Abstract
Objectives
To determine the efficacy of the physiological ICSI technique (PICSI) vs. conventional ICSI in the prognosis of couples with male factor, with respect to the following outcome measures: live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage rates.
Methods
A systematic review of the literature, extracting raw data and performing data analysis. Patient(s): Couples with the male factor, who were subjected to in-vitro fertilization. Main Outcome Measures: rates of live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage.
Results
In the systematic search, we found 2,918 studies and an additional study from other sources; only two studies fulfilled the inclusion criteria for this systematic review. The rates of live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage were similar for both groups.
Conclusion
There is no statistically significant difference between PICSI vs. ICSI, for any of the outcomes analyzed in this study. Enough information is still not available to prove the efficacy of the PICSI technique over ICSI in couples with male factor.
Keywords: PICSI, physiological ICSI, hyaluronic acid, HA sperm selection, male factor
INTRODUCTION
Age, associated pathologies, geographic location, consumption of alcohol, tobacco and other drugs, exposure to environmental and chemical contaminants, body and environmental temperatures, are some of the causes of male infertility (Gao et al., 2007; He et al., 2015; Imai et al., 2010; Verratti et al., 2008; Zou et al., 2011). Presently, the way to evaluate a semen sample is through direct spermatobioscopy, a descriptive tool that does not evaluate damage in sperm DNA (Morales et al., 2007; Espinoza-Navarro et al., 2010; World Health Organization, 2010; Cooper et al., 2010; González Ravina & Pacheco Castro, 2011). It is known that defects in genetic material, such as anomalies in chromatin condensation with respect to the sperm maturation process, the integrity of the DNA molecule in conjunction with the presence of DNA double chain ruptures, as well as in the single DNA chain, or the presence of chromosomal anomalies, are all related to infertility (Cortes-Gutiérrez et al., 2007). Oocytes are capable of repairing sperm damage, depending on the type of damage that is present in the spermatozoa (Castillo-Baso & García-Villafaña, 2012).
Diverse techniques have been developed for assisted reproduction to increase pregnancy likelihoods. One of the most used techniques is the intracytoplasmic sperm injection or conventional ICSI. However, in this technique sperm selection is subjective, since the embryologist chooses, under his/her criterion, which are the best spermatozoa seen at low resolution, thus eliminating the process of natural selection. There is a greater risk of congenital defects and miscarriages, since it is impossible to know whether the chosen spermatozoa have alterations in their nucleus or if there is DNA fragmentation (Castillo-Baso & García-Villafaña, 2012; González-Ortega et al., 2010).
Hence, the physiological ICSI technique arose (PICSI - physiologically selected intracytoplasmic sperm injection). This technique is based on the fact that the mature sperm head has a specific receptor that allows it to bind to hyaluronic acid (HA), the main component of the cumulus oophorous; this is in contrast to the immature spermatozoa, which do not have this ability to bind to HA. (Castillo-Baso & García-Villafaña, 2012; González-Ortega et al., 2010). It has been shown that spermatozoa that bind to HA have completed the spermatogenic process of remodeling the plasmatic membrane, cytoplasmic extrusion and nuclear maturity. Thus, they have a whole DNA and low frequency of aneuploidies and miscarriages. In this way, the genomic contribution of the spermatozoa to the zygotes can be compared to that of the spermatozoa that are selected by the cumulus oophorous during natural fertilization (Castillo-Baso & García-Villafaña, 2012; González-Ortega et al., 2010). PICSI has previously shown satisfactory results in diverse study groups, where the male factor was present and where the influence of sperm DNA fragmentation on reproduction techniques has been described (Castillo-Baso & García-Villafaña, 2012; Gongora-Rodriguez & Fontanilla-Ramirez, 2010; Parmegiani et al., 2010a; Majumdar & Majumdar, 2013). Nevertheless, they suggest doing further studies to this respect.
The objective of this systematic review is to determine the efficacy of the PICSI technique vs. the ICSI in the prognosis of couples with male factor, with respect to the following outcome measures: live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage rates.
MATERIALS AND METHODS
Inclusion Criteria
Type of studies
A controlled search for clinical trials was carried out, in English and Spanish, up to August of 2015, including the following MeSH terminology: "male infertility"; "male factor"; "ICSI"; "PICSI"; "Physiological ICSI"; "Intracytoplasmic Sperm Injection"; "Physiological Intracytoplasmic Sperm Injection"; "hyaluronic acid"; "HA sperm selection".
Type of participants
Couples with the male factor, comparing PICSI vs. ICSI. Studies which did not fulfill the inclusion criteria were taken off the search.
Type of intervention
The intervention of interest for this study is the systematic review of the literature, extraction of raw data and data analyses.
Outcome measures
The primary outcomes of this systematic review were: miscarriage, live births and clinical pregnancy. Secondary outcomes were: implantation, embryo quality and fertilization.
Search methods and selection of studies
Electronic search
The PICO (Santos et al., 2007) method was used to construct the research question and the bibliographic search. We performed a thorough literature search in PubMed, LILACS, Medigraphic, ELSEVIER and Cochrane. The upper time limit for the searches was August, 2015.
Search of other sources
The bibliographies of the included articles were searched, looking for additional references, and we contacted the main authors of the included trials, in order to solve questions and complete missing information.
Data collection and analysis
The systematic review was carried out according to recommendations from the Cochrane Collaboration (Higgins & Green, 2011). The Review Manager 5.3 (The Cochrane Collaboration, 2014) was used to do the analyses.
Study selection
In an independent manner, two authors read the publications which were found through the systematized search, in order to find the trials that fulfilled the inclusion criteria of this review. We put together a list of the excluded trials, together with reasons for exclusion. Disagreements were resolved through discussion and were arbitrated by a third and fourth author of the review, when needed. Missing information was requested from the original authors, when needed.
Manual searches were carried out for abstracts of the papers found, for their possible inclusion in the review. We rejected papers that were not a report of a prospective clinical trial, if they were not about couples with male factor and compared PICSI vs. ICSI, and if they did not present quantitative outcomes with respect to live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage rates.
Data extraction and management
Two reviewers, working independently, extracted data from each study, including them in an Excel sheet (search engine, title, authors, journal, years, system - SpermSlow, PICSI dish, others), designation of study (retrospective, prospective, prospective-randomized, other), type of study (abstract, full-text, other), type of intervention, inclusion criteria, exclusion criteria, objectives, results and results obtained from contact with authors). Differences in opinions were discussed and, when needed, a third person was consulted before the arbitrated consensus. In the case of missing data, or when there was a need for clarification, the study's authors were contacted.
Evaluation of the risk of bias in the included studies
The risk of bias in the included studies was evaluated, using the Cochrane Risk of Bias Tool (Higgins & Green, 2011); this was done independently by two of the authors. Any disagreement was resolved through discussion among the review authors, until consensus was reached. If the information was not available in the published document, we contacted one of the authors, in order to properly evaluate the trials.
We evaluated the following types of biases: random sequence generation (selection bias), allocation sequence concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other potential sources of bias. For the final risk of bias evaluation, we assigned values to "low risk of bias", "high risk of bias" or "uncertain risk of bias."
Analysis
Measuring treatment effects
In order to show the characteristics of the studies, including their results, the information is described from the quantitative point of view, in order to combine the results of the included studies; this was done as long as they had similar characteristics as a function of the outcome variable. The values described in each study were taken into account, just as they were reported by the authors of the original studies. In the case of missing information, we contacted the authors.
The following events were estimated, using odds ratio (OR) as a measurement of treatment effect, with its respective CI of 95%: live birth, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage rates. The statistical significance was established at a p<0.05 value. Outcome data were grouped for each study, using the Mantel-Haenszel (M-H) model and the randomized model.
The statistical heterogeneity was quantified using the statistical I2 package, which shows the variation proportion among the studies, with respect to total variation, that is, the proportion of the total variation that is attributable to heterogeneity (Higgins et al., 2003). To estimate the variance between the studies, we used the statistical Tau2 package (Higgins & Green, 2011).
All the data was analyzed using the Review Manager, version 5.3 statistical package (The Cochrane Collaboration, 2014), recommended by the Cochrane Collaboration (Higgins & Green, 2011). We reported our results according to the Guidelines for the Publication of Systematic Reviews and Meta-Analyses of Studies that Evaluate Health Interventions (Directrices para la Publicación de Revisiones Sistemáticas y Metaanálisis de Estudios que Evalúan Intervenciones Sanitarias - PRISMA) (Liberati et al., 2009).
RESULTS
Description of the studies
Search results
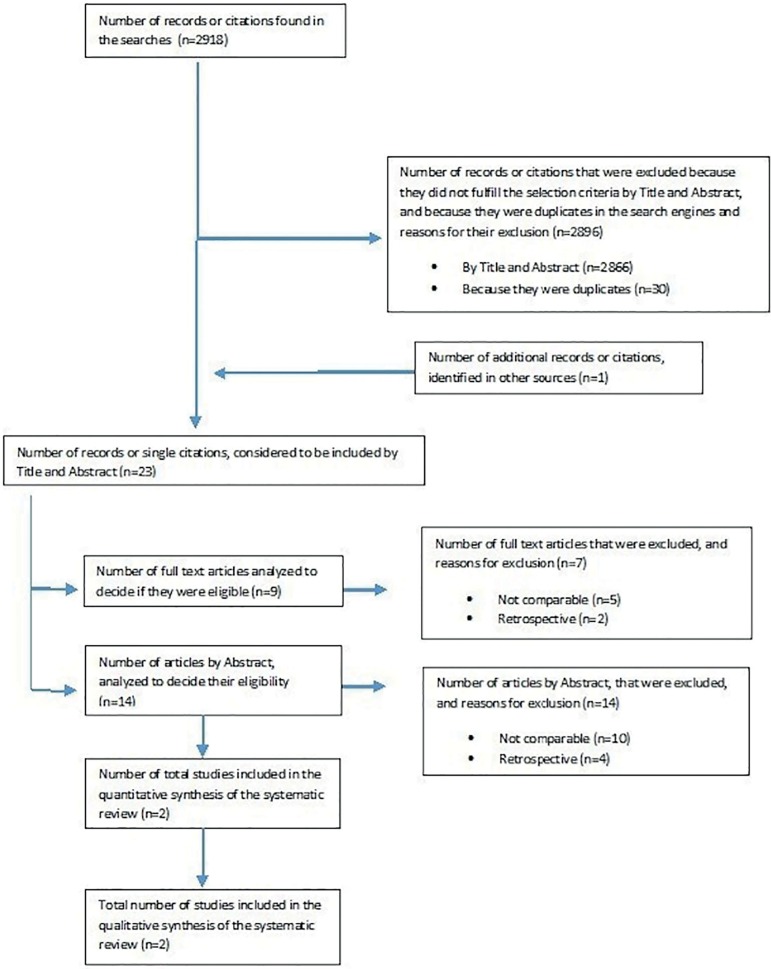
A total of 2,918 studies were found using all search engines (PubMed, LILACS, Medigraphic, ELSEVIER and Cochrane) and an additional study was found through other sources, up to August, 2015. From these, two studies were included in this systematic review (Castillo-Baso & García-Villafaña, 2012 ; Parmegiani et al., 2010a) (Figure 1).
Figure 1.
Flow diagram illustrating the selection of trials included in the meta-analysis
Included studies
All studies that fulfilled the inclusion criteria were included. Two publications were included (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a). The types of PICSI systems used by these authors were SpermSlow (Parmegiani et al., 2010a) and PICSI dish (Castillo-Baso & García-Villafaña, 2012).
From these two studies, data pertaining to a total of 340 women was analyzed. A total of 366 treatments or cycles were performed; of these, 364 cycles involved transfers (182 were performed using the PICSI technique, where all cycles involved transfers, and 184 using the ICSI technique, where only 182 cycles involved transfers).
Although practically the same objective was analyzed in both included studies (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a), Parmegiani et al. (2010a) divided their primary objective into three secondary objectives, of which only the last one was interesting to us, and this was the one that was taken into account.
Also, these authors (Parmegiani et al., 2010a) did not take into account sperm morphology; however, they considered these samples as having male factor due to the total number of spermatozoa and their motility. With respect to female patients, all were candidates for ICSI, with their own oocytes and fresh cycles (Castillo-Baso & García-Villafaña, 2012).
In the Castillo-Baso & Garcia-Villafaña (2012) study, only sperm morphology was taken into account. For our study's objectives, we only used, within the three described groups of sperm morphology (≤1, 2-4% and >4% with KRUGER), the ≤1 and 2-4%, morphology groups, considering them to bear the male factor. With respect to female patients, all were candidates for ICSI, with their own oocytes and fresh cycles.
Excluded studies
All studies which did not fulfill the inclusion criteria were excluded. Twenty one publications were excluded for reasons shown in Table 1.
Table 1.
Excluded studies and reasons for exclusion.
| Author | Reason for exclusion from study |
|---|---|
| Azevedo et al., 2013 | Retrospective study. It is only an abstract. Does not have complete information that is needed for its analysis. Does not analyze live birth outcomes. |
| Barak et al., 2001 | It is only an abstract. It does not have the complete information needed for its analysis. It does not analyze live birth, embryo quality and miscarriage rates. |
| Brassesco-Macazzaga et al., 2009 | It does not analyze the live birth and miscarriage outcomes. |
| Castillo-Baso et al., 2011 | It is only an abstract. It does not have the complete information needed for its analysis. It does not analyze the live birth and miscarriage outcomes. |
| Hambiliki & Bungum, 2012 | It is only an abstract. It does not have the complete information needed for analysis. Does not analyze live birth, implantation and miscarriage outcomes. |
| Lee et al., 2013 | Retrospective study. Only an abstract. It does not have the complete information needed for analyses. Does not analyze live birth outcomes. |
| Majumdar & Majumdar, 2013 | Patients with inexplicable infertility and normozoospermic males |
| Menezo et al., 2010 | It is only an abstract. It does not have the complete information needed for the analysis. Does not analyze outcomes related to live birth, fertilization and miscarriage rates. |
| Parmegiani et al., 2010b | Retrospective study |
| Parmegiani et al., 2012 | Compares two physiologic-ICSI systems: SpermSiow vs. PICSI |
| Santibáñez-Morales et al., 2012 | Retrospective study. It does not analyze live birth, fertilization and miscarriage outcomes. |
| Saymé et al., 2013 | Retrospective study. It is only an abstract, not having the complete information needed for analysis. It does not analyze live birth outcomes. |
| Van Den Bergh et al., 2009 | It does not analyze live birth, implantation, embryo quality, clinical pregnancy and miscarriage outcomes. |
| Worrilow et al., 2005 | It is only an abstract. It does not have the complete information needed for analysis. It does not analyze live birth and miscarriage outcomes. |
| Worrilow et al., 2006 | Only an abstract. It does not have the complete information needed for analysis. It does not analyze live birth outcomes. |
| Worrilow et al., 2007 | Is only an abstract. It does not have the complete information needed for the analysis. It does not analyze live birth outcomes |
| Worrilow et al., 2009 | It does not analyze live birth, fertilization and miscarriage outcomes. |
| Worrilow et al., 2010 | It does not analyze live birth and miscarriage outcomes. |
| Worrilow et al., 2011a | It Does not analyze live birth, fertilization and miscarriage outcomes. |
| Worrilow et al., 2011b | It does not analyze live birth and fertilization outcomes. |
| Worrilow et al., 2013 | It does not analyze live birth and embryo quality outcomes. |
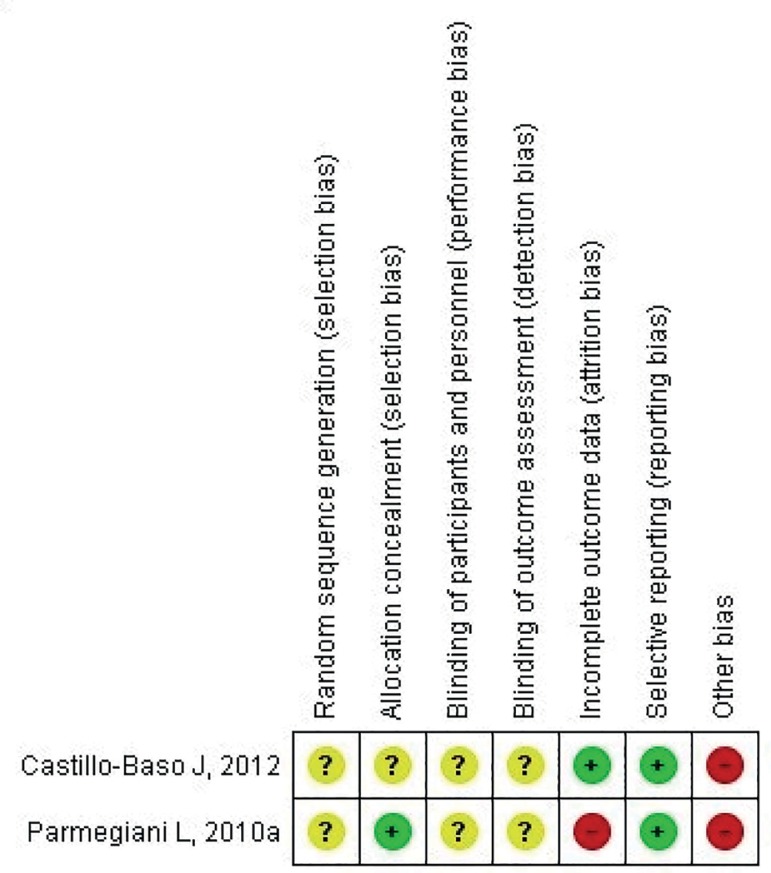
Risks of bias in the included studies
In Figure 2 we can see the different types of biases which may be present in the two papers included in this review; they are "risk of uncertain bias" (yellow: "'?" mark), "risk of low bias" (green: "+" sign) or "risk of high bias" (red: "-" sign). The "risk of uncertain bias" category is the most frequent. It is not considered to be a sign of bad quality of the included studies, given their nature. For the risk of random sequence generation (selection bias) or allocation sequence concealment (selection bias), only one study mentions being random, without mentioning the generation of the sequence and the fact that sealed envelopes were used, which were provided by a third party (Parmegiani et al., 2010a). The "risk of uncertain bias" was considered for both included studies (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a).
Figure 2.
Risks of bias of the included studies
With respect to the risk of blinding participants and personnel (performance bias) and blinding the outcome assessment (detection bias), none of the studies (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a) mentions blinding of the laboratory and medical personnel, as well as of the analysts of the results; we considered this to be "risk of uncertain bias". Thus, for the risk of incomplete outcome data (attrition bias), only one study shows it in its results, desertion of two patients, not mentioning their reasons - this was considered to be a "high risk bias" (Parmegiani et al., 2010a). For the second study (Castillo-Baso & García-Villafaña, 2012), all patients who started the treatment, finished it; this was considered as "a low risk bias". With respect to the selective outcome reporting bias (reporting bias), in both studies (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a) their objective was clear and they mention at the end whether or not it was reached; this was estimated as being "low risk of bias".
Finally, for other potential sources of bias, both studies bear "high risk biases" (Castillo-Baso & García-Villafaña, 2012; Parmegiani et al., 2010a), since one of them does not mention, within the described semen parameters, the patients' sperm morphology (Parmegiani et al., 2010a). In the case of the second study, that one does not mention sperm concentration and motility (Castillo-Baso & García-Villafaña, 2012).
Effects of interventions
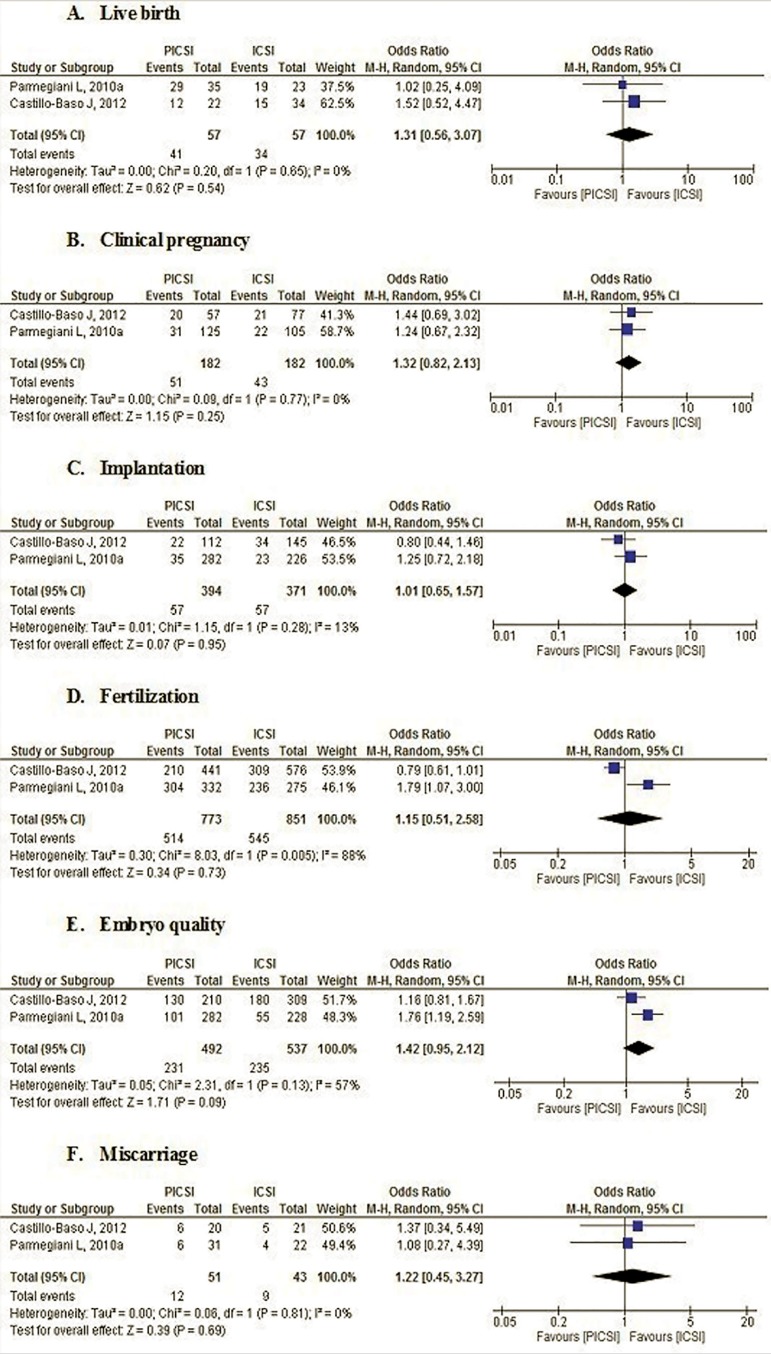
This systematic review shows that there is no statistically significant difference between both techniques, for none of the analyzed outcomes (Figure 3).
Figure 3.
Effects of interventions
For the outcome pertaining to live births, the results of the two studies (114 events) showed no significant difference between both techniques (OR=1.31, CI 95% 0.56-3.07, p=0.54). The I2 value was 0%, which shows "excellent statistical homogeneity".
For the clinical pregnancy outcome, results from both studies (364 events) showed no significant difference between the two techniques (OR=1.32, CI 95% 0.82-2.13, p=0.25). The I2 value was 0%, which shows "excellent statistical homogeneity".
With respect to the implantation outcome, the results of the two studies (765 events) showed no significant difference between both techniques (OR=1.01, CI 95% 0.65-1.57, p=0.95). The I2 value was 13%, which shows "low statistical heterogeneity".
For the fertilization outcome, the results of the two studies (1624 events), showed no significant difference between both techniques (OR=1.15, CI 95% 0.51-2.58, p=0.73). The I2 value was 88%, which shows "high statistical heterogeneity".
For the embryo quality outcome, the results of the two studies (1029 events) showed no significant difference between both techniques (OR=1.42, CI 95% 0.95-2.12, p=0.09). The I2 value was 57%, which indicates "moderate statistical heterogeneity".
With respect to the miscarriage outcome, the results of the two studies (94 events) showed no significant difference between PICSI vs. ICSI (OR=1.22, CI 95% 0.45-3.27, p=0.69). The I2 value was 0%, which shows "excellent statistical homogeneity".
DISCUSSION
The results of this systematic review were not statistically significant for all outcome measures. With respect to the risk of bias in the included studies, most of our results showed "uncertain risk of bias", since the randomization and blinding of participants is not essential, due to the nature of the studies. This risk was considered to be irrelevant, since in order to carry out the procedures, one must know which technique to apply and which one is adequate for each patient, and for this reason, we need to know the characteristics of the case. However, for the risk caused by other potential bias sources, both studies had a "high risk of bias," since they did not take into account sperm morphology, concentration and motility, which are fundamental parameters to determine the implementation of the PICSI or ICSI technique.
With respect to "statistical heterogeneity", we know that it only quantifies the variability between the study's results, and that it can be due to real differences related to the approach and execution of the included studies, or to other causes. In other words, it tries to quantify the variability in the results, that is measured in the different studies, with respect to the average global outcome, and to determine whether this variability is higher than what would be expected merely by chance.
The negative values of the statistical I2 are made to be equal to zero, so that the I2 is between 0% and 100%. A value of 0% shows that there is no observed heterogeneity and the greater values show a growing heterogeneity. Having markers that indicate the degrees of heterogeneity, 25% is considered to be "low statistical heterogeneity", 50% shows "moderate statistical heterogeneity" and 75% implies "high statistical heterogeneity". These markers are attributable to the statistical heterogeneity of the studies, and not to chance (Higgins et al., 2003). An I2 of 0% is considered to have "excellent statistical homogeneity" and if variability existed in the estimation of the effects, this would be due to sampling error in the trials, and not to heterogeneity. This is the case in outcomes of live births, clinical pregnancy and miscarriage, in our review, since the results do not vary more than what would be expected from influence by chance. Finding a "low statistical heterogeneity" for the implantation outcome leads us to consider that there is scarce variability attributable to statistical heterogeneity between the studies and not to chance. Also, for embryo quality outcomes, we found "moderate statistical heterogeneity", considering it to be a moderate variability, attributable to the statistical heterogeneity between the studies and not to chance. On the other hand, for the fertilization outcome, we found a "high statistical heterogeneity", showing that the greatest part of the variability between the studies is due to heterogeneity, more than chance.
In order to decrease the "statistical heterogeneity" in this systematic review, it is important to guarantee that there is no "clinical heterogeneity" that would make the combination of results impossible, but it is not possible to maintain a "low clinical heterogeneity" because few studies fulfilled our inclusion criteria; due to their high risk of bias, resulting in a limitation. As a consequence, only two studies were included in this systematic review.
Our results do not show a statistically significant difference when comparing PICSI vs. ICSI, and these results coincide with those from Majumdar & Majumdar, 2013; Hambiliki & Bungum, 2012; Worrilow et al., 2010. On the other hand, a statistically significant difference favors PICSI in the study by Worrilow et al. (2005; 2006; 2007; 2011a, 2011b; 2013). Over the years, these authors have studied the differences between these two techniques, with respect to diverse outcomes; there are variations between the studies concerning the following outcomes: fertilization, clinical pregnancy, implantation, miscarriage and embryo fragmentation. This coincides with Azevedo et al. (2013) and Lee et al. (2013), who also found statistically significant differences when comparing PICSI vs. ICSI with respect to the miscarriage outcome, and to implantation and clinical pregnancy in the case of the study by Lee et al. (2013).
As far as we know, this is the first systematic review that compares PICSI vs. ICSI in the prognosis of couples with male factor, taking into account the following outcome measures: live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage. We suggest that future studies be carried out according to the CONSORT guidelines; however, due to the nature of the intervention, it would be difficult to achieve blinding of the embryologist when performing the fertilization technique (PICSI vs. ICSI). The risk of bias could be reduced in blinding for outcome analysis and of the personnel performing the embryo transfers. It is important that these future studies provide quantitative information on results and that the rates of miscarriages, live births and clinical pregnancy be considered as primary results, without ignoring rates of implantation, fertilization and embryo quality, for the comparison of the techniques. We also recommend including the analysis of subgroups, in order to eliminate variables that affect results, such as sperm quality (morphology, concentration and motility), cause of female and male infertility, number and quality of transferred embryos, day of embryo transfer, fresh or frozen transfer, own oocyte or donated oocyte.
CONCLUSIONS
This systematic review showed no statistically significant difference between the PICSI and the ICSI techniques, for any of the studied outcome measures: live births, clinical pregnancy, implantation, embryo quality, fertilization and miscarriage rates.
Perhaps due to the small number of clinical studies included in this review, since few studies fulfilled our inclusion criteria, due to the high risk of bias of these, it was not possible to prove the statistical efficacy of the PICSI technique over the ICSI, in couples with male factor, with respect to the studied outcome measures.
More clinical studies are needed, in accordance with the CONSORT guidelines to reduce bias risks.
ACKNOWLEDGMENTS
The authors wish to thank Magda Atrián Salazar, for her review of this manuscript, Evelyn Aron for providing help with the English language, as well as Julián Ruiz Anguas, Ismael Horta Martínez and Luis Agustín Gallardo Trejo, for support given during the development of this study.
Footnotes
The study was carried out at: Hospital Universitario del Mar: Maestría en Medicina Reproductiva Humana, Universidad Autónoma de Barcelona, Barcelona, España.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
REFERENCES
- Azevedo AC, Albuquerque MCRM, Miyasato FC, Fujihara LS, Aranki JT, Albuquerque LET. Comparison Conventional PVP-ICSI vs. HA-PICSI: is there significant improvement in pregnancy rate? Fertil Steril. 2013;100(S530) doi: 10.1016/j.fertnstert.2013.07.286. [DOI] [Google Scholar]
- Barak Y, Menezo Y, Veiga A, Elder K. A physiological replacement for polyvinylpyrrolidone (PVP) in assisted reproductive technology. Hum Fertil (Camb) 2001;4:99–103. doi: 10.1080/1464727012000199371. [DOI] [PubMed] [Google Scholar]
- Brassesco-Macazzaga A, Del Río-Bueno F, Cairo-Doncos O, Rovira-Fontanals S, Monqaut A, Brassesco-Macazzaga M. Comparison between hyaluronan (SpermSlow) and polyvinylpyrrolidone media in sperm selection for intracytoplasmic sperm injection. Rev Int Androl. 2009;7:205–209. doi: 10.1016/S1698-031X(09)73387-4. [DOI] [Google Scholar]
- Castillo-Baso J, Garcia-Villafaña G, Santos-Haliscak R, Diaz P, Sepulveda-Gonzalez J, Hernandez-Ayup S. Embryo quality and reproductive outcomes of spermatozoa selected by physiologic-ICSI or conventional ICSI in patients with Kruger <4% and >4% normo-morphology. Fertil Steril. 2011;96(S159) doi: 10.1016/j.fertnstert.2011.07.623. [DOI] [Google Scholar]
- Castillo-Baso J, García-Villafaña G. Selección Rutinaria de Espermatozoides Utilizando la Tecnica "Physiological ICSI". Subespecialidad: Universidad Autónoma de Baja California; 2012. [Thesis] [Google Scholar]
- Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT, Vogelsong KM. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16:231–245. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- Cortes-Gutiérrez El, Dávila-Rodríguez MI, López-Fernández C, Fernández JL, Gosálvez J. Evaluación del daño en el DNA espermático. Actas Urol Esp. 2007;31:120–131. doi: 10.1016/S0210-4806(07)73609-4. [DOI] [PubMed] [Google Scholar]
- Espinoza-Navarro O, Cortés AS, Monreal J, Ferreccio C. Análisis de las variables en jóvenes sanos en Arica-Chile. Rev Méd Chile. 2010;138:1510–1516. doi: 10.4067/S0034-98872010001300006. [DOI] [PubMed] [Google Scholar]
- Gao J, Gao ES, Yang Q, Walker M, Wu JQ, Zhou WJ, Wen SW. Semen quality in a residential, geographic and age representative sample of healthy Chinese men. Hum Reprod. 2007;22:477–484. doi: 10.1093/humrep/del383. [DOI] [PubMed] [Google Scholar]
- Gongora-Rodriguez A, Fontanilla-Ramirez D. La fragmentación de ADN espermático, influencia sobre las técnicas de reproducción asistida y calidad embrionaria. Rev Colom Obstet Ginecol. 2010;61:160–164. [Google Scholar]
- González Ravina C, Pacheco Castro A. Implementación de los nuevos criterios de la OMS en la práctica clínica. Rev Asoc Est Biol Rep. 2011;16:4–9. [Google Scholar]
- González-Ortega C, Cancino-Villareal P, Pérez-Torres A, Vargas-Maciel MA, Martínez-Garza SG, Pérez Peña E, Gutiérrez-Gutiérrez AM. Inyección intracitoplásmica de espermatozoides morfológicamente seleccionados (IMSI) vs inyección intracitoplásmica de espermatozoides (ICSI) Ginecol Obstet Mex. 2010;78:652–659. [PubMed] [Google Scholar]
- Hambiliki F, Bungum M. Physiological ICSI (PICSI) versus standard ICSI: a prospective randomized sibling-oocyte trial. Hum Reprod. 2012;27:i62. [Google Scholar]
- He J, Cui J, Wang R, Gao L, Gao X, Yang L, Zhang Q, Cao J, Yu W. Exposure to Hypoxia at High Altitude (5380 m) for 1 Year Induces Reversible Effects on Semen Quality and Serum Reproductive Hormone Levels in Young Male Adults. High Alt Med Biol. 2015;16:216–222. doi: 10.1089/ham.2014.1046. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [[cited 2018 Mar 13]]. Version 5.1.0. [updated March 2011] Available from: http://handbook-5-1.cochrane.org/ [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai A, Ichigo S, Takagi H, Matsunami K, Suzuki N, Yamamoto A. Effects of cola intake on fertility: a review. Health. 2010;2:997–1001. doi: 10.4236/health.2010.29147. [DOI] [Google Scholar]
- Lee JH, Ryu MJ, Bark SH, Lee HS, Jeong HJ, Chung MK. The impact of strict sperm morphology on clinical outcome in couples undergoing conventional IVF, ICSI and Physiologic-ICSI (PICSI) cycles. Fertil Steril. 2013;100(S462-3) doi: 10.1016/j.fertnstert.2013.07.415. [DOI] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar G, Majumdar A. A prospective randomized study to evaluate the effect of hyaluronic acid sperm selection on the intracytoplasmic sperm injection outcome of patients with unexplained infertility having normal semen parameters. J Assist Reprod Genet. 2013;30:1471–1475. doi: 10.1007/s10815-013-0108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menezo Y, Junca AM, Dumont M, De Mouzon J, Cohen-Bacrie P, Khalifa MB. "Physiologic" (hyaluronic acid-carried) ICSI results in the same embryo quality and pregnancy rates as with the use of potentially toxic polyvinylpyrrolidone (PVP) Fertil Steril. 2010;94(S232) doi: 10.1016/j.fertnstert.2010.07.900. [DOI] [Google Scholar]
- Morales R, Lledo B, Ortiz Jose A, Rodriguez-Arnedo D, Fabregat A, Bernabeu R. Fragmentación del ADN espermático y su implicación en la fertilidad. Rev Iberoam Fertil. 2007;24:305–313. [Google Scholar]
- Parmegiani L, Cognigni GE, Bernardi S, Troilo E, Ciampaglia W, Filicori M. "Phisiologic ICSI": Hyaluronic acid (HA) favors selection of spermatozoa without DNA fragmentation and with normal nucleus, resulting in improvement of embryo quality. Fertil Steril. 2010a;93:598–604. doi: 10.1016/j.fertnstert.2009.03.033. [DOI] [PubMed] [Google Scholar]
- Parmegiani L, Cognigni GE, Ciampaglia W, Pocognoli P, Marchi F, Filicori M. Efficiency of hyaluronic acid (HA) sperm selection. J Assist Reprod Genet. 2010;27:13–16. doi: 10.1007/s10815-009-9380-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmegiani L, Cognigni GE, Bernardi S, Troilo E, Taraborrelli S, Arnone A, Maccarini AM, Filicori M. Comparison of two ready-to-use systems designed for sperm-hyaluronic acid binding selection before intracytoplasmic sperm injection: PICSI vs. Sperm Slow: a prospective, randomized trial. Fertil Steril. 2012;98:632–637. doi: 10.1016/j.fertnstert.2012.05.043. [DOI] [PubMed] [Google Scholar]
- Santibáñez-Morales A, Morales-Hernández FV, Vega-Hernández E, Regalado-Hernández JC, Sánchez-Serrano AP, Gaviño-Gaviño F, de la Jara Díaz J. Evaluación de resultados de PICSI en el Instituto Nacional de Perinatología Isidro Espinosa de los Reyes. Rev Mex Reprod. 2012;4:153–158. [Google Scholar]
- Santos CMC, Pimenta CAM, Nobre MRC. The PICO strategy for the research question construction and evidence search. Rev Lat Am. 2007;15:508–511. doi: 10.1590/S0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- Saymé K, Sollmann K, Mass DHA, Krebs T. The effect of hyaluronic acid coated pertri dish sperm selection (PICSI) on fertilization rate, embryo development and pregnancy rate and relationship to sperm quality in an IVF program. Fertil Steril. 2013;100(S529) doi: 10.1016/j.fertnstert.2013.07.284. [DOI] [Google Scholar]
- The Cochrane Collaboration . Review Manager (RevMan) RevMan, The Nordic Cochrane Centre; Copenhagen: The Nordic Cochrane Centre; 2014. Computer program. Version 5.3. [Google Scholar]
- Van Den Bergh MJG, Fahy-Deshe M, Hohl MK. Pronuclear zygote score following intracytoplasmatic injection of hyaluronan-bound spermatozoa: a prospective randomized study. Reprod Biomed Online. 2009;19:796–801. doi: 10.1016/j.rbmo.2009.09.022. [DOI] [PubMed] [Google Scholar]
- Verratti V, Berardinelli F, Di Giulio C, Bosco G, Cacchio M, Pellicciotta M, Nicolai M, Martinotti S, Tenaglia R. Evidence that chronic hypoxia causes reversible impairment on male fertility. Asian J Androl. 2008;10:602–606. doi: 10.1111/j.1745-7262.2008.00346.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO Laboratory Manual for the Examination and Processing of Human Semen. Geneva: World Health Organization; 2010. [Google Scholar]
- Worrilow KC, Huynh HT, Schillings WJ, Peters AJ, Johnston JB. Use of Hyaluronan Monolayer (HM), or PICSI Plate, in the Selection of Sperm for Intracytoplasmic Sperm Injection (ICSI) Fertil Steril. 2005;84(S16-7) doi: 10.1016/j.fertnstert.2005.07.039. [DOI] [Google Scholar]
- Worrilow KC, Huynh HT, Bower JB, Peters AJ, Johnston JB. The clinical impact associated with the use of PICSITM-derived embryos. Fertil Steril. 2006;86(S62) doi: 10.1016/j.fertnstert.2006.07.473. [DOI] [Google Scholar]
- Worrilow KC, Huynh HT, Bower JB, Anderson AR, Schillings W, Crain JL. PICSITM vs. ICSI: Statistically significant improvement in clinical outcomes in 240 in vitro fertilization (IVF) patients. Fertil Steril. 2007;88(S37) doi: 10.1016/j.fertnstert.2007.07.133. [DOI] [Google Scholar]
- Worrilow KC, Eid S, Matthews JM, Pelts EJ, Khoury C, Liebermann J. A multi-site clinical trial evaluating PICSI(r) versus Intracytoplasmic sperm injection (ICSI): positive clinical outcomes observed in a prospective, randomized and double-blinded study. Fertil Steril. 2009;92(S36-7) doi: 10.1016/j.fertnstert.2009.07.141. [DOI] [Google Scholar]
- Worrilow KC, Eid S, Matthews J, Pelts E, Khoury C, Liebermann J. Multi-site clinical trial evaluating PICSI, a method for selection of hyaluronan bound sperm (HBS) for use in ICSI: improved clinical outcomes. Hum Reprod. 2010;25:i7. doi: 10.1093/humrep/de.25.s1.4. [DOI] [Google Scholar]
- Worrilow KC, Eid S, Woodhouse D, Witmyer J, Khoury C, Liebermann J. Increased clinical pregnancy rates (CPR) and statistically significant decrease in loss rates using hyaluronan in sperm selection: prospective, multicenter, double-blind, randomized clinical trial. Fertil Steril. 2011;96(S179) doi: 10.1016/j.fertnstert.2011.07.696. [DOI] [Google Scholar]
- Worrilow KC, Eid S, Woodhouse D, Matthews J, Khoury CD, Witmyer J. Prospective, multi-center, double-blind, randomized clinical trial evaluating the use of hyaluronan bound sperm (HBS) in ICSI: statistically significant improvement in clinical outcomes. Fertil Steril. 2011;96(S58) doi: 10.1093/humrep/des417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worrilow KC, Eid S, Woodhouse D, Perloe M, Smith S, Witmyer J, Ivani K, Khoury C, Ball GD, Elliot T, Lieberman J. Use of hyaluronan in the selection of sperm for intracytoplasmic sperm injection (ICSI): significant improvement in clinical outcomes--multicenter, double-blinded and randomized controlled trial. Hum Reprod. 2013;28:306–314. doi: 10.1093/humrep/des417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Z, Hu H, Song M, Shen Y, Guo X, McElreavey K, Bittles AH, Wang W. Semen quality analysis of military personnel from six geographical areas of the People's Republic of China. Fertil Steril. 2011;95:2018–2023. doi: 10.1016/j.fertnstert.2011.02.052. [DOI] [PubMed] [Google Scholar]