Abstract
Background
Cerebral Palsy (CP) is the most common motor disability reason of childhood that occurs secondarily to non-progressive damage in the brain whose development is still ongoing.
Methods
6-year-old dystonic-spastic male CP patient received allogenic mesenchymal stem cells treatment four times as 1×106/kg in intrathecal and intravenous administration of Umbilical Cord-derived mesenchymal stem cells (UC-MSCs) ways. Before and after the treatment, the patient was followed-up with FIM (Functional Independent Measurement), GMFCS (Gross Motor Function Classification System 88), Tardieu Scale, TCMS (Trunk Control Measurement Scale), MACS (Manual Ability Classification Scale), CFSS (Communication Function Classification System) for 18 months and received intensive rehabilitation.
Results
Improvements were observed especially in functional scales except for the Tardieu Scale, and no adverse effects were detected aside from a slight pain in the back.
Conclusion
Wider future case studies on UC-MSCs will enable us to assess the efficacy of UC-MSCs which have positive impacts especially on functional scales.
Keywords: Cerebral palsy, Mesenchymal stem cell, Rehabilitation
Introduction
Non-progressive lesions in the brain cause Cerebral Palsy. There might be functional disabilities in children with CP and periventricular leukomalacia, intrauterine haemorrhagia; stiffness, contractures, muscle strength weakness, sensory defects, and difficulties in balance and motion control may also be observed (1). Physical therapy, neurectomy, botulinum toxin A and medications may be used in the treatment of CP. It has been reported in several case studies that the above mentioned therapies can improve the functions partially; however, the complete cure cannot be achieved through these interventions (2). It has also been reported in previous studies that in developed countries, 1.5~2.5 children per 1,000 of the total population had Spastic CP; and this rate might be higher in developing countries (3). In traumas, inflammations and cerebral diseases, the brain has a relatively low-level renewable capacity i.e. self-repair capacity (4). Animal experiments and clinical studies in recent years have reported positive outcomes in cell transplantation for the treatment of various diseases. The central nervous system may be regenerated with cytotherapy, which is an option that aims to replace the functionally depleted cells because of a traumatic brain injury (5, 6). In 1976, Allogenic Mesenchymal Stem Cell treatments were first reported in the stromal compartment of the bone marrow (7). Prior to this development, a few studies had reported positive outcomes of using Mesenchymal Stromal Cells to treat neurological diseases like spinal cord injury and basilar artery dissection (8, 9). In recent time, a case study reported that intrathecal infusion of autologous bone marrow mononuclear cells showed that cell transplantation was effective and safe, and had encouraging functional results in a cerebral palsy patient (10). In a traumatic brain injury model, Lee et al. (11) used a combination of stem cell therapy with rehabilitation and reported that recovery results were similar to those when rehabilitation was used alone.
In this case report, we investigated the safety and efficacy of intrathecal, intramuscular and intravenous applications of UC-MSCs in a child with Cerebral Palsy.
Case Presentation
6-year-old male child patient (30-week, 1918 gr) had dystonic CP which was effective more in the lower extremity than in the upper one. The patient applied to us with intrauterine bleeding. The patient was born with head circumference 28 cm, height 41 cm, after 2-week incubator follow-up, and the brain MRI was performed. The patient was diagnosed with CP, and has been followed-up ever since. The patient has received various medical treatments such as baclofen and rehabilitation and partial benefits were reported.
Patient Assessment Tests
Functional examination
Eating, grooming, bathing, upper body dressing, lower body dressing, toileting, bladder, management, bed to chair transfer, toilet transfer, shower transfer, locomotion (ambulatory or wheelchair level), stairs, cognitive comprehension, expression, social interaction, problem solving, memory etc. evaluated with Functional Independent Measurement (FIM) (Table 1) (9). Functional independence was evaluated with scoring ranging from 18 to 126. Gross Motor Function Classification System 88 (GMFCS) (10) used to determine the observational functional level in children with cerebral palsy.
Table 1.
Results of patient assessment tests
| Followed-up | ||
|---|---|---|
|
| ||
| Onset | Sixt month after first intervention | |
| Functional examination | ||
| Functional Independent Measurement (FIM) | 56/126 | 76/126 |
| Gross Motor Function Classification System 88 (GMFCS) | Level 5 (Carried on a wheelchair pulled by hands). | Level 3 (The patient walks by using the walking aids held by hands). |
| Upper extremity | ||
| MACS (Manual Ability Classification Scale) | Level 3 (The patient can hold and use objects with difficulty, preparing the activities takes time). | Level 2 (Handles most objects but with some reduced quality and/or speed) |
| Trunk control and sitting balance Assessment | ||
| Static sitting balance | 2/20 | 10/20 |
| Dynamic sitting balance | ||
| Selective movement control | 2/28 | 17/28 |
| Dynamic reaching (Equilibrium reactions) | 1/10 | 4/10 |
| Total score | 5/58 | 31/58 |
| Communication skills | ||
| Communication Function Classification System (CFSS) | Level 3 (Effective Sender and Effective Receiver with familiar partners). | Level 2 (Receptive and Productive skills are slow but fluent with familiar and foreign partners). |
Upper extremity
In daily life, how children with CP use their hands was assessed with MACS (Manual Ability Classification Scale) (Table 1) (11). Manual Ability Classification System (MACS) describes how children with cerebral palsy use their hands to handle objects in daily activities. MACS describe five levels. The levels are based on the children’s self-initiated ability to handle objects and their need for assistance or adaptation to perform manual activities in every day.
Trunk control and sitting balance assessment
The sitting balance and functional independency during sitting was assessed with Trunk Control Measurement Scale (TCMS) test (Table 1) (12). Static sitting balance, dynamic sitting balances are considered in the subheadings of selective movement control and dynamic reaching (Equilibrium Reactions). Scoring is done on 58 points.
Lower extremity examination
Lower extremities were assessed with Modified Tardieu Scale (13). This scale quantifies muscle spasticity by assessing the response of the muscle to stretch applied at specified velocities and the results are listed in Table 2.
Table 2.
Tardieu Scale Assessment in lower extremity
| MUSCLE | Right/Left | X1 | SpasticityAngle (R1–R2) 1 | X2 | SpasticityAngle (R1–R2) 2 |
|---|---|---|---|---|---|
| Knee Flexors | Right | 2 | 25 | 2 | 25 |
| Left | 2 | 35 | 2 | 35 | |
| KneeExtensors | Right | 2 | 5 | 2 | 5 |
| Left | 2 | 7 | 2 | 7 | |
| AnklePlantar Flexor (Gastrocnemius) | Right | 3 | 25 | 3 | 25 |
| Left | 3 | 20 | 3 | 20 | |
| AnklePlantar Flexor (Soleus) | Right | 3 | 25 | 3 | 25 |
| Left | 3 | 20 | 3 | 20 |
Communication skills
Communication Function Classification System (CFSS) (14) provides 5 levels (CFCS I, II, III, IV, V) to describe everyday communication performance patients with cerebral palsy (Table 1).
The patient had speaking disorder, and had saliva coming out of the mouth. The patient also had growth retardation and the family described occasional difficulty in swallowing in solid foods. There was clonus in both feet especially in the left foot. Babinski result was negative. Pendulum test was positive. Thomas bilateral test result was positive.
Procedure
The clinical trial cases from the Republic of Turkey was approved by the ministry of health departments in organ and tissue transplantation (permission number; 56733164/203). The family was informed about all possible consequences and a written consent was received from the family.
The applications were made in surgery conditions by using masque anesthesia.
The intrathecal application was performed through Lumbar 3~4 vertebrae with a 22-Gouge spinal needle. Intravenous application; within 60 minutes, 1×106 cell/kg was applied (Table 3) in 500 cc isotonic with slow infusion and the patient was followed-up in the hospital for 1 day.
Table 3.
Transplantation details
| Date (year/month/day) | Cell count (intravenous) | Cell count (intrathecal) | Cell viability (%) |
|---|---|---|---|
| 2017/03/02 | 15×106 | 15×106 | 90.20 |
| 2017/03/17 | 15×106 | 15×106 | 90.48 |
| 2017/03/30 | 15×106 | 15×106 | 90.40 |
| 2017/04/13 | 15×106 | 15×106 | 91.20 |
After the applications, the patient was restricted for movements for 2 days, and the family was warned against water contact in the injection areas.
Isolation of MSCs from umbilical cord
Umbilical cord was obtained from a full-term delivery with informed maternal consent. UC-MSCs were produced at the Good Manufacturing Practice facility of LivMedCell, Istanbul, Turkey. The cord was washed, blood vessels removed and tissue cut into pieces (5~10 mm2) and cultured in culture plates. The culture expansion of small pieces of tissue is known as the “explants method.” The explants were left undisturbed for one week to allow the migration of cells from the margins of explants. After reaching 70% to 80% confluency, adherent cells were harvested with trypsinization by 0.05% trypsin-EDTA (Gibco, Germany). Quality control and quality assurance for the production of these cells at were performed according to the standards of the Turkish Medicines and Medical Devices Agency (TMMDA).
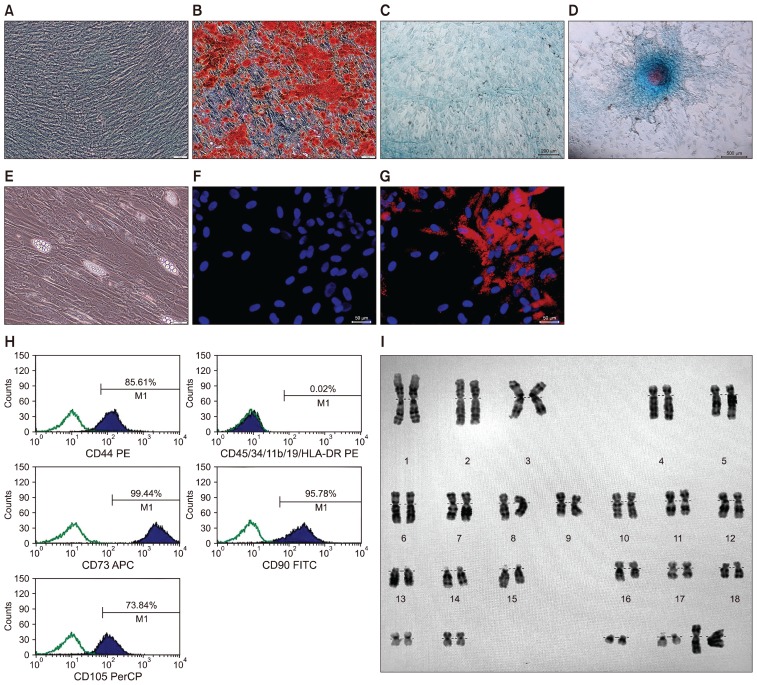
Characterization of UC-MSCs: Flow cytometry analysis of expressed surface antigens showed that these cells were uniformly positive for CD44, CD73, CD105 and CD90 and negative for the hematopoietic lineage markers CD34, CD45 and HLA-DR. MSC analysis kit (cat no:562245) was used for MSC characterization flow cytometry analysis. The kit contains control, positive cocktail and negative cocktail antibodies. Human MSCs were characterized by using the following conjugated monoclonal antibody combinations; negative cocktail (CD34 PE, CD19PE, CD45PE, CD11bPE and HLA-DR PE), positive coctail (CD90 FITC, CD44 PE, CD105 PerCP ve CD73 APC). Cells were analyzed on BD FACS Calibur (BD Bioscience, San Jose, CA) by using CellQuest Software program. The expression of negative and positive cocktail antibodies are shown on the histogram plot. Positive cocktail antibodies were analyzed on four histogram plots. Positive cocktail was shown in separate histograms because different color dyes were used for each of the antibodies (CD90 FITC, CD44 PE, CD105 PerCP ve CD73 APC). Negative cocktail antibodies are based on the average highest expression of the five antibodies, if one of the values is positive, the positive area will peak in the graph, so the negative cocktail values were shown on the same histogram plot, passing through the PE detector FL2 (All antibodies used in the negative cocktail are PE-labeled. For this reason, it can be shown on the same histogram). If the expression is high, each antibody is controlled separately. (Fig. 1H).
Fig. 1.
Characterization and differentiation of UC-MSCs. (A) Osteogenic differentiation control (B) and mineral nodules that stained by Alizarin Red S, of UC-MSCs cultured in osteogenic differentiation medium. (C) Chondrogenic differentiation control (D) and alcian blue staining of UC-MSCs cultured in chondrogenic differentiation medium. (E) Morphology, (F) adipogenic differentiation control and (G) Oil Red O staining of neutral lipid vacuole formation in UC-MSC cultured in adipogenic differentiation medium. (H) Flow cytometric analysis of cell surface markers of UC-MSCs at P3. (I) Chromosome karyotype analysis of the cultered UC-MSCs.
It has been showed that the telomerase activities of UC-MSCs stay stable during cell culture procedures (Data not shown). The expressions of some stem cell and differentiation markers such as TERT, POU5F1, SOX2, ZFP42, CD44, VCAM1, THY1, BMP2, RUNX-1, VIM, ICAM1, NES were determined (Data not shown). No structural or numerical chromosomal abnormalities were found in karyotype analyses of the cells (Fig. 1I).
The final UC-MSCs preparations used in the infusion were harvested from cell culture passage 3 and suspended at final densities that are 15×106/3 ml and 15×106/20 ml in normal saline.
In vitro differentiation of UC-MSCs
To induce adipogenic differentiation, cells were seeded onto six-well plates (P3; 3000 cells/cm2) and cultured with Mesencult MSC Basal Medium (StemCell Technologies Inc, Vancouver, BC, Canada) supplemented with 10% adipogenic supplement and 1% penicillin/streptomycin for 3 weeks. The medium was refreshed every 3~4 days. The formation of intracellular lipid droplets (Fig. 1E), which indicates adipogenic differentiation, was confirmed by staining with 0.5% oil red O (Sigma-Aldrich) (Fig. 1F, G).
For osteogenic differentiation, cells (P3; 3000 cells/cm2) were seeded on collagen-precoated (type I) coverslips in six-well plates. The differentiation medium composed of LDMEM supplemented with dexamethasone (0.1 mmol/L; Sigma-Aldrich), ascorbate-2-phosphate (0.05 mmol/L; Wako Chemicals, Richmond, VA), β-glycerophosphate (10 mmol/L; Sigma-Aldrich), primocin (2%; Invitrogen) and FBS (10%; Gibco/Life Sciences). Medium was refreshed twice a week. After four weeks, osteogenic differentiation was estimated by alizarin red staining. For Alizarin red staining, cells were fixed for 5 min in ice-cold 70% ethanol. The cells were stained with alizarin red solution (2%, pH 4.2) (Fig. 1A, B). Stained cells were dehydrated in pure acetone, fixed in acetone-xylene (1:1) solution and cleared with xylene.
For chondrogenic differentiation; MSCs isolated from the umbilical cord were induced in the following chondrogenic medium: DMEM, supplemented with 10% FBS, 2 mM L-glutamine, 50 μg/ml penicillin-streptomycin, 50 μg/ml ascorbic acid and 1 ng/ml human recombinant transforming growth factor β1 (TGF-β1). The differentiated cells were stained with alcian blue solution (Fig. 1C, D).
Rehabilitation program
As of the 3rd day of the application, intense physiotherapy and exercise program was started with the participation of the family. In each treatment session there were warm-up exercises, neck-trunk stabilization exercises, and postural control exercises. Exercises were done in the pool 3 days a week; and especially stretching exercises were applied to the extremities that had spasticity for longer durations. Exercises to develop the fine motor skills were prescribed.
No adverse effects were observed aside from a slight pain in the waist area during sitting up on the 1st day after the application. After the six months intervention results listed in Table 1 and 2.
Discussion
Mesenchymal stem cell is a new and promising treatment option in treating anomalies like CP that appear in the muscle-skeleton system depending on the permanent damage in the brain whose development is still ongoing. This is safe in terms of carsinogenity and biosafety (12). After 4 applications and within 1 year follow-up, no systemic adverse effects were observed in our case and following the intrathecal application, no local side-effects were detected in our case aside from a one-day mild back pain. Wang et al. (13) reported no adverse effects aside from mild temperature. No serious adverse effects have been reported in subarachnoid, intramuscular and intravenous applications in the literature (13–15). It is possible to react the lesion directly with subarachnoid application, local intramuscular injection may show increasing effects in the muscle mass and functions due to the secretion of several neurotropic factors (16). Similarly, with intravenous application, increases were reported in the hind limb activity and improvements in muscle functions in dogs with spinal cord injuries. Furthermore, the cells were detected in the liver and in the injured spinal cord and in the spleen. This situation might show the increasing effect of MSC on the liver to tolerate exercise (17).
MSCs have the ability to renew themselves, and may differentiate into various mesenchymal tissues (18). In addition, they may have positive effects on the cognitive functions in the brain with neuro-protection and neuro-regeneration. Several studies suggest that hAECs can exert neuro-protection and facilitate neuron regeneration in cerebral diseases like stroke, Parkinsonism in animal models of CNS disorders (19).
Sankar and Muthusamy (20) reported positive effects of MSC in central and peripheral tissues. It has been reported in previous studies that in monkeys with spinal cord injuries, MSCs supported the growth of host axons, avoided glial scar formation, avoided death of neurons, and induced new collateral sprouting without any inflammation or rejection. It has also been reported that MSCs can secrete neurotropic factors which promoted neuronal recovery of the damaged cells in the brain. These factors could also promote the synaptogenesis to re-innervate the lost connections. In addition, since hAECs show pluripotent properties, they can differentiate into a neuronal phenotype and thus replace the damaged or dead cells (21). Furthermore, hAECs can also act as “biological minipumps” in the CNS thus secreting necessary cytokines, growth factors, hormones, and/or neurotransmitters to restore cellular function. As a last item, hAECs can also improve stroke outcome potentially by modulating the inflammatory response (which contributes to the brain injury (21, 22)
In our case, we could not achieve any improvements in spasticity. Wang et al. reported improvements in muscle functions in cases that did not have any spasticity. There are several studies reporting obvious improvements in spasticity in some autologous MSC applications (21, 23).
In CP, application of UC-MSCs at earlier ages might bring higher achievement rates, which is also the case in any other treatment (24). An application that will be performed before complete neuron damage and joint contractures develop might increase the success of the treatment.
As a conclusion, we achieved improvements in cognitive skills, trunk control and hand skills; however, no improvements in spasticity. Future randomized-controlled and long-term studies may enlighten us on the superior sides and limitations of UC-MSCs Treatment.
Acknowledgment
We sincerely thanks Hande Başat, MD, and Physiotherapist Burcu Çaylı for their devoted rehabilitation treatment.
Footnotes
Potential Conflict of Interest
The authors have no conflicting financial interest.
References
- 1.Nelson KB. Can we prevent cerebral palsy? N Engl J Med. 2003;349:1765–1769. doi: 10.1056/NEJMsb035364. [DOI] [PubMed] [Google Scholar]
- 2.Koman LA, Smith BP, Shilt JS. Cerebral palsy. Lancet. 2004;363:1619–1631. doi: 10.1016/S0140-6736(04)16207-7. [DOI] [PubMed] [Google Scholar]
- 3.Paneth N, Hong T, Korzeniewski S. The descriptive epidemiology of cerebral palsy. Clin Perinatol. 2006;33:251–267. doi: 10.1016/j.clp.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Lu D, Mahmood A, Wang L, Li Y, Lu M, Chopp M. Adult bone marrow stromal cells administered intravenously to rats after traumatic brain injury migrate into brain and improve neurological outcome. Neuroreport. 2001;12:559–563. doi: 10.1097/00001756-200103050-00025. [DOI] [PubMed] [Google Scholar]
- 5.Longhi L, Zanier ER, Royo N, Stocchetti N, McIntosh TK. Stem cell transplantation as a therapeutic strategy for traumatic brain injury. Transpl Immunol. 2005;15:143–148. doi: 10.1016/j.trim.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Azari MF, Mathias L, Ozturk E, Cram DS, Boyd RL, Petratos S. Mesenchymal stem cells for treatment of CNS injury. Curr Neuropharmacol. 2010;8:316–323. doi: 10.2174/157015910793358204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976;4:267–274. [PubMed] [Google Scholar]
- 8.Ichim TE, Solano F, Lara F, Paris E, Ugalde F, Rodriguez JP, Minev B, Bogin V, Ramos F, Woods EJ, Murphy MP, Patel AN, Harman RJ, Riordan NH. Feasibility of combination allogeneic stem cell therapy for spinal cord injury: a case report. Int Arch Med. 2010;3:30. doi: 10.1186/1755-7682-3-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han H, Chang SK, Chang JJ, Hwang SH, Han SH, Chun BH. Intrathecal injection of human umbilical cord blood-derived mesenchymal stem cells for the treatment of basilar artery dissection: a case report. J Med Case Rep. 2011;5:562. doi: 10.1186/1752-1947-5-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Purandare C, Shitole DG, Belle V, Kedari A, Bora N, Joshi M. Therapeutic potential of autologous stem cell transplantation for cerebral palsy. Case Rep Transplant. 2012;2012:825289. doi: 10.1155/2012/825289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee AS, Tang C, Rao MS, Weissman IL, Wu JC. Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat Med. 2013;19:998–1004. doi: 10.1038/nm.3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phermthai T, Thongbopit S, Pokathikorn P, Wichitwiengrat S, Julavijitphong S, Tirawanchai N. Carcinogenicity, efficiency and biosafety analysis in xeno-free human amniotic stem cells for regenerative medical therapies. Cytotherapy. 2017;19:990–1001. doi: 10.1016/j.jcyt.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Ji H, Zhou J, Xie J, Zhong Z, Li M, Bai W, Li N, Zhang Z, Wang X, Zhu D, Liu Y, Wu M. Therapeutic potential of umbilical cord mesenchymal stromal cells transplantation for cerebral palsy: a case report. Case Rep Transplant. 2013;2013:146347. doi: 10.1155/2013/146347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehta T, Feroz A, Thakkar U, Vanikar A, Shah V, Trivedi H. Subarachnoid placement of stem cells in neurological disorders. Transplant Proc. 2008;40:1145–1147. doi: 10.1016/j.transproceed.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 15.Rengasamy M, Gupta PK, Kolkundkar U, Singh G, Balasubramanian S, SundarRaj S, Chullikana A, Majumdar AS. Preclinical safety & toxicity evaluation of pooled, allogeneic human bone marrow-derived mesenchymal stromal cells. Indian J Med Res. 2016;144:852–864. doi: 10.4103/ijmr.IJMR_1842_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cruz-Martinez P, Pastor D, Estirado A, Pacheco-Torres J, Martinez S, Jones J. Stem cell injection in the hindlimb skeletal muscle enhances neurorepair in mice with spinal cord injury. Regen Med. 2014;9:579–591. doi: 10.2217/rme.14.38. [DOI] [PubMed] [Google Scholar]
- 17.Kim Y, Jo SH, Kim WH, Kweon OK. Antioxidant and anti-inflammatory effects of intravenously injected adipose derived mesenchymal stem cells in dogs with acute spinal cord injury. Stem Cell Res Ther. 2015;6:229. doi: 10.1186/s13287-015-0236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei CC, Lin AB, Hung SC. Mesenchymal stem cells in regenerative medicine for musculoskeletal diseases: bench, bedside, and industry. Cell Transplant. 2014;23:505–512. doi: 10.3727/096368914X678328. [DOI] [PubMed] [Google Scholar]
- 19.Snyder EY, Yoon C, Flax JD, Macklis JD. Multipotent neural precursors can differentiate toward replacement of neurons undergoing targeted apoptotic degeneration in adult mouse neocortex. Proc Natl Acad Sci U S A. 1997;94:11663–11668. doi: 10.1073/pnas.94.21.11663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sankar V, Muthusamy R. Role of human amniotic epithelial cell transplantation in spinal cord injury repair research. Neuroscience. 2003;118:11–17. doi: 10.1016/s0306-4522(02)00929-6. [DOI] [PubMed] [Google Scholar]
- 21.Lindvall O, Kokaia Z. Recovery and rehabilitation in stroke: stem cells. Stroke. 2004;35(11 Suppl 1):2691–2694. doi: 10.1161/01.STR.0000143323.84008.f4. [DOI] [PubMed] [Google Scholar]
- 22.Broughton BR, Lim R, Arumugam TV, Drummond GR, Wallace EM, Sobey CG. Post-stroke inflammation and the potential efficacy of novel stem cell therapies: focus on amnion epithelial cells. Front Cell Neurosci. 2013;6:66. doi: 10.3389/fncel.2012.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaquero J, Zurita M, Rico MA, Bonilla C, Aguayo C, Fernández C, Tapiador N, Sevilla M, Morejón C, Montilla J, Martínez F, Marín E, Bustamante S, Vázquez D, Carballido J, Rodríguez A, Martínez P, García C, Ovejero M, Fernández MV Neurological Cell Therapy Group. Repeated subarachnoid administrations of autologous mesenchymal stromal cells supported in autologous plasma improve quality of life in patients suffering incomplete spinal cord injury. Cytotherapy. 2017;19:349–359. doi: 10.1016/j.jcyt.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein M. The treatment of cerebral palsy: what we know, what we don’t know. J Pediatr. 2004;145(2 Suppl):S42–S46. doi: 10.1016/j.jpeds.2004.05.022. [DOI] [PubMed] [Google Scholar]