Abstract
Background
Although there have been great advances in mechanisms and therapeutic methods of prostate cancer, the mortality rate of prostate cancer remains high. The castration-resistant prostate cancer (CRPC), which develops from hormone-sensitive prostate cancer, foreshadows a more dismal outcome. Concomitant with the researches in the mechanism of CRPC and therapy for CRPC, more and more landmark progress has been made in recent years.
Methods
A number of clinical and experimental studies were reviewed to indicate the novel advancement in the progressive mechanism and therapy of CRPC.
Results
The androgen receptor (AR) is still a vital driver in the progression of CRPC, while other multiple mechanisms also contribute to this progression, such as tumor immunity, cancer stem cells, epithelial–mesenchymal transition and DNA repair disorder. In terms of the therapeutic methods of CRPC, chemotherapy with drugs, such as docetaxel, has been the first-line therapy for CRPC for many years. Besides, newer agents, which target some of the above mechanisms, show additional overall survival benefits for CRPC patients. These therapies include drugs targeting the androgen axis pathway (androgen synthesis, androgen receptor splice variants, coactivators of AR and so on), PI3K-AKT pathway, WNT pathway, DNA repair, rearrangement of ETS gene, novel chemotherapy and immunotherapy, bone metastasis therapy and so on. Understanding these novel findings on the mechanisms of CRPC and the latest potential CRPC therapies will direct us for further exploration of CRPC.
Conclusion
Through comprehensive consideration, the predominant mechanism of CRPC might be the AR signal axis concomitant with tumor microenvironment, stress, immunity, tumor microenvironment and so on. For CRPC therapy, targeting the AR axis pathway and chemotherapy are the first-line treatments at present. However, with the advancements in CRPC therapy made by the researchers, other novel potential methods will occupy more and more important position in the treatment of CRPC, especially the therapies targeting the tumor microenviroment, tumor immunity and DNA repair and so on.
Keywords: CRPC, androgen receptor, tumor immunity, mechanism, therapy
Introduction
Prostate cancer, which has the highest incidence among male malignancies in European and American countries, seriously threatens human health and affects the patients’ life quality.1 According to the statistics, the incidence and mortality rates of prostate cancer have been increasing every year with the rapid increase in Chinese aging society. Specifically, the castration-resistant prostate cancer (CRPC), which develops from hormone-sensitive prostate cancer, has a much higher mortality rate compared with prostate cancer.2
The clinical prognosis of CRPC patients is still unsatisfactory despite the fact that several important mechanisms and therapy advancements of CRPC have been reported. New drugs such as docetaxel, abiraterone and enzalutamide that could delay, to a certain extent, the development of CRPC are still the main therapy agents for CRPC in clinical practice.3 In recent years, numerous progressive mechanisms and therapeutic targets of CRPC have been found due to the efforts of the researchers. In this paper, we will review the novel research advancements of the progressive mechanisms and therapy in CRPC.
The progressive mechanisms of CRPC
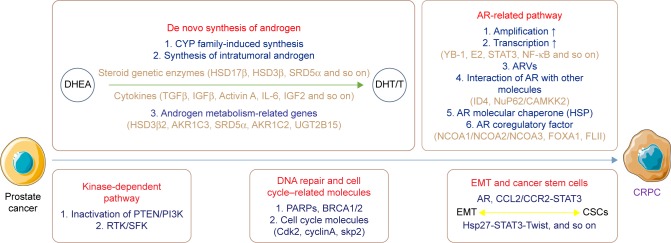
At present, gene alteration in the androgen axis and the kinase-dependent signal pathways are the most important mechanisms of CRPC genesis and development. However, accumulated evidences have indicated that tumor immunity, cancer stem cells (CSCs), epithelial–mesenchymal transition (EMT), DNA repairing disorder and other mechanisms might also participate in the progress of CRPC (Figure 1).
Figure 1.
Main progressive mechanisms of CRPC.
Abbreviations: AR, androgen receptor; ARVs, AR splice variants; CRPC, castration-resistant prostate cancer; CSCs, cancer stem cells; CYP, cytochrome P450; DHEA, dehydroepiandrosterone; DHT, dihydrotestosterone; EMT, epithelial–mesenchymal transition; HSP, heat shock protein; T, testosterone; HSP, heat shock protein.
De novo synthesis of androgen
The levels of intratumoral androgen in some CRPC patients were higher than in the primary prostate cancer patients, although serum testosterone (T) was at the castration level (<1.7 nmol/L) in these CRPC patients.4 According to the recent research, the mechanisms of de novo synthesis of androgen are discussed next.
Cytochrome P450 family-induced synthesis
The synthesis of T and dihydrotestosterone depends on the cytochrome P450 (CYP) family. CYP17, a member of the CYP family, has been proved to play a vital role in CRPC. Abiraterone acetate, one of the most common medicines for CRPC, is a kind of inhibitor of CYP17 and has been proved to improve the prognosis of CRPC patients.5
The synthesis of intratumoral androgen
According to previous researches, the levels of T and dihydrotestosterone are mainly dependent on the synthesis of intratumoral androgen, which is based on the conversion of dehydroepiandrosterone in the prostate cancer tissues after androgen deprivation therapy (ADT). This kind of intratumoral androgen synthesis mostly relies on some steroidogenic enzymes such as hydroxysteroid dehydrogenase (HSD)17β, HSD3β and steroid-5α-reductase.6
The activities of steroidogenic enzymes are also correlated with the expression of some other cytokines. Transforming growth factor beta could regulate the synthesis of the intratumoral androgen by upregulating HSD3β and downregulating HSD17β; insulin-like growth factor (IGF)-β could promote the synthesis of intratumoral androgen by increasing the expression of CYP17, AKR1C3 and HSD17β, so as to improve the development of CRPC.7 Moreover, activin A, interleukin (IL)-6 and IGF2 could also regulate the activities of the steroidogenic enzymes.8–10
Recently, it was indicated that arachidonic acid could induce the synthesis of StAR, which is bound to hormone-sensitive lipase and transforms the free cholesterol into androgen in the steroid synthesis-related cells.11
Elevation of the expression level of androgen metabolism–related genes
The upregulation of the expression level of the androgen metabolism–related genes, such as HSD3β2, AKR1C3, SRD5α, AKR1C2 and UGT2B15, also plays an important role in the development of CRPC.12
The regulatory effect of tumor microenvironment in CRPC
Recent studies have demonstrated that the synthesis of intratumoral androgen is related to the tumor microenvironment to a certain extent. The expression levels of steroidogenesis enzymes in the stromal cells are much higher in the CRPC cells. Meanwhile, the activity of prostate specific antigen (PSA) promoter, which is induced by dehydroepiandrosterone through androgen receptor (AR) activation in CRPC cells, could also be enhanced by prostate stromal cells.13 Besides, the anti-angiogenesis effect induced by vascular endothelial growth factor also plays a vital role in the progress of CRPC, while the vascular endothelial growth factor–targeted therapy was suggested to be useful for CRPC according to a study.14
The adaptive variation of AR-related pathway
During the progress of CRPC, the adaptive variation of AR-related pathway plays a vital role and the variation mainly focuses on the following parts.
The amplification of AR gene
The depletion of AR ligands could lead to the amplification of AR gene via feedback regulation.15 The overexpression and the importance of AR signaling in androgen-independent prostate cancer have been proved by reports.16,17 The amplification of AR gene could directly increase the expression level of AR and accelerate the development of CRPC. According to studies, glucocorticoid receptor could regulate some of AR targets in CRPC cells, and endostatin could inhibit glucocorticoid receptor–induced resistance upon AR antagonism.18,19
The transcription activity of AR gene
The regulation of AR transcription via cytokine plays an important role in the development of CRPC. YB-1 protein could combine with the Y-box domain in AR promoter and regulate the transcription of AR gene.20 The estrogen E2 could enhance the expression of SOX4, which is a member of the AR transcription factors in CRPC cells.21 Besides, STAT3, NF-κB and NF-κB/p52 could also activate the transcription of AR and increase its expression level through different pathways.22–24
The mutation of AR gene
The mutation of ligand-binding domain (LBD) or co-effective areas in AR gene could decrease the specificity of the combination between AR and its ligands, while the mutation of F876L region in AR gene has been demonstrated to be correlated with enzalutamide resistance in CRPC.25 Furthermore, the generation of AR splice variants (ARVs) is reported to play an important role in the development of CRPC, especially the AR-V7, which is transferred from AR due to a deficiency of LBD ligand. The expression of AR-V7 could activate the androgen synthesis–related genes and promote the progression of CRPC.26
The interactions between AR and other molecules
Besides the above signal pathways, the activity of AR is also correlated with some other molecules. The inactivation of inhibitor of differentiation 4 could activate the AR and promote CRPC.27 Nucleoporin62 and calcium/calmodulin-dependent protein kinase kinase 2 could impact the activity and development of CRPC.28
The regulator effect of AR molecular chaperone
As a molecular chaperone of AR, the expression of heat shock proteins (HSPs), especially HSP27 and HSP90, could be induced by ADT. It was reported that the activation of HSP27 and HSP90 might contribute to the resistance of ADT.29
The modulation of AR co-regulatory factor
The implementation of AR function was also associated with some co-regulatory factors. The nuclear receptor coactivators (NCOAs)1, NCOA2 and NCOA3, which are the members of non-receptor tyrosine kinase (SRC) family and coactivators of AR, have attracted special attention of the researchers.30 Meanwhile, forkhead box A1 (FOXA1), another cofactor, could modulate the transcription of AR and regulate the development of CRPC via GAT 3A2 gene.31
A recent study demonstrated that the Flightless I Homolog, FLII, could activate as a kind of transcriptional co-regulatory factor of AR and suppress the development of CRPC by regulating the cellular localization of AR in prostate cancer cells and inhibiting the expression of AR. This study revealed that FLII might be an important therapy target of CRPC.32
The regulator effect of kinase-dependent pathway
The kinase-dependent signal pathway, which is modulated by AR axis during ADT, also plays a vital role in the development of CRPC. The inactivation of PTEN gene in CRPC patients could activate PI3K resulting in AR activation.33 In recent years, it was reported that the receptor tyrosine kinases and SRC family kinases could regulate the AR signal and the development of CRPC by inducing the phosphorylation of AR and inhibiting the expressions of co-regulatory factors of AR.34
Modulation of DNA repair genes and cell cycle–related molecules
Mutation of DNA repair genes might play a vital role in CRPC.35 Poly (ADP-ribose) polymerase, which is a kind of DNA repair enzyme, could maintain the function of AR.36 Meanwhile, the mutation of BRCA1/2 gene, which is a member of DNA repair gene, was closely correlated with the development of CRPC.37 Furthermore, the androgen could inhibit the proliferation of AR-positive CRPC cells through the suppression of Cdk2, CyclinA and Skp2, which are typical members of cell cycle–related cytokines.38
The regulation of EMT and CSCs
In recent years, the importance of EMT and CSCs in the progressive CRPC has been demonstrated by various studies. The expression levels of E-cadherin, N-cadherin, Snail, Twist and other EMT markers are altered significantly during ADT. According to previous studies, ADT could trigger the appearance of EMT, which could further accelerate the development of CRPC.
CSC, a kind of potential malignant epithelial stem cell, might effect as an important regulatory target in CRPC. Some representative markers such as Nkx3.1, CD166, PSA−/LO, Nanog, Bmi-1 and SOX2 are shown to be correlated with the progress of CRPC on the grounds of recent studies.39,40
Furthermore, according to a recent study, the interaction between EMT and CSCs might also play a vital role in the recurrence and drug resistance of CRPC through AR, CCL2/CCR2-STAT3, Hsp27-STAT3-Twist and other pathways.41,42
The regulation of inflammation cytokines
The roles of inflammation factors in prostate cancer were proved by accumulating evidences during recent years (Table 1). IL-6 could induce the drug resistance of prostate cancer by activating SRC-1, regulating the expression of genes GRB2, SHC and JAK-1 and inhibiting the apoptosis of CRPC cells.43 IL-4, another important inflammation factor, could affect the coactivators of AR, such as CBP/P300 and NF-κB, and regulate the development of CRPC.44 IL-8, which could interact with NF-κB, is overexpressed in CRPC and could promote the angiogenesis and metastasis of CRPC through the SRC and FAK pathway.45 Furthermore, CXCR4, CXCR2/CXCR3, CXCR6 and CXCR7, which belong to the CXCR family, also play an important role in the development of CRPC via inflammation pathways according to recent studies.46–50 The roles of inflammation factors in cancers have been a hot issue in recent years, and a deeper and broader discussion is expected in future.
Table 1.
The regulation of inflammation factors in CRPC
| Cytokines | Signaling pathways | Target genes | Possible effect on cancer cells | References |
|---|---|---|---|---|
| IL-6 | Coactivator of AR | SRC-1/GRB2, SHC, JAK-1 | Inhibits apoptosis of the CRPC cells | 39 |
| IL-4 | Coactivator of AR | CBP/P300, NF-κB | Induces AR activation | 40 |
| IL-8 | Kinase-dependent pathway | NF-κB, SRC, FAK | Promotes angiogenesis and metastasis of CRPC | 41 |
| CXCR4 | IL-8 receptor | CXCL12/SDF-1 | Promotes proliferation, differentiation and metastasis | 42 |
| CXCR2/CXCR3 | / | / | Promotes proliferation and angiogenesis | 43 |
| CXCL16/CXCR6 | Akt pathway | IL-8, VEGF | Promotes selective metastasis to bone | 44 |
| CXCR7 | Akt pathway | IL-8/VEGF, EGFR | Promotes proliferation and metastasis | 45, 46 |
Note: “/” indicates unknown.
Abbreviations: AR, androgen receptor; CRPC, castration-resistant prostate cancer; IL, interleukin.
The regulation of ncRNAs in CRPC
The ncRNAs serve as a transcription regulator in CRPC (Table 2). It was known that miRNA could modulate the development of CRPC by regulating the cell cycle, cell differentiation and cell proliferation.51 Among the miRNAs, miR-1 and miR-206 could regulate the expression levels of glucose metabolism-related genes such as G6PD, TKT, PGD and GPD2 to affect the development of CRPC. Meanwhile, miR-185, miR-342, miR-17/92 and miR101 could regulate the development of CRPC through influencing SREBP, PPARA, COX-2 and other lipid metabolism-related pathways.52,53 Besides, miR-32, miR-148a, miR-99a, miR-2 and miR-221 also play an important role in CRPC via AR signals.54
Table 2.
The regulation of ncRNA in CRPC
| ncRNA | Names | Target gene | Possible effect on cancer cells | References |
|---|---|---|---|---|
| miRNA | miR-1 and miR-206 | G6PD, TKT, PGD and GPD2 | Regulates glucose metabolism | 48 |
| miR-185, miR-342, miR-17/92 and miR101 | SREBP, PPARA and COX-2 | Regulates lipid metabolism | 49 | |
| miR-32, miR-148a, miR-99a, miR-2 and miR-221 | AR | Activates AR signals | 50 | |
| lncRNA | PRNCR1, PCGEM1 and CTBP-AS | AR | Activates AR and promotes the transcription of AR | 51 |
| lncRNA-p21 | Warburg effect-related genes | Regulates the Warburg effect and HIF pathway | 52 | |
| HOTAIR | AR | Promotes the proliferation, invasion and metastasis of CRPC | 53 | |
| PCAT1 and ANRIL | PRC/AR | Modulates the expression of AR | 54, 55 |
Abbreviations: AR, androgen receptor; CRPC, castration-resistant prostate cancer; HIF, hypoxia-inducible factor; PRC, PGC-1-related coactivator.
According to studies, lncRNAs such as PRNCR1, PCGEM1 and CTBP-AS could promote the development of prostate cancer by activating and promoting the transcription of AR.55 lncRNA-p21 could promote the survival of prostate cancer cells through the Warburg effect and hypoxia-inducible factor pathway.56 In addition, HOTAIR, which is a member of lncRNA, could promote the proliferation, invasion and metastasis of CRPC via the modulation of epigenetics and transcription of AR.57 Similarly, the lncRNAs PCAT1 and ANRIL could modulate the expression of AR through interacting with the PGC-1-related coactivator family.58,59
The transformation of prostate cancer into neuroendocrine prostate cancer
Neuroendocrine prostate cancer (NEPC) is insensitive to the ADT. According to recent studies, the loss of RB1 and TP53 and the increase in MYCN and AURKA might be the reasons for the formation of NEPC.60 As a result, these genes related with the formation of NEPC are considered as a potential therapy target of NEPC.
The new advancement of CRPC therapy
Drugs targeting the androgen axis, cytotoxic drugs, immune drugs and drugs targeting bone metastasis (zoledronic acid, 233Ra and denosumab) are the main choices for clinical doctors for CRPC therapy.61,62 Moreover, the drugs targeting PI3K-AKT, WNT, DNA repair and other molecular signaling pathways were demonstrated to be essential in CRPC therapy, while the advances in prostate cancer immunity researches also indicated that immunotherapy might be indispensable in CRPC therapy in the future63,64 (Table 3).
Table 3.
Novel potential targets of CRPC therapy
| Possible targeting pathways | Targeting genes | Potential treatments | References |
|---|---|---|---|
| Androgen axis pathway | |||
| Inhibition of androgen synthesis | CYP17 | VT-464, TAK-700 | 64, 65 |
| Targeting HSP protein | HSP90/TCTP | Knockdown | 66 |
| ARVs | ARVs, calpain | ARN-509, niclosamide, ASC-J9, CUDC-101/TAS3681 | 29, 69–73 |
| AR-NTD | AR-NTD | EPI-001 | 75 |
| Antagonist of AR | AR | CB | 77 |
| Coactivators of AR | SRC | Dasatinib, saracatinib | 78 |
| Inhibitors of AR expression | AR | ENZ-4716 | 79 |
| PI3K-AKT pathways | PI3K-AKT | BEZ235, GDC0068 | 80 |
| WNT pathways | PORCN | 81 | |
| Targeting DNA repair | PARP | AZD-2281 | 82 |
| Targeting the rearrangement of ETS gene | TMPRSS2-ERG, FLI1 | DB1255, PLA2G7, YK-4-279 | 82, 84 |
| Chemotherapy | MMP2/9, WNT/β-actin | Saikosaponin-d, PEDF | 87, 88 |
| Immunotherapy | |||
| Vaccines | Peptide vaccine | PROSTVAC-VF | 90 |
| Nucleic acid vaccine | PTVG-HP | 91 | |
| Whole-cell vaccine | GVAX | 82 | |
| Dendritic cell vaccine | Sipulencel-T | 92 | |
| Immune checkpoints | CTLA-4 | Ipilimumab | 94 |
| PD-1 | Nivolumab, pembrotizumab | 95 | |
| MDSC | MDSC | Tasquinimod, lenalidomide | 96 |
| PSMA | PSMA | J591 | 97 |
| Bone metastasis | |||
| Chemotherapy | Osteoclast, RANKL | Bisphosphonates, denosumab | 98 |
| Radiotherapy | DNA of cancer cells | Radium-223 | 99 |
| ACK1/AR | AIM-100 | 100 | |
| Other potential drugs | |||
| Inhibitors of tyrosine kinase | IGF-1R | Figitumumab, cabozantinib | 101, 102 |
| Inhibitors of BET protein | BRD4 | GSK525762, OTX015 | 103, 104 |
| Inhibitors for NOTCH pathway | NOTCH | RO4929097 | 105 |
| Apoptosis and cell cycle pathway | Cell cycle | Escin | 107 |
Abbreviations: AR, androgen receptor; ARVs, AR splice variants; CRPC, castration-resistant prostate cancer; CTLA-4, cytotoxic T-lymphocyte-associated antigen-4; MDSC, myeloid-derived suppressor cell; NTD, N-terminal domain; PEDF, pigment epithelium-derived factor; PSMA, prostate-specific membrane antigen.
Targeting the androgen axis pathway
As a nuclear receptor related to steroidogenesis, AR is constituted by DNA-binding domain (DBD), LBD, N-terminal domain (NTD) and hinge region. The alteration in any component of AR structure might change the activity of AR and influence the development of CRPC.65 As a result, targeting the structural domain of AR is also a hotspot in CRPC.
Inhibition of androgen synthesis
The inhibitors of the key enzymes in androgen synthesis were indicated to have a satisfactory effect in clinical trials. The therapeutic effect of the combination of abiraterone acetate and prednisone for CRPC has been proved in clinical practice.66,67 Besides, VT-464, acting on CYP17, could suppress the proliferation of tumor and decrease the PSA level through inhibition of AR-axis.68 However, according to a clinical trial, TAK-700 (Orteronel), which also acts on CYP17, showed no significant effect on the overall survival time of CRPC patients.69
Although many new drugs might be effective for CRPC, administration of drugs that act upon the AR axis would still be the most essential and important method in CRPC clinical therapy for some time.
Targeting HSP protein
HSP protein is a very important target in CRPC therapy as mentioned before.29 The application of inhibitors targeting the HSP90 protein has been considered as a novel therapeutic strategy for CRPC patients with mutant AR.70 Knockdown of TCTP that interacts with HSP27 could suppress the survival and proliferation of CRPC cells.71 In recent years, some preclinical studies have indicated that silencing HSP27 or HSP90 could sensitize the prostate cancer cells to chemotherapy and radiation treatments, and several HSP protein inhibitors (tanespimycin, ganetespib, OGX-427) could delay castration resistance or prolong survival in CRPC.72–75 Thus, the combination of HSP blockage and other chemotherapy drugs could be a potential therapeutic strategy in patients with metastasis (m)CRPC.
Targeting the AR-LBD or ARVs
Enzalutamide and ARN-509 (apalutamide) show a great affinity for AR and are effective in CRPC that is resistant to bicalutamide.76 Recently, new drugs targeting AR-LBD and ARVs mainly focus on the following types.
Niclosamide, an antiparasitic drug approved by the US Food and Drug Administration was demonstrated to suppress the expression level of AR-V7, but not androgen receptor full length (AR-FL).77 It was also reported that niclosamide combined with current antiandrogen agents might possess a satisfactory effect in CRPC patients. Besides, drugs such as ASC-J9 (dimethylcurcumin) and inhibitors of calpain (CUDC-101 and TAS3681) might be useful for CRPC therapy by inhibiting ARVs, according to some studies.78–81
Targeting the AR-DBD
Some researchers believed that the alteration of AR-DBD might be correlated with the production of ARVs, and targeting AR-DBD could be a potential therapeutic strategy for CRPC.82
Targeting the AR-NTD
According to a study, the NTD of AR is responsible for AR transcriptional activity.83 As NTD is very important for the activity of all kinds of AR, targeting AR-NTD is expected to be used in CRPC. Several AR-NTD inhibitors (EPI-506, sintokamides) have been under preclinical experiments.82,84 As for EPI-506, it is the first agent that could suppress both canonical and variant-related AR signaling, and the ongoing Phase I/II study of EPI-506 (NCT02606123) will evaluate the benefit of EPI-506 in mCRPC patients. According to a study,82 EPI-001, the novel depressant of AR-NTD, showed a favorable effect on eliminating the castration resistance which was caused by ARVs.
Antagonist of AR
In clinic, bicalutamide, flutamide, nilutamide and other anti-androgen drugs are still considered as the first-line treatment for CRPC. However, the curative effects of these drugs are not everlasting, and the prostate cancer treated with ADT might advance to CRPC after 6 months.85
The core ligand of cyclobutane, which was used as the fourth-generation antiandrogen drug, might be of great importance in CRPC therapy through inhibition of nuclear translocation of AR.86
Targeting the coactivators of AR
According to a clinical trial, depressors of SRC kinase, such as dasatinib and saracatinib, showed a satisfactory effect in CRPC therapy by acting upon AR coactivators.87
Inhibiting AR expression
It might be possible to decrease the AR level by interfering with the expression of AR at the mRNA level. ENZ-4716 is a drug that confirms this hypothesis and is currently in Phase I clinical trial.88
Targeting the PI3K-AKT and WNT pathways
According to previous researches, both PI3K-AKT and WNT pathways play a vital role in the development of CRPC. BEZ235, one of the inhibitors of PI3K-mTOR, and GDC0068, one of the inhibitors of AKT, are both in Phase I clinical trials at present.89 Inhibition of WNT signal could potentiate the antitumor activity of the Plk1 inhibitor for CRPC.90 Besides, targeting PORCN (porcupine), which is essential for WNT pathway, might be a potential treatment method for CRPC.91
Targeting DNA repair
As mentioned earlier, mutations in DNA repair genes, such as BRCA2, homologous recombination, and nucleotide excision repair and mismatch repair, are common therapy targets in oncotherapy. For instance, inhibitors of poly (ADP-ribose) polymerase, especially olaparib (AZD-2281), showed satisfactory efficacy in CRPC patients according to the clinical trials.82
Targeting the rearrangement of ETS gene
ERG, ETV1, ETV6 and FLI1, which belong to the E twenty-six transcriptional factor family, are considered as the important oncogenes in different cancers.92 As one of the most important gene rearrangements in E twenty-six family, the gene rearrangement in TMPRSS2-ERG was deemed to be a potential target in CRPC therapy. Compounds targeting the rearrangement of TMPRSS2-ERG, such as DB1255 and PLA2G7, could regulate the biological function of prostate cells.93,94 Besides targeting the classical ERG pathway, YK-4-279 might be useful in inhibiting the proliferation and survival of CRPC cells by suppressing the FLI1 gene.95
Chemotherapy for CRPC
Although the side effects of chemotherapy are inevitable, chemotherapy in CRPC is nonnegligible because it is perfectly capable of killing prostate cancer cells.
Taxanes and epothilones are the typical drugs targeting the microtubules, while docetaxel and cabazitaxel are classical taxane drugs used in CRPC,96 and pemetrexed could be used for CRPC under docetaxel-resistant condition.97 As a newer trend of CRPC chemotherapy, the effect of applying taxanes in an earlier hormone-naive clinical setting of prostate cancer has been proved by studies.98,99 Cabazitaxel, the next generation of taxane drugs, has been shown to be an effective antitumor agent in docetaxel resistance cell lines.100,101 In recent years, some reports indicate that the taxanes may have cross-resistance with enzalutamide and abiraterone. As a result, the application of enzalutamide in prostate cancer patients has only a modest effect following docetaxel treatment.102–104
Besides the drugs mentioned earlier, several novel chemotherapy drugs have appeared recently. Saikosaponin-d possesses therapeutic potential for CRPC by reversing EMT and inhibiting the expression of MMP2/9 and WNT/β-actin.105 Moreover, the expression of pigment epithelium-derived factor also could enhance the efficacy of low-dose chemotherapy and improve the prognosis in CRPC.106
Immunotherapy in CRPC
Although immunotherapy in CRPC is still in its initial stage, the prospect of immunotherapy has received more attention in recent decades. Immunotherapy might be of significant importance in both therapy and prevention of CRPC.107
Vaccines for prostate cancer
After the idea of tumor vaccine came up, much effort was put into this field. Up to now, the application of vaccines in prostate cancer has mainly focused on the following:
Peptide vaccine: PROSTVAC-VF is a kind of peptide vaccine using PSA as the target antigen and is integrated with avipoxvirus, vaccinia and TRICOM. PROSTVAC-VF could prolong the survival time of the CRPC patients with a satisfactory tolerance according to the clinical trials.108
Nucleic acid vaccine: Nucleic acid vaccine is a kind of vaccine that could express the related target antigen and induce the related immunoreaction. PTVG-HP is a typical nucleic acid vaccine, and its target antigen is prostatic acid phosphatase. According to reports, PTVG-HP could induce the related immunoreaction and has shown a potential usage for CRPC.109
Whole-cell vaccine (WCV): The WCV could induce multiple kinds of antibodies, but the application of WCV is limited because the immunogenicity of WCV is poor in general. For prostate cancer and CRPC, GVAX, which is modified with costimulators, was effective in Phase I and II clinical trials, but was unsatisfactory in Phase III clinical trial.110 Under this condition, the application of WCV in prostate cancer still needs more research.
Dendritic cell (DC) vaccine: As the most effective antigen-presenting cell, DC is the first choice for preparation of autogenous cell vaccine. For CRPC, Sipulencel-T is the representative of DC vaccine and is able to induce CD4 and CD8 contraposing prostate cancer cells.111 According to studies, Sipulencel-T could improve the prognosis of the CRPC patients as well.
Immune checkpoints in prostate cancer
In the immune system, the immune checkpoint is a kind of inhibitory signal pathway, which is important for maintaining self-tolerance and regulating the duration. For prostate cancer, targeting cytotoxic T-lymphocyte-associated antigen-4 and programmed death protein-1 is the most effective strategy for immune checkpoint-related therapies.112 Ipilimumab, which could block or inhibit the cytotoxic T-lymphocyte-associated antigen-4, might prolong the progression-free survival time of CRPC patients, according to clinical trials.113 Nivolumab and pembrotizumab represent the immune drugs targeting the programmed death protein-1, but the therapeutic effect of them is not obvious.114
Recently, tasquinimod and lenalidomide that target the myeloid-derived suppressor cell showed the antitumor ability by the regulation of immune system and inhibition of angiogenesis in CRPC.115
Targeting the prostate-specific membrane antigen (PSMA)
PSMA, which is upregulated after ADT, has received more attention in recent decades. J591 is a monoclonal antibody of PSMA and might decrease the PSA level and prolong the survival time of CRPC patients.116
The therapy of bone metastasis in CRPC
Bisphosphonates and denosumab, which are the typical drugs for bone metastasis, also show their effectiveness in CRPC by targeting the osteoclasts, while denosumab might inhibit the metastasis of CRPC through RANKL pathway.117
Besides chemotherapy, radiotherapy could improve the prognosis of CRPC patients with bone metastasis. Radium-223, a kind of alpha particle radiopharmaceutical, has been proved to be effective in bone metastasis patients and prognosis with low clinical risks.118 According to the reports, ACK1/AR pathway could induce the phosphorylation of AR, as well as the upregulation of ataxia-telangiectasia mutated and the regulation of DNA damage, to accelerate the resistance to radiotherapy. AIM-100, an inhibitor of ACK1, could improve the effect of radiotherapy in CRPC.119
Other drugs for CRPC
Inhibitors of tyrosine kinase
IGF-1R, a member of tyrosine kinase, could interact with MAPK, PI3K/AKT and other signaling pathways to modulate the development of CRPC. It has been reported that figitumumab, an antibody of IGF-1R, could decrease the expression level of PSA and AR.120 Cabozantinib, another oral tyrosine kinase inhibitor, has a significant effect on decreasing the PSA level and suppressing the development of CRPC.121
Inhibitors of BET protein
As mentioned before, BER protein plays a vital role in CRPC through the AR signal pathway. GSK525762, which is the first inhibitor for BRD4 in clinical trial, shows satisfactory therapeutic effects for CRPC patients, while the clinical therapeutic effect of another inhibitor for BRD4, OTX015, still needs to be confirmed by more researches in the future.122,123
Inhibitors for NOTCH pathway
According to the recent research, NOTCH pathway is correlated with the development of CRPC. A novel inhibitor for NOTCH, RO4929097, could suppress the development of CRPC and might be a potential therapeutic target for CRPC.124
Apoptosis and cell cycle pathway
Escin, a natural compound that is extracted from buckeye, has been used for anti-inflammation and detumescence for a long time.125 A latest study demonstrated that escin could suppress the proliferation and survival of CRPC cells by regulating cell cycle and inducing apoptosis.126
Conclusion
Concomitant with the researches in the mechanism of CRPC and therapy for CRPC, more breakthrough progress has been made. Through comprehensive consideration, the predominant mechanism of CRPC might be the AR signal axis concomitant with other carcinogenesis signals, stress, immunity, tumor microenvironment and so on. With the latest findings in tumor microenvironment, tumor immunity and tumor metabolism, these fields might play indispensable roles in CRPC. However, the interactions between the above mechanisms and the other novel potential mechanisms are still uncertain.
Meanwhile, the clinical guidelines that were established by the European Association of Urology or the American Urological Association are the authoritative references for making therapeutic strategy for CRPC in clinic up to now. With the guidance of clinical guidelines for CRPC, the specific state of each patient, the affordability of the patients and other factors also need to be considered when formulating the therapeutic strategy. Unfortunately, the therapeutic effect is not satisfactory in some CRPC patients nowadays. Therefore, novel and effective therapeutic strategy for CRPC patients is very necessary and exigent in clinic. We hold that the detection of vital gene of CRPC and the application of targeting drugs for CRPC might play an important part in future, while targeting the individual gene expression will bring big rewards for the therapeutic effect and avoid the side effect. Furthermore, the immunotherapy and tumor vaccine of CRPC might be the focus of research in CRPC therapy in future. Although there are still numerous unsolved difficulties in the research upon the mechanism and therapy of CRPC, we believe that great progress would be made with the efforts of researchers all over the world in the future.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No 81272560, 81672524 and 81672528) and the Program for New Century Excellent Talents in University from the Department of Education of China (NCET-08-0223).
Footnotes
Author contributions
KC contributed to designing this study. KSW and HLR contributed to the collection and analysis of data, discussion, and writing of the manuscript. TBX, DL, HMY and XPZ contributed to the correction of grammatical errors in this article. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Mathas S, Misteli T. The dangers of transcription. Cell. 2009;139(6):1047–1049. doi: 10.1016/j.cell.2009.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 3.Petrylak DP. Practical guide to the use of chemotherapy in castration resistant prostate cancer. Can J Urol. 2014;21(2 Supp 1):77–83. [PubMed] [Google Scholar]
- 4.Montgomery RB, Mostaghel EA, Vessella R, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 2008;68(11):4447–4454. doi: 10.1158/0008-5472.CAN-08-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fizazi K, Scher HI, Molina A, et al. COU-AA-301 Investigators Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13(10):983–992. doi: 10.1016/S1470-2045(12)70379-0. [DOI] [PubMed] [Google Scholar]
- 6.Labrie F, Luu-The V, Belanger A, et al. Is dehydroepiandrosterone a hormone? J Endocrinol. 2005;187(2):169–196. doi: 10.1677/joe.1.06264. [DOI] [PubMed] [Google Scholar]
- 7.Lubik AA, Gunter JH, Hollier BG, et al. IGF2 increases de novo steroidogenesis in prostate cancer cells. Endocr Relat Cancer. 2013;20(2):173–186. doi: 10.1530/ERC-12-0250. [DOI] [PubMed] [Google Scholar]
- 8.Hofland J, van Weerden WM, Steenbergen J, Dits NF, Jenster G, de Jong FH. Activin A stimulates AKR1C3 expression and growth in human prostate cancer. Endocrinology. 2012;153(12):5726–5734. doi: 10.1210/en.2011-2065. [DOI] [PubMed] [Google Scholar]
- 9.Chun JY, Nadiminty N, Dutt S, et al. Interleukin-6 regulates androgen synthesis in prostate cancer cells. Clin Cancer Res. 2009;15(15):4815–4822. doi: 10.1158/1078-0432.CCR-09-0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubik AA, Gunter JH, Hollier BG, et al. IGF2 increases de novo steroidogenesis in prostate cancer cells. Endocr Relat Cancer. 2013;20(2):173–186. doi: 10.1530/ERC-12-0250. [DOI] [PubMed] [Google Scholar]
- 11.Locke JA, Guns ES, Lehman ML, et al. Arachidonic acid activation of intratumoral steroid synthesis during prostate cancer progression to castration resistance. Prostate. 2010;70(3):239–251. doi: 10.1002/pros.21057. [DOI] [PubMed] [Google Scholar]
- 12.Stanbrough M, Bubley GJ, Ross K, et al. Increased expression of genes converting adrenal androgens to testosterone in androgen-independent prostate cancer. Cancer Res. 2006;66(5):2815–2825. doi: 10.1158/0008-5472.CAN-05-4000. [DOI] [PubMed] [Google Scholar]
- 13.Mizokami A, Koh E, Izumi K, et al. Prostate cancer stromal cells and LNCaP cells coordinately activate the androgen receptor through synthesis of testosterone and dihydrotestosterone from dehydroepiandrosterone. Endocr Relat Cancer. 2009;16(4):1139–1155. doi: 10.1677/ERC-09-0070. [DOI] [PubMed] [Google Scholar]
- 14.Kelly WK, Halabi S, Carducci M, et al. Randomized, double-blind, placebo-controlled phase III trial comparing docetaxel and prednisone with or without bevacizumab in men with metastatic castration-resistant prostate cancer: CALGB 90401. J Clin Oncol. 2012;30(13):1534–1540. doi: 10.1200/JCO.2011.39.4767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mathas S, Misteli T. The dangers of transcription. Cell. 2009;139(6):1047–1049. doi: 10.1016/j.cell.2009.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linja MJ, Savinainen KJ, Saramaki OR, Tammela TL, Vessella RL, Visakorpi T. Amplification and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer Res. 2001;61(9):3550–3555. [PubMed] [Google Scholar]
- 17.Haapala K, Kuukasjarvi T, Hyytinen E, Rantala I, Helin HJ, Koivisto PA. Androgen receptor amplification is associated with increased cell proliferation in prostate cancer. Hum Pathol. 2007;38(3):474–478. doi: 10.1016/j.humpath.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Lee JH, Kang M, Wang H, et al. Endostatin inhibits androgen- independent prostate cancer growth by suppressing nuclear receptor-mediated oxidative stress. FASEB J. 2017;31(4):1608–1619. doi: 10.1096/fj.201601178R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arora VK, Schenkein E, Murali R, et al. Glucocorticoid receptor confers resistance to antiandrogens by bypassing androgen receptor blockade. Cell. 2013;155(6):1309–1322. doi: 10.1016/j.cell.2013.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shiota M, Takeuchi A, Song Y, et al. Y-box binding protein-1 promotes castration-resistant prostate cancer growth via androgen receptor expression. Endocr Relat Cancer. 2011;18(4):505–517. doi: 10.1530/ERC-11-0017. [DOI] [PubMed] [Google Scholar]
- 21.Yang M, Wang J, Wang L, et al. Estrogen induces androgen-repressed SOX4 expression to promote progression of prostate cancer cells. Prostate. 2015;75(13):1363–1375. doi: 10.1002/pros.23017. [DOI] [PubMed] [Google Scholar]
- 22.De Miguel F, Lee SO, Onate SA, Gao AC. Stat3 enhances transactivation of steroid hormone receptors. Nucl Recept. 2003;1(1):3. doi: 10.1186/1478-1336-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin RJ, Lho Y, Connelly L, et al. The nuclear factor-kappaB pathway controls the progression of prostate cancer to androgen-independent growth. Cancer Res. 2008;68(16):6762–6769. doi: 10.1158/0008-5472.CAN-08-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nadiminty N, Lou W, Sun M, et al. Aberrant activation of the androgen receptor by NF-kappaB2/p52 in prostate cancer cells. Cancer Res. 2010;70(8):3309–3319. doi: 10.1158/0008-5472.CAN-09-3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balbas MD, Evans MJ, Hosfield DJ, et al. Overcoming mutation-based resistance to antiandrogens with rational drug design. Elife. 2013;2:e00499. doi: 10.7554/eLife.00499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dehm SM, Tindall DJ. Alternatively spliced androgen receptor variants. Endocr Relat Cancer. 2011;18(5):R183–R196. doi: 10.1530/ERC-11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joshi JB, Patel D, Morton DJ, et al. Inactivation of ID4 promotes a CRPC phenotype with constitutive AR activation through FKBP52. Mol Oncol. 2017;11(4):337–357. doi: 10.1002/1878-0261.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karacosta LG, Kuroski LA, Hofmann WA, et al. Nucleoporin 62 and Ca(2+)/calmodulin dependent kinase kinase 2 regulate androgen receptor activity in castrate resistant prostate cancer cells. Prostate. 2016;76(3):294–306. doi: 10.1002/pros.23121. [DOI] [PubMed] [Google Scholar]
- 29.Azad AA, Eigl BJ, Murray RN, Kollmannsberger C, Chi KN. Efficacy of enzalutamide following abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer patients. Eur Urol. 2015;67(1):23–29. doi: 10.1016/j.eururo.2014.06.045. [DOI] [PubMed] [Google Scholar]
- 30.Zhou HJ, Yan J, Luo W, et al. SRC-3 is required for prostate cancer cell proliferation and survival. Cancer Res. 2005;65(17):7976–7983. doi: 10.1158/0008-5472.CAN-04-4076. [DOI] [PubMed] [Google Scholar]
- 31.Jozwik KM, Carroll JS. Pioneer factors in hormone-dependent cancers. Nat Rev Cancer. 2012;12(6):381–385. doi: 10.1038/nrc3263. [DOI] [PubMed] [Google Scholar]
- 32.Wang T, Song W, Chen Y, et al. Flightless I homolog represses prostate cancer progression through targeting androgen receptor signaling. Clin Cancer Res. 2016;22(6):1531–1544. doi: 10.1158/1078-0432.CCR-15-1632. [DOI] [PubMed] [Google Scholar]
- 33.Wang S, Gao J, Lei Q, et al. Prostate-specific deletion of the murine Pten tumor suppressor gene leads to metastatic prostate cancer. Cancer Cell. 2003;4(3):209–221. doi: 10.1016/s1535-6108(03)00215-0. [DOI] [PubMed] [Google Scholar]
- 34.Gelman IH. Androgen receptor activation in castration-recurrent prostate cancer: the role of Src-family and Ack1 tyrosine kinases. Int J Biol Sci. 2014;10(6):620–626. doi: 10.7150/ijbs.8264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mateo J, Boysen G, Barbieri CE, et al. DNA repair in prostate cancer: biology and clinical implications. Eur Urol. 2017;71(3):417–425. doi: 10.1016/j.eururo.2016.08.037. [DOI] [PubMed] [Google Scholar]
- 36.Schiewer MJ, Goodwin JF, Han S, et al. Dual roles of PARP-1 promote cancer growth and progression. Cancer Discov. 2012;2(12):1134–1149. doi: 10.1158/2159-8290.CD-12-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kote-Jarai Z, Leongamornlert D, Saunders E, et al. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230–1234. doi: 10.1038/bjc.2011.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kokontis JM, Lin HP, Jiang SS, et al. Androgen suppresses the proliferation of androgen receptor-positive castration-resistant prostate cancer cells via inhibition of Cdk2, CyclinA, and Skp2. PLoS One. 2014;9(10):e109170. doi: 10.1371/journal.pone.0109170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levesque E, Huang SP, Audet-Walsh E, et al. Molecular markers in key steroidogenic pathways, circulating steroid levels, and prostate cancer progression. Clin Cancer Res. 2013;19(3):699–709. doi: 10.1158/1078-0432.CCR-12-2812. [DOI] [PubMed] [Google Scholar]
- 40.Mitsiades N, Sung CC, Schultz N, et al. Distinct patterns of dysregulated expression of enzymes involved in androgen synthesis and metabolism in metastatic prostate cancer tumors. Cancer Res. 2012;72(23):6142–6152. doi: 10.1158/0008-5472.CAN-12-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shiota M, Bishop JL, Nip KM, et al. Hsp27 regulates epithelial mesenchymal transition, metastasis, and circulating tumor cells in prostate cancer. Cancer Res. 2013;73(10):3109–3119. doi: 10.1158/0008-5472.CAN-12-3979. [DOI] [PubMed] [Google Scholar]
- 42.Izumi K, Fang LY, Mizokami A, et al. Targeting the androgen receptor with siRNA promotes prostate cancer metastasis through enhanced macrophage recruitment via CCL2/CCR2-induced STAT3 activation. Embo Mol Med. 2013;5(9):1383–1401. doi: 10.1002/emmm.201202367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karkera J, Steiner H, Li W, et al. The anti-interleukin-6 antibody siltuximab down-regulates genes implicated in tumorigenesis in prostate cancer patients from a phase I study. Prostate. 2011;71(13):1455–1465. doi: 10.1002/pros.21362. [DOI] [PubMed] [Google Scholar]
- 44.Lee SO, Lou W, Nadiminty N, Lin X, Gao AC. Requirement for NF-(kappa)B in interleukin-4-induced androgen receptor activation in prostate cancer cells. Prostate. 2005;64(2):160–167. doi: 10.1002/pros.20218. [DOI] [PubMed] [Google Scholar]
- 45.Waugh DJ, Wilson C. The interleukin-8 pathway in cancer. Clin Cancer Res. 2008;14(21):6735–6741. doi: 10.1158/1078-0432.CCR-07-4843. [DOI] [PubMed] [Google Scholar]
- 46.Taichman RS, Cooper C, Keller ET, Pienta KJ, Taichman NS, McCauley LK. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Res. 2002;62(6):1832–1837. [PubMed] [Google Scholar]
- 47.Shen H, Schuster R, Lu B, Waltz SE, Lentsch AB. Critical and opposing roles of the chemokine receptors CXCR2 and CXCR3 in prostate tumor growth. Prostate. 2006;66(16):1721–1728. doi: 10.1002/pros.20476. [DOI] [PubMed] [Google Scholar]
- 48.Wang J, Lu Y, Wang J, Koch AE, Zhang J, Taichman RS. CXCR6 induces prostate cancer progression by the AKT/mammalian target of rapamycin signaling pathway. Cancer Res. 2008;68(24):10367–10376. doi: 10.1158/0008-5472.CAN-08-2780. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 49.Singh RK, Lokeshwar BL. The IL-8-regulated chemokine receptor CXCR7 stimulates EGFR signaling to promote prostate cancer growth. Cancer Res. 2011;71(9):3268–3277. doi: 10.1158/0008-5472.CAN-10-2769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang J, Shiozawa Y, Wang J, et al. The role of CXCR7/RDC1 as a chemokine receptor for CXCL12/SDF-1 in prostate cancer. J Biol Chem. 2008;283(7):4283–4294. doi: 10.1074/jbc.M707465200. [DOI] [PubMed] [Google Scholar]
- 51.Pasquinelli AE. MicroRNAs and their targets: recognition, regulation and an emerging reciprocal relationship. Nat Rev Genet. 2012;13(4):271–282. doi: 10.1038/nrg3162. [DOI] [PubMed] [Google Scholar]
- 52.Singh A, Happel C, Manna SK, et al. Transcription factor NRF2 regulates miR-1 and miR-206 to drive tumorigenesis. J Clin Invest. 2013;123(7):2921–2934. doi: 10.1172/JCI66353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hiroki E, Akahira J, Suzuki F, et al. Changes in microRNA expression levels correlate with clinicopathological features and prognoses in endometrial serous adenocarcinomas. Cancer Sci. 2010;101(1):241–249. doi: 10.1111/j.1349-7006.2009.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jalava SE, Urbanucci A, Latonen L, et al. Androgen-regulated miR-32 targets BTG2 and is overexpressed in castration-resistant prostate cancer. Oncogene. 2012;31(41):4460–4471. doi: 10.1038/onc.2011.624. [DOI] [PubMed] [Google Scholar]
- 55.Yang L, Lin C, Jin C, et al. lncRNA-dependent mechanisms of androgen-receptor-regulated gene activation programs. Nature. 2013;500(7464):598–602. doi: 10.1038/nature12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang F, Zhang H, Mei Y, Wu M. Reciprocal regulation of HIF-1alpha and lincRNA-p21 modulates the Warburg effect. Mol Cell. 2014;53(1):88–100. doi: 10.1016/j.molcel.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Scaravilli M, Porkka KP, Brofeldt A, et al. MiR-1247-5p is overexpressed in castration resistant prostate cancer and targets MYCBP2. Prostate. 2015;75(8):798–805. doi: 10.1002/pros.22961. [DOI] [PubMed] [Google Scholar]
- 58.Prensner JR, Iyer MK, Balbin OA, et al. Transcriptome sequencing across a prostate cancer cohort identifies PCAT-1, an unannotated lincRNA implicated in disease progression. Nat Biotechnol. 2011;29(8):742–749. doi: 10.1038/nbt.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yap KL, Li S, Munoz-Cabello AM, et al. Molecular interplay of the noncoding RNA ANRIL and methylated histone H3 lysine 27 by polycomb CBX7 in transcriptional silencing of INK4a. Mol Cell. 2010;38(5):662–674. doi: 10.1016/j.molcel.2010.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beltran H, Rickman DS, Park K, et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. Cancer Discov. 2011;1(6):487–495. doi: 10.1158/2159-8290.CD-11-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arsov C, Winter C, Rabenalt R, Albers P. Current second-line treatment options for patients with castration resistant prostate cancer (CRPC) resistant to docetaxel. Urol Oncol. 2012;30(6):762–771. doi: 10.1016/j.urolonc.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 62.Ryan CJ, Saylor PJ, Everly JJ, Sartor O. Bone-targeting radiopharmaceuticals for the treatment of bone-metastatic castration-resistant prostate cancer: exploring the implications of new data. Oncologist. 2014;19(10):1012–1018. doi: 10.1634/theoncologist.2013-0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Massari F, Maines F, Modena A, et al. Castration resistant prostate cancer (CRPC): state of the art, perspectives and new challenges. Anticancer Agents Med Chem. 2013;13(6):872–886. doi: 10.2174/18715206113139990077. [DOI] [PubMed] [Google Scholar]
- 64.Suarez C, Morales-Barrera R, Ramos V, et al. Role of immunotherapy in castration-resistant prostate cancer (CRPC) BJU Int. 2014;113(3):367–375. doi: 10.1111/bju.12110. [DOI] [PubMed] [Google Scholar]
- 65.Dar JA, Eisermann K, Masoodi KZ, et al. N-terminal domain of the androgen receptor contains a region that can promote cytoplasmic localization. J Steroid Biochem Mol Biol. 2014;139:16–24. doi: 10.1016/j.jsbmb.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Narayanan S, Srinivas S, Feldman D. Androgen-glucocorticoid interactions in the era of novel prostate cancer therapy. Nat Rev Urol. 2016;13(1):47–60. doi: 10.1038/nrurol.2015.254. [DOI] [PubMed] [Google Scholar]
- 67.Ye D, Huang Y, Zhou F, et al. A phase 3, double-blind, randomized placebo-controlled efficacy and safety study of abiraterone acetate in chemotherapy-naïve patients with mCRPC in China, Malaysia, Thailand and Russia. Asian J Urol. 2017;4(2):75–85. doi: 10.1016/j.ajur.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Toren PJ, Kim S, Pham S, et al. Anticancer activity of a novel selective CYP17A1 inhibitor in preclinical models of castrate-resistant prostate cancer. Mol Cancer Ther. 2015;14(1):59–69. doi: 10.1158/1535-7163.MCT-14-0521. [DOI] [PubMed] [Google Scholar]
- 69.Fizazi K, Jones R, Oudard S, et al. Phase III, randomized, double-blind, multicenter trial comparing orteronel (TAK-700) plus prednisone with placebo plus prednisone in patients with metastatic castration-resistant prostate cancer that has progressed during or after docetaxel-based therapy: ELM-PC 5. J Clin Oncol. 2015;33(7):723–731. doi: 10.1200/JCO.2014.56.5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Solit DB, Scher HI, Rosen N. Hsp90 as a therapeutic target in prostate cancer. Semin Oncol. 2003;30(5):709–716. doi: 10.1016/s0093-7754(03)00346-4. [DOI] [PubMed] [Google Scholar]
- 71.Baylot V, Katsogiannou M, Andrieu C, et al. Targeting TCTP as a new therapeutic strategy in castration-resistant prostate cancer. Mol Ther. 2012;20(12):2244–2256. doi: 10.1038/mt.2012.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.O’Malley KJ, Langmann G, Ai J, Ramos-Garcia R, Vessella RL, Wang Z. Hsp90 inhibitor 17-AAG inhibits progression of LuCaP35 xenograft prostate tumors to castration resistance. Prostate. 2012;72(10):1117–1123. doi: 10.1002/pros.22458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.He S, Zhang C, Shafi AA, et al. Potent activity of the Hsp90 inhibitor ganetespib in prostate cancer cells irrespective of androgen receptor status or variant receptor expression. Int J Oncol. 2013;42(1):35–43. doi: 10.3892/ijo.2012.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zoubeidi A, Zardan A, Beraldi E, et al. Cooperative interactions between androgen receptor (AR) and heat-shock protein 27 facilitate AR transcriptional activity. Cancer Res. 2007;67(21):10455–10465. doi: 10.1158/0008-5472.CAN-07-2057. [DOI] [PubMed] [Google Scholar]
- 75.Ischia J, Saad F, Gleave M. The promise of heat shock protein inhibitors in the treatment of castration resistant prostate cancer. Curr Opin Urol. 2013;23(3):194–200. doi: 10.1097/MOU.0b013e32835e9f1a. [DOI] [PubMed] [Google Scholar]
- 76.Tran C, Ouk S, Clegg NJ, et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324(5928):787–790. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu C, Lou W, Zhu Y, et al. Niclosamide inhibits androgen receptor variants expression and overcomes enzalutamide resistance in castration-resistant prostate cancer. Clin Cancer Res. 2014;20(12):3198–3210. doi: 10.1158/1078-0432.CCR-13-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yamashita S, Lai KP, Chuang KL, et al. ASC-J9 suppresses castration-resistant prostate cancer growth through degradation of full-length and splice variant androgen receptors. Neoplasia. 2012;14(1):74–83. doi: 10.1593/neo.111436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Libertini SJ, Tepper CG, Rodriguez V, Asmuth DM, Kung HJ, Mudryj M. Evidence for calpain-mediated androgen receptor cleavage as a mechanism for androgen independence. Cancer Res. 2007;67(19):9001–9005. doi: 10.1158/0008-5472.CAN-07-1072. [DOI] [PubMed] [Google Scholar]
- 80.Sun H, Mediwala SN, Szafran AT, Mancini MA, Marcelli M. CUDC-101, a novel inhibitor of full-length Androgen Receptor (flAR) and Androgen Receptor Variant 7 (AR-V7) Activity: mechanism of action and in vivo efficacy. Horm Cancer. 2016;7(3):196–210. doi: 10.1007/s12672-016-0257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Teply BA, Antonarakis ES. Novel mechanism-based therapeutics for androgen axis blockade in castration-resistant prostate cancer. Curr Opin Endocrinol Diabetes Obes. 2016;23(3):279–290. doi: 10.1097/MED.0000000000000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andersen RJ, Mawji NR, Wang J, et al. Regression of castrate-recurrent prostate cancer by a small-molecule inhibitor of the amino-terminus domain of the androgen receptor. Cancer Cell. 2010;17(6):535–546. doi: 10.1016/j.ccr.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 83.Banuelos CA, Lal A, Tien AH, et al. Characterization of niphatenones that inhibit androgen receptor N-terminal domain. PLoS One. 2014;9(9):e107991. doi: 10.1371/journal.pone.0107991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sadar MD, Williams DE, Mawji NR, et al. Sintokamides A to E, chlorinated peptides from the sponge Dysidea sp. that inhibit transactivation of the N-terminus of the androgen receptor in prostate cancer cells. Org Lett. 2008;10(21):4947–4950. doi: 10.1021/ol802021w. [DOI] [PubMed] [Google Scholar]
- 85.Michels J. Enzalutamide versus bicalutamide in castration-resistant prostate cancer: the STRIVE trial-there is no significant reduction in death (Yet) J Clin Oncol. 2017;35(1):123. doi: 10.1200/JCO.2016.67.4630. [DOI] [PubMed] [Google Scholar]
- 86.Pollock JA, Wardell SE, Parent AA, et al. Inhibiting androgen receptor nuclear entry in castration-resistant prostate cancer. Nat Chem Biol. 2016;12(10):795–801. doi: 10.1038/nchembio.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yu EY, Wilding G, Posadas E, et al. Phase II study of dasatinib in patients with metastatic castration-resistant prostate cancer. Clin Cancer Res. 2009;15(23):7421–7428. doi: 10.1158/1078-0432.CCR-09-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bianchini D, Omlin A, Pezaro C, et al. First-in-human Phase I study of EZN-4176, a locked nucleic acid antisense oligonucleotide to exon 4 of the androgen receptor mRNA in patients with castration-resistant prostate cancer. Br J Cancer. 2013;109(10):2579–2586. doi: 10.1038/bjc.2013.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Carver BS, Chapinski C, Wongvipat J, et al. Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell. 2011;19(5):575–586. doi: 10.1016/j.ccr.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li J, Karki A, Hodges KB, et al. Cotargeting polo-like kinase 1 and the Wnt/beta-catenin signaling pathway in castration-resistant prostate cancer. Mol Cell Biol. 2015;35(24):4185–4198. doi: 10.1128/MCB.00825-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang LS, Lum L. Delivery of the porcupine inhibitor WNT974 in mice. Methods Mol Biol. 2016;1481:111–117. doi: 10.1007/978-1-4939-6393-5_12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hollenhorst PC, McIntosh LP, Graves BJ. Genomic and biochemical insights into the specificity of ETS transcription factors. Annu Rev Biochem. 2011;80:437–471. doi: 10.1146/annurev.biochem.79.081507.103945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nhili R, Peixoto P, Depauw S, et al. Targeting the DNA-binding activity of the human ERG transcription factor using new heterocyclic dithiophene diamidines. Nucleic Acids Res. 2013;41(1):125–138. doi: 10.1093/nar/gks971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vainio P, Gupta S, Ketola K, et al. Arachidonic acid pathway members PLA2G7, HPGD, EPHX2, and CYP4F8 identified as putative novel therapeutic targets in prostate cancer. Am J Pathol. 2011;178(2):525–536. doi: 10.1016/j.ajpath.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rahim S, Beauchamp EM, Kong Y, Brown ML, Toretsky JA, Uren A. YK-4-279 inhibits ERG and ETV1 mediated prostate cancer cell invasion. PLos One. 2011;6(4):e19343. doi: 10.1371/journal.pone.0019343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kim SJ, Kim SI. Current treatment strategies for castration-resistant prostate cancer. Korean J Urol. 2011;52(3):157–165. doi: 10.4111/kju.2011.52.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Caffo O, Fratino L, Barbieri R, et al. Pemetrexed as second-line chemotherapy for castration-resistant prostate cancer after docetaxel failure: results from a phase II study. Urol Oncol. 2013;31(2):180–186. doi: 10.1016/j.urolonc.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 98.Shiota M, Yokomizo A, Eto M. Taxane chemotherapy for hormone-naive prostate cancer with its expanding role as breakthrough strategy. Front Oncol. 2015;5:304. doi: 10.3389/fonc.2015.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Botrel TE, Clark O, Lima Pompeo AC, et al. Efficacy and safety of combined Androgen Deprivation Therapy (ADT) and docetaxel compared with ADT alone for metastatic hormone-naive prostate cancer: a systematic review and meta-analysis. PLoS One. 2016;11(6):e0157660. doi: 10.1371/journal.pone.0157660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mita AC, Denis LJ, Rowinsky EK, et al. Phase I and pharmacokinetic study of XRP6258 (RPR 116258A), a novel taxane, administered as a 1-hour infusion every 3 weeks in patients with advanced solid tumors. Clin Cancer Res. 2009;15(2):723–730. doi: 10.1158/1078-0432.CCR-08-0596. [DOI] [PubMed] [Google Scholar]
- 101.Yap TA, Pezaro CJ, de Bono JS. Cabazitaxel in metastatic castration-resistant prostate cancer. Expert Rev Anticancer Ther. 2012;12(9):1129–1136. doi: 10.1586/era.12.88. [DOI] [PubMed] [Google Scholar]
- 102.Darshan MS, Loftus MS, Thadani-Mulero M, et al. Taxane-induced blockade to nuclear accumulation of the androgen receptor predicts clinical responses in metastatic prostate cancer. Cancer Res. 2011;71(18):6019–6029. doi: 10.1158/0008-5472.CAN-11-1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Badrising S, van der Noort V, van Oort IM, et al. Clinical activity and tolerability of enzalutamide (MDV3100) in patients with metastatic, castration-resistant prostate cancer who progress after docetaxel and abiraterone treatment. Cancer. 2014;120(7):968–975. doi: 10.1002/cncr.28518. [DOI] [PubMed] [Google Scholar]
- 104.Bianchini D, Lorente D, Rodriguez-Vida A, et al. Antitumour activity of enzalutamide (MDV3100) in patients with metastatic castration-resistant prostate cancer (CRPC) pre-treated with docetaxel and abiraterone. Eur J Cancer. 2014;50(1):78–84. doi: 10.1016/j.ejca.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 105.Zhong D, Zhang HJ, Jiang YD, et al. Saikosaponin-d: a potential chemotherapeutics in castration resistant prostate cancer by suppressing cancer metastases and cancer stem cell phenotypes. Biochem Biophys Res Commun. 2016;474(4):722–729. doi: 10.1016/j.bbrc.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 106.Nelius T, Martinez-Marin D, Hirsch J, et al. Pigment epithelium-derived factor expression prolongs survival and enhances the cytotoxicity of low-dose chemotherapy in castration-refractory prostate cancer. Cell Death Dis. 2014;5:e1210. doi: 10.1038/cddis.2014.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gulley JL, Madan RA. Developing immunotherapy strategies in the treatment of prostate cancer. Asian J Urol. 2016;3(4):278–285. doi: 10.1016/j.ajur.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kantoff PW, Schuetz TJ, Blumenstein BA, et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28(7):1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Becker JT, Olson BM, Johnson LE, Davies JG, Dunphy EJ, McNeel DG. DNA vaccine encoding prostatic acid phosphatase (PAP) elicits long-term T-cell responses in patients with recurrent prostate cancer. J Immunother. 2010;33(6):639–647. doi: 10.1097/CJI.0b013e3181dda23e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Karan D, Van Veldhuizen P. Combination immunotherapy with prostate GVAX and ipilimumab: safety and toxicity. Immunotherapy. 2012;4(6):577–580. doi: 10.2217/imt.12.53. [DOI] [PubMed] [Google Scholar]
- 111.Shore ND, Mantz CA, Dosoretz DE, et al. Building on sipuleucel-T for immunologic treatment of castration-resistant prostate cancer. Cancer Control. 2013;20(1):7–16. doi: 10.1177/107327481302000103. [DOI] [PubMed] [Google Scholar]
- 112.Antonarakis ES. Combining active immunotherapy with immune checkpoint blockade for the treatment of advanced prostate cancer. Asian J Androl. 2012;14(4):520–521. doi: 10.1038/aja.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kwon ED, Drake CG, Scher HI, et al. CA184-043 Investigators Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15(7):700–712. doi: 10.1016/S1470-2045(14)70189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sanlorenzo M, Vujic I, Daud A, et al. Pembrolizumab cutaneous adverse events and their association with disease progression. JAMA Dermatol. 2015;151(11):1206–1212. doi: 10.1001/jamadermatol.2015.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Madan RA, Karzai FH, Ning YM, et al. Phase II trial of docetaxel, bevacizumab, lenalidomide and prednisone in patients with metastatic castration-resistant prostate cancer. BJU Int. 2016;118(4):590–597. doi: 10.1111/bju.13412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Madan RA, Karzai FH, Ning YM, et al. Phase II trial of docetaxel, bevacizumab, lenalidomide and prednisone in patients with metastatic castration-resistant prostate cancer. BJU Int. 2016;118(4):590–597. doi: 10.1111/bju.13412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chu GC, Zhau HE, Wang R, et al. RANK- and c-Met-mediated signal network promotes prostate cancer metastatic colonization. Endocr Relat Cancer. 2014;21(2):311–326. doi: 10.1530/ERC-13-0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ryan CJ, Saylor PJ, Everly JJ, Sartor O. Bone-targeting radiopharmaceuticals for the treatment of bone-metastatic castration-resistant prostate cancer: exploring the implications of new data. Oncologist. 2014;19(10):1012–1018. doi: 10.1634/theoncologist.2013-0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mahajan K, Coppola D, Rawal B, et al. Ack1-mediated androgen receptor phosphorylation modulates radiation resistance in castration-resistant prostate cancer. J Biol Chem. 2012;287(26):22112–22122. doi: 10.1074/jbc.M112.357384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chi KN, Gleave ME, Fazli L, et al. A phase II pharmacodynamic study of preoperative figitumumab in patients with localized prostate cancer. Clin Cancer Res. 2012;18(12):3407–3413. doi: 10.1158/1078-0432.CCR-12-0482. [DOI] [PubMed] [Google Scholar]
- 121.Smith DC, Smith MR, Sweeney C, et al. Cabozantinib in patients with advanced prostate cancer: results of a phase II randomized discontinuation trial. J Clin Oncol. 2013;31(4):412–419. doi: 10.1200/JCO.2012.45.0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wyce A, Degenhardt Y, Bai Y, et al. Inhibition of BET bromodomain proteins as a therapeutic approach in prostate cancer. Oncotarget. 2013;4(12):2419–2429. doi: 10.18632/oncotarget.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Coude MM, Braun T, Berrou J, et al. BET inhibitor OTX015 targets BRD2 and BRD4 and decreases c-MYC in acute leukemia cells. Oncotarget. 2015;6(19):17698–17712. doi: 10.18632/oncotarget.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wyce A, Degenhardt Y, Bai Y, et al. Inhibition of BET bromodomain proteins as a therapeutic approach in prostate cancer. Oncotarget. 2013;4(12):2419–2429. doi: 10.18632/oncotarget.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sirtori CR. Aescin: pharmacology, pharmacokinetics and therapeutic profile. Pharmacol Res. 2001;44(3):183–193. doi: 10.1006/phrs.2001.0847. [DOI] [PubMed] [Google Scholar]
- 126.Piao S, Kang M, Lee YJ, et al. Cytotoxic effects of escin on human castration-resistant prostate cancer cells through the induction of apoptosis and G2/M cell cycle arrest. Urology. 2014;84(4):982.e1–982.e7. doi: 10.1016/j.urology.2014.06.019. [DOI] [PubMed] [Google Scholar]