Abstract
HIV-positive individuals are at increased risk for kidney disease, including HIV-associated nephropathy, non-collapsing focal segmental glomerulosclerosis, immune-complex kidney disease, and comorbid kidney disease, as well as kidney injury resulting from prolonged exposure to antiretroviral therapy or from opportunistic infections. Clinical guidelines for kidney disease prevention and treatment in HIV-positive individuals are largely extrapolated from studies in the general population, and do not fully incorporate existing knowledge of the unique HIV-related pathways and genetic factors that contribute to the risk of kidney disease in this population. We convened an international panel of experts in nephrology, renal pathology, and infectious diseases to define the pathology of kidney disease in the setting of HIV infection; describe the role of genetics in the natural history, diagnosis, and treatment of kidney disease in HIV-positive individuals; characterize the renal risk-benefit of antiretroviral therapy for HIV treatment and prevention; and define best practices for the prevention and management of kidney disease in HIV-positive individuals.
Keywords: Antiretroviral therapy, APOL1, CKD progression, HIV, Immune complex kidney disease, Podocytopathy, Renal pathology
INTRODUCTION
Worldwide, an estimated 37 million people are living with HIV infection, and more than 2 million new infections are diagnosed annually.1 HIV-positive individuals are at increased risk for both acute and chronic kidney disease (CKD). The classic kidney disease of HIV infection, HIV-associated nephropathy (HIVAN), has become less common with widespread use of antiretroviral therapy (ART); however, there has been a simultaneous increase in the prevalence of other kidney diseases. HIV-positive individuals are also exposed to life-long ART, with the potential to cause or exacerbate kidney injury. Newer guidelines recommending earlier initiation of ART may further reduce the incidence of HIVAN, but the overall risk-benefit for kidney health is unknown.
Clinical guidelines for CKD prevention and treatment in HIV-positive individuals are extrapolated from studies in the general population,2 and current therapies do not target unique HIV-related pathways and genetic factors that contribute to CKD progression. In March 2017, Kidney Disease: Improving Global Outcomes (KDIGO) convened a multidisciplinary, international panel of clinical and scientific experts to identify and discuss key issues relevant to the optimal diagnosis and management of kidney disease in HIV-positive individuals. The primary goals were to define the pathology of kidney disease in the setting of HIV infection; describe the role of genetics in the natural history, diagnosis, and treatment of kidney disease in HIV-positive individuals; characterize the renal risk-benefit of ART; and define best practices to delay the progression of kidney disease and to treat end-stage kidney disease (ESKD) in HIV-positive individuals.
RENAL PATHOLOGY IN THE SETTING OF HIV INFECTION
The spectrum of renal pathology in HIV-positive individuals is diverse, including lesions directly related to intrarenal HIV gene expression and lesions related to co-morbidities, drug effects, immune dysregulation, and co-infections.3 Kidney biopsy is required to distinguish between these lesions. A useful approach to classification is based on the major tissue compartment affected (Table 1). A brief description of each histologic lesion is provided below, and more comprehensive descriptions are available in the Supplementary Appendix.
Table 1.
Pathologic classification of HIV-related kidney diseases
| I. Glomerular Dominant* |
| a. Podocytopathies (all characterized by extensive foot process effacement)** |
| i. Classic HIVAN |
| ii. FSGS (NOS) in the setting of HIV |
| iii. Minimal change disease in the setting of HIV |
| iv. Diffuse mesangial hypercellularity in the setting of HIV |
| v. Other podocytopathy in the setting of HIV |
| b. Immune complex-mediated glomerular disease* |
| i. IgA nephropathy in the setting of HIV |
| ii. Lupus-like glomerulonephritis in the setting of HIV |
| iii. Lupus nephritis in the setting of HIV |
| iv. Membranous nephropathy in the setting of HIV |
| • Indicate whether HBV positive, HCV positive, PLA2R positive (should not preclude workup for other secondary causes) |
| v. Membranoproliferative pattern glomerulonephritis in the setting of HIV |
| • Indicate whether HCV positive (should not preclude workup for other secondary causes) |
| vi. Endocapillary proliferative and exudative glomerulonephritis in the setting of HIV |
| • Post-streptococcal, staphylococcal-associated, other |
| vii. Fibrillary or immunotactoid glomerulonephritis in the setting of HIV |
| viii. Other immune complex disease in the setting of HIV |
|
|
| II. Tubulointerstitial Dominant* |
| a. Tubulointerstitial injury in the setting of classic HIVAN |
| i. Hyaline droplet tubulopathy |
| ii. Tubular microcysts |
| iii. Tubulointerstitial inflammation |
| b. Acute tubular injury/ acute tubular necrosis |
| i. Ischemic |
| ii. Toxic (associated with ART vs other) |
| c. Drug-induced tubulointerstitial nephritis (other than ART) |
| i. Antibiotics |
| ii. Proton pump inhibitors |
| iii. NSAIDs |
| iv. Other |
| d. Direct renal parenchymal infection by pathogens (bacterial, viral, fungal, protozoal, etc.) |
| e. Immunologic dysfunction-related tubulointerstitial inflammation |
| i. Diffuse infiltrative lymphocytosis syndrome (DILS) |
| ii. Immune restoration inflammatory syndrome (IRIS) |
| f. Other tubulointerstitial inflammation in the setting of HIV |
|
|
| III. Vascular Dominant* |
| a. Thrombotic microangiopathy in the setting of HIV |
| b. Arteriosclerosis |
|
|
| IV. Other, in the setting of HIV infection |
| a. Diabetic nephropathy |
| b. Age-related nephrosclerosis |
Indicate the likelihood of HIV causality
Indicate association with APOL1 risk allele genotype
ART, antiretroviral therapy; HBV, hepatitis B virus; HCV, hepatitis C virus; FSGS, focal segmental glomerulosclerosis; HIV, human immunodeficiency virus; HIVAN, HIV-associated nephropathy; NSAID, nonsteroidal anti-inflammatory drug.
Glomerular dominant diseases: Podocytopathy
Glomerular dominant diseases include two main subcategories: podocytopathies and immune complex-mediated.
Four major subtypes of podocytopathy are seen in the setting of HIV: classic HIVAN, focal segmental glomerulosclerosis (FSGS) not otherwise specified (NOS), and rarer cases of minimal change disease and diffuse mesangial hypercellularity.4 All exhibit extensive podocyte foot process effacement and proteinuria, with absent or minimal immune complex deposition. There is a well-established causal relationship between HIVAN and HIV infection, mediated by direct HIV infection of renal epithelial cells, intrarenal viral gene expression, and dysregulation of host genes governing cell differentiation and cell cycle.5 The role of genetic susceptibility in the pathogenesis of HIVAN and other podocytopathies is discussed in detail in the next section.
We recommend distinguishing classic HIVAN from FSGS (NOS) in the setting of HIV infection. Direct causality of HIV can only be established with reasonable certainty in classic HIVAN and congenital cases of podocytopathy in infants born to HIV-positive mothers. We recommend that the biopsy report should indicate the degree of certainty that the pathology is causally related to HIV infection as high, moderate, or low.
Classic HIVAN
Classic HIVAN is defined as collapsing glomerulopathy and attendant tubulointerstitial disease, including tubular microcyst formation, interstitial inflammation, and tubular injury (Figure 1).6, 7 Glomerular “collapse” is defined as at least one glomerulus with collapse of glomerular basement membranes accompanied by hypertrophy and hyperplasia of the overlying glomerular epithelial cells. These hyperplastic cells may fill the urinary space, forming “pseudocrescents.”8, 9
Figure 1. Classic HIVAN and FSGS (NOS) in the setting of HIV.
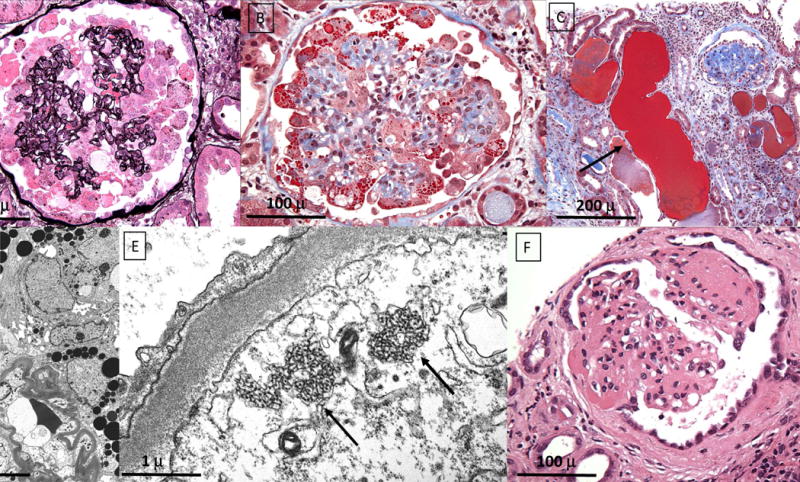
Classic HIVAN (A–E) shows typical global collapse of the glomerular tuft with loss of luminal patency and hypertrophy and hyperplasia of the overlying glomerular epithelial cells, some of which contain intracytoplasmic protein resorption droplets. (A, Jones methenamine silver x400; B, Masson trichrome, x400). The tubulointerstitium shows focal tubular microcysts containing glassy casts, associated with tubular atrophy, interstitial fibrosis and inflammation (C, Masson trichrome, x200). There is marked foot process effacement overlying the collapsed capillaries associated with glomerular epithelial cell hyperplasia forming a pseudocrescent. Some glomerular epithelial cells contain numerous intracytoplasmic protein resorption droplets. No immune type electron dense deposits are seen. (D, electron micrograph x4000). The glomerular endothelial cells contain multiple intracytoplasmic tubuloreticular inclusions (arrows). Foot processes are effaced. (E, electron micrograph, x40,000). FSGS (NOS) in the setting of HIV shows discrete segmental scars with segmental adhesions to Bowman’s capsule. No collapsing features or glomerular epithelial cell hyperplasia are identified. (F, H&E, x400).
By electron microscopy, diffuse podocyte foot process effacement and endothelial tubuloreticular inclusions (“interferon footprints”) are classic features.6, 7 By immunofluorescence, there may be staining for IgM, C3, and C1q in collapsed segments and mesangial areas.7 Protein resorption droplets may stain for albumin and immunoglobulin. In late stages, the sclerotic tuft is retracted into a tight solid sphere, capped by a monolayer of cobblestone epithelium; this has been described as resembling a “fetal glomerulus.”10 Phenotypic studies suggest that the glomerular epithelial cell monolayer is composed of parietal epithelial cells.8 In some cases, sequential biopsy and post-mortem studies have shown an evolution from collapsing glomerulopathy to FSGS (NOS).7
Tubulointerstitial disease is an invariable component of HIVAN and often appears out of proportion to the glomerular disease,6, 7 causing kidney enlargement and hyperechoic appearance by ultrasound. Tubular “microcysts” are dilated tubules (at least 3-fold larger than normal) containing glassy proteinaceous casts and lined by simplified epithelium. Tubular microcysts are easily distinguished from tubular “thyroidization” based on their larger diameter, irregular size, and the absence of tubular atrophy or colloid type casts.11 The microcysts may involve all tubular segments, and intracellular viral transcript expression has been demonstrated.12 Prominent interstitial inflammation7 and tubular degenerative and regenerative changes may also occur.13 Interstitial edema in the acute phase is followed by fibrosis and tubular atrophy.
FSGS (NOS) in the setting of HIV
In ART-treated patients, non-collapsing FSGS (NOS) is more commonly encountered at biopsy.9, 14–16 Causality is presumed when no other etiology for FSGS can be identified. Viral load is often undetectable, and biopsy findings may be difficult to distinguish from arterionephrosclerosis of hypertension, aging, and APOL1-associated nephropathy. Such cases typically lack prominent tubulointerstitial disease, and the degree of podocyte effacement is generally less severe than in HIVAN (Figure 1). These differences have been hypothesized to reflect attenuation of the renal phenotype by ART.9
Podocytopathy in perinatal HIV infection
In addition to classic HIVAN, children with perinatal HIV infection can present with minimal change disease or diffuse mesangial hypercellularity with numerous endothelial tubuloreticular inclusions and marked foot process effacement.17 Tubular microcysts and interstitial inflammation are often lacking. Such cases are rare in the ART era.
Glomerular dominant diseases: Immune complex kidney disease in the setting of HIV
Numerous forms of immune complex-mediated glomerular disease have been reported in HIV-positive individuals.18 We recommend that the commonly used term “HIV immune complex kidney disease” (HIVICK) be replaced with a specific description of the pattern of immune complex disease “in the setting of HIV.” The rationale for this approach is the heterogeneous spectrum of disease and the lack of certainty of HIV causality in most cases. Early studies that eluted glomerular immune deposits and demonstrated immune complexes containing HIV antigen and specific anti-HIV antibody were performed on a small number of well-characterized cases in the research setting and are not practicable in routine pathology laboratories.19, 20 Reflex diagnosis as “HIVICK” may preclude workup for other secondary, treatable causes.
A unique lupus-like nephritis with full house immune staining but with negative serologies and no clinical signs of systemic lupus erythematosus has been reported in HIV-positive individuals;21 true lupus nephritis also occurs.22 It remains unclear whether IgA nephropathy in the setting of HIV is coincidental and related to undergalactosylated IgA1, or due to deposition of IgA directed to viral antigen, as demonstrated in one well-characterized case.19 An unusual ultrastructural appearance of subepithelial deposits, or “ball in cup” lesion, has been described in reports from South Africa,10, 23 but is rarely observed in other settings. Other secondary causes should be sought in cases of membranous nephropathy (i.e., hepatitis B virus co-infection or anti-PLA2R autoantibodies) and membranoproliferative glomerulonephritis (hepatitis C virus co-infection).24–26
Tubulointerstitial disease in the setting of HIV
As described above, classic HIVAN is a pan-nephropathy with an important tubulointerstitial component;6, 7 in biopsies with undersampled glomeruli, the characteristic glomerular lesions may not be demonstrable. Acute tubular necrosis may occur in association with sepsis, volume depletion, and other ischemic or toxic insults.4 The commonly used antiretroviral agent tenofovir disoproxil fumarate can cause proximal tubulopathy with characteristic dysmorphic mitochrondria (Figure 2).27 Tubulointerstitial nephritis can occur secondary to antibiotics, proton pump inhibitors, nonsteroidal anti-inflammatory drugs, protease inhibitors, and other medications, as well as in response to mycobacterial infection.28–30 Direct infection of the renal parenchyma by other pathogens can also occur.7
Figure 2. Tenofovir nephrotoxicity.
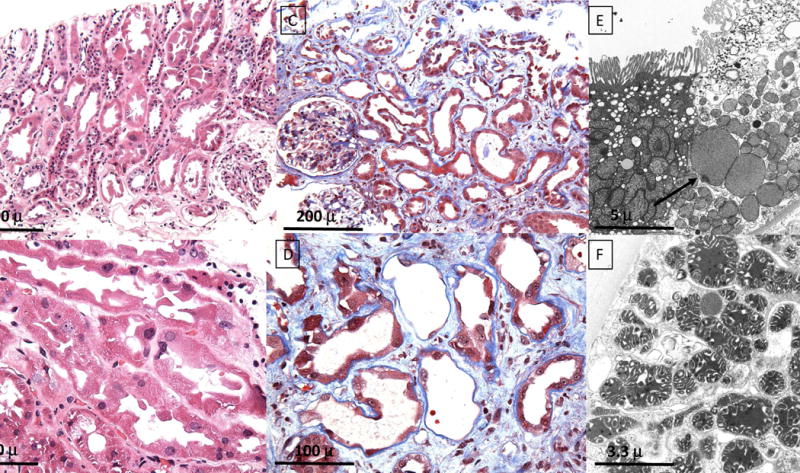
Acute tenofovir nephrotoxicity is characterized by irregular proximal tubular profiles with atypical, irregular lining epithelial cells and mild interstitial edema (A, H&E, x200). The atypical proximal tubular cells display loss of brush border, marked irregularity of tubular epithelial height and shape, focal shedding of cytoplasmic fragments, and enlarged atypical nuclei with prominent nucleoli (B, H&E, x400). Chronic nephrotoxicity displays increased separation of the irregular proximal tubules by interstitial fibrosis and mild inflammation with focal tubular atrophy (C, Masson trichrome, x200). The tubules show focal loss and flattening of lining epithelium leaving some desquamated tubular basement membranes, as well as prominent epithelial simplification and irregularity with atypical nuclei. There is intervening interstitial fibrosis and mild inflammation, without tubulitis (D, Masson trichrome, x400). The characteristic features are focal giant mitochondria with few residual peripheral cristae (arrow) within the proximal tubular epithelial cells, as well as cytoplasmic swelling with disruption of brush border, (E, electron micrograph x8000). In some cases, the dysmorphic mitochrondria exhibit irregular size and shape with bizarre patterning of their cristae (F, electron micrograph x12,000).
Two rare but distinct forms of tubulointerstitial injury relate to immunologic dysfunction in the setting of HIV infection. Diffuse infiltrative lymphocytosis syndrome (DILS) is a hyperimmune reaction against HIV that involves the kidneys in approximately 10% of cases.31–33 Immune restoration inflammatory syndrome (IRIS) is an inflammatory disorder associated with paradoxical unmasking or worsening of preexisting infectious processes after ART initiation,34 rarely involving the kidney. Both conditions are characterized by prominent CD8 T-cell infiltrates.
Vascular dominant diseases in the setting of HIV
Thrombotic microangiopathy was reported in the early years of the AIDS epidemic, but is rare in the ART era.35 A role for direct endothelial dysregulation by HIV has been proposed.36
Other pathologies in the setting of HIV
As patients with HIV infection age, comorbid kidney diseases such as diabetic nephropathy and arterionephrosclerosis are increasingly common. When secondary FSGS develops in these contexts, the potential overlap with HIV-related podocytopathy can be diagnostically challenging. Molecular approaches demonstrating renal epithelial cell infection by HIV have been used in the research setting for decades, but have not been incorporated into routine diagnostic practice.37 In addition to these established approaches, several novel and emerging techniques could be incorporated into research and diagnostic renal pathology to better characterize the causal relationship between HIV and specific histologic lesions and to further delineate the host pathways involved. The conference attendees identified several particularly relevant techniques (Supplementary Table 1).38, 39
GENETICS/ GENOMICS OF KIDNEY DISEASE IN THE SETTING OF HIV INFECTION
Classic HIVAN occurs predominantly in individuals of African ancestry, with 18–50 fold increased prevalence.40 Two mapping by admixture linkage disequilibrium studies published in 2008 identified a region on chromosome 22 strongly associated with idiopathic FSGS and HIVAN in African Americans;41, 42 however, fine-mapping revealed no coding variants to explain the association of intronic single nucleotide polymorphisms in the candidate gene MYH9 with kidney disease.43, 44 Subsequently, using data from the ‘1000 Genomes Project,’ Genovese et al. identified 2 missense variants (G1 allele) and a 6 bp deletion (G2 allele) in the adjacent APOL1 gene that were recessively associated with FSGS and non-diabetic ESKD.45 APOL1 encodes apolipoprotein L1, which confers innate immunity against most strains of Trypanosoma brucei;46, 47 G2 variants extend immunity to T.b. rhodesiense and G1 associates with asymptomatic carriage of T.b.gambiense, the causes of acute and chronic African human trypanosomiasis, respectively.45, 48 Coding variants in APOL1 are present only on African-ancestry haplotypes.49, 50
APOL1 was strongly associated with FSGS (odds ratio [OR] 17) and HIVAN (OR 29) in African Americans and with HIVAN in South Africans (OR 89).49, 51 In contrast, HIV-positive Ethiopians, who lack APOL1 risk variants, do not develop HIVAN.52 Subsequent studies have confirmed the strong association between the high-risk genotypes and the diagnosis of HIVAN (Table 2). The estimated lifetime risk associated with carrying two APOL1 risk alleles is 4% for FSGS in the absence of HIV infection, and as high as 50% for HIVAN (Supplementary Table 2).53 Despite the strong association, ~20–30% of African Americans with HIVAN have zero or one APOL1 risk allele, suggesting that other genetic, viral, or environmental factors contribute to HIVAN.54 Characteristics of APOL1-mediated kidney disease are summarized in Table 3.
Table 2.
Prevalence of APOL1 high-risk genotypes and association with kidney disease in HIV-positive African Americans and Black South Africans
| Histology | Population | Population Controls | Cases | Odds Ratio (95% CI) | Reference |
|---|---|---|---|---|---|
| HIVAN | African-American (n=54) | 13% | 72% | 29 (14, 68) | 49 |
| HIVAN | African-American (n=60) | 13% | 62% | – | 54 |
| HIVAN | South Africa (n=38) | 3% | 79% | 89 (18, 912) | 51 |
| HIV+ FSGS | African-American (n=35) | 13% | 63% | – | 57 |
| HIV+ FSGS | South Africa (n=22) | 3% | 8% | 2.1 (0.03, 44) | 51 |
| HIV+ ICD | African-American (n=31) | 13% | 3% | – | 57 |
| HIV+ ICD | South Africa (n=12) | 3% | 25% | 5.6 (0.4, 86) | 51 |
APOL1, apolipoprotein L1; CI, confidence interval; FSGS, focal segmental glomerulosclerosis; HIV, human immunodeficiency virus; HIVAN, HIV-associated nephropathy; ICD, immune complex kidney disease.
Table 3.
Features of APOL1-mediated kidney disease in the setting of HIV
| References | |
|---|---|
| • MYH9 variants are not independently associated with HIVAN or FSGS (NOS) | 45, 52, 152 |
| • APOL1 kidney disease manifests as HIVAN or FSGS (NOS) with or without microcystic tubular dilatation | 49, 56, 57 |
| • S342G and N388Y389/- confer risk of kidney disease; therefore genotyping only the G1 rs73385319 missense and G2 rs71785313 indel (i.e., insertion–deletion mutations) variants are sufficient to determine risk of CKD | 49 |
| • HIVAN is associated with low CD4+ cell counts, and often improves with effective ART | 56 |
| • HIV-associated FSGS is associated with higher CD4+ cell counts and occurs in patients undergoing ART | 56 |
| • APOL1 high-risk genotypes are associated with progression to ESKD in HIV-positive patients with non-HIVAN kidney diseases | 57 |
| • Histological features of HIVAN in patients carrying two copies of APOL1 risk variants are similar to those carrying 0 or 1 copies | 54 |
| • High-risk genotypes predict FSGS (NOS) or HIVAN, but kidney biopsy is required to distinguish between these two diagnoses | 56 |
| • HIV-infected children with CKD and high-risk genotypes have lower eGFR and experience more rapid progression | 58, 153 |
| • Multiple mechanisms have been proposed for APOL1-mediated podocyte injury, but they converge in perturbations of endosomal trafficking, increased membrane permeability, and cytotoxicity | 61, 63 – 65 |
| • APOL1, a component of the innate immune system, is up-regulated by interferons | 61, 62 |
| • High levels of APOL1 may be a “second hit” and sufficient to cause kidney disease | 61, 62 |
APOL1, apolipoprotein L1; ART, antiretroviral therapy; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; ESKD, end-stage kidney disease; FSGS (NOS), focal segmental glomerulosclerosis, not otherwise specified; HIV, human immunodeficiency virus; HIVAN, HIV-associated nephropathy.
The distribution of the APOL1 coding variants varies greatly among sub-Saharan African populations, with the highest frequencies reported in Western Africa (> 40% for G1) and much lower frequencies elsewhere in Africa (Supplementary Figure 1).50, 52, 55 As a consequence of the West African diaspora to the Americas and more recent African emigrations, APOL1 variants are widely dispersed globally (e.g., 21% and 13% for G1 and G2, respectively, in African Americans).45, 50
Prediction of histology
Given the strong genetic association, investigators in the United States (US) evaluated whether APOL1 genotype could be used to predict HIVAN or FSGS (NOS) histology in HIV-positive patients of African descent.56 Inclusion of the high-risk genotype did not significantly add to a predictive model including CD4+ cell count and HIV-RNA, suggesting that APOL1 genotype cannot replace kidney biopsy for definitive diagnosis of HIVAN.
Carriage of APOL1 high-risk genotypes in HIV-positive individuals is not associated with immune complex kidney disease (Table 2). In a US series, high-risk genotypes were present in only 3% of patients with biopsy-proven immune complex disease.57 Similarly, in a South African series, high-risk genotypes were present in 79% of HIVAN cases but in only 25% of those with HIV and immune complex kidney disease.51
Renal survival/ESKD risk
In general population studies, the high-risk APOL1 genotypes have been associated with increased risk of CKD progression and with lower estimated glomerular filtration rate (eGFR).58 In children with perinatal HIV infection, those with a high-risk genotype had a 3-fold increased odds of CKD and presented at a younger median age compared with those with zero or one risk allele.51 In HIV-positive adults with non-HIVAN kidney disease on biopsy, carriage of two APOL1 risk alleles was associated with more rapid progression and a 2-fold greater risk of ESKD.57 Carriage of two APOL1 risk alleles has been associated with proteinuria in HIV-infected women and with accelerated decline in longitudinal kidney function in unsuppressed HIV-infected men.59, 60
Mechanisms of APOL1-mediated disease
Two APOL1 risk alleles are required to confer increased risk of kidney disease. However, the presence of high-risk genotypes in healthy populations suggests that disease expression requires a “second hit,” such as infections (e.g., HIV, viral hepatitis, and others), interferon, gene-gene interactions, illicit drug use, and other CKD risk factors.
The mechanism of APOL1-mediated kidney disease is currently unknown. Evidence from in vitro experiments in human cells and APOL1 transgenic mouse models suggests that interferon upregulates APOL1 expression, causing podocyte injury.61, 62 Intracellular apolipoprotein L1 in renal epithelium may cause apoptosis or autophagy by increasing cellular and mitochondrial membrane permeability.63–65 In cell culture, G1 and G2 APOL1 variants induce intracellular loss of potassium, cell swelling, and cell lysis.66 Studies in yeast, Drosophila, and human cells indicate that variant apolipoprotein L1 depolarizes cell membranes, which disrupts intracellular processes including endosomal trafficking, vesicle acidification, and mitochondrial function.63–65
In vivo, the expression of high-risk APOL1 variants in transgenic mouse models has produced variable effects. In a model with inducible APOL1 expression, high-risk variants disrupted endosomal trafficking and vesicle acidification, similar to the effects observed in vitro. Affected animals developed podocyte death, proteinuria, and glomerulosclerosis.61 However, another transgenic mouse model with constitutive expression of APOL1-G2 did not develop kidney disease.67
APOL1 is encoded in the genome of only a few primate species, complicating the extrapolation of data from murine models. Mechanistic studies have also been limited by the use of overexpression assays. In vitro, the overexpression of wildtype APOL1-G0 in cultured human renal epithelial cells also induces cell death, suggesting that the overexpression model may not be biologically relevant.62, 68, 69
ANTIRETROVIRAL THERAPY (ART) NEPHROTOXICITY
HIV treatment guidelines recommend immediate initiation of ART in all HIV-positive individuals. Immunovirological control is an important strategy to reduce the incidence of acute kidney injury (AKI) and HIV-related kidney diseases.70–73
The presence of CKD affects the choice and dosing of renally-cleared antiretrovirals. Kidney function and CKD risk factors should be assessed prior to ART initiation (Figure 3). CKD risk scores have been developed to guide clinicians, although future studies are needed to determine their utility in diverse populations (Supplementary Table 3).74, 75
Figure 3. Recommendations at starting ART.
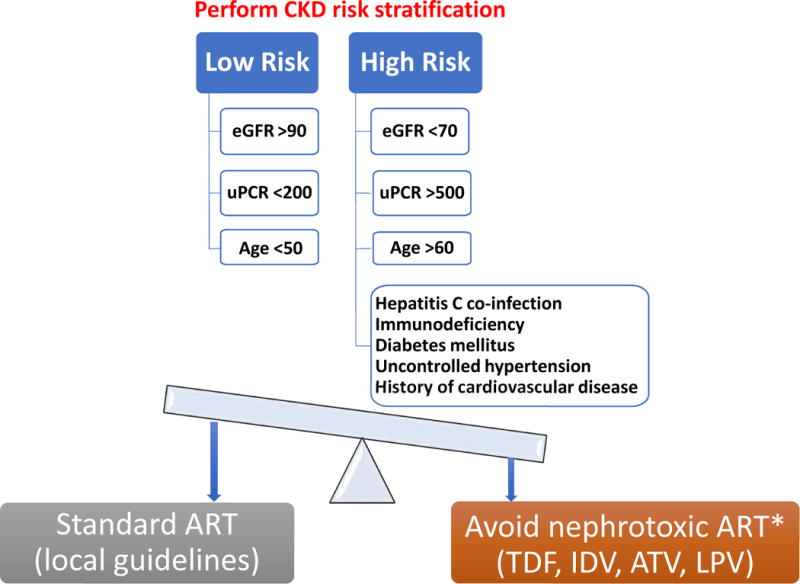
*if suitable alternatives available
ART, antiretroviral therapy; ATV, atazanavir; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate (CKD-EPI, expressed in ml/min/1.73 m2); IDV, indinavir; LPV, lopinavir; TDF, tenofovir disoproxil fumarate; uPCR, urine protein:creatinine ratio (values above are in mg/g; multiply by 0.10 to obtain values in mg/mmol).
The widely used antiretroviral agent tenofovir disoproxil fumarate (TDF) is generally safe and well tolerated, but has important potential for cumulative nephrotoxicity. Subclinical proximal tubular dysfunction (low level proteinuria and excessive phosphaturia) is common, and approximately 1–2% of recipients develop treatment-limiting tubulopathy.76 Risk factors for tubulopathy include aging, immunodeficiency, diabetes, prolonged exposure, and concomitant use of didanosine or ritonavir-boosted protease inhibitors.77 Severe tubulopathy may progress to eGFR decline, osteomalacia, and pathological fractures. In large observational studies, TDF has also been associated with decreased eGFR or creatinine clearance,78, 79 as well as with rapid eGFR decline and proteinuria.78, 79 Co-administration of TDF with ritonavir-boosted protease inhibitors increases the risk.78, 79 Although not well studied, the newer pharmacoenhancer cobicistat also increases tenofovir exposure and may increase the risk of toxicity. TDF discontinuation and switches from TDF to the newer prodrug tenofovir alafenamide (TAF) have been associated with improved kidney function, although the long-term safety of TAF is not known.80–83
Any drug (antiretroviral or other) may cause interstitial nephritis. New onset eGFR decline or proteinuria should prompt careful review of CKD risk factors and medications.29, 84 Among antiretrovirals, atazanavir and indinavir have been most commonly linked to interstitial nephritis and nephrolithiasis; other protease inhibitors have been implicated in case reports.85–89
Observational cohort studies have also linked atazanavir and lopinavir/ritonavir to rapid eGFR decline and incident CKD,78, 79 and switching from ritonavir-boosted atazanavir or lopinavir to boosted darunavir has been associated with improved kidney function.90 In settings where TAF, abacavir, and darunavir are available, the use of TDF, atazanavir, and lopinavir/ritonavir should ideally be avoided in those with CKD, rapid eGFR decline (> 3–5 ml/min/1.73 m2 per year), or at high CKD risk. The threshold for avoiding or discontinuing these agents may be influenced by local circumstances. In resource-limited settings, TDF dose adaptation may be an option. Dual therapy (i.e., boosted protease inhibitor plus lamivudine or raltegravir) has been proposed as a way to avoid concomitant use of boosted protease inhibitors with TDF, thereby minimizing the nephrotoxic potential.91–93
Pharmacological considerations
Several antiretrovirals require dose adjustment in individuals with decreased eGFR (Supplementary Table 4). If continued use of TDF is required when eGFR is < 60 ml/min/1.73 m2 (or < 70 ml/min/1.73 m2 with eGFR decline), dose adjustment should be considered.
Drug-drug interactions are common with ART. Several antiretrovirals induce or inhibit absorption (through P-glycoprotein), hepatic metabolism (through the cytochrome P450 system or glucuronidation), and/or tubular excretion (through organic anion/cation transporters, multidrug resistant/multidrug and toxin extrusion proteins) of co-administered medications. We recommend that clinicians consult available resources such as www.hiv-druginteractions.org.
CKD PROGRESSION AND ESKD IN THE SETTING OF HIV INFECTION
Risk factors for CKD
Both HIV-related and traditional CKD risk factors influence CKD development and progression (Figure 4). With improved longevity among HIV-positive individuals, traditional CKD risk factors, particularly hypertension and diabetes, are of increasing concern worldwide.94–96 Hepatitis B virus (HBV) and hepatitis C virus (HCV) co-infections are associated with a 2- to 3-fold increased risk of progressive CKD.97, 98 Other co-infections such as tuberculosis and syphilis may also contribute to CKD risk.99–101 In addition, severe AKI has been associated with a 3.8- to 20-fold increased risk of progression to ESKD.102
Figure 4. Risk factors and underlying etiologies of CKD in HIV-positive individuals.
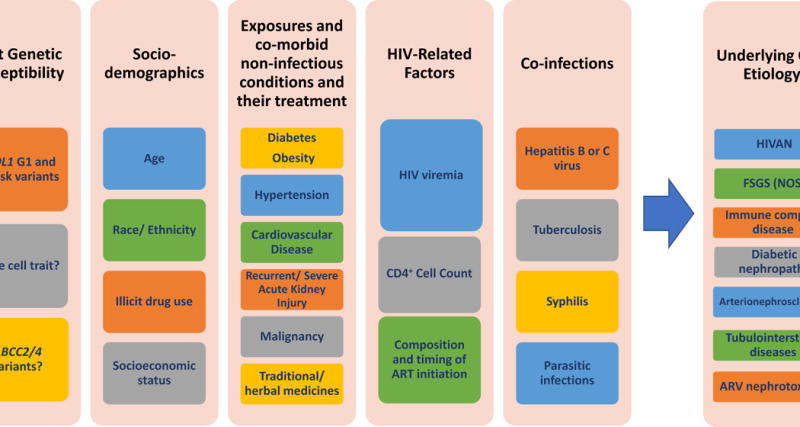
APOL1, apolipoprotein L1; ABCC, ATP-binding cassette transporter proteins; ARV, antiretrovial; CKD, chronic kidney disease; FSGS (NOS), focal segmental glomerulosclerosis, not otherwise specified; GN, glomerulonephritis; HIV, human immunodeficiency virus; HIVAN, HIV-associated nephropathy.
CKD screening and monitoring
Studies to inform the optimal CKD screening and monitoring strategies among HIV-positive individuals are lacking. Until such studies exist, current CKD guidelines should be followed.2, 103 CKD screening is recommended at the time of HIV diagnosis and ART initiation or modification (Figure 5).
Figure 5. Recommendations for kidney disease screening and monitoring in HIV-positive adults.
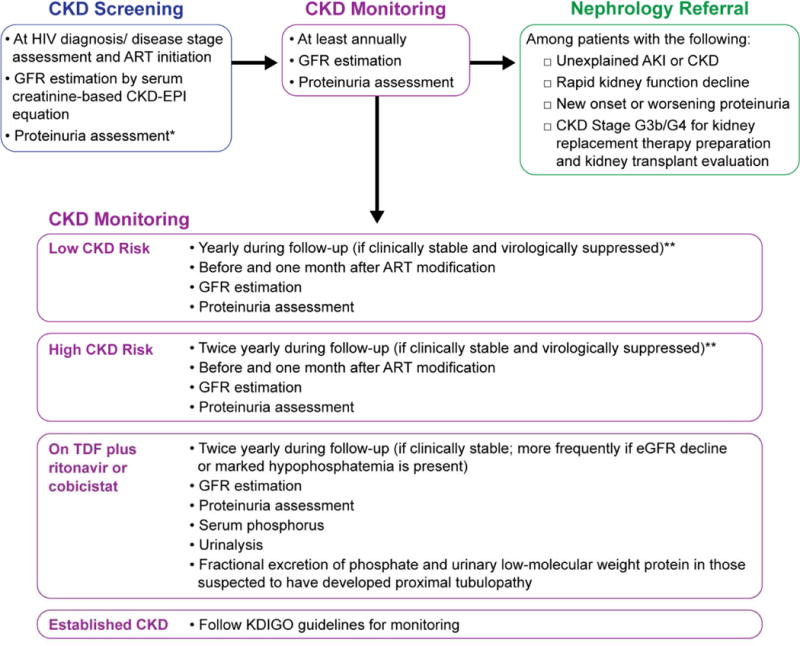
*Urinalysis should be performed in all HIV-positive individuals to detect worsening or new onset of proteinuria or hematuria. Where feasible, quantification of proteinuria (spot urine albumin:creatinine or protein:creatinine ratio) should also be performed.
**More frequent monitoring is recommended in persons who are clinically unstable, severely immunocompromised, or viremic.
AKI, acute kidney injury; ART, antiretroviral therapy; CKD, chronic kidney disease; CKD-EPI, CKD Epidemiology Collaboration; GFR, glomerular filtration rate; HIV, human immunodeficiency virus; KDIGO, Kidney Disease: Improving Global Outcomes; TDF, tenofovir disoproxil fumarate.
Serum creatinine is the preferred biomarker for estimating GFR.2, 103 Serum cystatin C may be considered in patients receiving medications that alter tubular creatinine handling. Cystatin C may also better predict long-term mortality,104, 105 but is susceptible to bias in the setting of inflammation. The serum creatinine-based CKD-EPI equation is generally preferred;2, 103 however, none of the available estimates have been validated in diverse populations or in the setting of drugs that alter creatinine secretion.106–108 Use of the antiretrovirals dolutegravir or rilpivirine or the pharmacoenhancers ritonavir or cobicistat may result in average reductions in calculated creatinine clearance of around 5–20 ml/min, which should be taken into account when interpreting eGFR or creatinine clearance.109 Clinicians should also be aware that serum creatinine measurements may not be standardized in resource-limited regions and that extrarenal factors may alter both serum creatinine and cystatin C concentrations (Supplementary Table 5).110–112 Rather than a single eGFR value, eGFR trajectories are useful for identifying individuals with progressive decline in kidney function.
Urinalysis should be performed in all HIV-positive individuals to detect worsening or new onset of proteinuria or hematuria. Where feasible, quantification of proteinuria (urine albumin:creatinine or protein:creatinine ratio) should also be performed. In individuals on TDF, urinalysis may also detect glycosuria, and plasma phosphate should be monitored if possible. Evaluation of cystatin C, low molecular weight (“tubular”) proteinuria, or phosphate reabsorption is not indicated in individuals with stable kidney function and no indication of TDF toxicity.113
In most HIV-positive individuals who are stable on ART, annual monitoring of kidney function appears appropriate. In those with or at increased risk of CKD and those who receive TDF with ritonavir- or cobicistat-boosted protease inhibitors, more frequent monitoring is recommended, typically 2–4 times per year depending on risk factors.113 Kidney function should also be carefully monitored during hospitalization, particularly in individuals receiving TDF and concomitant nephrotoxic medications.
If CKD is identified, patients should undergo work-up based on available resources and risk-stratification, including consideration of potential medication toxicity, screening for hypertension, diabetes, and co-infections, and assessment of region-specific risk factors such as traditional medicines. HIV-specific CKD risk scores may facilitate risk-stratification,74, 75 although these scores have not been validated in diverse populations or in resource-limited settings (Supplementary Table 3). Referral to nephrology should be considered in certain settings (Figure 5).103 When the cause of CKD is unclear, CKD progression is rapid, or prognostication is needed, a kidney biopsy should be considered.
CKD management
Evidence from observational studies strongly supports the beneficial effect of early ART initiation on the risk of classic HIVAN.114 The impact of ART on CKD progression in patients with immune complex kidney diseases is more variable.71, 72 Given the overwhelming benefit on survival, ART is recommended for all HIV-positive individuals.115 Evaluation of other treatment strategies for kidney disease in the setting of HIV has been limited to small, single-center studies with short duration, and has focused largely on HIVAN (Supplementary Table 6). No rigorous study has evaluated the efficacy of blood pressure control, diabetes treatment, or ACE-inhibitors and angiotensin receptor blockers in slowing CKD progression in HIV-positive individuals. However, extrapolating from the strong evidence supporting the efficacy of these interventions in the general population is reasonable (Table 4).103, 116, 117 Treatment of HBV, HCV, and tuberculosis co-infections should be considered based on existing treatment guidelines.118–121
Table 4.
Recommendations for management of CKD risk factors in HIV-positive individuals
| Risk Factor | Recommendations |
|---|---|
| Hypertension | |
| Non - proteinuric | • Target systolic blood pressure ≤140 mmHg116 |
| Proteinuric | • Target systolic blood pressure ≤130 mmHg116 • Preferred antihypertensive: ACE inhibitors or angiotensin receptor blockers116 |
| Diabetes mellitus | • Target hemoglobin A1c ~7%*103 |
| Hepatitis B virus co - infection | • Treat per existing guidelines118, 121 •TAF may be used in patients with eGFR ≥ 30 ml/min/1.73 m2.154 • Where TAF is unavailable or in patients with eGFR < 30 ml/min/1.73 m2, dose-adjusted TDF or entecavir may be considered. |
| Hepatitis C virus co - infection | • Treatment per existing guidelines120, 155 • In patients with HCV genotypes 1 or 4 and CKD G4/5, ribavirin-free grazoprevir and elbasvir regimens may be effective.156–158 • In patients with genotypes 2, 3, 5 or 6, sofosbuvir-based regimens are required; however, sofosbuvir-based regimens should be avoided or alternate-day sofosbuvir dosing should be considered in patients with eGFR <30 ml/min/1.73 m2.159–161 In addition, the combination of ledipasvir/sofosbuvir with TDF should be avoided. |
Kidney replacement therapy (KRT) in HIV-positive individuals
With ART, survival of HIV-positive individuals receiving KRT is comparable to their HIV-negative counterparts.122 Therefore, HIV serostatus should not influence candidacy for KRT. Observational studies demonstrate similar outcomes between hemodialysis (HD) and peritoneal dialysis (PD) among ART-treated individuals, and modality selection depends upon patient preference and regional resources.123, 124 Arteriovenous fistulas are the preferred vascular access, as arteriovenous grafts and catheters are associated with higher risk of infection and thrombosis.125 There is no evidence supporting isolation of HIV-positive patients in HD units, except those with HBV co-infection.126 Dialyzer reuse by the same patient is practiced in resource-limited settings as a cost-saving alternative. Evidence supporting the safety of dialyzer reuse by HIV-positive individuals is limited,127, 128 and precautions to avoid HIV transmission to other patients and dialysis staff must be adhered to. HIV-positive PD patients may have higher risk of PD-catheter infections; however, PD catheter failure rates are similar to that of HIV-negative patients.129 PD consumables must be discarded properly, as HIV persists in PD materials and fluid.130, 131
Kidney transplantation in HIV-positive individuals
Kidney transplantation in HIV-positive recipients is associated with excellent 1-year and 3-year recipient and allograft survival rates, intermediate to those observed in the overall US kidney transplant population and in a higher risk subgroup of recipients ≥ 65 years.132 Registry data also suggest good 5- and 10-year outcomes, with an improvement in survival compared to patients who remain on the waitlist.133 Studies in other settings have confirmed the safety of kidney transplantation in individuals with well-controlled HIV.132, 134–138 Eligible patients with advanced CKD and well-controlled HIV infection should be referred for kidney transplant evaluation (Table 5).
Table 5.
Selection criteria for potential HIV-positive kidney transplant recipients
| ➤ Meets standard criteria for kidney transplant recipients, PLUS the following: |
| ➤ Effective HIV suppression for ≥6 months prior to transplantation |
| • Undetectable plasma HIV-1 RNA |
| • CD4+ cell count >200 cells/mm3 |
| ➤ No active opportunistic infections |
| ➤ No prior history of: |
| • Progressive multifocal leukoencephalopathy |
| • Primary central nervous system lymphoma |
| • Pulmonary aspergillosis |
| • Visceral Kaposi’s sarcoma |
| • Coccidiomycosis |
| • Chronic intestinal cryptosporidiosis >1 month |
| ➤ Hepatology evaluation for patients co-infected with hepatitis B or hepatitis C virus et al. and Muller E et al.132, 137 |
Criteria adapted from Stock HIV, human immunodeficiency virus.
Immunosuppressant protocols for the general population can be applied to HIV-positive individuals. In view of the increased immunological risk, some centers prefer induction therapy with an interleukin-2 receptor antagonist, polyclonal antithymocyte globulin, or alemtuzumab.132, 134, 139 Tacrolimus is the calcineurin inhibitor of choice for maintenance immunosuppression.132,140
Existing guidelines for prophylaxis against opportunistic infections141, 142 and management of hepatitis co-infection should be followed.143, 144 HCV-co-infected recipients have poorer outcomes compared to recipients with HIV or HCV mono-infection, but still superior to those who remain on the waitlist. Clinicians should be aware of significant drug-drug interactions among immunosuppressive agents, ART, and antiviral medications for HCV co-infection. To minimize drug-drug interactions and achieve steady-state drug levels, integrase inhibitors and nucleoside reverse transcriptase inhibitors are the preferred antiretroviral agents, while protease inhibitors and the pharmacoenhancers ritonavir and cobicistat are best avoided.145 Given the complexity of issues, a multidisciplinary team comprising experts in transplant nephrology, infectious disease, and clinical pharmacology is imperative.
Given the strong association between the APOL1 risk variants and HIVAN, HIV-positive recipients of African descent and those who receive an allograft from a donor of African descent should be monitored for recurrent HIVAN.146 The relative contribution of donor and recipient APOL1 risk status to the risk of HIVAN recurrence is the subject of ongoing research. The APOL1 Long-term Kidney Transplantation Outcomes (APOLLO) Research Network147 will investigate the influence of donor APOL1 risk variants on long-term outcomes among recipients and African American donors, including those with HIV.
Based on experience in South Africa, there is growing evidence to support the safety of kidney transplantation from HIV-positive donors.148, 149 The US HIV Organ Policy Equity (HOPE) Act allows the use of organs from HIV-positive donors in approved research programs.150, 151 Questions remain about the implications of super-infection in settings where ART resistance is common.
CHILDREN AND ADOLESCENTS WITH HIV
As in adults, CKD screening and monitoring are recommended, and ART should be provided as per international and regional guidelines (Supplementary Table 7).2, 115
CONCLUSION
Despite improved survival with ART, HIV-positive individuals remain at increased risk for kidney disease. This report summarizes recommendations for diagnosis, management, and prevention of kidney disease in this population, including a proposed histologic classification. In the absence of data from randomized controlled trials, these recommendations reflect the expert opinion of conference attendees, incorporating combined clinical experience and evidence from observational studies and laboratory research. A second major outcome of this conference was the identification of knowledge gaps and areas for future research (Table 6), with the long-term goal of improving the diagnosis and management of kidney disease in HIV-positive individuals.
Table 6.
Controversies, knowledge gaps, and areas for future research
| Renal pathology |
| • What is the spectrum of renal pathology in the setting of HIV infection in the current era and in diverse patient populations? |
| • How do pathologic features correlate with the duration of ART, HIV viral load, racial and geographic origin, and APOL1 risk allele genotype? |
| • What is the relative contribution of de-differentiated podocytes versus parietal epithelial cells to the glomerular epithelial cell hyperplasia seen in HIVAN? |
| • What are the roles of specific HIV transcript expression in promoting proliferation and possible transdifferentiation of podocytes and parietal epithelial cells, and in mediating the tubular phenotype of cell cycle arrest and microcyst formation? |
| • What is the pattern of HIV viral transcript expression in specific renal cell types and tissue compartments in FSGS (NOS) and other non-HIVAN lesions in the setting of HIV? |
| • Is FSGS (NOS) in the setting of HIV representative of attenuated or partially treated HIVAN? |
| • How can immune complex disease that is causally related to HIV infection be distinguished from coincident disease? |
| • Can HIV infection of renal dendritic cells, infiltrating monocyte/macrophages, or intrinsic renal epithelial cells produce a viral reservoir that is capable of reactivation? |
| • What is the composition of the inflammatory infiltrates in HIV-related tubulointerstitial disease? |
| Genetics/ Genomics |
| • What is the prevalence of APOL1 risk alleles among ethnic and tribal populations in Sub-Saharan Africa, particularly in central and southeastern Africa? |
| • What is the prevalence of APOL1 risk alleles in African admixed populations as a consequence of the African diaspora in Central and South America and in the Caribbean? |
| • What other genes or viral or environmental factors cause HIVAN in 30% of individuals with 0 or 1 APOL1 risk alleles? Why isn’t HIVAN observed more frequently in other populations lacking APOL1 risk alleles? |
| • Why do APOL1 gain-of-function variants show recessive inheritance? |
| • Is a single copy of APOL1 G1 or G2 sufficient to cause HIVAN in a setting of HIV infection? |
| • What are the genetic and environmental factors which affect penetrance of APOL1 and does this differ by ethnicity or ancestry? |
| • What is the role of APOL1 in children with HIV infection? |
| • What are the mechanisms by which APOL1 precipitates kidney disease? Do these mechanisms differ in the setting of HIV infection? |
| • Is APOL1 an initiator of HIVAN or a progression factor? |
| • What are the public health implications of APOL1 in resource-limited settings? |
| Antiretroviral therapy and nephrotoxicity |
| • What is the clinical significance of TDF-induced sub-clinical renal tubular dysfunction, and what is the value of monitoring for low-molecular weight proteinuria and reduced phosphate reabsorption in patients on TDF? |
| • What is the rate of TDF nephrotoxicity in individuals without access to regular kidney function monitoring, including HIV-negative individuals taking TDF to prevent HIV infection? |
| • What is the long-term renal safety of TAF in individuals with a history of TDF-associated nephrotoxicity, CKD, or relevant comorbidities? |
| • What is the long-term safety of TAF in children, particularly with respect to bone health? |
| • Would epidemiologic studies linking ritonavir-boosted protease inhibitors to decreased eGFR yield similar results with cystatin C-based eGFR estimates? |
| Management of CKD and ESKD |
| • What are the optimal strategies for assessing and monitoring kidney health among ART-treated adults and children in resource-rich and resource-limited settings? |
| • Are existing CKD risk scores developed in HIV-positive US and European populations valid in other populations? |
| • How well do creatinine-based eGFR estimates predict true GFR in ART-treated individuals, especially those on ART that interferes with creatinine secretion and in sub-Saharan African populations? |
| • What is the role of serum cystatin C, alone or in combination with creatinine, in evaluating kidney function in specific clinical contexts, such as the use of ART that interferes with creatinine secretion? |
| • What is the clinical utility of novel urine biomarkers of kidney injury in assessing and monitoring kidney health? |
| • Are clinical guidelines for diabetes, hypertension, and cardiovascular disease developed in the general populations effective in preventing CKD onset and progression in HIV-positive individuals? |
| • Do ACE inhibitors and ARBs confer similar renoprotective effects among HIV-positive individuals with CKD as in the general population? |
| • What is the impact of tuberculosis co-infection and its treatment on the risks of CKD development and progression among HIV-positive individuals? |
| • What is the role of adjunctive therapy with corticosteroids or immunosuppressive therapy in patients with HIVAN or other kidney disease that may be causally related to HIV infection? |
| • What is the role of HIV infection in immune complex kidney disease, and what is the optimal therapy for specific immune complex diseases in this setting? |
| • Has the epidemiology of acute kidney injury changed in the era of modern ART, and what is the impact on CKD risk in the setting of HIV? |
| • What is the optimal antiviral therapy for HBV or HCV co-infection with regards to efficacy and safety in HIV-positive individuals? |
| • Does treatment of HBV or HCV co-infection impact CKD prognosis? |
| • How does the peritonitis risk among ART-treated HIV-positive patients undergoing peritoneal dialysis |
| compare to that of their HIV-negative counterparts? |
| • Are existing treatment guidelines for catheter-related infections developed in HIV-negative populations effective among HIV-positive patients with ESKD? |
| • What are the optimal strategies for anemia and mineral-bone disease management in the HIV-positive population with CKD or ESKD? |
| Kidney Transplantation |
| • Among HIV-positive patients being considered for kidney transplantation, what is the optimal timing of HBV or HCV treatment relative to kidney transplantation? This is particularly important based on the worse post-transplant outcomes among recipients with HIV-HCV co-infection. |
| • What is the optimal induction therapy for highly sensitized HIV-positive transplant recipients? |
| • What are the optimal ART and immunosuppressive regimens for HIV positive kidney transplant recipients? |
| • What is the optimal strategy for selecting and matching potential HIV-positive organ donors and recipients? |
| • What are the long-term implications of HIV-to-HIV kidney transplantation on patient and allograft outcomes and HIV disease course? |
ACE, angiotensin-converting enzyme; APOL1, apolipoprotein L1; ARB, angiotensin receptor blocker; ART, antiretroviral treatment; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; ESKD, end-stage kidney disease; FSGS, focal segmental glomerulosclerosis; GFR, glomerular filtration rate; HBV, hepatitis B virus; HCV, hepatitis C C; HIV, human immunodeficiency virus; HIVAN, HIV-associated nephropathy; NOS, not otherwise specified; TDF, tenofovir disoproxil fumarate; US, United States.
Supplementary Material
Acknowledgments
We gratefully acknowledge the African Association of Nephrology (AFRAN) for accommodating the KDIGO conference on the final day of the AFRAN congress.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE [individual author disclosures to be compiled]
The conference was sponsored by KDIGO and jointly held with AFRAN.
FAP has received honoraria for participating in advisory boards or speaker engagements from Gilead Sciences, MSD, and ViiV Healthcare; is an investigator for clinical trials sponsored by Janssen, Gilead Sciences, and ViiV Healthcare; has received research funding from Gilead Sciences and ViiV Healthcare. MME and NW have nothing to disclose.
References
- 1.UNAIDS. AIDSinfo. http://aidsinfo.unaids.org/ Accessed July 19, 2017)
- 2.Lucas GM, Ross MJ, Stock PG, et al. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96–138. doi: 10.1093/cid/ciu617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg AZ, Naicker S, Winkler CA, et al. HIV-associated nephropathies: epidemiology, pathology, mechanisms and treatment. Nat Rev Nephrol. 2015;11:150–160. doi: 10.1038/nrneph.2015.9. [DOI] [PubMed] [Google Scholar]
- 4.D’Agati V, Appel GB. HIV infection and the kidney. J Am Soc Nephrol. 1997;8:138–152. doi: 10.1681/ASN.V81138. [DOI] [PubMed] [Google Scholar]
- 5.Ross MJ. Advances in the pathogenesis of HIV-associated kidney diseases. Kidney Int. 2014;86:266–274. doi: 10.1038/ki.2014.167. [DOI] [PubMed] [Google Scholar]
- 6.Cohen AH, Nast CC. HIV-associated nephropathy. A unique combined glomerular, tubular, and interstitial lesion. Mod Pathol. 1988;1:87–97. [PubMed] [Google Scholar]
- 7.D’Agati V, Suh JI, Carbone L, et al. Pathology of HIV-associated nephropathy: a detailed morphologic and comparative study. Kidney Int. 1989;35:1358–1370. doi: 10.1038/ki.1989.135. [DOI] [PubMed] [Google Scholar]
- 8.Dijkman HB, Weening JJ, Smeets B, et al. Proliferating cells in HIV and pamidronate-associated collapsing focal segmental glomerulosclerosis are parietal epithelial cells. Kidney Int. 2006;70:338–344. doi: 10.1038/sj.ki.5001574. [DOI] [PubMed] [Google Scholar]
- 9.Wyatt CM, Klotman PE, D’Agati VD. HIV-associated nephropathy: clinical presentation, pathology, and epidemiology in the era of antiretroviral therapy. Semin Nephrol. 2008;28:513–522. doi: 10.1016/j.semnephrol.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wearne N, Swanepoel CR, Boulle A, et al. The spectrum of renal histologies seen in HIV with outcomes, prognostic indicators and clinical correlations. Nephrol Dial Transplant. 2012;27:4109–4118. doi: 10.1093/ndt/gfr702. [DOI] [PubMed] [Google Scholar]
- 11.Nadasdy T, Laszik Z, Blick KE, et al. Tubular atrophy in the end-stage kidney: a lectin and immunohistochemical study. Hum Pathol. 1994;25:22–28. doi: 10.1016/0046-8177(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 12.Ross MJ, Bruggeman LA, Wilson PD, et al. Microcyst formation and HIV-1 gene expression occur in multiple nephron segments in HIV-associated nephropathy. J Am Soc Nephrol. 2001;12:2645–2651. doi: 10.1681/ASN.V12122645. [DOI] [PubMed] [Google Scholar]
- 13.Rosenstiel PE, Gruosso T, Letourneau AM, et al. HIV-1 Vpr inhibits cytokinesis in human proximal tubule cells. Kidney Int. 2008;74:1049–1058. doi: 10.1038/ki.2008.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berliner AR, Fine DM, Lucas GM, et al. Observations on a cohort of HIV-infected patients undergoing native renal biopsy. Am J Nephrol. 2008;28:478–486. doi: 10.1159/000112851. [DOI] [PubMed] [Google Scholar]
- 15.Lescure FX, Flateau C, Pacanowski J, et al. HIV-associated kidney glomerular diseases: changes with time and HAART. Nephrol Dial Transplant. 2012;27:2349–2355. doi: 10.1093/ndt/gfr676. [DOI] [PubMed] [Google Scholar]
- 16.Mallipattu SK, Salem F, Wyatt CM. The changing epidemiology of HIV-related chronic kidney disease in the era of antiretroviral therapy. Kidney Int. 2014;86:259–265. doi: 10.1038/ki.2014.44. [DOI] [PubMed] [Google Scholar]
- 17.Strauss J, Abitbol C, Zilleruelo G, et al. Renal disease in children with the acquired immunodeficiency syndrome. N Engl J Med. 1989;321:625–630. doi: 10.1056/NEJM198909073211001. [DOI] [PubMed] [Google Scholar]
- 18.Nobakht E, Cohen SD, Rosenberg AZ, et al. HIV-associated immune complex kidney disease. Nat Rev Nephrol. 2016;12:291–300. doi: 10.1038/nrneph.2015.216. [DOI] [PubMed] [Google Scholar]
- 19.Kimmel PL, Phillips TM, Ferreira-Centeno A, et al. Brief report: idiotypic IgA nephropathy in patients with human immunodeficiency virus infection. N Engl J Med. 1992;327:702–706. doi: 10.1056/NEJM199209033271006. [DOI] [PubMed] [Google Scholar]
- 20.Kimmel PL, Phillips TM, Ferreira-Centeno A, et al. HIV-associated immune-mediated renal disease. Kidney Int. 1993;44:1327–1340. doi: 10.1038/ki.1993.386. [DOI] [PubMed] [Google Scholar]
- 21.Haas M, Kaul S, Eustace JA. HIV-associated immune complex glomerulonephritis with “lupus-like” features: a clinicopathologic study of 14 cases. Kidney Int. 2005;67:1381–1390. doi: 10.1111/j.1523-1755.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 22.Chang BG, Markowitz GS, Seshan SV, et al. Renal manifestations of concurrent systemic lupus erythematosus and HIV infection. Am J Kidney Dis. 1999;33:441–449. doi: 10.1016/s0272-6386(99)70180-0. [DOI] [PubMed] [Google Scholar]
- 23.Gerntholtz TE, Goetsch SJ, Katz I. HIV-related nephropathy: a South African perspective. Kidney Int. 2006;69:1885–1891. doi: 10.1038/sj.ki.5000351. [DOI] [PubMed] [Google Scholar]
- 24.Cheng JT, Anderson HL, Jr, Markowitz GS, et al. Hepatitis C virus-associated glomerular disease in patients with human immunodeficiency virus coinfection. J Am Soc Nephrol. 1999;10:1566–1574. doi: 10.1681/ASN.V1071566. [DOI] [PubMed] [Google Scholar]
- 25.Mohan S, Herlitz LC, Tan J, et al. The changing pattern of glomerular disease in HIV and hepatitis C co-infected patients in the era of HAART. Clin Nephrol. 2013;79:285–291. doi: 10.5414/CN107774. [DOI] [PubMed] [Google Scholar]
- 26.Stokes MB, Chawla H, Brody RI, et al. Immune complex glomerulonephritis in patients coinfected with human immunodeficiency virus and hepatitis C virus. Am J Kidney Dis. 1997;29:514–525. doi: 10.1016/s0272-6386(97)90332-2. [DOI] [PubMed] [Google Scholar]
- 27.Herlitz LC, Mohan S, Stokes MB, et al. Tenofovir nephrotoxicity: acute tubular necrosis with distinctive clinical, pathological, and mitochondrial abnormalities. Kidney Int. 2010;78:1171–1177. doi: 10.1038/ki.2010.318. [DOI] [PubMed] [Google Scholar]
- 28.Fine DM, Perazella MA, Lucas GM, et al. Kidney biopsy in HIV: beyond HIV-associated nephropathy. Am J Kidney Dis. 2008;51:504–514. doi: 10.1053/j.ajkd.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 29.Parkhie SM, Fine DM, Lucas GM, et al. Characteristics of patients with HIV and biopsy-proven acute interstitial nephritis. Clin J Am Soc Nephrol. 2010;5:798–804. doi: 10.2215/CJN.08211109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zaidan M, Lescure FX, Brocheriou I, et al. Tubulointerstitial nephropathies in HIV-infected patients over the past 15 years: a clinico-pathological study. Clin J Am Soc Nephrol. 2013;8:930–938. doi: 10.2215/CJN.10051012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox C, Walker-Bone K. Evolving spectrum of HIV-associated rheumatic syndromes. Best Pract Res Clin Rheumatol. 2015;29:244–258. doi: 10.1016/j.berh.2015.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoo J, Baumstein D, Kuppachi S, et al. Diffuse infiltrative lymphocytosis syndrome presenting as reversible acute kidney injury associated with Gram-negative bacterial infection in patients with newly diagnosed HIV infection. Am J Kidney Dis. 2011;57:752–755. doi: 10.1053/j.ajkd.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 33.Zafrani L, Coppo P, Dettwiler S, et al. Nephropathy associated with the diffuse infiltrative lymphocytosis syndrome. Kidney Int. 2007;72:219–224. doi: 10.1038/sj.ki.5002207. [DOI] [PubMed] [Google Scholar]
- 34.Martin-Blondel G, Debard A, Laurent C, et al. Mycobacterial-immune reconstitution inflammatory syndrome: a cause of acute interstitial nephritis during HIV infection. Nephrol Dial Transplant. 2011;26:2403–2406. doi: 10.1093/ndt/gfr197. [DOI] [PubMed] [Google Scholar]
- 35.Rarick MU, Espina B, Mocharnuk R, et al. Thrombotic thrombocytopenic purpura in patients with human immunodeficiency virus infection: a report of three cases and review of the literature. Am J Hematol. 1992;40:103–109. doi: 10.1002/ajh.2830400206. [DOI] [PubMed] [Google Scholar]
- 36.del Arco A, Martinez MA, Pena JM, et al. Thrombotic thrombocytopenic purpura associated with human immunodeficiency virus infection: demonstration of p24 antigen in endothelial cells. Clin Infect Dis. 1993;17:360–363. doi: 10.1093/clinids/17.3.360. [DOI] [PubMed] [Google Scholar]
- 37.Remark R, Merghoub T, Grabe N, et al. In-depth tissue profiling using multiplexed immunohistochemical consecutive staining on single slide. Sci Immunol. 2016;1:aaf6925. doi: 10.1126/sciimmunol.aaf6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newman AM, Liu CL, Green MR, et al. Robust enumeration of cell subsets from tissue expression profiles. Nat Methods. 2015;12:453–457. doi: 10.1038/nmeth.3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kula Xu GJ, Xu TQ, et al. Viral immunology. Comprehensive serological profiling of human populations using a synthetic human virome. Science. 2015;348:aaa0698. doi: 10.1126/science.aaa0698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kopp JB, Winkler C. HIV-associated nephropathy in African Americans. Kidney Int Suppl. 2003:S43–49. doi: 10.1046/j.1523-1755.63.s83.10.x. [DOI] [PubMed] [Google Scholar]
- 41.Kopp JB, Smith MW, Nelson GW, et al. MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat Genet. 2008;40:1175–1184. doi: 10.1038/ng.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kao WH, Klag MJ, Meoni LA, et al. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet. 2008;40:1185–1192. doi: 10.1038/ng.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Behar DM, Rosset S, Tzur S, et al. African ancestry allelic variation at the MYH9 gene contributes to increased susceptibility to non-diabetic end-stage kidney disease in Hispanic Americans. Hum Mol Genet. 2010;19:1816–1827. doi: 10.1093/hmg/ddq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nelson GW, Freedman BI, Bowden DW, et al. Dense mapping of MYH9 localizes the strongest kidney disease associations to the region of introns 13 to 15. Hum Mol Genet. 2010;19:1805–1815. doi: 10.1093/hmg/ddq039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010;329:841–845. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Perez-Morga D, Vanhollebeke B, Paturiaux-Hanocq F, et al. Apolipoprotein L-I promotes trypanosome lysis by forming pores in lysosomal membranes. Science. 2005;309:469–472. doi: 10.1126/science.1114566. [DOI] [PubMed] [Google Scholar]
- 47.Vanhamme L, Paturiaux-Hanocq F, Poelvoorde P, et al. Apolipoprotein L-I is the trypanosome lytic factor of human serum. Nature. 2003;422:83–87. doi: 10.1038/nature01461. [DOI] [PubMed] [Google Scholar]
- 48.Cooper A, Ilboudo H, Alibu VP, et al. APOL1 renal risk variants have contrasting resistance and susceptibility associations with African trypanosomiasis. Elife. 2017:6. doi: 10.7554/eLife.25461. ii: e25461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kopp JB, Nelson GW, Sampath K, et al. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. J Am Soc Nephrol. 2011;22:2129–2137. doi: 10.1681/ASN.2011040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Limou S, Nelson GW, Kopp JB, et al. APOL1 kidney risk alleles: population genetics and disease associations. Adv Chronic Kidney Dis. 2014;21:426–433. doi: 10.1053/j.ackd.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kasembeli AN, Duarte R, Ramsay M, et al. APOL1 Risk Variants Are Strongly Associated with HIV-Associated Nephropathy in Black South Africans. J Am Soc Nephrol. 2015;26:2882–2890. doi: 10.1681/ASN.2014050469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Behar DM, Kedem E, Rosset S, et al. Absence of APOL1 risk variants protects against HIV-associated nephropathy in the Ethiopian population. Am J Nephrol. 2011;34:452–459. doi: 10.1159/000332378. [DOI] [PubMed] [Google Scholar]
- 53.Dummer PD, Limou S, Rosenberg AZ, et al. APOL1 Kidney Disease Risk Variants: An Evolving Landscape. Semin Nephrol. 2015;35:222–236. doi: 10.1016/j.semnephrol.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Atta MG, Estrella MM, Kuperman M, et al. HIV-associated nephropathy patients with and without apolipoprotein L1 gene variants have similar clinical and pathological characteristics. Kidney Int. 2012;82:338–343. doi: 10.1038/ki.2012.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ko WY, Rajan P, Gomez F, et al. Identifying Darwinian selection acting on different human APOL1 variants among diverse African populations. Am J Hum Genet. 2013;93:54–66. doi: 10.1016/j.ajhg.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Atta MG, Estrella MM, Skorecki KL, et al. Association of APOL1 Genotype with Renal Histology among Black HIV-Positive Patients Undergoing Kidney Biopsy. Clin J Am Soc Nephrol. 2016;11:262–270. doi: 10.2215/CJN.07490715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fine DM, Wasser WG, Estrella MM, et al. APOL1 risk variants predict histopathology and progression to ESRD in HIV-related kidney disease. J Am Soc Nephrol. 2012;23:343–350. doi: 10.1681/ASN.2011060562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kopp JB, Winkler CA, Zhao X, et al. Clinical Features and Histology of Apolipoprotein L1-Associated Nephropathy in the FSGS Clinical Trial. J Am Soc Nephrol. 2015;26:1443–1448. doi: 10.1681/ASN.2013111242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Estrella MM, Li M, Tin A, et al. The association between APOL1 risk alleles and longitudinal kidney function differs by HIV viral suppression status. Clin Infect Dis. 2015;60:646–652. doi: 10.1093/cid/ciu765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Estrella MM, Wyatt CM, Pearce CL, et al. Host APOL1 genotype is independently associated with proteinuria in HIV infection. Kidney Int. 2013;84:834–840. doi: 10.1038/ki.2013.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beckerman P, Bi-Karchin J, Park AS, et al. Transgenic expression of human APOL1 risk variants in podocytes induces kidney disease in mice. Nat Med. 2017;23:429–438. doi: 10.1038/nm.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nichols B, Jog P, Lee JH, et al. Innate immunity pathways regulate the nephropathy gene Apolipoprotein L1. Kidney Int. 2015;87:332–342. doi: 10.1038/ki.2014.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fu Y, Zhu JY, Richman A, et al. APOL1-G1 in Nephrocytes Induces Hypertrophy and Accelerates Cell Death. J Am Soc Nephrol. 2017;28:1106–1116. doi: 10.1681/ASN.2016050550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kruzel-Davila E, Shemer R, Ofir A, et al. APOL1-Mediated Cell Injury Involves Disruption of Conserved Trafficking Processes. J Am Soc Nephrol. 2017;28:1117–1130. doi: 10.1681/ASN.2016050546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ma L, Chou JW, Snipes JA, et al. APOL1 Renal-Risk Variants Induce Mitochondrial Dysfunction. J Am Soc Nephrol. 2017;28:1093–1105. doi: 10.1681/ASN.2016050567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Olabisi OA, Zhang JY, VerPlank L, et al. APOL1 kidney disease risk variants cause cytotoxicity by depleting cellular potassium and inducing stress-activated protein kinases. Proc Natl Acad Sci U S A. 2016;113:830–837. doi: 10.1073/pnas.1522913113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bruggeman LA, Wu Z, Luo L, et al. APOL1-G0 or APOL1-G2 Transgenic Models Develop Preeclampsia but Not Kidney Disease. J Am Soc Nephrol. 2016;27:3600–3610. doi: 10.1681/ASN.2015111220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wan G, Zhaorigetu S, Liu Z, et al. Apolipoprotein L1, a novel Bcl-2 homology domain 3-only lipid-binding protein, induces autophagic cell death. J Biol Chem. 2008;283:21540–21549. doi: 10.1074/jbc.M800214200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lan X, Jhaveri A, Cheng K, et al. APOL1 risk variants enhance podocyte necrosis through compromising lysosomal membrane permeability. Am J Physiol Renal Physiol. 2014;307:F326–336. doi: 10.1152/ajprenal.00647.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Atta MG, Gallant JE, Rahman MH, et al. Antiretroviral therapy in the treatment of HIV-associated nephropathy. Nephrol Dial Transplant. 2006;21:2809–2813. doi: 10.1093/ndt/gfl337. [DOI] [PubMed] [Google Scholar]
- 71.Booth JW, Hamzah L, Jose S, et al. Clinical characteristics and outcomes of HIV-associated immune complex kidney disease. Nephrol Dial Transplant. 2016;31:2099–2107. doi: 10.1093/ndt/gfv436. [DOI] [PubMed] [Google Scholar]
- 72.Foy MC, Estrella MM, Lucas GM, et al. Comparison of risk factors and outcomes in HIV immune complex kidney disease and HIV-associated nephropathy. Clin J Am Soc Nephrol. 2013;8:1524–1532. doi: 10.2215/CJN.10991012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ibrahim F, Naftalin C, Cheserem E, et al. Immunodeficiency and renal impairment are risk factors for HIV-associated acute renal failure. AIDS. 2010;24:2239–2244. doi: 10.1097/QAD.0b013e32833c85d6. [DOI] [PubMed] [Google Scholar]
- 74.Mocroft A, Lundgren JD, Ross M, et al. Development and validation of a risk score for chronic kidney disease in HIV infection using prospective cohort data from the D:A:D study. PLoS Med. 2015;12:e1001809. doi: 10.1371/journal.pmed.1001809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Scherzer R, Gandhi M, Estrella MM, et al. A chronic kidney disease risk score to determine tenofovir safety in a prospective cohort of HIV-positive male veterans. AIDS. 2014;28:1289–1295. doi: 10.1097/QAD.0000000000000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Woodward CL, Hall AM, Williams IG, et al. Tenofovir-associated renal and bone toxicity. HIV Med. 2009;10:482–487. doi: 10.1111/j.1468-1293.2009.00716.x. [DOI] [PubMed] [Google Scholar]
- 77.Hamzah L, Jose S, Booth JW, et al. Treatment-limiting renal tubulopathy in patients treated with tenofovir disoproxil fumarate. J Infect. 2017;74:492–500. doi: 10.1016/j.jinf.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 78.Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23–32. doi: 10.1016/S2352-3018(15)00211-8. [DOI] [PubMed] [Google Scholar]
- 79.Scherzer R, Estrella M, Li Y, et al. Association of tenofovir exposure with kidney disease risk in HIV infection. AIDS. 2012;26:867–875. doi: 10.1097/QAD.0b013e328351f68f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jose S, Hamzah L, Campbell LJ, et al. Incomplete reversibility of estimated glomerular filtration rate decline following tenofovir disoproxil fumarate exposure. J Infect Dis. 2014;210:363–373. doi: 10.1093/infdis/jiu107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Post FA, Tebas P, Clarke A, et al. Brief Report: Switching to Tenofovir Alafenamide, Coformulated With Elvitegravir, Cobicistat, and Emtricitabine, in HIV-Infected Adults With Renal Impairment: 96-Week Results From a Single-Arm, Multicenter, Open-Label Phase 3 Study. J Acquir Immune Defic Syndr. 2017;74:180–184. doi: 10.1097/QAI.0000000000001186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ryom L, Mocroft A, Kirk O, et al. Predictors of estimated glomerular filtration rate progression, stabilization or improvement after chronic renal impairment in HIV-positive individuals. AIDS. 2017;31:1261–1270. doi: 10.1097/QAD.0000000000001464. [DOI] [PubMed] [Google Scholar]
- 83.Waheed S, Attia D, Estrella MM, et al. Proximal tubular dysfunction and kidney injury associated with tenofovir in HIV patients: a case series. Clin Kidney J. 2015;8:420–425. doi: 10.1093/ckj/sfv041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hamzah L, Booth JW, Jose S, et al. Renal tubular disease in the era of combination antiretroviral therapy. AIDS. 2015;29:1831–1836. doi: 10.1097/QAD.0000000000000736. [DOI] [PubMed] [Google Scholar]
- 85.Chughlay MF, Njuguna C, Cohen K, et al. Acute interstitial nephritis caused by lopinavir/ritonavir in a surgeon receiving antiretroviral postexposure prophylaxis. AIDS. 2015;29:503–504. doi: 10.1097/QAD.0000000000000563. [DOI] [PubMed] [Google Scholar]
- 86.Doco-Lecompte T, Garrec A, Thomas L, et al. Lopinavir-ritonavir (Kaletra) and lithiasis: seven cases. AIDS. 2004;18:705–706. doi: 10.1097/00002030-200403050-00022. [DOI] [PubMed] [Google Scholar]
- 87.Hamada Y, Nishijima T, Watanabe K, et al. High incidence of renal stones among HIV-infected patients on ritonavir-boosted atazanavir than in those receiving other protease inhibitor-containing antiretroviral therapy. Clin Infect Dis. 2012;55:1262–1269. doi: 10.1093/cid/cis621. [DOI] [PubMed] [Google Scholar]
- 88.Schmid S, Opravil M, Moddel M, et al. Acute interstitial nephritis of HIV-positive patients under atazanavir and tenofovir therapy in a retrospective analysis of kidney biopsies. Virchows Arch. 2007;450:665–670. doi: 10.1007/s00428-007-0418-3. [DOI] [PubMed] [Google Scholar]
- 89.Shafi T, Choi MJ, Racusen LC, et al. Ritonavir-induced acute kidney injury: kidney biopsy findings and review of literature. Clin Nephrol. 2011;75(Suppl 1):60–64. doi: 10.5414/cn106469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jose S, Nelson M, Phillips A, et al. Improved kidney function in patients who switch their protease inhibitor from atazanavir or lopinavir to darunavir. AIDS. 2017;31:485–492. doi: 10.1097/QAD.0000000000001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cahn P, Andrade-Villanueva J, Arribas JR, et al. Dual therapy with lopinavir and ritonavir plus lamivudine versus triple therapy with lopinavir and ritonavir plus two nucleoside reverse transcriptase inhibitors in antiretroviral-therapy-naive adults with HIV-1 infection: 48 week results of the randomised, open label, non-inferiority GARDEL trial. Lancet Infect Dis. 2014;14:572–580. doi: 10.1016/S1473-3099(14)70736-4. [DOI] [PubMed] [Google Scholar]
- 92.Perez-Molina JA, Rubio R, Rivero A, et al. Dual treatment with atazanavir-ritonavir plus lamivudine versus triple treatment with atazanavir-ritonavir plus two nucleos(t)ides in virologically stable patients with HIV-1 (SALT): 48 week results from a randomised, open-label, non-inferiority trial. Lancet Infect Dis. 2015;15:775–784. doi: 10.1016/S1473-3099(15)00097-3. [DOI] [PubMed] [Google Scholar]
- 93.Raffi F, Babiker AG, Richert L, et al. Ritonavir-boosted darunavir combined with raltegravir or tenofovir-emtricitabine in antiretroviral-naive adults infected with HIV-1: 96 week results from the NEAT001/ANRS143 randomised non-inferiority trial. Lancet. 2014;384:1942–1951. doi: 10.1016/S0140-6736(14)61170-3. [DOI] [PubMed] [Google Scholar]
- 94.Abraham AG, Althoff KN, Jing Y, et al. End-stage renal disease among HIV-infected adults in North America. Clin Infect Dis. 2015;60:941–949. doi: 10.1093/cid/ciu919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 96.Wong C, Gange SJ, Buchacz K, et al. First Occurrence of Diabetes, Chronic Kidney Disease, and Hypertension Among North American HIV-Infected Adults, 2000–2013. Clin Infect Dis. 2017;64:459–467. doi: 10.1093/cid/ciw804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lucas GM, Jing Y, Sulkowski M, et al. Hepatitis C viremia and the risk of chronic kidney disease in HIV-infected individuals. J Infect Dis. 2013;208:1240–1249. doi: 10.1093/infdis/jit373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mocroft A, Neuhaus J, Peters L, et al. Hepatitis B and C co-infection are independent predictors of progressive kidney disease in HIV-positive, antiretroviral-treated adults. PLoS One. 2012;7:e40245. doi: 10.1371/journal.pone.0040245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jha V, Prasad N. CKD and Infectious Diseases in Asia Pacific: Challenges and Opportunities. Am J Kidney Dis. 2016;68:148–160. doi: 10.1053/j.ajkd.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 100.Shen TC, Huang KY, Chao CH, et al. The risk of chronic kidney disease in tuberculosis: a population-based cohort study. QJM. 2015;108:397–403. doi: 10.1093/qjmed/hcu220. [DOI] [PubMed] [Google Scholar]
- 101.Wen YK, Chen ML. Crescentic glomerulonephritis associated with miliary tuberculosis. Clin Nephrol. 2009;71:310–313. doi: 10.5414/cnp71310. [DOI] [PubMed] [Google Scholar]
- 102.Choi AI, Li Y, Parikh C, et al. Long-term clinical consequences of acute kidney injury in the HIV-infected. Kidney Int. 2010;78:478–485. doi: 10.1038/ki.2010.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3:1–150. [Google Scholar]
- 104.Choi A, Scherzer R, Bacchetti P, et al. Cystatin C, albuminuria, and 5-year all-cause mortality in HIV-infected persons. Am J Kidney Dis. 2010;56:872–882. doi: 10.1053/j.ajkd.2010.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shlipak MG, Matsushita K, Arnlov J, et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med. 2013;369:932–943. doi: 10.1056/NEJMoa1214234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Inker LA, Wyatt C, Creamer R, et al. Performance of creatinine and cystatin C GFR estimating equations in an HIV-positive population on antiretrovirals. J Acquir Immune Defic Syndr. 2012;61:302–309. doi: 10.1097/QAI.0b013e31826a6c4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lucas GM, Cozzi-Lepri A, Wyatt CM, et al. Glomerular filtration rate estimated using creatinine, cystatin C or both markers and the risk of clinical events in HIV-infected individuals. HIV Med. 2014;15:116–123. doi: 10.1111/hiv.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Seape T, Gounden V, van Deventer HE, et al. Cystatin C- and creatinine-based equations in the assessment of renal function in HIV-positive patients prior to commencing Highly Active Antiretroviral Therapy. Ann Clin Biochem. 2016;53:58–66. doi: 10.1177/0004563215579695. [DOI] [PubMed] [Google Scholar]
- 109.Yombi JC, Pozniak A, Boffito M, et al. Antiretrovirals and the kidney in current clinical practice: renal pharmacokinetics, alterations of renal function and renal toxicity. AIDS. 2014;28:621–632. doi: 10.1097/QAD.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 110.Knight EL, Verhave JC, Spiegelman D, et al. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65:1416–1421. doi: 10.1111/j.1523-1755.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 111.Stevens LA, Levey AS. Measurement of kidney function. Med Clin North Am. 2005;89:457–473. doi: 10.1016/j.mcna.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 112.Stevens LA, Schmid CH, Greene T, et al. Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int. 2009;75:652–660. doi: 10.1038/ki.2008.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yombi JC, Jones R, Pozniak A, et al. Monitoring of kidney function in HIV-positive patients. HIV Med. 2015;16:457–467. doi: 10.1111/hiv.12249. [DOI] [PubMed] [Google Scholar]
- 114.Yahaya I, Uthman AO, Uthman MM. Interventions for HIV-associated nephropathy. Cochrane Database Syst Rev. 2009:CD007183. doi: 10.1002/14651858.CD007183.pub2. [DOI] [PubMed] [Google Scholar]
- 115.World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. Geneva Switzerland: 2014. p. 184. [PubMed] [Google Scholar]
- 116.Kidney Disease: Impproving global Outcomes (KDIGO) Blood Pressure Working Group. KDIGO Clinical Practice Guidelines for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Intl Suppl. 2012;2:337–414. [Google Scholar]
- 117.Wright JT, Jr, Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.World Health Organization. Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. Geneva Switzerland: p. 166. [PubMed] [Google Scholar]
- 119.Nahid P, Dorman SE, Alipanah N, et al. Executive Summary: Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis. 2016;63:853–867. doi: 10.1093/cid/ciw566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pol S, Jadoul M, Vallet-Pichard A. An update on the management of hepatitis C virus-infected patients with stage 4–5 chronic kidney disease while awaiting the revised KDIGO Guidelines. Nephrol Dial Transplant. 2017;32:32–35. doi: 10.1093/ndt/gfw023. [DOI] [PubMed] [Google Scholar]
- 121.Terrault NA, Bzowej NH, Chang KM, et al. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261–283. doi: 10.1002/hep.28156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ahuja TS, Grady J, Khan S. Changing trends in the survival of dialysis patients with human immunodeficiency virus in the United States. J Am Soc Nephrol. 2002;13:1889–1893. doi: 10.1097/01.asn.0000019773.43765.bf. [DOI] [PubMed] [Google Scholar]
- 123.Ahuja TS, Collinge N, Grady J, et al. Is dialysis modality a factor in survival of patients with ESRD and HIV-associated nephropathy? Am J Kidney Dis. 2003;41:1060–1064. doi: 10.1016/s0272-6386(03)00204-x. [DOI] [PubMed] [Google Scholar]
- 124.Soleymanian T, Raman S, Shannaq FN, et al. Survival and morbidity of HIV patients on hemodialysis and peritoneal dialysis: one center’s experience and review of the literature. Int Urol Nephrol. 2006;38:331–338. doi: 10.1007/s11255-006-0080-8. [DOI] [PubMed] [Google Scholar]
- 125.Mitchell D, Krishnasami Z, Young CJ, et al. Arteriovenous access outcomes in haemodialysis patients with HIV infection. Nephrol Dial Transplant. 2007;22:465–470. doi: 10.1093/ndt/gfl629. [DOI] [PubMed] [Google Scholar]
- 126.Wreghitt TG. Blood-borne virus infections in dialysis units–a review. Rev Med Virol. 1999;9:101–109. doi: 10.1002/(sici)1099-1654(199904/06)9:2<101::aid-rmv234>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 127.Current trends recommendations for providing dialysis treatment to patients infected with human T-lymphotropic virus type III/lymphadenopathy-associated virus. MMWR. 1986;35:376–378. 383. [PubMed] [Google Scholar]
- 128.Centers for Disease Control and Prevention (CDC); Preventing infections in dialysis setting guideline. https://www.cdc.gov/infectioncontrol/guidelines/dialysis/index.html. (Accessed July 19, 2017)
- 129.Ndlovu KC, Sibanda W, Assounga A. Peritonitis outcomes in patients with HIV and end-stage renal failure on peritoneal dialysis: a prospective cohort study. BMC Nephrol. 2017;18:48. doi: 10.1186/s12882-017-0466-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Farzadegan H, Ford D, Malan M, et al. HIV-1 survival kinetics in peritoneal dialysis effluent. Kidney Int. 1996;50:1659–1662. doi: 10.1038/ki.1996.482. [DOI] [PubMed] [Google Scholar]
- 131.Ndlovu KC, Sibanda W, Assounga A. Detection of human immunodeficiency virus-1 ribonucleic acid in the peritoneal effluent of renal failure patients on highly active antiretroviral therapy. Nephrol Dial Transplant. 2017;32:714–721. doi: 10.1093/ndt/gfx001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Stock PG, Barin B, Murphy B, et al. Outcomes of kidney transplantation in HIV-infected recipients. N Engl J Med. 2010;363:2004–2014. doi: 10.1056/NEJMoa1001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Locke JE, Gustafson S, Mehta S, et al. Survival Benefit of Kidney Transplantation in HIV-infected Patients. Ann Surg. 2017;265:604–608. doi: 10.1097/SLA.0000000000001761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gathogo EN, Hamzah L, Hilton R, et al. Kidney transplantation in HIV-positive adults: the UK experience. Int J STD AIDS. 2014;25:57–66. doi: 10.1177/0956462413493266. [DOI] [PubMed] [Google Scholar]
- 135.Gathogo EN, Shah S, Post FA. Kidney transplant outcomes in HIV serodiscordant recipient pairs. AIDS. 2017;31:1199–1201. doi: 10.1097/QAD.0000000000001457. [DOI] [PubMed] [Google Scholar]
- 136.Locke JE, Mehta S, Sawinski D, et al. Access to Kidney Transplantation among HIV-Infected Waitlist Candidates. Clin J Am Soc Nephrol. 2017;12:467–475. doi: 10.2215/CJN.07460716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Muller E, Barday Z, Mendelson M, et al. HIV-positive-to-HIV-positive kidney transplantation–results at 3 to 5 years. N Engl J Med. 2015;372:613–620. doi: 10.1056/NEJMoa1408896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Waheed S, Sakr A, Chheda ND, et al. Outcomes of Renal Transplantation in HIV-1 Associated Nephropathy. PLoS One. 2015;10:e0129702. doi: 10.1371/journal.pone.0129702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.McLean FE, Gathogo E, Goodall D, et al. Alemtuzumab induction therapy in HIV-positive renal transplant recipients. AIDS. 2017;31:1047–1048. doi: 10.1097/QAD.0000000000001413. [DOI] [PubMed] [Google Scholar]
- 140.Gathogo E, Harber M, Bhagani S, et al. Impact of Tacrolimus Compared With Cyclosporin on the Incidence of Acute Allograft Rejection in Human Immunodeficiency Virus-Positive Kidney Transplant Recipients. Transplantation. 2016;100:871–878. doi: 10.1097/TP.0000000000000879. [DOI] [PubMed] [Google Scholar]
- 141.EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–398. doi: 10.1016/j.jhep.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 142.Karuthu S, Blumberg EA. Common infections in kidney transplant recipients. Clin J Am Soc Nephrol. 2012;7:2058–2070. doi: 10.2215/CJN.04410512. [DOI] [PubMed] [Google Scholar]
- 143.Kidney Disease: Improving Global Outcomes. KDIGO clinical practice guidelines for the prevention, diagnosis, evaluation, and treatment of hepatitis C in chronic kidney disease. Kidney Int Suppl. 2008;109:S1–S99. doi: 10.1038/ki.2008.81. [DOI] [PubMed] [Google Scholar]
- 144.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 145.Sawinski D, Shelton BA, Mehta S, et al. Impact of Protease Inhibitor based Anti-Retroviral Therapy on Outcomes for HIV+ Kidney Transplant Recipients. Am J Transplant. 2017 Jul 11; doi: 10.1111/ajt.14419. [DOI] [PubMed] [Google Scholar]
- 146.Canaud G, Dejucq-Rainsford N, Avettand-Fenoel V, et al. The kidney as a reservoir for HIV-1 after renal transplantation. J Am Soc Nephrol. 2014;25:407–419. doi: 10.1681/ASN.2013050564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.APOL1 Long-term Kidney Transplantation Outcomes Network (APOLLO) Clinical Centers (Collaborative U01), RFA-DK-16-025. Department of Health and Human Services N, editor. https://grants.nih.gov/grants/guide/rfa-files/RFA-DK-16–025.html. Accessed June 19, 2017.
- 148.Muller E, Barday Z, Kahn D. HIV-positive-to-HIV-positive kidney transplantation. N Engl J Med. 2015;372:2070–2071. doi: 10.1056/NEJMc1503288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Muller E, Kahn D, Mendelson M. Renal transplantation between HIV-positive donors and recipients. N Engl J Med. 2010;362:2336–2337. doi: 10.1056/NEJMc0900837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Organ procurement and transplantation: implementation of the HIV Organ Policy Equity Act. Final rule. Fed Regist. 2015;80:26464–26467. [PubMed] [Google Scholar]
- 151.Boyarsky BJ, Segev DL. From Bench to Bill: How a Transplant Nuance Became 1 of Only 57 Laws Passed in 2013. Ann Surg. 2016;263:430–433. doi: 10.1097/SLA.0000000000001352. [DOI] [PubMed] [Google Scholar]
- 152.Papeta N, Kiryluk K, Patel A, et al. APOL1 variants increase risk for FSGS and HIVAN but not IgA nephropathy. J Am Soc Nephrol. 2011;22:1991–1996. doi: 10.1681/ASN.2011040434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Purswani MU, Patel K, Winkler CA, et al. Brief Report: APOL1 Renal Risk Variants Are Associated With Chronic Kidney Disease in Children and Youth With Perinatal HIV Infection. J Acquir Immune Defic Syndr. 2016;73:63–68. doi: 10.1097/QAI.0000000000001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sax PE, Wohl D, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomised, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615. doi: 10.1016/S0140-6736(15)60616-X. [DOI] [PubMed] [Google Scholar]
- 155.Abboud O, Becker G, Bellorin-Font E, et al. KDIGO clinical practice guidelines on hepatitis C in chronic kidney disease acknowledged by ISN. Nat Clin Pract Nephrol. 2008;4:648–649. doi: 10.1038/ncpneph0953. [DOI] [PubMed] [Google Scholar]
- 156.Mendizabal M, Reddy KR. Chronic hepatitis C and chronic kidney disease: Advances, limitations and unchartered territories. J Viral Hepat. 2017;24:442–453. doi: 10.1111/jvh.12681. [DOI] [PubMed] [Google Scholar]
- 157.Pockros PJ, Reddy KR, Mantry PS, et al. Efficacy of Direct-Acting Antiviral Combination for Patients With Hepatitis C Virus Genotype 1 Infection and Severe Renal Impairment or End-Stage Renal Disease. Gastroenterology. 2016;150:1590–1598. doi: 10.1053/j.gastro.2016.02.078. [DOI] [PubMed] [Google Scholar]
- 158.Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4–5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537–1545. doi: 10.1016/S0140-6736(15)00349-9. [DOI] [PubMed] [Google Scholar]
- 159.Bhamidimarri KR, Czul F, Peyton A, et al. Safety, efficacy and tolerability of half-dose sofosbuvir plus simeprevir in treatment of Hepatitis C in patients with end stage renal disease. J Hepatol. 2015;63:763–765. doi: 10.1016/j.jhep.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 160.Dumortier J, Bailly F, Pageaux GP, et al. Sofosbuvir-based antiviral therapy in hepatitis C virus patients with severe renal failure. Nephrol Dial Transplant. 2016 Oct 19; doi: 10.1093/ndt/gfw348. pii: gfw348. [DOI] [PubMed] [Google Scholar]
- 161.Saxena V, Koraishy FM, Sise ME, et al. Safety and efficacy of sofosbuvir-containing regimens in hepatitis C-infected patients with impaired renal function. Liver Int. 2016;36:807–816. doi: 10.1111/liv.13102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kim PS, Woods C, Georgoff P, et al. A1C underestimates glycemia in HIV infection. Diabetes Care. 2009;32:1591–1593. doi: 10.2337/dc09-0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Slama L, Palella FJ, Jr, Abraham AG, et al. Inaccuracy of haemoglobin A1c among HIV-infected men: effects of CD4 cell count, antiretroviral therapies and haematological parameters. J Antimicrob Chemother. 2014;69:3360–3367. doi: 10.1093/jac/dku295. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


