Abstract
Isolated medial patellar subluxation (MPS), in the absence of a previous lateral retinacular release, is a poorly recognized clinical condition characterized by chronic anterior knee pain that is exacerbated with knee flexion. This type of patellar instability is often overlooked, and a high index of suspicion is needed for appropriate diagnosis and treatment. The purpose of this Technical Note is to describe a surgical technique to reconstruct the lateral patellofemoral ligament with an allograft gracilis tendon. By restoring stability to the lateral side of the patella, this minimally invasive technique successfully treats cases of isolated MPS.
Medial patellar subluxation (MPS) is a poorly recognized clinical condition characterized by chronic anterior knee pain that is exacerbated with knee flexion.1 Betz et al.2 first described MPS in 1987 by as a complication following lateral retinacular release. Since then, multiple cases of iatrogenic, traumatic, and isolated medial subluxation have been reported.1 Isolated MPS in the absence of a previous lateral release is often overlooked, and a high index of suspicion is needed for appropriate diagnosis and treatment. There is limited literature describing isolated MPS; only a few reports have been published regarding the findings and treatment outcomes.1
Numerous surgical procedures to correct the medial patellar instability have been described; options have included repair of the lateral retinaculum with imbrication, reconstruction of the retinaculum with local soft-tissue augmentation, and lateral patellotibial reconstruction.1 The biomechanical importance of the lateral patellofemoral ligament (LPFL) as a passive restraint to medial patellar translation has been recently appreciated.3, 4 As such, reconstruction of the LPFL has gained in popularity as an effective operation to treat medial instability and has become a more commonly reported surgical technique for the treatment of MPS. Several methods of LPFL reconstruction have been described, with primary differences consisting of graft choice and patellar fixation.5, 6, 7, 8, 9
This Technical Note describes a surgical technique to reconstruct the LPFL with an allograft gracilis tendon. The graft is secured in a tunnel within the extensor retinaculum and periosteum over the patella, thus avoiding bone tunnels or patellar fixation, which can create a stress riser within the patella. By restoring stability to the lateral side of the patella, this minimally invasive technique successfully treats cases of isolated MPS.
Surgical Technique
A demonstration of the reconstruction technique in a cadaveric left knee is provided in Video 1. Table 1 describes the preoperative evaluation and diagnosis of MPS. The indications and contraindications of the procedure are presented in Table 2. The pearls and pitfalls are summarized in Table 3.
Table 1.
Evaluation and Diagnosis of Medial Patellar Subluxation
| Patient history | Pain is localized to the inferomedial patella and anteromedial joint line. Pain with knee flexion activities such as squatting. Often the patient is aware that the direction of instability is medial. |
| Physical exam | Active and passive range of motion is painful during the first 30° of knee flexion. Patella translation is assessed at knee extension and 30° of flexion. Medial apprehension test. Lateral patellar float sign—the patella translates laterally and rotates or tilts upward with medial pressure on the patella. Manual centering test. |
Table 2.
Indications and Contraindications of Lateral Patellofemoral Ligament Reconstruction
| Indications | Symptomatic isolated medial patellar subluxation Iatrogenic MPS following a lateral retinacular release Lateral patellar laxity Failed nonsurgical treatment Accompanying a medial stabilization procedure in patients with bidirectional patellar instability |
| Contraindications | Concomitant arthritis of the patellofemoral joint Voluntary recurrent dislocations Ongoing infection |
Table 3.
Pearls and Pitfalls
|
|
Patient Positioning and Preparation
Preoperatively, the patient receives an adductor canal nerve block with indwelling catheter. The patient is then positioned supine, and a lateral post is used with the bed kept flat. The patient is examined under anesthesia to confirm the diagnosis of medial patellar instability. Lateral forces are applied to the patella in full knee extension and 30° of flexion. The contralateral knee should be examined for side-to-side comparison. A nonsterile leg tourniquet is placed high on the leg and set at 225 to 250 mmHg. A small bump is placed under the hip to prevent external rotation. If desired, fluoroscopy can be brought in from the ipsilateral side of the bed when needed. The surgical area is prepped in standard fashion, and sterile drapes are applied.
Diagnostic Arthroscopy
Diagnostic arthroscopy is routinely performed, and intra-articular findings are noted. Patellar alignment and position, the shape of the patella and the femoral trochlea, laxity on both medial and lateral sides, and the degree of lateral side tightness are all evaluated. These findings determine the surgical plan that is required. To confirm MPS, the patellofemoral compartment is viewed from the anterolateral portal. With the knee at full knee extension, lateral laxity and medial tilt of the patella can be identified. As the knee is flexed to 30°, the patella moves medially and can subluxate over the edge of the medial facet of the trochlea (Fig 1). In addition to diagnostic purposes, associated conditions such as patella or trochlea chondral injuries can be addressed concurrently.
Fig 1.
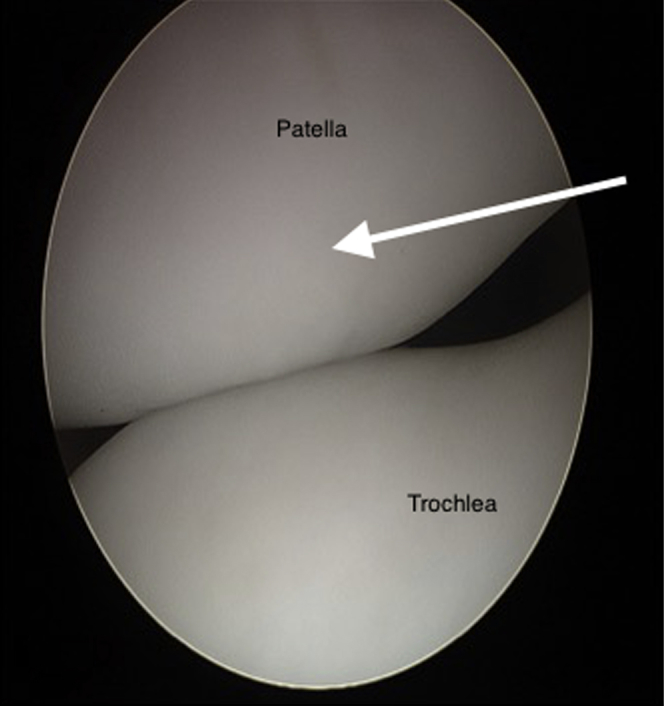
Left knee viewed from the anterolateral portal with a 30° arthroscope. Medial patellar subluxation at 30° of knee flexion is clearly visualized.
Graft Preparation
A double-bundled gracilis allograft tendon is chosen to reconstruct the native LPFL. Typically, at least 20 cm of tendon is needed to ensure that the graft is of sufficient length. The ultimate length depends on the size and age of the individual patient. The ends of the graft are prepared with no. 2 FiberLoop (Arthrex, Naples, FL) using the SpeedWhip (Arthrex) technique to assist with graft passage.
Surgical Approach
A 3- to 4-cm midline skin incision is then made centered over the superior one-third of the patella. Skin flaps are developed to expose the patella. Hemostasis is obtained with electrocautery. A lateral release and tibial tubercle transfer may be performed if indicated to center the patella in the trochlea. If used, the incision can be extended distally. The lateral release is repaired by rotating a flap of tissue from the adjacent iliotibial band to close the defect. This prevents the development of lateral side laxity and allows the reconstructed ligament to be optimally tensioned. A 1-cm incision is then placed in the periosteum at the level of the proximal patella. A second 1-cm incision is made at the lateral border of the patella. The 2 incisions are connected subperiosteally (Fig 2).
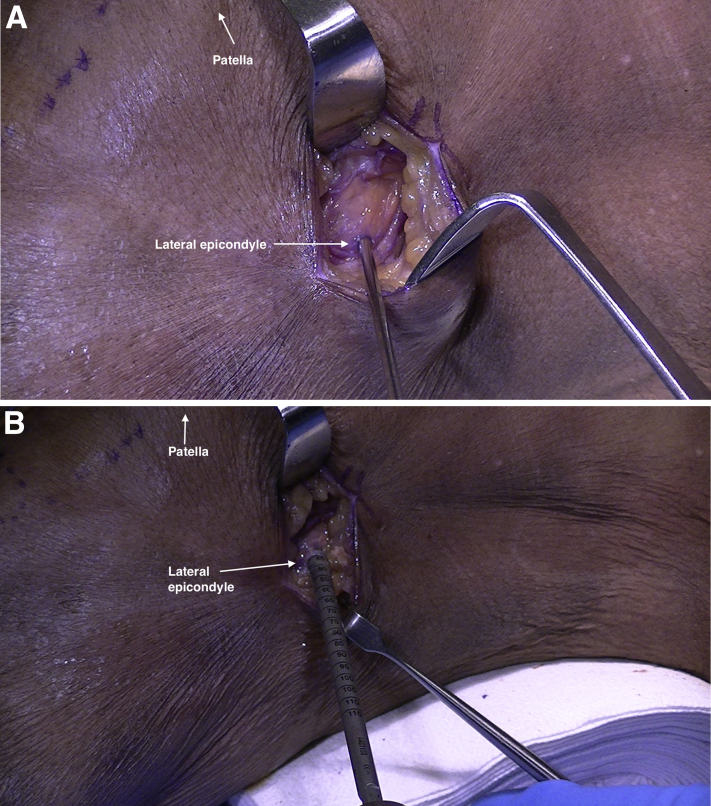
Fig 2.
A 3- to 4-cm midline skin incision is made centered over the superior one third of the patella. (A) A 1-cm incision is placed in the periosteum at the level of the proximal patella. (B) A second 1-cm incision is made at the lateral border of the patella. (C) The 2 incisions are connected subperiosteally (left knee).
Femoral Tunnel Placement
The appropriate location for the LPFL femoral attachment at the lateral epicondyle is identified, and a small 2- to 3-cm longitudinal incision is made at that site to allow for tunnel placement. The knee is slightly flexed to facilitate palpation. The graft may be placed in the second layer of the lateral retinaculum superficial to the joint capsule. It should remain extra-articular so as not to interfere with healing. Using a long, curved clamp, the selected soft-tissue interval is developed in the lateral retinaculum from the edge of the patella to the lateral epicondyle (Fig 3). With the tip of the clamp overlying the lateral epicondyle, the fascia is incised. The tip of a 2.7-mm passing pin is placed at the LPFL attachment site; the pin is directed slightly anteriorly then advanced toward the medial side of the femur and out the medial femoral cortex (Fig 4A). A blind tunnel is then reamed into the femur the size of the doubled graft (Fig 4B). For a gracilis graft, this is usually 6 mm in diameter. Care is taken to keep shy of the far cortex.
Fig 3.
The appropriate location for the LPFL femoral attachment at the lateral epicondyle is identified, and a small 2- to 3-cm longitudinal incision is made at that site to allow for tunnel placement. Using a long, curved clamp, the selected soft-tissue interval is developed in the lateral retinaculum from the edge of the patella to the lateral epicondyle (left knee).
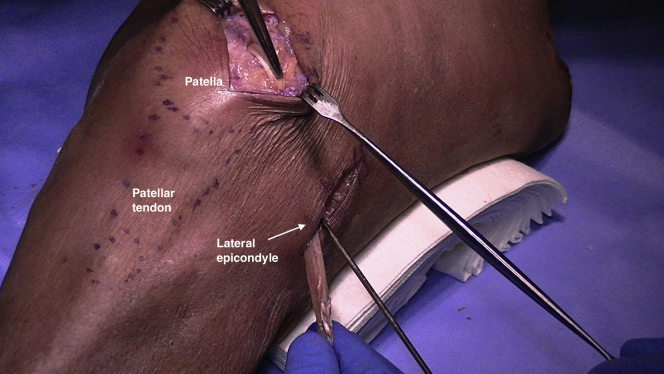
Fig 4.
(A) The tip of a 2.7-mm passing pin is placed at the lateral epicondyle; the pin is directed slightly anteriorly then advanced toward the medial side of the femur. (B) A blind tunnel is then reamed into the femur the size of the doubled graft (left knee).
Graft Passage and Fixation
Passing and securing the graft follow tunnel placement. The gracilis allograft is looped through the subperiosteal tunnel. With a passing suture, the free ends of the graft are then passed through the retinacular tunnel exiting at the epicondyle (Fig 5). The suture is passed through the passing pin, and the pin is then pulled out the medial femur to pass the graft into the femoral tunnel. Proper graft tension is obtained by holding the knee in approximately 30° of flexion with the patella reduced in the trochlea. After cycling the knee several times, a nitinol wire is placed into the tunnel and the graft is then secured to the LPFL attachment site with an interference screw (Arthrex); generally a 6 × 23 mm screw is sufficient. The periosteum is sutured to the graft, and then the retinaculum is closed over the graft with nonabsorbable suture (Fig 6). Patellar mobility is assessed, and quadriceps contraction is simulated with a towel clip to verify full excursion. Full knee range of motion should be achieved. Repeat arthroscopy is performed, demonstrating the patella to be centered and stable.
Fig 5.
The gracilis allograft is looped through the subperiosteal tunnel. With a passing suture, the free ends of the graft are then passed through the retinacular tunnel exiting at the epicondyle (left knee).
Fig 6.
The periosteum is sutured to the graft, and then the retinaculum is closed over the graft with nonabsorbable suture (left knee).
Closure
The wounds are irrigated copiously, and the tourniquet is released. All bleeding should be controlled. The iliotibial band and deep fascia are closed with a no. 0 Vicryl suture (Ethicon, Summerville, NJ). A medium Hemovac drain (Zimmer Surgical, Dover, OH) is placed in the wound (optional), and the subcutaneous layer and skin are closed in standard fashion. The leg is placed in a hinged knee brace locked in full extension. If used, the drain is removed on the first postoperative day.
Postoperative Protocol
Weight bearing as tolerated is allowed immediately postoperatively in a hinged knee brace locked in full extension. A home exercise program emphasizing passive knee range of motion and voluntary quadriceps control is started on the first postoperative day. Formal physical therapy is started 3 to 4 days after surgery once the indwelling catheter is removed. The leg is immobilized in a brace during weight-bearing activities for 4 to 6 weeks until limb control is sufficient to prevent rotational stress on the knee. Functional training of the limb, including rotational activities, is begun at 12 weeks. Patients are allowed to return to stressful activities, including sports, by 6 to 9 months after their reconstruction.
Discussion
The anatomical and biomechanical importance of the LPFL in preventing MPS has been recently appreciated.4 It is located in the deep layer of the lateral retinaculum and attaches to the superior-lateral aspect of the patella.10 The femoral insertion is at the lateral epicondyle with a fan-like expansion of the fibers predominantly in the posterior region proximal to the lateral epicondyle. The mean length of the LPFL is 42.1 mm, with a mean width of 16.1 mm. The LPFL has been shown to stabilize the patella and function as a passive restraint to medial patellar translation from full knee extension to approximately 30° of flexion.3 As such, reconstruction of the LPFL has gained in popularity as an effective operation to treat medial instability and has become a more commonly reported surgical technique for the treatment of MPS. Several methods of LPFL reconstruction have been described with primary differences consisting of graft choice and patellar fixation.5, 6, 7, 8, 9
Teitge and Torga Spak5 described a technique for LPFL reconstruction using an autograft that includes a portion of the quadriceps tendon as well as an attached bone block removed from the superior central one third of the patella. The bone block is countersunk into the femur at the lateral epicondyle and fixed with a lag screw. The tendon is passed through a transverse patellar bone tunnel, out the medial side, and sutured onto the anterior surface of the patella. Saper and Shneider7 described a technique of LPFL reconstruction using a superficial quadriceps tendon autograft. A partial-thickness graft, taken from the most superficial layer of the tendon, is harvested from the central third of the quadriceps tendon, leaving its patellar insertion intact. The end of the graft is turned laterally and attached at the lateral epicondyle with a knotless anchor. Borbas and colleagues8 reported a technique using a free gracilis autograft through 2 convergent patellar bone tunnels and fixed at the femur with an interference screw. Udagawa et al.6 reconstructed the LPFL with a gracilis autograft through a single transverse patellar tunnel. The graft was secured at both the femur and patella with suspensory fixation. Beckert et al. reported a technique using a 2-tailed semitendinosus allograft. The graft is fixed at the femur with suspensory fixation, and the 2 limbs are sutured to the anterior aspect of the patella.9
The described technique for LPFL reconstruction with a gracilis allograft is a simple procedure to address MPS with little associated morbidity. Advantages of this technique are that it is dependable and reproducible and is a simplification of graft fixation. It also avoids the use of bone tunnels, screws, and anchors in the patella, thereby avoiding the devastating complication of a patella fracture. As it relies on soft-tissue fixation at the patella, it can be used in both primary and revision cases and will not interfere with prior bone tunnels or anchors that may have been used in the setting of a medial patellofemoral ligament reconstruction.
There are a few concerns with the procedure worth noting. Nonanatomic femoral tunnel placement will result in inappropriate graft behavior during knee range of motion and produce suboptimal outcomes. Excessive lateral patellar constraint results in a painful, overconstrained patella. Symptomatic hardware can also occur when the femoral interference screw is left proud. Lastly, postoperative stiffness can occur if rehabilitation and aggressive motion are not encouraged after surgery.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Material support for this study was received from Summit Surgical, Seattle, WA.
Supplementary Data
Lateral patellofemoral ligament reconstruction using a gracilis allograft in a cadaveric left knee. After a 3- to 4-cm midline skin incision is made centered over the superior one-third of the patella, a 1-cm incision is placed in the periosteum at the level of the proximal patella. A second 1-cm incision is made at the lateral border of the patella. The two incisions are connected subperiosteally. The appropriate location for the LPFL femoral attachment at the lateral epicondyle is identified, and a small 2- to 3- cm longitudinal incision is made at that site to allow for tunnel placement. Using a long, curved clamp, the selected soft tissue interval is developed in the lateral retinaculum from the edge of the patella to the lateral epicondyle. The tip of a 2.7 mm passing pin is placed at the lateral epicondyle; the pin is directed slightly anteriorly then advanced toward the medial side of the femur. A blind tunnel is then reamed into the femur the size of the doubled graft. The gracilis allograft is looped through the subperiosteal tunnel. With a passing suture, the free ends of the graft are then passed through the retinacular tunnel exiting at the epicondyle. The periosteum is sutured to the graft, and then the retinaculum is closed over the graft with nonabsorbable suture.
References
- 1.Saper M.G., Shneider D.A. Medial patellar subluxation: diagnosis and treatment. Am J Orthop. 2015;44:499–504. [PubMed] [Google Scholar]
- 2.Betz R.R., Magill J.T., Lonergan R.P. The percutaneous lateral retinacular release. Am J Sports Med. 1987;15:477–482. doi: 10.1177/036354658701500508. [DOI] [PubMed] [Google Scholar]
- 3.Merican A.M., Kondo E., Amis A.A. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech. 2009;42:291–296. doi: 10.1016/j.jbiomech.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Kramers-de Quervain I.A., Biedert R., Stüssi E. Quantitative gait analysis in patients with medial patellar instability following lateral retinacular release. Knee Surg Sports Traumatol Arthrosc. 1997;5:95–101. doi: 10.1007/s001670050034. [DOI] [PubMed] [Google Scholar]
- 5.Teitge R.A., Spak R.T. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20:998–1002. doi: 10.1016/j.arthro.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Udagawa K., Niki Y., Matsumoto H. Lateral patellar retinaculum reconstruction for medial patellar instability following lateral retinacular release: a case report. Knee. 2014;21:336–339. doi: 10.1016/j.knee.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Saper M.G., Shneider D.A. Lateral patellofemoral ligament reconstruction using a quadriceps tendon graft. Arthrosc Tech. 2014;3:e445–e448. doi: 10.1016/j.eats.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borbas P., Koch P.P., Fucentese S.F. Lateral patellofemoral ligament reconstruction using a free gracilis autograft. Orthopedics. 2014;37:e665–e668. doi: 10.3928/01477447-20140626-66. [DOI] [PubMed] [Google Scholar]
- 9.Beckert M., Crebs D., Nieto M., Gao Y., Albright J. Lateral patellofemoral ligament reconstruction to restore functional capacity in patients previously undergoing lateral retinacular release. World J Clin Cases. 2016;4:202. doi: 10.12998/wjcc.v4.i8.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Navarro M.S., Navarro R.D., Akita Junior J., Cohen M. Anatomical study of the lateral patellofemoral ligament in cadaver knees. Rev Bras Ortop. 2008;43:300–307. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lateral patellofemoral ligament reconstruction using a gracilis allograft in a cadaveric left knee. After a 3- to 4-cm midline skin incision is made centered over the superior one-third of the patella, a 1-cm incision is placed in the periosteum at the level of the proximal patella. A second 1-cm incision is made at the lateral border of the patella. The two incisions are connected subperiosteally. The appropriate location for the LPFL femoral attachment at the lateral epicondyle is identified, and a small 2- to 3- cm longitudinal incision is made at that site to allow for tunnel placement. Using a long, curved clamp, the selected soft tissue interval is developed in the lateral retinaculum from the edge of the patella to the lateral epicondyle. The tip of a 2.7 mm passing pin is placed at the lateral epicondyle; the pin is directed slightly anteriorly then advanced toward the medial side of the femur. A blind tunnel is then reamed into the femur the size of the doubled graft. The gracilis allograft is looped through the subperiosteal tunnel. With a passing suture, the free ends of the graft are then passed through the retinacular tunnel exiting at the epicondyle. The periosteum is sutured to the graft, and then the retinaculum is closed over the graft with nonabsorbable suture.