Abstract
Background
The study aims were to examine daily associations between marijuana and alcohol use and the extent to which the association differs as a function of cannabis use disorder (CUD) and/or alcohol use disorder (AUD) diagnosis.
Methods
Timeline Followback interview data collected in a study of veterans (N=127) recruited from a Veterans Affairs hospital who reported at least one day of co-use of marijuana and alcohol in the past 180 days (22,860 observations). Participants reported 40% marijuana use days, 28% drinking days, with 37% meeting DSM-5 criteria for CUD, 40% for AUD, and 15% for both. Use of marijuana on a given day was used to predict a three-level gender-adjusted drinking variable (heavy: ≥ 5 (men)/4 (women) drinks; moderate: 1 – 4/3 drinks; or None: 0 drinks). A categorical four-level variable (no diagnosis, AUD, CUD, or both) was tested as a moderator of the marijuana-alcohol relationship.
Results
Multilevel modeling analyses demonstrated that participants were more likely to drink heavily compared to moderately (OR=2.34) and moderately compared to not drinking (OR =1.61) on marijuana use days relative to non-use days. On marijuana use days, those with AUD and those with AUD+CUD were more likely to drink heavily (OR=1.91; OR=2.51, respectively) but those with CUD were less likely to drink heavily (OR=.32) compared to moderately; non-significant differences between any vs. moderate drinking in interaction models.
Conclusions
Heavy drinking occurs on days when marijuana is also used. This association is particularly evident in individuals diagnosed with both alcohol and cannabis use disorders and alcohol use disorders alone but not in those with only cannabis use disorders. Findings suggest that alcohol interventions may need to specifically address marijuana use as a risk factor for heavy drinking and AUD.
Keywords: Alcohol, marijuana, alcohol use disorder, cannabis use disorder, comorbidity
1. Introduction
Marijuana, the most used illicit drug in the U.S. and the world, is frequently used in association with alcohol. Marijuana use is prospectively associated with both heavy drinking and with the development and maintenance of alcohol use disorders (AUDs) (Blanco et al., 2016; Weinberger, Platt, & Goodwin, 2016) as well as with the deleterious AUD treatment outcomes (Aharonovich et al., 2005; Mojarrad, Samet, Cheng, Winter, & Saitz, 2014; Subbaraman, 2016). Co-use of marijuana and alcohol is associated with heavy episodic drinking and alcohol use disorders (Brière, Fallu, Descheneaux, & Janosz, 2011; Midanik, Tam, & Weisner, 2007; Subbaraman & Kerr, 2015). Among marijuana users with marijuana use disorder (CUD), there is increased likelihood for development of a comorbid AUD (Agosti, Nunes, & Levin, 2002; Regier et al., 2014; Stinson, Ruan, Pickering, & Grant, 2006), with nationally representative data indicating that 68% of individuals with current CUD and over 86% of those with a history of CUD meeting criteria for an AUD (Agrawal et al., 2007; SAMHSA, 2016). Marijuana dependence doubles the risk for long-term persistent alcohol problems (Copeland et al., 2012), and marijuana-dependent alcohol users are three times more likely to develop alcohol dependence than non-marijuana-involved drinkers (Lopez-Quintero et al., 2010). Co-use (concurrent or simultaneous) of marijuana and heavy alcohol use are linked to a number of behavioral problems (Harrington et al., 2012) with exceptionally heightened risk for impaired driving (Biecheler, Peytavin, Group, Facy, & Martineau, 2008; Li et al., 2012), psychiatric comorbidity (Midanik et al., 2007), and poor clinical treatment outcomes (Staiger, Richardson, Long, Carr, & Marlatt, 2012). Importantly, the risk associated with the use of marijuana in combination with alcohol is greater than that from either drug alone (Volkow, Baler, Compton, & Weiss, 2014). Thus, increased attention has been called to the importance of examining inter-relations among alcohol and marijuana use patterns and the impact of the use of one substance on risk of excessive use of the other (Staiger et al., 2012; Yurasek, Aston, & Metrik, 2017).
The majority of the epidemiological studies using individual-level outcomes indicate that marijuana use increases or complements alcohol consumption (reviewed in Subbaraman, 2016). Similarly, studies of economic policies that reduce access to alcohol or increase the price of alcohol demonstrate complementary reductions in both alcohol and marijuana use (Williams, Pacula, Chaloupka, &Wechsler, 2004; Farrelly, Bray, Zarkin, Wendling, & Pacula, 1999; Pacula, 1998). However, longitudinal general population studies that mostly used state-level data on marijuana policy (e.g., marijuana decriminalization) suggest marijuana and alcohol can be substitutes (Subbaraman, 2016). Research with individuals using marijuana for medicinal purposes also indicates that alcohol use is lower or less likely with concurrent marijuana use (Lin, Ilgen, Jannausch, & Bohnert, 2016; Nunberg, Kilmer, Pacula, & Burgdorf, 2013). These findings suggest that individuals who use marijuana for medicinal (but not recreational) purposes may use it as a harm-reduction strategy to substitute for alcohol (Lin et al., 2016; Loflin et al., 2017; Metrik et al., in press.). Preliminary evidence of alcohol substitution was also noted in a clinical study where controlled abstinence from marijuana was linked with increased alcohol craving and consumption among individuals with AUD (Peters & Hughes, 2010) and also in an experimental study that demonstrated decreased alcohol consumption over time when smoked marijuana was available during an operant task (Mello, Mendelson, Kuehnle, & Sellers, 1978). Collectively, this research indicates that marijuana use is strongly linked with alcohol use, although whether marijuana serves as a complement to or substitute for alcohol use remains unclear.
These mixed findings on co-occurrence between alcohol and marijuana use behaviors may reflect methodological limitations of correlational research which precludes causal inference. Similarly, epidemiological and laboratory studies are not designed to determine whether marijuana and alcohol use are linked at the event-level within individuals in a natural setting. The few experimental studies have primarily focused on pharmacokinetic interactions (Ballard & De Wit, 2010; Hartman et al., 2015; Lukas et al., 1992; Lukas & Orozco, 2001) or on performance impairments from combined use of marijuana and alcohol (Chait and Perry, 1994; Heishman et al., 1997; Ramaekers et al., 2011), and thus offer limited information on marijuana’s influence on alcohol consumption. Although several studies have asked respondents to recall their most recent marijuana-alcohol use event (Barrett, Darredeau, & Pihl, 2006; Jenkinson, Jolley, & Dietze, 2014; Mcketin, Chalmers, Sunderland, & Bright, 2014), they cannot distinguish different use events within the same person. Therefore, it is critical to use nuanced methods that examine co-use of marijuana and alcohol, such as event or daily level. To our knowledge, there have been only a few event-level studies on the co-occurrence of marijuana and alcohol use. One recent study used ecological momentary assessment methods to characterize the context of adolescent simultaneous marijuana and alcohol use, but did not examine event-level associations between the two behaviors (Lipperman-Kreda, Gruenewald, Grube, & Bersamin, 2017). Another study examining daily marijuana and alcohol use found that marijuana intoxication was greater on days when participants used any alcohol or had five or more alcoholic drinks on one occasion (Hughes et al., 2014). However, whether marijuana use predicted heavy drinking was not examined. Furthermore, neither study examined whether meeting criteria for alcohol or cannabis use disorder moderated the concurrent marijuana and alcohol use. A recent online daily diary study showed evidence for complementary alcohol and marijuana use at both the within- and between-person levels (O’Hara, Armeli, & Tennen, 2016). However, individuals with coping-oriented patterns of substance use showed evidence of substitution by increasing levels of drinking while decreasing marijuana use.
Heterogeneous samples may have contributed to the mixed findings in research examining marijuana-alcohol associations. For example, marijuana use may be associated with worse drinking outcomes among heavy drinkers, especially those with AUD. For these individuals, learned associations of conjoint use (e.g., urge to drink due to anticipation of increased positive subjective effects or anticipation of anxiety reduction) may be particularly salient. Marijuana also impairs executive control functioning (Desrosiers, Ramaekers, Chauchard, Gorelick, & Huestis, 2015; Metrik et al., 2012; Ramaekers et al., 2006), which may already be reduced among chronic heavy drinkers (Ramaekers et al., 2016; Ramaekers et al., 2011). Thus, in individuals with AUD, marijuana use may increase alcohol craving and may result in heavy drinking. Likewise, given that individuals with CUD are known to be at greater risk for problematic drinking (Copeland et al., 2012; Lopez-Quintero et al., 2010), and CUD and AUD are highly comorbid (Regier et al., 2014; Stinson et al., 2006), alcohol involvement may be even greater in individuals with the dual diagnoses of CUD and AUD.
The current study extends the growing literature on the association of marijuana and alcohol use and use disorders by using event-level data to examine daily associations between marijuana and alcohol use in a clinical population with high base rates of use of these substances. The sample was recruited from the Veterans Health Administration (VHA) facility to capitalize on the disproportionately high rates of substance use disorders in veterans relative to the general population (Seal et al., 2011). Veterans are at increased risk for substance use disorders because of the significantly elevated rates of mental health disorders such as posttraumatic stress disorder and major depressive disorder, which are strongly associated with using alcohol and marijuana specifically to cope with aversive psychological and mood states as well as with sleep disturbance (Metrik et al., 2016). Returning veterans experience high rates of suicide and impaired psychosocial functioning post-deployment, which further exacerbate the severity of substance use disorders in this vulnerable population (Spelman, Hunt, Seal, & Burgo-Black, 2012). Participants were selected based on co-use of marijuana and alcohol with a full range of marijuana and alcohol involvement (ranging in frequency from occasional to daily use and from non-problematic to pathological levels of use). As there may be different associations for any use versus level of alcohol use, we examined any alcohol use as well as heavy and moderate levels of drinking. There are two main hypotheses of this study. First, we hypothesized that marijuana use (versus nonuse) on a given day will be associated with greater alcohol consumption (i.e., greater likelihood of heavy drinking, ≥5 (men)/4 (women) drinks, versus moderate drinking (1–4/3 drinks); and moderate drinking versus none) on that day. Second, we examined the potential moderating effects of AUD and CUD diagnosis, as ascertained by the Structured Clinical Interview for DSM (First, Spitzer, Gibbon, 2002), on the marijuana-alcohol relationship. Specifically, we expected that marijuana use on a given day will be associated with heavy alcohol use that day specifically among individuals with a diagnosis of AUD or CUD but not among individuals without these diagnoses. Furthermore, we expected that a dual diagnosis of CUD and AUD would amplify the association between marijuana and alcohol use relative to a single diagnosis of AUD or CUD.
2. Methods
2.1 Sample and Procedure
Data were drawn from a larger prospective study examining marijuana use and affective disorders in returning OEF/OIF/OND veterans who were deployed post 9/11/2001 and who used marijuana at least once in his/her lifetime. Participants were recruited from a VHA facility in the Northeast US and by utilizing the VHA OEF/OIF/OND Roster, an accruing database of combat veterans who have returned from military service in Iraq and Afghanistan (see Metrik et al., 2016 for details of recruitment procedures). All participants were residing in a state with medical marijuana laws (i.e., RI, MA, and CT). Veterans were screened for eligibility by telephone and were invited for a baseline visit, at which time they signed informed consent and completed a battery of interview and self-report assessments. Participants were not required to utilize any of the VHA services in order to participate in the study and, importantly, were told that all information collected as part of this study would be kept confidential, would have no connection to their medical record, and would not affect services they receive at the VHA. The study was approved by the university and local VHA Institutional Review Boards. Participants were compensated $50 upon completion of the study session. Sample demographics are presented in Table 1. Notably, the vast majority of the sample (94%) was comprised of men.
Table 1.
Sample Demographics and Substance Use Characteristics
| Variable | n | % |
|---|---|---|
| Sex (Male) | 119 | 94 |
| Race | ||
| White | 99 | 78 |
| Black/African American | 5 | 4 |
| Asian | 3 | 2 |
| Native Hawaiian/Pacific Islander | 0 | 0 |
| Multiracial/Other | 20 | 16 |
| Ethnicity | ||
| Hispanic/Latino(a) | 91 | 72 |
| Marital Status | ||
| Single/Never Married | 53 | 42 |
| Married/Living with Partner | 43 | 34 |
| Divorced/Separated | 31 | 24 |
| Employment Status | ||
| Employed | 93 | 73 |
| Unemployed | 35 | 28 |
| Student | 36 | 28 |
| Military service | 14 | 11 |
| DSM-5 Criteria | ||
| Cannabis Use Disorder, current | 47 | 37 |
| Cannabis Use Disorder, lifetime | 75 | 59 |
| Alcohol Use Disorder, current | 51 | 40 |
| Alcohol Use Disorder, lifetime | 111 | 87 |
| Comorbid Alcohol and Cannabis Use Disorder, current | 19 | 15 |
| Cannabis use history variables | ||
| Cannabis ounces used per week | ||
| Less than 1/16th | 57 | 45 |
| 1/16th | 7 | 6 |
| 1/8th | 18 | 14 |
| More than 1/8th | 45 | 35 |
| Combined use of alcohol and cannabis | ||
| Never | 18 | 14 |
| Seldom | 63 | 50 |
| Occasionally | 25 | 20 |
| Frequently | 12 | 9 |
| Repeatedly | 9 | 7 |
| M | SD | |
|
|
||
| Age | 29.98 | 7.13 |
| Years of Education | 13.11 | 1.86 |
| Timeline Follow back summary variables: | ||
| Times used marijuana on an average day | 2.61 | 2.95 |
| % cannabis use days | 40.18 | 40.72 |
| % drinking days | 27.62 | 29.16 |
| % heavy drinking days (men: ≥5/women: ≥4) | 15.03 | 23.36 |
| % Moderate drinking days (men: 1–4/women:1–3) | 22.67 | 25.24 |
| No. of drinks per drinking day | 5.31 | 3.65 |
| % same-day cannabis and alcohol use days | 8.98 | 18.04 |
| % tobacco use days* | 80.57 | 31.40 |
| No. of tobacco cigarettes per smoking day* | 10.72 | 7.45 |
(for n = 70 tobacco smokers)
Measures
Demographic Information. Demographic and background information, such as sex, ethnicity, marital status, was collected at baseline and verified through the VHA Computerized Patient Record System (CPRS).
Structured Clinical Interview for DSM Non-Patient Edition (SCID-NP) was used to determine diagnosis of lifetime and past-year DSM-5 CUD and AUD (First, Spitzer, Gibbon, 2002) based on endorsement of 2+ of 11 symptoms.
The Time-Line Follow-Back (TLFB; Dennis et al., 2004; Sobell and Sobell, 1992) covered the 180 days prior to the visit and was used to determine percent of marijuana use days, alcohol use days (measured in standard drinks, defined as 12 oz. of beer, 5 oz. of wine, or 1.5 oz. 80-proof distilled spirits), heavy drinking days (gender-adjusted for 5/4 drinks), other drug (any drug other than marijuana) use days, and tobacco cigarette use days. The TLFB is a calendar-assisted structured interview, which provides a way to cue memory to enhance recall accuracy. The TLFB interview is established as a psychometrically sound retrospective method for assessing alcohol use (Sobell & Sobell, 1992) and marijuana use (Dennis et al., 2004) and has been shown to give highly valid estimates of substance use with high levels of agreement with biological measures (Hjorthøj, Hjorthøj, & Nordentoft, 2012). TLFB has high test-retest reliability and stability over periods of 180-days (Carey, 1997) and up to one year (Sobell & Sobell, 1992).
Data Analysis
Because data were nested within individuals, multilevel modeling (Raudenbush & Bryk, 2002; Snijders, & Bosker, 1999) was used to test first two hypotheses. R (R Core Team, 2013) was used to conduct all analyses; specifically, ordinal (Christensen, 2015) for nominal cumulative link mixed models was used to examine the prediction of daily alcohol quantity by marijuana use. In order to test to the proportional odds assumption, we compared model fit between two models: one in which the 3-level drinking variable was treated as an ordinal outcome and one in which it was treated as a nominal outcome. Model comparisons revealed that the less parsimonious model (with nominal outcomes) fit better, suggesting it as the more appropriate model (χ2 (1) = 60.83, p <.001).
Two dependent variables were calculated from TLFB data: any alcohol use (binary variable: any drinks versus no drinks) and gender-adjusted drinking quantity (no use = 0 drinks, moderate use: 1–4 (men)/3 (women) drinks, and heavy use: ≥5/4 drinks). Models included fixed effects of percent of marijuana use days (between-person), daily marijuana use (binary), age, sex, any cigarette use (binary), and other drug use (binary), day of the week (binary: weekend or weekday), and random effects for individual. Day of the week was included as a fixed effect given previous studies have identified it as a significant predictor of both alcohol and marijuana use (Jackson, Colby, & Sher, 2010; Patrick, Yeomans-Maldonado, & Griffin, 2016). For the model examining moderation by diagnosis, a single diagnostic variable was calculated to categorize individuals into one of four categories: no diagnosis, CUD, AUD, and dual-diagnosis of CUD with AUD. For these analyses, no daily marijuana use and no diagnosis group were designated as reference groups in order to compare hypothesized effects. Dependent variables, other fixed effects, and random effects remained the same as previously described linear mixed models. Analyses excluding female participants (6%) produced the same findings and therefore results for the full sample are presented.
3. Results
1. Descriptive Statistics
The data presented here were subset from the original dataset to include only individuals (N = 127) who used alcohol and marijuana on at least one day in the 180-day TLFB assessment period, resulting in 22,860 daily observations. Table 1 presents sample demographics and substance use descriptive statistics. Across all observations, subjects reported alcohol use on 6,313 days (28%), using marijuana on 9,186 days (40%), using both marijuana and alcohol on 2,052 days (9%), using other drugs on 1,430 days (6%), and smoking cigarettes on 10,152 days (45%). Participants averaged 22.66 moderate drinking days and 15.03 heavy drinking days and 8.98 same-day marijuana and alcohol use days across the 180-day TLFB assessment period.
Table 2 displays sample demographics and substance use descriptives as a function of diagnosis (None, AUD, CUD, and comorbid AUD + CUD).
Table 2.
Demographics and Substance Use Characteristics by Diagnostic Group
| None (n=48) | AUD (n=32) | CUD (n=28) | AUD/CUD(n=19) | |
|---|---|---|---|---|
| Demographics | ||||
| Age (M, SD) | 29.58(4.76) | 30.62(10.16) | 26.68(5.47) | 31.84(8.15) |
| Years Ed (M, SD) | 13.21(1.97) | 13.22(1.45) | 12.96(1.5) | 12.89(2.62) |
| Sex (% Male) | 94 | 97 | 86 | 100 |
| Race (% Caucasian) | 83 | 94 | 82 | 79 |
| TLFB Variables | ||||
| % Drinking days | 18.25(23.28) | 50.82(31.15) | 13.59(21.01) | 32.87(26.03) |
| % cannabis use days | 33.62(41.86) | 11.49(19.59) | 74.6(30.0) | 54.36(37.29) |
| % Co-use days | 6.15(15.05) | 5.21(6.86) | 9.96(20.29) | 21.02(28.04) |
| % Heavy drinking days | 6.15(15.05) | 27.53(29.23) | 5.85(12.49) | 25.38(27.44) |
2. Association between Marijuana and Alcohol Use
Table 3 presents bivariate correlations across individuals and across observations. At the daily level (all TLFB observations across individuals), any marijuana use was associated with any drinking, (r = .10, p <.001) and number of drinks per drinking day (r = .09, p <.001). At the aggregate level (TLFB observations collapsed across individual and day), marijuana use frequency was significantly associated with drinking frequency (r = .24, p<.001).
Table 3.
Individual (Between-subjects) and Event-level (Within-subjects) Correlations
| Measure | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| 1. Alcohol Use | -- | .78*** | .94*** | .10*** | −.01 | .01 |
| 2. DDD | .06 | -- | .88*** | .09*** | .02** | −.02** |
| 3. 3-Level Drinking | .74*** | .31*** | -- | .07*** | .01 | −.01* |
| 4. Marijuana use | .24** | −.01 | −.10 | -- | .05*** | .18*** |
| 5. Drug use | −.09 | .06 | −.04 | .09 | -- | .13*** |
| 6. Cigarettes per day | −.03 | .03 | −.07 | .23** | .19* | -- |
Note. Upper diagonal represents correlations at the daily level (within-subjects) and bottom diagonal represents correlations collapsed across individuals (between-subjects). For correlations across individuals, alcohol, marijuana, drug, and cigarette use were summed for each individuals across 180 TLFB days, DDD = Drinks per Drinking Day. 3-Level Drinking = categorical drinking variable for no drinking, moderate drinking (1–4/3 drinks for men/women), or heavy drinking (≥5/4 drinks for men/women). Marijuana Use = Dichotomous (0/1) any marijuana use, Alcohol Use = Dichotomous (0/1) any alcohol use; Drug Use = Dichotomous (0/1) for any other illicit drug use. For correlations between two binary variables (Alcohol use, any Marijuana use, Drug Use, Cigarette use), spearman rank coefficients were used; for all other correlations, Pearson correlations were calculated.
p < .05;
p < .01,
p < .001.
In order to examine whether marijuana use on any given day predicted extent of alcohol use, we ran the first mixed effects nominal cumulative link model described above, predicting the 3-level drinking variable from any marijuana use, controlling for age, sex, any cigarette use, any drug use, and the day of the week. Analyses (Table 4) revealed that marijuana use on a given day predicted drinking quantity. Specifically, on days where marijuana was used, odds of moderate (1–4/3 drinks) compared to no drinking (Est. = .48, p < .001, OR =1.61) and heavy (≥5/4 drinks) drinking compared to moderate drinking (Est. = .85, p < .001, OR=2.34) were greater.
Table 4.
Nominal Cumulative Link Mixed Effects model
| Estimate | SE | P | Lower CI | OR | Upper CI | |
|---|---|---|---|---|---|---|
| Age | 0.06 | .03 | .03 | 1.06 | 1.07 | 1.08 |
| Sex (ref: male) | −1.21 | .88 | .17 | .18 | .30 | .41 |
| Any Cig | 0.61 | .09 | <.001 | 1.54 | 1.83 | 2.21 |
| Any Drug | 1.38 | .11 | <.001 | 3.16 | 3.96 | 5.08 |
| Weekend | 1.13 | .04 | <.001 | 2.89 | 3.10 | 3.36 |
| % of marijuana use days | −0.02 | .01 | <.001 | .98 | .98 | .98 |
|
| ||||||
| Threshold Coefficients | ||||||
|
| ||||||
| Intercept, Moderate vs. None | 1.24 | 1.29 | - | - | - | - |
| Intercept, Heavy vs. None | 2.69 | 1.29 | - | - | - | - |
| Any marijuana use, Moderate vs. None | 0.48 | .07 | <.001 | 1.40 | 1.61 | 1.86 |
| Any marijuana use, Heavy vs. Moderate | 0.85 | .07 | <.001 | 1.99 | 2.34 | 2.75 |
|
| ||||||
| log-likelihood: −12061.77 | AIC: 24145.54 | |||||
Note. Threshold coefficients represents contrasts at each level of the nominal drinking outcome, 0 = No drinking, 1 = Moderate drinking (1–4/3 drinks for men/women), 2 = Heavy drinking (≥5/4 drinks for men/women). Lower and Upper CI represent bootstrapped 95% Confidence Intervals; bolded effects are statistically significant. Predictors in top panel are held constant across thresholds. All effects are within-person at the daily level, with the exception of Age, Sex, and % marijuana use days, which were between person.
3. Association between Cannabis and Alcohol Use by Alcohol and Cannabis Use Disorder
We conducted an additional nominal cumulative link mixed model in order to examine whether diagnosis (None, AUD, CUD, and comorbid AUD + CUD) moderated the relationship between marijuana use and drinking quantity. As described above, the model included the main effects of marijuana use on any given day and the diagnostic variable, as well as the interaction between marijuana use and diagnosis (Table 5), with diagnosis treated as three dummy codes (no diagnosis as the reference group). As in the previous model, analyses revealed a main effect of any marijuana use on moderate drinking over no drinking (Est. = .36, p < .01, OR = 1.43) and on heavy drinking over moderate drinking (Est. = .36, p =.02, OR= 1.43).
Table 5.
Nominal Cumulative Link Mixed Effects mod
| Estimate | se | P | Lower CI | OR | Upper CI | |
|---|---|---|---|---|---|---|
| Age | 0.05 | .03 | .09 | 1.04 | 1.05 | 1.05 |
| Sex (ref: male) | −0.87 | .80 | .28 | .26 | .42 | .59 |
| Any tobacco cigarette | 0.61 | .09 | <.001 | 1.53 | 1.83 | 2.22 |
| Any drug | 1.36 | .11 | <.001 | 3.16 | 3.90 | 5.04 |
| Weekend | 1.14 | .04 | <.001 | 2.92 | 3.12 | 3.41 |
| % of marijuana use days | −0.01 | .01 | .08 | .99 | .99 | .99 |
|
| ||||||
| Threshold Coefficients | ||||||
|
| ||||||
| Intercept, Moderate vs. None | −2.08 | 1.18 | - | - | - | - |
| Intercept, Heavy vs. None | −3.58 | 1.18 | - | - | - | - |
|
| ||||||
| Outcome: None vs. Moderate Drinking | ||||||
|
| ||||||
| Any marijuana use | 0.36 | .13 | .006 | 1.07 | 1.43 | 1.91 |
| AUD | 2.32 | .49 | <.001 | 9.26 | 10.20 | 12.39 |
| CUD | −0.42 | .58 | .47 | .44 | .66 | .99 |
| AUD/CUD | 1.15 | .59 | .05 | 2.51 | 3.15 | 4.18 |
| Any marijuana use × AUD | 0.06 | .18 | .75 | .71 | 1.06 | 1.59 |
| Any marijuana use × CUD | 0.12 | .21 | .57 | .71 | 1.13 | 1.80 |
| Any marijuana use × AUD/CUD | 0.29 | .18 | .12 | .95 | 1.33 | 1.95 |
|
| ||||||
| Outcome: Moderate vs. Heavy Drinking | ||||||
|
| ||||||
| Any marijuana use | 0.36 | .15 | .02 | 1.00 | 1.43 | 1.99 |
| AUD | 2.14 | .50 | <.001 | 7.48 | 8.51 | 10.92 |
| CUD | 0.46 | .58 | .43 | 1.06 | 1.58 | 2.32 |
| AUD/CUD | 1.72 | .60 | .004 | 4.37 | 5.59 | 7.59 |
| Any marijuana use × AUD | 0.65 | .20 | .001 | 1.23 | 1.91 | 3.12 |
| Any marijuana use × CUD | −1.15 | .24 | <.001 | .19 | .32 | .55 |
| Any marijuana use × AUD/CUD | 0.92 | .21 | <.001 | 1.73 | 2.51 | 3.89 |
|
| ||||||
| log-likelihood: −11794.66 | AIC: 23635.31 | |||||
Note. Threshold coefficients represents contrasts at each level of the nominal drinking outcome, 0 = No drinking, 1 = Moderate drinking (1–4/3 drinks for men/women), 2 = Heavy drinking (≥ 5/4 drinks for men/women). Lower and Upper CI represent bootstrapped 95% Confidence Intervals; bolded effects are statistically significant. Predictors in top panel are held constant across thresholds. All effects are within-person at the daily level, with the exception of Age, Sex, AUD/CUD, and % marijuana use days, which were between person.
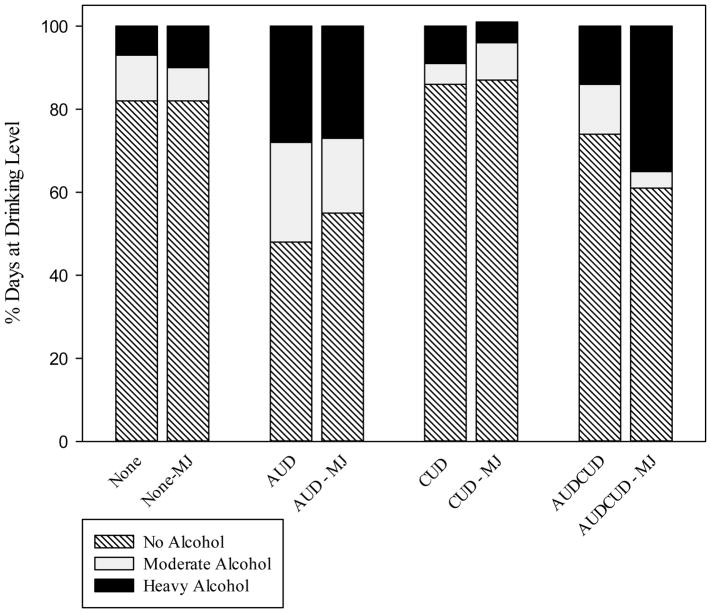
A main effect of AUD was also observed on moderate drinking over no drinking (Est. = 2.32, p < .001, OR=10.20), as well as heavy drinking over moderate drinking (Est. = 2.14, p < .001, OR=8.51), compared to those with no diagnosis. A main effect of the combined diagnosis group was also observed on heavy drinking over moderate drinking (Est. = 1.72, p < .01, OR=5.59). No such main effects were observed for CUD. Importantly, there was a significant interaction observed between diagnostic group and marijuana use. Specifically, marijuana use predicted heavy drinking compared to moderate drinking (Est. = .65, p = .001, OR=1.91) in those with AUD compared to those with no diagnosis. However, among those with only CUD, marijuana use predicted significantly less heavy drinking compared to moderate drinking (Est. = −1.15, p < .001, OR=.32). Finally, marijuana use also predicted more heavy drinking compared to moderate drinking (Est. = .92, p < .001, OR=2.51) in those with combined AUD and CUD compared to those with no diagnosis. No significant interaction effects were observed for the comparison between moderate use and no use. Figure 1 presents percent of days at each drinking level (None, moderate, and heavy) on marijuana use days versus non-marijuana use days grouped by diagnosis (None, AUD, CUD, and comorbid AUD + CUD). Overall, results suggested that, relative to those without a diagnosis, among individuals with AUD (alone or with a comorbid CUD), marijuana use at the daily level was associated with higher rates of heavy alcohol use, but not necessarily moderate use.
Figure 1.
Vertical Axis represents percent of days at each drinking level (None = 0 drinks, Moderate = 1–4 drinks for men (1–3 drinks for women); Heavy = ≥5 drinks for men (≥4 drinks for women)), for each group on the horizontal axis. None = No diagnosis and non-marijuana use days, None-MJ = No Diagnosis on marijuana use days; AUD = AUD diagnosis only on non-marijuana use days; AUD-MJ = AUD diagnosis on marijuana use days; CUD = CUD diagnosis on non-marijuana use days; CUD-MJ = CUD diagnosis on marijuana use days; AUDCUD = AUD+CUD diagnosis on non-marijuana use days; AUDCUD-MJ = AUD+CUD diagnosis on marijuana use days.
Interaction of Diagnostic Group and Marijuana use on Alcohol Use
4. Discussion
The current study aimed to extend the literature on marijuana and alcohol co-use by examining the role of marijuana use in alcohol consumption among individuals with and without alcohol and cannabis use disorders. The study’s aims were to use event-level data to examine: (1) the association of marijuana use on any given day with level of alcohol use (any, moderate, heavy drinking) on that day; and (2) the moderating effects of AUD and CUD diagnoses on the association between marijuana and levels of alcohol use on a given day. Results indicated that on any given day when marijuana was used relative to non-use days, participants were significantly more likely to drink alcohol than they were to not drink. Importantly, on days when marijuana was used, heavy drinking (≥5/4 drinks for men/women) was more likely than drinking at moderate levels (1–4/3 drinks), which was in turn more likely than not drinking at all. Among individuals meeting criteria for AUD with or without CUD, marijuana use on any given day was predictive of heavy drinking levels (relative to moderate or no drinking). In contrast, among individuals with only CUD, marijuana use on any given day was associated with reduced likelihood of drinking heavily relative to drinking moderately that day.
This is one of the first studies to examine event-level patterns of marijuana and alcohol co-use, and current findings support results from prospective investigations in clinical samples. In a number of studies of individuals engaged in substance use treatment, those who used marijuana at study entry (Mojarrad et al., 2014), during AUD treatment (Subbaraman, Metrik, Patterson, & Swift, 2017), or post-discharge from psychiatric inpatient treatment (Aharonovich et al., 2005) were observed to have reduced odds of successfully achieving abstinence from alcohol at the end of treatment and one year post-treatment. Our findings are also consistent with those from general population surveys demonstrating prospective associations between marijuana use and a twofold increase in the likelihood of receiving an AUD diagnosis (Blanco et al., 2016) as well as in maintenance of AUD (Weinberger et al., 2016). To date, no prior study has collected daily marijuana and alcohol use data to specifically examine the impact of marijuana use on the extent of alcohol involvement on a given day. Taken together, our event-level findings and those from prospective studies generally support the complementary role of marijuana in drinking behavior, particularly among those who use alcohol at pathological levels.
The finding that marijuana use was associated with increased alcohol consumption among individuals with AUD may be explained by reduced inhibitory control from using marijuana (Metrik et al., 2012; Ramaekers et al., 2006). This potential for impaired control over drinking may in turn contribute to more alcohol related problems, as decline in executive functioning has been implicated in increased ad libitum alcohol consumption (Jones et al., 2013). Alternatively, because individuals with AUD drink primary for negative reinforcement (Pacher, Ndor, Tkai, & Kunos, 2006), marijuana may be uniquely associated with heavy alcohol use among those who rely on alcohol to cope with stress and other negative affective states in the absence of more effective coping skills (as in the current sample of OIF/OEF/OND veterans). On the other hand, for some individuals with AUD, marijuana use and alcohol consumption may be commonly paired and marijuana may be used purposefully in order to enhance alcohol’s pleasurable effects (Lukas et al., 1992; Lukas & Orozco, 2001). Therefore, in those with AUD, marijuana-related cues may trigger urges to drink as a learned or as a pharmacologic response to marijuana use to a greater degree than in individuals with a sole diagnosis of CUD. Indeed, individuals with CUD alone were not more likely to drink heavily on marijuana use days.
In contrast to the complementary nature of daily marijuana-alcohol associations among those with AUD, individuals with CUD diagnosis only (i.e., no AUD diagnosis) were more likely to drink at moderate drinking levels (1 – 4/3 drinks for men/women) than they were to drink heavily (≥5/4 drinks) when they used marijuana. Although not hypothesized, this finding indicates that demand for alcohol is diminished in the presence of marijuana but only for marijuana users without any evidence of AUD. Our finding signals potential substitution effect, although full substitution pattern (marijuana replacing alcohol) is certainly not evident in these data. Nevertheless, several lines of research have similarly suggested that marijuana use by medical marijuana users, who typically endorse stable daily or almost daily patterns of marijuana use (Lin et al., 2016; Walsh et al., 2013), is associated with past history of alcohol misuse but lower current alcohol problem severity as compared to recreational marijuana users (Lin et al., 2016; Loflin et al., 2017). Whether marijuana use is an effective harm-reduction strategy when used as a substitute for alcohol, at least by those without AUD, deserves further scientific investigation.
These findings have significant clinical implications. First and foremost, individuals with AUD and those with co-morbid AUD and CUD disorders are a group that are high risk and may pose a significant challenge for treatment providers. For individuals with AUD including those with co-occurring CUD, our data underscore the importance of assessment and psychoeducation on the role that marijuana may play in placing an individual at greater risk for increased drinking. This public health message is important to deliver in the context of often conflicting clinical and media messages on marijuana’ therapeutic potential. The present study highlights the need for both treatment and intervention programs to assess both marijuana and alcohol use on a regular and consistent basis. The findings on marijuana’s association with heavy drinking can significantly impact a large proportion of individuals currently in treatment for AUD for whom use of marijuana may serve as a relapse trigger leading to increased desire to use alcohol. For these individuals, recommending marijuana cessation may improve alcohol treatment outcomes. This is particularly important because many patients seeking treatment specifically for AUD may not be aware or motivated to make concurrent changes in their marijuana use.
Limitations
The findings of the study should be considered in the context of some limitations. Despite the TLFB method’s established reliability and validity, this retrospective reporting method may carry recall bias that could have influenced the observed patterns of substance use. This bias may be particularly pronounced in day-level analysis of assessment windows covering longer time intervals such as 60 days (Hoeppner, Stout, Jackson, & Barnett, 2010) and is of concern with respect to the analysis of within-person, day-level association of behaviors with varying base-rate frequency (Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998). Prior research also demonstrates that TLFB reports may underestimate frequency and quantity of alcohol consumed (Searles, Helzer, Rose, & Badger, 2002). However, retrospective assessment on the TLFB has been shown not to be temporally biased; that is reports did not change with increasing time intervals from 30 to 60 to 366 days (Searles et al., 2002) or in comparison of 30 and 180-day time intervals (Carey, 1997). Thus, the observed associations in this study are likely stable although may be conservative estimates of the actual substance use behaviors. Temporal order between use of marijuana and alcohol cannot be established with this type of assessment. A small number of women in our sample limits the generalizability of our findings to both sexes. However, the disproportionally male composition of this sample is representative of the veteran population with men comprising 92% as reported in the national veteran surveys (National Center for Veterans Analysis and Statistics, 2017). This was a study of associations, with future studies benefitting from a more comprehensive analysis of environmental factors such as social contextual cues (Jackson et al., 2010). Finally, the sample, comprised of individuals residing across three Northeastern states, was enrolled in a single site, a VHA facility. Although a veteran population is an ideal one in which to investigate comorbidity between CUD and AUD, future multi-site research should seek to confirm these findings in a broader population.
Conclusions
These findings add important information to the small body of literature on event-level associations between marijuana and alcohol use. Results suggest that heavy drinking is more likely to occur on days when marijuana is used among individuals with AUD as well as those with comorbid AUD and CUD, but not among those with a single diagnosis of CUD. Differentiating heavy from moderate drinking levels, as well as examining synergistic effects of diagnosis, clarified mixed findings from previous studies that failed to consider variability in alcohol and drug diagnoses. Marijuana users who meet criteria for AUD and CUD diagnoses appear to be at greatest risk for problem drinking on days when they also use marijuana. This level of heavy drinking is commonly associated with long-term persistent alcohol problems. An important question for future research to examine is the association between actual quantities of marijuana use and alcohol use as well as “in the moment” associations between marijuana and alcohol use with ecological momentary assessment (EMA) data and with experimental studies on acute effects of marijuana on alcohol consumption. Real-time assessment of day-level associations between marijuana and alcohol use in EMA research would help address current concerns about the potential bias of retrospective reporting. Current findings and our ongoing studies on co-use will inform alcohol treatment efforts for comorbid CUD and AUD and help guide public health policy on this comorbidity that is more disabling, chronic, and costly to society than CUD alone.
Acknowledgments
This work was supported by R01 DA033425 (PIs Metrik, Borsari). The authors have no conflicts of interest to declare (None).
Funding for this research, data analysis, and manuscript preparation was supported by National Institute on Drug Abuse grant R01 DA033425 to Drs. Metrik and Borsari. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors have no conflict of interest to declare. The authors gratefully acknowledge Cassandra Delapaix (Tardif), Rebecca Swagger, Madeline Benz, Hannah Wheeler, Suzanne Sales, and Julie Evon for their contribution to the project.
References
- Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. The American Journal of Drug and Alcohol Abuse. 2002;28(4):643–652. doi: 10.1081/ada-120015873. https://doi.org/10.1081/ADA-120015873. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Lynskey MT, Madden PAF, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: Results from the national epidemiological survey on alcohol and related conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. https://doi.org/10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Liu X, Samet S, Nunes E, Waxman R, Hasin D. Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: A prospective study. American Journal of Psychiatry. 2005;162(8):1507–1514. doi: 10.1176/appi.ajp.162.8.1507. https://doi.org/10.1176/appi.ajp.162.8.1507. [DOI] [PubMed] [Google Scholar]
- Ballard ME, De Wit H. Combined effects of acute, very-low-dose ethanol and delta(9)-tetrahydrocannabinol in healthy human volunteers. Pharmacology, Biochemistry and Behavior. 2010;97:627–631. doi: 10.1016/j.pbb.2010.11.013. https://doi.org/10.1016/j.pbb.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett SP, Darredeau C, Pihl RO. Patterns of simultaneous polysubstance use in drug using university students. Human Psychopharmacology. 2006;21:255–263. doi: 10.1002/hup.766. https://doi.org/10.1002/hup.766. [DOI] [PubMed] [Google Scholar]
- Biecheler MB, Peytavin JF, Facy F, Martineau H Group the S. SAM survey on “drugs and fatal accidents”: search of substances consumed and comparison between drivers involved under the influence of alcohol or cannabis. Traffic Injury Prevention. 2008;9(1):11–21. doi: 10.1080/15389580701737561. [DOI] [PubMed] [Google Scholar]
- Blanco C, Hasin DS, Wall MM, Flórez-Salamanca L, Hoertel N, Wang S, Kerridge BT, Olfson M. Cannabis Use and Risk of Psychiatric Disorders. JAMA Psychiatry. 2016;73(4):388. doi: 10.1001/jamapsychiatry.2015.3229. https://doi.org/10.1001/jamapsychiatry.2015.3229. [DOI] [PubMed] [Google Scholar]
- Brière FN, Fallu JS, Descheneaux A, Janosz M. Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addictive Behaviors. 2011;36:785–788. doi: 10.1016/j.addbeh.2011.02.012. https://doi.org/10.1016/j.addbeh.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Carey KB. Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychology of Addictive Behaviors. 1997;11(1):26. [Google Scholar]
- Carney MA, Tennen H, Affleck G, Del Boca FK, Kranzler HR. “Levels and patterns of alcohol consumption using timeline follow-back, daily diaries and real-time” electronic interviews. Journal of studies on alcohol. 1998;59(4):447–454. doi: 10.15288/jsa.1998.59.447. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. 2016 (HHS Publication No. SMA 16–4984, NSDUH Series H-51). Retrieved from http://www.samhsa.gov/data/
- Chait LD, Perry JL. Acute and residual effects of alcohol and marijuana, alone and in combination, on mood and performance. Psychopharmacology. 1994;115:340–349. doi: 10.1007/BF02245075. [DOI] [PubMed] [Google Scholar]
- Christensen RHB. Ordinal - Regression Models for Ordinal Data. 2015 Retrieved from http://www.cran.r-project.org/package=ordinal/
- Copeland W, Angold A, Shanahan L, Dreyfuss J, Dlamini I, Costello E. Predicting persistent alcohol problems: A prospective analysis from the Great Smoky Mountain Study. Psychological Medicine. 2012;42(9):1925–1935. doi: 10.1017/S0033291711002790. https://doi.org/10.1017/S0033291711002790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Funk R, Harrington Godley S, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(2):125–133. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Desrosiers NA, Ramaekers JG, Chauchard E, Gorelick DA, Huestis MA. Smoked cannabis’ psychomotor and neurocognitive effects in occasional and frequent smokers. Journal of Analytical Toxicology. 2015;39(4):251–261. doi: 10.1093/jat/bkv012. https://doi.org/10.1093/jat/bkv012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly MC, Bray JW, Zarkin GA, Wendling BW, Pacula RL. The effects of prices and policies on the demand for marijuana: Evidence from the National Household Surveys in Drug Abuse (NBER Working Paper No. 6940) Cambridge, MA: National Bureau of Economic Research; 1999. Retrieved from http://www.webcitation.org/6XLlbgezE. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Harrington M, Baird J, Lee C, Nirenberg T, Longabaugh R, Mello MJ, Woolard R. Identifying subtypes of dual alcohol and marijuana users: A methodological approach using cluster analysis. Addictive Behaviors. 2012;37:119–123. doi: 10.1016/j.addbeh.2011.07.016. https://doi.org/10.1016/j.addbeh.2011.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, Brown TL, Milavetz G, Spurgin A, Gorelick DA, Gaffney G, Huestis MA. Controlled cannabis vaporizer administration: Blood and plasma cannabinoids with and without alcohol. Clinical Chemistry. 2015;61(6):850–869. doi: 10.1373/clinchem.2015.238287. https://doi.org/10.1373/clinchem.2015.238287. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Arasteh K, Stitzer ML. Comparative effects of alcohol and marijuana on mood, memory, and performance. Pharmacology Biochemistry and Behavior. 1997;58(1):93–101. doi: 10.1016/s0091-3057(96)00456-x. [DOI] [PubMed] [Google Scholar]
- Hjorthøj CR, Hjorthøj AR, Nordentoft M. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances — Systematic review and meta-analysis. Addictive Behaviors. 2012;37:225–233. doi: 10.1016/j.addbeh.2011.11.025. https://doi.org/10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Stout RL, Jackson KM, Barnett NP. How good is fine-grained Timeline Follow-back data? Comparing 30-day TLFB and repeated 7-day TLFB alcohol consumption reports on the person and daily level. Addictive Behaviors. 2010;35(12):1138–1143. doi: 10.1016/j.addbeh.2010.08.013. https://doi.org/10.1016/j.addbeh.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Fingar JR, Budney AJ, Naud S, Helzer JE, Callas PW. Marijuana use and intoxication among daily users: An intensive longitudinal study. Addictive Behaviors. 2014;39(10):1464–1470. doi: 10.1016/j.addbeh.2014.05.024. https://doi.org/10.1016/j.addbeh.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Colby SM, Sher KJ. Daily patterns of conjoint smoking and drinking in college student smokers. Psychology of Addictive Behaviors. 2010;24(3):424–35. doi: 10.1037/a0019793. https://doi.org/10.1037/a0019793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkinson R, Jolley D, Dietze P. “Weekend on the town”: Discrete sessions of drug use for a sample of young psychostimulant users. Drug and Alcohol Review. 2014;33(4):428–435. doi: 10.1111/dar.12168. https://doi.org/10.1111/dar.12168. [DOI] [PubMed] [Google Scholar]
- Jones A, Christiansen P, Nederkoorn C, Houben K, Field M, Lesch O. Fluctuating disinhibition: implications for the understanding and treatment of alcohol and other substance use disorders. Frontiers in Psychiatry. 2013;4(140):1–10. doi: 10.3389/fpsyt.2013.00140. https://doi.org/10.3389/fpsyt.2013.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li MC, Brady JE, Dimaggio CJ, Lusardi AR, Tzong KY, Li G. Marijuana use and motor vehicle crashes. Epidemiologic Reviews. 2012;34(34):65–72. doi: 10.1093/epirev/mxr017. https://doi.org/10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LA, Ilgen MA, Jannausch M, Bohnert KM. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addictive Behaviors. 2016;61:99–103. doi: 10.1016/j.addbeh.2016.05.015. https://doi.org/10.1016/j.addbeh.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Gruenewald PJ, Grube JW, Bersamin M. Adolescents, alcohol, and marijuana: Context characteristics and problems associated with simultaneous use. Drug and Alcohol Dependence. 2017;179:55–60. doi: 10.1016/j.drugalcdep.2017.06.023. https://doi.org/10.1016/j.drugalcdep.2017.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loflin M, Earleywine M, Bonn-Miller M. Medicinal versus recreational cannabis use: Patterns of cannabis use, alcohol use, and cued-arousal among veterans who screen positive for PTSD. Addictive Behaviors. 2017;68:18–23. doi: 10.1016/j.addbeh.2017.01.008. https://doi.org/10.1016/j.addbeh.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Pérez De Los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug and Alcohol Dependence. 2010;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. https://doi.org/10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukas S, Benedikt R, Mendelson JH, Kouri E, Sholar M, Amass L. Marihuana attenuates the rise in plasma ethanol levels in human subjects. Neuropsychopharmacology. 1992;7(1):77–81. [PubMed] [Google Scholar]
- Lukas SE, Orozco S. Ethanol increases plasma D 9 -tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers. Drug and Alcohol Dependence. 2001;64:143–149. doi: 10.1016/s0376-8716(01)00118-1. [DOI] [PubMed] [Google Scholar]
- Mcketin R, Chalmers J, Sunderland M, Bright DA. Recreational drug use and binge drinking: Stimulant but not cannabis intoxication is associated with excessive alcohol consumption. Drug and Alcohol Review. 2014:1–10. doi: 10.1111/dar.12147. https://doi.org/10.1111/dar.12147. [DOI] [PubMed]
- Mello NK, Mendelson JH, Kuehnle JC, Sellers ML. Human polydrug use: Marihuana and alcohol. The Journal of Pharmacology and Experimental Therapeutics. 1978;207(3):922–935. [PubMed] [Google Scholar]
- Metrik J, Bassett S, Aston ER, Jackson K, Borsari B. Medicinal versus recreational cannabis use among returning veterans. Translational Issues in Psychological Science. doi: 10.1037/tps0000133. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, Borsari B. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychology of Addictive Behaviors. 2016;30(7):743–754. doi: 10.1037/adb0000210. https://doi.org/10.1037/adb0000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Kahler CW, Reynolds B, Mcgeary JE, Monti PM, Haney M, Rohsenow DJ. Balanced placebo design with marijuana: Pharmacological and expectancy effects on impulsivity and risk taking. Psychopharmacology (Berl) 2012;223(4):489–499. doi: 10.1007/s00213-012-2740-y. https://doi.org/10.1007/s00213-012-2740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence. 2007;90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024. https://doi.org/10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojarrad M, Samet JH, Cheng DM, Winter MR, Saitz R. Marijuana use and achievement of abstinence from alcohol and other drugs among people with substance dependence: A prospective cohort study. Drug and Alcohol Dependence. 2014;142:91–97. doi: 10.1016/j.drugalcdep.2014.06.006. https://doi.org/10.1016/j.drugalcdep.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics. Profile of Veterans: 2015. 2017 Retrieved from https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2015.pdf.
- Nunberg H, Kilmer B, Pacula RL, Burgdorf J. An analysis of applicants presenting to a medical marijuana specialty practice in California. Journal of Drug Policy and Analysis. 2013;4(1):1941–2851. doi: 10.2202/1941-2851.1017. https://doi.org/10.2202/1941-2851.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara RE, Armeli S, Tennen H. Alcohol and cannabis use among college students: Substitutes or complements? Addictive Behaviors. 2016;58:1–6. doi: 10.1016/j.addbeh.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher PL, Ndor S, Tkai B, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacological Reviews. 2006;58(3):389–462. doi: 10.1124/pr.58.3.2. https://doi.org/10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula R. Does increasing the beer tax reduce marijuana consumption? Journal of Health Economics. 1998;17(5):557–585. doi: 10.1016/s0167-6296(97)00039-8. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Yeomans-Maldonado G, Griffin J. Daily reports of positive and negative affect and alcohol and marijuana use among college student and nonstudent young adults. Substance Use & Misuse. 2016;51(1):54–61. doi: 10.3109/10826084.2015.1074694. https://doi.org/10.3109/10826084.2015.1074694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters EN, Hughes JR. Daily marijuana users with past alcohol problems increase alcohol consumption during marijuana abstinence. Drug and Alcohol Dependence. 2010;106:111–118. doi: 10.1016/j.drugalcdep.2009.07.027. https://doi.org/10.1016/j.drugalcdep.2009.07.027. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Kauert G, van Ruitenbeek P, Theunissen EL, Schneider E, Moeller MR. High-potency marijuana impairs executive function and inhibitory motor control. Neuropsychopharmacology. 2006;31(10):2296–2303. doi: 10.1038/sj.npp.1301068. https://doi.org/10.1038/sj.npp.01068. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Theunissen EL, De Brouwer M, Toennes SW, Moeller MR, Kauert G. Tolerance and cross-tolerance to neurocognitive effects of THC and alcohol in heavy cannabis users. Psychopharmacology. 2011;214(2):391–401. doi: 10.1007/s00213-010-2042-1. https://doi.org/10.1007/s00213-010-2042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers JG, van Wel JH, Spronk DB, Toennes SW, Kuypers KPC, Theunissen EL, Verkes RJ. Cannabis and tolerance: acute drug impairment as a function of cannabis use history. Scientific Reports. 2016;6:26843. doi: 10.1038/srep26843. https://doi.org/10.1038/srep26843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. JAMA. 2014;264(19):2511–2518. [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. https://doi.org/10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Searles JS, Helzer JE, Rose GL, Badger GJ. Concurrent and retrospective reports of alcohol consumption across 30, 90 and 366 days: interactive voice response compared with the Timeline Follow Back. Journal of Studies on Alcohol. 2002;63(3):352–362. doi: 10.15288/jsa.2002.63.352. [DOI] [PubMed] [Google Scholar]
- Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Sobell L, Sobell M. Timeline Follow-Back: A technique for assessing self-reported alcohol consumption. In: Allen J, Litten RZ, editors. Psychosocial and Biological Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. Journal of General Internal Medicine. 2012;27(9):1200–1209. doi: 10.1007/s11606-012-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staiger PK, Richardson B, Long CM, Carr V, Marlatt GA. Overlooked and underestimated? Problematic alcohol use in clients recovering from drug dependence. Addiction. 2012;108:1188–1193. doi: 10.1111/j.1360-0443.2012.04075.x. https://doi.org/10.1111/j.1360-0443.2012.04075.x. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychological Medicine. 2006;36(10):1447. doi: 10.1017/S0033291706008361. https://doi.org/10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS. Substitution and Complementarity of Alcohol and Cannabis: A Review of the Literature. Substance Use & Misuse. 2016;51(11):1399–1414. doi: 10.3109/10826084.2016.1170145. https://doi.org/10.3109/10826084.2016.1170145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Kerr WC. Simultaneous vs. concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcoholism, Clinical and Experimental Research. 2015;39(5):872–879. doi: 10.1111/acer.12698. https://doi.org/10.1111/acer.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, Swift R. Cannabis use during treatment for alcohol use disorders predicts alcohol treatment outcomes. Addiction. 2017;112(4):685–694. doi: 10.1111/add.13693. https://doi.org/10.1111/add.13693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse Health Effects of Marijuana Use. New England Journal of Medicine. 2014;370(23):2219–2227. doi: 10.1056/NEJMra1402309. https://doi.org/10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh Z, Callaway R, Belle-Isle L, Capler R, Kay R, Lucas P, Holtzman S. Cannabis for therapeutic purposes: Patient characteristics, access, and reasons for use. International Journal of Drug Policy. 2013;24:511–516. doi: 10.1016/j.drugpo.2013.08.010. https://doi.org/10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, Goodwin RD. Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States. Drug and Alcohol Dependence. 2016;161:363–367. doi: 10.1016/j.drugalcdep.2016.01.014. https://doi.org/10.1016/j.drugalcdep.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Liccardo Pacula R, Chaloupka FJ, Wechsler H. Alcohol and marijuana use among college students: economic complements or substitutes? Health Economics. 2004;13(9):825–843. doi: 10.1002/hec.859. [DOI] [PubMed] [Google Scholar]
- Yurasek A, Aston ER, Metrik J. Co-use of alcohol and cannabis: a review. Current Addiction Reports. 2017;4(2):184–193. doi: 10.1007/s40429-017-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]