Abstract
Objective
Suicide risk mitigation by reducing access to lethal means, such as firearms and potentially lethal medications, is a highly-recommended practice. To better understand groups of patients at risk of suicide in medical settings, demographic and clinical risk factors were compared for patients who die by suicide using firearms or other means to matched patients who did not die by suicide (controls).
Methods
A case-control study of 2674 suicide cases from 2010 – 2013, from eight healthcare systems within the Mental Health Research Network, matched to 267,400 controls. In 2016, the association of suicide by firearms or other means with medical record information on demographics, general medical disorders (GMD) and mental disorders (MD) was assessed.
Results
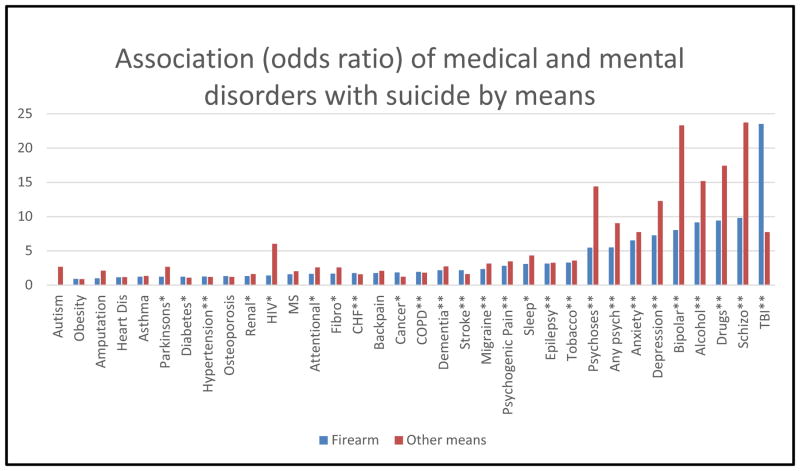
Patients with any mental disorder were more likely to die by non-firearm means. Fourteen GMDs had statistically significant odds ratios for firearm suicide particularly, traumatic brain injury (TBI) = 23.53 (18.84 – 29.39; p<.001), epilepsy = 3.17 (1.97 – 5.08; p<.001), psychogenic pain 2.82 (1.53–5.19, p<.001), migraine 2.35 (1.64–3.36, p<.001), and stroke 2.20 (1.66–2.93; p<.001). Fifteen GMDs had significant odds ratios for other means, with particularly high ratios for TBI 7.74 (5.71–10.50; p<.001), epilepsy 3.28 (2.07–5.21; p<.001), HIV 6.03 (3.60–10.10; p<.001), and migraine 3.17 (2.44–4.11; p<.001).
Conclusions
Medical providers should consider targeting suicide risk screening in patients with any mental disorder, TBI, epilepsy, HIV, psychogenic pain, stroke and migraine. When suicide risk is detected, counseling on reducing access to lethal means should include both firearms and other means for at risk groups.
Keywords: Suicide, Lethal Means, Firearms, Medical Illness Burden, Traumatic Brain Injury
INTRODUCTION
Suicide is the 10th leading cause of death among all persons and the third leading cause of death among middle-aged persons 20–50 years (1). The fatality rates of suicide attempts vary substantially depending on means: firearms 85%, suffocation 69%, poisoning/overdose 2%, other means 2% (2). While homicide and accidental shootings receive the most attention in the media and in policy contexts, 63% of firearm injuries in the United States are self-inflicted (3). Approximately 50% of all suicide deaths occur by firearm, 20% by suffocation/hanging, 20% by medication or chemical poisoning, and 10% by other methods (e.g., jumping, sharp object, drowning) (2, 4).
The recent rise in suicide mortality (5) and recognition of the healthcare setting as an opportunity for prevention (4, 6, 7), led to recommendations for providers in multiple health care settings to increase suicide screening and conduct means restriction counseling for at-risk patients (8). Means restriction counseling occurs when a medical or behavioral health provider advises a patient, their family or both to voluntarily remove access to objects that may be used for suicide such as firearms, potentially lethal medications, sharp objects, and suffocation instruments (9). When patients are identified at risk for suicide in primary care, typically during depression screening, means restriction counseling is a highly recommended risk management practice (10). Patients and family members are usually receptive to means restriction counseling when suicide risk is identified (11, 12).
Despite these recommendations, means restriction counseling delivery rates are low in provider surveys. Only 4–14% of emergency department physicians and 22% of psychologists discuss means following a suicide attempt (13, 14). This is concerning because 10% patients who make non-fatal suicide attempts will go on to die by suicide, and 25% will have a subsequent non-fatal attempt (15, 16). Some have suggested that means restriction counseling rates may be low because providers do not believe in its effectiveness, (17) and instead focus on mitigating intent. Suicidal intent is impulsive or not planned in advance in 82% of attempts (18) and estimated to last from 5 minutes to 1 hour (19, 20). The opportunity for providers to intervene effectively when suicide intention arises is dependent on patients accessing care during times of crisis. Means restriction counseling is a promising approach to save lives by creating a barrier to the impulsive intent of self-harm that is independent of the patient voluntarily accessing care. Effective and efficient means restriction counseling relies on reliably identifying which patients to screen for suicide to determine those who would benefit.
Identifying patients at risk for suicide in general medical settings is challenging. Recent evidence suggests that relying solely on pre-existing mental diagnoses or expectation that patients will spontaneously volunteer risk symptoms is problematic (10, 21). For example, of people who die by suicide, 57% of veterans (22) and 50% of civilians (4), had no recorded history of a mental disorder (MDs) at the time of their death. Yet, 45% of patients seek medical care within one month prior to suicide death (4, 23). These findings highlight a gap in the current implementation of suicide risk detection in general medical settings, which typically only occurs following a positive depression screen.
Identifying general medical disorders (GMDs) that may be significant risk factors for suicide is important to inform suicide risk detection. Using the same data source as the current study, our group conducted one of the largest US based studies examining the association of common GMDs with suicide (24). Findings indicated particularly high odds ratios for traumatic brain injury, sleep disorders and HIV/AIDs, after controlling for mental health and substance use conditions. The current study will build our previous work to examine the association of GMDs and MDs with specific means for suicide.
The objectives of this study were to identify patients most at risk for suicide death by firearms as compared to other means using data that are readily available to health care providers. We compared patients who died by firearm versus other means of suicide to matched patients who did not die by suicide (controls) and explored demographic and clinical variables as predictors for risk by means of suicide death. Understanding this constellation of risk factors has the potential to inform suicide risk assessment and prevention practices that incorporate more informed means restriction counseling.
METHODS
Sample, Settings, and Data
In 2016, we conducted a case-control study of 2,674 adult and adolescent patients who died by suicide and 267,400 patients who did not die by suicide. Patients were members served by eight learning healthcare systems within the Mental Health Research Network (26). The network sites in this study included: Henry Ford Health System (Michigan), HealthPartners (Minnesota), Harvard Pilgrim Health Care (Massachusetts), and Kaiser Permanente health systems in Colorado, Georgia, Hawaii, Oregon, and Washington. Each site offers integrated medical and mental health care services including individual and group therapy, intensive outpatient programs, and psychiatric medication management. These sites cover 3,041,000 total lives with population demographics mirroring the surrounding urban and suburban geographic areas. Detailed population demographics and health plan characteristics stratified by site are available via the Mental Health Research Network website (26).
A random sample of 100 control patients were matched to each of the 2,674 suicide cases by site and year of death. The date of suicide death was considered the index date for cases and their matched controls were assigned the same index date. All participants were continuously enrolled in a health plan for at least 10 months during the year prior to the index date, which allows for a small dis-enrollment gap during the month of death. Each site received Institutional Review Board approval.
All data were extracted from a Virtual Data Warehouse that includes electronic health record and insurance claims data (27–29). The Virtual Data Warehouse is a set of variables with mutually agreed upon validated definitions across each site to facilitate multisite research projects across the network. This allows each site to retain their own private patient medical and mental health record data, but overcome the challenge of data harmonization inherent in multisite research. There are routine data quality verifications to ensure the standard variables are defined similarly across systems. Death data are verified with mortality records from national, state, and local public health organizations by Social Security numbers or a combination of patient names, birthdates, and demographic profiles.
To identify patients who died by suicide and method of suicide, we used International Classification of Diseases, 10th revision (ICD-10) codes of X72–74 to define firearm suicide and ICD-10 codes of X60–71, X75–84 and Y87.0 to define other means (30). Other means included all non-firearm means, with poisoning and hanging/suffocation being the most common. International Classification of Diseases, 9th revision (ICD-9) codes were captured from health system encounters (in-patient and out-patient), to ascertain diagnoses within the year prior to the date of death for all study patients (31). Diagnoses were extracted for 12 major mental health and substance use conditions and 19 GMDs (Table 2). Demographic information on age and sex were available from the data warehouse and neighborhood income and education were estimated using geocoded addresses and census block data.
TABLE 2.
Association of mental and medical disorders with suicide by means (risk adjusted for sex and age)
| Mental Disorder | Means group | % cases with condition (Firearm n= 1298; Other means n =1376) | OR | 95% CI | Inter group p-val |
|---|---|---|---|---|---|
| Any psychiatric disorder | Firearm | 55.39 | 5.51* | (4.92 – 6.16)* | .001 |
| Other mean | 66.93 | 9.04* | (8.06 – 10.15)* | ||
| Alcohol abuse or dependence | Firearm | 12.71 | 9.15* | (7.66 – 10.93)* | .003 |
| Other mean | 16.72 | 15.19* | (13.04 – 17.68)* | ||
| Anxiety disorder | Firearm | 21.96 | 6.53* | (5.68 – 7.50)* | .001 |
| Other mean | 28.20 | 7.74 * | (6.84 – 8.75)* | ||
| Attention disorder | Firearm | 1.62 | 1.65 | (1.06 – 2.57) | .017 |
| Other mean | 3.34 | 2.60* | (1.92 – 3.53)* | ||
| Autism | Firearm | 0i | - | - | .913 |
| Other mean | .36i | 2.04 | (.84 – 4.97) | ||
| Bipolar | Firearm | 4.01 | 8.04* | (5.97 – 10.83)* | .001 |
| Other mean | 11.70 | 23.32* | (19.43 – 27.98)* | ||
| Dementia | Firearm | 2.31 | 2.20* | (1.50 – 3.29)* | .915 |
| Other mean | 2.25 | 2.75* | (1.89 – 3.99)* | ||
| Depression | Firearm | 35.13 | 7.29* | (6.46 – 8.23)* | .001 |
| Other mean | 48.69 | 12.28* | (10.96 – 13.74)* | ||
| Drug abuse or dependence | Firearm | 6.63 | 9.43* | (7.44 – 11.95)* | .001 |
| Other mean | 11.05 | 17.42* | (14.51 – 20.92)* | ||
| Other Psychosis | Firearm | 2.62 | 5.49* | (3.79 – 7.96)* | .001 |
| Other mean | 4.87 | 14.39* | (10.96 – 18.89)* | ||
| Schizophrenia | Firearm | 1.31 | 9.82* | (5.82 – 16.56)* | .003 |
| Other mean | 3.20 | 23.74* | (16.89 – 33.36)* | ||
| Sleep disorder | Firearm | 17.23 | 3.09* | (2.65 – 3.59)* | .003 |
| Other mean | 19.62 | 4.33* | (3.76 – 4.97)* | ||
| Prior suicide attempt (E950 – 958) | Firearm | 8.40 | 271.62* | (186.59 – 395.40)* | .011 |
| Other mean | 13.23 | 323.84* | (243.38 – 430.88)* | ||
| Tobacco use | Firearm | 22.57 | 3.29* | (2.87 – 3.78)* | .645 |
| Other mean | 20.06 | 3.61* | (3.14 – 4.14)* | ||
| Medical Disorders | |||||
| Amputation | Firearm | .31i | 1.00 | (.37 – 2.72) | .533 |
| Other mean | .44i | 2.13 | (.94 – 4.83) | ||
| Asthma | Firearm | 5.55 | 1.23 | (.97 – 1.56) | .199 |
| Other mean | 6.83 | 1.35* | (1.09 – 1.67)* | ||
| Back pain | Firearm | 21.80 | 1.78* | (1.10 – 6.54)* | .3 |
| Other mean | 23.26 | 2.10* | (1.84 – 2.39)* | ||
| Traumatic brain injury | Firearm | 9.48 | 23.53* | (18.84 – 29.39)* | .001 |
| Other mean | 3.42 | 7.74* | (5.71 – 10.50)* | ||
| Cancer | Firearm | 11.33 | 1.86* | (1.55 – 2.24)* | .001 |
| Other mean | 6.18 | 1.25 | (0.99 – 1.57) | ||
| CHF | Firearm | 5.55 | 1.76* | (1.36 – 2.27)* | .024 |
| Other mean | 3.34 | 1.60* | (1.17 – 2.17)* | ||
| COPD | Firearm | 11.40 | 1.94* | (1.62 – 2.33)* | .062 |
| Other mean | 8.79 | 1.84* | (1.57 – 2.23)* | ||
| Diabetes | Firearm | 13.56 | 1.25* | (1.06 – 1.48)* | .002 |
| Other mean | 9.81 | 1.11 | (0.92 – 1.33) | ||
| Epilepsy | Firearm | 1.46 | 3.17* | (1.97 – 5.08)* | .966 |
| Other mean | 1.38 | 3.28* | (2.07 – 5.21)* | ||
| Fibromyalgia | Firearm | 3.00 | 1.68* | (1.21 – 2.33)* | .004 |
| Other mean | 5.23 | 2.61* | (2.04 – 3.32)* | ||
| Heart disease | Firearm | 9.94 | 1.15 | (0.94 – 1.39) | .004 |
| Other mean | 6.69 | 1.18 | (.95 – 1.48) | ||
| HIV/AIDS | Firearm | .39i | 1.41 | (.58 – 3.45) | .023 |
| Other mean | 1.16 | 6.03* | (3.60 – 10.10)* | ||
| Hypertension | Firearm | 30.74 | 1.28* | (1.12 – 1.47)* | .001 |
| Other mean | 24.93 | 1.22* | (1.04 – 1.40)* | ||
| Migraine | Firearm | 2.47 | 2.35* | (1.64 – 3.36)* | .002 |
| Other mean | 4.51 | 3.17* | (2.44 – 4.11)* | ||
| Multiple Sclerosis | Firearm | .31i | 1.61 | (0.59 – 4.38) | .510 |
| Other mean | .44i | 2.05 | (.91 – 4.61) | ||
| Obesity | Firearm | 4.85 | 0.93 | (.72 – 1.20) | .946 |
| Other mean | 4.87 | 0.90 | (.70 – 1.15) | ||
| Osteoporosis | Firearm | 1.46 | 1.32 | (.83 – 2.11) | .351 |
| Other mean | 2.11 | 1.20 | (.82 – 1.75) | ||
| Parkinson’s | Firearm | .69i | 1.24 | (.63 – 2.44) | .423 |
| Other mean | .87 | 2.70 * | (1.50 – 4.87)* | ||
| Psychogenic pain | Firearm | .8 | 2.82* | (1.53 – 5.19)* | .001 |
| Other mean | 1.38 | 3.47* | (2.19 – 5.51)* | ||
| Renal disorder | Firearm | 7.01 | 1.34 | (1.07 – 1.68) | .199 |
| Other mean | 5.89 | 1.62* | (1.27 – 2.05)* | ||
| Stroke | Firearm | 4.31 | 2.20* | (1.66 – 2.93)* | .064 |
| Other mean | 2.33 | 1.62* | (1.13 – 2.33)* |
p<.01.
Percentages are calculated independently for each mean category. For example, any psychiatric disorder by other means has 921 patients with a psychiatric disorder among 1,376 patients who died by other means (66.93%). i: Cell size is less than 10 cases, interpret with caution.
ICD9 codes included the following: mental health and substance use conditions (290–319), asthma (493), back pain (720.0–724.9), cancer (140–209), congestive heart failure (CHF) (402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428), COPD (490–492, 494, 496), diabetes mellitus (250), epilepsy (345), fibromyalgia (729.1), heart disease (410–414), HIV/AIDS (042,043,044,V08), hypertension (401), migraine (346), multiple sclerosis (340), osteoporosis (733.0–733.09), Parkinson’s disease (332), psychogenic pain (307.8, 307.89), renal disease (403, 582, 583, 585, 586, 588, 404.02, 404.12, 404.92, 593.9), sleep disorder (291.82, 307.4, 327, 780.5), and traumatic brain injury (800, 801, 803, 804, 850–854).
Statistical Analyses
All statistical analyses were carried out using SAS 9.4. Descriptive statistics summarized demographic variables, MDs, and GMDs for each suicide death group (firearms and other means). To determine the association of MDs and GMDs with suicide death, we used a series of logistic regressions to calculate odds ratios (ORs) and 95% confidence intervals (CIs). Four separate models were analyzed to determine the relative contributions of demographic and clinical variables to odds for suicide by firearms or other means. Multivariable models 1 and 2 were fit using logistic regression with dependent variables: 1.) firearm suicide vs. control 2.) other means suicide vs. control. Co-variates included age, sex, and condition (e.g. diabetes). For models 1 and 2, separate models were run for each of the 35 conditions and the odds ratios for each condition are reported (Table 2).
To evaluate the difference in association between suicide and individual conditions between the firearm vs. other means group, model 3 included a gun*condition interaction term. The interaction p-value detects whether there are statistically significant differences between the firearm and other means groups. If this is significant, the two models (1 & 2) are sufficient to describe the associations.
Due to large gender differences in the means of suicide, we isolated the impact of gender and comorbidity using an interaction in a fourth logistic regression model. To determine comorbidity, we defined a variable for zero, one, or two or more GMDs using the following: asthma, back pain, TBI, cancer, CHF, COPD, diabetes, heart disease, HIV, hypertension, epilepsy, migraine, multiple sclerosis, osteoporosis, Parkinson’s, psychogenic pain, renal disorders, and stroke. To isolate the effect of GMD comorbidity from MDs, we defined a binary covariate for presence of any MD, that was only included in model 4. Additionally, we included age, education and income as covariates in the model. Separate models were run for firearm and other means groups. We were primarily interested in the odds ratios associated with different comorbidity levels (0,1,2+) within each gender.
RESULTS
Our sample included 2,674 cases of suicide death, 1,298 (49%) by firearm and 1,376 (51%) by other means. Suicide death cases were mostly men (77%) with a higher proportion of men among firearm (89.2%) versus other means (66.4%). Most cases (61.3%) had at least one MD with the highest prevalence for alcohol, anxiety, depression, and sleep disorders, respectively. This rate is higher compared to previous studies conducted by the network that report 50% of suicide cases with MDs, due to the inclusion of dementia and tobacco smoker in the MD definition. A substantial portion of cases did not have a psychiatric disorder diagnosed in the year prior to suicide death (44.61% for firearms and 33.07% for other means). Compared to controls (Table 1), firearm suicide cases were significantly more likely to be older, male, have lower education, or have lower incomes. Deaths by other means showed similar patterns, but did not show differences in education.
TABLE 1.
Suicide cases vs. controls by means and demographic variables
| Firearm | Other means | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Controls (n=129,800) | Controls % | Cases (n = 1298) | Cases % | P-val | Controls (n=137,600) | Controls % | Cases (n = 1376) | Cases % | P-val | |
| Average Age (years) | 39.5 +/− 22 | 53 +/− 19.1 | .001 | 39.1 +/− 21.9 | 47.1 +/− 18.4 | .001 | ||||
| <20 years | 33900 | 26% | 66 | 5% | 36177 | 26% | 149 | 11% | ||
| 21–30 years | 12820 | 10% | 120 | 9%, | 13790 | 10% | 135 | 10% | ||
| 31–40 years | 17245 | 13% | 146 | 11%, | 18475 | 13% | 181 | 13% | ||
| 41–50 years | 21416 | 16% | 238 | 18%, | 22989 | 17% | 326 | 24% | ||
| 51–60 years | 21005 | 16% | 281 | 22% | 22239 | 16% | 303 | 22% | ||
| 61–70 years | 12642 | 10% | 182 | 14% | 13209 | 10% | 132 | 10% | ||
| 71–80 years | 6990 | 5% | 149 | 11%, | 6986 | 5% | 72 | 5% | ||
| >80 years | 3781 | 3% | 116 | 9% | 3735 | 3% | 78 | 6% | ||
| Female (%) | 68145 | 52.5% | 140 | 10.8% | .001 | 52.5% | 33.6% | .001 | ||
| College education (%) | 45430 | 35% | 428 | 33% | .001 | 35% | 36% | .077 | ||
| Average yearly household neighborhood income ($) | $68,466 +/− $28,743 | $65,793 +/− $27,371 | .001 | $70,382 +/− $29,457 | $68,502 +/− $29,544 | .007 | ||||
We found that age and sex (Table 1) varied significantly between cases and controls, and therefore, we adjusted for sex and age only in our subsequent models for testing the association between specific MDs and GMDs and suicide by firearms vs. other means. Adjustment primarily reduced the odds for firearm suicide among many conditions by correcting for cases being primarily male and older. The clinical differences between college education and income, while statistically significant, were not substantial enough to be considered clinically meaningful and for this reason were not included.
In Table 2, we compared the odds of MDs between suicide cases and controls. We observed significant odds ratios for both means for all mental disorders, except autism. Notably, the odds ratios were significantly larger for the other means group compared to the firearms group across all mental disorders except autism, sleep and tobacco (inter-group p-val). For example, the odds for depression in the other means group is 12.28 times higher for cases versus controls and this odds ratio is significantly higher than the odds for depression in the firearm group of 7.29. This implies that patients with mental disorders are more likely to use a non-firearm mean for suicide.
Table 2 also shows the odds for GMDs between suicide cases and controls. The odds for 14 GMDs are statistically significant, but substantially lower than MDs with some notable exceptions. For firearm suicide, the odds were particularly high for TBI = 23.53 and epilepsy = 3.17. For other means, we identified 15 GMDs with significant odds ratios with particularly high ratios for TBI = 7.74, epilepsy = 3.28, HIV = 6.03, migraine = 3.17 and psychogenic pain = 3.47.
In our analysis of GMD comorbidity burden, we found that for males, increasing GMD comorbidity burden was indicative of increasing odds for firearm suicide (0 vs. 2+ conditions: OR = 1.94 (1.64 – 2.78), but not for other means of suicide (0 vs. 2+ conditions: OR = 1.23 (1.0, 1.48). For females, we found the opposite pattern, with larger odds for other means of suicide as comorbidity burden increased (0 vs 2+ conditions: OR = 2.41 (1.94 – 3.04)), but not for firearms (0 vs 2+ conditions: OR = 0.99 (0.66, 1.47).
DISCUSSION
We aimed to identify salient risk factors that are easily identifiable by general medical and mental health providers for firearm suicide as compared to other means of suicide. Our findings indicate that for nearly all mental and substance use disorders, the odds for suicide death with firearms was substantially less than the odds with non-firearm means. The most common non-firearm means in our sample, consistent with national statistics (5), were medication overdose and suffocation/hanging. Assessing for stockpiles of medications and objects (e.g., ropes, belts) used for hanging, which are often easily available in the home, is advised for patients at risk of suicide with mental health and substance use histories (7). Surprisingly, we observed that substance use disorders had higher odds for suicide compared to many other mental disorders. This indicates the need for suicide risk mitigation for all means as a key component of substance use treatment. There are several trainings for mental health and medical providers available on lethal means restriction counseling that emphasize motivational methods to engage both patients and family members in safety planning (7, 32). Family members are essential to help monitor access to all types of lethal means that may be readily available within the home, particularly non-firearm means that may be easily acquired by persons at risk. Ease of accessing non-firearm means may deter some providers from means assessment because eliminating access may seem impossible. Some non-firearm means, particularly overdose by non-opioid medications, are less lethal due to lower case fatality rates (33); however, non-firearm means accounted for more suicide deaths among all MDs. Counseling to reduce access to the most toxic substances or medications in overdose (e.g. opioids) and materials used for suffocation (e.g. ropes) would reach the largest groups of patients dying by non-firearm means.
The probability for co-occurring MDs should contextualize our results for the association of GMDs with suicide. There is an established and well-recognized direct causal relationship between MDs and suicide with 90% of decedents’ families reporting mental symptoms prior to death (34). Our group conducted a prior study that compared the association of GMDs and suicide with and without MD controls (24). For the current study, we chose not to control for MDs in our GMDs analysis for individual conditions because half of patients who die by suicide do not have a MD diagnosed in the medical record. Therefore, we assume many have undiagnosed MDs and our results for GMDs illuminate which disorders should trigger additional risk screening. For GMDs, we do not assume that our results indicate a direct causal association with suicide; instead, we suggest that the associations with GMDs established here indicate which GMDs may co-occur with MDs and increase risk for suicide. Interestingly, the GMDs with the highest association for suicide in our results are those with high rates of comorbidity with MDs or characterized by organic injury to the brain. In the firearms group, these included TBI, epilepsy, psychogenic pain, migraine, and stroke. For other means, we observed substantially increased odds for TBI, epilepsy, HIV, migraine, and psychogenic pain. There is some prior literature from smaller samples, or large samples from other countries, suggesting each of these conditions may have an association with mental health comorbidity, suicide ideation, or suicide attempt (35–40).
We chose to control for MDs in the comorbidity analysis because, we wanted to try to isolate the impact of GMD comorbidity, however we acknowledge that our estimates are potentially biased due to MD under-diagnosis. Our results should still be a flag for providers to pay attention to patients with GMD comorbidity for suicide risk. We observed that the risk for suicide in women with multiple comorbidities was notably higher for other means, but not for firearms. It is possible that much of this risk comes from prescription pain medication overdoses among women in their middle ages, especially white women (41). Among the substances used for overdose, prescription pain medications (e.g., opioids) are the most lethal (42). Our results show especially high risk for other means among those with fibromyalgia, back pain, psychogenic pain, and migraine, which are chronic pain conditions that are more common in women (43), frequently involve pain medication prescription and have high mental health comorbidity (44–46). This would indicate that women with multiple comorbidities and/or conditions that involve prescription pain medications are a high-risk group, who medical providers may consider screening for suicide and subsequent assessment for stockpiles of medication as a lethal means for suicide.
For men, the impact of GMD comorbidity increased risk for firearm suicide, but not for other means. These findings are consistent with national surveillance data showing that men, 45–64 years of age, have the highest rate of firearm suicide death (42). Additionally, in the US, 45% of males own a firearm compared to 11% of women (47). In light of these data, general medical providers may consider suicide risk screening and subsequent assessment for access to firearms in men with multiple GMD comorbidity. A Florida law known as “docs vs. glocks” which prohibited physicians from asking about or documenting gun ownership in medical records, was recently found to be unconstitutional (48). A federal court determined that physician’s right to free speech includes discussing firearms with patients and that this doesn’t impinge upon the second amendment right to bear arms.
CONCLUSIONS
Our analysis implicates several novel groups of patients that medical and mental health providers may consider for suicide risk assessment and means restriction counseling beyond mental disorders. This includes those with TBIs, HIV, epilepsy, pain conditions, stroke and migraine. Men with medical comorbidities should be targeted for suicide risk screening and counseled to reduce access to firearms when risk is detected. Those with substance use disorders should be screened for suicide and assessed for access to both firearm and other means. Our results suggest a need for an analysis that directly investigates the link between prescription pain medication overdose and suicide mortality among women with pain conditions.
Figure 1.
Odds ratios for firearm and other means of suicide among all medical and mental health conditions*One mean group (e.g. firearms only or other means only) had significant association (p<.05) with suicide death
**Both mean groups had significant association (p<.05) with suicide death
TABLE 3.
Risk for medical comorbidity burden by suicide method among males and females
| Male or female | Chronic condition comparison | Firearms OR | Firearms 95% CI | Others means OR | Other means 95% CI |
|---|---|---|---|---|---|
| Male | 0 vs. 1 | 1.25* | (1.06 – 1.48)* | 1.11 | (.93 – 1.32) |
| Male | 0 vs. 2+ | 1.94* | (1.64 – 2.78)* | 1.23 | (1.0 – 1.48) |
| Male | 1 vs. 2+ | 1.55* | (1.32 – 1.83)* | 1.11 | (.92 – 1.34) |
| Female | 0 vs. 1 | .99 | (.65 – 1.50) | 1.53* | (1.19 – 1.97)* |
| Female | 0 vs. 2+ | .99 | (.66 – 1.47) | 2.41* | (1.91 – 3.04)* |
| Female | 1 vs. 2+ | 1.00 | (.64 – 1.56) | 1.58* | (1.25 – 1.99)* |
p<.01.
Risk adjusted for sex, age, college education, income, site, and mental disorders. All co-variates entered the logistic regression significantly at p<.01 except college education and income for the firearm group.
Acknowledgments
Contributors: The fourteen listed authors were the sole contributors to this manuscript. Dr. C was responsible for all aspects of the study including overseeing data collection and ensuring data integrity from all sites. Ms. Y drafted the manuscript. Ms. Y, Drs. A, B, C and D had full access to the study data to evaluate the accuracy of the analysis. Ms. Y, Drs. A, B, C, and D were responsible for study concept and design. Critical revision of the manuscript was conducted by all authors. Dr. D was responsible for statistical analysis.
Conflict of Interest: The authors declare no conflicts of interest
Funders: All authors were supported by an award from the National Institute of Mental Health (NIH)
Prior presentations: There have been no prior presentations of this work
Contributor Information
Jennifer M. Boggs, Kaiser Permanente Colorado - Institute for Health Research, Denver, Colorado
Arne Beck, Kaiser Permanente of Colorado - Institute for Health Research, Denver, Colorado.
Sam Hubley, University of Colorado School of Medicine - Family Medicine, Aurora, Colorado.
Edward L. Peterson, Henry Ford Health System - Public Health Sciences
Yong Hu, Henry Ford Health System - Center for Health Policy & Health Services Research, Detroit, Michigan.
L. Keoki Williams, Henry Ford Health System.
Deepak Prabhakar, Henry Ford Health System - Behavioral Health Services, Michigan.
Rebecca C. Rossom, HealthPartners, HealthPartners Institute - Minneapolis, Minnesota
Frances Lynch, Center for Health Research, Kaiser Permanente Northwest, Portland, Oregon.
Christine Y. Lu, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston, Massachusetts
Beth E. Waitzfelder, Kaiser Permanente Hawaii - Center for Health Research, Honolulu, Hawaii
Ashli A. Owen-Smith, Georgia State University - School of Public Health, Atlanta, Georgia
Gregory E. Simon, Kaiser Permanente Washington Health Research Institute, Seattle, Washington
Brian K. Ahmedani, Henry Ford Health System - Center for Health Policy & Health Services Research, Detroit, Michigan
References
- 1.Centers for Disease Control and Prevention (CDC) Injury Prevention & Control: Data & Statistics (WISQARSTM): Fatal Injury Reports. 2016 [02/08/2017]. Available from: https://www.cdc.gov/injury/wisqars/fatal_injury_reports.html.
- 2.Vyrostek SB, Annest JL, Ryan GW. Surveillance for fatal and nonfatal injuries--United States, 2001. MMWR Surveill Summ. 2004;53(7):1–57. [PubMed] [Google Scholar]
- 3.Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: Final Data for 2014. Centers for Disease Control and Prevention, National Vital Statistics Reports; 2014. [PubMed] [Google Scholar]
- 4.Ahmedani BK, Simon GE, Stewart C, Beck A, Waitzfelder BE, Rossom R, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870–7. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention NCfHS. Suicide and Self-Inflicted Injury Atlanta, GA. 2014 [02/08/2017]. Available from: https://www.cdc.gov/nchs/fastats/suicide.htm.
- 6.Stone DM, Crosby AE. Suicide Prevention. Am J Lifestyle Med. 2014;8(6):404–20. doi: 10.1177/1559827614551130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suicide Prevention Resource Center (SPRC) CALM: Counseling on Access to Lethal Means Waltham, MA. 2017 [03/01/2017]. Available from: http://www.sprc.org/resources-programs/calm-counseling-access-lethal-means.
- 8.The Joint Commission. Sentinel Event Alert: Detecting and treating suicide ideation in all settings. 2016 Feb 24; [02/08/2017] Available from: https://www.jointcommission.org/assets/1/18/SEA_56_Suicide.pdf. [PubMed]
- 9.Bryan CJ, Stone SL, Rudd MD. A practical, evidence-based approach for means-restriction counseling with suicidal patients. Prof Psychol Res Pr. 2011;42(5):339. [Google Scholar]
- 10.McDowell AK, Lineberry TW, Bostwick JM. Practical suicide-risk management for the busy primary care physician. Mayo Clin Proc. 2011;86(8):792–800. doi: 10.4065/mcp.2011.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kruesi MJ, Grossman J, Pennington JM, Woodward PJ, Duda D, Hirsch JG. Suicide and violence prevention: parent education in the emergency department. J Am Acad Child Adolesc Psychiatry. 1999;38(3):250–5. doi: 10.1097/00004583-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 12.McManus BL, Kruesi MJ, Dontes AE, Defazio CR, Piotrowski JT, Woodward PJ. Child and adolescent suicide attempts: an opportunity for emergency departments to provide injury prevention education. Am J Emerg Med. 1997;15(4):357–60. doi: 10.1016/s0735-6757(97)90124-8. [DOI] [PubMed] [Google Scholar]
- 13.Brent DA, Bridge J. Firearms availability and suicide evidence, interventions, and future directions. Am Behav Sci. 2003;46(9):1192–210. [Google Scholar]
- 14.Sullivan G. Assessment of firearm access. Behavioral Emergencies Update: Section on clinical emergencies and crises. 2004 [cited (Spring/Summer)]. Available from: http://www.apa.org/divisions/div12/sections/section7/news/sp04/access.html.
- 15.Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide Attempt as a Risk Factor for Completed Suicide: Even More Lethal Than We Knew. Am J Psychiatry. 2016;173(11):1094–100. doi: 10.1176/appi.ajp.2016.15070854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beghi M, Rosenbaum JF, Cerri C, Cornaggia CM. Risk factors for fatal and nonfatal repetition of suicide attempts: a literature review. Neuropsychiatr Dis Treat. 2013;9:1725–36. doi: 10.2147/NDT.S40213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Betz ME, Sullivan AF, Manton AP, Espinola JA, Miller I, Camargo CA, Jr, et al. Knowledge, attitudes, and practices of emergency department providers in the care of suicidal patients. Depress Anxiety. 2013;30(10):1005–12. doi: 10.1002/da.22071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewiecki EM, Miller SA. Suicide, guns, and public policy. Am J Public Health. 2013;103(1):27–31. doi: 10.2105/AJPH.2012.300964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baca-Garcia E, Diaz-Sastre C, Basurte E, Prieto R, Ceverino A, Saiz-Ruiz J, et al. A prospective study of the paradoxical relationship between impulsivity and lethality of suicide attempts. J Clin Psychiatry. 2001;62(7):560–4. doi: 10.4088/jcp.v62n07a11. [DOI] [PubMed] [Google Scholar]
- 20.Simon OR, Swann AC, Powell KE, Potter LB, Kresnow MJ, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(1 Suppl):49–59. doi: 10.1521/suli.32.1.5.49.24212. [DOI] [PubMed] [Google Scholar]
- 21.Ilgen MA, Bohnert AS, Ignacio RV, McCarthy JF, Valenstein MM, Kim HM, et al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67(11):1152–8. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- 22.Basham C, Denneson LM, Millet L, Shen X, Duckart J, Dobscha SK. Characteristics and VA health care utilization of U.S. Veterans who completed suicide in Oregon between 2000 and 2005. Suicide Life Threat Behav. 2011;41(3):287–96. doi: 10.1111/j.1943-278X.2011.00028.x. [DOI] [PubMed] [Google Scholar]
- 23.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmedani BK, Peterson EL, Hu Y, Rossom RC, Lynch F, Lu CY, Waitzfelder BE, Owen-Smith AA, Hubley S, Prabhakar D, Williams LK. Major Physical Health Conditions and Risk of Suicide. American Journal of Preventive Medicine. 2017 Jun 12; doi: 10.1016/j.amepre.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossom RC, Simon GE, Beck A, Ahmedani BK, Steinfeld B, Trangle M, et al. Facilitating Action for Suicide Prevention by Learning Health Care Systems. Psychiatr Serv. 2016;67(8):830–2. doi: 10.1176/appi.ps.201600068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mental Health Research Network. Oakland, CA: Kaiser Permanente Northern California; 2015. Available from: http://hcsrn.org/mhrn/en/ [Google Scholar]
- 27.Wagner EH, Greene SM, Hart G, Field TS, Fletcher S, Geiger AM, et al. Building a research consortium of large health systems: the Cancer Research Network. J Natl Cancer Inst Monogr. 2005;(35):3–11. doi: 10.1093/jncimonographs/lgi032. [DOI] [PubMed] [Google Scholar]
- 28.Hornbrook MC, Hart G, Ellis JL, Bachman DJ, Ansell G, Greene SM, et al. Building a virtual cancer research organization. J Natl Cancer Inst Monogr. 2005;(35):12–25. doi: 10.1093/jncimonographs/lgi033. [DOI] [PubMed] [Google Scholar]
- 29.Go AS, Magid DJ, Wells B, Sung SH, Cassidy-Bushrow AE, Greenlee RT, et al. The Cardiovascular Research Network: a new paradigm for cardiovascular quality and outcomes research. Circ Cardiovasc Qual Outcomes. 2008;1(2):138–47. doi: 10.1161/CIRCOUTCOMES.108.801654. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization (WHO) International Classification of Diseases, Tenth Revision. 2012 [02/08/2017]. Available from: http://www.who.int/classifications/icd/en/
- 31.Centers for Disease Control and Prevention NCfHS. International Classification of Diseases,Ninth Revision, Clinical Modification (ICD-9-CM) Atlanta, GA. 2010 [02/19/2017]. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD9-CM/2010.
- 32.Shea SC. Training Institute for Sucide Assessment & Clinical Interviewing (TISA) 2017 [01/19/2017]. Available from: http://www.suicideassessment.com/home.html.
- 33.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 2000;90(12):1885–91. doi: 10.2105/ajph.90.12.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 35.Teasdale TW, Engberg AW. Suicide after traumatic brain injury: a population study. J Neurol Neurosurg Psychiatry. 2001;71(4):436–40. doi: 10.1136/jnnp.71.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mula M, Sander JW. Suicidal ideation in epilepsy and levetiracetam therapy. Epilepsy Behav. 2007;11(1):130–2. doi: 10.1016/j.yebeh.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 37.Ferrer P, Ballarin E, Sabate M, Vidal X, Rottenkolber M, Amelio J, et al. Antiepileptic drugs and suicide: a systematic review of adverse effects. Neuroepidemiology. 2014;42(2):107–20. doi: 10.1159/000356807. [DOI] [PubMed] [Google Scholar]
- 38.Keiser O, Spoerri A, Brinkhof MW, Hasse B, Gayet-Ageron A, Tissot F, et al. Suicide in HIV-infected individuals and the general population in Switzerland, 1988–2008. Am J Psychiatry. 2010;167(2):143–50. doi: 10.1176/appi.ajp.2009.09050651. [DOI] [PubMed] [Google Scholar]
- 39.Colman I, Kingsbury M, Sareen J, Bolton J, van Walraven C. Migraine headache and risk of self-harm and suicide: A population-based study in Ontario, Canada. Headache. 2016;56(1):132–40. doi: 10.1111/head.12710. [DOI] [PubMed] [Google Scholar]
- 40.Friedman LE, Gelaye B, Bain PA, Williams MA. A Systematic Review and Meta-analysis of Migraine and Suicidal Ideation. Clin J Pain. 2016 Sep 17; doi: 10.1097/AJP.0000000000000440. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Center for Behavioral Health Statistics and Quality SAaMHSAS. Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: 2015 Contract No.: HHS Publication No. SMA 15-4927, NSDUH Series H-50. [Google Scholar]
- 42.Centers for Disease Control and Prevention (CDC) Vital signs: overdoses of prescription opioid pain relievers and other drugs among women--United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(26):537–42. [PMC free article] [PubMed] [Google Scholar]
- 43.Munce SE, Stewart DE. Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics. 2007;48(5):394–9. doi: 10.1176/appi.psy.48.5.394. [DOI] [PubMed] [Google Scholar]
- 44.Edlund MJ, Martin BC, Devries A, Fan MY, Braden JB, Sullivan MD. Trends in use of opioids for chronic noncancer pain among individuals with mental health and substance use disorders: the TROUP study. Clin J Pain. 2010;26(1):1–8. doi: 10.1097/AJP.0b013e3181b99f35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Outcalt SD, Kroenke K, Krebs EE, Chumbler NR, Wu J, Yu Z, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38(3):535–43. doi: 10.1007/s10865-015-9628-3. [DOI] [PubMed] [Google Scholar]
- 46.Bruffaerts R, Demyttenaere K, Kessler RC, Tachimori H, Bunting B, Hu C, et al. The associations between preexisting mental disorders and subsequent onset of chronic headaches: a worldwide epidemiologic perspective. J Pain. 2015;16(1):42–52. doi: 10.1016/j.jpain.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 47.Hepburn L, Miller M, Azrael D, Hemenway D. The US gun stock: results from the 2004 national firearms survey. Inj Prev. 2007;13(1):15–9. doi: 10.1136/ip.2006.013607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.United States Court of Appeals for the Eleventh Circuit, D.C. Docket No. 1:11-cv-22026-MGC Sess. (2017).