Abstract
Background
Task-sharing with teachers to promote youth mental health is a promising but underdeveloped strategy in improving care access in low-income countries.
Aims
To assess feasibility, acceptability, and utility of the teacher accompaniment phase of a school-based teacher accompagnateur pilot study (TAPS) in Haiti.
Methods
We assigned student participants, ages 18–22 (n=120) to a teacher participant (n=22) within four Haitian schools; we instructed participants to arrange meetings with their assigned counterparts to discuss mental health treatment, academic skills, and/or well-being. We measured student and teacher perceived feasibility, acceptability, and utility of meetings with self-report Likert-style questions. We examined overall program feasibility by the percentage of students with a documented meeting, acceptability by a composite measure of student satisfaction, and utility by the percentage with identified mental health need who discussed treatment with a teacher.
Results
Favorable ratings support feasibility, acceptability, and utility of teacher-accompagnateur meetings with students. The majority of students (54%) met with a teacher. Among students with an identified mental disorder, 43.2% discussed treatment during a meeting.
Conclusions
This accompaniment approach to mental health task-sharing with teachers provided a school-based opportunity for students with mental health need to discuss treatment and has potential relevance to other low-income settings.
Introduction
Mental and substance use disorders were the leading contributor to years lived with disability (YLDs) among all health conditions globally in 2015 (Institute for Health Metrics and Evaluation [IHME], 2016). Likewise, they led contributions to YLDs in both low-income and lower middle-income countries (LMICs) (IHME, 2016), where the majority of individuals with severe mental disorders receive no treatment for these conditions (Demyttenaere et al., 2004; Wang et al., 2007). Given the critical shortage of clinicians who can deliver treatment for mental disorders in LMICs (Kakuma et al., 2011), the scientific literature has focused on strategies that leverage scarce specialized human resources through collaborative care and task-sharing. Task-sharing refers to the reassignment of specific healthcare related tasks from a health professional with a higher level of training or specialization to another health professional or layperson with less biomedical expertise (Eaton et al., 2011; Patel et al., 2013; WHO et al., 2007). In addition to augmenting local capacities for treatment delivery, task-sharing can promote treatment utilization through community-based outreach, health surveillance, education, and other practical support.
The substantial global mental health treatment gap disproportionately affects youth (Kieling et al., 2011; Patel et al., 2008). Moreover, several barriers to accessing care, such as cost, ease of communication with healthcare providers, and anticipated care effectiveness that particularly impact youth may be exacerbated for those living in LMICs (Ambresin et al., 2013; Blum et al., 2012; Patel et al., 2013; Patton et al,. 2016). Early detection and treatment of mental disorders are critical since adolescent mental disorders are strongly associated with adult mental health (Kessler et al., 2005; Patton et al., 2014), risk for other non-communicable diseases (Ngo et al., 2013), and negative future social and economic outcomes (Naicker et al., 2013). Among promising strategies to facilitate youth care access in LMICs is development of school-based platforms to provide guidance and support that facilitate help-seeking (Patton et al., 2016) and service delivery (Mnookin, 2016). School-based health promotion has had demonstrated success for health education, screening, and other interventions for a variety of health conditions (Langford et al., 2014), including mental disorders. Indeed, school-based mental health promotion, prevention, and surveillance programs have been shown effective across diverse contexts; however, the majority of studies come from high-income settings (Barry et al., 2013; Fazel et al., 2014a, 2014b; Patel et al. 2013). Moreover, despite evidence of effectiveness of task-sharing with community health workers (CHWs) for mental health promotion in LMICs (Baingana et al., 2015), fewer data address a broad scope of application for mental-health task-sharing with teachers. Additionally, relatively few data are available evaluating the feasibility and acceptability of mental health task-sharing in LMICs (Padmanathan & De Silva, 2013). This lacune is particularly salient to the sustainability of teacher-led interventions, given concerns that teachers are already overburdened in low-resource settings (Fazel et al, 2014b; Rajaraman et al, 2012).
In this paper, we examine a novel school-based approach to task sharing with teachers to promote youth mental health in Haiti; this accompaniment approach draws from a successful model deploying CHWs as health accompagnateurs to promote treatment adherence for AIDS and TB in rural Haiti (Walton et al., 2004). Accompaniment expands the scope of support beyond a narrow focus on treatment—for example, by providing psychosocial support and facilitating linkage to clinical resources—in order to mitigate social structural impediments to adherence. This approach has been adapted for patients who had experienced treatment failure for drug resistant HIV in Boston (Behforouz, Farmer & Mukherjee, 2004), for multi-drug resistant tuberculosis in urban Peru (Shin et al., 2004), and to improve adherence to tuberculosis therapy following treatment default in Tomsk (Gelmanova et al., 2011). In addition to evidence of the transferability of the accompaniment dimension of community-based patient care across diverse social contexts, it has also been adapted for task-sharing with different levels of healthcare providers. Although the accompaniment role was extended to nurses in the latter program, it has not been adapted for teachers.
After a major earthquake in Haiti in 2010 resulted in mass casualties and infrastructural damage, new efforts to improve mental health were undertaken by Haiti’s Ministry of Health and a number of NGOs (Raviola et al., 2013). The NGO Zanmi Lasante— which has been providing healthcare in Haiti’s Central Plateau for over 25 years— was especially well-positioned to launch a comprehensive plan to improve access to mental health care in the communities it serves (Raviola et al., 2012, 2013). This plan included training and deploying CHWs as accompagnateurs to facilitate community-based access to newly expanded mental health services. This accompaniment approach—already culturally familiar given that it had first been developed to serve a rural Haitian community—also had strategic appeal to help Haitian youth navigate mental health support and services by investing teachers with relevant knowledge, skills, informational resources, and a liaison with clinical services to make them “adolescent friendly” (WHO, 2012). As respected and accessible members of the community, teachers are situated to understand social and academic challenges their students face and offer informed guidance.
In this paper, we describe formative research examining the initial iteration of a school-based teacher-accompagnateur program in Haiti’s Central Plateau. Specifically, the Teacher-Accompagnateur Pilot Study (TAPS; Eustache et al., 2014) intervention comprised three sequential phases: (1) mental health training for teacher participants (Eustache et al, 2017a), (2) school-based mental health screening of study participants (Eustache et al, 2017b), and (3) facilitating 1:1 brief teacher-student meetings to support treatment navigation and/or strategies to promote academic success or well-being. Aims of the present study—focused on the latter phase—were to assess feasibility and acceptability of promoting youth mental health via the platform of school-based teacher accompaniment. We also examined potential utility of this teacher-accompagnateur model of task-sharing to address the considerable mental health needs of student participants (see Eustache et al, 2017b) by facilitating user access to information and practical support concerning mental health care.
Method
We used a prospective design to examine the feasibility, acceptability, and utility of a school-based mental health intervention delivered in 2013. We focus here on the teacher accompaniment phase. Written informed consent was obtained for each study participant. The study was approved by both the Institutional Review Board of the Harvard Faculty of Medicine and the Zanmi Lasante Ethics Committee.
Study sample
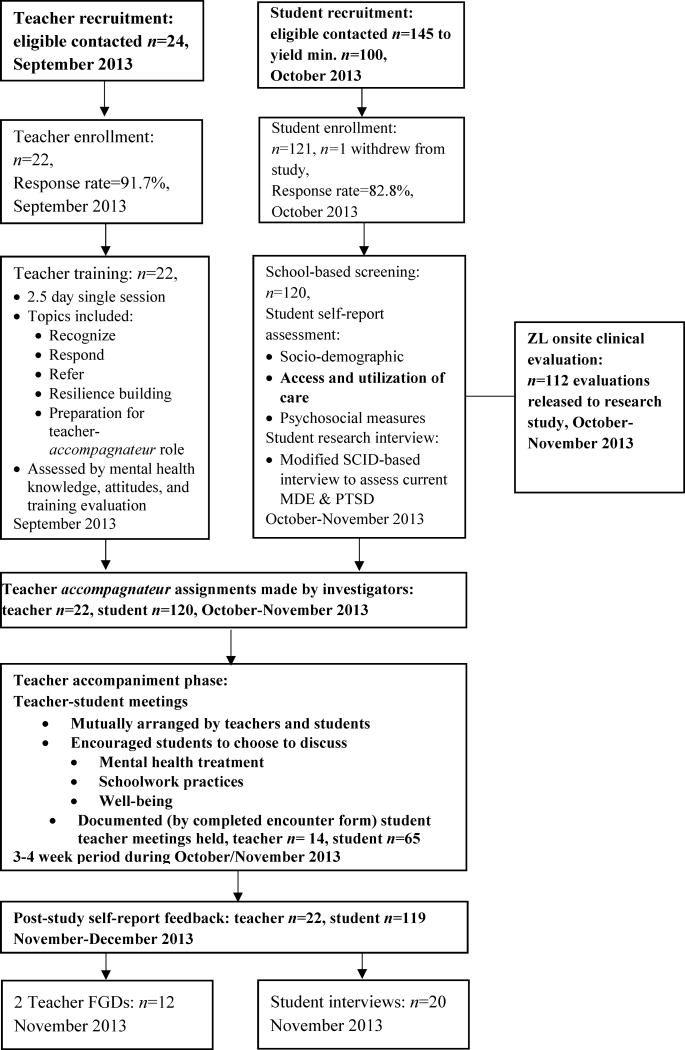
Four secondary schools were invited—and agreed—to participate in this pilot study. Selection was both purposive (based on their proximal location to two ZL clinics in Haiti’s Central Plateau and to allow maximal variety of school populations by encompassing both public and private schools) and by convenience. The study population included two groups of participants recruited from the four schools—teachers and students—each with a complementary role. Selection of teacher participants was purposive and based on nomination by principals of the participating schools where they were teaching (n=22). We identified eligible student study participants using school enrollment records and randomly selected young adult students (ages 18–22 years) within each of four participating schools, yielding a sample of 120 (Figure 1).
Figure 1.
Flow sheet summary of Teacher-Accompagnateur Pilot Study (TAPS) phases and procedures
Bold text indicates key procedure or data source for current investigation
Study procedures
We focus here on procedures most relevant to the accompaniment (intervention) phase of TAPS. Figure 1 summarizes the phases and procedures of the overarching study which included training for teacher study participants focused on recognizing, responding to, and referring students at risk for mental illness, as well as supporting resilience (Eustache et al, 2017a). This training, held just prior to the start of the academic year, also oriented teacher participants to study procedures and materials for structuring brief teacher-student meetings during the ensuing 3–4 week TAPS intervention phase. Baseline psychosocial assessment of student participants also preceded the accompaniment phase (see Eustache et al, 2017b).
School-based baseline psychosocial assessment of student participants
At the start of the 2013 academic year, student participants responded to a battery of self-report psychosocial assessments as well as sociodemographic and healthcare utilization questions. Next, we conducted a structured research interview based on content from the major depressive episode (MDE) and posttraumatic stress disorder (PTSD) modules of the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 2010). We focused on MDE and PTSD given evidence of their elevated risk following disasters (Goldmann & Galea, 2014) and that they may be prevalent in Haiti (Wagenaar et al., 2012; Cerda et al., 2013); hence they were particularly relevant to the school-based setting. Study diagnostic assignments of MDE, PTSD, and subthreshold variants showed good convergent validity with self-report measures of symptomatology associated with related constructs (Eustache et al, 2017b).
ZL clinical mental health assessment
Following the research assessments, participants were encouraged to undergo an onsite clinical mental health assessment intended to facilitate access to a local clinician independently of TAPS. Mental health clinicians (each with formal training in psychology, social work, or psychiatry and experience in diagnostic assessment and treatment of mental illness in the local Haitian context) performed these assessments using the standard ZL clinical mental health assessment form, where they noted their recommendations and referrals to a local ZL clinic, when appropriate. Although this clinical evaluation was not formally part of the study, participants were invited to release information from the ZL clinical mental health assessment to the study.
Teacher-student accompaniment
We assigned each student participant to a teacher participant counterpart within his or her respective school. Teachers also received a list of assigned students. We instructed participants to arrange to meet with their assigned counterparts at school at least once over the 3–4 weeks post screening to discuss mental health treatment, academic skills, and/or well-being. Teachers were provided with structured encounter forms to guide their discussion and document each meeting. Members of the research team were available to teacher participants to answer questions and facilitate clinical referrals; the study coordinator also made ad hoc phone calls and visits to teachers to offer additional support during this timeframe.
Study participant debriefing and additional feedback
After the accompaniment phase, teacher and student participants responded to self-report questionnaires with Likert-style questions regarding their experience of participation in and feedback about TAPS.
Study assessments
Self-report assessments were translated from English into Haitian Creole by a bilingual speaker, independently back translated, and adjusted in consultation with one or more members of the Haiti-based research team. Baseline psychosocial assessments developed or adapted for the study, including a diagnostic interview, are described in detail elsewhere (Eustache et al, 2017b).
ZL clinical assessment forms
We invited participants to authorize release of health information recorded on the standard ZL mental health assessment form (ZL, 2012) used for clinical care during their onsite clinical interview. We reviewed available forms (n=112) for clinician recommendations for follow-up, if any.
Teacher-student meeting encounter forms
For each meeting, teachers completed a one-page encounter form comprising a checklist of topics discussed with students. Suggested topics encompassed three general categories of skills and practices supporting 1) mental health treatment (e.g., understanding recommendations, making an appointment, adhering to recommendations or medication, finding transportation to an appointment); 2) effective schoolwork practices (e.g., time management skills, finding a good environment for homework); and 3) emotional well-being and resilience building (e.g., coping skills, sleep, nutrition, problem solving).
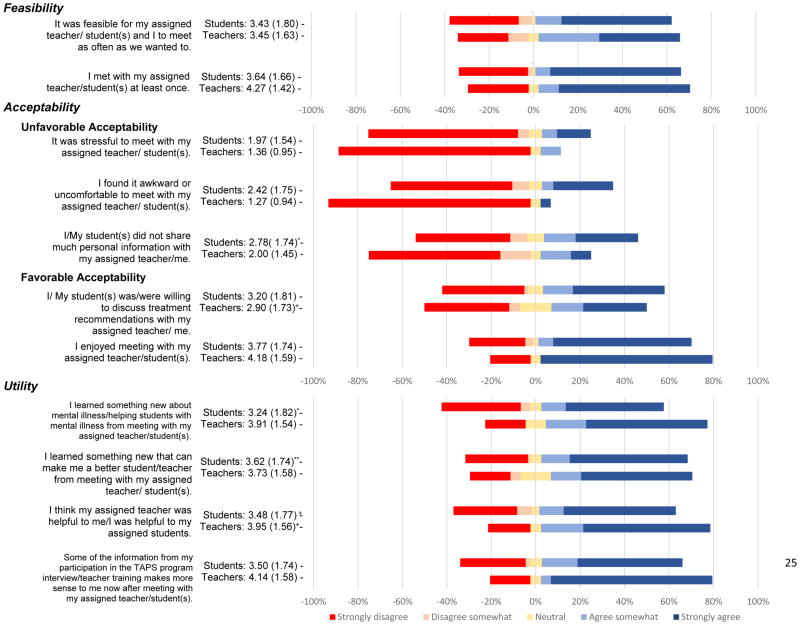
Student and teacher participant post-TAPS feedback
We developed self-report assessments using 5-point Likert-style questions about participation in TAPS. Among these, 11 items for students and 11 corresponding items for teachers assessed dimensions of feasibility, user acceptability, and perceived utility of TAPS based on experience with teacher-student meetings (see Figure 2). Three additional items addressed user satisfaction among student participants pertaining to the overall TAPS program (e.g., “I would participate in the TAPS program again”). Numeric values for these latter three items were averaged and combined into a single indicator of student user satisfaction with their overall experience of TAPS. Internal consistency reliability was measured by Cronbach’s α (α=.51).
Figure 2. Feasibility, acceptability, and utility of teacher-accompagnateur meetings perceived by student and teacher study participants.
*Indicates n=118, ** indicates n=117, + indicates n=21. For all other student responses n=119, and for all other teacher responses n=22.
Data management
Self-report response data were entered into Excel and verified. Written narrative data from the “General Impression” and “Plan/Disposition” sections of the ZL clinical assessment forms were translated into English and entered into an Excel spreadsheet; additional checked or encircled responses relating to recommendations for follow-up or support were entered into Excel and verified. Clinician recommendations were coded by consensus among three study investigators into three mutually exclusive categories where the ZL clinical assessment: 1) indicated mental health need and specified a recommended clinical intervention (e.g. medication, interpersonal psychotherapy, re-evaluation); 2) noted some mental health need and recommendation for psychosocial support (e.g. psychoeducation, relaxation, coping strategies); 3) did not indicate any need for mental health intervention. Finally, we examined and described additional clinician recommendations in non-mutually exclusive domains concerning other health and academic needs.
Statistical Analysis
Identification of student participants with mental health need
We operationalized “mental health need” in two ways as reflected either by a research interview based study diagnosis of a mental disorder or a clinical interview based identification of a broader psychosocial need. The former was recognized by a student’s meeting study criteria for a diagnosis of MDE, PTSD, or subthreshold MDE or PTSD during the SCID-based research interview assessment (n=44; Eustache et al, 2017b). The latter was recognized by a written ZL clinical assessment recommending either a specific clinical intervention or some kind of psychosocial support for an identified mental health need (i.e., comprising respondents in either the first or second categories described above). Although available evidence supports the validity of the MDE and PTSD diagnostic constructs measured by the SCID in Haiti (Bolton et al., 2012; Rahill et al., 2015; Rasmussen et al., 2015), the operationalization of mental health need identified by a clinical interview may have greater local contextual salience.
Quantitative assessment of feasibility, acceptability, and utility
We operationalized feasibility as evidence that TAPS procedures could be carried out by participants and acceptability of TAPS procedures as user satisfaction (cf. Padmanathan & De Silva, 2013). Our proxy measure for feasibility was the percentage of student participants who attended a teacher-student meeting as documented by a returned encounter form; for acceptability, our proxy was the mean score on a composite measure of student satisfaction with the TAPS program overall. Perceived feasibility and acceptability were also assessed through examination of the distribution and mean values of responses to 7 relevant items posed to both teacher and student participants following the teacher accompaniment phase of the study, regarding their experience of the teacher-student meetings (Figure 2).
We operationalized utility as evidence that the TAPS intervention—and teacher-accompagnateur meetings, in particular—provided information or help of potential value in promoting student mental health or well-being and assessed utility as follows. First, we examined perceived utility of the program by calculating mean values and distributions of responses to 4 relevant items posed to both teacher and student participants (Figure 2). Next, we calculated the percentage of student participants with mental health need—as operationalized in the two aforementioned ways—who met with a teacher-accompagnateur. Further, we examined the number of those students who also discussed treatment during a meeting to determine the number of participants with mental health need who accessed treatment-relevant support through teacher meetings.
In a post-hoc exploratory analysis, we also examined whether teacher-accompagnateur meetings may have provided potentially unique benefit to students beyond relocating or replicating services offered within the health sector. First, we used a multivariable regression to examine whether meeting with a teacher significantly predicted student satisfaction with TAPS independently of ZL clinical assessment identified mental health need. Second, we examined the percentage of students who had discussed treatment with a teacher-accompagnateur among the student participants with a mental health need who had not accessed any health or mental health services in the past year.
Results
Table 1 displays selected sample characteristics. Notably, student participants were two-thirds male. Teacher participants were also predominantly male. A majority of study participants met our study definition of having mental health need. Following their ZL clinical assessment, 53 and 32 students, respectively, warranted a recommendation that follow-up mental health care or psychosocial support could be helpful; thus, 70.8% of students (n=85) had an identified mental health need. In addition, we have previously reported that 36.7% of student participants were assigned a diagnosis of MDE, PTSD, or a subthreshold variant by research interview (Eustache et al, 2017b).
Table 1.
Sample Characteristics
| Student participants, n=120 unless otherwise indicated | |
|---|---|
| Measure | Mean (SD) or % (n) |
| Socio-demographic | |
| Age (in years) | 19.5 (1.37) |
| Gender (% female) | 33.3% (40) |
| Days of school attended per week, on average (n=118) | 4.7 (1.34) |
| Attends Public School | 50.0% (60) |
| Participation in TAPS | |
| Held documented meeting with teacher | 54.2 %(65) |
| Discussed mental health treatment issues with teacher | 40.8% (49) |
| Discussed effective schoolwork practices with teacher | 53.3% (64) |
| Discussed emotional well-being and resilience-building skills with teacher | 53.3% (64) |
| Identified mental health need | |
| SCID-based study diagnosis* | |
| MDE | 7.5% (9) |
| MDE subthreshold variant | 18.3% (22) |
| PTSD | 10.8% (13) |
| PTSD subthreshold variant | 10.0% (12) |
| MDE, PTSD, and/or subthreshold variant* | 36.7% (44) |
| No past year utilization of mental health or any health services | 15.8% (19) |
| No SCID-based study diagnosis* | 63.3% (76) |
| ZL clinical assessment-based mental health recommendations | |
| Clinical follow-up or support | 70.3% (85) |
| No utilization of mental health or any health services in past year | 31.7% (38) |
| No support or follow-up | 22.5% (27) |
| ZL clinical assessment unavailable | 6.7% (8) |
| Additional recommendations based on ZL clinical assessment | |
| Other kind of health follow-up | 15.8% (19) |
| Academic support | 5.0% (6) |
| Teacher involvement in mental health support | 8.3% (10) |
| Teacher participants (n=22) | |
| Measure | Mean (SD) or % (n) |
| Socio-demographic | |
| Age (in years) | 40.1 (7.16) |
| Gender (% female) | 18.2 (4) |
| Participation in TAPS | |
| Held documented meeting with student | 63.6 (14) |
SCID-based diagnoses and mental health and health services utilization reported previously in Eustache et al, 2017b.
Quantitative assessment of feasibility, acceptability, and utility
Feasibility of teachers meeting with students during the accompaniment phase was only moderate: 54.2% of students and 63.6% of teachers held documented meetings. However, student ratings demonstrated acceptability of the overall TAPS program, as reflected by high mean scores on our composite measure of user satisfaction (M=4.09, SD=1.01). In addition, student and teacher perceptions of both feasibility and acceptability of meetings were generally favorable (Figure 2). For example, the majority of teachers and students (77.3% and 68.9%, respectively) somewhat or strongly agreed that they enjoyed meeting and only a minority within each group somewhat or strongly agreed that they found meeting stressful (teachers: 9.1%, students: 21.9%) or awkward (teachers: 4.5%, students: 31.9%). That being said, nearly half of students indicated not having shared much personal information in a meeting, whereas teachers perceived them to be more forthcoming. Finally, students and teachers each reported moderate to strong agreement with statements concerning several dimensions of program utility (Figure 2).
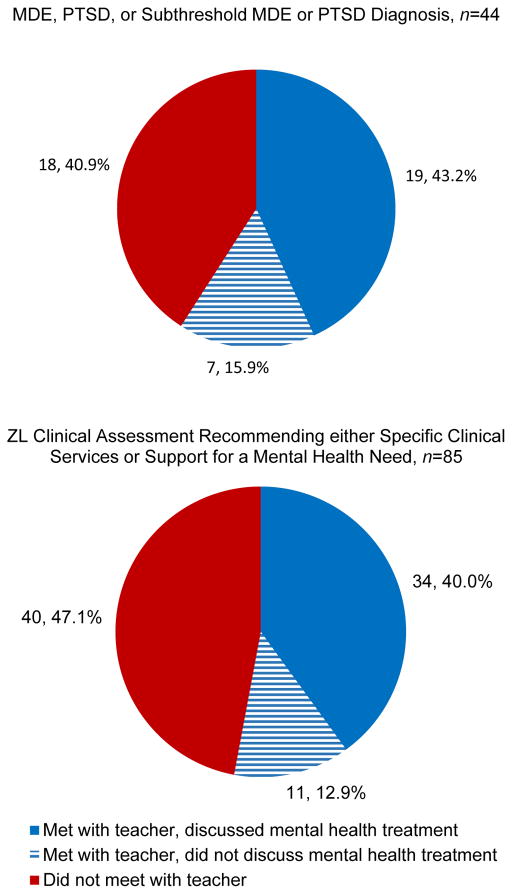
Over half of student participants with identified mental health need met with a teacher-accompagnateur, supporting that a school-based meeting with a teacher may be an effective strategy to reach youth who would benefit from mental health care or psychosocial support. In particular, 59.1% of students with a diagnosis of MDE, PTSD, or subthreshold variant met with a teacher and 43.2% discussed treatment adherence in their meeting. Moreover, 52.9% of students whose ZL clinical assessment-identified mental health need met with a teacher and 40.0% discussed treatment-related issues during a meeting (Figure 3).
Figure 3.
Percentage of students with identified mental health need (as operationalized in two ways) who met with a teacher-accompagnateur and who discussed treatment during a meeting
Student participation in teacher-student meetings was significantly associated with higher student user satisfaction ratings with TAPS (B=.70, 95% CI=.34,1.07, p<.001) in a multivariable linear regression, when controlling for a ZL clinical assessment-identified mental health need, general healthcare utilization in the past year, mental healthcare utilization in the past year, school type, school attendance, age, and gender.
Among the student participants with a diagnosis of MDE, PTSD, or a subthreshold variant who had not accessed any mental or general health services in the past year (n=19), a majority (52.6%; n=10) met with a teacher-accompagnateur and discussed a dimension of understanding, navigating, or adhering to treatment. Likewise, student participants with ZL clinical assessment-identified mental health need who had not utilized any health services (n=38), 34.2% (n=13) discussed treatment during a meeting. In other words, meetings with teacher-accompagnateurs provided an entrée to a conversation about mental health treatment for approximately one-third of student participants with mental health need who had not accessed care.
Discussion
Study findings support that a teacher-accompagnateur program has conceptual appeal and potential utility in Haiti’s Central Plateau to both teachers and students as a school-based platform for providing information and support to students that can help them navigate local mental health services. First, a majority of students were able to meet with a teacher-accompagnateur during the intervention period. Second, student and teacher responses both reflect favorable ratings of the feasibility, acceptability, and utility of the program. Notwithstanding the absence of a culture of mental health treatment seeking in Haiti prior to availability of services (WHO, 2010), findings support that students were generally willing to discuss mental health treatment with teachers. We considered the possibility that students’ perception of the program’s utility might have resulted from access to an onsite clinician at their school rather than the opportunity to meet with a teacher-accompagnateur. However, our finding that meeting with a teacher-accompagnateur predicted student satisfaction with TAPS supports that teacher accompaniment was valuable to students independent of input from an onsite mental health clinician.
We have previously reported that the burden of mental illness was considerable in this study population of school-going transitional age youth. We have also previously reported that an unacceptably high percentage of study participants with full-syndrome or subthreshold diagnosis of MDE or PTSD had not accessed mental health care and, indeed, many had not accessed any care in the health sector over the previous year (Eustache et al, 2017b). This study’s findings indicate that the TAPS program may have provided a channel for discussion of treatment for a substantial proportion (43.2%) of students who received a study diagnosis. Further, among those with a diagnosis who had not previously accessed care, over half availed themselves of an opportunity to discuss mental health treatment with a teacher-accompagnateur.
Likewise, we found the TAPS program provided a resource for the discussion of treatment with a teacher-accompagnateur for a similar proportion (40.0%) of participants with ZL clinical assessment-identified mental health need. Additionally, among the latter participants who had not utilized care over the past year, approximately a third (34.2%) discussed mental health treatment with a teacher-accompagnateur.
It is noteworthy both that a large proportion of student participants were identified as having mental health need by the ZL clinical assessment, and also that the recommended follow-up for them comprised a broad spectrum of possibilities that included interventions that could conceivably be offered in a school-based setting (e.g., psychoeducation, relaxation training, social support) rather than necessarily in a mental health clinic. Haiti’s youth face extraordinary psychosocial stressors relating to widespread poverty, a series of natural disasters, a cholera epidemic, as well as experiencing or witnessing violence. Thus, study findings suggest that teacher accompaniment could potentially provide monitoring and early intervention to help resolve social stressors and mitigate psychosocial distress, beyond facilitating access to clinical services by providing relevant information and practical assistance.
Limitations
There are several limitations of this study. First, access to ZL health services may have contributed to greater willingness to engage in discussions about mental health with teachers. Moreover, generalizability to younger adolescents is limited as the student sample consisted exclusively of youth 18–22 years old. Additionally, teacher participants, selected by nomination by their principal, may not be representative of other secondary school teachers in Haiti. Next, because we did not directly observe the teacher-student meetings, we could not assess the quality and extent of discussion about treatment. Additionally, potential social desirability bias may have overestimated the degree of student satisfaction with the TAPS program and our proxy for user satisfaction may have been limited by its poor internal consistency reliability. Nevertheless, findings provide evidence that at least some respondents with mental health need gained access to information and guidance—possibly for the first time—via a trained teacher-accompagnateur in their school-setting. Finally, although a majority of student participants managed to meet with a teacher, a substantial portion of the sample did not have a meeting. Given evidence of the value of teacher-student meetings to students, developing mechanisms to increase student and teacher participation in the meetings could enhance the program’s utility.
Conclusion
The teacher accompaniment model has potential utility to respond, in part, to the urgent mental health needs of youth in LMICs and aligns with the global priority of improving their access to quality care, as articulated by the Grand Challenges in Global Mental Health initiative (Collins et al., 2011). In contrast to much of the existing literature on mental health task-sharing with teachers in LMICs focused on whether teachers can lead interventions as well as specialists (Fazel et al., 2014b), this formative research develops the role of teachers as accompagnateurs who can understand their students’ complex psychosocial needs and also provide a bridge from the school setting to clinical care. Specifically, findings suggest that task-sharing with teachers as accompagnateurs may open or enhance the channels of communication and navigation for youth in accessing mental health services. Strategies that tap teachers’ experience and expertise to faciliate youth access to mental healthcare hold promise and are relatively underutilized. Teachers’ professional orientation towards youth well-being, and longitudinal perspective on changes in pupils’ behavior uniquely situate them to promote youth mental health. Further research will be beneficial to understanding how this role could also concomitantly address psychosocial needs to pre-empt the necessity of clinical intervention, improve student academics, and make a positive shift in school climate (Durlak et al., 2011), and decrease stigma (Behforouz et al., 2004).
Acknowledgments
We are grateful to the leadership of Zanmi Lasante as well as at the four schools who so generously accommodated the planning and implementation of the mental health training and its accompanying school-based pilot study. We thank Shin Daimyo, Georges Alexis, Elysee Noesil, Ernst Origene, Handy Petit-Homme, and other colleagues at Partners In Health and Zanmi Lasante as well as Claire Pernar and Megan Benson Stack at Harvard Medical School for their support of the planning, management, and implementation of the study and trainings. We thank Marie-Christine Ouellet Ph.D. and her team, École de psychologie, Université Laval, Québec, Canada for providing the French translation of the SCID. We express here our profound gratitude to the student and teacher study participants for their time and generous feedback, and from whom we learned so much.
Funding
Research reported in this publication was supported by National Institute of Mental Health of the National Institutes of Health under award number R21MH093298 (Co-PIs, Becker and Eustache). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. Journal of Adolescent Health. 2013;52(6):670–681. doi: 10.1016/j.jadohealth.2012.12.014. [DOI] [PubMed] [Google Scholar]
- Baingana F, Al’Absi M, Becker AE, Pringle B. Global research challenges and opportunities for mental health and substance-use disorders. Nature. 2015;527(7578):S172–S177. doi: 10.1038/nature16032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry MM, Clarke AM, Jenkins R, Patel V. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC public health. 2013;13(1):835. doi: 10.1186/1471-2458-13-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behforouz HL, Farmer PE, Mukherjee JS. From directly observed therapy to accompagnateurs: enhancing AIDS treatment outcomes in Haiti and in Boston. Clinical Infectious Diseases. 2004;38(Supplement 5):S429–S436. doi: 10.1086/421408. [DOI] [PubMed] [Google Scholar]
- Blum RW, Bastos FI, Kabiru CW, Le LC. Adolescent health in the 21st century. The Lancet. 2012;379(9826):1567. doi: 10.1016/S0140-6736(12)60407-3. [DOI] [PubMed] [Google Scholar]
- Bolton P, Surkan PJ, Gray AE, Desmousseaux M. The mental health and psychosocial effects of organized violence: A qualitative study in northern Haiti. Transcultural psychiatry. 2012;49(3–4):590–612. doi: 10.1177/1363461511433945. [DOI] [PubMed] [Google Scholar]
- Cerdá M, Paczkowski M, Galea S, Nemethy K, Péan C, Desvarieux M. Psychopathology in the aftermath of the Haiti earthquake: A population-based study of posttraumatic stress disorder and major depression. Depression and anxiety. 2013;30(5):413–424. doi: 10.1002/da.22007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, … Glass RI. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J, … Polidori G. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child development. 2011;82(1):405–432. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- Eaton J, McCay L, Semrau M, Chatterjee S, Baingana F, Araya R, … Saxena S. Scale up of services for mental health in low-income and middle-income countries. The Lancet. 2011;378(9802):1592–1603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- Eustache E, Becker AE, Wozo Ekip. Developing Research Capacity for Mental Health Interventions for Youth in Haiti. Frontiers in Neuroscience for Global Health/Tenth Anniversary of Brain Disorders in the Developing World: Research across the Lifespan 2014 [Google Scholar]
- Eustache E, Gerbasi ME, Fawzi MS, Fils-Aimé JR, Severe J, Raviola GJ, … Becker AE. Mental health training for secondary school teachers in Haiti: a mixed methods, prospective, formative research study of feasibility, acceptability, and effectiveness in knowledge acquisition. Global Mental Health. 2017a;4 doi: 10.1017/gmh.2016.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eustache E, Gerbasi ME, Smith Fawzi MC, Fils-Aimé JR, Severe J, Raviola GJ, … Becker AE. High burden of mental illness and low utilization of care among school-going youth in Central Haiti: A window into the youth mental health treatment gap in a low-income country. International Journal of Social Psychiatry. 2017b May;63(3):261–74. doi: 10.1177/0020764017700174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools in high-income countries. The Lancet Psychiatry. 2014a;1(5):377–387-8. doi: 10.1016/S2215-0366(14)70312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel M, Patel V, Thomas S, Tol W. Mental health interventions in schools in low-income and middle-income countries. The Lancet Psychiatry. 2014b;1(5):388–398. doi: 10.1016/S2215-0366(14)70357-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer R, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP, January 2010 Revision) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2010. [Google Scholar]
- Gelmanova IY, Taran DV, Mishustin SP, Golubkov AA, Solovyova AV, Keshavjee S. ‘Sputnik’: a programmatic approach to improve tuberculosis treatment adherence and outcome among defaulters. The International Journal of Tuberculosis and Lung Disease. 2011;15(10):1373–1379. doi: 10.5588/ijtld.10.0531. [DOI] [PubMed] [Google Scholar]
- Goldmann E, Galea S. Mental health consequences of disasters. Annual review of public health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME) GBD Compare. Seattle, WA: IHME, University of Washington; 2016. Retrieved from: http://vizhub.healthdata.org/gbd-compare. [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, … Scheffler RM. Human resources for mental health care: current situation and strategies for action. The Lancet. 2011;378(9803):1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, … Rahman A. Child and adolescent mental health worldwide: evidence for action. The Lancet. 2011;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Langford R, Bonell CP, Jones HE, et al. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database of Systematic Reviews. 2014:4. doi: 10.1002/14651858.CD008958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mnookin S. Out of the shadows: making mental health a global development priority report. Geneva: World Bank Group and World Health Organization; 2016. [Google Scholar]
- Naicker K, Galambos NL, Zeng Y, Senthilselvan A, Colman I. Social, demographic, and health outcomes in the 10 years following adolescent depression. Journal of Adolescent Health. 2013;52(5):533–538. doi: 10.1016/j.jadohealth.2012.12.016. [DOI] [PubMed] [Google Scholar]
- Ngo VK, Rubinstein A, Ganju V, Kanellis P, Loza N, Rabadan-Diehl C, Daar AS. Grand challenges: integrating mental health care into the non-communicable disease agenda. PLoS Med. 2013;10(5):e1001443. doi: 10.1371/journal.pmed.1001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Social science & medicine. 2013;97:82–86. doi: 10.1016/j.socscimed.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology and Psychiatry. 2008;49(3):313–334. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Patel V, Kieling C, Maulik PK, Divan G. Improving access to care for children with mental disorders: a global perspective. Archives of disease in childhood. 2013;98(5):323–327. doi: 10.1136/archdischild-2012-302079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, … Moran P. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. The Lancet. 2014;383(9926):1404–1411. doi: 10.1016/S0140-6736(13)62116-9. [DOI] [PubMed] [Google Scholar]
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, … Kakuma R. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahill GJ, Joshi M, Lescano C, Holbert D. Symptoms of PTSD in a sample of female victims of sexual violence in post-earthquake Haiti. Journal of Affective disorders. 2015;173:232–238. doi: 10.1016/j.jad.2014.10.067. [DOI] [PubMed] [Google Scholar]
- Rajaraman D, Travasso S, Chatterjee A, Bhat B, Andrew G, Parab S, Patel V. The acceptability, feasibility and impact of a lay health counsellor delivered health promoting schools programme in India: a case study evaluation. BMC health services research. 2012;12(1):127. doi: 10.1186/1472-6963-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen A, Eustache E, Raviola G, Kaiser B, Grelotti DJ, Belkin GS. Development and validation of a Haitian Creole screening instrument for depression. Transcultural psychiatry. 2015;52(1):33–57. doi: 10.1177/1363461514543546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raviola G, Eustache E, Oswald C, Belkin GS. Mental health response in Haiti in the aftermath of the 2010 earthquake: a case study for building long-term solutions. Harvard review of psychiatry. 2012;20(1):68–77. doi: 10.3109/10673229.2012.652877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raviola G, Severe J, Therosme T, Oswald C, Belkin G, Eustache FE. The 2010 Haiti earthquake response. Psychiatric Clinics of North America. 2013;36(3):431–450. doi: 10.1016/j.psc.2013.05.006. [DOI] [PubMed] [Google Scholar]
- Shin S, Furin J, Bayona J, Mate K, Kim JY, Farmer P. Community-based treatment of multidrug-resistant tuberculosis in Lima, Peru: 7 years of experience. Social science & medicine. 2004;59(7):1529–1539. doi: 10.1016/j.socscimed.2004.01.027. [DOI] [PubMed] [Google Scholar]
- Wagenaar BH, Hagaman AK, Kaiser BN, McLean KE, Kohrt BA. Depression, suicidal ideation, and associated factors: a cross-sectional study in rural Haiti. BMC psychiatry. 2012;12(1):149. doi: 10.1186/1471-244X-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton DA, Farmer PE, Lambert W, Leandre F, Koenig SP, Mukherjee JS. Integrated HIV prevention and care strengthens primary health care: lessons from rural Haiti. Journal of public health policy. 2004;25(2):137–158. doi: 10.1057/palgrave.jphp.3190013. [DOI] [PubMed] [Google Scholar]
- Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, … Haro JM. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. The Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Culture and Mental Health in Haiti: A Literature Review. Geneva: WHO; 2010. Retrieved from: http://www.who.int/mental_health/emergencies/culture_mental_health_haiti_eng.pdf. [Google Scholar]
- World Health Organization. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. 2007 Retrieved from: http://apps.who.int/iris/bitstream/10665/43821/1/9789241596312_eng.pdf.
- World Health Organization. Making health services adolescent friendly: Developing national quality standards for adolescent friendly health services. 2012 Retrieved from: http://207.58.191.15:8180/xmlui/bitstream/handle/123456789/372/2013%20-%20Standars%20for%20adolescents%20Health%20Services%20%209789241503594_eng.pdf?sequence=1.
- Lasante Zanmi. Zanmi Lasante-Departement De Sante Mentale et Service Psychosocial Evaluation de Sante Mentale--Adulte. Mirebalais, Haiti: 2012. [Google Scholar]