Abstract
We examined concurrency among sexual partners reported by men who have sex with men (MSM) with recent (acute or early) HIV infection in San Diego, California (2002-2015). Partners overlapping in time in the past 3 months were considered concurrent. Logistic generalized linear mixed models were used to identify factors associated with concurrency at the partner-level. 56% (388/699) of partners were concurrent to ≥1 other partner. The odds of concurrency were higher among partners >10 years younger than the participant (vs. within 10 years of age) (adjusted odds ratio [AOR]=2.22, 95% confidence interval [CI]: 1.09-4.52), longer term partners (AOR per month=1.02, 95% CI: 1.01-1.03), and partners met online (AOR=1.56, 95% CI: 0.98-2.48). Concurrency is common among partners of recently HIV-infected MSM. Tailored HIV prevention strategies for MSM with older partners, longer term partners, and partners met online may help minimize the potential impact of concurrency on HIV transmission.
Keywords: concurrency, acute and early HIV infection, HIV transmission, MSM
INTRODUCTION
Men who have sex with men (MSM) remain disproportionately affected by HIV in the United States with approximately two-thirds of HIV diagnoses among adults and adolescents in 2014 attributable to male-to-male sexual contact (1). Sexual partner concurrency (i.e., “overlapping sexual partnerships”) (2) is hypothesized to facilitate HIV transmission in the context of recent (acute or early) infection by enhancing the probability that one’s partners are exposed during their period of increased infectiousness following HIV acquisition (3,4). High rates of concurrency have been documented among MSM in the United States (5–8), and it has been estimated that MSM are 2-3 times as likely as heterosexual men to report concurrent partners in the past year (9). As such, concurrency may contribute to the continued burden of HIV infection among MSM in the United States.
Few epidemiologic studies have been adequately designed (10,11) to provide empirical evidence consistent with the synergistic effect of concurrency and recent HIV infection on transmission as demonstrated in simulation studies (12,13). Recognizing that concurrency’s potential impact on HIV transmission would manifest as an increased risk of HIV acquisition for one’s concurrent sexual partners, Rosenberg et al. utilized partner-level data collected from an online sample of MSM to examine concurrency at the partner-level and whether concurrency was more common among participants’ non-Hispanic, black sexual partners (14), and thus whether concurrency may at least partially explain the racial/ethnic disparities in HIV infection among MSM in the United States (15). While Rosenberg et al.’s work expanded our understanding of the implications of concurrency in terms of the potential risk of HIV acquisition for concurrent sexual partners, their analysis was restricted to sexual partners reported by MSM who did not report an HIV-positive serostatus. Given that concurrency is hypothesized to facilitate one’s risk of HIV transmission during recent infection, in the present study, we extended Rosenberg et al.’s approach to sexual partners reported by MSM with recent HIV infection. More specifically, we examined whether several known and likely risk factors for HIV infection measured at the partner-level (i.e., condomless anal intercourse, substance use during sex, meeting location, relationship type, partnership duration, sexual mixing patterns) are associated with concurrency at the partner-level. Evidence of such associations would provide additional insight on potential mechanisms (i.e., concurrency) underlying the influence of these factors on the risk of HIV acquisition as well as the types of sexual partners that may be placed at increased risk due to their partners’ concurrency during recent infection, which could ultimately inform the development of effective strategies to prevent the spread of HIV in the context of sexual partner concurrency among MSM.
METHODS
Study Population
From January 2002 to June 2015, 485 adults and adolescents (≥16 years of age) diagnosed with recent HIV infection at testing centers in San Diego, California were enrolled in the San Diego Primary Infection Resource Consortium (SD-PIRC) and offered partner services to facilitate HIV testing of their recent sexual and needle-sharing contacts. As previously described (8,16), through 2006, recent infection was documented among individuals reporting possible exposure to HIV or symptoms consistent with acute infection in the presence of one of the following: (1) negative HIV antibody (Ab) test (enzyme-linked immunoassay [EIA] or rapid test) followed by positive HIV Ab test in the past 12 months, (2) a negative HIV Ab test and positive HIV RNA, or (3) positive HIV Ab test and detuned EIA results consistent with early infection (Vironostika LS EIA, bioMerieux; Durham, NC). Starting in 2007, the Early Test protocol was implemented to screen for recent infection among all individuals seeking HIV testing: rapid HIV Ab testing followed by detuned EIA testing for those with positive rapid test results and HIV nucleic acid amplification testing (NAAT) for those with negative rapid test results (17). Acute infection was documented among rapid test negative and NAAT positive individuals, while early infection was documented among rapid test positive individuals with detuned test results consistent with early infection. Available clinical data (i.e., serology and date of last negative HIV test result) were used to calculate the estimated date of infection (EDI) for SD-PIRC participants (2002-2015) (18). All participants provided written informed consent.
Data Collection
As previously described (8), SD-PIRC participants completed computer-assisted self-interviews (CASIs) between January 2002 and November 2008 (Wave 1), May 2009 and May 2011 (Wave 2), or June 2011 and June 2015 (Wave 3). CASIs collected data on socio-demographics (age; race/ethnicity; education), sexual behaviors in the past three months (number of male sexual partners), and illicit drug use in the past three months (marijuana; methamphetamine; ecstasy; amyl nitrite; cocaine; gamma-hydroxybutyric acid; ketamine; heroin). Illicit drug use was not collected prior to 2003 during Wave 1. Detailed data were also collected on up to three partners in the past 12 months in Wave 1, up to two partners in the past three months in Wave 2, and up to three partners in the past three months in Wave 3. In relation to reported partners, CASIs collected data on their age, gender, race/ethnicity, HIV status, and meeting location (park, bathhouse, circuit party, through friends, bar or club, work or school, on a business trip or vacation, Internet, or other). Relationship type was also collected for each reported partner (except during CASIs completed prior to 2003 during Wave 1): main partner (someone you consider your primary sex partner, boyfriend, or spouse), regular partner (someone with whom you have had sex on a regular basis, but do not consider a main partner), friend (someone with whom you socialize and have had sex more than once on a non-regular basis), acquaintance (someone with whom you do not socialize, but have had sex more than once on a non-regular basis), one-time partner (someone with whom you had sex once and may have sex with again), unknown partner (someone with whom you had sex once, but could not contact again if you wanted to), or trade partner (someone with whom you exchanged money, drugs, or other goods for sex). Data on the timing of sexual intercourse with partners was collected by asking participants “How long ago did you first have sex with [partner]?” and “How long ago did you last have sex with [partner]?” in days, weeks, months, or years. Participants also reported on their sexual activity (e.g., any condomless anal intercourse [CAI] [Waves 1 and 2] and frequency of CAI [Wave 3]) and illicit drug use during sex with partners in the past 12 (Wave 1) or three (Waves 2 and 3) months.
Sexual Partner Concurrency
We classified partners with overlapping periods of sexual activity in the past three months as concurrent. As previously described (8), we first converted participants’ responses to questions about the timing of sexual intercourse with partners to days to identify their period of sexual activity with each partner (i.e., dates of first and last sexual intercourse). Next, we identified concurrent partners by examining the overlap between periods of sexual activity for each pair of partners reported by a participant. When periods of sexual activity with partners in a pair overlapped, those partners were considered concurrent. However, when periods of sexual activity with partners in a pair overlapped by only one day, the partners were not considered concurrent because we could not determine whether their periods of sexual activity truly overlapped or whether the participant’s period of sexual activity with one partner only began after that with the other partner had ended. Partners whose period of sexual activity with a participant was concurrent to that of at least one other partner reported by the participant were classified as having any concurrent partners.
Partner Characteristics
Partner-level data were used to classify each partner with respect to HIV status (HIV-negative vs. HIV-positive or status unknown), relationship type (main partnerships vs. casual partnerships with regular partners, friends, acquaintances, one-time partners, unknown partners, or trade partners), meeting location (Internet vs. other), any CAI in the past 12 (Wave 1) or three (Waves 2 and 3) months, and any illicit drug use during sex in the past 12 (Wave 1) or three (Waves 2 and 3) months. Sexual mixing patterns within partnerships were characterized with respect to age (partner >10 years younger than participant, partner and participant within 10 years of age, or partner >10 years older than participant) and race/ethnicity (partner of a different race/ethnicity than the participant vs. partner of the same race/ethnicity as the participant). Partnership duration in months was calculated based on the reported timing of sexual intercourse with partners.
Statistical Analysis
We restricted our analysis to 699 sexual partners reported by 299 SD-PIRC participants with recent HIV infection who were biologically male, completed CASIs within one year of their EDI, reported sex with a male in the past three months, and provided data needed to classify concurrency (Figure 1). To account for the correlation between partners reported by (i.e., nested within) the same participant, logistic generalized linear mixed models (GLMMs) were used to identify partner characteristics associated with concurrency at the partner-level. Although participants’ recent sexual contacts were recruited to participate in the study, there was not enough information in the data to fit models with multiple levels of nesting within participants. Thus, we excluded 10 participants who were recruited as sexual contacts of previously enrolled participants from the analysis. Unadjusted and adjusted odds ratios and corresponding 95% confidence intervals (CIs) were examined for several known and likely risk factors for HIV infection measured at the partner-level (i.e., CAI, substance use during sex, meeting location, relationship type, partnership duration, sexual mixing patterns). To control for participant characteristics and potential changes in behavior with partners following HIV diagnosis, the final model was also adjusted for participant age, race/ethnicity, number of male sexual partners (past three months), and enrollment year, as well as the timing of sexual partnership formation with respect to HIV diagnosis (i.e., before vs. after). In a sensitivity analysis, we excluded partners reported by participants who completed CASIs during the second data collection wave since partner-specific data were collected for fewer partners during Wave 2 compared to Waves 1 and 3. To understand their potential impact on HIV transmission, we examined whether the partner-level factors identified as associated with concurrency were also associated with HIV transmission behaviors (i.e., CAI). Finally, we examined differences in the proportion of main and casual partners with concurrent partners, and whether the type of relationship (casual only vs. ≥1 main) to concurrent partners differed for main and casual partners. SAS 9.4 (SAS Institute, Inc.; Cary, NC) was used to conduct all analyses.
Figure 1.
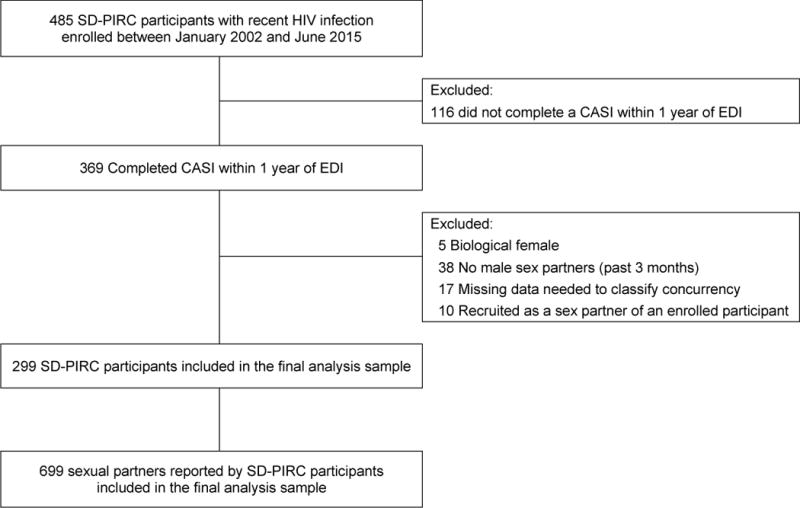
Flowchart of sexual partners reported by SD-PIRC participants included in the final analysis sample. Abbreviations: SD-PIRC = San Diego Primary Infection Resource Consortium; CASI = computer-assisted self-interview; EDI = estimated date of infection.
RESULTS
In our sample of MSM with recent HIV infection (N=299), 41% were under 30 years of age (median=33 years; IQR=26-41), 63% were white, non-Hispanic, and 90% reported at least some college education (Table 1). At enrollment, the median time since HIV infection was 85 days (IQR=40-103), while the median time since HIV diagnosis was 21 days (IQR=14-28). Illicit drug use was common within our sample with 59% of participants reporting any illicit drug use (excluding marijuana) in the past three months. Participants reported a median of six male sexual partners (IQR=2-11) in the past three months, with 54% reporting ≥1 concurrent partner.
Table I.
Characteristics of MSM with recent (acute or early) HIV infection enrolled in the San Diego Primary Infection Resource Consortium (2002-2015).
| (N=299) | ||
|---|---|---|
|
| ||
| n | % | |
| Data collection wave | ||
| Wave 1: January 2002 - November 2008 | 179 | 59.9 |
| Wave 2: May 2009 - May 2011 | 51 | 17.1 |
| Wave 3: June 2011 - June 2015 | 69 | 23.1 |
| Median days since EDI | 85.0 | IQR=40.0-103.0 |
| Median days since HIV diagnosis | 21.0 | IQR=14.0-28.0 |
| Age group (years) | ||
| 18-24 | 53 | 17.7 |
| 25-29 | 69 | 23.1 |
| 30-39 | 96 | 32.1 |
| ≥40 | 81 | 27.1 |
| Race/Ethnicity | ||
| White, non-Hispanic | 187 | 62.5 |
| Black, non-Hispanic | 15 | 5.0 |
| Hispanic | 69 | 23.1 |
| Othera | 28 | 9.4 |
| Education | ||
| Less than high school | 4 | 1.3 |
| High school graduate | 27 | 9.0 |
| Some college or university | 129 | 43.1 |
| Completed college or more education | 139 | 46.5 |
| Illicit drug use (past 3 months) | ||
| Any illicit drug useb | 126 | 58.6 |
| Marijuana | 100 | 46.5 |
| Amyl nitrite (poppers) | 86 | 40.0 |
| Methamphetamine | 60 | 27.9 |
| Ecstasy | 43 | 20.0 |
| Gamma-hydroxybutyric acid (GHB) | 39 | 18.1 |
| Cocaine | 31 | 14.4 |
| Ketamine | 11 | 5.1 |
| Heroin | 1 | 0.5 |
| Median # male sexual partners (past 3 months) | 6.0 | IQR=2.0-11.0 |
| Any concurrent sexual partners (past 3 months) | 157 | 53.8 |
Numbers may not sum to column total due to missing data; percentages may not sum to 100 due to rounding or omission of one category for binary variables.
Abbreviations: MSM=men who have sex with men; EDI=estimated date of infection; IQR=interquartile range.
Other includes: 13 Asian; 6 Native American; 5 Hawaiian or other Pacific Islander; 4 other race/ethnicity.
Excludes marijuana and missing for 84 participants (not collected from 2002 to 2003 during Wave 1).
Participants reported on 699 partners in the past three months (63% reported during Wave 1; 13% reported during Wave 2; 24% reported during Wave 3) with whom they had been in a sexual partnership for a median of 0.79 months (IQR=0.03-6.97) (Table 2). Of these partners, 80% were casual, 61% were within 10 years of age of the participant, 48% were of the same race/ethnicity as the participant, 41% were of an unknown HIV status, and 49% were met via the Internet. Illicit drug use (excluding marijuana) during sex was reported with 32% of partners and CAI was reported with 51% of partners. Overall, 56% of partners were concurrent to ≥1 other partner (57% of partners reported during Wave 1; 39% of partners reported during Wave 2; 61% of partners reported during Wave 3).
Table II.
Partner characteristics by concurrency among sexual partners reported by MSM with recent (acute or early) HIV infection enrolled in the San Diego Primary Infection Resource Consortium (2002-2015).
| Partner Characteristics | No concurrent partners (N=311) |
≥1 concurrent partner (N=388) |
Total (N=699) |
|||
|---|---|---|---|---|---|---|
| Median partnership duration (in months) | 0.03 | IQR=0.03-0.99 | 2.95 | IQR=0.13-11.77 | 0.79 | IQR=0.03, 6.97 |
| Relationship typea | ||||||
| Main partner | 42 | 16.4 | 73 | 23.0 | 115 | 20.1 |
| Regular partner | 12 | 4.7 | 42 | 13.3 | 54 | 9.4 |
| Friend/acquaintance | 51 | 19.9 | 114 | 36.0 | 165 | 28.8 |
| One-time partner | 64 | 25.0 | 44 | 13.9 | 108 | 18.9 |
| Anonymous (unknown) partner | 81 | 31.6 | 39 | 12.3 | 120 | 20.9 |
| Trade partner | 6 | 2.3 | 5 | 1.6 | 11 | 1.9 |
| HIV serostatus | ||||||
| HIV-negative | 105 | 34.7 | 174 | 45.8 | 279 | 40.9 |
| HIV-positive | 57 | 18.8 | 66 | 17.4 | 123 | 18.0 |
| HIV status unknown | 141 | 46.5 | 140 | 36.8 | 281 | 41.1 |
| Age mixing | ||||||
| >10 years younger than participant | 54 | 17.6 | 103 | 27.0 | 157 | 22.8 |
| Within 10 years of the participant’s age | 187 | 60.9 | 233 | 61.0 | 420 | 61.0 |
| >10 years older than participant | 66 | 21.5 | 46 | 12.0 | 112 | 16.3 |
| Race/ethnicity mixing | ||||||
| Different race/ethnicity than the participant | 151 | 49.2 | 207 | 54.3 | 358 | 52.0 |
| Same race/ethnicity as the participant | 156 | 50.8 | 174 | 45.7 | 330 | 48.0 |
| Met partner via the Internet | 135 | 44.1 | 203 | 52.3 | 338 | 48.7 |
| Any CAI with partner | 152 | 49.8 | 200 | 51.6 | 352 | 50.8 |
| Illicit drug use during sex with partner | ||||||
| Any illicit drug useb | 98 | 34.2 | 120 | 31.2 | 218 | 32.4 |
| Marijuana | 34 | 12.5 | 52 | 13.6 | 86 | 13.1 |
| Amyl nitrite (poppers) | 52 | 18.6 | 68 | 17.7 | 120 | 18.1 |
| Methamphetamine | 55 | 19.8 | 61 | 15.9 | 116 | 17.5 |
| Ecstasy | 12 | 4.4 | 10 | 2.6 | 22 | 3.4 |
| Gamma-hydroxybutyric acid (GHB) | 16 | 5.8 | 22 | 5.7 | 38 | 5.8 |
| Cocaine | 10 | 3.7 | 10 | 2.6 | 20 | 3.1 |
| Ketamine | 3 | 1.1 | 1 | 0.3 | 4 | 0.6 |
| Heroin | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
Numbers may not sum to column total due to missing data; percentages may not sum to 100 due to rounding or omission of one category for binary variables.
Abbreviations: MSM=men who have sex with men; IQR=interquartile range; CAI=condomless anal intercourse
Missing for 126 partners (not collected from 2003 to 2003 during Wave 1).
Excludes marijuana.
After adjusting for participant and partner characteristics, the odds of concurrency were higher among partners >10 years younger than the participant (vs. within 10 years of age) (adjusted odds ratio [AOR]=2.22, 95% CI: 1.09, 4.52), longer term partners (AOR per month=1.02, 95% CI: 1.01, 1.03), and partners met via the Internet (AOR=1.56, 95% CI: 0.98, 2.48) (Table 3). Our sensitivity analysis excluding partners reported by participants who completed CASIs during the second data collection wave yielded qualitatively similar results. CAI was more frequently reported with longer (≥6 months) than shorter (<6 months) term partners (OR=1.58, 95% CI: 1.08, 2.29), but neither sexual mixing with respect to age nor meeting partners via the Internet were associated with CAI.
Table III.
Partner characteristics associated with concurrency among sexual partners reported by MSM with recent (acute or early) HIV infection enrolled in the San Diego Primary Infection Resource Consortium (2002-2015).
| Partner Characteristics | OR (95% CI) | Adjusteda OR (95% CI) |
|---|---|---|
| Partnership duration (in months) | 1.02 (1.01, 1.03) | 1.02 (1.01, 1.03) |
| Main partner | 1.13 (0.71, 1.81) | 0.86 (0.47, 1.54) |
| HIV-negative partner | 1.42 (0.99, 2.05) | 1.27 (0.81, 1.99) |
| Age mixing | ||
| >10 years younger than participant | 1.47 (0.91, 2.38) | 2.22 (1.09, 4.52) |
| Within 10 years of the participant’s age | Ref | Ref |
| >10 years older than participant | 0.66 (0.40, 1.07) | 0.60 (0.32, 1.12) |
| Race/ethnicity mixing | ||
| Different race/ethnicity than the participant | Ref | Ref |
| Same race/ethnicity as the participant | 0.86 (0.59, 1.25) | 0.84 (0.52, 1.35) |
| Met partner via the Internet | 1.33 (0.92, 1.94) | 1.56 (0.98, 2.48) |
| Any CAI with partner | 1.09 (0.76, 1.55) | 0.82 (0.52, 1.30) |
| Illicit drug use during sex with partnerb | 0.96 (0.63, 1.46) | 1.03 (0.61, 1.74) |
Abbreviations: MSM=men who have sex with men; OR=odds ratio; CI=confidence interval; CAI=condomless anal intercourse.
N=498; In addition to the partner characteristics listed, the final model was adjusted for the participant’s age, race/ethnicity, number of male sexual partners (past 3 months), and enrollment year, as well as the timing of the participant’s HIV diagnosis relative to the formation of the sexual partnership (i.e., before vs. after).
Excluding marijuana.
Although there was no statistically significant association between relationship type and concurrency, 63% (73/115) of main partners were concurrent to another partner and 53% (244/458) of casual partners were concurrent to another partner. Compared to concurrent casual partners (64%; 155/244), a greater proportion of concurrent main partners overlapped with casual partners only (84%; 61/73) (chi-square test statistic=10.39, p-value=0.001; does not account for correlation between partners reported by the same participant as GLMM did not converge).
DISCUSSION
Using SD-PIRC data from 2002 to 2015, we found a high prevalence of concurrency among sexual partners (56%) reported by MSM with recent HIV infection in San Diego, California. This finding is consistent with that (58%) observed among sexual partners reported by a slightly younger (median age=26 years; IQR=21-36) and more racially and ethnically diverse (54% white, non-Hispanic; 16% black, non-Hispanic; 15% Hispanic) online sample of MSM who did not report being HIV-positive (14). Despite the fact that partners in our sample were reported by MSM with recent HIV infection, this consistency is expected given that concurrency is not hypothesized to increase one’s risk of HIV acquisition, but rather one’s risk of transmitting HIV from one concurrent sexual partner to another during the highly infectious period following HIV acquisition (2,4). Thus, the high prevalence of concurrency we observed among sexual partners of MSM with recent HIV infection underscores the potentially important role concurrency may play in sustaining the MSM HIV epidemic.
Nearly one quarter of the sexual partners reported by MSM in our sample were age discordant where the partner was at least 10 years younger than the participant. Compared to age concordant partners (i.e., the partner and the participant were within 10 years of age), these age discordant partners had twice the odds of having a concurrent partner. Previous research suggests that older partner selection is associated with HIV acquisition among young MSM, which has primarily been attributed to the elevated prevalence of HIV among older MSM (19–24). However, our findings suggest that concurrency among age discordant partnerships of MSM with recent HIV infection may also contribute to the increased risk of HIV infection experienced by young MSM with older partners.
We also found that longer term partners had a higher odds of concurrency, which may reflect an increased opportunity to acquire concurrent partners relative to partnerships of a shorter duration. Prior work suggests that HIV transmission risk behaviors (i.e., CAI) are associated with greater partner familiarity within both main (25–27) and casual (28–30) MSM partnerships. Given that 80% of partners reported by our sample were casual, our finding that a greater proportion of long-term partnerships engaged in CAI suggests that partnership duration may be linked to partner familiarity. However, familiarity may not always be an indicator of closeness or open communication between casual partners (29–31). One study found that engaging in CAI with partners assumed to be seroconcordant may be as common as engaging in CAI with partners known to be seroconcordant in the context of casual partnerships (32). Zablotska et al. argue that partner familiarity may facilitate HIV transmission within casual partnerships by fostering a “false sense of trust” and motivating CAI despite potentially limited communication about HIV serostatus or concurrency (29). Moreover, most concurrent main (84%) and casual (64%) partners in our sample overlapped with casual partners only. While casual partners concurrent to main partners may be protected by negotiated safety agreements made with main partners (e.g., agreements to consistently use condoms or practice other risk reduction strategies with outside partners) (33,34), such agreements are uncommon in the context of less intimate, casual partnerships. Although prior work suggests that 39% (35) to 68% (36) of HIV transmission events among MSM in the United States occur within main partnerships, our findings suggest that long-term, casual partners of MSM with recent HIV infection may be particularly vulnerable to HIV due to high rates of CAI coupled with concurrency.
Partners met via the Internet also had a higher odds of concurrency. Although CASIs listed the Internet as a location for meeting sexual partners, following the introduction of geosocial networking (GSN) applications in 2009, Wave 3 participants interpreted the Internet to mean online more generally and often reported meeting partners via both Internet websites (e.g., Adam4Adam.com and Manhunt.com) and GSN applications (e.g., Grindr and Jack’d). The popularity of online sex-seeking among MSM and the efficiency with which MSM are able to identify anonymous sexual partners online (37–39) has led to concerns about the impact of online sex-seeking on the spread of HIV/STIs (40,41). Previous research suggests MSM who engage in online sex-seeking more frequently report sexual risk behaviors, including CAI (42,43) and multiple sexual partners (38,42–45). Liau et al. proposed that these findings may be explained by online sex-seeking being more appealing to MSM who engage in sexual risk behaviors (self-selection hypothesis) and/or online sex-seeking promoting risk (accentuation hypothesis) (37). While research has more consistently provided support for the self-selection hypothesis (43,44), mixed findings have been reported with respect to the frequency of CAI with partners met online versus offline (43,46–50), and thus past research has provided less support for the accentuation hypothesis. While our findings neither prove nor disprove either hypothesis, we found that concurrency was more common among partners met online, which provides insight on how online sex-seeking could potentially enhance one’s risk of HIV acquisition and merits further examination in future research.
Our study had several limitations. First, partner-level and behavioral data may have been inaccurately or incompletely reported due to social desirability bias and recall bias. Although CASIs have been shown to minimize under-reporting due to social desirability bias (51,52), some partners may have been misclassified with respect to concurrency because our definition of concurrency relies on accurate reporting of the timing of sexual intercourse with reported partners. Second, participants reported a median of six sexual partners in the past three months, but data were only collected for up to three partners. As such, we may have underestimated the prevalence of concurrency and our findings may not be generalizable to all recent sexual partners of MSM with recent HIV infection. Third, the accuracy of data on partners’ age, race/ethnicity, and HIV serostatus is unknown because partners were not interviewed directly as part of SD-PIRC. Fourth, the CASIs administered across data collection waves varied slightly. More specifically, not all questions were asked during each data collection wave, which limited the availability of covariate data across waves. Furthermore, the number of partners for whom data were collected differed across waves (i.e., up to three partners during Waves 1 and 3; up to two partners during Wave 2) and may explain why fewer partners reported during Wave 2 were classified as concurrent. However, findings from our sensitivity analysis suggest that this had little impact on the factors identified as associated with concurrency at the partner-level. Finally, due to our small sample size we were unable to examine factors associated with concurrency by relationship type (i.e., main vs. casual).
Conclusions
We found that concurrency is common among sexual partners of MSM with recent HIV infection, which suggests that their sexual networks may be highly connected and thus amplify the spread of HIV. We also identified a relationship between concurrency and several risk factors for HIV among sexual partners. These findings provide insight on one possible mechanism by which these factors may increase one’s risk of HIV acquisition and shed light on the characteristics of sexual partners that may be placed at risk as a result of their partners’ concurrency during recent HIV infection. Targeted delivery of pre-exposure prophylaxis and other HIV prevention strategies to young MSM with older partners, MSM who meet partners on the Internet, MSM with casual partners, and MSM with longer term partners who may not perceive themselves to be at risk of HIV acquisition due to their partner’s concurrency could potentially minimize the impact of concurrency and help reduce HIV incidence among MSM.
Acknowledgments
Sources of Funding:
This work was supported by the National Institute on Drug Abuse [grant number K01 DA040543 to H.A.P.]; the National Institute of Allergy and Infectious Diseases [grant numbers U01 AI43638, R01 HD083042, R01 MH100974, R24 AI106039, P01 AI074621, P30 AI035214]; the California HIV Research Program [grant number RN07-SD-702]; and the California Collaborative Treatment Group [grant number El11-SD-005]. MK receives funding to the institution and has served on an advisory board to Gilead Sciences.
Footnotes
Conflicts of Interest
The authors have no other conflicts of interest to declare.
Ethical approval: UCSD’s Institutional Review Board approved the study protocol. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Centers for Disease Control and Prevention. Diagnoses of HIV Infection in the United States and Dependent Areas, 2014. HIV Surveillance Report. 2015;26 Availbale at: http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf. Accessed 26 August 2016. [Google Scholar]
- 2.UNAIDS. Consultation on concurrent sexual partnerships: recommendations from a meeting of the UNAIDS reference group on estimates, modelling and projecion held in Nairobi Kenya. 2009 Availbale at: http://www.epidem.org/sites/default/files/reports/Concurrency_meeting_recommendations_Updated_Nov_2009.pdf. Accessed 10 November 2015.
- 3.Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11(5):641–648. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Morris M, Goodreau SM, Moody J. Sexual networks, concurrency, and STD/HIV. In: Holmes KK, Sparling PF, Stamm WE, Piot P, Wasserheit J, editors. Sexually Transmitted Diseases. 4th. New York, NY: McGraw Hill; 2008. [Google Scholar]
- 5.Bohl DD, Raymond HF, Arnold M, McFarland W. Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sex Transm Infect. 2009;85(5):367–369. doi: 10.1136/sti.2009.036723. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg ES, Khosropour CM, Sullivan PS. High prevalence of sexual concurrency and concurrent unprotected anal intercourse across racial/ethnic groups among a national, Web-based study of men who have sex with men in the United States. Sex Transm Dis. 2012;39(10):741–746. doi: 10.1097/OLQ.0b013e31825ec09b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tieu HV, Nandi V, Frye V, et al. Concurrent partnerships and HIV risk among men who have sex with men in New York City. Sex Transm Dis. 2014;41(3):200–208. doi: 10.1097/OLQ.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pines HA, Wertheim JO, Liu L, Garfein RS, Little SJ, Karris MY. Concurrency and HIV transmission network characteristics among men who have sex with men with recent HIV infection. AIDS. 2016 doi: 10.1097/QAD.0000000000001256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glick SN, Morris M, Foxman B, et al. A comparison of sexual behavior patterns among men who have sex with men and heterosexual men and women. J Acquir Immune Defic Syndr. 2012;60(1):83–90. doi: 10.1097/QAI.0b013e318247925e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knopf A, Morris M. Lack of association between concurrency and HIV infection: an artifact of study design. J Acquir Immune Defic Syndr. 2012;60(1):e20–21. doi: 10.1097/QAI.0b013e3182460b79. author reply e21. [DOI] [PubMed] [Google Scholar]
- 11.Morris M. Barking up the wrong evidence tree. Comment on Lurie & Rosenthal, “Concurrent partnerships as a driver of the HIV epidemic in sub-Saharan Africa? The evidence is limited”. AIDS Behav. 2010;14(1):31–33. doi: 10.1007/s10461-009-9639-6. discussion 34-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eaton JW, Hallett TB, Garnett GP. Concurrent sexual partnerships and primary HIV infection: a critical interaction. AIDS Behav. 2011;15(4):687–692. doi: 10.1007/s10461-010-9787-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodreau SM, Cassels S, Kasprzyk D, Montano DE, Greek A, Morris M. Concurrent partnerships, acute infection and HIV epidemic dynamics among young adults in Zimbabwe. AIDS Behav. 2012;16(2):312–322. doi: 10.1007/s10461-010-9858-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenberg ES, Rothenberg RB, Kleinbaum DG, Stephenson RB, Sullivan PS. The implications of respondent concurrency on sex partner risk in a national, web-based study of men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2013;63(4):514–521. doi: 10.1097/QAI.0b013e318294bcce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wejnert C, Hess KL, Rose CE, Balaji A, Smith JC, Paz-Bailey G. Age-Specific Race and Ethnicity Disparities in HIV Infection and Awareness Among Men Who Have Sex With Men—20 US Cities, 2008-2014. J Infect Dis. 2016;213(5):776–783. doi: 10.1093/infdis/jiv500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drumright LN, Little SJ, Strathdee SA, et al. Unprotected anal intercourse and substance use among men who have sex with men with recent HIV infection. J Acquir Immune Defic Syndr. 2006;43(3):344–350. doi: 10.1097/01.qai.0000230530.02212.86. [DOI] [PubMed] [Google Scholar]
- 17.Morris SR, Little SJ, Cunningham T, Garfein RS, Richman DD, Smith DM. Evaluation of an HIV nucleic acid testing program with automated Internet and voicemail systems to deliver results. Ann Intern Med. 2010;152(12):778–785. doi: 10.1059/0003-4819-152-12-201006150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Le T, Wright EJ, Smith DM, et al. Enhanced CD4+ T-cell recovery with earlier HIV-1 antiretroviral therapy. N Engl J Med. 2013;368(3):218–230. doi: 10.1056/NEJMoa1110187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris M, Zavisca J, Dean L. Social and sexual networks: their role in the spread of HIV/AIDS among young gay men. AIDS Educ Prev. 1995;7(5 Suppl):24–35. [PubMed] [Google Scholar]
- 20.Service S, Blower SM. HIV transmission in sexual networks: an empirical analysis. Proc Biol Sci. 1995;260(1359):237–244. doi: 10.1098/rspb.1995.0086. [DOI] [PubMed] [Google Scholar]
- 21.Service SK, Blower SM. Linked HIV epidemics in San Francisco. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;11(3):311–313. doi: 10.1097/00042560-199603010-00016. [DOI] [PubMed] [Google Scholar]
- 22.Blower SM, Service SK, Osmond DH. Calculating the odds of HIV infection due to sexual partner selection. AIDS Behav. 1997;1(4):273–274. [Google Scholar]
- 23.Hurt CB, Matthews DD, Calabria MS, et al. Sex with older partners is associated with primary HIV infection among men who have sex with men in North Carolina. J Acquir Immune Defic Syndr. 2010;54(2):185–190. doi: 10.1097/QAI.0b013e3181c99114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin F, Grulich AE, Mao L, et al. Sexual partner’s age as a risk factor for HIV seroconversion in a cohort of HIV-negative homosexual men in Sydney. AIDS Behav. 2013;17(7):2426–2429. doi: 10.1007/s10461-012-0350-7. [DOI] [PubMed] [Google Scholar]
- 25.Davidovich U, de Wit JB, Stroebe W. Behavioral and cognitive barriers to safer sex between men in steady relationships: implications for prevention strategies. AIDS Educ Prev. 2004;16(4):304–314. doi: 10.1521/aeap.16.4.304.40398. [DOI] [PubMed] [Google Scholar]
- 26.Theodore PS, Duran RE, Antoni MH, Fernandez MI. Intimacy and sexual behavior among HIV-positive men-who-have-sex-with-men in primary relationships. AIDS Behav. 2004;8(3):321–331. doi: 10.1023/B:AIBE.0000044079.37158.a9. [DOI] [PubMed] [Google Scholar]
- 27.Hoff CC, Chakravarty D, Beougher SC, Neilands TB, Darbes LA. Relationship characteristics associated with sexual risk behavior among MSM in committed relationships. AIDS Patient Care STDS. 2012;26(12):738–745. doi: 10.1089/apc.2012.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prestage G, Van De Ven P, Grulich A, Kippax S, McInnes D, Hendry O. Gay men’s casual sex encounters: discussing HIV and using condoms. AIDS Care. 2001;13(3):277–284. doi: 10.1080/09540120120043928. [DOI] [PubMed] [Google Scholar]
- 29.Zablotska IB, Grulich AE, De Wit J, Prestage G. Casual sexual encounters among gay men: familiarity, trust and unprotected anal intercourse. AIDS Behav. 2011;15(3):607–612. doi: 10.1007/s10461-010-9675-2. [DOI] [PubMed] [Google Scholar]
- 30.Prestage G, Jin F, Grulich A, de Wit J, Zablotska I. Gay men are less likely to use condoms with casual sex partners they know ‘well’. AIDS Behav. 2012;16(3):664–668. doi: 10.1007/s10461-011-9952-8. [DOI] [PubMed] [Google Scholar]
- 31.Rouwenhorst E, Mallitt KA, Prestage G. Gay men’s use of condoms with casual partners depends on the extent of their prior acquaintance. AIDS Behav. 2012;16(6):1589–1596. doi: 10.1007/s10461-011-0092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zablotska IB, Imrie J, Prestage G, et al. Gay men’s current practice of HIV seroconcordant unprotected anal intercourse: serosorting or seroguessing? AIDS Care. 2009;21(4):501–510. doi: 10.1080/09540120802270292. [DOI] [PubMed] [Google Scholar]
- 33.Kippax S, Crawford J, Davis M, Rodden P, Dowsett G. Sustaining safe sex: a longitudinal study of a sample of homosexual men. AIDS. 1993;7(2):257–263. [PubMed] [Google Scholar]
- 34.Kippax S, Noble J, Prestage G, et al. Sexual negotiation in the AIDS era: negotiated safety revisited. AIDS. 1997;11(2):191–197. doi: 10.1097/00002030-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PloS one. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 37.Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33(9):576–584. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- 38.Phillips G, 2nd, Magnus M, Kuo I, et al. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behav. 2014;18(9):1630–1637. doi: 10.1007/s10461-014-0760-9. [DOI] [PubMed] [Google Scholar]
- 39.Cooper A. Sex and the Internet: a guidebook for clinicians. New York: Brunner-Routledge; 2002. [Google Scholar]
- 40.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284(4):447–449. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 41.Tashima KT, Alt EN, Harwell JI, Fiebich-Perez DK, Flanigan TP. Internet sex-seeking leads to acute HIV infection: a report of two cases. Int J STD AIDS. 2003;14(4):285–286. doi: 10.1258/095646203321264926. [DOI] [PubMed] [Google Scholar]
- 42.Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young internet-using men who have sex with men. Am J Public Health. 2008;98(6):1059–1067. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jenness SM, Neaigus A, Hagan H, Wendel T, Gelpi-Acosta C, Murrill CS. Reconsidering the internet as an HIV/STD risk for men who have sex with men. AIDS Behav. 2010;14(6):1353–1361. doi: 10.1007/s10461-010-9769-x. [DOI] [PubMed] [Google Scholar]
- 44.Lehmiller JJ, Ioerger M. Social networking smartphone applications and sexual health outcomes among men who have sex with men. PLoS One. 2014;9(1):e86603. doi: 10.1371/journal.pone.0086603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith DM, Drumright LN, Frost SD, et al. Characteristics of recently HIV-infected men who use the Internet to find male sex partners and sexual practices with those partners. J Acquir Immune Defic Syndr. 2006;43(5):582–587. doi: 10.1097/01.qai.0000243100.49899.2a. [DOI] [PubMed] [Google Scholar]
- 46.Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44(2):235–243. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- 47.Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue’s role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Arch Sex Behav. 2013;42(2):291–302. doi: 10.1007/s10508-011-9854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007;19(6):822–827. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- 49.Rosser BR, Miner MH, Bockting WO, et al. HIV risk and the internet: results of the Men’s INTernet Sex (MINTS) Study. AIDS Behav. 2009;13(4):746–756. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosser BR, Oakes JM, Horvath KJ, Konstan JA, Danilenko GP, Peterson JL. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s INTernet Sex Study-II (MINTS-II) AIDS Behav. 2009;13(3):488–498. doi: 10.1007/s10461-009-9524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 52.Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sex Transm Infect. 2005;81(5):421–425. doi: 10.1136/sti.2004.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]


