowmick U, Kalra SK, Mahapatra AK. Pediatric cerebellopontine angle medulloblastomas. J Pediatr Neurosci. 2008;3:127–30. [Google Scholar]
- 14.Cordon BJ, Strauss LC, Killmond T, Carson BS, Wharam MD, Kumar AJ, et al. Cisplatin, Ara-C and etoposide (PAE) in treatment of recurrent childhood brain tumours. J Neuro Oncol. 1991;11:57–63. doi: 10.1007/BF00166998. [DOI] [PubMed] [Google Scholar]
- 15.Boukobza M, Polivka M. Medulloblastoma of the cerebellopontine angle in a child: a case report and review of the literature. J Mol Biomark Diagn. 2016;13:3. [Google Scholar]