Abstract
All-inside anterior cruciate ligament reconstruction passed through a series of modifications over the past 2 decades, maintaining 2 common factors: half tunnels in both the femur and tibia and introduction of the graft into the knee through an arthroscopic portal. One of the disadvantages noted with this technique is the excessive cost of the instrumentation needed to perform it and its economic impact on the health care system. We describe a modification of the original technique, both maintaining the cortical bone in an intact state and avoiding the retrograde drill aiming device.
For anterior cruciate ligament (ACL) reconstruction, we can use a variety of grafts and fixation techniques. Regardless of the technique, tunnel placement is based on knowledge of the ACL footprint, as well as arthroscopic evaluation of the ruptured ACL scar tissue, through a biological and anatomic approach.
Because of the advantage of using sockets instead of full bone tunnels, which preserves bone stock and probably results in less graft motion and synovial fluid leakage,1 some authors prefer the all-inside technique for ACL reconstruction. One of the graft constructs described for this technique is a 4-strand semitendinosus (4ST).
In 1997 Stähelin and Weiler2 published an all-inside technique in which the tibial socket was made inside out and the graft was fixed with interference screws at both ends. This technique never gained popularity, mostly because it was technically demanding and the graft was fixed at an incorrect flexion angle (both tibial and femoral fixation were performed at 100° of flexion).
We describe an easy and reproducible all-inside ACL reconstruction technique, with a 4ST graft construct and 2 adjustable cortical suspensory fixation devices, in which the femoral socket is made through a standard anteromedial (AM) portal and the tibial socket is made through an anterolateral (AL) portal for inside-out tunnel drilling using a flexible reamer. As a result, the retrograde drill aiming device is avoided and final fixation of the graft at the desired degree of flexion is allowed (Video 1).
Surgical Technique
Step 1: Portal Setup
We use 2 arthroscopic portals: 1 AM portal and 1 AL portal at the inferior pole of the patella.
Step 2: Graft Harvest
The semitendinosus (ST) graft is harvested with the knee flexed at 90°. A 3- to 4-cm vertical skin incision is made over the pes anserinus. When the sartorial fascia is exposed, a parallel incision is made above the hamstring. The ST is identified and detached from its adhesions. Keeping the knee flexed at 90° and the hip externally rotated, after releasing the ST distally, we use a closed tendon stripper.
Step 3: Graft Preparation
The graft is prepared on the GraftLink preparation table (Arthrex, Naples, FL) by quadrupling the ST and fashioning it into a double loop. An ACL TightRope RT (Arthrex) is placed at both ends. A No. 0 FiberWire locking whipstitch (Arthrex) is used to suture together both ends of the graft and close the loop. Two circumferential No. 0 FiberWire sutures incorporating all 4 tendon strands are placed at both ends of the graft, at 1 and 2 cm. These sutures create a coupled 4-strand construct. Normally, 20-25 mm of graft at each end is inserted into the sockets. Pre-tensioning of the graft at 85 N is performed for 15 minutes (Fig 1, Table 1).
Fig 1.
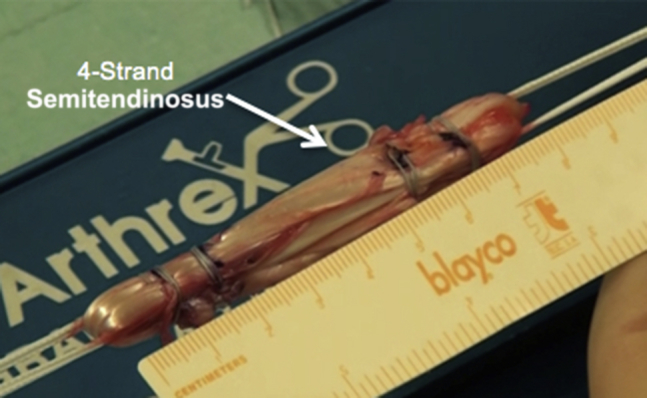
Graft preparation by quadrupling the semitendinosus and fashioning it into a double loop. Two circumferential sutures incorporating all 4 tendon strands are placed at both ends, at 1 and 2 cm.
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Setup | Tourniquet should not be used. An inflow saline solution pressure of 70-80 mm Hg can be used. Hemostasis should be carefully controlled carefully with a radiofrequency system. | The effect of tourniquet on the vessels and soft tissues remains unclear, as does its impact on increasing the risk of thrombosis and neuromuscular deterioration after ACL reconstruction. |
| Graft preparation | The end of the 4 strands should be moved to one extremity of the graft, incorporated between the first and second circumferential No. 0 FiberWire sutures, and inserted into the tibial socket. According to the length, calculations should be made to incorporate at least 10-15 mm and 15-20 mm of the graft inside the femoral and tibial socket, respectively. |
The risk of slippage or acute rupture of the graft is mostly generated by careless graft preparation. |
| Tibial socket creation | The surgeon should set the tibial drill guide aimer at 55° and drill from the anteromedial aspect of the proximal tibia, near the medial collateral ligament, to facilitate the exit of the nitinol wire through the AL portal. An extra margin of 5 mm should be given between the measure of the graft that will be placed inside the socket and the length of the socket. |
Increasing the inclination of the tibial tunnel will give a longer tunnel, which is useful to avoid the graft bottoming out. Insertion of the flexible reamer should be performed under direct visualization to avoid damaging the cartilage of the lateral condyle. |
ACL, anterior cruciate ligament; AL, anterolateral.
Step 4: Tibial Socket Creation
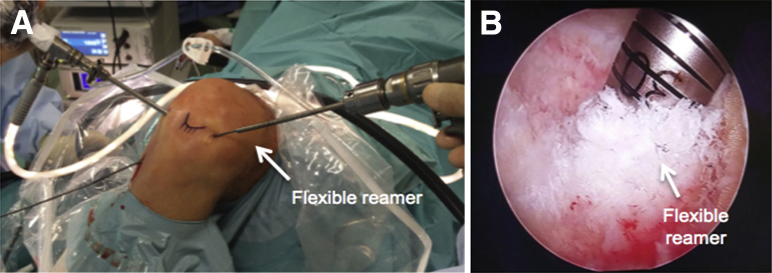
The tibial socket is made using a 55° tibial drill guide aimer (Acufex Director Drill Guide; Smith & Nephew, Andover, MA), inserted from the standard AM portal in the center of the ACL tibial footprint. A guide pin is then inserted from the AM aspect of the proximal tibia, followed by a 4.5-mm cannulated drill bit. Both the drill bit and guide pin are removed, and a nitinol wire is passed through the hole created in the tibial cortex and exits through the AL portal (Fig 2). In an inside-out fashion, a flexible reamer (Clancy Flexible Drill; Smith & Nephew) with the same diameter as the graft is used to create a socket measuring approximately 25 mm (Figs 3 and 4). A looped passing suture is then shuttled into the joint and docked on the AM portal for later use (Table 1).
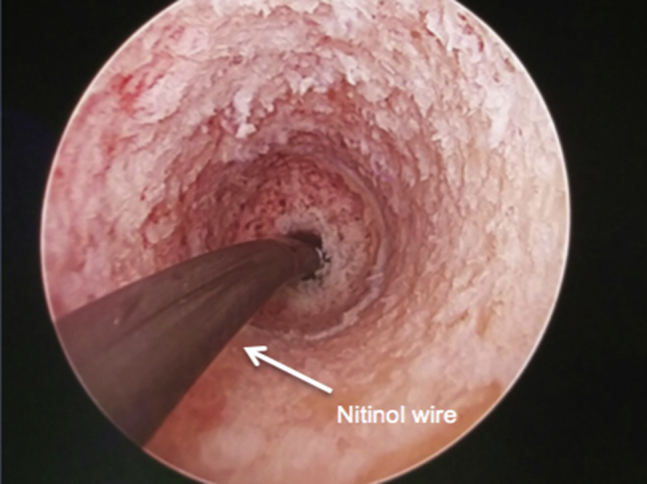
Fig 2.
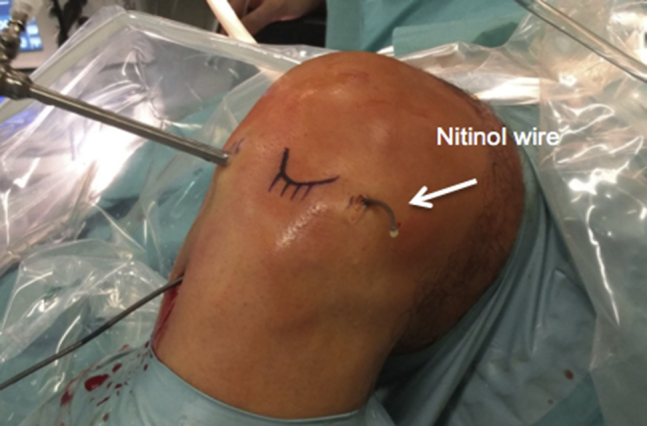
Left knee at 90° of flexion with an abduction post placed next to the thigh. A nitinol wire is exiting through the anterolateral portal.
Fig 3.
(A) Left knee at 90° of flexion with an abduction post placed next to the thigh. Inside-out drilling of the tibial socket is performed with a flexible reamer through the anterolateral portal. (B) Arthroscopic view of the flexible reamer inside the joint creating the tibial socket.
Fig 4.
Tibial socket arthroscopic view.
Step 5: Femoral Socket Creation
The ACL femoral footprint is identified, and a punch is used to mark the center, at 90° of knee flexion. Next, at 120°, a femoral guide pin (Transportal ACL Guide; Arthrex) is inserted through the AM portal and a calibrated spade-tip pin is used. A 4.5-mm cannulated drill bit is used through the guide pin and, finally, a low-profile reamer with the same diameter as the femoral end of the graft is used to create a socket measuring approximately 25 mm. A looped passing suture is then shuttled into the joint, retrieved through the AM portal, and docked. A rasp is used at this point to create an oval femoral drill hole that is more oval, increasing the graft insertion area.
Step 6: Graft Passage and Fixation
Once both passing sutures are retrieved and free of soft-tissue bridges, the femoral cortical suspensory fixation device is shuttled into the knee, using the femoral passing suture. The surgeon passes the graft into the femoral socket by pulling the fixation device until the desired measurement (approximately 2 cm). Special care should be taken at this point to not over-pull the button, creating soft-tissue interposition. Next, the tibial cortical suspensory fixation device is shuttled into the joint and exits through the tibial cortex, using the tibial passing suture. The fixation device is pulled to secure the button on the tibial cortex and to advance the graft into the tibial socket (±2 cm). With the knee placed at 0° of extension, final graft tensioning is performed on the femoral and tibial sides. Cycling of the knee is then performed approximately 25 times, and final tensioning is repeated. Graft tension is verified with a probe (Fig 5).
Fig 5.
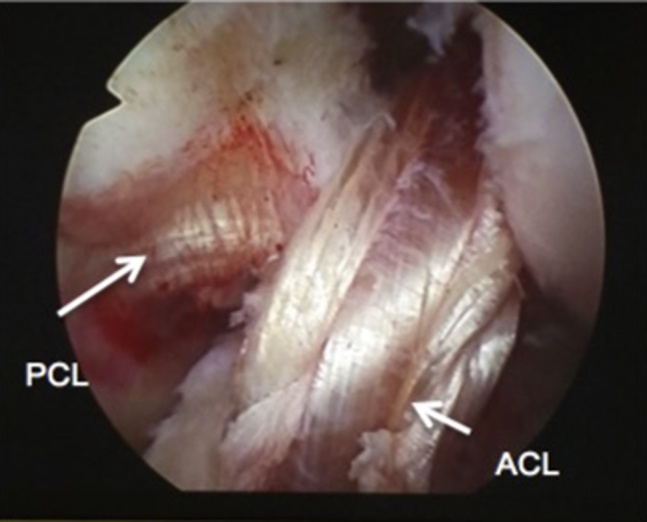
All-inside anterior cruciate ligament (ACL) reconstruction using 4-strand semitendinosus: left knee arthroscopic view. (PCL, posterior cruciate ligament.)
Discussion
The all-inside 4ST technique is one of the most popular techniques chosen for ACL reconstruction.3 It spares the gracilis (reducing the weakness of the hamstring muscles), preserves bone stock, and maintains the cortical bone in an intact state.
The greatest disadvantages noted for the all-inside technique are (1) the learning curve, because it is technically more challenging; (2) the potential risk of the graft “bottoming out,” resulting in inadequate tension; and (3) its high cost, because it requires a single-use retrograde drill aiming device for each tunnel. Our 4ST construct allows the possibility of saving the gracilis, which has been shown to have some impact on controlling the internal rotation and screw-home mechanism of the tibia, which will diminish the effect of dynamic instability under rotational loads of the knee, especially during some types of sports, when both the ST and gracilis are used for ACL grafting.4 With this graft construct, we always obtain a larger graft diameter (mean, 8.6 mm) than with the standard ST-gracilis graft, which according to Magnussen et al.5 is associated with a lower rate of revision (diameter >8 mm). A drawback of this 4ST construct is the length of the graft, which in some cases could be insufficient. On the other hand, we know from the literature that almost 80% of the population has a ST tendon length of 28 cm or more and that 10 to 15 mm and 15 to 20 mm of the graft length inside the femoral and tibial tunnels, respectively, are sufficient for graft healing,6 which means it is appropriate for the large majority of the cases. The adjustable-length loop button has the necessary biomechanical properties regarding ultimate failure strength, displacement, and stiffness for initial fixation in ACL reconstruction,7 avoiding the complications of the interference screws and allowing a 360° filling of the socket, which probably results in less graft motion and synovial fluid leakage into the socket.
There is a lack of consensus regarding pre-tensioning and preconditioning protocols in the literature.8 Some authors recommend graft pre-tensioning at 500 N, but it has been shown that high-load pre-tensioning results in alteration of the collagen fibrillar ultrastructure. On the other hand, recent literature has reported that the intra-articular graft tension was significantly lower than the applied tension from outside of the joint, even after cyclic loading and pre-tensioning, so the answer to this question remains unclear. For this reason, we follow the majority of studies (80%), which use at least 1 pre-tensioning or preconditioning protocol between 80 and 89 N.8
A limitation of the described technique is the impossibility of preserving the ACL tibial remnant, which we know contributes to its proprioception and vascularization, biomechanically protecting the graft.9 Therefore, when the ACL rupture leaves a large tibial remnant, to preserve it, we recommend alternative techniques as previously described (complete outside-in tibial tunnel).10
Our technique represents an important step forward because we can keep the philosophy of the all-inside ACL reconstruction and its main steps, and adapt it to any adjustable-length loop button and, at the same time, we can decrease the cost of surgery and instrumentation by avoiding the retrograde drill aiming device (Fig 6). The noted advantages have a direct economic impact on the all-inside ACL reconstruction technique, making it more accessible, while its simplicity and reproducibility are maintained.
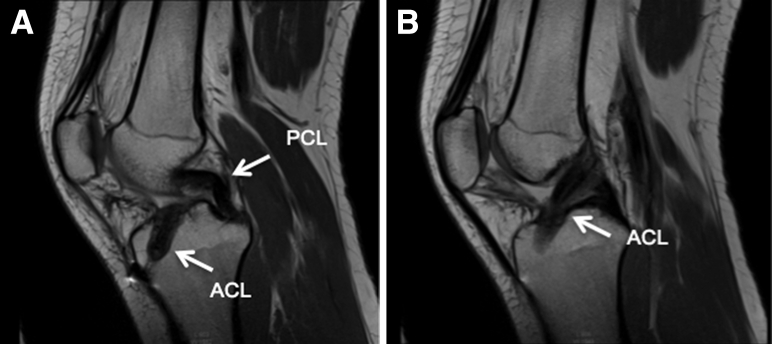
Fig 6.
(A, B) Sagittal views of anterior cruciate ligament (ACL) reconstruction on magnetic resonance imaging at 6 months postoperatively. (PCL, posterior cruciate ligament.)
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Inside-out tibial tunnel drilling technique, with flexible reamer, for all-inside anterior cruciate ligament reconstruction, using a 4-strand semitendinosus. Left knee.
References
- 1.Blackman A.J., Stuart M.J. All-inside anterior cruciate ligament reconstruction. J Knee Surg. 2014;27:347–352. doi: 10.1055/s-0034-1381960. [DOI] [PubMed] [Google Scholar]
- 2.Stähelin A.C., Weiler A. All-inside anterior cruciate ligament reconstruction using semitendinosus tendon and soft threaded biodegradable interference screw fixation. Arthroscopy. 1997;13:773–779. doi: 10.1016/s0749-8063(97)90019-0. [DOI] [PubMed] [Google Scholar]
- 3.Lubowitz J.H., Ahmad C.S., Amhad C.H., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Gobbi A., Domzalski M., Pascual J., Zanazzo M. Hamstring anterior cruciate ligament reconstruction: Is it necessary to sacrifice the gracilis? Arthroscopy. 2005;21:275–280. doi: 10.1016/j.arthro.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 5.Magnussen R.A., Lawrence J.T.R., West R.L., Toth A.P., Taylor D.C., Garrett W.E. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 6.Zantop T., Ferretti M., Bell K.M., Brucker P.U., Gilbertson L., Fu F.H. Effect of tunnel-graft length on the biomechanics of anterior cruciate ligament-reconstructed knees: Intra-articular study in a goat model. Am J Sports Med. 2008;36:2158–2166. doi: 10.1177/0363546508320572. [DOI] [PubMed] [Google Scholar]
- 7.Petre B.M., Smith S.D., Jansson K.S. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: A comparative biomechanical study. Am J Sports Med. 2013;41:416–422. doi: 10.1177/0363546512469875. [DOI] [PubMed] [Google Scholar]
- 8.Jisa K.A., Williams B.T., Jaglowski J.R., Turnbull T.L., LaPrade R.F., Wijdicks C.A. Lack of consensus regarding pretensioning and preconditioning protocols for soft tissue graft reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:2884–2891. doi: 10.1007/s00167-015-3530-y. [DOI] [PubMed] [Google Scholar]
- 9.Dallo I., Chahla J., Mitchell J.J., Pascual-Garrido C., Feagin J.A., LaPrade R.F. Biologic approaches for the treatment of partial tears of the anterior cruciate ligament. A current concepts review. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967116681724. 2325967116681724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silva A., Sampaio R. Quadruple semitendinosus graft construct and suspensory button fixation for anterior cruciate ligament reconstruction. Arthrosc Tech. 2015;4:e801–e806. doi: 10.1016/j.eats.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Inside-out tibial tunnel drilling technique, with flexible reamer, for all-inside anterior cruciate ligament reconstruction, using a 4-strand semitendinosus. Left knee.