Abstract
Transgender people experience a disproportionate burden of human immunodeficiency virus (HIV) and incarceration. Discrimination, victimization, poverty, and poor mental health drive vulnerability to HIV and related infections, as well as risk of arrest, detention, and incarceration. In this paper, we systematically review published data on HIV, sexually transmitted infections, viral hepatitis, and tuberculosis among incarcerated transgender people; describe potential structural determinants of HIV risk and transmission; identify gaps in the literature; and make recommendations for research and interventions to address this neglected population. We found that HIV and related infections among incarcerated transgender people have received little attention in the epidemiologic literature. The limited data available, which date from 1992, demonstrate high prevalence of HIV and sexually transmitted infections in this population internationally. Transgender people who had not had genital surgery were typically placed in jails and prisons corresponding to birth-assigned sex rather than gender identity. Once incarcerated, they routinely faced harassment, physical abuse, and sexual violence from inmates and staff and denial of access to medically necessary gender-affirming therapies. More HIV research with incarcerated transgender populations is urgently needed to inform correctional policy change that centers human rights and structural interventions, such as stigma reduction, pre-arrest diversion, and access to HIV prevention methods and gender-affirming care during incarceration.
Keywords: hepatitis, HIV, human rights, prison, sexually transmitted infections, stigma, transgender persons, tuberculosis
INTRODUCTION
Transgender people experience high rates of arrest and incarceration. The US Bureau of Justice Statistics reports that 870 of every 100,000 adult US residents (0.87%) were incarcerated in jails or under the jurisdiction of state or federal prisons during 2015, the most recent year for which data were available (1, 2). However, according to findings of the 2015 US Transgender Survey (USTS; n = 27,715), 1 in every 50 transgender respondents (2.0%) reported being incarcerated in the prior year—more than twice the rate of the general population (3). Black transgender women (9.0%) and transgender people who had been homeless in the prior year (7.0%) were more likely to report having been incarcerated.
According to findings of the US National Transgender Discrimination Survey (NTDS; n = 6,450), nearly 1 in 6 transgender adults (16.0%) reported having been incarcerated at some point in their lives (4). History of incarceration varied by race. Forty-seven percent of black respondents (n = 290) reported a history of incarceration, followed by 30% of American Indian (n = 75), 25% of Latino/Latina (25.0%; n = 294), 21% of multiracial (n = 736), and 13.0% of Asian (n = 137) respondents. Reisner et al. (5) found that 19.0% of the 3,878 transgender women in the NTDS data set had a history of incarceration and those who had been incarcerated were more likely to be people of color, have low income, and have low educational attainment compared with those who had not been incarcerated. These racial, economic, and class-based disparities mirror the disparities found in the general population and reflect the impact of intersectional disadvantage (i.e., multiple social categories such as race, gender, and socioeconomic status that intersect at the individual level and reflect interlocking systems of oppression (6)) on incarceration of transgender populations (7, 8). The USTS and NTDS are the largest surveys of transgender people available; however, authors of smaller studies conducted outside the United States have reported similar patterns in many places, including Serbia, Mongolia, Thailand, and Jamaica (9–12).
Structural stigma is a powerful driver of incarceration. Stigma is a social process of devaluing a group of people on the basis of an attribute labelled as negative; structural stigma refers specifically to processes that constrain access to resources, such as housing and employment (13, 14). Enacted stigma, also known as discrimination, has been associated with lack of access to gender-affirming medical care and with disproportionate rates of violence, poverty, homelessness, and participation in street economies (e.g., sex work and drug sales) (3–5, 15, 16). Forty-eight percent of USTS respondents (n = 27,715) reported being harassed in public in the prior year because of their gender identity (3). One-fourth of respondents who sought gender-affirming hormone therapy reported being denied this care and more than half of those who sought transition-related surgery in the past year were denied. Greater than 90.0% of NTDS participants (n = 6,450) reported experiencing discrimination at work, with 47.0% reporting being fired, not hired, or denied a promotion because they were transgender; the rate of unemployment among these participants was twice the national average (4). Nearly one-third (29.0%) of the USTS respondents (n = 27,715) were living in poverty, more than twice the rate in the US adult population (14.0%). Twenty percent had participated in sex work, drug sales, and other currently criminalized work at some point in their lives (3). Globally, many transgender women report being arrested on suspicion of sex work, simply for walking outside or possessing condoms (4, 17).
The same structural forces that drive incarceration have also been associated with human immunodeficiency virus (HIV) and related infections among incarcerated people (18, 19). Inmates around the world experience a high prevalence of infectious diseases, including HIV (20, 21), sexually transmitted infections (STIs) (22–26), viral hepatitis (20), and tuberculosis (TB) (20). Of the 10.2 million people incarcerated globally, it is estimated that 3.8% have HIV, 15.1% have hepatitis C, 4.8% have chronic hepatitis B, and 2.8% have active TB (20).
The estimated prevalence of HIV among nonincarcerated transgender people is higher than among the general population of incarcerated people (27, 28). A full review of HIV, STI, viral hepatitis, and TB among nonincarcerated transgender people is outside the scope of this manuscript; however, we briefly summarize the range of data here. In a global meta-analysis of HIV infection among 11,066 transgender women in 15 countries, Baral et al. (29) found a disturbing prevalence of 19.0%. HIV prevalence among transgender men has been reported as high as 8.0% in a small (n = 25), multicountry, internet-based, cross-sectional sample of transgender men who have sex with men (30). However, HIV research with transgender men is limited and often includes small sample sizes, making it difficult to generalize results (31).
Data on prevalence of STIs and viral hepatitis among transgender people vary greatly by study sample (e.g., clinical, community) and gender trajectory (e.g., masculine/male, feminine/female, gender nonbinary). Few studies have used probability sampling approaches that could offer externally valid prevalence estimates of STIs and viral hepatitis among transgender populations (30). In a retrospective review of electronic health records of transgender men and women at a clinic in Boston, Massachusetts (n = 145), researchers found the prevalence of STIs and viral hepatitis (i.e., herpes, syphilis, chlamydia, gonorrhea, and hepatitis C) to range between 2.0% and 3.0% (32). Little has been published on TB among transgender people beyond a case report by the US Centers for Disease Control and Prevention in 2000 that described an outbreak in a social network of transgender people in Baltimore, Maryland, and New York, New York (33).
The published literature on the health of incarcerated transgender people is even more limited (7, 34). Research on transgender people in prison has primarily appeared in the legal and policy literature, and focused on human rights issues such as access to gender-affirming medical therapies (e.g., hormone therapy, genital reconstruction surgeries), sex-segregated housing, and violent victimization by correctional staff and by other inmates.
International and constitutional laws have asserted that incarcerated people are entitled to a standard of health care equivalent to that available outside of prisons (35). The World Professional Association for Transgender Health’s most recent standards of care note that gender-affirming therapy is a medical necessity for transgender people with gender dysphoria (36), a severe and persistent discomfort with one’s assigned sex and/or physical sex characteristics (37). Untreated gender dysphoria can lead to significant mental health issues including suicidality; gender-affirming therapies are widely accepted as best practices for treating gender dysphoria (38).
In 2009, Brown et al. (39) synthesized policies on provision of gender-affirming care in state and federal prisons across the United States. They found wide variability in access to hormone therapy, including initiation or continuation of hormones, and uniform denial of surgical treatments (39). In 2015, Routh et al. (40) found that more states are providing statutory or policy guidelines for protection of transgender inmates from violence; however, there is a shortage of guidance on transgender medical issues. Specifically, 28 states do not allow transgender inmates to obtain gender-affirming care once incarcerated; 20 of these states do not allow for continuation of hormone therapy started before arrest. Only 7 states allow for gender-affirming surgery.
Globally, jails and prisons typically are segregated by sex, whereby inmates are housed together on the basis of their genital anatomy. Transgender people who have not had genital surgery are typically placed in jails and prisons corresponding to their birth-assigned sex rather than their gender identity. There, they routinely face harassment, physical abuse, and sexual violence from other inmates and staff (41–43). Alternatively, they may be placed in solitary confinement as a form of protective custody to prevent violence from other inmates or because prison systems are unsure where to house them (40). Solitary confinement is also a correctional tool that is widely used in prisons across the world to punish inmates who fail to adhere to carceral rules and regulations or who demonstrate violent or disruptive behavior (44, 45). The United Nations Committee Against Torture has explicitly described solitary confinement as cruel and inhumane, citing deleterious effects on incarcerated people’s mental and physical health, and has recommended that the practice be abolished (46).
Several correctional facilities in places as far apart as New York, New York; San Francisco, California; Thailand; and Turkey have initiated segregated housing specifically for sexual minority and/or transgender inmates (47–50). In such settings, transgender individuals placed in segregated housing as protective custody may maintain contact with a community of inmates. To our knowledge, data have not been published on the safety or health of inmates housed on the basis of sexual or gender minority status.
Among USTS respondents (n = 27,715) who had been incarcerated in the prior year, violent victimization was common: 23.0% reported physical assault and 20.0% reported sexual assault by staff or by other inmates (3). Victimization was often recurrent: 19.0% of those physically assaulted and 23.0% of those sexually assaulted by staff reported 8 or more occurrences. Similarly, 10.0% of transgender inmates who were physically assaulted and 23.0% of those who were sexually assaulted by other inmates reported 8 or more occurrences (3). According to a US Bureau of Justice Statistics report, in 225 state and federal prisons, 358 local jails, and 15 special correctional facilities in 2011–2012, transgender inmates were 5 times more likely to be sexually assaulted by facility staff than was the general population in jails and prisons, and greater than 9 times more likely to be sexually assaulted by other inmates (51, 52).Housing discrimination, high rates of violent victimization, and poor access to gender-affirming care affect transgender people within and outside carceral systems, and each of these factors has been linked to increased HIV vulnerability (30, 53, 54).
Given these overlapping drivers of incarceration and HIV among transgender people, as well as the known disparities in HIV, STIs, viral hepatitis, and TB among incarcerated people (compared with nonincarcerated people), it is important to understand the scope of these infectious diseases among incarcerated transgender people and the contexts in which they occur. Addressing the health of prisoners is a pressing public health and human rights concern (55). Recurrent arrest and imprisonment is common among incarcerated people, including those who are transgender (56). Movement between prison and the community creates opportunities for the acquisition and transmission of infectious diseases on either side of the prison wall and raises concerns for public health (55).
The human right to the highest attainable standard of health applies to everyone, including incarcerated people (57). A human rights approach to the health of incarcerated people requires prioritizing the needs of the most vulnerable inmates, including transgender people. A first step toward addressing those needs is to understand their scope. Therefore, the purpose of this systematic review is to synthesize published data on the epidemiology of HIV, STIs, viral hepatitis, and TB among incarcerated transgender people. To elucidate potential structural determinants of transmission and/or acquisition in carceral settings, we extracted data on transgender-specific human rights contexts (i.e., housing segregation, violent victimization, and access to gender-affirming therapy) of the carceral settings in which these infections were reported.
METHODS
Search strategy and inclusion criteria
We conducted a comprehensive search of 4 databases of peer-reviewed health literature: PubMed, CINAHL, PsycINFO, and SCOPUS. A Boolean search strategy was developed to identify citations at the intersection of 2 topical foci: 1) transgender populations AND 2) incarceration settings. Controlled vocabulary searches were run in each database to identify terms that describe common incarceration settings such as prisons, jails, penitentiaries, detention centers, and correctional centers. Equivalent key and text word and subject terms related to “incarceration settings” were developed and specified per database. Search terms for transgender studies were inclusive of transgender men (assigned female sex at birth) and transgender women (assigned male sex at birth). To ensure we did not miss data, we included older, less commonly used terms such as “transsexualism,” which was the primary PubMed medical subject heading term for “transgender” between 2001 and 2012 (it is now “transgender persons”), and “transvestism.” Although this review focused on HIV-related outcomes among incarcerated transgender people, we did not limit the search by adding terms about HIV. This allowed us to explore the research context within which HIV-related studies with this population were being conducted. The search included all studies published before March 24, 2017, in any language.
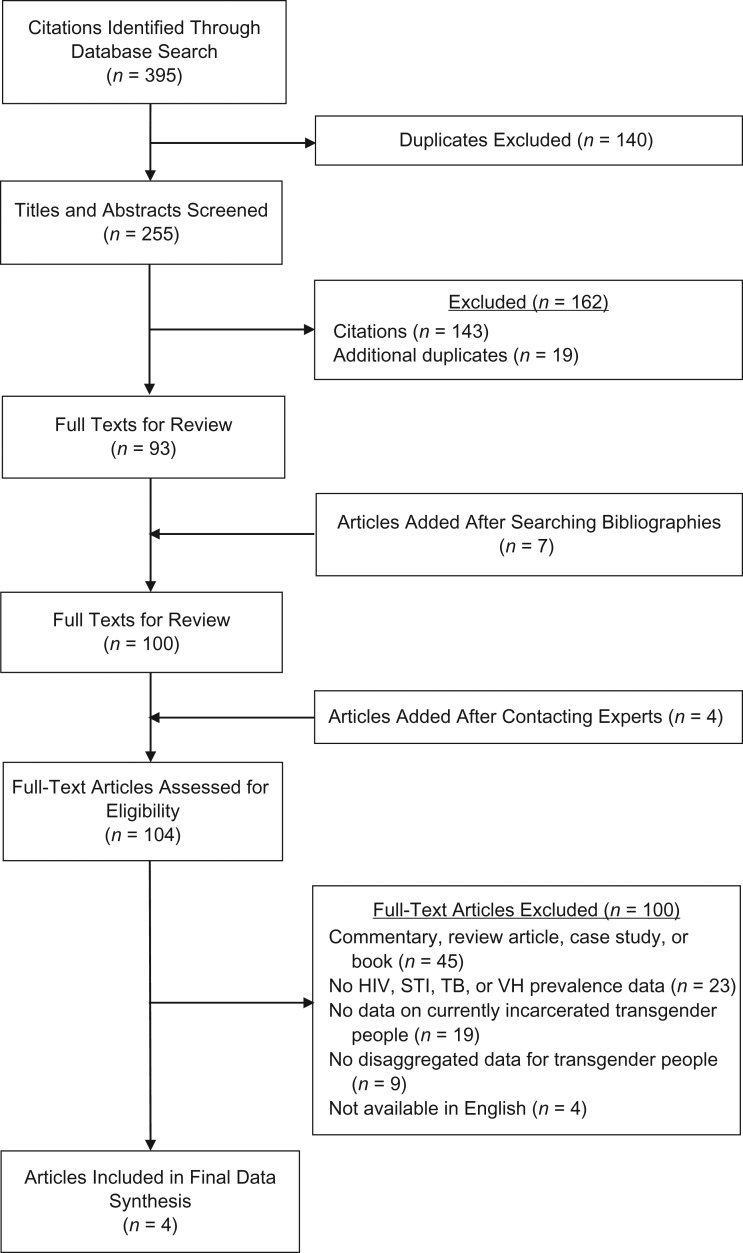
The initial search of all databases identified 395 citations (Figure 1). After 140 duplicates were removed, the remaining 255 articles were included in the title and abstract review, which was conducted by 2 independent reviewers. Articles (n = 143) were excluded if they were clearly not relevant (i.e., not about transgender people or incarceration) or focused on legal cases related to the rights of transgender inmates and detainees. If either reviewer indicated an article should be included, it was retained for full text review. An additional 19 duplicate articles were identified and removed during the title and abstract review. The bibliographies of key articles were searched to identify any relevant literature that may have been missed; as a result, 7 articles were added. Three experts who have published multiple articles on HIV among transgender populations were contacted; the 4 additional articles recommended by these experts were included in our review. A total of 104 articles were retained for full-text review.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram for systematic search of peer-reviewed literature on incarcerated transgender people internationally, 1992–2016.
The full-text review and data extraction were conducted concurrently by 1 reviewer; questions and discrepancies were resolved by the lead author. For all full-text articles reviewed, we recorded type of incarceration (e.g., prison, jail, immigration detention, youth detention), stage of incarceration (e.g., arrest, during, reentry), whether any common human rights issues related to incarcerated transgender populations were addressed (e.g., sex-segregated housing, access to gender-affirming health care, physical and sexual violence), and any data provided on the prevalence of HIV, STIs, viral hepatitis, and/or TB, including self-reported, clinical, or laboratory data. Full-text articles were excluded from data extraction if they were a commentary, review article, or book; only reported on a history of incarceration rather than data collected during incarceration; did not present any quantitative data on prevalence of HIV, STIs, hepatitis, or TB; did not provide data disaggregated for transgender people; or were not available in English. Only 4 articles met the inclusion criteria.
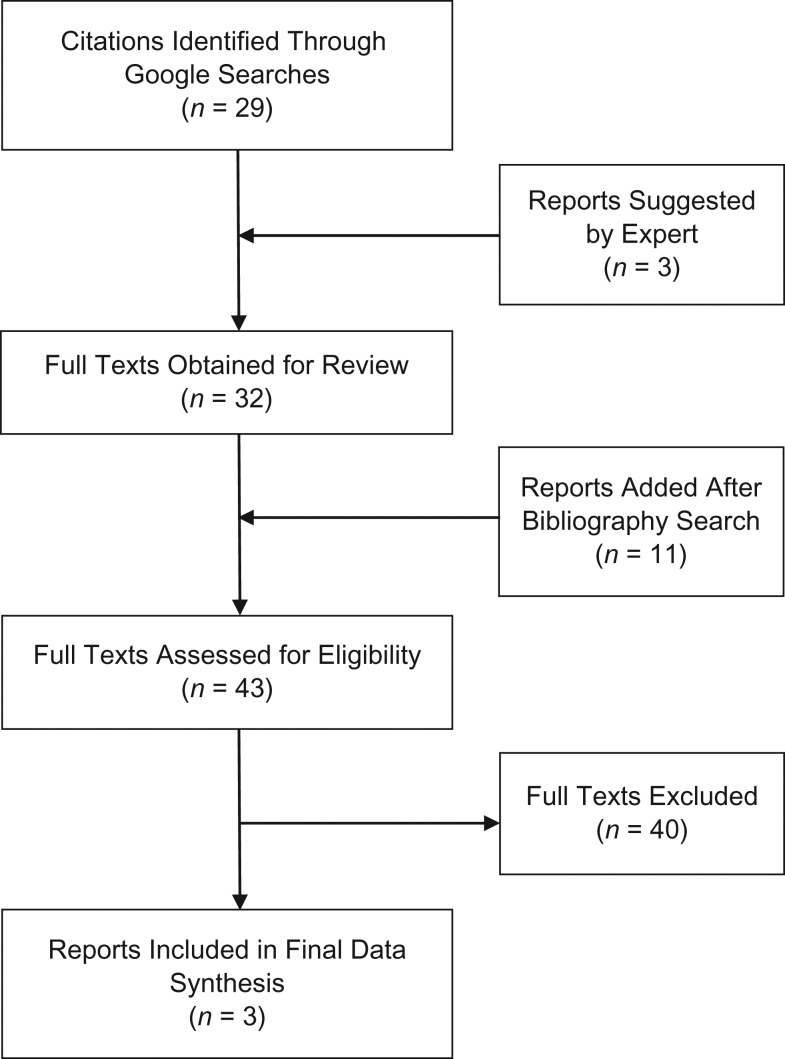
To supplement the limited data available in the peer-reviewed literature, we conducted a systematic search of the gray literature using Google Scholar and Google Search (Figure 2). Combinations of the following terms were used: transgender, LGBT [lesbian, gay, bisexual, transgender], prison, jail, incarceration, youth detention, and immigration detention. Twenty-nine relevant citations were identified and full texts were pulled for review. One report was a literature review that included a lengthy bibliography. This bibliography was also searched for relevant citations, and those full texts were obtained for review, which resulted in 11 additional full-text sources. Experts recommended 3 additional gray literature sources, and these were added to the full-text review. Applying the same criteria to the gray literature full-text review as for the peer-reviewed literature caused 40 reports to be excluded, which resulted in a total of 3 reports that met the inclusion criteria.
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram for systematic search of gray literature on incarcerated transgender people internationally, 1992–2016.
RESULTS
The systematic review of the peer-reviewed (n = 4; Table 1) and gray literature (n = 3; Table 2) resulted in 7 articles with prevalence data on HIV, STIs, viral hepatitis, and/or TB (43, 58–63). All data were cross-sectional and focused on transgender women or transgender people as a group; none focused specifically on transgender men. Of the 4 articles from the peer-reviewed literature, 2 were published in the last 5 years (62, 63): the Mexico City, Mexico, study (n = 84) was published in 2015, and the Milan, Italy, study (n = 117) was published in 2016. The other 2 articles were published more than 2 decades ago: the Sao Paulo, Brazil, study (n = 82) was published in 1996 (60), and the California study (n = 86) was published in 1992 (61). The oldest identified peer-reviewed study was the only one conducted in the United States (61). All gray literature articles were published in the last decade, with 2 articles published in 2011 (Black and Pink, United States n > 1,200) (43); Hearts on a Wire Collective, Pennsylvania, n = 59) (58). Various convenience sampling strategies were used. In the United Nations Office on Drugs and Crime (UNODC) report (Argentina; n = 11), transgender individuals were not sampled intentionally; rather, HIV prevalence data were reported from a single-day visit to the transgender unit at a federal prison (59). Black and Pink distributed a survey to the national readership of its monthly newspaper (approximately 7,000 sexual and gender minority prisoners) (43). The data presented are from lesbian, gay, bisexual, transgender, and queer prisoners who chose to respond and may represent a biased sample. Comparably, for the Hearts on a Wire Collective report, transgender prisoners were recruited through the social networks of currently and formerly incarcerated transgender people and were sent the survey by mail (58). This relatively small sample also included transgender individuals who had recently been released from prison (58).
Table 1.
International Peer-Reviewed and Gray Literature With Data on Transgender Inmates, 1992–2016
| First Author, Year (Reference No.) | Peer-Reviewed Literature or Gray Literature | Location, Year of Data Collection | Facility Type | Study Design | Gender of Transgender Sample |
|---|---|---|---|---|---|
| Colchero, 2015 (63) | Peer reviewed | Mexico City, Mexico, 2012 | Prison | Cross-sectional | TW |
| Crepet, 2016 (62) | Peer reviewed | Milan, Italy, 2012–2013 | Centers of Identification and Expulsion | Cross-sectional | TGa |
| Varella, 1996 (60) | Peer reviewed | Sao Paulo, Brazil, 1990 | Prison | Cross-sectional | TW |
| Valenta, 1992 (61) | Peer reviewed | California, 1987 | State prison | Cross-sectional | TW |
| Lydon, 2015 (43) | Gray | Multiple sites, United States, 2014 | Prisons | Cross-sectional | TW, TS, NBG |
| Hariga, 2011 (59) | Gray | Argentina, 2008 | Federal prison | Cross-sectional legal report | TGa |
| Emmer, 2011 (58) | Gray | Pennsylvania, 2009 | State prisons, jails, detention centers | Community survey | TG and gender-variant people |
Abbreviations: NBG, nonbinary gender; TG, transgender; TW, transgender women; TS, 2-spirit.
a Current gender identity and sex assigned at birth not specified.
Table 2.
Human Immunodeficiency Virus, Sexually Transmitted Infection, Tuberculosis, and Viral Hepatitis Prevalence Data in International Published Literature on Transgender Inmates, 1992–2016
| First Author, Year (Reference No.) | HIV Prevalence | STI Prevalence | Hepatitis Prevalence | Tuberculosis Prevalence | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Laboratory Data | Self-Report | Laboratory Data | Self-Report | Laboratory Data | Self-Report | Laboratory Data | Self-Report | |||||||||
| No.a | % | No.a | % | No.a | % | No.a | % | No.a | % | No.a | % | No.a | % | No.a | % | |
| Colchero, 2015 (63) | 84 | 31.9 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Crepet, 2016 (62) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 117 | 10.3 |
| Varella, 1996 (60) | 82 | 78.0 | NR | NR | NR | NR | 82 | 39.0c | NR | NR | 82 | 12.0d | NR | NR | 82 | 13.0e |
| Valenta, 1992 (61) | 76b | 3.9b | NR | NR | Syphilis, 86 | Syphilis, 11.6 | 86 | 30.2c | NR | NR | 86 | 25.6d | NR | NR | NR | NR |
| Lydon, 2015 (43) | TW: NR | NR | 137 | 13.0 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | |
| TS: NR | NR | 51 | 6.0 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| NBG: NR | NR | 62 | 13.0 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| Hariga, 2011 (59) | 11f | 54.5 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Emmer, 2011 (58) | NR | NR | 59 | 33.9 | NR | NR | NR | NR | NR | NR | 59 | Hep C 20.3d | NR | NR | NR | NR |
Abbreviations: Hep B, hepatitis B; Hep C, hepatitis C; HIV, human immunodeficiency virus; NBG, nonbinary gender; NR, not reported; STI, sexually transmitted infection; TW, transgender women; TS, 2-spirit.
a Total sample size (i.e., denominator, number of respondents for question).
b In the abstract, the authors state that 76 of 86 participants were tested for HIV seropositivity. On page 247, the authors state 3 of 69 participants tested were HIV-antibody positive (61).
c Any history of STIs.
d Any history of hepatitis. Manuscript reports 4 people with positive hepatitis B soluble antigen, but the number tested is unknown.
e Any history of tuberculosis.
f A total of 11 detainees were hosted in the transgender unit on the day when the United Nations Office on Drugs and Crime visited the Federal Penitentiary System in Argentina (59).
HIV
Overall, 6 of the 7 studies reported data on HIV prevalence (43, 58–61, 63). Sample size varied among the studies; for example, only 1 study included more than 100 people (43), and another study included only 11 (59). In the peer-reviewed literature, HIV prevalence and laboratory-confirmed HIV results were reported in 3 of the 4 studies; HIV prevalence ranged from a low of 3.9% in the California study (n = 86) (61) to a high of 78.0% in the Sao Paulo, Brazil, study (n = 82) (60). The most recent study was conducted in Mexico City in 2012; the authors reported an HIV prevalence of 31.9% among 84 transgender women in 4 prisons (63). According to the 2011 report on the Pennsylvania prison system by Hearts on a Wire Collective (n = 59) (58), 33.9% of 59 inmates self-reported living with HIV. In a more recent survey of incarcerated sexual and gender minorities across the United States (43), the prevalence of self-reported HIV was 13.0% among transgender women (n = 137), 13.0% among gender nonbinary people (i.e., not exclusively male or female identified; n = 62), and 6.0% among 2-spirit (i.e., nonbinary gender specifically associated with Native American cultures; n = 51) identified inmates. Overall sample sizes were not provided for each subpopulation; however, the number of people who responded to the HIV status question was reported (43). The only report with medically confirmed HIV status was based on a United Nations Office on Drugs and Crime visit to a correctional facility in Argentina, where 54.5% of the 11 transgender inmates were living with HIV (59).
STIs
We were unable to identify any STI prevalence data published since 1996 from incarcerated transgender populations. The only laboratory-confirmed data were from the Valenta et al. 1992 study (61) in California prisons (n = 86), in which an 11.6% prevalence of syphilis was reported. However, no data were provided on current symptoms or treatment of any STI, including syphilis. In the same study (61), a 30.2% self-reported lifetime history of any STI was reported. According to the 1996 Brazilian study (n = 82) by Varella et al. (60), 39.0% of incarcerated transgender women reported a lifetime history of any STI.
Viral hepatitis and TB
None of the identified studies provided data on laboratory-confirmed viral hepatitis. The rate of self-reported history of hepatitis (unknown type) was as low as 12.0% in the study from Brazil (60) and as high as 25.6% in the study conducted in California (61). Of the 59 transgender inmates in the report by Hearts on a Wire Collective in Pennsylvania, 20% reported a history of hepatitis C (58). TB prevalence data were reported in 2 of the peer-reviewed studies. In the Sao Paulo, Brazil, study (n = 82) (60), 13.0% of inmates reported a history of TB. More recently, Crepet et al. (62) found that 10.3% of 117 transgender inmates in a detention center in Milan (the only center of identification and expulsion that housed transgender inmates, of 4 such centers that were studied) in 2012–2013 had positive TB screening results, based on a standard symptom screener. Transgender detainees in this study had 4.8-fold odds of having TB-positive screening results compared with cisgender men and cisgender women. None of the gray literature reports provided data on TB (62).
Human rights context
The peer-reviewed literature that reported data on infectious disease prevalence provided minimal information on access to gender-affirming care, housing segregation, or violent victimization. However, all gray literature reports placed health data in the context of these and other human rights issues. Of the 4 peer-reviewed articles, 1 mentioned housing and violence (Mexico City; n = 84) (63), and 1 article discussed access to hormone therapy (California; n = 86) (61). Of the 3 gray literature articles, 2 described all 3 transgender-specific human rights issues (i.e., gender-affirming care, housing segregation, and violent victimization) (43, 58), and 1 (Argentina; n = 11) described only housing (59) (Table 3).
Table 3.
Housing Segregation, Physical and Sexual Violence, and Access to Hormone Therapy Reported in International Peer-Reviewed Health Literature and Gray Literature on Infectious Diseases in Carceral Settings, 1992–2016
| First Author, Year (Reference No.) | Peer-Reviewed Literature or Gray Literature | Access to Gender-Affirming Hormones and/or Surgery | Housing Segregation | Violence |
|---|---|---|---|---|
| Colchero, 2015 (63) | Peer reviewed | NR | “In three of the centers, transgender women and gay men live in an independent wing, which is separated from where other men live. In the remaining center, most of the transgender women were found at the same wing where people with HIV live. All people living with HIV and AIDS in prisons in Mexico City are transferred to this wing in this prison” (p. s101). | “In detention centers, as verbally expressed by transgender women that declined to participate, non-participation was related to the fear of getting an HIV-positive result, and particularly associated with the anxiety of been transferred to the only prison that offers HIV treatment in the city, which is perceived as having a very violent environment” (p. s102). |
| Crepet, 2016 (62) | Peer reviewed | NR | NR | NR |
| Varella, 1996 (60) | Peer reviewed | NR | NR | NR |
| Valenta, 1992 (61) | Peer reviewed | “In 1987, prison policy was for inmates who presented proof of being treated with estrogens or progestogens prior to incarceration to continue to receive treatment while in prison. This was discontinued in 1988 due to concerns about risk of high blood pressure, elevated lipids, and thromboembolic disease. Hormone therapy was abruptly stopped in all inmates” (p. 242). | NR | NR |
| Lydon, 2015 (43)a | Gray |
|
|
|
| ||||
| Hariga, 2011 (59) | Gray | NR | “A specific unit with trained staff has been established to hold the transgender population” (p. 14). “Proposed education, work and other activities are designed based on the needs of the population. All detainees expressed their great satisfaction with this arrangement in the classification. Their specific needs are addressed, including in terms of commodities” (p. 14). | NR |
| Emmer, 2011 (58) | Gray |
|
|
|
|
Abbreviations: HIV, human immunodeficiency virus; NBG, nonbinary gender; NR, not reported; TW, transgender women; TS, 2-spirit.
a A total of 950 participants reported on gender identity: 15% TW, 5% TS, 7% NBG.
b Total sample size.
c Sample size information not reported in article (i.e., numerator and denominator not reported).
d Number represents number of participants placed in solitary confinement for safety or other reasons.
e A total of 37 participants were taking hormones before incarceration.
f Also called “restricted housing” in report (p. 19).
Access to gender-affirming care
The Valenta et al. study (61) focused on hormone levels and noted that prison policy allowed for continuation of hormone therapy for inmates who had been treated before incarceration. However, the authors also noted this policy was abruptly discontinued in 1988 because of concerns about adverse physical effects (e.g., lipid levels, blood pressure, thromboembolic disease). Two reports from the United States (Lydon et al., n > 1,200 (43); Emmer et al., n = 59 (58)) noted that 43.2% to 44.0% of transgender inmates who requested hormones reported being denied access, and Lydon et al. (43) noted that 40.0% of transgender inmates who requested surgery (number not reported) had their request denied.
Housing segregation
Housing situations for transgender inmates varied widely by study and setting. Colchero et al., in Mexico City (n = 84) (63), identified 3 centers where transgender women and gay men were housed together in a separate wing of the men’s facility, apart from the general population, whereas most transgender women were housed in a separate wing specifically for people living with HIV. In the United Nations Office on Drugs and Crime report (59), Hariga praised the establishment of a transgender-specific unit in an Argentinian prison, noting that it provided activities and commodities designed to address the needs of transgender inmates and that all inmates expressed satisfaction with this arrangement. In the Hearts on a Wire Collective report (58), almost 70.0% of transgender inmates reported being housed with the general population; the remainder were in various forms of separated housing (specifically, 5.1% in administrative segregation; 6.8% in solitary confinement, and 17.0% in protective custody). Emmer et al. (58) noted that some transgender inmates desired segregation because it provided greater safety from the violence of other inmates; yet, they also acknowledged that segregation is isolating and psychologically challenging. Data on the overall housing situation for transgender inmates was not provided in the Black and Pink report on US prisons (43), but the authors did note that two-thirds of transgender women (n = 114) in solitary confinement reported being placed there for their safety, including 23.0% who were placed there for safety against their will (43). Similarly, 65.0% of gender nonbinary inmates (n = 52) and 70.0% of 2-spirit inmates (n = 46) reported being placed in solitary confinement for their safety (43).
Violent victimization
Although Colchero et al. (63) did not provide statistics on violence in prison in Mexico City in their study, they did note that incarcerated transgender women verbally expressed fear of study participation because, if they tested positive for HIV, they would be transferred to the only prison in the city that provided HIV treatment, and that facility was perceived as very violent (63). The 2 gray literature reports, which were drawn from convenience samples in the United States (43, 58), provided detailed self-reported data on violence against transgender inmates. In the Black and Pink report, Lydon et al. (43) noted that 79.0%, 68.0%, and 57.0% of transgender women (n = 137), gender nonbinary people (n = 62), and 2-spirit people (n = 51), respectively, reported being raped by inmates; 22.0% (n = 137), 23.0% (n = 62), and 14.0% (n = 51), respectively, reported being raped by staff. Inmates in the Pennsylvania correctional system (n = 59) reported nearly ubiquitous verbal harassment by staff (79.7%) and inmates (90.0%), as well as a high prevalence of physical and sexual assault by staff (27.1% and 27.1%, respectively) and other inmates (52.5% and 44.1%, respectively) (58). Inmates described bathrooms and showers as particularly vulnerable locations for humiliation and violence, and they described searches as times when they were likely to experience verbal and sexual harassment (58).
DISCUSSION
We systematically reviewed the peer-reviewed and gray literature on the prevalence of HIV, STIs, viral hepatitis, and TB among incarcerated transgender people. Surprisingly little data were found. Only 1 study of HIV prevalence in Mexico City (63), 1 study of TB in Milan (62), and no studies of viral hepatitis among transgender women had been published in the peer-reviewed literature in the last 2 decades. Although prevalence of HIV among transgender participants was high, none of the peer-reviewed studies provided comparative data among nontransgender inmates. Authors of the peer-reviewed studies rarely contextualized their findings with data on transgender human rights conditions (i.e., housing segregation, violent victimization, and access to gender-affirming therapy). However, the authors of the gray-literature reports focused on these issues, finding that access to gender-affirming care was poor, housing policies were inconsistent, and violent victimization was pervasive.
This review highlights how little is known about the health of incarcerated transgender people. Epidemiologic data were remarkably limited on the prevalence of HIV, STIs, viral hepatitis, and TB — infectious diseases known to disparately affect incarcerated populations (20). The data that exist are outdated, sporadic, inconsistent in their operationalization of gender identity, and lack laboratory measures for specific STIs, types of viral hepatitis, and active versus latent TB infections. Importantly, none of the peer-reviewed studies included female prisons or transgender men. Access to hormone therapy when needed, good mental health, and freedom from violence have been consistently correlated with lower HIV vulnerability and are key health indicators for transgender people (27, 64); yet, none of the peer-reviewed studies included data on these factors. Research is urgently needed to fill these gaps.
The dearth of health data on transgender people who are incarcerated reflects historical invisibility of transgender populations in policy, legal, and health care systems (65). Similarly, transgender populations are often rendered invisible in research studies that fail to distinguish birth-assigned sex from gender identity (66). Failure to actively recruit transgender participants for studies often results in small sample sizes of transgender people and limits the ability to generalize findings (27). Research on the size of transgender populations is limited; yet, these data are essential for population-level planning and resource allocation (67).
Recommendations for future research must consider the unique challenges posed when seeking to conduct ethical research with incarcerated transgender populations. For example, autonomous decision-making, widely recognized as a necessary condition for informed consent, may not be achievable in a prison or jail where well-being is often contingent on conformity to behavioral standards and obedience toward authority (68). Similarly, ensuring privacy and confidentiality can be challenging in correctional settings (68, 69), especially when inmate supervision is required. These barriers may be amplified for transgender people who are multiply marginalized, particularly when asked to participate in research about heavily stigmatized topics such as HIV and sexual behavior. Despite the existence of several ethical and legal standards for research with incarcerated populations,(68, 70, 71), the ethical concerns noted in the present review have implications for research rigor, particularly the effect of social desirability bias on data validity. As noted by the Institute of Medicine (71), these concerns should not deter research with incarcerated groups, especially when research confers health-related benefits. Indeed, academic researchers and community-based organizations have used creative strategies to collect urgently needed data (17, 72, 73).
The limited data that exist are consistent with a high prevalence of HIV and related infections among transgender populations. Preventing acquisition and transmission of HIV in prisons will require access to effective HIV prevention modalities, including condoms, pre-exposure prophylaxis, and antiretroviral therapy. Although a few facilities provide access to condoms for inmates, many carceral settings defer the provision of condoms for fear it promotes sex in prison. A recent study of inmates in a Los Angeles, California, jail examined condom use among transgender women (n = 19) and men who have sex with men (n = 81) (74). Anal sex was common (53.0%) and condom use was inconsistent. Specifically, 75.0% of transgender women and men who have sex with men reported at least 1 act of condomless anal sex in the prior 30 days (74). According to qualitative findings from the study, limiting condom distribution to 1 per inmate per week was insufficient and likely related to low condom use. Expanding the number of facilities that provide condoms and ensuring unfettered access may be an important strategy for reducing transmission of HIV and STIs among transgender people in prison.
Routine screening for STIs is uncommon in most jails and prisons (75). STI testing and treatment are typically provided for inmates who report symptoms (76). However, the National Commission on Correctional Health Care recommends routine testing for gonorrhea and chlamydia on intake for sexually active men and women up to age 25 years (77). Access to routine, private, confidential, voluntary testing for HIV and STIs, early treatment for HIV and STIs, and provision of pre- and postexposure prophylaxis (28, 73, 78) could reduce the prevalence of HIV and other STIs in jails and prisons, including among transgender people.
Experiences of violent victimization, especially sexual violence, are disturbingly common in carceral settings and disproportionately affect incarcerated transgender people. Whereas 4.0% of the general incarcerated population in the United States has experienced sexual assault in prisons (52), transgender prisoners are up to 13 times more likely to be sexually assaulted than their nontransgender counterparts (79). Human rights standards, the US constitution, and the US Prison Rape Elimination Act are all policy documents that can be used to address transgender rights issues, including prevention of sexual violence as well as access to safe housing and gender-affirming hormone therapy while incarcerated (35, 46, 80). As exemplified in the United Nations Office on Drugs and Crime report on a prison in Argentina, facilities can successfully develop gender-affirming policies, train staff to implement these policies, and improve conditions for transgender inmates (59). Consistent with medical necessity and standards of care, transgender people should be provided access to gender-affirming therapy, regardless of whether they were receiving treatment before incarceration (73).
Systematic data on the relationship between housing assignment and vulnerability to violence among transgender people are limited. Findings reported in the gray literature indicate that inmates differ in housing preferences; some report feeling safer when segregated and others prefer to be housed with the general population (58). Housing assignments should be made with careful consideration of gender identity, safety needs, mental health, and inmate preferences (73). Involuntary segregation should be avoided whenever possible, and solitary confinement should not exceed the 14 days considered humane by the United Nations Commission on Torture. Inmates report showers to be the time when they are most vulnerable to violence and harassment. Whenever feasible and acceptable, transgender inmates should be provided opportunities to use shower and bathroom facilities privately, separate from the general population. Efforts to fully implement the recommendations of the Prison Rape Elimination Act should continue.
An important opportunity for prevention of many of the negative effects of incarceration includes implementation of pre-arrest diversion programs. These programs give law enforcement officers the formal discretion to divert an offender away from the traditional criminal justice system without first making an arrest, and most programs focus on minor drug offenses (81). Individuals can be referred to case management and/or supportive services instead of arrest and jail, thereby gaining immediate access to services and avoiding a criminal record. Seattle’s Law Enforcement Assisted Diversion program for minor drug and prostitution offenses has demonstrated success and may serve as a model for other cities (82). In a nonrandomized, controlled evaluation in which the Law Enforcement Assisted Diversion intervention condition (n = 203) was compared with the system-as-usual control condition (n = 115), program participants had 60.0% lower odds of arrest during the 6 months after evaluation entry, and 58.0% and 39.0% lower odds of, respectively, arrest and of being charged with a felony over the longer term (82).
In conclusion, this systematic review found a paucity of data on HIV, STIs, viral hepatitis, and TB among incarcerated transgender people. Where data existed, the prevalence of HIV and STIs was high. Ethical, innovative research is needed to fill wide gaps in knowledge about the prevalence and determinants of HIV and related infections among incarcerated transgender people. One way to fill this gap would be to ensure that both assigned sex at birth and gender identity are included in data collection efforts, including those that occur as part of the Prison Rape Elimination Act. In addition, transgender-specific studies are needed to identify and address the unique needs of this population.
The high prevalence of HIV and other STIs among incarcerated transgender people highlights the urgent need for prevention. Improved access to HIV and other STI testing, and condoms and other prevention modalities is key. Identifying and addressing violent victimization, particularly sexual violence, as well as other human rights concerns in jails and prisons may also reduce the risk for transmission of HIV and other infectious diseases. Systematic tracking of key indicators can provide important information on the efficacy of these measures in improving the health and safety of incarcerated transgender people.
Prevention of incarceration itself is an important tool for reducing HIV and other infectious diseases. Pre-arrest diversion programs are promising interventions. However, it may be even more effective to address the structural stigma and social exclusion that drive disproportionate incarceration among transgender people and affect how they are treated once in the criminal justice system (5, 13, 83–85).
ACKNOWLEDGMENTS
Author affiliations: Center for Public Health and Human Rights, Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland (Tonia C. Poteat, Mannat Malik, Chris Beyrer).
This work has been supported by a grant from the Bill and Melinda Gates Foundation to the Center for Public Health and Human Rights and facilitated by the infrastructure and resources provided by the Johns Hopkins University Center for AIDS Research (grant P30AI094189), a National Institutes of Health–funded program.
The authors thank Leena Aurora, Dr. Andrea Wirtz, and Dr. Mitchell Wharton for their contributions to the study.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest: none declared.
Abbreviations
- HIV
human immunodeficiency virus
- NTDS
National Transgender Discrimination Survey
- STI
sexually transmitted infection
- TB
tuberculosis
- USTS
United States Transgender Survey
REFERENCES
- 1. Kaeble D, Glaze L. Correctional Populations in the United States US Department of Justice; 2016. https://www.bjs.gov/content/pub/pdf/cpus15.pdf. Updated January 12, 2016. Accessed October 1, 2017. (Report NCJ 250374).
- 2. Carson EA, Anderson E. Prisoners in 2015 US Department of Justice; 2016. http://www.bjs.gov/content/pub/pdf/p15.pdf. Updated December 2016. Accessed October 1, 2017. (Report NCJ 250229).
- 3. James SE, Herman JL, Rankin S, et al. The Report of the 2015 US Transgender Survey Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 4. Grant JM, Mottet LA, Tanis J, et al. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011. [Google Scholar]
- 5. Reisner SL, Bailey Z, Sevelius J. Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the US. Women Health. 2014;54(8):750–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sexton L, Jenness V, Sumner JM. Where the margins meet: a demographic assessment of transgender inmates in men’s prisons. Justice Q. 2010;27(6):835–866. [Google Scholar]
- 8. Drake B. Incarceration gap widens between whites and blacks. Washington, DC: Pew Research Center; 2013; http://www.pewresearch.org/fact-tank/2013/09/06/incarceration-gap-between-whites-and-blacks-widens/. Published September 6, 2013. Updated September 6, 2016. Accessed April 25, 2017. [Google Scholar]
- 9. Simić M, Rhodes T. Violence, dignity and HIV vulnerability: street sex work in Serbia. Sociol Health Illn. 2009;31(1):1–16. [DOI] [PubMed] [Google Scholar]
- 10. Peitzmeier SM, Yasin F, Stephenson R, et al. Sexual violence against men who have sex with men and transgender women in Mongolia: a mixed-methods study of scope and consequences. PLoS One. 2015;10(10):e0139320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Newman PA, Lee SJ, Roungprakhon S, et al. Demographic and behavioral correlates of HIV risk among men and transgender women recruited from gay entertainment venues and community-based organizations in Thailand: implications for HIV prevention. Prev Sci. 2012;13(5):483–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Logie CH, Lacombe-Duncan A, Wang Y, et al. Prevalence and correlates of HIV infection and HIV testing among transgender women in Jamaica. AIDS Patient Care STDs. 2016;30(9):416–424. [DOI] [PubMed] [Google Scholar]
- 13. White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22–29. [DOI] [PubMed] [Google Scholar]
- 16. Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ghoshal N, Knight K Rights in Transition: Making Legal Recognition for Transgender People a Global Priority. New York, NY: Human Rights Watch; 2016; https://www.hrw.org/world-report/2016/rights-in-transition. Updated January 2016. Accessed April 30, 2017. [Google Scholar]
- 18. Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet. 2016;388(10042):390–400. [DOI] [PubMed] [Google Scholar]
- 19. Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–1102. [DOI] [PubMed] [Google Scholar]
- 21. Tarver BA, Sewell J, Oussayef N. State laws governing HIV testing in correctional settings. J Correct Health Care. 2016;22(1):28–40. [DOI] [PubMed] [Google Scholar]
- 22. Sánchez Recio R, Alonso Pérez de Ágreda JP, Santabárbara Serrano J. Sexually transmitted infections in male prison inmates: risk of development of new diseases [in Spanish]. Gac Sanit. 2016;30(3):208–214. [DOI] [PubMed] [Google Scholar]
- 23. Garaycochea Mdel C, Pino R, Chavez I, et al. Sexually transmitted infections in women living in a prison in Lima, Peru [in Spanish]]. Rev Peru Med Exp Salud Publica. 2013;30(3):423–427. [PubMed] [Google Scholar]
- 24. Sieck CJ, Dembe AE. Results of a pilot study of pre-release STD testing and inmates’ risk behaviors in an Ohio prison. J Urban Health. 2011;88(4):690–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zachariah R, Harries AD, Chantulo AS, et al. Sexually transmitted infections among prison inmates in a rural district of Malawi. Trans R Soc Trop Med Hyg. 2002;96(6):617–619. [DOI] [PubMed] [Google Scholar]
- 26. Javanbakht M, Boudov M, Anderson LJ, et al. Sexually transmitted infections among incarcerated women: findings from a decade of screening in a Los Angeles County Jail, 2002–2012. Am J Public Health. 2014;104(11):e103–e109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388(10042):412–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Westergaard RP, Spaulding AC, Flanigan TP. HIV among persons incarcerated in the USA: a review of evolving concepts in testing, treatment, and linkage to community care. Curr Opin Infect Dis. 2013;26(1):10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Baral SD, Poteat T, Strömdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–222. [DOI] [PubMed] [Google Scholar]
- 30. Poteat T, Scheim A, Xavier J, et al. Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr. 2016;72(suppl 3):S210–S219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Reisner SL, Hughto JM, Pardee DJ, et al. LifeSkills for men (LS4M): pilot evaluation of a gender-affirmative HIV and STI prevention intervention for young adult transgender men who have sex with men. J Urban Health. 2016;93(1):189–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Reisner SL, Vetters R, White JM, et al. Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. AIDS Care. 2015;27(8):1031–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Centers for Disease Control and Prevention (CDC) HIV-related tuberculosis in a transgender network–Baltimore, Maryland, and New York City area, 1998–2000. MMWR Morb Mortal Wkly Rep. 2000;49(15):317–320. [PubMed] [Google Scholar]
- 34. Tewksbury R, Potter RH. Transgender prisoners: a forgotten group In: Stojkovic S, ed. Managing Special Populations in Jails and Prisons. Kingston, NJ: Civic Research Institute; 2005:15-1–15-14. [Google Scholar]
- 35. Lines R. From equivalence of standards to equivalence of objectives: the entitlement of prisoners to health care standards higher than those outside prisons. Int J Prison Health. 2006;2(4):269–280. [Google Scholar]
- 36. Coleman E, Bockting WO, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2011;13:165–232. [Google Scholar]
- 37. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association Publishing; 2013. [Google Scholar]
- 38. Bauer GR, Scheim AI, Pyne J, et al. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15:525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brown GR, McDuffie E. Health care policies addressing transgender inmates in prison systems in the United States. J Correct Health Care. 2009;15(4):280–291. [DOI] [PubMed] [Google Scholar]
- 40. Routh D, Abess G, Makin D, et al. Transgender inmates in prisons. Int J Offender Ther Comp Criminol. 2017;61(6):645–666. [DOI] [PubMed] [Google Scholar]
- 41. Jenness V, Smyth M. The passage and implementation of the Prison Rape Elimination Act: legal endogeneity and the uncertain road from symbolic law to instrumental effects. Stanford Law Pol Rev. 2011;22:489. [Google Scholar]
- 42. Mann R. The treatment of transgender prisoners, not just an American problem–a comparative analysis of American, Australian, and Canadian prison policies concerning the treatment of transgender prisoners and a universal recommendation to improve treatment. Law Sex. 2006;15:91. [Google Scholar]
- 43. Lydon J, Carrington K, Low H, et al. Coming Out of Concrete Closets: A Report on Black & Pink’s National LGBTQ Prisoner Survey. Dorchester, MA: Black & Pink; 2015. [Google Scholar]
- 44. Ahalt C, Haney C, Rios S, et al. Reducing the use and impact of solitary confinement in corrections. Int J Prison Health. 2017;13(1):41–48. [DOI] [PubMed] [Google Scholar]
- 45. National Institute of Justice What is administrative segregation? Washington, DC: National Institute of Justice; March 26, 2012. https://www.nij.gov/journals/269/pages/administrative-segregation.aspx. Accessed August 14, 2017. [Google Scholar]
- 46. Lobel J. Prolonged solitary confinement and the Constitution. Univ Pa J Const Law. 2009;11(1):115–138. [Google Scholar]
- 47. Goksel DN. Aiding Turkey’s gay inmates. The New York Times; May 26, 2016. https://www.nytimes.com/2014/05/27/opinion/aiding-turkeys-gay-inmates.html?_r=0. Accessed April 30, 2017. [Google Scholar]
- 48. Kronholm A. ‘This is about more than just prisons’: Thailand tries out a special wing for transgender inmates. The Washington Post; March 26, 2017. https://www.washingtonpost.com/world/asia_pacific/thailands-transgender-inmates-offered-separate-detention-still-craving-hormones/2017/03/15/05e4b3fe-0444-11e7-ad5b-d22680e18d10_story.html?utm_term=0.6abef2628619. Accessed April 30, 2017. [Google Scholar]
- 49. Curry C. Rikers Island jail to open special housing unit for trans women inmates. Vice News; December 2, 2016. https://news.vice.com/article/rikers-island-jail-to-open-special-housing-unit-for-trans-women-inmates. Accessed April 30, 2017. [Google Scholar]
- 50. Queally J. San Francisco jails to house transgender inmates based on gender preference. Los Angeles Times; September 10, 2015. http://www.latimes.com/local/lanow/la-me-ln-transgender-san-francisco-jails-20150910-story.html. Accessed April 30, 2017. [Google Scholar]
- 51. Beck AJ. Sexual victimization in prisons and jails reported by inmates, 2011–12: supplemental tables: prevalence of sexual victimization among transgender adult inmates. Washington, DC: Bureau of Justice Statistics; 2014. https://www.bjs.gov/content/pub/pdf/svpjri1112_st.pdf. Accessed April 30, 2017. [Google Scholar]
- 52. Beck AJ. Sexual victimization in prisons and jails reported by inmates, 2011–12. Washington, DC: Bureau of Justice Statistics; May, 2013. https://www.bjs.gov/content/pub/pdf/svpjri1112.pdf. Accessed April 30, 2017. [Google Scholar]
- 53. Brewer RA, Magnus M, Kuo I, et al. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014;104(3):448–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Beck AJ. PREA Data Collection Activities, 2015 Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2015. [Google Scholar]
- 55. Rubenstein LS, Amon JJ, McLemore M, et al. HIV, prisoners, and human rights. Lancet. 2016;388(10050):1202–1214. [DOI] [PubMed] [Google Scholar]
- 56. Westergaard RP, Rich JD. HIV and re-incarceration: time for a comprehensive approach. Lancet HIV. 2014;1(2):e54–e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sen A. Why and how is health a human right? Lancet. 2008;372(9655):2010. [DOI] [PubMed] [Google Scholar]
- 58. Emmer P, Lowe A, Marshall RB This is a prison, glitter is not allowed: experiences of trans and gender variant people in Pennsylvania’s prison systems. Philadelphia, PA: Hearts on a Wire Collective; 2011. [Google Scholar]
- 59. Hariga F. Evaluation and recommendations for the improvement of the health programmes, including for the prevention and treatment of drug dependence and of HIV and AIDS, implemented in the establishments under the responsibility of the Federal Penitentiary Service in Argentina. Vienna, Austria: United Nations Office on Drugs and Crime; 2011. [Google Scholar]
- 60. Varella D, Tuason L, Proffitt MR, et al. HIV infection among Brazilian transvestites in a prison population. AIDS Patient Care STDs. 1996;10(5):299–302. [DOI] [PubMed] [Google Scholar]
- 61. Valenta LJ, Elias AN, Domurat ES. Hormone pattern in pharmacologically feminized male transsexuals in the California State prison system. J Natl Med Assoc. 1992;84(3):241–250. [PMC free article] [PubMed] [Google Scholar]
- 62. Crepet A, Repetto E, Al Rousan A, et al. Lessons learnt from TB screening in closed immigration centres in Italy. Int Health. 2016;8(5):324–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Colchero MA, Cortés-Ortiz MA, Romero-Martínez M, et al. HIV prevalence, sociodemographic characteristics, and sexual behaviors among transwomen in Mexico City. Salud Publica Mex. 2015;57(suppl 2):s99–s106. [DOI] [PubMed] [Google Scholar]
- 64. Grinsztejn B, Jalil EM, Monteiro L, et al. Unveiling of HIV dynamics among transgender women: a respondent-driven sampling study in Rio de Janeiro, Brazil. Lancet HIV. 2017;4(4):e169–e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bauer GR, Hammond R, Travers R, et al. “I don’t think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care. 2009;20(5):348–361. [DOI] [PubMed] [Google Scholar]
- 66. Poteat T, German D, Flynn C. The conflation of gender and sex: gaps and opportunities in HIV data among transgender women and MSM. Glob Public Health. 2016;11(7–8):835–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. McFarland W, Wilson E, Fisher Raymond H. How many transgender men are there in San Francisco? [published online ahead of print May 1, 2017]. J Urban Health. (doi: 10.1007/s11524-017-0150-5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kalmbach KC, Lyons PM Jr. Ethical and legal standards for research in prisons. Behav Sci Law. 2003;21(5):671–686. [DOI] [PubMed] [Google Scholar]
- 69. Seal DW, Eldridge GD, Zack B, et al. HIV testing and treatment with correctional populations: people, not prisoners. J Health Care Poor Underserved. 2010;21(3):977–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lerner BH. Subjects or objects? Prisoners and human experimentation. N Engl J Med. 2007;356(18):1806–1807. [DOI] [PubMed] [Google Scholar]
- 71. Institute of Medicine Ethical Considerations for Research Involving Prisoners. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 72. Jenness V. From policy to prisoners to people: a‘soft mixed methods’ approach to studying transgender prisoners. J Contemp Ethnogr. 2010;39(5):517–553. [Google Scholar]
- 73. Sevelius J, Jenness V. Challenges and opportunities for gender-affirming healthcare for transgender women in prison. Int J Prison Health. 2017;13(1):32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Harawa NT, Sweat J, George S, et al. Sex and condom use in a large jail unit for men who have sex with men (MSM) and male-to-female transgenders. J Health Care Poor Underserved. 2010;21(3):1071–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Parece MS, Herrera GA, Voigt RF, et al. STD testing policies and practices in US city and county jails. Sex Transm Dis. 1999;26(8):431–437. [DOI] [PubMed] [Google Scholar]
- 76. Brown K. Managing sexually transmitted diseases in jails. Providence, RI: The Body; September, 2003. http://www.thebody.com/content/art12916.html#difficulties. Accessed August 14, 2017. [Google Scholar]
- 77. National Commission on Correctional Health Care STD testing for adolescents and adults upon admission to correctional facilities. Chicago, IL: National Commission on Correctional Health Care; October, 2014. http://www.ncchc.org/std-testing-upon-admission. Accessed August 14, 2017. [DOI] [PubMed] [Google Scholar]
- 78. Hammett TM. Sexually transmitted diseases and incarceration. Curr Opin Infect Dis. 2009;22(1):77–81. [DOI] [PubMed] [Google Scholar]
- 79. Jenness V, Fenstermaker S. Agnes goes to prison: gender authenticity, transgender inmates in prisons for men, and pursuit of “the real deal”. Gend Soc. 2014;28(1):5–31. [Google Scholar]
- 80. Lines R. The right to health of prisoners in international human rights law. Int J Prison Health. 2008;4(1):3–53. [DOI] [PubMed] [Google Scholar]
- 81. Piper BJ, Desrosiers CE, Fisher HC, et al. A new tool to tackle the opioid epidemic: description, utility, and results from the Maine Diversion Alert program. Pharmacotherapy. 2017;37(7):791–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Collins SE, Lonczak HS, Clifasefi SL. Seattle’s Law Enforcement Assisted Diversion (LEAD): program effects on recidivism outcomes. Eval Program Plann. 2017;64:49–56. [DOI] [PubMed] [Google Scholar]
- 83. Slamah K, Winter S, Ordek K. Violence against trans sex workers (TSWs): stigma, exclusion, poverty and death. Res Sex Work. 2010:30–31. [Google Scholar]
- 84. Perez-Brumer AG, Reisner SL, McLean SA, et al. Leveraging social capital: multilevel stigma, associated HIV vulnerabilities, and social resilience strategies among transgender women in Lima, Peru. J Int AIDS Soc. 2017;20(1):21462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Ganju D, Saggurti N. Stigma, violence and HIV vulnerability among transgender persons in sex work in Maharashtra, India. Cult Health Sex. 2017;19(8):903–917. [DOI] [PMC free article] [PubMed] [Google Scholar]