Abstract
Introduction:
Electronic Health Records (EHRs) and Health Information Exchanges (HIEs) are changing surveillance and analytic operations within local health departments (LHDs) across the United States. The objective of this study was to analyze the status, benefits, barriers, and ways of overcoming challenges in the implementation of EHRs and HIEs in LHDs.
Methods:
This study employed a mixed methods approach, first using the 2013 National Profile of LHDs survey to ascertain the status of EHR and HIE implementation across the US, as well as to aid in selection of respondents for the second, interview-based part of project. Next, forty-nine key-informant interviews of local health department staff were conducted. Data were coded thematically and independently by two researchers. Coding was compared and re-coded using the consensus definitions.
Results:
Twenty-three percent of LHDs nationwide are using EHRs and 14 percent are using HIEs. The most frequently mentioned benefits for implementation were identified as care coordination, retrieval or managing information, and the ability to track outcomes of care. A few mentioned barriers included financial resources, resistance to change, and IT related issues during implementation.
Discussion:
Despite financial, technical capacity, and operational constraints, leaders interviewed as part of this project were optimistic about the future of EHRs in local health departments. Recent policy changes and accreditation have implications of improving processes to affect populations served.
Conclusions:
Overcoming the challenges in implementing EHRs can result in increased efficiencies in surveillance and higher quality patient care and tracking. However, significant opportunity cost does exist.
Introduction
Local health departments (LHDs) are experiencing changes in provision and sustainability of several essential public health services with the implementation of Electronic Health Records (EHRs) and Health Information Exchanges (HIEs) [1]. The health informatics agenda is being propelled in health care and expanding to public health agencies through the enactment of legislation and support of regulations [2]. EHRs and HIEs are beneficial in improving population health surveillance and outcomes [3,4,5], but the barriers to implementation of these systems are abundant and challenging to overcome [6,7,8].
Legislation
Health care legislation has served as a catalyst for the evolution of health informatics, including for EHRs and HIEs. The Health Information Technology for Economic and Clinical Health (HITECH) Act of the American Recovery and Reinvestment Act of 2009 was created to drive the adoption and use of health information technology in the United States. HITECH’s provisions and grants have potential to impact the way LHDs receive and use information [9]. Under HITECH, a Meaningful Use (MU) incentive program provided monetary incentives to eligible health care providers and hospitals [10]. Such legislation established health informatics as a priority for clinical, patient-centered care and have significant implications for governmental public health although public health was not a substantial consideration of these laws [11].
Electronic Health Records
EHRs contain longitudinal patient health information in electronic form resulting from one or more visits in a health care setting [12]. EHRs are potentially instrumental in a variety of situations, including support during disasters [13] and emergencies [14], in correctional facilities to monitor human rights concerns and safety violations [15], and for surveillance and management of STDs [16] and chronic diseases [17]. In health care, EHR systems have improved management of clinical practices, expanded collection of condition-specific information, reduced medical errors, and created linkages to improve population health outcomes [18,19]. Benefits for public health agencies are less well characterized. However, existing literature suggests benefits might include: accommodation of large amounts of data, ease of data extraction for analysis, provision of real time information for policy decisions [18], and accurate communication between clinical and research components of health [14]. Recently emerged qualities include interoperability portability and support for mobile work [20]. Also, the adoption of EHR systems among interdisciplinary care teams has increased the need to share quality information, coordinate care, and communicate [20]. Barriers to implementation of EHRs in the health care realm have been explored at some length. These include privacy and security concerns [2,21] and leadership inadequately addressing resistance to health informatics [21,22,23].
While this has been widely studied in the health care and hospital system space, little is known about EHR uptake (or lack thereof) in the public health space [24]. Early studies into EHRs uptake in public health agencies do not believe the benefits outweigh the deterrents of implementation and the EHRs themselves. These perceived deterrents of EHRs are costs of equipment and future maintenance [25], lack of interoperability [14], resistance to share data with other agencies, lack of skilled and trained staff [21], and safety and quality issues [26]. Health departments may use EHRs for clinical case management, to contribute to HIEs, or may draw clinical information from HIEs or EHR systems directly for surveillance purposes.
Health Information Exchange
HIEs are the paths through which patient-level information is shared electronically across different organizations, increasing the coordination of care with potential to improve public health, health status, health care safety and quality of health care [18,27]. The implementation and use of EHRs increases the utility of HIEs. Since EHRs contain patient information over time from multiple locations, successful implementation of a robust HIE is associated with an increased likelihood of continuity of care and improved delivery of service using EHRs [16]. Without HIEs, patient information and other data are siloed at the respective locations. Interoperability of HIEs has focused on benefits of billing efficiencies in health care and access to clinical data, but is slowly proving its full capabilities to improve population health [28]. In a systematic review, Rudin et al [29] found that efficiencies in charges, hospital admissions, quality adherence to guidelines, communication, and patient satisfaction were all the positive outcomes of HIE implementation in the hospital setting.
The challenges to implement HIEs are similar to those of EHRs, such as lack of communication with information systems and inconsistent collection methods among different agencies. Shah et al [30] indicated that both modifiable aspects, such as staffing and financial barriers, and non-modifiable aspects, such as geography were highly associated with uptake of information systems. In addition, LHD characteristics, such as, length of tenure of top executive, having an information specialist on staff, and performing more clinical services were associated with the implementation of HIEs [30]. Despite the challenges, EHRs and HIEs have the ability to improve care delivery and outcomes, and inform population health interventions and policy [31].
Although legislation has increased priority of health informatics in public health agencies, the literature suggests there are still barriers challenging the implementation of EHRs and HIEs. The literature indicated the usefulness and quality efficiencies EHRs can provide as well as, the costs, resistance, and time considerations. HIEs have proven to increase efficiencies [29] through accurate care continuity but also experience resistance in data sharing agreements and concerns of value [32]. Despite the studies, low implementation persists. This study examines the current use of EHRsand health information exchanges in LHDs. It also seeks to understand the perceived benefits and barriers, and to draw strategies to overcome challenges from health informatics experts in LHDs who work with these systems daily.
Methods
Sample
An exploratory mixed method approach was used, employing both quantitative survey data and qualitative key-informant interview data to characterize the status of EHR and HIE implementation, as well as explore the phenomenon behind implementation in this study [33]. Although mixed methods approaches are not common in information systems research, such an approach is used in other fields to produce rich insights and facilitate development of theoretical perspectives [34]. The integration of quantitative and qualitative methods offers a deeper view of public health informatics in LHDs.
The first phase of this project used quantitative data from the 2013 National Profile of Local Health Departments [35] conducted by the National Association of County and City Health Officials. The 2013 National Profile included all the nation’s 2,800 LHDs (condensed to 2,532 reporting units) in the study population, but only 625 LHDs received the portion of the survey containing questions regarding public health informatics. These 625 LHDs were selected based on stratified random sampling by size of population served by the LHD. Of those 625 LHDs, 490 responded for an 82 percent response rate. From these respondents, self-reported data indicated the status of EHRs and HIEs implementation among LHDs.
The qualitative data were collected next using on purposive variation selection of key informants based on their LHDs’ population size and various levels of information system implementation from the aforementioned 490 respondents of the 2013 National Profile. Forty-nine in-depth, key informant interviews of LHD staff, leaders and health information specialists were collected regarding the perceived philosophical, legal, cultural, and infrastructural benefits and barriers to growing uptake of information systems. Interview were approximately 60 minutes on average by telephone, and digitally recorded by the principal investigators following the participant’s consent. The Georgia Southern IRB approved this study (H14374).
The quantitative data provided a cross-sectional view of EHR and HIE implementation among LHDs in the United States through a question regarding LHD’s level of activity for information technology areas. The qualitative data provided more thorough explanations and interpretations to further characterize the findings of the quantitative data. Use of the exploratory mixed methods approach also improves the validity of the study by one set of data, corroborating the other [33,34].
Quantitative Analysis
The quantitative data were analyzed using descriptive and associative inferential analyses to compute percentages of the varying levels of EHR and HIE implementation in LHDs. This analysis was based on estimation weights provided by the 2013 National Profile study Larger LHDs were oversampled and appropriate statistical weights were applied to account for the sampling design. Further details about the National Profile study are available elsewhere [35].
Qualitative Instrument and Analysis
The instrument for the qualitative interviews was designed to delve into the dynamic nature of health informatics in LHDs. It was a semi-structured interview guide, developed through review of literature [36,37,38,39,40,41] and findings of two focus groups conducted with health informatics professionals. Additionally the instrument was pre-tested independently with seven LHD staff prior to the interviews. Major domains of the instrument examined the systems and uses of health informatics, integration and exchange of data and systems, EHRs, MU, HIEs, ACA, leadership and future of health informatics within a LHD context. Questions regarding EHRs, MU, and HIEs were covered in the informatics capacity and set-up section.
The qualitative interviews were transcribed, verified, and coded independently and thematically by two researchers. The recordings were stored in password-protected files and identifying information was removed during the transcription process. Iterative coding and recoding was conducted to maximize intercoder reliability Data were managed and analyzed using NVivo 10.
Results
The overall project included multiple areas of health informatics from 49 key informant interviews from staff within LHDs. This article focuses on four main sections: (a) status of EHRs, MU, and EHRs, (b) perceived and actual benefits of implementation of EHRs, MU, and HIEs, (c) barriers to implementation of EHRs, MU, and HIEs, and (d) and strategies for implementation of EHRs in LHDs. Quantitative results are drawn from responses of 505 LHDs based on the National Profile study (33). Qualitative findings are drawn from 12 respondents were from LHDs that had implemented some form of both EHRs and HIEs, 20 were from LHDs that had not implemented either, and 17 were from LHDs that had implemented one or the other. The majority were from locally-governed LHDs, followed by state- governed LHDs and LHDs with shared governance.
Status
The 2013 National Profile of LHDs identified 23 percent of LHDs reporting that they had implemented EHRs and 14 percent working with HIEs. However, 31 percent had no activity related to implementation of EHRs and 41 percent related to HIE implementation as shown in Figure 1. The findings for the qualitative portion of the study are consistent with the national results in that most of LHDs had no activity related to the implementation of EHRs and HIEs. For EHRs, most of the LHDs had no activity, followed by full implementation and investigated or planned to be implemented. Also, most of the LHDs had no access to HIEs, while a few had limited access and even less had full access.
Figure 1.
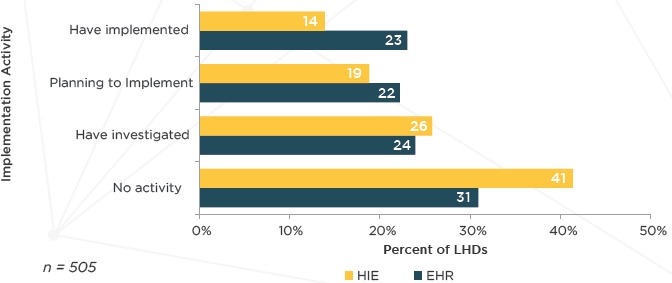
Percent of LHDs by Implementation Activity Level of EHRs and HIEs
Table 1 depicts the characteristics associated with the LHDs included in the qualitative portion of the study. The majority of the respondents were from locally-governed LHDs, LHDs with 25,000 to 99,999 population sizes, and in the Midwest census region.
Table 1.
Characteristics of LHDs Included in the Qualitative Data
| CHARACTERISTICS | NUMBER OF LHDS (n = 49) |
|---|---|
| GOVERNANCE CATEGORY | |
| State | 12 |
| Local | 34 |
| POPULATION SIZE SERVED | |
| >1,000,000 | 3 |
| 500,000 – 999,999 | 5 |
| 250,000 – 499,999 | 4 |
| 100,000 – 249,999 | 8 |
| 50,000 –99,999 | 11 |
| 25,000 – 49,999 | 12 |
| CENSUS REGION | |
| South | 10 |
| West | 10 |
| Northeast | 13 |
| Midwest | 16 |
Major themes from responses of questions regarding EHRs, MU, and HIEs were as follows. EHRs were divided into sub-themes: status of EHR implementation, no implementation of EHRs, perceived benefits of EHRs if not implemented, implementation of EHRs, actual benefits of EHRs if implemented, and barriers and overcoming barriers if implemented. MU was covered under the EHR section as: MU status and requirements, benefits, barriers, and downsides to meeting MU stages. Responses to HIE questions resulted into sub-themes: status of implementation, impact of HIEs, LHD contributions to HIEs, and surveillance using HIEs.
Meaningful Use
Our qualitative interviews show that LHDs with EHR systems lacked readiness about MU requirements. Only 1 of 49 respondents reported meeting stage 2 requirements and 2 of the 49 respondents had met stage 1. Although the respondents were familiar with some of the requirements of MU, most could not say with certainty if their EHR system was compliant at any stage [12/49]. A common form of response for uncertainty included: “And maybe we haven’t. I just know that some of the forms that we have within our EHR are geared towards Meaningful Use, that we have to document for Meaningful Use, but perhaps we haven’t met it yet, that might be true.” Some LHDs had not met any stage [6/49] or had no action [3/49] toward meeting MU. Seven of the 49 respondents found no relevance in reaching MU of EHRs due to having no EHR system, exemption or not meeting criteria, or the state department having control over decision.
The state health agency was mentioned both as a facilitator and limitation to achieving MU compliance, as some LHDs were given the authority to create their own electronic information systems, while other LHDs were included in an overall statewide initiative or excluded from the decision-making process. Two differing themes were commonly expressed: “Stage one was a statewide rollout. The state was actually monitoring our Meaningful Use” and “there is no sort of Meaningful Use expectations at the local level. I think there are some small, at the state-wide level, I think there are some few areas where there’s some level of direct service that happens that maybe impacted but by and large though it’s a provider world that is very concerned about that but we are really not connected to any Meaningful Use expectations at all.”
Five LHDs were in the process of meeting stage 1 or 2. Among the LHDs who reached or were in the process of reaching MU stages, the benefits were community- and administrative- focused. Community-focused themes were community good and linkage of public health to clinical health, while administrative-focused themes were monetary incentives, inclusion in performance evaluation, and reduction in paper records. One LHD respondent mentioned that their staff, “have been very positive about the role of public health but I think within the Meaningful Use was they began to see more of a linkage with more on the clinical care side of the medical model approach and they understand we are dealing with some of the same things.”
Although many reported having experienced the advantages of achieving MU, the obstacles were substantial, mostly relating to staff capacity and technological issues with information systems. Staff- related challenges included resistance to change, an ignorance of the systems, and an increase in work due to change in prioritization and retention of records. In addition, upgrades were not available for all information systems. Staff from 2 LHDs that had worked toward MU indicated there were no downsides to achieving MU and were enjoying the benefits. Among respondents who had not met any stage and had no action towards meeting MU, the barriers were based on 12 responses and illustrated in Table 2. Issues surrounding technology [6] and financial factors [5] were top mentioned concerns.
Table 2.
Responses Regarding Barriers to Reaching MU
| BARRIERS | n | SELECTED QUOTES |
|---|---|---|
| Financial | 4 | There were concerns with money and funding and there were also concerns with what type of system, because they again need to look at how it links up with these other entities where we might need to get the data. |
| Issues with Technology | 3 | The biggest barrier for us was actually a glitch in our EHR for one specific provider. There are electronic -- Meaningful Use passed certain percentage for medication. And our electronic health records up until this year had a problem. |
| Education/Training | 2 | Getting everybody educated about what it [MU] means, the value, and do it and moving forward what are the parameters, what does it mean to us, that’s kind of we are starting as far as within the HIPAA requirements and those kind of things we are going through and reviewing a lot of that also. |
| Measures | 1 | The other thing that we are waiting to hear more about is [system] measures. We know kind of what they are, but we are really kind of confused about how they are utilized or how they are monitoring or what we should be doing or can we bill for them, so I don’t think that area has been addressed at all in our state and it’s an area that I think needs to be addressed and probably I am sure people in our state office have talked about it, but that’s the other area, but I don’t know if that’s a barrier to Meaningful Use. It may be. |
| Providers are inconsistent | 1 | We at this clinic, have a very large number of providers upwards of 30 some different providers, that rotate through. They are here for two years and then they leave, and we get a new group of providers. Constantly training providers in how to use the EHR the Meaningful Use criteria has been a barrier with the consistency or the components of who are providers. One of the other barriers is a consistent person that could educate providers on Meaningful Use, and so the training has been limited. |
| Resources | 1 | The biggest barriers are resources. Our number one job is not Meaningful Use and our number one is not working with health information exchange but we have to do things on their schedule and then if we have just make changes our systems we don’t always have the money to do it. So, time becomes an issue because the competing priority, money becomes an issue because we have to pay our vendors and then people have to stop doing their day to day job to work with the health information exchange for them to help their customers meet Meaningful Use. |
Benefits of EHRs and HIEs
Although only 16 of the 49 LHDs had implemented EHRs, all respondents provided information on perceived or actual benefits. The most frequently mentioned perceived benefits were care coordination [17], retrieval or management of information [16], and tracking outcomes of care [9]. A majority of the respondents which mentioned care coordination as a benefit were from LHDs with shared governance, followed by state governed LHDs, and local-governed LHDs. Benefits were closely related to data accuracy, security, interoperability and outcomes. A few were related to resources, decision-making and planning, and other operational factors. Expected benefits from staff at LHDs that had not yet implemented EHRs aligned closely with benefits reported by those staff at LHDs that had implemented EHRs.
Four of the respondents indicated having full access to HIEs, 20 had limited access, and 21 had no HIE access. The LHDs with full access to HIEs were all locally-governed. Two of the LHDs with full access were serving populations of 25,000 to 49,999, while the others were from populations of 500,000 or more and 25,000 or less. Responses to questions regarding HIE contribution, impact, and surveillance are also included in Table 3. LHDs indicated EHRs contribute to HIEs by providing a better continuity of care for patient [3] and a full picture of patient care [3]. Three LHDs mentioned EHRs having no contribution, but were hopeful for future inclusion. HIEs were most frequently impacting LHD activities through disease surveillance [11] and coordination of care [9]. Surveillance using HIEs was a popular topic and provided by most LHD respondents [36/49].
Table 3.
Benefits of EHRs and HIEs
| EHR AND HIE BENEFIT | n | SELECTED QUOTES |
|---|---|---|
| Care Coordination | 17 | One thing is EHRs definitely have provided a lot more coordination across program areas, especially those that are infected with HIV and STD. It also provides us an opportunity to kind of launch innovative programs. |
| Retrieve or manage information | 16 | That would be accessible from each station as opposed to hunting down the chart that maybe hidden somewhere in somebody’s desk, if they would communicate also with our local hospitals, we could collect information more quickly. You would have more real time access to information. |
| Track outcomes of care | 9 | And just tracking in general, like I’ve told you before with Access that we use our tracking as hit or miss, there may be doubles. In this reporting system, there might be built into it some sort of system where you can pull numbers, because public health is about numbers. |
| Increased efficiencies | 8 | Obviously, there is an advantage to increase the efficiency as far as having the electronic medical record system, all the way down to just all the manual processes that we have to do with medical records via filing lab slips and actually putting the record piece together, and having to send them to storage. That is extremely considered thoughtful, because when you have those other factors such as time span looking for lost records or not having a record when patient shows up here because it did not come from another site. |
| Accurate records | 8 | When you wrote it, you could just write badly and decide what you were trying to say. This has made a big difference to our link. The person who is able to use that paper has to pull the patient chart; everything got put on there and add what was missing or check with the provider Usually they check with the provider It took more time to gather information. There are lots of benefits I see as far as having accurate records that are easy to search and better documentation if it’s electronic and not on paper, easier to read and search. All that kind of data is definitely improved with electronic records. |
| Share Information | 7 | Easier to share data with partners in the community, collaborators. If you take out identifiers and anything that would be confidential which you should be able to do with electronic health records. |
| Secure or protect again loss | 6 | It’s costly, but the data is secure, we have contract, the data is completely compliant with HIPAA requirement, it’s convenient, and don’t need to carry a hard copy. They can access at patient’s home when they do home visits and also if any emergency situation happens the system can come back within a couple of hours. |
| Interoperability | 6 | One of the biggest benefits is communication through an HIE with our local clinics and hospitals as well as some of the tertiary care hospitals for patient care. So, that’s a huge benefit. |
| Immunization completion information | 6 | We have a fairly new immunization information system and there are three ways that it gets updated through our public health clinic. We also have our information updating our registry electronically through our state health information exchange, so we are getting the stuff from the pharmacy and from any providers and hospital providers that are connected to their health information exchange and we still for those providers that are connected to their health information exchange, they can log into a portal and enter information through their EMRs or we will get the paper work and do data entry. |
| HIE CONTRIBUTION | ||
| Better continuity of care for patient | 3 | The health information exchange improves the continuity for patients., Let’s say the patient stays in the hospital and discharged, then come to the clinic for follow-up, we have no way sort of calling over to the hospital and asking them to send it. We don’t have any way to get that information, so they often come to the clinic and we are not prepared to see them. |
| Full picture of patient care | 3 | We are finding that for our clients and if they wind up going to the hospital or with any of the major providers, persons who are seen by multiple entities now with the exchange a particular, whoever it is that they go to next has a more of a complete picture of what has been done, what any kind of diagnosis or health experience the person might have or whether they were in the emergency room. And that’s the information now that we have that we can use that we didn’t necessarily have timely access to before. |
| HIE IMPACT | ||
| Disease surveillance | 11 | We are able to see what we are doing and identify what we spent time on and identify areas that need improvement and identify. For example the hepatitis C outbreak, we would have had no idea that was happening if we didn’t have access to data systems or why, and partly I mean it makes it sounds we are incompetent but partly we are just overwhelmed in the sheer volume of clients we have, nobody really has the time to reflect on what’s actually happening and the data systems have a lot of setup reports that we can run that will show us what’s actually happening. |
| Coordination of care | 9 | For coordination of care it’s possible that our patients might get vaccinated somewhere else and vice versa, we might vaccinate somebody else’s patients temporarily. So we’re utilizing that program, I would even say what the registrar is doing with birth and death records. Those records can also be viewed electronically by other entities, whether it’s a funeral director, or physician, or the State Department of Health. So, it definitely, it helps. We wouldn’t think of a death certificate as necessarily coordination of care. |
| HIE SURVEILLANCE | ||
| Non-mandatory communicable disease data | 14 | One of the things would be an easy application to be able to pull cause of death data directly from an EHR. That data is heavily used in surveillance in terms of looking at trends and being able to see where there may be new interventions needed but the problem that you lose then is you lose one of the key things in classifying death data is that relationship of what cause what and what was really the underlying cause. |
| Chronic conditions | 12 | There’s a lot of stuff we could do around the diabetes and high blood pressure, some of those chronic diseases that at this point that we’re not really doing. Because I said most of what we currently do is around what’s reportable as far as these infectious diseases. So, I think if more people could make it easier to share data, whether that’s through an electronic medical record or some sort of a system, we could possibly look at more things that are factors for chronic disease. |
| Mandatory communicable disease data | 8 | Communicable disease, it’s not something we can get into an electronic health record of a patient at the hospital. We cannot do that but if somebody comes into the hospital with tuberculosis and diagnosed and we can get into the system and see where the lab data is and all that kind of stuff. |
| All types of community health data | 6 | With local data, we can look at obesity level, diabetes levels, all those kinds of chronic disease stuff, communal obviously, disease related information, all that kind of stuff. It would be really nice to be able to see, I mean even in terms of food deserts. One of our rural communities is trying to get a grocery store and we were able to pull up data that showed that the areas of food consider the food deserts so that contributes to health make a need of plausible reason for a need to have a grocery store located there for them. So, all that kinds of stuff will be great to have. We have never been able to do that before and pull it up by zip code. Some of our zip codes and communities are too small that the state probably won’t allow some of the data to be pulled up because it might be identifiable information I guess that’s what they call it but it would be nice to show if there are communities that are so higher in certain things. |
Non-mandatory reporting of communicable diseases [14] and chronic conditions [12] were the most frequently mentioned data pulled or planned to be pulled from EHRs. Noteworthy responses for benefits of HIE access were zip code level, demographic data, and all types of community health data for support to receive grants and continuation of local programs. Disease surveillance data of communities which LHDs serve was a common theme to sustain programming and improve population health outcomes. Eight of the respondents mentioned not planning on pulling any data in the foreseeable future, some due to the lack of capacity. Illustrative quotes of the most frequently mentioned responses are indicated in Table 3.
Barriers to implementation of EHRs and HIEs
Twenty-one LHD staff reported having implemented an EHR system. Eighteen of those respondents indicated the barriers to implementation experienced while in the process. Costs, staff (lack of, training, resistance), and issues related to the technology (interoperability, privacy, issues during implementation) were among the most frequently mentioned barriers. One LHD respondent mentioned, “There were a lot of IT issues, huge, either things, servers down, or connections not working right or the whole system being very, very slow because it comes out of our state office, kind of complicated. So, we had a lot of IT issues, provider resistance and some of our electronic health records they are very slow to get designed because they are designed by our state office to integrate with our billing system.” Thirteen of the responses were from county LHDs indicating costs or financial resources and resistance to change as the most frequently observed barrier Three of the respondents were from multi-county LHDs and observed interoperability as a barrier. Cost or financial resources, an unavailable champion, IT related issues during implementation and privacy concerns were equally mentioned among the responses from city LHD respondents. For LHDs covering more than one city, the most observed barriers were interoperability, lack of staff, partners not having electronic data, and resistance to change. Ranked staff barriers indicated resistance from having to learn a new system and changing the way it has ‘always been done’. In addition, IT issues such as internet not reliable and implementation not being available for all information systems can exacerbate the already challenging situation. Illustrative quotes are included in Table 4. Only four LHD respondents indicated having full access to an HIE. Of those four two LHD respondents mentioned barriers as the state requirement came before HIE readiness and no clinical data. One LHD respondent explained, “The barrier was that health information exchange wasn’t ready but the state was mandating that we use the health information exchange for all reporting. So, any provider that wanted to get Meaningful Use dollars had to go through the health information exchange, so we didn’t have any problems for people wanting to connect and we can accept the data, it’s pretty easy, so the barrier was really just getting the health information exchange to be ready. So, until they were ready we finally just accepted the data directly from the providers, their EMR to our immunization information system, it was a direct connection and now that health information exchange is ready we are moving things back to have the providers’ EMR talk to the health information exchange and the health information exchange sends up the immunization record.”
Table 4.
Barriers to Implementation of EHRs
| BARRIERS | n | SELECTED QUOTES |
|---|---|---|
| EHR CHALLENGES/BARRIERS TO IMPLEMENTATION, IF IMPLEMENTED | ||
| Cost or Financial Resources | 10 | One of the biggest barriers to doing this is funds and resources primarily for changing and for actually getting the system and we did get some money from the state and federal government in order to get to purchase and implement a particular system. |
| Resistance to change | 9 | One unintentional consequence that we experienced sort of going through the EHR process is that not all of our providers were amiable or even sometimes has the expertise to utilize to its fullest extent the EHR. I know that we had a couple of providers who were sort of opposed to learning and I think we even had some early retirements. Internally our barriers have been we had a staff of public health nurses who have been here for 20 years, so that has been a challenge for them to use electronic health records. Other than that I think it’s really worked well for us internally but in terms of exchanging information externally, that’s not possible. |
| Interoperability | 7 | I think one of the challenges for us is we work in a community that has two very large health care systems, and our patients for us, from our clinic is one of the major health care systems and the electronic medical records do not communicate at all, and so that is then a major barrier as far as continuity of care for that patient, it would be helpful if there was cross-wiring that could occur or if we just had access to the other hospital system’s record, but we don’t. So, that’s a major barrier. I do think that our system is slow and so providers will say that it’s a barrier to productivity, it’s not the most fluid system I’ve ever worked in, so it does take a lot of time to document and sign off on labs and things like that. |
| IT related issues during implementation | 5 | Just internally we did have a little bit of technical assistance but staff had to spend, and especially those division managers, did spend a lot of time getting up to speed on what it was and then just working through the some of the technical glitches internally just to make sure that our IT system and infrastructure was deported and right now we have gotten down to the identification of down to the simple fact right now is we are going to upgrade our wireless process throughout the building so we have a more consistent and trustworthy networking system. |
| Lack of training for usefulness and uses for EHRs | 5 | The biggest barrier is trying to deal with that learning to use the system that are rather complex. The one that is chosen is fairly useful but required a significant amount of planning prior to the implementation, and constant maintenance of tables for inventory management, pricing and those kind of things, it requires constant maintenance, and essentially I had to devote one person that solely deals with the maintenance and upkeep of the EMR tables and information system background for the clinicians. |
| REASONS FOR NOT IMPLEMENTING EHRS | ||
| Money or funding/Financial resources | 13 | I think it comes down to time and money, getting the resources to help us do it, having the time necessary to really do that, and the resources necessary to understand it, amalgamate direction. |
| No clinical services | 11 | We don’t have clinics that we run. We don’t have clinical services in that typical fashion like the primary health clinic or the specialty care clinic, so we don’t have to do electronic health records in that way. |
| Priority is low | 4 | It has just taken a backseat as far as priorities go and it just hasn’t reached the top level of priorities here. There has been other things that have usurped the priorities. |
| Training, lack of | 4 | A second one would be the knowledge and the staff to implement that. Again, you will be relying on our whole city’s IS department which very few people for them to get involved and that would probably require them to hire someone for us. And I don’t see that happening. |
Thirty-one respondents provided reasons for not implementing EHRs. Having no clinical services was the top reason for not implementing EHRs in LHDs with population sizes of 1,000,000 or more and 25,000 to 49,999. Funding or financial resources were frequently mentioned in LHDs serving populations of 500,000 to 999,999; 100,000 to 249,999; 50,000 to 99,999; and 25,000 or fewer. For LHDs serving populations of 250,000 to 499,999, benefits were unknown was a major reason for not implementing EHRs. One LHD respondent said, “I think that’s another one of our hesitancies, because we don’t really know at this point how it would benefit, I think if we could see how it works in other providers, and could really see some benefits from it, it might be something that we would be more interested in, but at this point with the recording keeping that we are already doing, we don’t, I don’t really know what the benefit would be.” Confirmation for the barriers mentioned by LHDs who have implemented EHRs, costs, staff (resistance, training, priority), and IT related issues (capacity, control) were also issues mentioned as reasons for not implementing EHRs. Quotes for the most frequently mentioned themes are indicated in Table 4.
Overcoming challenges to implementation of EHRs
Sixteen responses from smaller (25,000 – 49,999 population size) and medium (50,000 – 499,999 population size) LHDs provided strategies to overcome challenges during the implementation of EHRs. These strategies indicate the emphasis on people inside and outside the LHD. Involvement of internal and external stakeholders and the reduction of barriers for resistance to implementation are common themes. Teamwork [3] or building relationships through staff involvement and communication in the implementation process was the most frequently mentioned strategy. This strategy was most common among the state- governed LHDs. A respondent expressed, “there is good chance for small offices because we work as a team and we have, if we need a laugh or cry we choose to laugh and we work at it together. We have one nurse who is our tech savvy nurse. So, then questions regarding anything technical or electronically with those we ask her. She has been more than happy to teach us and write reports.” In addition, having a relationship with board of health and external organizations can assist with securing funding, advocacy, support, and buy-in from stakeholders. Training [2], providing computers with Wi-Fi access [1], and constructing planning or steering committees [1] reduce barriers and assist with the resistance during the transition of technology. Training was mentioned as the top strategy among local- and shared-governed LHDs. An example was,
“A lot of training with staff so that they were very comfortable with the templates, the HR and try to have someone who is more of an expert sit with them and show them some of the short-cuts or little things that are lost sometimes in training, short cuts and what not to do and things like that. We worked very hard on the IT issues, we needed to have expanded bandwidth, we finally-we were very flexible in trying to work with the provider and what worked best for them as far as do they want to use Wi-Fi with a small laptop or if they wanted a desktop. So, we tried very hard to accommodate the providers as to what would work best for them, not to change their process but to work with them to make it easier, it took a long time for the IT issues to iron out and I think having an expanded bandwidth and working very closely with our IT people in our state office to lot of bugs worked out, so I would say that’s what-those were the things that we did.”
Additional strategies are included in Table 5. These indicate external assistance and buy-in to improve the implementation process. Grant funding can decrease the financial barriers and consultant help and quality improvement can improve efficiency and productivity during the process.
Table 5.
Strategies Used to Overcome Challenges of Implementation of EHRs
| THEME | n | SELECTED QUOTES |
|---|---|---|
| Getting buy-in from stakeholders | 2 | A lot of it is the process, getting the right people to buy into the system, and buy into the ultimate goals of better care, coordinated care, and providing people the opportunity to ensure treatment. Once you can sell them on ultimate goals of the project, and the reasoning behind it, the right people to buy in, really helps to reduce some of those barriers. Being sensitive to them as well, see legitimate concerns. |
| Grant Monies | 2 | We got one of the ARRA grants and we had to put in a new system and we got it in a system, worked with all the technology functions that we needed, like web services and also accepted things through various HL7 messages through SFTP and we were ready to share data. The barrier was that health information exchange wasn’t ready but the state was mandating that we use the health information exchange for all reporting. So, any provider that wanted to get Meaningful Use dollars had to go through the health information exchange, so we didn’t have any problems for people wanting to connect and we can accept the data, it’s pretty easy, so the barrier was really just getting the health information exchange to be ready. So, until they were ready we finally just accepted the data directly from the providers, their EMR to our immunization information system, it was a direct connection and now that health information exchange is ready we are moving things back to have the providers’ EMR talk to the health information exchange and the health information exchange sends up the immunization record. And there was a grant that the immunization group got that helped pay for the providers’ EHR vendor to get them to connect for bidirectional queries, so it will be date and query and the history and we provided that to some of our providers. |
| Consultant’s help/obtain external help | 1 | On the movement thing and the process, we made the changes, I had an outside person come do some process improvement things with us, so that it wasn’t just all coming from me and when that person said, well this doesn’t make any sense because right now at the very beginning, our provider was walking over 100 steps just to get the clinic area. And we had what we call the screening room. So, that if there were 20 patients in the lobby, they took one person at a time to the screening room so that created backups for that. So, we made a whole bunch of slow changes to increase our efficiency and productivity and there was always happiness after that, but the change it had to be done. |
| Planning or steering committee | 1 | I tried to give people who were upset about those things more decision making within other things that we could be more flexible on, does it make sense. |
| Provision of computers and Wi-Fi to staff | 1 | We worked very hard on the IT issues, but needed to have expanded bandwidth. We were very flexible in trying to work with the provider and what worked best for them as far as do they want to use Wi-Fi with a small laptop or if they wanted a desktop. So, we tried very hard to accommodate the providers as to what would work best for them, not to change their process but to work with them to make it easier, it took a long time for the IT issues to iron out and I think having an expanded bandwidth and working very closely with our IT people in our state office to lot of bugs worked out, so I would say that’s what- those were the things that we did. |
Discussion
Implementation of new technology is inevitably coupled with challenges. The same is true of EHR and HIE implementation in LHDs. The key informant interviewees’ LHDs had implemented various information systems slightly above the national averages for EHRs and below for HIEs (23 of 49 for EHRs and 4 of 49 for HIEs, compared to 23 percent and 14 percent nationally). Previous studies confirm the many benefits and barriers of EHRs and HIEs, but few studies focus on deeper reasons behind the continued blockades to experiencing the advantages. The rationales were a main point of inquiry in this project. Money or the lack thereof is a persistent issue for LHDs, especially among medium and smaller LHDs. However, staff involvement and training can reduce internal barriers in order to experience benefits, such as care coordination and management of data information for population health.
The findings of this study align with the Organizational Innovation framework in describing the influences of individuals, organizations, and environment have on the implementation of EHRs and HIEs [42]. Individual influences on the implementation were described through the lack of trained staff and resistance of staff to learn new systems and new workflow processes. Organizational influences were observed through LHD differences in governance type and the control of informatics and operational decisions. Interoperability of surrounding organizations, such as hospitals, medical laboratories and state health departments, and the size of the population of LHDs were influences of the environment. Organizational innovation framework served as a guide to characterize the various responses of the LHD staff.
One of the most important benefits among LHDs for the use of EHRs and HIEs, regardless of implementation status, was care coordination. This was for both clinical care practices as well as greater effectiveness in programs and interventions, appropriate treatment at various locations, and follow-up and continued care of discharged patients. Care coordination is a high priority amongst LHD respondents and as a contributor to HIEs. Siloed data are inefficient for patient care and population health, which is supported by the results of this study. Additional benefits of EHRs and HIEs mentioned were monetary incentives, insertion into performance evaluations, and increase of storage space due to a reduction in paper records.
The lack of financial resources is a difficult challenge to overcome. Prioritization and allocation of funds from state and federal leadership now could lead to better workflow processes and cost efficiencies in the future. Acquiring and sustaining buy-in from these leaders stresses how EHRs and HIEs would benefit the population in which they serve. Grant funding could alleviate some of the financial pressure of LHDs, such as an ARRA grant which assists with systems and technology functions.
This study includes limitations of self-reported data, which were not independently verified. This study is based on the most recent available data. Although, this research used two individual interviewers and a standardized instrument to reduce interview biases, there is always a possibility. In addition, this research is based on a purposive selection of a small group. These results may not be transferable to all LHDs nationwide.
Recent policy changes have helped increase priority of health informatics in the public health sector with implications on improving the processes to affect the health of the populations served. With EHRs and HIEs in place, public health agendas can include clinical care data and more widely address population level concerns [43]. Interoperability of systems can assist in timely and efficient alerts, emergency response, population research, detailed analysis, refined interventions, future preparations for health, and overall coordination of care for patients [13,33].
HIEs are important community partners; our study results regarding low HIE connectivity may have implications for PHAB standards requiring health departments to collaborate in assessing and assuring provision of essential public health services [44]. Public Health Accreditation Board (PHAB) urges local health departments to achieve accreditation through regular community health assessments, community health improvement planning, communication and data exchange, and evidence based decision making [45]. Informatics capacities and connectivity to EHRs and HIEs can assist LHDs in utilization of big data to improve assessment and surveillance, and superior connectivity with data on social determinants of health.
Recommendations for the future of health informatics in public health are to continually work toward the integration of health care and public health through EHR and HIE implementation [31]. In addition, leadership should include staff in the decisions to implement health informatics through positive yet clear communication and continually training to stay current. Although legislation can motivate change, accompanying funding to increase the ability of LHDs to implement services which can change population health now and in the future. EHRs and HIEs can provide continuity of care for patients, improve health outcomes, and inform population health interventions and policy.
Conclusion
Changes in the provision and sustainability of essential public health services with the implementation of EHRs and HIEs are being experienced in LHDs nationwide. This study characterized the current use of EHRs and HIEs in LHDs and illuminated the perceived benefits, barriers, and strategies to overcoming challenges from LHDs who use health informatics. Despite financial, technical capacity and operational constraints in the implementation of electronic health records and health information exchanges, leaders were optimistic about the future of EHRs in local health departments. Strategies, such as teamwork, training, and securing support and buy-in from stakeholders, are relatively simple approaches to improving implementation of new technologies in LHDs. The opportunity for EHRs to improve surveillance and prevention of chronic disease, reduce disparities, and target interventions is a worthy effort [17,46]. Leadership is an essential component in the success of EHR and HIE implementation, and should seek to improve the status in LHDs for future efficiencies, continuity of patient care, and overall outcomes in populations served by LHDs.
Acknowledgements
We gratefully acknowledge the de Beaumont Foundation for funding this research.
Appendix A. LHD Informatics Study: Qualitative Interview Guiding Questions
Hello and thank you for participating in this interview on health informatics capacity of local health departments. Again, my name is _____ and I am _______ at the JPHCOPH, Georgia Southern University.
This interview will last between 50-60 minutes. As explained to you earlier, your participation is absolutely voluntary. You can decline to answer any question, and if you wish to discontinue your participation at any time during the interview process, please feel free to do so. With your permission, we would like to record this interview. This recording will be used exclusively for capturing data and it will be deleted once the transcription is completed. The transcripts will contain no identifying information. Your identity and specific identity of the organization you work for will be confidential and any reports generated from this session will include only de-identified responses. Before verbally consenting to participation in this interview, I would like to make sure that you understand the purpose of this study Do you have any questions about the purpose of the study and/or the manner in which this interview data will be used? With your consent, we will begin the interview, and it will be recorded. (Consent)
Section 1: Data Systems
We will use the term “public health informatics” in this interview. There are several definitions but in this context, by public health informatics, we mean systematic application of information, analytics, computer science and technology to support the day to day work of public health, including surveillance, reporting, and health promotion. It is both the IT infrastructure and how you use information in your public health work.
(Adapted from O’Carroll et al., 2003: 5; American Medical Informatics Association (AMIA))
Would you start by telling us how you are involved with public health informatics in your health department? Do you have any responsibilities in this area?
Would you tell me about how your LHD uses data and information in your everyday work; e.g. as it relates to assessment, designing public health policies/regulations/interventions, quality improvement and assurance? Please let me know what kinds of data you use to do this work, too.
-
What kinds of different data systems/registries/etc. does your organization maintain?
Do they communicate with each other?
What kinds of challenges have you had integrating the datasets?
How have you overcome those challenges?
Who do you exchange data/information with and are you able to do it electronically?
{If the respondent is totally blank, then ask questions about data use in specific programs such as: do you collect and/or exchange immunizations? Do you use and exchange data for surveillance? Who do you exchange such data with? And how?}
Section 2: Informatics capacity and set up
4) I would like to take a few minutes to talk with you about Electronic Health Records. First, I will ask you to differentiate between EHR use in your LHD in a clinical setting versus using EHRs for surveillance purposes. With respect to EHR implementation clinically, would you say there has been: “No activity” “Have investigated,” “Planning to implement,” or “Have implemented?” Again, that list is: ““No activity,” “Have investigated,” “Planning to implement,” and “Have implemented.”
{If Prompted: “An electronic health record (EHR) is a digital version of a patient’s medical record that can be securely shared digitally to authorized users}.
-
If No Activity, Have investigated, Planning to Implement:
Why have you not implemented Electronic Health Records?
What would be the benefit of implementing Electronic Health Records?
-
If Have Implemented:
What does implementation of Electronic Health Records look like in your LHD? Have you implemented all components of it or just some components (for example scheduling and billing component but not clinical component of EHRs)?
What have been the benefits of implementing Electronic Health Records?
-
What barriers did you encounter while implementing Electronic Health Records?
How did you overcome those barriers to implementing Electronic Health Records?
5) How are you interacting with HIEs, if at all?
How are HIEs impacting your LHD’s activities, such as surveillance, coordination of care, etc.?
What types of data can you or are you planning to pull from EHRs for surveillance purposes?
-
If they have a clinical EHR
Are you contributing your LHD’s clinical EHR to the Health Information Exchange? Any benefits of doing so?
6) I am wondering – more broadly – how is the Affordable Care Act impacting your LHD’s informatics functioning and capacities, if at all?
7) Should the strategy for doing chronic disease surveillance be different than communicable disease surveillance? Why so/not?
8) If they have implemented EHRs: Has your LHD met stage 1 or stage 2 Meaningful Use requirements for your LHD’s clinical systems EHRs?
If LHD has not implemented EHRs, ask if it is state health agency’s responsibility rather than LHD.
What is their involvement in Meaningful Use requirements?
Any barriers to implementation?
What has been the upside of meeting Meaningful Use requirements?
Any downsides?
Section 3. Future of Informatics:
Let’s shift to the final few questions, where we will talk about the future of informatics.
9) What role can leadership play in building capacity of LHDs for informatics?
10) What future plans and/or current strategies, if any do you have for expanding your informatics capacity, particularly data collection from your various data systems?
Broadly speaking, what would you say you see as the major barriers to doing more with data and informatics in local health departments?
With whom do you plan to exchange electronic data?
11) I would like to end this interview with you by entertaining a blank slate scenario. Set aside all of the legal, technological, and financial restrictions you face in your day-to-day work. Imagine you could have any sort of data or information you wanted to help assess, assure and improve population health. What types of information would you want, and what would you do with that information? Be specific.
Let the individuals talk this out, prompt to get as many as possible
OK – thank you for that list – I am now going to read back that list to you and ask what resources will you be willing to devote (e.g., people, funds)? Let’s still set aside technological and legal constraints for the moment. So, keeping in mind that you have a limited budget and prioritizing some of this data collection will have an opportunity cost – please tell me what resources will you be willing to devote to get the data?
Repeat list
Thank you for participating in this important project. If you have any additional questions or thoughts, please contact---
References
- 1.Cheatham M. Informatics works in local health departments. NAACHO Exchange. 2013; 12(1), 1–2. [Cited 2015 Jul 8]. Available from: http://eweb.naccho.org/eweb/DynamicPage.aspx?WebCode=proddetailadd&ivd_prc_prd_key=20b8f8b3-8fbd-4809-a329-937a74d76e5c&Action=Add&site=naccho&ObjectKeyFrom=1A83491A-9853-4C87-86A4-F7D95601C2E2&DoNotSave=yes&ParentObject=Cen-tralizedOrderEntry&ParentDataObject=Invoice%20Detail [Google Scholar]
- 2.Fernandez-Aleman J, Carrion Senor I, Angel Oliver Lozoya P, Toval A. Security and privacy in electronic health records: A systematic literature review. J Biomed Informatics. 2013; 46; 541–562. [DOI] [PubMed] [Google Scholar]
- 3.Birkhead G, Klompas M, Shah N. Uses of electronic health records for public health surveillance to advance public health. Ann Rev Public Health. 2015; 36: 345–359. [DOI] [PubMed] [Google Scholar]
- 4.Dixon BE, Gibson PJ, Frederickson Comer K, Rosenman M. Measuring Population Health Using Electronic Health Records: Exploring Biases and Representativeness in a Community Health Information Exchange. Stud Health Technol Inform. 2015; 216:1009. [PubMed] [Google Scholar]
- 5.Diez Roux AV, Katz M, Crews DC, Ross D, Adler N. Social and Behavioral Information in Electronic Health Records: New Opportunities for Medicine and Public Health. Am J Prev Med. 2015. December; 49(6):980–983. doi: 10.1016/j.amepre.2015.08.027 [DOI] [PubMed] [Google Scholar]
- 6.Friedman DJ, Parrish RG, Ross DA. Electronic health records and US public health: Current realities and future promise. Am J Public Health. 2013; 103: 1560–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayatollahi H, Mirani N, Haghani H. Electronic health records: what are the most important barriers? Perspect Health Inf Manag. 2014. October 1; 11:1c. eCollection 2014. [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse CS, Regier V, Rheinboldt KT. Barriers over time to full implementation of health information exchange in the United States. JMIR Med Inform. 2014. September 30; 2(2):e26. doi: 10.2196/medinform.3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Assessing the status and prospects of state and local health department information technology infrastructure. 2013; [cited 2015 Oct 5]. Available from: http://aspe.hhs.gov/basic-report/assessing-status-and-prospects-state-and-local-health-department-information-technology-infrastructure
- 10.Kirkwood J, Jarris P. Aligning health informatics across the public health enterprise. J Public Manag Pract. 2012; 18(3): 288290. [DOI] [PubMed] [Google Scholar]
- 11.Burke T. The health information technology provisions in the American Recovery and Reinvestment Act of 2009: implications for public health policy and practice. Public Health Rep. 2010; 125(1): 141–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Health Information and Management Systems Society (HIMSS). 2015; [cited on 2015 Aug 25]. Available from: www.himss.org/library/ehr/
- 13.Brown S, Fischetti L, Graham G, Bates J, Lancaster A, McDaniel D, Gillon J, Darbe M, Kolodner R. Use of electronic health records in disaster response: The experience of Department of Veterans Affairs after Hurricane Katrina. A J Public Health. 2007; 97: S136–S141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffman S, Podgurski A. Big bad data: law, public health, and biomedical databases. J Law Med Ethics. 2013; 41(1): 56–60. [DOI] [PubMed] [Google Scholar]
- 15.Glowa-Kollisch S, Andrade K, Stazesky R, Teizeira P, Kaba F, Macdonald R, Rosner Z, Selling D, Parsons A, Venters H. Data-driven human rights: Using the electronic health record to promote human rights in jail. Health and Human Rights. 2014; 16(1): 157–165. [PubMed] [Google Scholar]
- 16.Paneth-Pollak R, Schillinger J, Borreli J, Handel S, Pathela P, Blank S. Using STD electronic medical record data to drive public health program decisions in New York City. Am J Public Health. 2010; 100: 586–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tomasallo C, Hanrahan L, Tandias A, Chang T, Cowan K, Guilbert T. Estimating Wisconsin asthma prevalence using clinical electronic health records and public health data. Am J Public Health. 2014; 104: e65–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menachemi N, Collum T. Benefits and drawbacks of electronic health record systems. Risk Manag Healthcare Policy. 2011; 4: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsolo K. In search of a Data-in-Once, electronic health record-linked, multicenter registry-how far we have come and how far we still have to go. eGEMs (Generating Evidence and Methods to improve patient outcomes. 2012; 1(1): 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen L, Bellucci E, Thuy Nguyen L. Electronic health records implementation: An evaluation of information system impact and contingency factors. Intl J of Med Informatics. 2014. 83; 779–796. [DOI] [PubMed] [Google Scholar]
- 21.Tripp S. The introduction of electronic records into the community public health workforce. Community Pract. 2013; 86(7): 28–31. [PubMed] [Google Scholar]
- 22.Scheck McAlearney A, Robbins J, Kowalczyk N, Chisolm D, Song P. The role of cognitive and learning theories in supporting successful EHR system implementation training: A qualitative study. Med Care Res Rev. 2012; 69: 294–315. [DOI] [PubMed] [Google Scholar]
- 23.McAlearney A, Hefner J, Sieck C, Huerta T. The journey through grief: Insights from a qualitative study of electronic health record implementation. Health Serv Res. 2015; 50(2), 462–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCullough JM1, Zimmerman FJ, Bell DS, Rodriguez HP. Local public health department adoption and use of electronic health records. J Public Health Manag Pract. 2015. Jan-Feb; 21(1):E20–8. doi: 10.1097/PHH.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 25.Yoon-Flannery K, Zandieh SO, Kuperman GJ, Langsam DJ, Hyman D, Kaushal R. A qualitative analysis of an electronic health record (EHR) implementation in an academic ambulatory setting. Informatics in Prim Care. 2008; 16: 277284. [DOI] [PubMed] [Google Scholar]
- 26.Zandieh SO, Yoon-Flannery K, Kuperman GJ, Langsam DJ, Hyman D, Kaushal R. Challenges to EHR implementation in electronic-versus paper-based office practices. J Gen Internal Med. 2008; 23: 755–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MDenpDD T, Asikainen P, Gissler M, Siponen K, Maass M, Saxranto K, Suominen T. The utilization rate of the regional health information exchange: how it impacts on health care delivery outcomes. J Public Health Manag Pract. 2012; 18(3): 215–223. [DOI] [PubMed] [Google Scholar]
- 28.Hessler B, Soper P, Bondy J, Hanes P, Davidson A. Assessing the relationship between health information exchanges and public health agencies. J of Public Health Manag Pract. 2009; 15(5): 416–424. [DOI] [PubMed] [Google Scholar]
- 29.Rudin R, Motala A, Goldzweig CL, Shekelle PG. Usage and effect of Health Information Exchange. Ann Internal Med. 2014; 161:803–811 [DOI] [PubMed] [Google Scholar]
- 30.Shah GH, Leider JP, Castrucci B, Williams K, Luo H. Characteristics of local health departments associated with their implementation of electronic health records and other informatics systems. Public Health Rep. 2016. 131(2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vest JR, Issel LM. Factors related to public health data sharing between local and state health departments. Health Services Research. 2014; 49: 373–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeager V, Walker D, Cole E, Mora A, Diana M. Factors related to health information exchange participation and use. J Med Sys. 2014;38:78–87. [DOI] [PubMed] [Google Scholar]
- 33.Creswell J. Research design: Qualitative, quantitative and mixed methods approaches (2nd ed.). Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- 34.Venkatesh V, Brown S, Bala H. Bridging the qualitative-quantitative divide: Guidelines for conducting mixed methods research in information systems. MIS Quarterly. 2013; 37(1): 21–54. [Google Scholar]
- 35.National Association of City and County Health Officials [NACCHO]. 2013 National Profile of Local Health Departments. 2014; [cited 2015 Aug 1]. Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-National-Profile-of-Local-Health-Departments-report.pdf
- 36.ONC. The National Alliance for Health Information Technology Report to the Office of the National Coordinator for Health Information Technology on Defining Key Health Information Technology Terms April 28, 2008. Dept. of Health & Human Services. Office of the National Coordinator for Health Information Technology (ONC). http://cdm16064.contentdm.oclc.org/cdm/singleitem/collection/p266901coll4/id/2086/rec/10. Accessed May 13, 2013.
- 37.Cherry BJ, Ford EW, Peterson LT. Experiences with electronic health records: early adopters in long-term care facilities. Health Care Manage Rev. 2011. Jul-Sep; 36(3):265–74. doi: 10.1097/HMR.0b013e31820e110f. [DOI] [PubMed] [Google Scholar]
- 38.Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Ann Rev Public Health. 2009; 30:151–74. [DOI] [PubMed] [Google Scholar]
- 39.IOM (Institute of Medicine). 2012. Primary Care and Public Health: Exploring Integration to Improve Population Health Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 40.Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evidence Report/Technology Assessment (Full Rep). 2006. April; (132):1–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vest JR, Menachemi N, Ford EW. Governance’s Role in Local Health Departments’ Information System and Technology Usage. J Public Health Manag Pract. 2012. March; 18(2):160–8. [DOI] [PubMed] [Google Scholar]
- 42.Damanpour F. Organizational innovation: A meta-analysis of effects of determinants and moderators. Acad Manag J. 1991; 34(3): 555–590. [Google Scholar]
- 43.Calman N, Hauser D, Lurio J, Wu W, Pichardo M. Strengthening public health and primary care collaboration through electronic health records. Am J Public Health. 2012; 102: e13–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.PHAB Health Accreditation Board. (2013). Standards & Measures Version 1.5. Retrieved from http://www.phaboard.org/wp-content/uploads/SM-Version-1.5-Board-adopted-FINAL-01-24-2014.docx.pdf
- 45.Lovelace, K & Shah, G. (2016). Using information systems to improve mid-sized local health department’s effectiveness in a time of rapid change. J Public Health Manag Pract, 22(Suppl 6), S89–S94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vogel J, Brown J, Land T, Platt R, Klompas M. MDPHnet: Secure, distributed sharing of electronic health record data for public health surveillance, evaluation, and planning. Am J Public Health. 2014; 104: 2265–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]


