Summary
New‐onset refractory status epilepticus (NORSE) is a rare condition where refractory seizures occur with no obvious cause in an otherwise healthy individual. We report here the first case of a patient with NORSE caused by Jamestown Canyon virus, an emerging virus throughout North America. This is the first patient with Jamestown Canyon virus encephalitis treated by a specific antiviral agent, in this case intravenous ribavirin, with electroencephalography (EEG) evidence of improvement. This is finally the first reported death caused by this virus, here secondary to intensive care unit complications. Therefore, Jamestown Canyon virus should be considered as a NORSE etiology, and ribavirin may be an effective treatment of that condition, especially if used early.
Keywords: Status epilepticus, Jamestown Canyon virus, New‐onset refractory status epilepticus, Ribavirin, EEG
Key points.
Jamestown Canyon virus is an emerging virus causing meningitis/encephalitis in North America
This is the first NORSE associated with Jamestown Canyon virus infection, causing moreover the first death reported with this virus, secondary to ICU complications
That patient showed however clear electroencephalograhic sign of improvement with intravenous ribavirin, a treatment never reported before for that condition
Introduction
New‐onset refractory status epilepticus (NORSE) is a rare condition where refractory seizures occur with no obvious cause in an otherwise healthy individual.1 Although auto‐immune etiology prevails as the most common final diagnosis (37%), a significant proportion is still considered cryptogenic (52%) and a proven infectious cause remains uncommon (8%).2
Jamestown Canyon virus is a rare RNA‐arbovirus classified within the California serogroup.3 Only 31 cases have been identified in the United States between 2000 and 2013, with no associated death.3 More than half of these patients had a meningitis/encephalitis presentation.
Here we report the case of a patient with a febrile illness evolving to NORSE who responded to intravenous ribavirin with undeniable electroencephalography (EEG) improvement. Unfortunately, the patient subsequently died from infectious complications.
Case report
A 31‐year‐old French‐Canadian man, living in a suburban area, presented to the emergency room in late August 2016 with a 3‐day history of headache, rigors, fever, and myalgia. Blood tests showed only mild lymphopenia and the patient was released with a diagnosis of viremia, treated with analgesic. Two days later, he presented again with 2 tonic–clonic seizures, without regaining consciousness, and leading to intubation along with anesthesia under propofol, combined with phenytoin and levetiracetam. Initial magnetic resonance imaging (MRI) was unremarkable. Lumbar puncture (LP) showed a mild elevation of cerebrospinal fluid (CSF) proteins (0.71 g/L, normal <0.45) without significant elevation of white blood cell (WBC) count, all other parameters being normal. He was then transferred to our tertiary center for neurological expertise.
Repetitive electrical seizures (starting from right anterior temporal region and then generalizing over 2 minutes) on continuous‐EEG monitoring led to numerous therapy trials against refractory status epilepticus, including lacosamide, topiramate, midazolam, ketamine, phenobarbital, ketogenic diet, pentobarbital, valproate acid, steroids, and magnesium. Every attempt to decrease anesthetic therapy led to electrical status epilepticus relapse.
On day 6 after initial presentation, a second LP demonstrated further elevation in protein (1.29 g/L) and WBC count (36, 100% monocytes). Comprehensive infectious and autoimmune testing was completed, including left frontal cortical and leptomeningeal biopsy, demonstrating a lymphocytic encephalitis. On day 34, a serological positive test for Jamestown Canyon virus was obtained, later confirmed by Plaque Reduction Neutralization Test (PRNT). Considering the fact that the patient was in ileus (probably caused by barbiturate, the ketogenic diet formulation used in our center favoring constipation and the long intensive care unit stay), intravenous ribavirin was obtained through Health Canada. Treatment started on day 41 (initial ribavirin bolus of 25 mg/kg, followed by 12 mg/kg q6 h for 4 days and then 6 mg/kg q8 h, planned for a total of 21 days). On continuous‐EEG monitoring, the patient demonstrated a significant improvement (Figures 1 and 2), with progressive and eventually complete disappearance of epileptiform activity on day 51 (day 10 of ribavirin therapy) while being able, in the meantime, to decrease anesthetics by about 80%.
Figure 1.
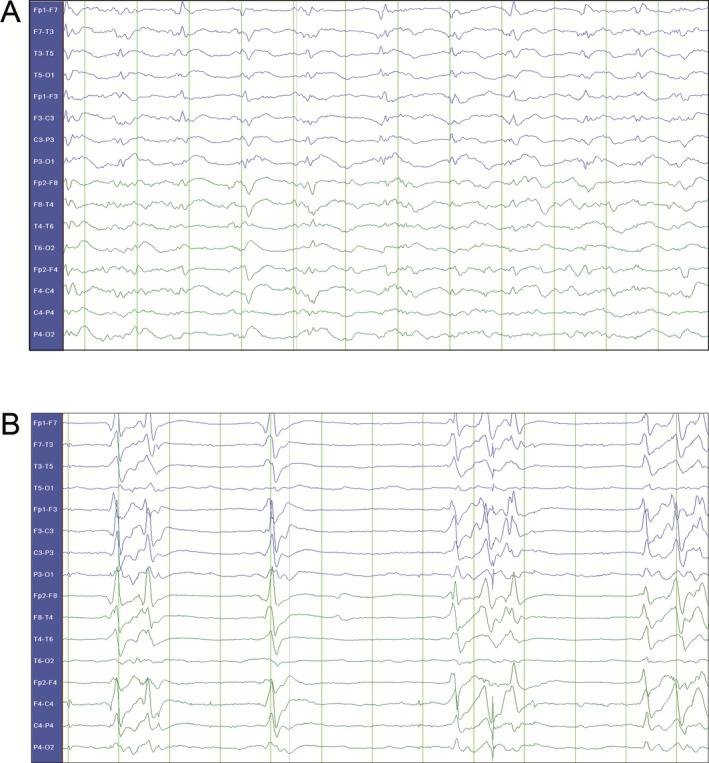
EEG monitoring initial evolution. (A) Generalized periodic discharges with epileptiform morphology on day 3 after initial presentation (anesthetic drug used: ketamine 40 mg/h and midazolam 40 mg/h), and (B) burst‐suppression with epileptiform discharges on day 44 after initial presentation, 3 days after the beginning of ribavirin (anesthetic drug uses: ketamine 450 mg/h, pentobarbital 1.5 mg/kg/h and midazolam 30 mg/h).
Figure 2.
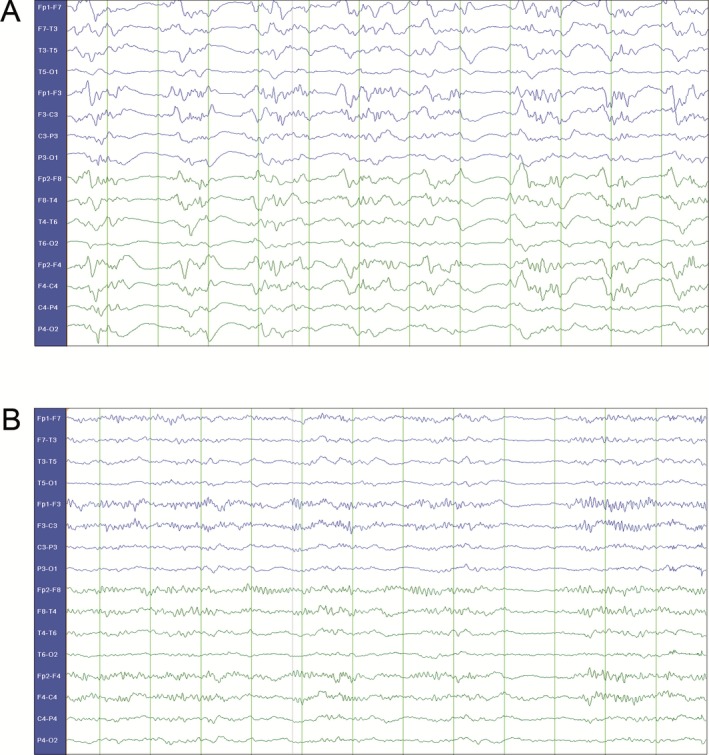
EEG monitoring late evolution. Progressive disappearance of epileptiform activity on continuous EEG monitoring: (A) On day 48, 7 days after the beginning of ribavirin (anesthetic drug used: ketamine 500 mg/h, midazolam 30 mg/h, pentobarbital ceased the day before), and (B) on day 51, 10 days after the beginning of ribavirin (anesthetic drug used: ketamine 150 mg/h and midazolam 30 mg/h). The last EEG is an anterior predominant alpha activity compatible with alpha coma, which may be caused by encephalitis aftermath, the anesthetic drugs, or both.
Unfortunately, the patient developed a septic shock at the same time, with profound metabolic imbalance, rapidly evolving to multiorgan failure and died within 24 hours. An intestinal origin was suspected based on multiple blood cultures positive for Enterococcus faecium.
Discussion
To the best of our knowledge, this is the first case of NORSE associated with Jamestown Canyon virus encephalitis. The initial febrile presentation, the LP profile, the seasonal timing (concordant with arboviral infection), in addition to northeastern USA/Québec being already recognized as a Jamestown Canyon emerging endemic region ( 5 cases, including our, were reported in the province of Quebec, Canada, in 2016),4 all strongly supported the serologic findings. It is also unfortunately the first death reported in the medical literature to be related to that virus, caused here by long intensive care unit (ICU) stay complications.
Moreover, this is the first report of intravenous ribavirin treatment in Jamestown Canyon virus encephalitis. This is an antiviral agent active against RNA virus.5 One study, using a randomized controlled trial, examined the efficacy of intravenous ribavirin in La Crosse encephalitis (also part of the California serogroup) in 15 children.6 Considering the low mortality of that condition (0.3‐1%) and despite significant neurological morbidity in these patients (12%),7 the study was stopped prematurely because of serious side effects (hyperammonemia in one, pancreatitis in another).6 Because our patient had a long ICU stay in refractory status epilepticus, we considered using ribavirin despite the reported risk.
Although we were unable to complete a neurological exam without sedation, the significant EEG improvement led us to believe that ribavirin threatment was effective since it was the only change done in our therapeutic approach at that time, even if it was late in the course of the disease. A timely diagnosis, which always represents a major challenge in a rare disease presenting in the ICU, may have led to a better outcome. We therefore support the concept that NORSE treatment should always target a specific etiology if possible.2 We also submit that Jamestown Canyon virus should be considered among these etiologies. Finally, intravenous ribavirin may be an effective treatment of this condition and should be considered, especially in such an aggressive presentation. More study considering the use of ribavirin in Jamestown Canyon virus infection would be of interest.
Disclosure
None of the authors has any conflicts of interest to disclose. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Biography
Martin Savard is a neurologist and neurocritical care consultant at Laval University, Quebec City.

References
- 1. Hirsh LJ, Gaspard N, van Baalen A, et al. Proposed consensus definition for new‐onset refractory status epilepticus (NORSE), febrile infection‐related epilepsy syndrome (FIRES), and related conditions. Epilepsia 2018;59:739–744. [DOI] [PubMed] [Google Scholar]
- 2. Gaspard N, Foreman BP, Alvarez V, et al. New‐onset refractory status epilepticus: Etiology, clinical features, and outcome. Neurology 2015;85:1604–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pastula DM, Smith DE, Beckham JD, et al. Four emerging arborviral diseases in North America: Jamestown Canyon, Powassan, chikungunya, and Zika virus diseases. J Neurovirol 2016;22:257–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ouhoummane N, Turcotte ME, Irace‐Cima A, et al. Rapport de surveillance du virus du Nil occidental et autres arbovirus: saison 2016. INSPQ. 31 août 2017.
- 5. Haddow AD, Haddow AD. The use of oral ribavirin in the management of La Crosse viral infections. Med Hypotheses 2009;72:190–192. [DOI] [PubMed] [Google Scholar]
- 6. McJunkin JE, Nahata MC, De Los Reyes EC, et al. Safety and pharmacokinetics of ribavirin for the treatment of la crosse encephalitis. Pediatr Infect Dis J 2011;30:860–865. [DOI] [PubMed] [Google Scholar]
- 7. McJunkin JE, de los Reyes EC, Irazuzta JE, et al. La Crosse encephalitis in children. N Engl J Med 2001; 344:801–807. [DOI] [PubMed] [Google Scholar]


