Abstract
Smoking tobacco contributes to 11.5% of deaths worldwide and, in some countries, more hospitalizations than alcohol and drugs combined. Globally in 2015, 25% of men and 5% of women smoked. In the United States, a higher proportion of people in prison smoke than do community-dwelling individuals. To determine smoking prevalence in prisons worldwide, we systematically reviewed the literature using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines; we also examined whether prisons banned smoking or treated smokers. We searched databases for articles published between 2012 and 2016 and located 85 relevant articles with data representing 73.5% of all incarcerated persons from 50 countries. In 35 of 36 nations (97%) with published prevalence data, smoking for the incarcerated exceeded community rates 1.04- to 62.6-fold. Taking a conservative estimate of a 2-fold increase, we estimated that, globally, 14.5 million male and 26,000 female smokers pass through prisons annually. Prison authorities’ responses include permitting, prohibiting, or treating tobacco use. Bans may temporarily improve health and reduce in-prison health care costs but have negligible effect after prison release. Evidence-based interventions for smoking cessation effective outside prisons are effective inside; effects persist after release. Because smoking prevalence is heightened in prisons, offering evidence-based interventions to nearly 15 million smokers passing through yearly would improve global health.
Keywords: correctional, criminal justice, incarcerated, jail, prison, smoking, tobacco
INTRODUCTION
Globally in 2015, 1 in 4 men, and 1 in 19 women, smoked tobacco daily (1). Smoking tobacco is a major cause of preventable disease and death in most countries. Worldwide, 11.5% of deaths are attributable to smoking (1), and in Australia, for example, smoking contributes to more hospitalizations than alcohol and illicit drug use combined (2, 3). Smoking rates have fallen in many resource-rich countries since the end of the last century, due in part to policy changes such as tobacco tax increases; restrictions on tobacco advertising, promotion, and sponsorship; mass media campaigns; and pictorial health-warning labels (1, 4). Despite this overall decline in smoking prevalence, reductions have not been uniform, with smoking rates remaining higher among the poor, the less educated, and individuals with less access to prevention or treatment (5, 6). Internationally, a group that remains at greatest risk for smoking and its associated health consequences is people who have been imprisoned. In spite of the steady drop in smoking prevalence in countries such as the United States and Australia (1–4), people in carceral settings remain a population with high rates of smoking and less access to treatment or prevention for smoking (7).
For decades, the United States has led the world with its imprisonment rate (8), and the subpopulations incarcerated at the highest rates are those most likely to smoke: men, younger persons, and the poor and less educated (9, 10). In 2004, before smoking bans became commonplace in US correctional facilities, the prevalence of smoking was 56.2% among all Americans who spent time in prison or jail, and/or experienced homelessness—a rate 2.7 times that for community-dwelling citizens (11). (This figure comes from an analysis based on National Health Interview Survey data; the analysis did not disaggregate the homeless and the incarcerated.) Whether this US pattern whereby smokers and those most likely to smoke are overrepresented in correctional populations is replicated internationally is unknown, although it is documented in a number of high-resource countries in a study that first appeared online in 2012 (12). If, worldwide, correctional settings hold a concentrated number of smokers, tobacco cessation efforts in these settings would likely be cost-effective. To understand the prevalence of smoking in carceral settings internationally, a systematic review of the literature on smoking by confined persons is warranted.
In response to the high rates of smoking among individuals entering prisons and jails, many high-resource countries have instituted smoking bans in correctional facilities. The most common justification for smoking bans is to protect the health of persons who live and work in prisons by reducing smoking and exposure to secondhand smoke. Unwanted exposure to secondhand smoke was declared cruel and unusual punishment and outlawed by the US Supreme Court (13). Other justifications given by prison authorities for smoking bans are to reduce the cost of providing medical care, including hospitalizations, for prison employees and persons living in prisons. Smoking bans in prison are associated with an adjusted incidence rate ratio of 0.91 (95% confidence interval: 0.88, 0.95) in tobacco-related deaths and, once in place over 9 years, an adjusted cancer mortality rate ratio of 0.81 (95% confidence interval: 0.74, 0.90) (14). In addition, some prisons banned smoking to reduce “frills,” along with other amenities such as weight lifting equipment, musical instruments, and crafts programs (15). Last, smoking bans can reduce the risk of arson and burn injuries (16).
Opposition to bans has stemmed from many sources. Libertarians advocate for the right of incarcerated people to smoke if they choose and discuss the real or perceived likelihood that bans will lead to riots (17). As pointed out by Araromi (18), the European Prison Rules of 2006 state that “persons deprived of their liberty retain all rights that are not lawfully taken away by the decision sentencing them or remanding them in custody,” and the United Nations Human Rights Committee likewise stipulated that incarcerated persons retain rights except those unavailable by virtue of confinement. Many defend access to tobacco as an antidote to boredom and a stress reliever in the difficult circumstances of incarceration (19). Last, cigarettes have traditionally been used as a surrogate currency (20) because possessing money is outlawed in most prisons. Now that smoking bans have been imposed, commissary-bought packets of ramen noodles or stamps (21) have become the new currency in some systems.
Nonetheless, smoking bans without treatment of the underlying addiction to tobacco may have little effect on lifetime health. Little attention has been paid to postrelease rates of smoking and evidence that bans produce lasting change in smoking is sparse (22). Because measures to prevent disease need to be sustained to have an influence, health care planners should consider the effect of in-prison smoking bans on smoking after release from prison. One study of 129 persons who smoked before entry and were released from a county jail in Massachusetts showed that, without intervention other than a smoking ban, prevalence of smoking reverts quickly, with 97% of entrants resuming smoking within 6 months after release (23). There is evidence that counselling and behavioral interventions for smoking cessation in prisons show similar effects to those in community settings (24, 25) and there is support for the effectiveness of combined pharmacologic and psychological interventions during incarceration (26–28).
In this paper, we review systematically the prevalence of smoking in prison and corresponding community settings worldwide. We also review the implementation of bans on smoking in prison and interventions to reduce smoking during and after incarceration. Finally, we discuss the short- and long-term effects of decreasing smoking in the custodial environment. We anticipated much of the literature would describe conditions in industrialized nations, because incarceration rates tend to be higher in more-affluent countries (8) and data collection in prisons may be greater in high-resource nations. We also anticipated that smoking bans in correctional settings would be shown to have short-term effects on reducing smoking and exposure to secondhand smoke and improving health indicators but little, if any, long-time effect on smoking rates after release.
METHODS
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (29), with modifications to incorporate previously conducted systematic reviews (30), we conducted a comprehensive systematic review of published and grey literature covering the period 2012–2016, to not overlap with a very comprehensive past review (12). We searched PubMed using the following search terms: (prison* OR jail* OR inmate OR inmates OR “correctional facility” OR incarcerated OR desmoteric OR carceral OR “Prisons” [Mesh:NoExp]) AND (Smok* OR “tobacco use” OR Cigar* OR “smoking”[MeSH Terms] OR “Tobacco Products”[Mesh]). Other searches in PubMed included the tobacco terms and (1) “institutionalized” and (2) “compulsory.” We also searched Excerpta Medica dataBASE for articles using the aforementioned carceral and tobacco terms. We also searched Cumulative Index to Nursing and Allied Health Literature, Cochrane Database, and PsychInfo.
We noted that a number of published papers on tuberculosis in carceral settings included data on smoking. Mentions of tobacco in reports of tuberculosis may be because smokers have complaints similar to symptoms of tuberculosis (e.g., cough), smoking may predispose persons to acquisition of tuberculosis (e.g., via altered immunity), or smoking may simply be a confounder for heightened tuberculosis disease severity (e.g., both linked to poverty) (31). Because of this strong association, a second search of PubMed was made for articles on tuberculosis using the following terms: (prison* OR jail* OR inmate OR inmates OR “correctional facility” OR incarcerated OR desmoteric OR carceral OR “Prisons”[Mesh:NoExp]) AND tuberculosis) limited to publication in 2012– 2016. A search of these articles and the references of a systematic review found by the search (32) generated additional relevant articles not found without tuberculosis as a search term.
We searched African Journals Online with the search terms of prisons and smoking, jails and smoking, prisons and tobacco, jails and tobacco; its search engine did not support strategies with as many Boolean operators as PubMed. Similar search terms were used for Literatura Latinoamericana y del Caribe en Ciencias de la Salud and the Chinese National Knowledge Infrastructure. Last, we used snowball sampling by searching references of relevant articles and articles that cited articles with relevant data.
We searched for data on the World Health Organization website for data on smoking bans, specifically on a website listing bans in government settings (33). Comparison data for the community came from the World Health Organization Tobacco Report 2015 (34), which contained data on smoking rates by 5-year intervals (e.g., 2005, 2010, 2015). Data for the year closest to the year for which correctional data are available are presented for comparison (e.g., World Health Organization data for 2 years before or 2 years after the year that the study collected data). Also, we consulted a study using Global Burden of Disease data (1).
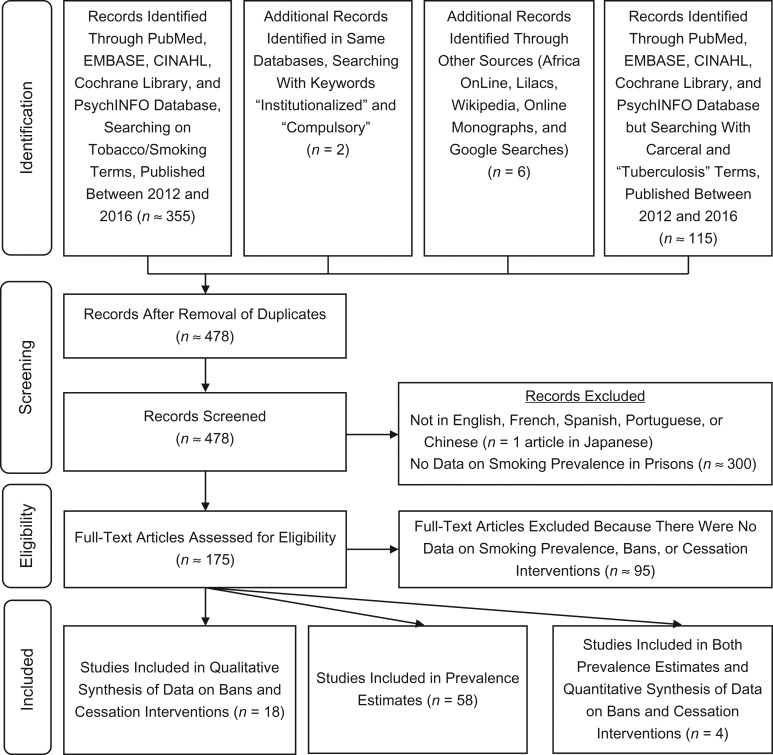
Our multilingual research team was literate in English, French, Spanish, Portuguese, and Chinese and was able to search these sources in these languages to extract data from relevant literature. Reports using the tobacco and carceral keywords were first scanned by title, then abstract, then full text, if the extractor judged that the article would have unduplicated data on smoking prevalence. For articles with nonstandard keywords (e.g., tuberculosis), some articles were opened and tables searched for the term “smok*” without reading the abstract first. Eligible articles were read by at least 2 readers. Because of multiple extractors, the numbers for abstracts scanned and articles read in entirety are estimates rather than exact numbers (noted as “approximately” in Figure 1). Data are presented for men and women and for adults older than age 15 years. When possible, we distinguished reports on prevalence and interventions for those awaiting trial versus sentenced populations, if the correctional system of a nation segregated the 2 groups. For prevalence data, if data collection spanned 2 calendar years, the data were attributed to the year that contained the majority of collection months. If the data gathered spanned multiple years, we attributed the data to the last year in the time period.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses schema for article selection on smoking in prison, with data published in years 2012–2016. The following databases were searched: PubMed, Excerpta Medica dataBASE (Embase), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, PsychINFO, Africa Journals Online, and Literatura Latinoamericana y del Caribe en Ciencias de la Salud (Lilacs). Because of multiple extractors, the numbers reported for abstracts scanned and articles read in their entirety are estimates rather than exact numbers; these values are shown as approximate.
Because others have recently conducted excellent reviews of smoking bans and cessation interventions (12, 14, 22, 35), we informally reviewed those reviews and checked whether additional studies could be added, rather than conducting original, exhaustive searches on these topics. From these, we gleaned which prison systems had bans and the effect of behavioral and pharmacologic interventions in prisons. We consulted the World Prison Brief (8) for data on prison system sizes.
ANALYSIS
We calculated the fold increase in smoking prevalence for prisons over that for the general population. We also estimated how many individuals enter and are released from prison, using data from the United Nations, which found that the average prison population turns over 3 times over the course of a year (36). From this point, we could estimate the number of individuals who would be affected if all countries had cessation interventions in their prisons.
RESULTS
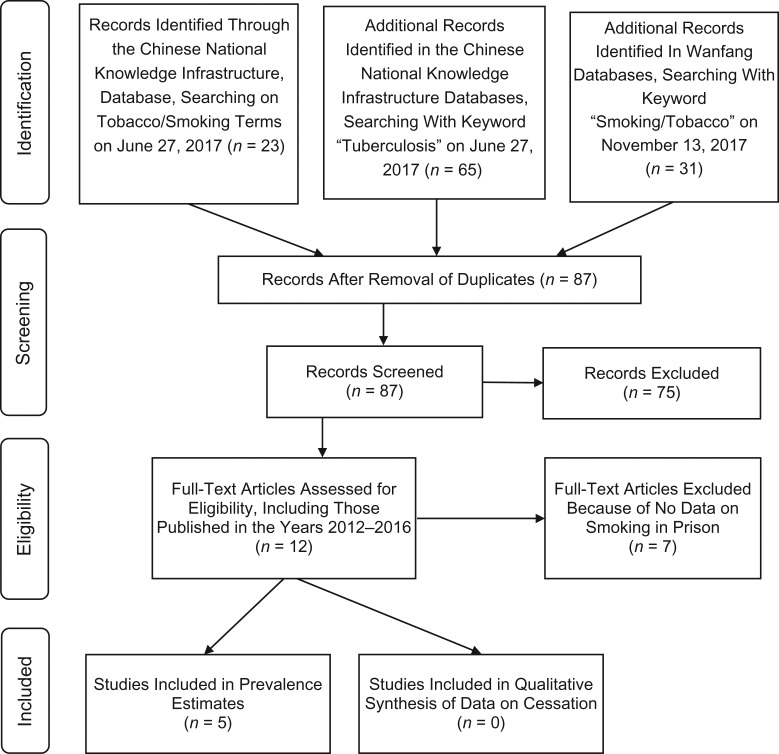
Our initial search on tobacco-related terms in PubMed and Excerpta Medica dataBASE netted 285 articles published between 2012 and 2016; all but 1 was in English, French, Spanish, or Portuguese. A search on Africa Journals Online netted an additional 3 articles; Cumulative Index to Nursing and Allied Health Literature and Literatura Latinoamericana y del Caribe en Ciencias de la Salud identified zero additional peer-reviewed articles. The Chinese National Knowledge Infrastructure netted 5 articles; subsequent searches on the Chinese database Wanfang added no extra articles (Figures 1 and 2). We found an additional 14 papers when we used tuberculosis search terms on PubMed. Most articles were from industrialized countries, especially the United States, Australia, and Brazil. No data were published on Caribbean nations, but personnel from Health Through Walls, a nongovernmental organization working primarily in prisons in Haiti, the Dominican Republic, Jamaica, and some African nations, note that habitual smoking is rare in prisons in low-resource countries (Dr. John P. May, Health Through the Walls, personal communication, 2017).
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses schema for article selection from the Chinese National Knowledge Infrastructure and Wanfang databases on smoking in prison, with data published in years 2012–2016.
Prevalence
The prevalence of smoking is high among persons in prisons worldwide. For granular data on persons in US prisons, and the general population and minority subpopulation in Australia facilities, see Web Appendices 1 and 2, Web Tables 1 and 2, and Web Figure 1 (available at https://academic.oup.com/aje). For details country by country on remaining nations, grouped by region, see Tables 1–4. A review chapter (12) published in 2012 also cited information on prevalence for Poland (81%) published in 2006 (39), and Lithuania (85.5%) in 2007 (40), 2 countries for which we found no more recent data. In all but 1 article, we found higher levels of smoking in prison compared with the community, ranging, for example, from more than 5-fold higher in Iran to just short of 2-fold higher in Uganda, South Africa, and Chile. In no country was smoking among the prison population consistently lower than in was at the community level. Although data were scarce, this pattern was repeated when the correctional population was analyzed by sex and smoking among men and women was compared with that occurring at community levels (e.g., among Greek men in prison vs. in the community, 75.5% vs. 55.7%, respectively; Pakistani women in prison vs. in the community, 60.9% vs. 3.7%, respectively). There was a trend of higher levels among men than among women in prison (e.g., men vs. women in Mexico prisons, 61.5% vs. 53.8%, respectively) that was repeated in the general population (Mexico community, men vs. women: 25.4% vs. 8.4%, respectively). In a single-prison study in China, most men who had ever smoked said they were former smokers.
Table 2.
Prevalence of Smoking in General Population and in Prison by Sex, Asia and Pacific Island, 2012–2016
| First Author, Year (Reference No.) | Location | Study Population | Year Data Collected | In Prison, % | General Population,a % | Fold Increase | No. of Incarcerated Study Subjects | Prison Populationb |
|---|---|---|---|---|---|---|---|---|
| Mixed Sex Studies | ||||||||
| Chen, 2014 (66) | China | Cases of xerophthalmia | 2013 | 74.7 | 26.3 | 2.84 | 79 | 1,657,812 |
| Tiwari, 2014 (67) | India | 5 central jails of Chhattisgarh State in a sample of 506 persons in prison | 2013 | 56.2 | 11.0 | 5.11 | 506 | 418,536 |
| Al-Darraji, 2014 (68) | Malaysia | TB study, prison of 340 | 2010 | 98.2c | 23.7c | 4.14 | 286 | 38,387 |
| Margolis, 2013 (69) | Malaysia | TB study, prison of 288 | 2011 | 98.1 with prior history | 23.7 | 4.14 | 266 | 36,608 |
| Muir, 2016 (70) | New Zealand | TB and LTBI | 2011 | 60–80 | 17.9d | 3.35 | Not specified | 8,604 |
| Soomro, 2016 (71) | Pakistane | 300 persons in prison | 2015 | 62.0 | 21.6 | 2.87 | 300 | 79,700 |
| Morishita, 2017 (72) | Philippines | TB | 2015 | 82.4c | 25.3c | 3.26 | 6,133 | 120,076 |
| Studies in Men | ||||||||
| Liu, 2015 (73) | China, Xi’an city | Study of health status | 2013–2014 | 63.3 | 49.3 | 1.28 | 627 | 1,565,400 |
| Wang, 2016 (74) | China, Nantong, Jiangsu province; | Smoking status before prison:
|
2014 |
|
49.3 | 0.56f | 2,205 | 1,565,400 |
| Shi, 2015 (75) | China, Hongzehu, Jiangsu province | Cases of hypertension | 2014 | 65.3 | 49.3 | 1.32 | 300 | 1,565,400 |
| Torwane, 2013 (76) | India | Half with psychiatric issues, half without | 2013 | 77.0c | 11.0c | 7.00 | 244 | 353,961 |
| Naik, 2014 (22) | India | 1,600 convicted persons in prison | Not given | 78.3c | 11.0c | 7.27 | 1,600 | 353,961 |
| Chen, 2012 (77) | Taiwan | Smoking before prisons | 2000 | 90.7 | 33.5d | 2.72 | 589 | 51,689 |
| Li, 2013 (78) | Taiwan | Controls in cancer study | 2008 | 89.1 | 33.5d | 2.61 | 709 | 57,642 |
| Studies in Women | ||||||||
| Khan, 2012 (79) | Pakistan | Study of depression in women’s prison of 140 | 2008 | 60.9 | 3.7 | 16.49 | 64 | 931 |
| Liu, 2015 (80) | China, city of Xi’an | Study of health status | 2013–2014 | 30.6 | 2.0 | 15.3 | 500 | 107,131 |
Abbreviations: LTBI, latent tuberculosis infection; TB, tuberculosis.
a Data on general population from the World Health Organization (34), unless otherwise stated.
b Data from World Prison Brief data (8).
c In this region, the prevalence of smoking among prison population was very high in comparison with the general population in Malaysia (98.2% vs. 23.7%) and Australia (74% vs. 14.3%), Indian men (>75% vs. 11%), and Filipinos in the context of a TB study (82.4% vs. 25.3%).
d Data from Ng (46).
e Pakistan tested levels of smoking among particular groups (52% of murderers and 72% of thieves) and found it much higher than the general population (21.2%).
f Only among Chinese men, who in the general population have some of the highest rates of smoking in the world, was smoking in prison not consistently higher.
Table 3.
Prevalence of Smoking in General Population and in Prison by Sex, Mid-Eastern and African Countries, 2012–2016
| First Author, Year (Reference No.) | Location | Study Population | Year Data Collected | In Prison, % | General Population,a % | Fold Increase | No. Incarcerated Study Subjects | Prison Populationb |
|---|---|---|---|---|---|---|---|---|
| Mixed Sex Studies | ||||||||
| Kwabla, 2015 (81) | Ghana | TB study | 2014 | 43.7 | 6.1 | 7.16 | 161 | 13,164 |
| Mamani, 2016 (82) | Iran | LTBI study | 2013 | 81.9c | 10.9c | 7.53 | 1,208 | 226,220 |
| Khajedaluee, 2016 (83) | Iran | Study participants with HTLV-I, HBV, HCV, and KSHV | 2008 | 70.2 | 11.8 | 5.95 | 1,114 | 168,516 |
| Mor, 2015 (84) | Israel, Eritrea, Sudan, Ethiopia | Undocumented, detained migrants with radiograph suggestive of TB | 2009 | 48.4 | 19.9d | 2.43 | 62 | 20,164 |
| Kinyanjui, 2013 (85) | Kenya | Prison population in Kenya | 2011 | 32.7 (14.0% in past week) | 13.5 | 1.04; 2.42 | 395 | 52,000 |
| Mnisi, 2013 (86) | South Africa | TB | 2010 | 59.9 | 19.4 | 3.09 | 202 | 163,312 |
| Ekouevi, 2013 (87) | Togo | Study of HIV seroprevalence in the prison population | 2011 | 31.9 | 3.9d | 8.18 | 1,342 | 4,060 |
| Owokuhaisa, 2014 (88) | Uganda | TB study | 2012 | 19.7e | 10.1e | 1.95 | 677 | 34,940 |
| Studies of Men | ||||||||
| Fuge, 2016 (89) | Ethiopia | Persons screened for pulmonary TB | 2013 | 54.9 | 8.1 | 6.78 | 164 | 100,572 |
| Akaji, 2013 (20) | Nigeria | Study of tobacco use | 2010 | 53.6e | 15.0e | 3.57 | 224 | 45,689 |
| Jaquet, 2016 (90) | Senegal | Men incarcerated in Lome, Togo; and in Dakar, Senegal | 2014 | 64.2 | 23.5 | 2.73 | 333 | 8,355 |
| Telisinghe, 2014 (91) | South Africa | TB study | 2010 |
|
32.0 | 1.81 | 981 | 159,618 |
| Nyasulu, 2015 (92) | South Africa | Those treated for TB | 2010 |
|
32.0 | 1.53 | 1,140 | 159,618 |
| Jaquet, 2016 (90) | Togo | Men incarcerated in Lome, Togo; and in Dakar, Senegal | 2013 | 29.4 | 13.8d | 3.57 | 347 | 4,372 |
| Studies of Women | ||||||||
| Abera, 2016 (93) | Ethiopia | 738 persons in prison in 9 major prison setups in Tigray region | 2013 | 31.3 | 0.5 | 62.60 | 16 | 3,630 |
| Fageeh, 2014 (94) | Saudi Arabia | Saudi Arabia women at Briman Prison, Jedda, n = 300 | 2012 | 18.6c | 2.8c | 6.64 | 204 | 2,793 |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HTLV, human T-cell leukemia virus type I; KSHV, Kaposi sarcoma–associated herpes virus; LTBI, latent tuberculosis infection; TB, tuberculosis.
a Data on General Population from the World Health Organization (34), unless otherwise stated.
b Data from World Prison Brief data (8).
c In the Middle East, few data were located. Iran and Saudi Arabia had a higher level of smoking among general (94%) and female carceral (18.6%) populations than the general population (10.9%) and general female population (2.8%), respectively.
d Data from Ng (46).
e In Africa, we located data for 6 countries. Higher levels were found among mixed sex prison studies in Nigeria (53.6%) and Uganda (19.7%) than in the general community (15% and 10.1%) respectively.
Table 1.
Prevalence of Smoking in General Population and in Prison by Sex, Europe, 2012–2016
| First Author, Year (Reference No.) | Location | Study Population | Year Data Collected | In Prison, % | General Population,a % | Fold Increase | No. of Incarcerated Study Subjects | Prison Populationb |
|---|---|---|---|---|---|---|---|---|
| Mixed Sex Studiesc | ||||||||
| Jaka, 2014 (51) | Albania | Study of health status | 2013 | 59.1 | 29.3 | 2.02 | 401 | 5,201 |
| Jacomet, 2016 (52) | France | Surveillance for infectious disease | 2013 | 83.8 | 24.7 | 3.39 | 357 | 72,796 |
| Ceelen, 2012 (53) | Netherlands | Study of health history | 2009 | 75.6 | 26.7 | 2.85 | 264 | 15,235 |
| Turan, 2015 (54) | Turkey | Persons with COPD | 2013 | 68.7 | 25.9d | 2.65 | 109 | 158,837 |
| Carnie, 2016 (41) | Scotland | 9 Scottish prisons | 2015 | 72.0 | 18.7e | 3.85 | Not specified | 7,611 |
| Studies of Men | ||||||||
| Singleton, 2003 (55); Jayes, 2016 (56) | England | 4 prisons with smoke-free wings | 1997 | 85.0 of remand 78.0 of sentenced | 23e | 3.39 | Not specified | 61,252 |
| Chariot, 2014 (57) | France | Fitness assessment while incarcerated | 2012 | 70.3f | 30.4g | 2.30 | 10,726 | 80,489 |
| Makris, 2012 (27) | Greece | 204 men in prison | 2010 | 75.5 | 55.7d | 1.36 | 204 | 10,810 |
| McCaffrey, 2012 (58) | Ireland | General health care study of the Irish prison population | 2000 | 91.0f | 32.3e | 2.82 | Not specified | 2,864 |
| Mannocci, 2015 (59) | Italy | Study of health status while incarcerated | 2011 | 69.7 | 29.0 | 2.40 | 121 | 64,966 |
| Pinto, 2015 (60) | Portugal | Youth in detention (ages 13–19 years) | Not specified | 40.0 current; 90.0 “early initiation” | 28.8 | 1.39 | 30 | 13,065 |
| Vera-Remartínez, 2014 (61) | Spain | Study in prison (n = 1,170) | 2013 | 71.0 | 29.9g | 2.37 | 1,022 | 70,692 |
| Ritter, 2013 (62) | Switzerland | Switzerland | 2010 | 84.0 | 25.5 | 3.29 | Not specified | 5,834 |
| Winetsky, 2014 (63) | Tajikistan | TB | 2010 | 38.6 | 30.0 | 1.29 | 1,317 | 9,168 |
| Studies of Women | ||||||||
| Singleton, 2003 (55); Jayes 2016 (56) | England | Remand and sentenced persons in prison | 1997 | 83.0 of remand 81.0 in prison | 20.1e | 4.03 | Not specified | 3,350 |
| Sahajian, 2012 (64) | France | Detained women | 2008 | 37.5f | 22.6g | 1.66 | 354 | 1,828 |
| Mir, 2015 (65) | Germany | Women entrants | 2012 | 80.7 | 24.4 | 150 | ||
| McCaffrey, 2012 (58) | Ireland | General health care study of the Irish prison population | 2000 | 100f | 29.6e | 3.38 | Not specified | 84 |
| Vera-Remartínez, 2013 (61) | Spain | Study in prison (n = 1,170) | 2013 | 58.2f | 22.3g | 2.61 | 55 | 4,521 |
Abbreviations: COPD, chronic obstructive pulmonary disease; TB, tuberculosis.
a Data on general population from the World Health Organization (34), unless otherwise stated.
b Data from World Prison Brief (8).
c There is a consistent pattern in which the prevalence of smoking is nearly always very high among studies of prison populations of mixed sex, ranging from 59.1% in Albania to 68.7% in Turkey to greater than 70% in the Netherlands and Greece and greater than 80% in England and Switzerland.
d The prevalence of smoking in the general community ranges from 25.9% in Turkey to 55.7% in Greece.
e Data from Ng (46).
f Where comparable data exist, men in prison have higher levels of smoking than women, as in France (70.3% vs. 37.5%) and Spain (71.0% vs. 58.2%). In Ireland, however, both sexes have very high levels of smoking: 91% for men and 100% for women in the prison.
g This trend of higher levels among men mirrors that in the general populations in France (30.4% vs. 22.6%) and Spain (29.9% vs. 22.3%).
Table 4.
Prevalence of Smoking in General Population and in Prison by Sex, the Americas, 2012–2016
| First Author, Year (Reference No.) | Location | Study Population | Year Data Collected | In Prison, % | General Population,a % | Fold Increase | No. of Incarcerated Study Subjects | Prison Populationb |
|---|---|---|---|---|---|---|---|---|
| Mixed Sex Studies | ||||||||
| Carbone, 2015 (95) | Brazil | TB study, in a prison | 2013 | 54.8c | 15.2 | 3.61 | 3,380 | 622,202 |
| Nogueira, 2012 (96) | Brazil | TB study, 1 jail, 1 prison | 2008 | 61.2c | 17.6c | 3.48 | 2,237 | 451,429 |
| Valença, 2015 (97) | Brazil | TB study, 1 prison | 2012–2013 | 68.4c | 15.2 | 4.5 | 301 | 622,202 |
| Aguilera, 2016 (98) | Chile | TB study | 2012–2013 | 68.5 | 40.1 | 1.71 | 336 | 45,501 |
| Studies of Men | ||||||||
| Estevan, 2013 (99) | Brazil | Study of TB rates | 2010 | 55.4d | 22.1d | 2.51 | 249 | 461,444 |
| Bautista-Arredondo, 2015 (100) | Mexico | Prison population | 2010 | 61.5 | 25.4 | 2.42 | 1,934 | 209,188 |
| Fernandez-Prada, 2013 (101) | Mexico | TB in HIV+ prison population | 2010 | 85.2 | Unknown tobacco prevalence in HIV+ men | 27 | 209,188 | |
| Studies of Women | ||||||||
| Zonta, 2012 (102) | Brazil | Cervical cancer in prison of 409 women | 2006 | 66.7d | 15.5d | 4.30 | 27 | 20,264 |
| dos Anjos Sde, 2013 (103) | Brazil | Cervical cancer | 2009 | 44.5d | 13.3d | 3.35 | 36 | 34,807 |
| Bautista-Arredondo, 2015 (100) | Mexico | 17,000 persons in prison at 4 Mexico City prisons | 2010 | 53.8 | 8.4 | 6.40 | 520 | 9,839 |
Abbreviations: HIV, human immunodeficiency virus; TB, tuberculosis.
a Data on general population from the World Health Organization (34), unless otherwise stated.
b Data from World Prison Brief data (8).
c Extensive data were located for Brazil, which consistently showed higher levels among general prison populations (54.8%, 61.2%, 68.4%) than general populations (17.6%).
d Brazilian data confirmed higher levels among female (66.7% and 44.5%) and male (55%) incarcerated subjects than females (15.5% and 13.3) and males in the community (22.1%).
The typical step-up, or fold increase in smoking prevalence for prisons relative to the general community ranged from 1.7 to more than 8-fold overall, and 1.3- to 7.3-fold for men and 1.7- to 62.6-fold for women. In prisons where smoking was not banned, prevalence was observed just once to be lower than that in the country as a whole (see Tables 1–4). We can make a prediction of how many smokers go through prison if we multiply the typical step-up by the percentage of smokers in the general population, and then multiply the product by the number of persons imprisoned worldwide. Conservatively, we estimate that overall the smoking prevalence doubles from community to prison. We know that 25% of men and 5% of women in the world smoke (1). By multiplication, then at least 50% of men and 10% of women in carceral settings are smokers. If the daily census of persons in prison is about 10 million (n = 9,673,000 men and n = 87,000 women) (8) and the typical yearly churn through a prison, or “institution throughput,” is 3 times the daily count (38), approximately 30 million persons overall (n = 29,020,000 men and n = 262,000 women) move through the criminal justice systems of the world each year, of whom 14,510,000 men and 26,000 women are smokers.
Bans
The Web Appendices 1 and 2 illustrate the effect of bans in the United States and Australia, respectively. In the United States, bans in the Federal Bureau of Prisons and most state prisons have meant that nearly all the 1.6 million persons serving felony sentences are prohibited from smoking. This has resulted in health improvements for prison health services, as analyzed by Binswanger et al. (14) and shown in Web Appendix 1. Most jails in the United States also operate as smoke-free facilities (35). The cost savings of bans there have not been systematically studied (35). Web Table 3 shows that bans are sporadic in Chinese prisons. Web Table 4 provides data on the bans on smoking for several other countries.
Interventions
Results of interventions published between 2012 and 2016 are shown in Table 5. Most persons imprisoned report that they want to quit but need help to do so (36, 41). Health education alone does not appear to help (42), nor does employing a “criminal justice tobacco control coordinator” (43). A randomized trial in Rhode Island demonstrated that in-prison delivery of motivational interviewing and cognitive behavioral therapy resulted in a significant improvement in smoking cessation that persisted for at least 6 months after release (24, 44). In an Australian prison trial, quit rates with cognitive behavioral therapy were similar to results achieved in the community, and adding a tricyclic antidepressant did not enhance quit rates (28). Even with published evidence that behavioral interventions work to reduce smoking in prison, correctional systems have been slow to adopt this preventive health tool. About half of the studies examined nicotine replacement therapy (Table 5).
Table 5.
Summary of Smoking Cessation Interventions Published Between 2012 and 2016a
| First Author, Year (Reference No.) | Intervention | Trial Design | Cessation Measurement | Timing of Measurement | Strength of Triala | Outcome: Change in Behavior |
|---|---|---|---|---|---|---|
| Akbar, 2012 (42) | Oral health education | Pre/Post | Self-report | In facility | Weak | No change |
| Etter, 2012 (104) | Counseling, NRT | Pre/Post | Self-report | In facility | Weak | No change |
| Makris, 2012 (27) | Varenicline + counseling | Pre/Post | Self-report plus biological | In facility | Weak | 30.7% abstinent at 3 months; 20.2% at 1 year |
| Clarke, 2013 (25), 2011 (44), 2015 (105) | CBT, MI | RCT | Biological | After release | Strong | 7-day point abstinence, 3-week follow-up, 35% (intervention) and 7% (control); 3-month follow-up, 12% (intervention) and 2% (control). |
| Richmond, 2013 (28) | CBT + NRT, with nortriptyline or placebo | RCT | Self-report plus biological | In facility | Strong | No effect of added nortriptylineContinuous abstinence at 3 months (23.8% treatment vs. 16.4% control); 6 months (17.5% vs. 12.3%); 12 months (11.7% vs. 11.9%) |
| Naik, 2014 (24) | MI | RCT | Self-report plus biological | In facility | Moderate | At 6 months, 16% in intervention stopped smoking, reduction in CO level |
| Jalali, 2015 (106) | MI + NRT | RCT | Self-report plus biological | In facility | Strong | 90-day follow-up. Significant reductions in CO, CPD, and Fagerstrom score in MI only and MI-NRT groups between pre- and post-tests and pre-test and follow-up. No differences between post-test and follow-up. |
| Turan, 2016 (107) | NRT, varenicline, bupropion | Pre/Post | Self-report | In facility | Weak | 30-day follow-up, 22.5% reported some reduction in smoking. |
Abbreviations: CBT, cognitive-based therapy; CO, carbon monoxide; CPD, cigarettes per day; MI, motivational interviewing; NRT, nicotine replacement therapy; Pre/Post, preintervention and postintervention; RCT, randomized clinical trial.
a Adapted from de Andrade and Kinner (37), with permission from BMJ Publishing Group Ltd. Copyright 2017.
Potential effect, globally, of decreasing smoking
Worldwide, with about 15 million smokers in prison at least part of the year and 5 million confined at any given point in time, cessation interventions delivered in the correctional setting have the potential to reach many bypassed by traditional outreach. Behavioral interventions in prisons are replicable even in middle-income countires (45) and, if results of replication mirror results in initial studies, about 10% of participants may remain abstinent after release from prison. With 20 million individuals being released and returned to their communities, half of whom are smokers, in-prison programs could globally result in as many as 2 million fewer smokers resettling in communities around the world.
DISCUSSION
We systematically reviewed the data on the level of smoking in prisons and corresponding community settings, examined the implementation of bans on smoking in prison, and reported on postrelease relapse to smoking. In addition, we studied the range of options for decreasing smoking in the custodial environment and reviewed the health effects of bans and interventions. By including “tuberculosis” as a search term, our literature search yielded more articles than in previous reviews. By reviewing several non-US databases, we report on a greater portion of the world’s literature on smoking in prisons. We calculated how many people would stop smoking if every correctional facility in the world offered behavioral, pharmacologic, or a combination of interventions for smoking cessation.
We have findings from 50 countries, which represent 73.5% of all incarcerated persons in the world (8). In 35 of 36 of nations (97%) with published prevalence data, smoking by incarcerated people exceeded community rates 1.04- to 62.6-fold. Only in Chinese men’s prisons were rates not consistently higher, but China has been experiencing a tremendous increase in smoking in the general male population since 2006 (46). In a study of Chinese citizens entering a methadone maintenance program after failing treatment in compulsory drug rehabilitation centers, researchers reported 99% had ever smoked and 89% currently used tobacco (47).
About one-fifth of the data on smoking rates came from tuberculosis studies in which smoking prevalence was an ancillary finding: Smoking likely heightens risk for tuberculosis disease (48, 49). Public health officials understand how prisons serve as incubators for tuberculosis and how disease control depends on focusing national control efforts in prisons. The overall health of individuals in prison, including the presence of noncommunicable disease (e.g., cardiovascular disease; cancer associated with smoking), may be less of a priority for these officials and are not the prime reason for these prison studies.
Overall, we found high levels of smoking among people who entered or were held in prisons, and those levels were higher than in the corresponding communities. This finding is to be expected given the overrepresentation in prisons and jails of vulnerable groups who have high levels of drug use in general and of smoking in particular. In many countries, incarcerated individuals could be missed by traditional public health interventions to reduce smoking or have less access to smoking cessation interventions. This marginalized group could constitute a hidden population difficult to access for prevention and treatment.. These findings underscore the critical importance of evidence-based treatment for substance use disorders, including smoking cessation, in prison settings. With an estimated 30 million people passing through prisons globally each year (38), failure to bring evidence-based treatment to scale in prison settings, particularly those where the prevalence of smoking is high, will have a substantial and measurable negative effect on public health.
Nevertheless, instead of providing treatment, the more common response by prison authorities has been the introduction of bans on smoking. Typically, these have been implemented in stages; for example, bans initially may be applied to the incarcerated population and indoor spaces only and then expanded to include outdoor spaces and prison staff. It appears that only a complete ban throughout the correctional facility, enforced outdoors and indoors, for both staff and the people incarcerated, extinguishes smoking in the facility. However, there is no evidence that suppressing smoking during incarceration translates into smoking cessation after release. Indeed, in studies that examined smoking rates after release, researchers showed that in the absence of an intervention other than a smoking ban, smoking rapidly reverted to baseline levels after release (23, 50).
Smoking cessation interventions are effective in reducing smoking during incarceration (Table 5). Smoking cessation interventions in US facilities, beyond just imposing bans, date back over a decade, when, in a randomized clinical trial of a behavioral intervention and nicotine replacement therapy, tobacco cessation rates were comparable to community rates (5, 26). Nicotine replacement therapy is an effective intervention in the community, in prisons where cigarettes are permitted or illicitly available (26), or short-term in a jail with or without a smoking ban. Regrettably, nicotine replacement therapy products are not routinely available in prisons and when they are available for sale in prison commissaries, they are often exorbitantly priced (35).
If, indeed, smoking rates are elevated in prisons, then public health services would be wise to introduce tobacco cessation interventions in the prison setting. Treatment that has worked in community settings has been found to be effective in the setting of incarceration, allaying fears that interventions in prison would have to be fundamentally different. The question seems to be one of political will and feasibility to introduce smoking interventions into correctional settings. In a recent trial in the middle-income country of Nigeria, conducted more recently than during our study period of 2012–2016, researchers demonstrated that implementing a group-level intervention of cognitive behavioral therapy was feasible in its prison system (45), suggesting that feasibility concerns can be addressed in other countries and settings.
Limitations
Some studies had very small samples and some data were extracted from studies where smoking was not the primary outcome. Thus, the data presented cannot be assumed to be representative of each country’s prison population. Nevertheless, this is the first time, to our knowledge, that such an extensive review of smoking prevalence in prison has been undertaken. Moreover, the elevated prevalence of smoking among persons in prison highlights the need for more research in this area. There were insufficient data to determine a pattern of decreased smoking prevalence in those countries with prison smoking bans. Tracking changes in smoking prevalence over time, especially among prison entrants, will be especially important in the jurisdictions that have implemented smoking bans. Last, we did not assign a point person to record the screening process, which led to an inability to create a precise Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram.
Conclusions
More work is required to identify and overcome barriers to providing treatment in prison. It was beyond the scope of this review to consider what effects the bans had on the prevalence of smoking after release, but it would appear that virtually all formerly incarcerated persons resume smoking once released. Even though smoking bans provide a temporary break from smoking and exposure to secondhand smoke, they appear to be insufficient on their own to increase the proportion of former smokers after release. The challenge is to promote long-term cessation during incarceration and prevention of relapse after release into the community or at other facilities (e.g., halfway houses) that may not have smoking bans. Given efforts to promote reductions in the prevalence of smoking worldwide, neglecting the vulnerable populations hidden in prisons is an injustice and one that is likely to perpetuate health disparities.
Areas for future research include the assessment of the health and survival benefits of introducing smoking bans in prisons, for persons who dwell in prisons and for staff who work in those environments. The postrelease effects of evidence-based interventions for smoking cessation in prison settings worldwide need to be measured. The costs of tobacco bans are likely negligible and, although cost analysis research is lacking, the cost of delivering smoking cessation interventions is likely to be modest, relative to their benefit. Thorough cost analysis would inform policy makers how feasible delivering effective interventions can be (35).
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia (Anne C. Spaulding, Cynthia E. Chico, Nancy Morisseau, Ana Drobeniuc, Rebecca Fils-Aime, Junyu Chen); University of Alaska Anchorage, Anchorage, Alaska (Gloria D. Eldridge); Discipline of Addiction Medicine, Central Clinical School, University of Sydney, New South Wales, Australia (Carolyn Day); Department of the Attorney-General and Justice, Northern Territory Correctional Services, Darwin, Australia (Robyn Hopkins); and Program of International Research and Training, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, Australia (Xingzhong Jin, Kate A. Dolan).
We are grateful for the help provided by Shenita Peterson, of the Woodruff Health Sciences Library, Emory University. We also appreciate the assistance Ariana N. Gobaud provided with proofing the final document. We thank Dr. John May for the information on smoking in Caribbean prisons.
A.C.S. has received honoraria from Ogilvy CommonHealth Market Access, Health Advances LLC, and Rand Corporation; she has received grants through her institution from Gilead Sciences. The other authors report no conflicts.
REFERENCES
- 1. GBD 2015 Tobacco Collaborators Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Australian Institute of Health and Welfare 2008 Australia’s health 2008. Cat. no. AUS 99. Canberra, Australian Capital Territory, Australia: Australian Institute of Health and Welfare. https://www.aihw.gov.au/getmedia/106ff693-72d0-4fd5-98d9-24259254d77f/ah08.pdf.aspx?inline=true. Accessed July 15, 2017.
- 3. Australian Institute of Health and Welfare 2012 Australia’s health 2012. Australia’s health series no.13. Cat. no. AUS 156. Canberra, Australian Capital Territory, Australia: Australian Institute of Health and Welfare. https://www.aihw.gov.au/getmedia/5fd0fcfe-bac9-4a4c-8128-1152d0ae9d8d/14178.pdf.aspx?inline=true. Accessed July 15, 2017.
- 4. Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014;370(1):60–68. [DOI] [PubMed] [Google Scholar]
- 5. Passey M, Bonevski B. The importance of tobacco research focusing on marginalized groups. Addiction. 2014;109(7):1049–1051. [DOI] [PubMed] [Google Scholar]
- 6. Twyman L, Bonevski B, Paul C, et al. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kennedy SM, Sharapova SR, Beasley DD, et al. Cigarette smoking among inmates by race/ethnicity: impact of excluding African American young adult men from national prevalence estimates. Nicotine Tob Res. 2016;18(suppl 1):S73–S78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Prison Brief World prison brief data. http://www.prisonstudies.org/world-prison-brief-data. Accessed February 18, 2017.
- 9. Jamal A, King BA, Neff LJ, et al. Current cigarette smoking among adults – United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205–1211. [DOI] [PubMed] [Google Scholar]
- 10. So M, Lemon TL, Spaulding AC The lifetime prevalence of incarceration among men in the United States by race and educational level: implications for health? Presented at the 50th Annual Meeting of the Society of Epidemiologic Research, Seattle, Washington, June 20–23, 2017.
- 11. Centers for Disease Control Prevention QuickStats: cigarette smoking prevalence among adults aged 18 years who have ever spent 24 hours on the streets, in a shelter, or in a jail or prison, by sex—United States, 2004. MMWR Morb Mortal Wkly Rep. 2006;55:287. [Google Scholar]
- 12. Baybutt M, Ritter C, Stöver H. Chapter 16: Tobacco use in prison settings: a need for policy implementation In: Enggist S, Møller L, Galea G, et al., eds. Prisons and Health. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2014:138 http://www.euro.who.int/__data/assets/pdf_file/0005/249188/Prisons-and-Health.pdf. [Google Scholar]
- 13. Helling v. McKinney, 509 US, 25 (1993). [Google Scholar]
- 14. Binswanger IA, Carson EA, Krueger PM, et al. Prison tobacco control policies and deaths from smoking in United States prisons: population based retrospective analysis. BMJ. 2014;349:g4542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson WW, Bennett K, Flanagan TJ. Getting tough on prisoners: results from the National Corrections Executive Survey, 1995. Crime Delinq. 1997;43:24–41. [Google Scholar]
- 16. Thornley S, Dirks KN, Edwards R, et al. Indoor air pollution levels were halved as a result of a national tobacco ban in a New Zealand prison. Nicotine Tob Res. 2013;15(2):343–347. [DOI] [PubMed] [Google Scholar]
- 17. Butler TG, Yap L. Smoking bans in prison: time for a breather? Med J Aust. 2015;203(8):313. [DOI] [PubMed] [Google Scholar]
- 18. Araromi MA. Prisoners’ rights under the Nigerian law: legal pathways to progressive realization and protection. J Sust Dev Law Policy. 2015;6(1):169–198. [Google Scholar]
- 19. Department of Health and Prison Health Service Toolkit for Developing Smoking Cessation Services in Prisons London, UK: Department of Health; 2003. http://webarchive.nationalarchives.gov.uk/20120106110849/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4034484.pdf. Accessed April 7, 2018.
- 20. Akaji EA, Folaranmi N. Tobacco use and oral health of inmates in a Nigerian prison. Niger J Clin Pract. 2013;16(4):473–477. [DOI] [PubMed] [Google Scholar]
- 21. Gibson-Light M. Must work for food: the politics of nutrition and informal economy in an American prison. Paper presented at the 111th Annual Meeting of the American Sociological Association, Seattle, Washington, 2016.
- 22. Djachenko A, St. John W, Mitchell C. Smoking cessation in male prisoners: a literature review. Int J Prison Health. 2015;11(1):39–48. [DOI] [PubMed] [Google Scholar]
- 23. Lincoln T, Tuthill RW, Roberts CA, et al. Resumption of smoking after release from a tobacco-free correctional facility. J Correct Health Care. 2009;15(3):190–196. [DOI] [PubMed] [Google Scholar]
- 24. Naik S, Khanagar S, Kumar A, et al. Assessment of effectiveness of smoking cessation intervention among male prisoners in India: a randomized controlled trial. J Int Soc Prev Community Dent. 2014;4(suppl 2):S110–S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clarke JG, Stein LA, Martin RA, et al. Forced smoking abstinence: not enough for smoking cessation. JAMA Intern Med. 2013;173(9):789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cropsey K, Eldridge G, Weaver M, et al. Smoking cessation intervention for female prisoners: addressing an urgent public health need. Am J Public Health. 2008;98(10):1894–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Makris E, Gourgoulianis KI, Hatzoglou C. Prisoners and cigarettes or ‘imprisoned in cigarettes’? What helps prisoners quit smoking? BMC Public Health. 2012;12:508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Richmond R, Indig D, Butler T, et al. A randomized controlled trial of a smoking cessation intervention conducted among prisoners. Addiction. 2013;108(5):966–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stovold E, Beecher D, Foxlee R, et al. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Rev. 2014;3:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chan ED, Kinney WH, Honda JR, et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis (Edinb). 2014;94(6):544–550. [DOI] [PubMed] [Google Scholar]
- 32. Edge CL, King EJ, Dolan K, et al. Prisoners co-infected with tuberculosis and HIV: a systematic review. J Int AIDS Soc. 2016;19(1):20960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. World Health Organization. Tobacco control database for the WHO European region. http://data.euro.who.int/tobacco/. Accessed November 1, 2017.
- 34. World Health Organization WHO global report on trends in prevalence of tobacco smoking 2015. World Health Organization; 2015. http://apps.who.int/iris/bitstream/10665/156262/1/9789241564922_eng.pdf. Accessed January 29, 2018.
- 35. Kennedy SM, Davis SP, Thorne SL. Smoke-free policies in US prisons and jails: a review of the literature. Nicotine Tob Res. 2015;17(6):629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sweeting H, Hunt K. Evidence on Smoking and Smoking Restrictions in Prisons: A Scoping Review for the Scottish Prison Service’s Tobacco Strategy Group 2015. http://www.sphsu.mrc.ac.uk/op25-sps-literature-review-v2.pdf. Accessed January 25, 2018.
- 37. de Andrade D, Kinner SA. Systematic review of health and behavioural outcomes of smoking cessation interventions in prisons. Tob Control. 2017;26(5):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. United Nations Office on Drugs and Crime. Regional Office for South Asia Prevention of Spread of HIV Amongst Vulnerable Groups in South Asia 2008. https://www.unodc.org/pdf/india/our_work_sa_prisons.pdf. Accessed June 26, 2017.
- 39. Sieminska A, Jassem E, Konopa K. Prisoners’ attitudes towards cigarette smoking and smoking cessation: a questionnaire study in Poland. BMC Public Health. 2006;6:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Narkauskaite L, Juozulynas A, Mackiewicz Z, et al. The prevalence of psychotropic substance use and its influencing factors in Lithuanian penitentiaries. Med Sci Monit. 2007;13(3):CR131–CR135. [PubMed] [Google Scholar]
- 41. Carnie J, Broderick R Scottish Prison Service Prisoner Survey 2015. 2016. www.sps.gov.uk/Corporate/Publications/Publication-4565.aspx. Accessed July 5, 2017.
- 42. Akbar T, Turner S, Themessl-Huber M, et al. The health-promoting prison: can it improve oral health? An evaluation of an Oral Health Improvement Project for high-security prisoners. Int J Health Promot Educ. 2012;50(4):169–177. [Google Scholar]
- 43. Eadie D, MacAskill S, McKell J, et al. Barriers and facilitators to a criminal justice tobacco control coordinator: an innovative approach to supporting smoking cessation among offenders. Addiction. 2012;107(suppl 2):26–38. [DOI] [PubMed] [Google Scholar]
- 44. Clarke JG, Martin RA, Stein L, et al. Working Inside for Smoking Elimination (Project W.I.S.E.) study design and rationale to prevent return to smoking after release from a smoke free prison. BMC Public Health. 2011;11:767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Onyechi KC, Eseadi C, Umoke PC, et al. Effects of a group-focused cognitive behavioral health education program on cigarette smoking in a sample of Nigerian prisoners. Medicine (Baltimore). 2017;96(1):e5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. 2014;311(2):183–192. [DOI] [PubMed] [Google Scholar]
- 47. Li L, Sangthong R, Chongsuvivatwong V, et al. Lifetime multiple substance use pattern among heroin users before entering methadone maintenance treatment clinic in Yunnan, China. Drug Alcohol Rev. 2010;29(4):420–425. [DOI] [PubMed] [Google Scholar]
- 48. Lin HH, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med. 2007;4(1):e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bishwakarma R, Kinney WH, Honda JR, et al. Epidemiologic link between tuberculosis and cigarette/biomass smoke exposure: limitations despite the vast literature. Respirology. 2015;20(4):556–568. [DOI] [PubMed] [Google Scholar]
- 50. Pezzino G, Remington PL, Anderson H, et al. Impact of a smoke-free policy on prisoners in Wisconsin, United States. Tob Control. 1992;1(3):180–184. [Google Scholar]
- 51. Jaka D, Roshi E, Burazeri G. Prison health in transitional Albania. Med Arh. 2014;68(3):188–190. [PubMed] [Google Scholar]
- 52. Jacomet C, Guyot-Lénat A, Bonny C, et al. Addressing the challenges of chronic viral infections and addiction in prisons: the PRODEPIST study. Eur J Public Health. 2016;26(1):122–128. [DOI] [PubMed] [Google Scholar]
- 53. Ceelen M, Dorn T, Buster M, et al. Health-care issues and health-care use among detainees in police custody. J Forensic Leg Med. 2012;19(6):324–331. [DOI] [PubMed] [Google Scholar]
- 54. Turan O. Smoking status and the presence of chronic obstructive pulmonary disease in prison. J Addict Med. 2015;9(2):118–122. [DOI] [PubMed] [Google Scholar]
- 55. Singleton N, Farrell M, Meltzer H. Substance misuse among prisoners in England and Wales. Int Rev Psychiatry. 2003;15(1–2):150–152. [DOI] [PubMed] [Google Scholar]
- 56. Jayes LR, Ratschen E, Murray RL, et al. Second-hand smoke in four English prisons: an air quality monitoring study. BMC Public Health. 2016;16:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chariot P, Beaufrère A, Denis C, et al. Detainees in police custody in the Paris, France area: medical data and high-risk situations (a prospective study over 1 year). Int J Legal Med. 2014;128(5):853–860. [DOI] [PubMed] [Google Scholar]
- 58. McCaffrey M, Goodman P, Gavigan A, et al. Should any workplace be exempt from smoke-free law: the Irish experience. J Environ Public Health. 2012;2012:545483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mannocci A, Masala D, Mipatrini D, et al. The relationship between physical activity and quality of life in prisoners: a pilot study. J Prev Med Hyg. 2015;56(4):E172–E175. [PMC free article] [PubMed] [Google Scholar]
- 60. Pinto RJ, Fernandes AI, Mesquita C, et al. Childhood adversity among institutionalized male juvenile offenders and other high-risk groups without offense records in Portugal. Violence Vict. 2015;30(4):600–614. [DOI] [PubMed] [Google Scholar]
- 61. Vera-Remartínez EJ, Borraz-Fernández JR, Domínguez-Zamorano JA, et al. [Prevalence of chronic diseases and risk factors among the Spanish prison population]. Rev Esp Sanid Penit. 2014;16(2):38–47. [DOI] [PubMed] [Google Scholar]
- 62. Ritter C, Elger BS. Second-hand tobacco smoke in prison: tackling a public health matter through research. Public Health. 2013;127(2):119–124. [DOI] [PubMed] [Google Scholar]
- 63. Winetsky DE, Almukhamedov O, Pulatov D, et al. Prevalence, risk factors and social context of active pulmonary tuberculosis among prison inmates in Tajikistan. PLoS One. 2014;9(1):e86046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Sahajian F, Lamothe P, Fabry J, et al. Consumption of psychoactive substances among 535 women entering a Lyon prison (France) between June 2004 and December 2008. Rev Epidemiol Sante Publique. 2012;60(5):371–381. [DOI] [PubMed] [Google Scholar]
- 65. Mir J, Kastner S, Priebe S, et al. Treating substance abuse is not enough: comorbidities in consecutively admitted female prisoners. Addict Behav. 2015;46:25–30. [DOI] [PubMed] [Google Scholar]
- 66. Chen T. Epidemiological investigation and risk factors of dry eye among persons of the prison system. Anhui Med J. 2014;35(12):1718–1721. [Google Scholar]
- 67. Tiwari R, Megalamanegowdru J, Agrawal R, et al. Oral health in correctional facilities: a study on knowledge, attitude and practice of prisoners in central India. Chettinad Health City. 2014; 3(3):109–114. [Google Scholar]
- 68. Al-Darraji HA, Kamarulzaman A, Altice FL. Latent tuberculosis infection in a Malaysian prison: implications for a comprehensive integrated control program in prisons. BMC Public Health. 2014;14:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Margolis B, Al-Darraji HA, Wickersham JA, et al. Prevalence of tuberculosis symptoms and latent tuberculous infection among prisoners in northeastern Malaysia. Int J Tuberc Lung Dis. 2013;17(12):1538–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Muir S, Marshall B. Changes in health perceptions of male prisoners following a smoking cessation program. J Correct Health Care. 2016;22(3):247–256. [DOI] [PubMed] [Google Scholar]
- 71. Soomro NA, Channa NA, Amur SA, et al. Factors associated with delinquent behaviour of inmates at Naara jail Hyderabad, Pakistan. Rawal Med J. 2016;41(4):441–445. [Google Scholar]
- 72. Morishita F, Garfin AM, Lew W, et al. Bringing state-of-the-art diagnostics to vulnerable populations: the use of a mobile screening unit in active case finding for tuberculosis in Palawan, the Philippines. PLoS One. 2017;12(2):e0171310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Liu F. Investigation on Status Quo and Countermeasures of Chronic Diseases and Lifestyle in Prisoners in Xi’an. China Master’s Theses Full-text Database. 2015. http://cdmd.cnki.com.cn/Article/CDMD-90032-1015961373.htm. Accessed January 25, 2018.
- 74. Wang B, Gao H, Liu L, et al. The symptoms and influential factors of hyperlipidemia among prisoners in Nantong. Chin J Prev Control Chronic Dis. 2016;24(11):836–839. [Google Scholar]
- 75. Shi H, Qian D. Disease cognition and health behaviors among patients with hypertension in prison. J Nanjing Med Univ. 2015;15(1):31–34. [Google Scholar]
- 76. Torwane NA, Hongal S, Sahu RN, et al. Assessment of prevalence of tobacco consumption among psychiatric inmates residing in Central Jail, Bhopal, Madhya Pradesh, India: a cross-sectional survey. Ind Psychiatry J. 2013;22(2):161–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Chen ML, Yang KL, Chen HS, et al. Prevalences of betel nut chewing and cigarette smoking among male prisoners before their imprisonment in Taiwan. J Dent Sci. 2012;7(2):165–170. [Google Scholar]
- 78. Li YF, Sung FC, Tsai MH, et al. Interactions between cigarette smoking and polymorphisms of xenobiotic-metabolizing genes: the risk of oral leukoplakia. Dis Markers. 2013;34(4):247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Khan TM, Hussain H, Khan G, et al. Incidence of depression among incarcerated woman in central prison, Peshawar, Pakistan. Eur J Gen Med. 2012;9(1):33–38. [Google Scholar]
- 80. Liu F, Hua Y, Yan S, et al. Investigation of the health status and quality of life of the female prisoners in Shanxi province. Med Soc. 2015;28(5):67–70. [Google Scholar]
- 81. Kwabla MP, Ameme D, Nortey P. Pulmonary tuberculosis and its risk factors among inmates of a Ghanaian prison. Int J Trop Dis Health. 2015;9(3):1–10. [Google Scholar]
- 82. Mamani M, Mahmudian H, Majzoobi MM, et al. Prevalence and incidence rates of latent tuberculous infection in a large prison in Iran. Int J Tuberc Lung Dis. 2016;20(8):1072–1077. [DOI] [PubMed] [Google Scholar]
- 83. Khajedaluee M, Babaei A, Vakili R, et al. Sero-prevalence of bloodborne tumor viruses (HCV, HBV, HTLV-I and KSHV Infections) and related risk factors among prisoners in Razavi Khorasan Province, Iran, in 2008. Hepat Mon. 2016;16(12):e31541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mor Z, Weinstein O, Tischler-Aurkin D, et al. The yield of tuberculosis screening of undocumented migrants from the Horn of Africa based on chest radiography. Isr Med Assoc J. 2015;17(1):11–13. [PubMed] [Google Scholar]
- 85. Kinyanjui DW, Atwoli L. Substance use among inmates at the Eldoret prison in Western Kenya. BMC Psychiatry. 2013;13:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mnisi T, Tumbo J, Govender I. Factors associated with pulmonary tuberculosis outcomes among inmates in Potchefstroom Prison in North West province. South Afr J Epidemiol Infect. 2013;28(2):96–101. http://www.sajei.co.za/index.php/SAJEI/article/view/490/709 [Google Scholar]
- 87. Ekouevi DK, D’almeida S, Salou M, et al. HIV seroprevalence among inmates in Togo. Med Mal Infect. 2013;43(7):279–285. [DOI] [PubMed] [Google Scholar]
- 88. Owokuhaisa J, Thokerunga E, Bazira J. Prevalence of pulmonary tuberculosis among prison inmates at Mbarara central prison, South Western Uganda. Adv Res. 2014;2(11):618–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Fuge TG, Ayanto SY. Prevalence of smear positive pulmonary tuberculosis and associated risk factors among prisoners in Hadiya Zone prison, Southern Ethiopia. BMC Res Notes. 2016;9:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Jaquet A, Wandeler G, Tine J, et al. HIV infection, viral hepatitis and liver fibrosis among prison inmates in West Africa. BMC Infect Dis. 2016;16:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Telisinghe L, Fielding KL, Malden JL, et al. High tuberculosis prevalence in a South African prison: the need for routine tuberculosis screening. PLoS One. 2014;9(1):e87262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Nyasulu P, Mogoere S, Umanah T, et al. Determinants of pulmonary tuberculosis among inmates at Mangaung maximum correctional facility in Bloemfontein, South Africa. Tuberc Res Treat. 2015;2015:752709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Abera SF, Adane K. Burden and determinants of smoking among prisoners with respiratory tract infection: a cross-sectional study of nine major prison setups in Northern Ethiopia. PLoS One. 2016;11(12):e0168941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Fageeh WM. Sexual behavior and knowledge of human immunodeficiency virus/aids and sexually transmitted infections among women inmates of Briman Prison, Jeddah, Saudi Arabia. BMC Infect Dis. 2014;14:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Carbone Ada S, Paião DS, Sgarbi RV, et al. Active and latent tuberculosis in Brazilian correctional facilities: a cross-sectional study. BMC Infect Dis. 2015;15:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Nogueira PA, Abrahão RM, Galesi VM. Tuberculosis and latent tuberculosis in prison inmates. Rev Saude Publica. 2012;46(1):119–127. [DOI] [PubMed] [Google Scholar]
- 97. Valença MS, Scaini JL, Abileira FS, et al. Prevalence of tuberculosis in prisons: risk factors and molecular epidemiology. Int J Tuberc Lung Dis. 2015;19(10):1182–1187. [DOI] [PubMed] [Google Scholar]
- 98. Aguilera XP, González C, Nájera-De Ferrari M, et al. Tuberculosis in prisoners and their contacts in Chile: estimating incidence and latent infection. Int J Tuberc Lung Dis. 2016;20(1):63–70. [DOI] [PubMed] [Google Scholar]
- 99. Estevan AO, Oliveira SM, Croda J. Active and latent tuberculosis in prisoners in the Central-West Region of Brazil. Rev Soc Bras Med Trop. 2013;46(4):515–518. [DOI] [PubMed] [Google Scholar]
- 100. Bautista-Arredondo S, González A, Servan-Mori E, et al. A cross-sectional study of prisoners in Mexico City comparing prevalence of transmissible infections and chronic diseases with that in the general population. PLoS One. 2015;10(7):e0131718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Fernández-Prada M, Romero BM, Martínez-Diz S. [Regarding “Active tuberculosis in a cohort of HIV-infected inmates in a prison in Mexico City: epidemiological and clinical characteristics”]. Salud Publica Mex. 2013;55(4):365–366. [PubMed] [Google Scholar]
- 102. Zonta MA, Monteiro J, Santos G Jr, et al. Oral infection by the human papilloma virus in women with cervical lesions at a prison in São Paulo, Brazil. Braz J Otorhinolaryngol. 2012;78(2):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. dos Anjos Sde J, Ribeiro SG, Lessa PR, et al. [Risk factors for cancer of the cervix in women prisoners]. Rev Bras Enferm. 2013;66(4):508–513. [DOI] [PubMed] [Google Scholar]
- 104. Etter JF, Ritter C, Christie DH, et al. Implementation and impact of anti-smoking interventions in three prisons in the absence of appropriate legislation. Prev Med. 2012;55(5):475–481. [DOI] [PubMed] [Google Scholar]
- 105. Clarke JG, Martin SA, Martin RA, et al. Changes in smoking-related symptoms during enforced abstinence of incarceration. J Health Care Poor Underserved. 2015;26(1):106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Jalali F, Afshari R, Babaei A, et al. Comparing motivational interviewing-based treatment and its combination with nicotine replacement therapy on smoking cessation in prisoners: a randomized controlled clinical trial. Electron Physician. 2015;7(6):1318–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Turan O, Turan PA. Smoking-related behaviors and effectiveness of smoking cessation therapy among prisoners and prison staff. Respir Care. 2016;61(4):434–438. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.