Abstract
Nanoparticle-based therapeutic, prevention, and detection modalities have the potential to greatly impact how diseases are diagnosed and managed in the clinic. With the wide range of different nanomaterials available to nanomedicine researchers, the rational design of nanocarriers on an application-specific basis has become increasingly commonplace. In this review, we provide a comprehensive overview on an emerging platform: cell membrane coating nanotechnology. As one of the most fundamental units in biology, a cell carries out a wide range of functions, including its remarkable ability to interface and interact with its surrounding environment. Instead of attempting to replicate such functions via synthetic techniques, researchers are now directly leveraging naturally derived cell membranes as a means of bestowing nanoparticles with enhanced biointerfacing capabilities. This top-down technique is facile, highly generalizable, and has the potential to greatly augment the potency and safety of existing nanocarriers. Further, the introduction of a natural membrane substrate onto the surface of a nanoparticle has enabled additional applications beyond those already associated with the field of nanomedicine. Despite the relative youth of the cell membrane coating technique, there exists an impressive body of literature on the topic, which will be covered in detail in this review. Overall, there is still significant room for development, as researchers continue to refine existing workflows while finding new and exciting applications that can take advantage of this emerging technology.
Keywords: biomimetic nanomedicine, drug delivery, medical imaging, immunotherapy, detoxification
Table of content entry

Cell membrane coating is an emerging nanotechnology. By cloaking nanomaterials in a layer of natural cell membrane, which can be derived from a variety of cell types, it is possible to fabricate nanoplatforms with enhanced surface functionality. This can lead to increased nanoparticle performance in complex biological environments, which can benefit applications like drug delivery, imaging, phototherapies, immunotherapies, and detoxification.
1. Introduction
Nanotechnology-based solutions, nanoparticles in particular, have become increasingly prevalent in medical research, as they can offer significant advantages in both efficacy and safety when compared with current therapeutic and diagnostic modalities.[1–5] From a reductionist perspective, the design of a nanoparticle formulation can generally be divided into two segments. The first is incorporation of a payload that carries out an application-specific function, such as the killing of cancer cells or providing imaging contrast. The second, which we focus on in this review, is providing the loaded nanoparticle with an effective means of interacting with its environment, both by decreasing nonspecific interactions while increasing specific targeting. Regardless of how promising an experimental compound or material is in vitro, efficient biointerfacing is a prerequisite for successful translation in vivo.[6] Once administered into the body, a nanoparticle encounters a highly complex environment that is inherently adept at recognizing and eliminating foreign elements. For example, in the bloodstream there are various protein-based and cellular constituents; contact with any of these can quickly compromise performance.[7,8] Uptake by the reticuloendothelial system before a nanoparticle can reach its target is one of the major hurdles that almost all platforms must overcome.[9,10] Along with reducing nonspecific nanoparticle uptake, the addition of specific targeting mechanisms can help to further boost efficacy by promoting preferential accumulation at a site of interest.[11,12] Ultimately, the goal is to engineer nanoparticles with surfaces that enable them to be ignored by everything except for their target, a task that has proven to be exceptionally difficult.
Given the importance of nanoparticle biointerfacing, the purposeful engineering of their surfaces is now understood to be a critical aspect in the overall design process. Traditionally, the gold-standard has been to introduce the synthetic polymer polyethylene glycol (PEG) onto the particle surface.[13,14] PEGylation creates a hydration layer, while also providing steric stabilization. The end result is a stealthy nanoparticle surface that interacts less with its environment, enabling significantly enhanced blood circulation. To add targeting functionality, a wide range ligands, including antibodies, aptamers, peptides, and small molecules, can be further included.[15] While synthetic strategies for prolonging circulation and adding targeting functionality have demonstrated incredible utility for enhancing nanodelivery platforms, there is still significant room for improvement. PEG has proven effective at minimizing nonspecific interactions in complex media, but there are increasing reports of immune responses against the synthetic polymer, and the presence of antibodies against PEG can potentially impact performance over multiple administrations.[16,17] Additionally, bottom-up targeting ligand conjugation strategies become increasingly difficult, especially for large-scale manufacturing, as more surface functionalities are required.
Due to the challenges facing synthetic nanoparticle functionalization strategies, there have recently been considerable efforts dedicated towards bioinspired nanotechnology, where design cues for effective design are taken from nature.[18–21] This can take many forms, such as the mimicry of physical properties, including shape and flexibility,[22] and the direct leveraging of naturally derived materials.[21] Considering the inherently biological nature of nanoparticle interactions in vivo, biomimicry is a rational approach towards effective nanoparticle designs, as it leverages naturally occurring strategies that have been refined by the process of evolution. Consider the cell, one of the most fundamental units of biology, which is particularly adept at carrying out defined functions within complex environments. Either independently or as part of a multicellular organism, a cell comes into contact with a wide range of proteins, other cells, and extracellular matrices, but elegantly manages to carry out the specific tasks necessary for its survival. By employing biomimetic design principles, researchers hope to capture the incredible sensitivity and specificity that are inherent in nature.
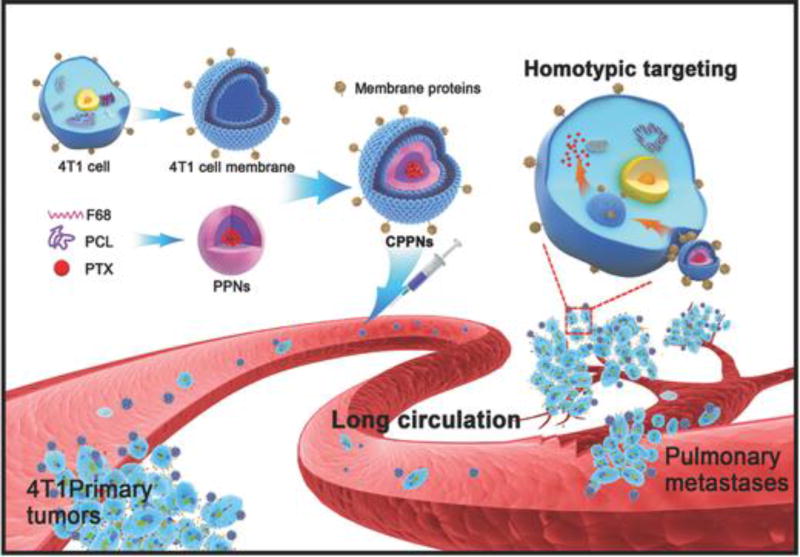
Spawning from this movement is a new class of biomimetic nanoparticles that combine the advantages of both natural and artificial nanomaterials.[23–26] Cell membrane-coated nanoparticles are characterized by a synthetic nanoparticulate core cloaked by a layer of natural cell membrane (Figure 1). Cell membrane coating is a platform technology that presents a facile top-down method for designing nanocarriers with surfaces that directly replicate the highly complex functionalities necessary for effective biointerfacing. Cell membrane-coated nanoparticles inherently mimic the properties of the source cells from which the membrane is derived, bestowing a wide range of functions such as long circulation and disease-relevant targeting.[23,24] In this review, we provide a comprehensive overview of this new technology, from its initial development to the current state of the art. A specific emphasis is placed on the different types of membrane coatings currently employed, along with their special features. Their advantages for specific applications are covered in depth, including some applications that uniquely benefit from the presence of biological membranes. The utility of the cell membrane coating approach will undoubtedly expand as time progresses, and we conclude with discussion on potential future directions.
Figure 1.
Cell membrane-coated nanoparticles. A variety of cell types have been used as sources of membranes to coat over nanoparticles. Each cell membrane type can utilize unique properties to provide functionalities to nanoparticulate cores, the material of which can be varied depending on the desired application.
2. Development of Cell Membrane Coating Technology
Synthetic functionalization strategies have been successfully employed to greatly enhance nanoparticle performance for a wide range of different applications. In many cases, they do an excellent job of replicating individual biological interactions found in nature. However, as researchers continue to push the boundaries of nanomedicine, bottom-up fabrication strategies become increasingly difficult to replicate the collective functions of biological systems because in reality they are incredibly complex and multifactorial. Additionally, synthetic platforms must also overcome the fundamental fact that they are, by their very nature, foreign. As such, researchers have recently turned towards biomimicry as a guiding principle for the design of next generation nanoplatforms.[18–20,27,28] By leveraging the mechanisms and interactions crafted by nature over the course of millions of years of evolution, significant steps have been made towards further improving nanoparticle functionality while streamlining development.
2.1 Background
The cell is one of the most fundamental units of life, and it must perform a variety of complex functions in order to survive and proliferate. To do such, cells must interact with their surrounding environments, and it is their outermost layer, consisting of cell membrane, that bears the bulk of this responsibility. Cell membrane is composed of a mixture of lipids, proteins, and carbohydrates. Lipids are largely responsible for the bilayer structure and fluidity of the membrane, while also playing a role in signaling. Proteins, either transmembrane or membrane-anchored, and carbohydrates are responsible for providing the interfacing functionalities of the membrane. For example, carbohydrate chains terminated in specific sugar residues demonstrate important roles in cellular recognition.[29,30] Proteins play major roles in signaling and adhesion;[31,32] the expression profile of surface protein markers determines important characteristics about individual cell types, including where they localize,[33] how they respond to environmental cues,[34] and how they exert influences on other cells.[35] While knowledge is still accumulating on the role of individual protein markers, at least some information is available regarding the function of many. Notable examples, like the “self-marker” CD47, have significant implications for the design of biomimetic nanocarriers.[36] Adhesion and binding molecules present on specific cell subsets also have the potential for guiding the design of platforms that exhibit organotropism.[37] Researchers have used surface glycan-mimicking molecules to improve colloidal stability or to increase targeting specificity, particularly towards immune cell subsets.[38,39] Proteins or their derivatives, including those such as the minimal “self-peptide” derived from CD47,[40] can be directly conjugated onto nanoparticles surfaces. Taking advantage of such native functionalities originating from the cell membranes has become a topic of significant interest. While biomimetic design strategies exist in many different forms, from mimicking the physical properties of cells to the identification of natural targeting ligands,[18,22] one of the most appealing approaches is the direct use of cellular membrane components for nanoparticle functionalization.[21]
2.2 Initial concept of cell membrane coating technology
In 2011, the cell membrane coating technology was first reported, in which researchers directly leveraged entire cell membranes as a material for nanoparticle coating.[23] By transferring the outermost layer of a cell directly onto the surface of a nanoparticle, the complexity of the membrane, with all of its lipids, proteins, and carbohydrates, can be faithfully preserved, enabling the resultant membrane-coated nanoparticle to take on many of the properties exhibited by the source cell. This concept was first demonstrated using red blood cells (RBCs) as the source of membrane material (Figure 2).[23] RBCs, which are responsible for oxygen delivery within the body, are known to have a lifespan of up to 4 months in humans. The ability of these cells to circulate for extended periods of time, a highly desirable property for nanoparticle drug delivery, is mediated by RBC surface markers, including CD47 and an array of complement regulatory proteins.[27,36] In the initial proof-of-concept study, membrane ghosts were first obtained via the hypotonic lysing of the RBCs, and the membrane was fashioned into vesicles via a combination of sonication and mechanical extrusion through porous membranes. When subsequently co-extruded with preformed polymeric cores made from poly(lactic-co-glycolic acid) (PLGA), the resultant nanoparticles exhibited a core-shell structure when viewed under transmission electron microscopy (TEM), with the membrane surrounding the core. Size and zeta potential measurements were also consistent with a layer of membrane coating around the cores. Notably, the nanoparticles were able to circulate for extended periods of time when administered intravenously in a mouse model, with an elimination half-life of approximately 40 hours, outperforming a PEGylated control. This long circulation property was attributed to the natural RBC membrane and highlighted the potential of cell membrane coatings for nanoparticle functionalization.
Figure 2.
RBC membrane-coated nanoparticles. Cell membrane can be derived from RBCs using hypotonic treatment. When co-extruded with polymeric nanoparticulate cores, RBC membrane-coated nanoparticles are formed. The nanoparticles retain many of the same surface markers as the original RBCs, including the self-marker CD47 that allows for immune evasion and long blood circulation. Reproduced with permission.[23] Copyright 2011, National Academy of Sciences.
2.3 Characteristic analyses
Further studies on RBC membrane-coated nanoparticles (RBC-NPs) have helped to provide a greater understanding of their unique properties. For example, it was confirmed that the membrane functionalization process successfully translocated the self-marker CD47, which was present at a density consistent with the source RBCs.[41] Further, gold immunostaining was employed to demonstrate that the protein was incorporated in a right-side-out orientation, which is essential for its proper functioning. This allows CD47 to correctly interface with its corresponding receptor, thus lowering macrophage uptake. Glycoprotein and sialic acid assays also demonstrated that carbohydrate residues from the cell membrane were found almost exclusively on the outer face of the nanoparticles, again consistent with a right-side-out coating.[42] The importance of surface proteins and carbohydrates for nanoparticle stability was also highlighted, as removal via trypsinization destabilized RBC-NPs at physiologically relevant salt concentrations. Another independent study using a dye quenching system also arrived at the conclusion that a majority of the membrane on RBC-NPs exists in a right-side-out orientation.[43] In another study, biotinylated PLGA cores were used to demonstrate the completeness of membrane coatings; at sufficient ratios of membrane to polymer, streptavidin-induced crosslinking of the biotinylated PLGA cores could be entirely prevented.[42] Due to the charge asymmetry inherent to biological membranes, it has been demonstrated that a negative nanoparticle surface best facilitates membrane coating, whereas positively nanoparticle substrates interact strongly with the membranes, leading to a crosslinked network. Finally, nanoparticles of varying sizes, ranging from tens of nanometers to several hundred nanoparticles, have been successfully coated with cell membrane.[42]
Following the initial reports on RBC-NPs, the strategy of using cell membranes to functionalize nanoparticle surfaces has since been shown to be highly generalizable, expanding to cover a wide range of different nanomaterials combined with membranes derived from various cells types. Cell membrane-coated nanoparticles have also been incorporated into other formats, such as into hydrogels,[44] or can be fabricated via templated synthesis schemes in which the nanoparticulate core is formed in situ.[45] All of these variations, along with their applications, will be covered in depth in subsequent sections.
2.4 Methods of coating
Cell membrane-coated nanoparticles can be fabricated using several different methods. Initial works relied exclusively on physical extrusion in which nanoparticulate cores and purified membrane are co-extruded through a porous membrane.[23] This method was adapted from the synthesis of synthetic liposomes, and the mechanical force provided by the extrusion is believed to disrupt the membrane structure and enable it to reform around the nanoparticulate cores. More recently, a sonication-based approach has been employed.[46] Using this technique, the two components are subjected to disruptive forces provided by ultrasonic energy, resulting in the spontaneous formation of a core-shell nanostructure. Results from this method are consistent with those of particles made using physical extrusion, with the added benefit of less material loss. In terms of the mechanism responsible for membrane coating, it is believed that a combination of the semi-stable nature of bare nanoparticulate cores and cell membrane-derived vesicles, along with the charge asymmetry of biological membranes, makes the core-shell configuration with right-side-out membrane orientation energetically favorable.
Other novel methods for the encapsulation of nanoparticulates into cell membranes have been reported. Very recently, a microfluidic system that combines rapid mixing with electroporation has been employed to successfully coat RBC membrane around magnetic nanoparticles.[47] The reported device consisted of a Y-shaped merging channel, S-shaped mixing channel, and an electroporation zone right before the outlet. By fine-tuning the pulse voltage and duration, as well as the flow velocity, high-quality particles with complete coatings and exceptional stability were fabricated. Beyond techniques that use purified membrane material, there is a unique approach based on the in situ packaging of nanomaterials using live cells.[48] In this fabrication scheme, cells were first incubated with iron-oxide nanoparticles, gold nanoparticles, or quantum dots. It was then demonstrated that, when incubated in serum-free media, the cells could secrete vesicles containing the exogenous nanoparticles.
3. RBC Membrane-Coated Nanoparticles
RBCs are nature’s long circulating carriers. These cells live up to 120 days in humans, enabling them to fulfill their important biological function of transporting oxygen. With limited immune cell clearance, RBC membrane was an attractive first choice for cell membrane coating onto nanoparticles. The RBC-NP became the first cell membrane-coated system reported, and it is currently the most well-studied in the field. The rapid expansion of this platform is partially due to the ease of cell collection and lack of intracellular organelles, which make membrane collection simple and scalable for efficient manufacturing. In addition, RBC-NPs have the clearest path towards translation, as blood transfusions are common, and there is the potential to use type-matched RBCs as membrane sources to maximize biocompatibility for wide clinical use.
3.1 Drug delivery
Drug delivery is traditionally one of the staples of nanomedicine, and thus there has been a significant amount of research applying RBC-NPs for a variety of drug delivery applications. In one of the first examples, doxorubicin (DOX) was loaded into poly(lactic acid) PLA cores and subsequently coated with RBC membrane.[49] Two different methods of drug loading, physical encapsulation and chemical conjugation, were assessed for encapsulation efficiency and drug release kinetics. Physical encapsulation of DOX was achieved by mixing the drug with PLA polymer in the organic phase, follow by nanoprecipitation into an aqueous phase. In the chemical conjugation method, ring-opening polymerization was used to make a DOX-PLA polymer conjugate, which was then directly precipitated into an aqueous phase to form nanoparticles. It was demonstrated that the chemical conjugation of DOX to the PLA enabled higher drug loading and provided a more sustained release over time. Additionally, the layer of membrane coating served as a diffusional barrier that further slowed drug release kinetics. When incubated with Kasumi-1 leukemia cells, both drug-loaded nanoformulations demonstrated increased cytotoxicity compared with free drug, which is likely due to their ability to overcome the drug-efflux mechanisms present in the cells. A similar DOX-loaded RBC-NP formulation was used to treat a murine model of lymphoma, demonstrating a marked ability to increase survival compared with equivalent doses of free drug.[50] It was further shown that the RBC-NP nanocarriers themselves were generally safe and did not display any myelosuppression effect, whereas free drug caused an obvious reduction in multiple immune cell subsets. In addition, no anti-RBC antibodies were detected in mouse serum even after multiple RBC-NP administrations, indicating no acute or long-term immune responses against the nanoparticles. The safety and long-term applicability of using RBC membrane coatings was also demonstrated using an iron oxide nanoparticle platform.[51] In the study, it was demonstrated that RBC membrane coating significantly outperformed PEG in terms of enhancing circulation. As previously shown, upon repeat administration, PEGylated nanoparticles had increasingly short circulation times due to the accelerated blood clearance phenomenon, which is orchestrated by anti-PEG IgM and IgG antibodies that form after each injection. The RBC-NPs, however, did not cause an increase in IgM or IgG antibodies after multiple injections, and thus the long circulation time of the particles was consistent over multiple injections. In addition to avoiding the accelerated blood clearance phenomenon, RBC-NP administration caused no overt signs of toxicity and the level of myeloid-derived suppressor cells were consistent with baseline values. Taken together, these studies indicate that RBC membrane coating may serve as a viable alternative to PEG that can be used without fear of immunogenicity.
Despite the fact that a major advantage of cell membrane-coated nanoparticles is the ability to transfer over native functionalities via associated surface markers, several strategies have been developed to add further membrane surface functionality. Typical functionalization techniques rely on chemical conjugation, such as sulfhydryl-, carboxyl-, and amine-based reactions. However, when working with biological membranes, one challenge is that components such as proteins are prone to denaturation compared to purely synthetic nanoparticles. To preserve the membrane’s biological activity, alternatives to chemical conjugation need to be considered, and so far, several non-disruptive functionalization techniques have been developed to address this potential issue. One strategy has been to use a lipid-tethering technique to introduce additional ligands onto RBC-NP surfaces.[52] In the study, different molecules, such as the small molecule folate or the aptamer AS1411, were attached via a linker to a lipid anchor. The product could then be inserted into RBC membrane, which was subsequently used to prepare targeted RBC-NPs. Using the targeted versions of the nanoparticles, it was demonstrated that uptake to cells overexpressing the corresponding receptors could be significantly enhanced. In a separate example, maleimide-terminal PEG linkers were attached to the RBC membrane via a succinimidyl ester, enabling surface decoration with thiolated enzymes.[53] Using a thiolated recombinant hyaluronidase as a model enzyme, nanoparticles capable of more efficiently diffusing through the hyaluronic acid-rich extracellular matrices of tumors were fabricated. In a similar fashion, streptavidin can be inserted into the RBC membrane to allow for binding of extrinsic ligands modified with biotin. This two-step functionalization method was used to modify RBC-NPs with a positively charged candoxin-derived peptide, providing the nanoparticles with brain endothelial cell targeting abilities.[54] When loaded with DOX, these brain-targeting nanoparticles could more effectively treat mouse gliomas compared to the unmodified RBC-NPs. Beyond physical conjugation, other strategies such as co-administration with tumor-penetrating peptide iRGD have been used to further boost the natural tumor accumulation of RBC-NPs.[55] Paclitaxel (PTX)-loaded RBC-NPs injected in combination with the peptide showed increased drug delivery to tumors and sites of metastasis, and treatment with the nanoparticles could inhibit tumor growth in a 4T1 mouse tumor model.
To directly navigate nanoparticles to a desired location, RBC membrane can be coated over cores with a magnetic component for guided delivery. In the first example of such a system, the chemotherapeutics PTX and DOX were encapsulated along with iron oxide nanocrystals in O-carboxymethyl-chitosan nanoparticles via a double emulsion process.[56] The membrane coating significantly attenuated cellular uptake compared to a PEGylated version of the nanoformulation. After further functionalizing with RGD on the surface using a lipid-insertion approach, the targeted formulation was effectively internalized by Lewis lung carcinoma cells, an effect that was further facilitated by application of magnetic field. Using a mouse model with the same cells, the membrane-coated nanoformulation with the RGD targeting ligand very efficiently localized to the tumor in the presence of a magnetic field. Due to the improved localization to the tumor site, as well as the expedited cellular uptake, the drug-loaded nanoparticles were able to significantly control tumor growth while prolonging survival. Safety studies showed the membrane-coated formulation did not elevate serum antibody levels, whereas administration of the clinically used Taxol formulation resulted in spikes of IgE levels. Further, the membrane-coated formulation did not have leuko-depletive effects compared with Taxol.
Beyond standard encapsulation and delivery of chemotherapeutics, more sophisticated strategies for triggered release have demonstrated compatibility with the RBC membrane coating approach. In the first such example, a near infrared (NIR)-triggered formulation was made by incorporating a thermosensitive lipid into the nanoparticle core material.[57] In the system, the chemotherapeutic PTX was incorporated into polycaprolactone (PCL) cores coated with 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC), which has a melting transition temperature of 41.5 °C. An outer RBC membrane layer included a lipophilic dye 1,1-dioctadecyl-3,3,3,3-tetramethylindotricarbocyanine iodide (DiR), which can induce hyperthermia upon excitation. It was demonstrated that, upon laser excitation, the release of drug was facilitated as the core lost structural integrity. Combined with an increase in cell permeability during laser excitation, PTX was rapidly delivered intracellularly, enhancing cytotoxicity of the nanoformulation. Using a 4T1 mouse breast cancer model, it was shown that the nanoformulation could much more effectively localize to the tumor compared with free DiR, and this enabled a significant rise in temperature when the tumor was excited with NIR light. This ultimately translated to improved tumor control and reduction in the number of lung metastases when mice were treated with the thermally sensitive nanoparticle. In a similar system, DOX and the photosensitizer chlorin e6 (Ce6) were loaded into mesoporous silica nanoparticles and coated with RBC membrane.[58] The membrane coating helped to trap the drug within the mesoporous structure until far-red laser irradiation, during which the Ce6 generated reactive oxygen species (ROS) and disrupted the membrane structure, triggering drug release. Similarly, the Ce6- and DOX-loaded mesoporous silica nanoparticles were able to deliver the DOX to tumor sites in a responsive manner, leading to a control of tumor growth and metastasis formation in a 4T1 mouse tumor model. Using this system, it was also demonstrated that intracellular ROS production after nanoparticle uptake positively correlated with the laser power, indicating that the same Ce6-generated ROS that triggered drug release could continue to act as a photodynamic therapy, combining with the chemotherapy to improve tumor cell destruction. In another example, a layer of TiO2 was coated around docetaxel (DTX)-encapsulated SiO2 nanoparticles, and subsequently coated with RBC membrane.[59] The TiO2 enabled the photocatalytic degradation of the membrane coating upon ultraviolet (UV) irradiation, facilitating drug release. Similar to the Ce6 photosensitizer, the TiO2 is able to generate ROS that can degrade the membrane coating as well as act directly as a photodynamic therapy to improve cytotoxicity to cancer cells. In some cases, the drug delivery vehicle can also act as the photosensitizer. A very recent example used hollow mesoporous nanoparticles made of Prussian blue, a material that is inherently adept at photothermal conversion, to load DOX at extremely high weight ratios.[60] Coating the particles with a layer of RBC membrane helped to stabilize the nanoparticles over time and improved their safety profile. The longer circulation time provided by the RBC membrane layer allowed for improved localization to the tumor site, and when combined with NIR laser irradiation, the triggered drug release resulted in significant control of tumor growth.
In contrast to externally triggered release, RBC-NPs have also been modified to release payloads in response to natural environmental changes around tumor sites, such as increased local acidity. For example, a PTX-polymer prodrug made using pH-sensitive poly(L-γ-glutamylcarbocistein) (PGSC) was self-assembled into nanoparticles and wrapped in RBC membrane.[61] When incubated at a pH of 6.5, PTX release was faster than when incubated at a normal body pH of 7.4. Wrapping in RBC membrane significantly reduced uptake into macrophages, helping the particles to evade the immune system and circulate long enough to reach the acidic tumor microenvironment, where the PTX was triggered to release and exert an antitumor effect. Antitumor efficacy has also been achieved with a pH-responsive nanogel delivering a chemotherapy and cytokine combination.[62] Oppositely charged chitosan derivatives and a crosslinker were used to encapsulate PTX and interleukin (IL)-2, a T cell-supporting cytokine, into a nanogel formulation. RBC membrane was then extruded around the nanogel to facilitate membrane coating, which was used to protect the payload while allowing for long circulation and passive accumulation to the tumor site. Once in a weakly acidic tumor microenvironment, the negatively charged amphoteric chitosan derivative protonates and becomes positively charged, and electrostatic repulsion causes disintegration of the core and release of the chemotherapy and cytokine. With this strategy, the RBC-NPs had increased release of PTX and IL-2 at pH 6.5 compared to pH 7.4, an extended blood circulation time, and at least a fivefold increase in tumor delivery of both cargos. Enhanced delivery of the chemo-immunotherapy and the tumor microenvironment pH-triggered release led to improved antitumor efficacy in an aggressive B16-F10 melanoma model. In a different example, drug-loaded and pH-responsive RBC-NPs were formulated by remote loading into RBC membrane-derived vesicles.[63] To accomplish this, additional cholesterol was supplemented to RBC vesicles to further stabilize the membrane structure and enable the retention of a pH gradient across the RBC membrane. Using this stable pH gradient, small molecule therapeutics such as DOX and vancomycin were able to be remotely loaded into the vesicle interiors until destabilization of the RBC membrane vesicles prompted drug release in acidic conditions. The improved delivery and drug release were shown to improve therapeutic efficacy of DOX in a 4T1 mouse breast cancer model, and it also significantly decreased methicillin-resistant Staphylococcus aureus (MRSA) burden in a murine skin infection model.
While most examples of RBC membrane-coated nanodelivery systems have been for the delivery of chemotherapeutics to tumors, there is an emerging use of such technology for treatment of bacterial infection. Core-shell gelatin nanoparticles loaded with the antibiotic vancomycin were coated with RBC membrane to make a combinatorial platform featuring environmentally sensitive antibiotic delivery and detoxification.[64] Using this system, vancomycin could be loaded at approximately 11.4 wt% into the gelatin core, and the membrane coating minimized uptake by macrophages. An advantage of using a gelatin-based nanoparticle is that it can responsively disintegrate in the presence of gelatinase, which is secreted locally by a wide range of bacteria. As an added benefit, the particles attenuated hemolysis induced by the exotoxin-rich medium of various bacteria. In a separate example, vancomycin-loaded nanogels generated by in situ gelation within RBC vesicles also showed promise for intracellular antibacterial treatment.[65] The gel was fabricated using a disulfide-based crosslinker, which contributed redox-responsiveness to the system. The responsiveness was confirmed in the presence of a reducing agent, which significantly enhanced drug release. The same effect was not observed when a similar non-responsive nanogel was fabricated. The nanoparticle played multiple roles to aid in the clearance of bacteria. First, the RBC membrane neutralized pore-forming toxins secreted by bacteria, which better enabled phagocytic uptake by macrophages and decreased bacterial virulence. Further, due to the loaded drug and redox responsive core, the vancomycin was released once taken up into the reducing environment of infected cells, enabling the treatment of intracellular bacteria and lowering the burden of live bacteria within macrophages when compared with free drug.
It is sometimes desirable to deliver large payloads to the inside of a cell. Such is the case for some intrabodies, which are antibodies that target intracellular targets not found on cell surfaces. The membrane-coating strategy has been adapted to deliver these biomolecules; antibodies against the cytoplasmic tumor marker, human telomerase reverse transcriptase (hTERT), were formed into nanoparticle cores before being coated with RBC membrane.[66] The antibody cores were synthesized by resuspending lyophilized hTERT antibodies in hydrochloric acid and titrating with sodium hydroxide until the isoelectric point was reached and the antibodies spontaneously precipitated out into nanoparticles. The collected particles could then be extruded with RBC membrane to form coated nanoparticles approximately 200 nm in size. It was shown that both the coated and uncoated nanoparticulate forms of the antibodies facilitated uptake into cells and prolonged circulation, but the coated version largely outperformed the uncoated antibody nanoparticles. Regarding nonspecific uptake, the membrane coating also helped to reduce macrophage uptake. To test the activity of the particles, a telomerase activity assay was performed. It was shown that the membrane-coated particles performed the best, decreasing telomerase activity to near 50% of original levels. Finally, histological analysis of tumor sections collected after injection of the formulations showed the highest degree of localization for the membrane-coated formulation. Overall, this work demonstrated a promising approach to enabling targeting of intracellular therapeutic targets that are difficult to access by traditional antibody administration.
3.2 Imaging and photoactivatable therapy
Imaging and photo-based therapies are important aspects of nanomedicine, especially given the wide range of nanomaterials that have the potential excel at such applications. Like with nanoparticle-based drug delivery, it has been demonstrated that RBC membrane coating holds great utility when applied to these other areas of research. In a first proof-of-concept study, it was shown that gold nanoparticles, which have unique optical properties that are useful for detection and photothermal applications, could be successfully functionalized with membrane coatings.[67] The coating of membrane led to a slight increase in nanoparticle size due to the new core-shell structure, and stability was maintained in both phosphate buffered saline (PBS) and fetal bovine serum (FBS) for at least three days. Using a thiolated dye, it was demonstrated that the nanoparticles with membrane coatings could preclude binding and subsequent quenching by the gold cores. Using large polystyrene nanoparticles coated with antibodies against the self-marker CD47, it was also demonstrated that the membrane was largely configured in a right-side-out orientation. Finally, the coating helped to significantly reduce uptake by macrophage cells, which could easily be visualized using brightfield microscopy. With these results, it was postulated that membrane coating could help to reduce the rate of in vivo clearance compared to uncoated gold nanoparticles.
Beyond metallic nanoparticles, inorganic nanoparticles are also commonly used. In one instance RBC membrane was coated around upconversion nanoparticles (UCNPs) for tumor imaging.[68] In the work, it was shown that membrane-coated UCNPs could inhibit the binding of a protein corona, whereas uncoated particles attracted a significant layer of proteins when exposed to human plasma, which also led to significant increases in size. The particles were further functionalized via a lipid anchor with folic acid, which was used to help the particles efficiently target folate receptor-overexpressing cancer cells in vitro. The coated particles also exhibited a better targeting effect compared with folate-functionalized bare UCNPs, leading to increased blood residence and enhanced tumor localization in an MCF-7 tumor xenograft model in nude mice. After administration, it was further demonstrated that mouse blood chemistry remained normal and there was no readily observable damage of major organs upon histological analysis.
It was later demonstrated that RBC membrane-functionalized gold nanocages could be used to photothermally ablate cells after intracellular uptake (Figure 3).[69] The membrane coating enabled significantly enhanced circulation within the blood compared to non-functionalized nanocages, which led to decreased liver distribution and enhanced tumor uptake. Using a murine 4T1 tumor model, the nanoparticles could be used to elevate temperatures from 35 °C to 47.1 °C at the tumor site upon a ten-minute irradiation with a NIR laser. The induced hyperthermia had a significant impact on tumor growth and greatly extended survival. A similar photothermal effect was also demonstrated with RBC membrane-coated iron oxide nanoclusters.[70] After demonstrating successful coating, it was shown that the particles could be used to kill cells in a photoactivatable manner. Enhanced circulation increased the local concentration of particles in MCF-7 breast cancer xenografts, leading to control of tumor growth when subject to five minutes of laser irradiation. As an added benefit, the platform doubled as a magnetic resonance imaging (MRI) contrast agent for theranostic applications, with a darker and longer lasting signal observed in the tumor area compared to uncoated iron oxide clusters. Similar RBC membrane-coated iron oxide nanoparticles were also fabricated using a microfluidic electroporation method instead of extrusion.[47] Consistent with the particles made using the extrusion protocol, the electroporation coated particles demonstrated the ability to simultaneously image tumors via MRI and photothermally ablate tumors upon irradiation. Additionally, RBC membrane-coated nanoparticles have been made with components that can combine photothermal abilities with chemotherapy delivery as detailed in the previous section.[57–60] In these cases, the photothermal components can be used to simply trigger drug release or as part of a photoablation-chemotherapy combination treatment.
Figure 3.
RBC membrane-coated gold nanocages for photothermal therapy. RBC membrane coating allows gold nanocages to circulate longer in the bloodstream and accumulate in tumors efficiently. When irradiated with an NIR laser, the nanocage cores raise the local temperature, thus enabling control of tumor growth. Reproduced with permission.[69] Copyright 2014, American Chemical Society.
Other than the use of synthetic materials, nanoparticle platforms based on natural and organic compounds have been taken advantage of as photothermal agents. In one case, melanin nanoparticles were coated with RBC membrane for combination photothermal therapy and photoacoustic imaging.[71] Natural melanin nanoparticles were extracted from the ink sacs of cuttlefish, and the resulting particles were between 100–200 nm in size. It was confirmed that these natural melanin particles had high photothermal conversion efficiency, enabling them to raise the temperature of solution more efficiently than control melanin-like polydopamine nanoparticles. After coating with RBC membrane, the resulting particles retained the photothermal conversion capabilities of their uncoated counterparts and were stable for at least a week. Further, they showed no toxicity when incubated with cells until radiation was applied. In vivo, the circulation of the coated particles was significantly enhanced compared with uncoated melanin particles, and accumulation was preferentially increased within the tumor in A549 xenografts. After intravenous administration, it was shown that the coated particles could be used to generate photoacoustic contrast at the tumor site, and local application enabled a significant rise in temperature at the tumor site upon irradiation. Finally, when used to treat a tumor, the irradiated membrane-coated particle virtually eliminated tumor growth. In comparison, tumors treated with an uncoated formulation and irradiated with the same power of laser still grew.
In general, RBC membrane coating can improve the circulation time of photothermal nanoparticles, which causes improved localization to tumors via the enhanced permeation and retention (EPR) effect and enhances photothermal therapy. In combination with RBC-NPs, there have been recent efforts to strengthen the EPR effect and further increase tumor accumulation by modulating the tumor microenvironment. Cyclopamine, a steroidal alkaloid, has been used to disrupt the thick extracellular matrix of pancreatic ductal adenocarcinomas and improve blood permeability for gold RBC-NPs.[72] RBC membrane-coated gold nanorods were developed that provided a nearly 15-fold increase in blood retention compared to uncoated gold nanorods with no significant effect on photothermal conversion efficacy. At the same time, to combat the limited blood vessel availability and dense tissue of pancreatic ductal adenocarcinomas, cyclopamine treatment of human Capan-2 xenografts was explored. Daily oral administration of cyclopamine over three weeks yielded 60% reduction in tumor fibronectin expression, doubling the number of functional blood vessels, and improved tumor perfusion as shown by ultrasound imaging of tumors after microbubble injection. This modulated tumor microenvironment allowed for an almost twofold increase in coated gold nanorod accumulation compared to the accumulation in untreated tumors. Combined with laser irradiation, mice treated with cyclopamine and the biomimetic nanorods caused significant regression of tumor growth, while treatment with the nanorods alone or the cyclopamine alone yielded negligible results. Enhanced localization of photothermal nanoparticles was also realized using an endothelin A (ETA) receptor antagonist BQ123 to selectively dilate tumor vasculature.[73] By occupying the ETA receptor, which is overexpressed in tumors, vasoconstriction can be selectively blocked and blood perfusion throughout the tumor can increase. Confirming this idea, intraperitoneal injection of BQ123 into nude mice bearing HCT116 human colon carcinoma tumors resulted in a rapid dilation of tumor vessels by about 25%, increasing blood oxygen saturation levels to that of the surrounding normal tissue. Fluorescent imaging of labeled polypyrrole RBC-NPs after injection into BQ123 treated tumors demonstrated a 1.37 times higher local concentration of particles at the tumor site compared to untreated tumors. Co-administration of the RBC-mimicking polypyrrole nanoparticles and BQ123 followed by NIR irradiation in tumor-bearing mice yielded the highest temperature in the focal range, and this significantly suppressed tumor growth compared to the RBC-NPs alone or a combination therapy using a PEGylated polypyrrole nanoparticle with NIR irradiation.
Unlike photothermal therapy, which depends on local heating to create hyperthermia, photodynamic therapy relies on photosensitizers to generate ROS upon laser irradiation as the mode of killing. For both strategies, however, increased local concentration of the active agent to the tumor site can greatly enhance efficacy. Cell membrane coating has thus been used to enhance photodynamic nanoplatforms in much the same way as those for photothermal therapy. For example, UCNPs coated with a layer of the photosensitizer merocyanine 540 were subsequently coated with a layer of RBC membrane.[74] Upon NIR irradiation, the energy emitted by the nanoparticles transferred to the photosensitizer, facilitating the production and release of singlet oxygen capable of killing cancer cells. Using a singlet oxygen detecting sensor 9,10-anthracenediylbis(methylene)dimalonic acid, it was determined that the membrane-coated particles could very effectively generate reactive oxygen molecules. Upon incubation with cells and irradiation, the particles could effectively kill cells in vitro. Particles could also be further functionalized via lipid anchoring of both folate and triphenylphosphonium (TPP), the latter of which was used to target mitochondria to maximize the effect of ROS, with little detrimental effect on the long circulation of the coated particles. The dual-targeted nanoparticles could efficiently localize to established murine B16 tumors using the folate receptors, and the TPP allowed internalized particles to bind to the mitochondria. Upon laser application, the resulting photodynamic therapy could significantly control tumor growth and prolong survival, and almost all mice in the dual-targeted formulation survived past 30 days, whereas all control mice died within 2 weeks. In another similar scheme, bismuth nanoparticles were coated in RBC membrane that was further functionalized with folate via lipid-insertion.[75] When irradiated with x-rays, the nanoparticles promoted the generation of free radicals and demonstrated the ability to control tumor growth in a 4T1 mouse tumor model. The formulation was also shown to be safe and was cleared from the body within 15 days.
A challenge for applying photodynamic therapy to tumors is that oftentimes the inner parts of the tumor is hypoxic, and the lack of oxygen will lead to decreased efficacy of the treatment. To address this issue, one group designed an oxygen self-enriched platform in which perfluorocarbon was used as an oxygen carrier.[76] To accomplish this, they employed a human serum albumin nanoparticulate core loaded with indocyanine green (ICG) as the photosensitizer and perfluorotributylamine as the oxygen carrier. To confirm successful loading of the photosensitizer, flow cytometry was used to demonstrate colocalization of ICG with a dye inserted into the RBC membrane. When irradiated in solution, the particles with encapsulated ICG were able to locally raise the temperature, while the addition of the perfluorocarbon in the cores significantly enhanced singlet oxygen production. Coating the dual-loaded cores with RBC membrane enabled immune evasion with reduced uptake into macrophages, but high uptake into cancer cells was preserved. With regards to enhancing photodynamic therapy, it was shown that after nanoparticle delivery into cells followed by irradiation, the level of intracellular ROS was increased, which translated to a marked reduction in cancer cell viability in vitro. Notably, the RBC-NP formulation circulated in the blood for much longer than the uncoated formulation, which enabled significantly enhanced tumor uptake in a biodistribution study with tumor-bearing mice. Finally, upon treatment, the nanoparticle group with irradiation exhibited significantly controlled tumor growth, with virtually all of the tumors having been eliminated over the course of 2 weeks.
In a similar work, oxygen delivery was used to enhance cancer radiotherapies. To develop this formulation, perfluorocarbon was loaded into PLGA cores, then cloaked with RBC membrane.[77] It was shown that the particles had good oxygen-carrying capacity, and significantly raised oxygen levels when pre-oxygenated and added to deoxygenated water. The membrane-coated particles were able to circulate for significantly longer than the uncoated perfluorocarbon-loaded PLGA nanoparticles. Tumor histology taken 24 hours after injection of the particles into 4T1 tumor-bearing mice demonstrated that the nanoparticles could traverse past the vasculature into the interior of the tumor, while intact RBC controls localized only with vessels. To confirm the ability of the nanoformulation to oxygenate tumors, photoacoustic imaging revealed that there was more oxygenated hemoglobin residing in the tumor for the membrane-coated particles compared with the uncoated group. Comparing tumor histological sections from both groups over time, the coated formulation showed decreasing hypoxyprobe signal and hypoxia-inducible factor (HIF)-1α signal, indicating hypoxia relief. Finally, to test their hypothesis, the nanoformulation was administered and 24 hours later x-rays were used to irradiate the tumor. It was demonstrated that nanoparticle pre-administration improved the efficacy of x-ray irradiation, and the effectiveness could be easily visualized 24 hours after treatment using histology. This example proved to be a valid strategy for rationally combining different modalities to maximize efficacy based on inherent tumor biology.
3.3 Detoxification
Beyond traditional nanomedicine modalities such as drug delivery and imaging, the use of natural membrane coatings opens up additional applications that leverage the biological interactions inherent to surface proteins found on the cell surface. One such area is detoxification, which takes advantage of the fact that most toxins, regardless of their mode of action, must in some way interact with cellular membranes.[78] Further, these interactions are often mediated by specific cellular receptors, with strong affinities that can easily be leveraged. To prove this concept, RBC membrane-coated nanosponges were employed to neutralize α-hemolysin from Staphylococcus aureus (Figure 4).[79] By incubating the nanosponges with the toxin, it was possible to completely abrogate the hemolytic effect of the toxin. Neither PEGylated PLGA nanoparticles nor PEGylated liposomes were able to neutralize the toxin in this manner, as neither could bind an appreciable amount of the toxin. Further, it was demonstrated that RBC vesicles alone also could not prevent hemolysis, likely due to their ability to fuse with healthy RBCs and transfer the hemolytic toxins. This is something that is believed to be prevented when membrane is coated onto a stabilizing nanoparticle substrate. The toxin neutralization effect was demonstrated in vivo by subcutaneously administering the toxin alone or pre-complexed with nanosponges. With nanosponge complexation, there was no visible skin damage, while toxin alone caused significant lesion formation. Finally, in a lethal toxin challenge model, the RBC nanosponges were able to significantly enhance survival in both a prophylactic and therapeutic setting. This concept has also been proven for other toxins such as melittin,[79] as well as for streptolysin-O.[79,80]
Figure 4.
RBC membrane-coated nanosponges for toxin neutralization. Pore-forming toxins can insert into the RBC membrane on the surface of the nanosponges, where they are retained and neutralized. By safely sequestering the toxins, RBC nanosponges spare healthy RBCs from being lysed. Reproduced with permission.[79] Copyright 2013, Nature Publishing Group.
The ability of the RBC nanosponges to display efficacy in a bacterial infection model was studied more in depth using group A Streptococcus (GAS).[81] In vitro, it was demonstrated that the nanosponges could neutralize the bioactivity streptolysin-O, both preventing hemolysis and preventing the ability of the toxin to induce cell death on keratinocytes. Further, the nanosponges had a protective effect on macrophages, preventing both toxin-mediated and bacteria-mediated death. This also enabled a J774 macrophage cell line to enhance their killing of the bacteria, leading to lower bacterial recovery when co-incubated with the nanosponges, likely due to the decreased virulence of the bacteria once disarmed of their toxins. Further, the nanosponges also rescued the ability of neutrophils to kill the bacteria, with the effect being observed both in whole blood and for purified neutrophils. Fewer bacteria were recovered from culture, and there was a marked increase in the amount of neutrophil extracellular traps. Finally in a live murine infection model, mice were challenged subcutaneously with GAS bacteria, followed by treatment with the nanosponges. The nanosponge-based detoxification led to significantly decreased lesion sizes and a correspondingly lowered bacterial count. Decreased inflammation around the infected region was also observed.
The nanosponge concept has been applied in several different formats. In one instance, RBC nanosponges were incorporated into a hydrogel matrix for localized treatment of MRSA infection via toxin neutralization.[44] It was demonstrated that, as the amount of crosslinker used was increased, fewer nanosponges were released from the hydrogel over time. Additionally, absorption capacity significantly increased for the nanosponge-incorporated hydrogel versus an empty hydrogel. From a functional perspective, the nanosponge gel was able to prevent hemolysis from both pure α-hemolysin and supernatant from α-hemolysin-rich MRSA culture. In vivo, the gel was able to facilitate retention of the nanosponge locally at the site of injection, with about 80% of the nanosponges left in the hydrogel at the site of injection after 2 days. In comparison, free nanosponges were only retained at a rate of around 25% over the same time period. The retention enabled effective neutralization of a bolus dose of α-hemolysin administered subcutaneously. To study the antibacterial efficacy of the nanosponge gel, a live subcutaneous infection model of MRSA was initiated followed by injection with the nanosponge gel or empty hydrogel. The nanosponge-containing formulation significantly reduced lesion formation, preventing a major symptom of the bacterial infection. Such nanosponge-hydrogel platforms can also be made using 3D bioprinting with custom design templates, such as porous discs to filter blood for toxin absorption with minimal disruption to blood flow.[82] As described earlier, a nanogel system has also been employed for simultaneous antibiotic delivery and detoxification.[65] Finally, nanomotors have been use to create “motor sponges” capable of directed movement.[83] In the system, gold nanowire motors capable of being propelled by ultrasound were employed. After successfully confirming membrane coating and validating coverage with a thiolated dye exclusion assay, propulsion was demonstrated, with the velocity of the motor sponges increasing with increasing transducer voltage at a frequency of 2.83 MHz. The propulsion could also be performed in whole blood, which suggests applicability towards further in vivo use. Finally, it was demonstrated that, with ultrasound, the motor sponges were able to more effectively neutralize toxin compared with unmanipulated motor sponges, which is likely due to an increase in the probability of toxin interaction.
The concept of nanosponges has also been demonstrated for detoxification of small molecules. In one example, organophosphates were shown to be detained using RBC nanosponges.[84] This class of small molecule toxins include commonly used pesticides, as well as biological warfare agents like VX and sarin gas. Their toxic effect occurs by the irreversible inactivation of acetylcholinesterase (AChE), an enzyme expressed at neural synapses that is responsible for breaking down the neurotransmitter acetylcholine. Accumulation of acetylcholine results in constant activation of the nervous system, which can be lethal. As RBCs also express AChE, it was demonstrated that RBC nanosponges could effectively bind to dichlorvos, a model organophosphate, and prevent its ability to deactivate endogenous AChE. This effect was exclusive to membrane-coated nanoparticles, as neither PEGylated liposomes nor polymeric nanoparticles could prevent deactivation. In both intravenous and oral models of dichlorvos challenge, the RBC nanosponges could therapeutically rescue the mice, which died within minutes when left untreated. This allowed the mice to retain a majority of endogenous RBC AChE activity, which recovered to baseline within 4 days after treatment. In another example, RBC membrane-coated nanoparticles were used as nanoabsorbents to prevent the activity of toxic small molecule drugs.[85] The effect was demonstrated to be charge-dependent, as they could bind DOX, which is positively charged, very effectively, but not methotrexate. While both bare-PLGA nanoparticles and RBC nanoabsorbents could bind drug, only the coated particles were stable in serum. It was finally shown that cell viability could be rescued after exposure to DOX in the presence of the RBC nanoabsorbents.
In the final example, nanosponges have been used to address autoimmune disorders mediated by pathological antibodies.[46] In autoimmune hemolytic anemia (AIHA), the body produces antibodies against its own RBCs, which facilitates the destruction of healthy cells and can lead to dangerously low erythrocyte counts. While such autoimmune disorders can be addressed via broad immunosuppression, these treatments are nonspecific and can carry significant risks. Other more drastic treatment options include splenectomy or the use of cytotoxic drugs, which can have severe consequences. To address these issues, it was proposed that RBC nanosponges could serve as decoys for the autoimmune antibodies, thereby rescuing healthy RBCs from attack. In vitro, the nanosponges were confirmed to effectively bind anti-RBC antibodies, preventing their ability to agglomerate RBCs in an agglutination assay. Further, pre-complexation prevented ill effects of antibody administration intraperitoneally, which normally causes a drastic reduction of RBC count, hemoglobin concentration, and hematocrit levels. It was further demonstrated that the RBC nanosponges could treat AIHA in a therapeutic scenario using an induced anemia mouse model. Importantly, there was no detectable presence of anti-RBC antibodies in healthy mice challenged with nanosponges complexed with antibodies, indicating that the treatment would likely not elicit further autoimmunity.
3.4 Immune modulation
With the ability of the RBC nanosponges to neutralize biological and chemical toxins, the platform has a valuable niche in vaccine design. The first example of employing RBC nanosponges for immune modulation involved their use for antivirulence vaccination (Figure 5).[86] In this case, the natural affinity of RBC nanosponges for certain bacterial toxins and the nanosponges’ ability to neutralize these virulence factors were leveraged to safely deliver the toxins back to the immune system in the form of a “nanotoxoid”. This strategy can be used to overcome challenges facing traditional toxoid vaccines, which are generated either by chemical or thermal denaturation, or by subunit engineering. While such approaches make the toxin safe to administer, they often come at the expense of decreased immunogenicity or antigenicity. In this work, it was confirmed that the toxicity of α-hemolysin from S. aureus was attenuated in a time-dependent fashion when heated, underscoring the delicate balance that must be struck using such a denaturation approach. Nanotoxoids fashioned from α-hemolysin inserted into RBC nanosponges, on the other hand, were completely safe both in vitro and in vivo without the need for denaturation. When administered into mice, the nanotoxoid formulation consistently outperformed a heat-denatured toxin formulation, which ultimately translated to improved survival and reduced skin lesion formulation in animal studies involving intravenous and subcutaneous challenge, respectively, of bolus toxin. The approach has been further demonstrated to promote germinal center formation, indicating the ability of nanotoxoids to induce B cell maturation, and can significantly reduce bacterial burden in a live MRSA challenge model.[87]
Figure 5.
RBC membrane-coated nanotoxoids for antivirulence vaccination. a) Nanotoxoids are fabricated by inserting pore-forming toxins into RBC membrane-coated nanoparticles, a process that neutralizes their toxicity. Reproduced with permission.[86] Copyright 2013, Nature Publishing Group. b) Without protective immunity, subcutaneous injection of MRSA bacteria will cause the formation of skin lesions. c) After immunization, the immune system produces antibodies that can neutralize toxins and lessen cell damage at the site of infection, reducing bacterial colonization and invasiveness. Reproduced with permission.[87] Copyright 2016, Wiley-VCH.
The concept of nanotoxoids has recently been expanded to be adapted for on-demand fabrication using naturally derived bacterial secretions.[88] A challenge in the design of antivirulence vaccines is that oftentimes bacteria will secrete a multitude of toxins, whereas most vaccines train the immune system against only one antigen. This can ultimately compromise efficacy, resulting in an inability to effectively combat live bacterial infection. The use of individual toxins also requires prior knowledge of their function and the ability to purify the toxin either from the natural source or recombinant. At times, even extensive knowledge about a toxin does not guarantee that it can be applicable towards vaccine design. To address this, RBC nanosponges were incubated with hemolytic protein fractions derived directly from MRSA bacteria culture. It was confirmed that, even after washing away unbound proteins, the nanosponges could retain several characteristic toxins, including α-hemolysin γ-hemolysin, and Panton-Valentine leukocidin. It was also shown that nanosponge complexation helped to completely attenuate the toxicity of the hemolytic proteins, preserving both RBCs and dendritic cells. For the protein fraction itself, even extensive and harsh heat denaturation could not completely remove the original toxicity. Multi-antigen nanotoxoids prepared from nanosponges complexed with the hemolytic proteins were further demonstrated to be safe in vivo and could induce significant germinal center formation. Importantly, elevated antibody titers were demonstrated for all three toxins compared with the heat denatured formulation. Finally, in models of both skin infection and bacteremia, vaccination with the multi-antigen nanotoxoid formulation significantly decreased the burden of disease. This style of on-demand nanotoxoid fabrication has the potential to be expanded to many other types of bacteria using different kinds of cell membranes or protein preparations.
In addition to antibacterial vaccines, RBC-NPs have also been explored in antitumor vaccination schemes. To facilitate delivery, RBC membrane was coated onto PLGA nanoparticles where the polymer was pre-conjugated to a peptide sequence found in hgp100, a melanoma-associated antigen.[89] By employing a thiol bond for linking the peptide antigen, the antigen release was sensitive to reducing environments, which could potentially aid in intracellular antigen delivery. The particle was further functionalized with a mannose group via the lipid-insertion technique to more efficiently localize to antigen presenting cells in vivo. Finally, a toll-like receptor (TLR)-4 agonist, monophosphoryl lipid A (MPLA), was included as an immunological adjuvant and was able to facilitate dendritic cell maturation. In a prophylactic vaccination scenario, formulations were administered three times before challenge, and the targeted RBC-NP formulation with MPLA successfully prevented tumor occurrence in a B16-F10 tumor model. Further, the formulation demonstrated significant ability to control tumor growth in a therapeutic scenario, leading to reduced primary tumor growth and metastatic lesion formation. This efficacy was correlated to enhanced T cell responses. Finally, it was demonstrated that, despite the inclusion of an adjuvant with RBC membrane material, the approach was safe and did not generate autoimmunity against endogenous RBCs.
3.5 Detection
While examples are currently limited, membrane-coated particles have also been employed for biodetection schemes. In one example, RBC-NPs have been employed to bind and enrich influenza viruses.[90] To facilitate viral entry into cells, virus attachment to cells is initiated through interaction between hemagglutinin on the virus surface and sialic acid on cell membranes. It was proposed that RBC-NPs could take advantage of RBC surface sialic acid to also bind to the viruses. RBC membrane was first coated onto superparamagnetic iron oxide-containing PLGA cores, then immunogold staining and electron microscopy was used to confirm the core-shell structure and an abundance of sialic acid moieties on the surface of the coated particles. Upon mixing of influenza viruses and the RBC-NPs, both dynamic light scattering and nanoparticle tracking analysis showed population size increases indicative of particle binding, a phenomenon that was not observed during incubation of the viruses with PEGylated nanoparticles. Application of a magnetic field was subsequently used to separate out and enrich bound viruses. This extracted sample could then be used for different practical applications such as titer studies, plaque assays, and polymerase chain reaction with enhanced signal due to viral enrichment during the isolation process. Such viral isolation and enrichment are valuable for research and diagnostics on low concentration samples or with low sensitivity assays.
RBC nanosponges have also been used to detain, enrich, and identify unknown cell-specific effector proteins secreted by pathogens.[91] For this endeavor, human and mouse RBCs were used to make RBC nanosponges, along with mouse macrophage-coated nanosponges. These particles were incubated with the supernatant of pathogens in order to bind any cell membrane-targeted virulence factors that were present. Loaded nanosponges were then purified out from unbound components, digested, and the proteins were precipitated out and processed for identification using a quantitative mass spectrometry technique. With this “Biomimetic Virulomics” workflow, GAS-secreted virulence factors against human RBCs were enriched and identified; this included known RBC-attacking toxins, as well as proteins with currently no well-defined function. Additionally, the technique was also applied to analyze the affinity of protein secretions from Schistosoma mansoni eggs towards mouse RBCs and macrophages, demonstrating different binding profiles depending on the membrane type. In the future, this workflow can be broadened using other types of cell membrane-coated nanosponges to identify cell-specific virulence factors produced by almost any pathogen in a high throughput and precise manner.
4. Platelet Membrane-Coated Nanoparticles
With the success of RBC-NPs, other types of blood cells with unique functionalities have also been investigated as membrane sources. One important cell type that has been explored is platelets, which are anuclear fragments from megakaryocytes. The main function of platelets is maintaining hemostasis, as they are naturally recruited to sites of vascular injury to trigger a cascade that leads to clot formation, starting the healing process. Additionally, platelets have various other functions and have been implicated in the pathogenesis of a variety of diseases, ranging from cancer and atherosclerosis to bacterial infections. Like the immunomodulatory markers on RBCs, these disease-relevant platelet functions are largely a consequence of their surface marker expression, which can be transferred onto nanoparticles via membrane coatings.
4.1 Drug delivery
In the first instance of using platelet membrane to coat nanoparticles, a polymeric PLGA core was employed (Figure 6).[24] Platelet membrane was obtained using a repeated freeze-thaw process, and coated onto the polymeric cores, forming platelet membrane-coated nanoparticles (PNPs). Physicochemical characterization showed increases in size and zeta potential as indicators of successful coating, which was further confirmed by the characteristic core-shell structure shown by TEM. Using immunogold staining for extracellular CD47, it was demonstrated that the membrane was coated onto the cores largely in the right-side-out orientation. Importantly, it was confirmed that the resulting PNPs carried the entire array of platelet surface markers on their surface, including important immunomodulatory proteins as well as those implicated in binding interactions. These proteins, specifically the collagen binding proteins and CD47, were shown to retain their functionality. The coated nanoparticles were confirmed to bind human type IV collagen via membrane glycoprotein receptors, which is one of the major functions of platelets. They also had reduced macrophage uptake compared with bare nanoparticles, an effect that was reduced by blocking the CD47 present on the surface, and the membrane coating also reduced complement activation. Prior to in vivo use, it was confirmed that potentially thrombogenic compounds normally present within platelets were not present in the final formulation, leading to reduced concerns of spontaneous activation and clotting of endogenous platelets. Further, the PNPs were stable both in solution and after reconstitution from a lyophilized state, ensuring their suitability for injection even after extended storage. Finally, the particles did not lead to any appreciable toxicity in a blood chemistry panel.
Figure 6.
Platelet membrane-coated nanoparticles (PNPs) for biointerfacing. Nanoparticles coated with platelet membrane can utilize a unique set of transferred surface integrins and markers to evade the immune system and bind to sites that naturally recruit platelets. PNPs can deliver antineoplastic drugs to damaged vasculature by binding to exposed collagen and can kill pathogens by binding to them and releasing loaded antibacterial drugs. Reproduced with permission.[24] Copyright 2015, Nature Publishing Group.
To prove the applicability of these particles towards the treatment of diseases, two different animal models were employed. In the first, DTX was loaded into the PLGA cores using a co-preciptation method and used to treat post-angioplasty restenosis. Coronary angioplasty is an important procedure that can manually clear occluded vessels, but commonly causes vascular injury. The intimal layer often dramatically thickens in response and prevents flow through the vessels, causing restenosis. In a rat model of angioplasty-induced arterial injury, the PNPs were shown to target damaged vasculature in vivo and could be retained at the site for over 120 hours, while intact arteries did not appreciably bind the particles. The extended delivery of DTX by PNPs significantly decreased the overgrowth of the intimal layer in the DTX-loaded PNP group, whereas unloaded PNPs and free DTX were all similar to the untreated group in developing restenosis. The ability of the PNPs to bind to exposed collagen may also have implications in the future for the direct treatment of atherosclerosis, in which fatty plaque buildup revolves around collagen, smooth muscle cell and macrophage proliferation, and arterial damage.
In the second model, antibiotic resistant MRSA were employed. The bacteria are known to express a serine-rich adhesin for platelets, and oftentimes bacteria will bind to platelets to act as a shield and prevent detection by the immune system. By incubating PNPs with MRSA in vitro, binding was visually confirmed by scanning electron microscopy as well as by flow cytometric analysis. Afterwards, the antibiotic vancomycin was loaded into the particles using a double emulsion technique. Vancomycin dissolved in basic solution was sonicated with PLGA to form the first emulsion, then sonicated again in an aqueous solution to form a water/oil/water emulsion. The platelet membrane coating around the vancomycin particles allowed for increased binding, better targeting of the antibiotic to the bacteria, and improved bactericidal efficacy in vitro. In vivo, a systemic infection model was employed. Mice were challenged with MRSA252 bacteria and subsequently treated with intravenous injections of the vancomycin-loaded nanoparticles. It was demonstrated that the PNP formulation consistently outperformed both free drug as well as drug loaded into RBC-NPs. Notably, the particles outperformed free drug, which was administered at a 6 times higher dose. The improved efficacy at a drastically lower drug dose highlights the significant impact of targeted delivery and its implications for addressing hard to treat bacterial infections.
With their relevance in tumorigenesis, platelet membrane-coated nanocarriers have also been widely used for cancer drug delivery. In the first example, platelet membrane was coated around DOX-loaded nanogels.[92] The nanogels were fabricated via a single emulsion method by mixing acrylamide monomers and crosslinkers in the organic phase with an aqueous phase containing DOX, hexane, and surfactants. During the mixing of the two phases, tetramethylethylenediamine was added to initiate the polymerization of the acrylamide, thus forming nanogels encapsulating DOX. An acid-labile crosslinker was selected to bestow environmental sensitivity to the final formulation, which translated to the increased release of DOX in lower pH solutions in vitro. The formulation was further functionalized with tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) to further induce cell death via binding with death receptors on cancer cells. The combination of DOX and TRAIL in the nanoparticle formulation led to a potent formulation against a human breast cancer cell line in vitro, due to the synergy of inducing apoptosis using both intrinsic and extrinsic pathways. In vivo, the membrane-coated formulation demonstrated enhanced tumor targeting, likely due to the presence of P-selectin on the nanoparticle surface, which targets the overexpressed CD44 on the breast cancer cells. Finally, in an MDA-MB-231 tumor xenograft model, the nanoformulation was able to strongly control tumor growth, with almost no observed growth over the observation period, and significantly reduced the number of metastatic nodules. In both cases, efficacy required the platelet membrane coating, highlighting its ability to specifically deliver drugs to the target site of interest using natural targeting ligands found on the original cell.
In another example of cancer treatment, platelet-functionalized silica particles were used to achieve targeted delivery to circulating tumor cells.[93] In the work, the authors took advantage of the fact that cancer cells in the bloodstream can promote thrombosis and bind to platelets via fibrin deposition to evade destruction by immune cells. Using a sucrose gradient method to isolate platelet membrane-derived vesicles, the purified material was coated onto silica particles via (3-aminopropyl) triethoxysilane (APTES) functionalization. The resulting coated particles demonstrated a rough morphology compared to the relatively smooth exterior of uncoated particles. Immunostaining was used for both flow cytometry and fluorescent imaging to confirm the preservation of platelet proteins markers and glycans on the particles. To model the adhesion of the coated particles to fibrin under blood flow conditions, the particles were run through a fibrin-coated microtube. Membrane-coated particles were found to strongly adhere to the fibrin in the presence of calcium, confirming the thrombus-targeting property of the particles even in a fluid environment. To incorporate a therapeutic payload, TRAIL was attached to the particle surface through biotin-streptavidin interaction. The process of conjugation did not affect the potency of the ligand, and the particles could kill cancer cells in a dose-dependent manner. In vivo, it was demonstrated that in a circulating tumor cell model where mice were injected with cancer cells followed by the particles, membrane functionalization enabled efficient colocalization of the two. Finally, the same procedure was used with a luciferase-expressing tumor cell line to test efficacy, and drastically reduced luciferase signal was found in the lungs of mice treated with the membrane-coated particles functionalized with TRAIL.
In the final example, engineered nanoplatelets were used to treat multiple myeloma.[94] Using an acid-responsive polymeric nanoparticulate core made of dextran, the small molecule inhibitor bortezomib was loaded and platelet membrane was coated onto the surface. In vitro, the platelet membrane-functionalized formulation killed cancer cells in a bortezomib dose-dependent manner, outperforming the non-functionalized drug-loaded nanoparticles. The nanoparticle surface was additionally functionalized with alendronate to bestow bone-targeting functionality, enabling enhanced accumulation of the particles near the cancer site. The bone-targeted formulation could bind efficiently to calcium-rich hydroxyapatite in vitro and showed strong signal in mouse femur tissues and bone marrow. Finally, the particles were decorated with tissue plasminogen activator (tPA), which can help to dissolve dangerous clots that arise as a result of multiple myeloma treatment. The enzyme retained its functionality and was able to maintain activity in circulation longer than free tPA. Further, untreated mice injected with fibrinogen and thromboplastin developed lung clots, but treatment using PNPs with tPA was able to significantly reduce thrombosis. Efficacy of the complete nanoformulation was evaluated in a mouse model of multiple myeloma. The targeted platelet membrane-coated formulations, both with and without tPA, strongly enhanced survival and induced more apoptosis in the bone marrow compared to other groups. However, subsequent histological analysis of lungs showed less thrombosis for the tPA-containing formulation, demonstrating the benefit of combining multiple treatment modalities into a single nanoparticle.
4.2 Imaging and photoactivatable therapy
The ability of PNPs to specifically target many disease sites gives them incredible utility for photo-based applications. To this end, magnetic iron oxide nanoparticles have been coated with platelet membrane and used for combinatorial imaging and photothermal therapy of tumors (Figure 7).[95] After confirming coating via physicochemical characterization and TEM, it was demonstrated that the platelet membrane and iron oxide nanoparticles colocalized well upon cellular uptake, indicating the stability of membrane coating. After coating, the iron oxide retained its superparamagnetic properties, suggesting little impact of the membrane layer on MRI efficiency. In vitro, the membrane-coated particles demonstrated minimal macrophage uptake similar to RBC-NPs, and significantly enhanced uptake by MCF-7 cancer cells. In vivo, this immune evasion and increased cancer cell binding translated to long particle circulation and improved tumor targeting in an MCF-7 xenograft model, shown through pharmacokinetic and biodistribution studies, respectively. The tumor accumulation of the nanoparticles proved useful during MRI, enabling obvious darkening in the tumor site and exemplifying their utility in cancer diagnosis. In addition to diagnosis, the work also demonstrated the photothermal killing capacity of the nanoparticle formulation. Upon NIR laser irradiation, the PNPs exhibited cytotoxicity in vitro, and significantly enhanced tumor temperature in vivo due to the high local concentration of the nanoparticles at the irradiation site. This effect could be further enhanced by applying a magnetic field near the tumor. After the single treatment, there was significant efficacy against the MCF-7 tumor xenografts with minimal growth over thirty days. The formulation was also demonstrated to have little effect on blood chemistry and did not increase the number of myeloid-derived suppressor cells or serum antibody levels even after repeated administrations.
Figure 7.
Platelet membrane-coated magnetic nanoparticles for combination MRI imaging and photothermal therapy. The retention of self-marker CD47 on the platelet membrane coating reduces the macrophage uptake of PNPs, allowing for long circulation of the particles and passive tumor accumulation via the enhanced permeation and retention effect. The high concentration of the coated iron oxide cores in the tumor can be used for MRI imaging of the tumor location and photothermal therapy for cancer cell killing. Reproduced with permission.[95] Copyright 2017, Wiley-VCH.
4.3 Detoxification
In the final example of PNP applications, immune thrombocytopenia purpura (ITP) was addressed by using the nanoparticles to bind and remove pathological anti-platelet antibodies that drive progression of the disease (Figure 8).[96] The autoantibodies arising from the disease cause platelet destruction, which can lead to uncontrolled and potentially lethal bleeding if platelet counts drop to unsafe levels. Currently, most therapies to address ITP are nonspecific, and they often have significant side effects that can be worse than the disease itself. As an alternative treatment strategy, it was proposed that PNPs be used as decoys for the autoantibodies to bind to, sparing healthy platelets. In vitro, it was demonstrated that the nanoparticles could efficiently bind the antibodies, which was not observed for PEGylated nanoparticles. At increasing dosages, the particles could prevent autoantibodies from attaching to healthy platelets, both in preincubation and co-incubation settings. Using a mouse model of antibody-induced thrombocytopenia, it was demonstrated that PNPs could help to preserve platelet counts, both when preincubated together with anti-platelet antibodies and when administered therapeutically after establishment of the disease. Finally, using a tail-tip excision bleeding model, it was demonstrated that mice receiving treatment with PNPs had a normal bleeding response. However, untreated mice or those treated with PEGylated nanoparticles had difficulty with clot formation due to low platelet numbers, as indicated by a longer bleeding time. Along with using RBC-NPs to address autoimmune anemia, the current work further validates the concept of using antibody decoys to address autoimmune diseases mediated by antibodies against endogenous cells.
Figure 8.
Platelet membrane-coated nanoparticles for clearance of pathological antibodies. a) Platelet-derived membrane vesicles are coated onto polymeric nanoparticle cores. b) In autoimmune thrombocytopenia, endogenous antibodies against platelets facilitate their clearance by macrophages. c) Platelet membrane-coated nanoparticles can serve as decoys and bind to anti-platelet antibodies. Absorption of the pathological antibodies spares native platelets, reducing the severity of disease. Reproduced with permission.[96] Copyright 2016, Elsevier Ltd.
5. White Blood Cell Membrane-Coated Nanoparticles
Membrane derived from white blood cells (WBCs), the last major category of blood cells, has also recently been used for nanoparticle coating. Leukocytes help to carry out immune functions, and consist of many different subsets including macrophages, dendritic cells, B cells, T cells, neutrophils, and others. Compared with RBCs or platelets, WBCs are nucleated and have more complex intracellular components, which necessitates more complicated workflows for obtaining their membranes. However, WBCs have unique properties that enable site-specific targeting, especially their interactions with tumors or vascular abnormalities, and thus their membrane can carry exceptional utility that makes their use worthwhile.
5.1 Drug delivery
WBC membrane-coated nanoparticles (WBC-NPs) have commonly been proposed for use in cancer drug delivery. One such rationale is that leukocytes can target sites of inflammation, which has long been linked to some cancers and tumor vasculature remodeling. In one example, membrane derived from leukocytes were obtained via a sucrose density gradient purification process and coated onto the surface of nanoporous silicon microparticles (Figure 9).[97] The surface of the bare particles was functionalized with the positive APTES functional group, which enabled stable interaction with the membrane coating material. The successful coating of the membrane onto the surface of the particles was visualized by electron microscopy, and it was shown that the coated particles could interact with wheat germ agglutinin to indicate the presence of important surface glycans. The coated particles were also less subject to antibody opsonization and serum protein adsorption compared to bare particles. Particles coated with J774 or THP-1 macrophage cell membranes were particularly adept at preventing uptake when incubated with the cell line from which the membrane was derived. The WBC-NPs also preferentially bound to activated endothelium via lymphocyte function-associated antigen 1 (LFA-1), as evidenced by the clustering of endothelial intercellular adhesion molecule 1 (ICAM-1) around the nanoparticles. The ability of the nanoparticles to transverse across layers of inflamed endothelium like their cellular counterparts was confirmed in a transwell chamber assay, with the coated nanoparticles showing a fourfold increase in transportation compared to the bare nanoparticles. The nanoporous silicon microparticles could be loaded with DOX by resuspension of the particles in the drug solution and mixing. When loaded with DOX, the membrane coating enabled the particles to traverse across the endothelial layer to preferentially kill cancer cells at the bottom of the well. In contrast, free drug or drug-loaded uncoated particles both preferentially killed the endothelial cells instead of moving across the barrier. In vivo, the coatings helped to prevent liver uptake as well as phagocytosis by Kupffer cells. This immune evasion, along with the particle’s tumortropism through inflamed endothelium, led to more accumulation in B16 mouse melanoma tumors than uncoated particles, with intravital microscopy revealing the particles residing within the tumor microvasculature.
Figure 9.
Leukocyte membrane-coated particles. Porous silicon microparticles can be functionalized with positively-charged surface groups to facilitate surface coating with leukocyte membrane. The coated particles retain the ability to home to tumors and transverse across inflamed endothelium using surface markers inherent on white blood cells. Reproduced with permission.[97] Copyright 2012, Nature Publishing Group.
Besides enhanced immune evasion and inflammation targeting, it is hypothesized that WBC membrane can also help target tumors through specific receptor-ligand binding. To investigate this, monocyte membrane was coated around PLGA nanoparticles loaded with DOX.[98] The presence of CD49d, a surface marker and primary ligand to vascular cell adhesion molecule 1 (VCAM-1), was first confirmed on the coated particles through western blotting, and its functionality as a targeting mechanism was then investigated in vitro. When incubated with MCF-7 cancer cells, the coated nanoparticles were taken up by more cells when compared to uncoated particles. However, upon incubation with mouse skeletal myocyte cells, which lack VCAM-1 and many other cell adhesion molecules, little difference was observed between the coated and uncoated particles. Finally, it was demonstrated that the nanoformulation with membrane coating better killed cancer cells in vitro compared with unfunctionalized particles, likely due to the enhanced cell uptake provided by the adhesion receptor-ligand interactions.
In a later example, mesoporous silica nanocapsules camouflaged in macrophage membrane were employed for targeted tumor treatment in vivo.[99] First, mesoporous silica-coated gold nanoparticles were fabricated, followed by removal of the gold cores. The macrophage membrane was then coated onto the hollow nanoparticles and the coating was confirmed by electron microscopy, as well as by both size and zeta measurements. It was confirmed that the macrophage membrane could decrease uptake by macrophages, and also allow for longer circulation with decreased organ uptake compared with uncoated particles. Subsequently, DOX was used as a model drug to load inside of the nanoparticles. The loading was confirmed using UV-visible spectroscopy, and it was shown that the drug could be efficiently delivered by the nanoparticles into murine 4T1 cells. In tumor-bearing mice, the coating helped to significantly decrease liver and spleen uptake while increasing tumor uptake, with particle signal still colocalized with the tumor up to 72 hours after administration. Combined with the intracellular DOX delivery, treatment with the particles resulted in impressive control of tumor growth over time.
While the previous works focused on targeting primary cancer sites, further use had been found for WBC-NPs in addressing metastatic disease. In one example, liposomes loaded with the anticancer drug emtansine were coated with membrane derived from RAW264.7 mouse macrophages.[100] Lipophilic emtansine was encapsulated into liposomes by adding the drug to 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE) and distearoyl phosphatidylethanolamine (DSPE)-PEG during liposome synthesis, achieving an encapsulation efficiency of 96.7%. After extrusion of the liposomes with macrophage membrane, the presence of integrins α4 and β1, which collectively form α4β1 and can target VCAM-1 expressed by some cancer cells, was confirmed on both the source RAW264.7 cells as well as on the final nanoformulation. VCAM-1 was also confirmed on murine 4T1 breast cancer cells, a highly metastatic cell line used to model the progressive spread of metastases in human mammary cancers. It was shown that the membrane-coated liposomes could efficiently target the cancer cells in vitro and that the effect was abrogated by blocking α4β1, demonstrating the cancer cell affinity and specificity of the membrane coating. In line with previous studies, it was shown that regular liposomes were highly taken up by macrophages, whereas the coated formulation had reduced uptake. Both immune evasion and VCAM-1 targeting enabled the coating to greatly enhance blood residence time and lung uptake in a metastatic tumor model. After injection, internalization by cancer cells was confirmed by immunofluorescent histological analysis of lung tissue. Finally, in a therapeutic scenario, the membrane-coated formulation was best able to prevent the formation of metastatic lung nodules. In contrast, free drug had little effect, while control liposomes and coated liposomes that were blocked by α4β1 antibody had an intermediary effect.
In another example, neutrophil membrane was used to coat PLGA nanoparticles loaded with carfilzomib, a second-generation proteasome inhibitor.[101] It has been demonstrated that neutrophils play a role in the formation of premetastatic niches and can also interact with circulating tumor cells. These interactions are mediated by a variety of surface marker interactions between the neutrophils and the cancer cells. After successfully coating the loaded PLGA cores, it was confirmed that key adhesion surface markers such as L-selectin, LFA-1, and β1 integrin were retained. The membrane-coated formulation was able to better adhere to 4T1 breast cancer cells under shear conditions similar to that of blood circulation, and was also internalized by different endocytic pathways compared with uncoated nanoparticles. The improved cellular binding and uptake pathway provided by the neutrophil membrane coating allowed for accelerated apoptosis of 4T1 cells when sheared with the coated particles in blood, compared to treatment with free drug or drug-loaded uncoated nanoparticles. An in vivo flow cytometry experiment was designed to showcase circulating tumor cell targeting, where mice were injected intravenously with cancer cells expressing green fluorescent protein, followed by dye-loaded nanoparticles. The artery of the ear was visualized with a laser and concurrent fluorescent signal peaks in two different channels were recorded as an indication of neutrophil membrane-coated nanoparticle and circulating tumor cell clusters. To confirm the premetastatic niche targeting capability, human umbilical vein endothelial cells (HUVECs) were activated by TNFα, and it was shown that the membrane-coated nanoparticles could much more efficiently target these cells. Once an antibody against adhesion molecule ICAM-1 was introduced into the system, the enhanced targeting effect was diminished, confirming that the interaction of markers between the neutrophil membrane and endothelium was necessary for targeted binding and thus not observed for bare particles. Particle homing to premetastatic niches was further demonstrated in a metastatic 4T1 murine model. Intravenous injection of 4T1 cancer cells caused enhanced lung expression of laminin, the main target of β1, in preparation for metastasis formation. Intravenous injection of neutrophil membrane-coated nanoparticles in this premetastatic model resulted in substantial and widespread particle accumulation in the laminin-rich areas compared to the relatively sparse clustering of uncoated nanoparticles in the lungs. The ability to target established metastasis was also confirmed, as the nanoformulation signal localized well with the bioluminescent signal from luciferase-expressing 4T1 cells residing in metastatic lung nodules. Finally, in a treatment model of early metastasis, significant inhibition of lung nodule formulation and immune-suppressing neutrophil presence was observed for mice treated with the neutrophil membrane-coated nanoformulation. Similar results were found in the treatment of mice with established metastases, with significantly reduced metastatic nodules and an increased degree of cancer cell apoptosis being observed only in mice treated with the coated formulation.
Beyond basic drug delivery applications, synergistic combination therapies have also been demonstrated using WBC-mimicking nanoparticles. Localized low-dose irradiation (LDI) was used to prime tumor sites for targeting by T cell membrane-coated nanoparticles as a potential means of treating gastric cancer.[102] PLGA particles loaded with PTX as a model drug were extruded with cytotoxic T cell membrane derived from human blood samples. T cell markers such as LFA-1 and CD3z were confirmed to be present on the derived membranes, and the immune evasion ability of the final coated nanoparticles was indicated via reduced phagocytosis by THP-1 human monocyte cells. The loaded drug maintained its activity after the synthesis process, as coincubation of the particles and MKN-45 cancer cells resulted in dose dependent cytotoxicity. Interestingly, in an in vivo xenograft model, localization of the membrane-coated nanoparticles to the tumor was significantly enhanced when the tumor was first treated with low-dose irradiation, compared to tumor accumulation of the nanoparticles without irradiation. Immunohistochemical staining for ICAM-1 revealed that the adhesion molecule was upregulated on the tumor vessels after irradiation, which can enhance particle accumulation by providing more ligands to bind with the LFA-1 present on the coated particle surface. In a treatment model, LDI was given to tumor-bearing mice one day before the first treatment, followed by two injections of nanoparticles given one week apart. The combination of LDI and the membrane-coated PTX nanoparticles led to nearly complete control of tumor growth, with 40% of the mice achieving complete remission. Either treatment alone was significantly less effective, supporting the idea that taking advantage of the biological response to LDI can enhance the binding interaction between the tumor and T cell membrane-coated nanoparticles, and subsequently enhance antitumor efficacy.
5.2 Imaging and photoactivatable therapy
Like with RBC and platelet membranes, the ability of WBC-NPs to target specific locations has led them to be utilized for imaging and photothermal therapies. In the first example, gold nanoshells were camouflaged using macrophage membrane (Figure 10).[103] The nanoshells were fabricated using a mesoporous silica nanoparticle templating approach, and the particles were loaded with the NIR fluorescent dye, Cy7. When coated with macrophage membrane, the particles displayed enhanced uptake when incubated in vitro with 4T1 mouse breast cancer cells, and when irradiated, the nanoparticles could efficiently kill the cells. Further, it was demonstrated that the macrophage membrane coating could significantly prolong the circulation of the nanoparticles compared with bare particles, which correlated with enhanced tumor uptake in a murine xenograft model of 4T1. Combining the administration of this formulation with laser irradiation led to near complete control of tumor growth. Notably, the uncoated nanoparticles, which demonstrated poor circulation and tumor accumulation, only had a modest effect. Histological analysis on organs after treatment revealed the absence of any significant damage caused by the formulation, suggesting a favorable safety profile.
Figure 10.
Macrophage membrane-coated gold nanoshells for photothermal therapy. a) Macrophage cells are used as the source for membrane vesicles, which can be used to form a coating around gold nanoshells. b) The macrophage membrane coating can shield gold nanoshells from macrophage uptake and facilitate enhanced tumor accumulation. The gold nanoshell cores can generate hyperthermia upon laser irradiation for tumor ablation. Reproduced with permission.[103] Copyright 2016, American Chemical Society.
In a later example, β-NaYF4:Er3+,Yb3+ UCNPs were also coated with macrophage membrane.[104] After performing the coating process, a distinct membrane layer could be visualized under TEM, which provided the particles with stability in both PBS and FBS. Upon excitation with an NIR laser, the particles exhibited a strong green fluorescence, showing retention of the upconversion properties of the core after coating. Compared with bare UCNPs, the membrane-coated versions also had better compatibility with cells in vitro, exhibiting decreased toxicity. The macrophage membrane enabled more efficient targeting and uptake in MCF-7 cancer cells in vitro, confirmed via both flow cytometry and inductively coupled plasma atomic emission spectroscopy (ICP-AES) analysis of Yb3+ content. Like in the previous example, the membrane coating helped to increase the circulation time of the particles and significantly enhanced tumor uptake in a xenograft model of MCF-7, as indicated with the strong upconversion luminescence signal in tumors treated with the coated nanoparticles upon irradiation. Finally, the toxicity of the particles was evaluated. No significant body weight change was observed over the course of fifteen days, and major parameters for liver and kidney function were consistent with baseline levels. Further, none of the major hematological parameters, including WBC, platelet, and RBC counts were affected.
5.3 Detoxification
Binding and recognition of pathogen-associated molecular patterns and cytokines is a key protective role of leukocytes, and can be harnessed by WBC-NPs as a mechanism for endotoxin removal and inflammation reduction. One such use is for the treatment of sepsis, a life-threatening complication of systemic bacterial infection that is triggered by the release of bacterial endotoxins and the overproduction of proinflammatory cytokines. In a recent work, macrophage membrane was coated onto PLGA nanoparticles to absorb the endotoxin lipopolysaccharide (LPS) along with proinflammatory cytokines for sepsis treatment.[105] Western blots confirmed the presence of key cytokine-binding receptors like CD126, CD120a/b, and CD119 that can sequester IL-6, TNF, and interferon (IFN)-γ, respectively. These receptors remained functional after coating, and the coated nanoparticles removed cytokines from solution in a concentration-dependent manner. Western blots of the membrane coated-nanoparticles also showed a retention of surface proteins critical for lipopolysaccharide (LPS) binding, such as CD14 and TLR-4. When incubated with LPS, it was found that 1 mg of nanoparticles could remove 62.5 ng of the endotoxin, a phenomenon that was reduced in the presence of anti-CD14 or anti-TLR-4 antibodies. To show the neutralization of LPS, different cell lines were incubated with LPS with or without macrophage-mimicking nanoparticles. It was found that the cultures treated with the nanoparticles had less LPS-induced cellular effects like TLR-4 activation, intracellular nitric oxide production, and E-selectin expression. This protective efficacy was not observed for cells treated with LPS and RBC-NPs or PEGylated nanoparticles, showing that the LPS neutralization is a specific property of the macrophage membrane. Similar results were found in vivo, as macrophage membrane-coated nanoparticles prevented an increase in TNF or IL-6 cytokines in mouse plasma and greatly improved survival after an intravenous injection of LPS, while the RBC membrane-coated and PEGylated versions of the nanoparticles did not show efficacy. Finally, the therapeutic potential of the nanoformulation was tested in a mouse bacteremia model. A lethal intraperitoneal injection of Escherichia coli was administered to mice, but treatment with macrophage membrane-coated nanoparticles conferred survival for 40% of the mice, and significantly decreased bacterial burden in nearly every organ.
5.4 Detection
The biological functions of WBCs, such as cancer cell targeting and immune evasion, can be leveraged in the unique design of new nanoscale platforms for detection and isolation purposes. To this end, magnetic iron oxide nanoclusters were coated with leukocyte membrane as a means of providing facile immunofunctionalization (Figure 11).[106] The cells were cultured such that azide groups were metabolically incorporated into the membrane phospholipids, and the resulting functionalized membrane could be efficiently conjugated to dibenzocyclooctyne-modified antibodies via click chemistry. After coating, it was demonstrated that the nanoparticles could still be efficiently captured by a magnetic field, and further functionalization with antibodies against epithelial cell adhesion molecule (EpCAM) was confirmed by immunofluorescence staining. The particles could efficiently bind and capture cancer cells that highly express EpCAM, including MCF-7, HepG2, and Caco2 cell lines, with a capture efficiency of around 95%. This binding was exclusive to EpCAM expression, as cells with little expression of EpCAM did not bind. It was proposed that this strategy of decorating antibodies onto a membrane surface was superior to using antibody-conjugated particles without membrane coating, as the membrane fluidity of the coated particles can allow the antibodies to dynamically form multivalent interactions with the target cells for enhanced binding efficacy. Indeed, immobilization of the membrane fluidity via crosslinking had a negative impact on binding efficiency of the particles. Further, the membrane with antibody functionalization helped to decrease nonspecific uptake by macrophages, reducing the binding and collection of undesired cells in a cancer cell-spiked sample. Finally, it was demonstrated that the membrane-coated particles demonstrated better capture efficiency of MCF-7 cells in RBC-lysed human blood compared with a commercially available magnetic bead, and with less immune cell contamination.
Figure 11.
Antibody-decorated leukocyte membrane-coated magnetic nanoclusters for circulating tumor cell enrichment. Azide-functionalized leukocyte membrane can be coated onto iron oxide nanoclusters and subsequently bind modified antibodies onto the membrane surface. Particles decorated with an anti-EpCAM antibody attach to circulating tumor cells in blood samples, and the bound target cells can then be isolated by magnetic extraction. The leukocyte membrane coating prevents nonspecific binding to other white blood cells in the sample for reduced contamination of the purified circulating tumor cells. Reproduced with permission.[106] Copyright 2016, Wiley-VCH.
6. Cancer Cell Membrane-Coated Nanoparticles
Moving beyond cells originating from the blood, another major source of membrane can be from malignant cells. Aberrant cells can display many properties that make them well-suited for use with the cell membrane coating technology. Because of their robustness, it is easy to culture and obtain their membrane material in vitro. In particular, there are also unique properties exhibited by cancer cells, such as the ability to self-target, which can be leveraged for cancer drug delivery and imaging purposes, and antigenic display, which can be taken advantage of for immune modulation.
6.1 Drug delivery
One of the most unique aspects of cancer cells that has been leveraged as part of the membrane-coated nanoparticle technology is there ability for homotypic targeting. This concept was first demonstrated using membrane from melanoma cells coated onto PLGA nanoparticle cores (Figure 12).[25] The coating was successfully confirmed by slight increases in size and zeta measurements after coating, as well as directly by TEM imaging. Further, it was demonstrated that the cancer cell membrane-coated nanoparticles (CCNPs) had protein expression profiles close to that of the purified cell membrane, and membrane elements were selectively purified and enriched throughout the fabrication process compared to raw cancer cell lysates. The particles were stable over time and demonstrated good colocalization of membrane and core upon uptake by bone-marrow derived dendritic cells, demonstrating the stability of the core-shell structure. To support the concept of homotypic binding, MDA-MB-435 cells, a human melanoma cell line characterized by its propensity to aggregate in clusters, were used to fabricate CCNPs. It was then confirmed by both flow cytometry and fluorescent imaging that the CCNPs had much higher binding to the original cancer cells, whereas RBC-NPs and bare cores had little uptake. This selective uptake was further confirmed when using non-cancerous human foreskin fibroblasts, which had similar levels of uptake of the cores compared with the membrane-coated particles.
Figure 12.
Cancer cell membrane-coated nanoparticles for anticancer vaccination and homotypic targeting. Polymeric nanoparticles coated with cancer cell membrane can deliver a wide range of cancer surface antigens to immune cells for processing and training against cancer cells. The cancer cell membrane also contains homotypic adhesion molecules that are retained onto the nanoparticles after coating for targeted tumor delivery. Reproduced with permission.[25] Copyright 2014, American Chemical Society.
A later work expanded this homotypic targeting concept for drug delivery using magnetic nanoparticles.[107] Negatively charged magnetic iron oxide nanoparticles were dispersed in a dextran solution and added dropwise to a DOX solution, at which point the positively charged drug adsorbed onto the particles via electrostatic interaction. The DOX-loaded iron oxide nanoparticles were subsequently loaded into membrane derived from a variety of different cancer cell lines. Upon loading, clusters of iron oxide nanoparticles could be observed under electron microscopy. After processing, the particles retained membrane markers while losing many intracellular components, and the membrane material and drug colocalized well upon internalization with the original cancer cells. Further, the DOX was found to be released by the particles in a pH-dependent manner, and the particles did not elicit any acute cytokine production upon intravenous administration. Using a panel of different cells and nanoparticles coated with various types of cell membranes, homotypic and heterotypic binding between the two were assessed by flow cytometry and fluorescent imaging. It was determined that CCNPs were taken up best by the cells from which the membrane coating was derived, and heterotypic binding of coated nanoparticles to mismatched cell lines was minimal. This effect was also observed in vivo in a dual tumor model. Nanoparticles coated with membrane derived from H22 cancer cells preferentially accumulated in H22 tumors in mice, even when the same mouse also had a tumor composed of UM-SCC-7 cancer cells on the other flank. In the same model, preferential accumulation into the UM-SCC-7 tumor was achieved when nanoparticles coated with UM-SCC-7 membrane were administered, demonstrating that nanoparticles of one source cell only efficiently targeted tumors grown from the same source cell. This translated to striking efficacy results when treating the same tumor, and the effect was significantly attenuated when using CCNPs from another source cell. Taking advantage of the core material, a magnetic field could also be applied to guide nanoparticles to the tumor site and further enhance efficacy.
In addition to targeting the primary tumor, the homotypic targeting strategy is also capable of addressing metastasis. In one example, murine 4T1 breast cancer cell membrane was coated onto polymeric nanoparticles loaded with PTX (Figure 13).[108] Membrane antigens such as Thomsen–Friedenreich antigen and E-cadherin, both of which are implicated in the formation of metastasis and homotypic binding, were confirmed via western blot. The surface adhesion molecules CD44 and CD326 were also found present on the membrane surface, both of which help metastatic cells adhere to sites distant from the primary tumor. In vitro, it was shown that the CCNPs preferentially bind to the source 4T1 cells in a similar manner to the previous examples. On the other hand, binding to a control mouse lung fibroblast cell line, as well as uptake by macrophages, was low for the formulation. This increased affinity to the source cell also enhanced the efficacy of the loaded drug, enabling the CCNPs to outperform both free drug and uncoated nanoparticles. In 4T1 tumor-bearing mice, the coated particles preferentially targeted both the tumor and the lungs, a known site of metastasis, compared with uncoated particles. Finally, the formulation exhibited impressive control of tumor growth in a mouse tumor model. There was virtually no tumor growth or lung metastasis formation, and the particles were able to outperform the clinical PTX formulation Taxol.
Figure 13.
Cancer cell membrane-coated nanoparticles for targeted cancer drug delivery. Surface markers like Thomsen–Friedenreich antigen, E-cadherin, CD44, and CD326 can be transferred onto the surface of cancer cell membrane-coated nanoparticles to target to tumors of the same cancer type. When loaded with anticancer drugs like PTX, the CCNPs preferentially bind and release the drugs to cancer cells in the primary tumor as well metastatic tumors. Reproduced with permission.[108] Copyright 2016, Wiley-VCH.
Chemotherapeutic delivery into solid tumors can suffer from drug resistance due to the hypoxic environment. CCNPs have recently been designed to deliver a combination of a chemotherapeutic drug DOX and an oxygen carrier hemoglobin to overcome chemoresistance stemming from tumor hypoxia.[109] MCF-7 cancer cell membrane was coated onto PLGA nanoparticles loaded with DOX and hemoglobin to form dual-loaded CCNPs. The nanoformulation showed homotypic binding properties, with the highest DOX uptake exhibited by the parent MCF-7 cells compared with DOX uptake into other cancerous and noncancerous cells. The CCNPs also showed higher cytotoxicity than the free drug or drug-loaded uncoated nanoparticles. To test the ability of the loaded oxygen to mitigate the effect tumor hypoxia, the dual-loaded CCNPs were incubated with MCF-7 cells in hypoxic conditions. After treatment with nanoparticles, mechanisms responsible for drug efflux such as HIF-1α, multidrug resistance gene 1, and P-glycoprotein were all downregulated. With this oxygen interference and improved cellular uptake due to the membrane coating, more DOX was able to accumulate in the cancer cells than uncoated particles or non-oxygenated particles. Similarly, when administered to tumor-bearing mice, the DOX signal in the tumors of mice treated with CCNPs was significantly higher than that of the uncoated nanoparticles, with the addition of loaded oxygen increasing DOX accumulation by 30% compared to the non-oxygenated coated nanoparticle. As the MCF-7 membrane coating and the oxygen loading were shown to work synergistically to increase DOX uptake into tumor cells, mice treated with the coated, dual-loaded nanoparticles showed significantly controlled tumor growth, with 100% surviving until the end of the study.
Beyond active delivery, the CCNPs have also been combined with photoactivatable techniques to trigger release of the targeted drug on-demand. In this case, 4T1 membrane was coated around gold nanocages that were loaded with chemotherapeutic drug DOX.[110] After confirming successful coating of the nanocages, it was shown that the final particles could cause a marked increase in local temperature upon NIR irradiation. This local heating helped to facilitate drug release by increasing the permeability and fluidity of the cell membrane barrier, significantly quickening the release kinetics compared to samples that were not subject to irradiation. When incubated with the source 4T1 cells, the membrane-coated formulation helped to significantly increase uptake of the DOX due to homotypic binding. The signal of the drug was further amplified upon irradiation, demonstrating triggered release within the cells. This combination also had the best effect in killing the cells, significantly outperforming the free drug. In vivo, tumor-bearing mice administered CCNPs of the same source cell followed by irradiation experienced the highest DOX levels in the tumor tissue. The local temperature at the tumor site was also significantly increased upon irradiation of the tumor after treatment with the membrane-coated formulation due to the targeting and increased local concentration of the nanoparticles. Notably, localization of DOX in the heart was significantly reduced when administered in particulate form versus as a free drug, which translated to reduced heart toxicity upon histological evaluation. Finally, when used to treat tumor-bearing mice therapeutically, the coated nanoformulation paired with irradiation was able to effectively control tumor growth and metastasis, with minimal signs of growth throughout the duration of the experiment.
6.2 Imaging and photoactivatable therapy
The natural ability of CCNPs to exhibit homotypic targeting, as well as to localize to metastatic sites, makes them well-suited for use in diagnostic imaging and phototherapies. For imaging, cancer cell membrane has been coated around UCNPs for highly specific tumor visualization (Figure 14).[111] Much like with other types of membrane, these β-NaYF4:Er3+,Yb3+ UCNPs were readily coated with membrane derived from cancer cells. The resulting particles exhibited lower immune cell uptake and long circulation on par with that of RBC-NPs, while outperforming control particles functionalized with folic acid as a model targeting ligand. Subsequently, a panel of nanoparticles were made from various cancer cell lines and their cellular uptakes by MDA-MB-435 cancer cells were tested. It was demonstrated by flow cytometry that only nanoparticles made using MDA-MB-435 membrane, as well as folate-functionalized nanoparticles, could efficiently be taken up. Further, using a mouse MDA-MB-435 tumor xenograft model and in vivo upconversion luminescence, it was shown that only MDA-MB-435 CCNPs could efficiently localize to the tumor, again outperforming the folate formulation. This improvement was most likely due to the better circulation and tumor avidity of the CCNPs. The particles were demonstrated to be safe, with no major impact on weight change, organ histology, or liver and kidney markers in a blood chemistry panel.
Figure 14.
Cancer cell membrane-coated upconversion nanoparticles for tumor imaging. Upconversion nanoparticles coated with cancer cell membrane have long blood residence due to immune escape, and can specifically target homologous cancer cells in vivo due to adhesion markers present on the cell membrane. When administered intravenously, the cancer cell membrane-coated nanoparticles actively migrate to the tumor site and emit strong luminescence under NIR irradiation. Reproduced with permission.[111] Copyright 2016, Wiley-VCH.
The concept was further expanded to a multi-modal theranostic system, capable of imaging with multiple techniques as well as photothermal therapy. To accomplish this, ICG dye was loaded into PLGA as the core material for CCNPs.[112] In this case, the MCF-7 cancer cell membrane was hybridized with PEG prior to extrusion with the cores in order to form a hybrid coating that can target cancer cells and reduce nonspecific binding between the nanoparticles and serum proteins. After synthesis, the authors confirmed that the fluorescence intensity of the coated nanoparticles was comparable to free ICG, and that the photoacoustic properties were ICG concentration-dependent. The photothermal conversion of the formulation was also tested in vitro, with the nanoparticle-constrained ICG showing higher energy conversion efficiency compared to free ICG. Important markers for homotypic binding and adhesion, including EpCAM, N-cadherin, and galectin-3, were confirmed to be present on the particles and endowed the coated nanoparticles with strong homotypic binding to MCF-7 cells. Upon irradiation of nanoparticle-laden MCF-7 cell cultures, those incubated with the CCNP formulation were almost completely killed, while around 50% of the cells treated with the purely PEGylated control survived. In vivo, the specific tumor targeting capabilities were confirmed both by fluorescence imaging as well as by photoacoustic imaging. Only the CCNP formulation had significant signal in the tumor compared with the free dye and PEGylated controls. Finally, the antitumor efficacy was tested using an MCF-7 xenograft model. Laser irradiation after an injection of coated ICG-nanoparticles caused a local temperature increase at the tumor site that completely eliminated the tumors with no recurrence eighteen days after the single treatment.
The cancer cell membrane targeting approach has also been applied towards improving photodynamic therapy. Due to the importance of oxygen for effective photodynamic therapy, monitoring and identifying oxygen levels in tumor microenvironments can provide valuable information regarding the predicted efficacy of photodynamic therapy. To achieve both a photodynamic effect and oxygen sensing, Pt(II) meso-tetra(4-carboxyphenyl)porphyrin and Zr6 cluster were used to form a porphyrinic-metal organic framework (MOF), and subsequently coated with cancer cell membrane to allow for homotypic targeting and immune cell evasion in the bloodstream.[113] In normoxic oxygen environments, the coated nanoparticles displayed a weak phosphorescence, but with the decrease in oxygen levels, phosphorescence signal increased dramatically and could be easily visualized using a hand-held UV lamp. When incubated with cells, irradiated nanoparticles showed high levels of ROS induction, and as the oxygen level in the culture environment was decreased, the level of ROS decreased in an inverse relationship to the phosphorescence measurements. Functionalization with cancer cell membrane improved the cytotoxicity of the nanoparticles towards cancer cells due to the preferential homotypic uptake, with irradiated nanoparticles in normoxic environments reducing cell viability at much lower doses for 4T1 cells compared to non-cancerous COS7 cells. In vivo, 4T1 cancer cell membrane-coated MOFs could effectively localize to 4T1 tumors, with particles localizing equally to both tumors in a dual tumor-bearing mouse model. Oxygen sensing was also tested in vivo by mimicking a hypoxic environment via ligation of the hind limbs of mice. Particles injected subcutaneously into both of the hind limbs showed dim phosphorescence, but upon ligation of the left hind leg, particles injected into the left side of the mouse showed increasing phosphorescence intensity, while particles injected into the right side of the mouse remained dim. Finally, in a therapeutic setting, the membrane-coated particles in combination with laser irradiation were able to halt cancer progression significantly better than uncoated particles in a mouse 4T1 cancer model.
Beyond monitoring low oxygen levels, many formulations include oxygen delivery as a strategy to overcome hypoxic conditions. In one such example, cancer cell membrane was coated around a porous zeolitic imidazolate framework embedded with catalase and Al(III) phthalocyanine chloride tetrasulfonic acid as the photosensitizer.[114] The purpose of this design was to self-sufficiently provide oxygen in order to enhance photodynamic therapy efficacy in hypoxic tumor regions. As in previous examples, the cancer cell membrane was shown to improve nanoparticle uptake into cells of the same origin. When the particles were made with HeLa cell membranes, they could more efficiently target the HeLa cells in culture, compared to limited uptake into COS7 monkey kidney cells. In vitro, once the nanoparticles were delivered into cells and irradiated, it was demonstrated that they could efficiently induce the production of ROS. This combination of increased uptake into cancer cells and ROS generation enabled significant induction of apoptosis in HeLa cells, something that was not observed for various control formulations. The efficient apoptosis was also measured using a cytotoxicity study, with a much steeper dose response to photosensitizer concentration for cells incubated with the membrane-coated particles compared with uncoated formulations, and minimal toxicity on control COS7 cells due to the decreased rate of uptake. In vivo, the oxygen-generating catalase was shown to retain its functionality, with mice injected with the catalase-containing formulation demonstrating reduced expression of HIF-1α in collected tumor sections. Tumor-bearing mice were also used to confirm that the membrane-coated formulations could localize to tumor sites effectively and could evade the immune system to circulate in the bloodstream for longer than uncoated formulations. Finally, using a murine tumor model, the coated formulation containing both the catalase and the photosensitizer caused nearly complete elimination of tumors, whereas other groups showed increasing tumor size over time. Organ sections collected at the end of the study also showed normal morphology, and blood markers for liver health remained close to baseline, indicating the safety of the platform.
This strategy was further adapted to include cancer cell starvation as a therapeutic modality. In a separate work, a porphyrin metal-organic PCN-224 framework was used as a nanophotosensitizer, and was subsequently loaded with both glucose oxidase and catalase before the loaded framework was coated with cancer cell membrane.[115] In this case, the glucose oxidase was used to deplete intracellular glucose, leading to cancer cell starvation. When the formulation was incubated with cancer cells in the presence of glucose, a significant pH drop was observed, signifying glucose breakdown and subsequent production of hydrogen peroxide. In the second step of the process, catalase in the particle induced the breakdown of H2O2 into O2. The increased oxygen concentration in the system then significantly enhanced the ROS production in response to excitation of the photosensitizer with irradiation. After characterizing each step of the reaction, the targeting of the particles to cancer cells via membrane coating was assessed. Particles were made using murine 4T1 membrane, and these particles preferentially targeted the source cells compared with control COS7 cells. Further, the membrane helped to significantly decrease the macrophage uptake compared with uncoated particles. In vivo delivery of the nanoreactor to tumors was also much improved by the cancer cell membrane coating. Using an animal tumor model, the CCNP formulation, along with light irradiation, led to significant control of tumor growth, virtually eliminating it.
In a related work, researchers took advantage of the hypoxia in tumors, as well as the acceleration of hypoxia caused by photodynamic therapy, to trigger the activity of a drug under bioreductive conditions. In this case, the same PCN-224 MOF was loaded with the drug tirapazamine and subsequently coated with cancer cell membrane.[116] After confirming coating using physicochemical characterization and western blot protein analysis, powder x-ray diffraction was used to confirm that the loading and coating procedures were mild enough to not disturb the native crystalline pattern of the PCN-244 framework. The coated formulation demonstrated a significant homotypic binding effect, most efficiently localizing to the source 4T1 cells compared with several different control cell lines, while reducing nonspecific uptake by macrophages. When cultured with 4T1 cells and irradiated, the 4T1 CCNPs were able to produce ROS intracellularly. When testing the cytotoxicity of the particles under a variety of conditions, it was confirmed that irradiation, along with a hypoxic environment to activate the tirapazamine, had the highest degree of killing. This cytotoxicity was heightened in cultures of the source cancer cells due to the increased concentration of nanoparticles in the cells after uptake. In vivo, the membrane coating had a marked effect on the localization of the particles, significantly increasing uptake in the tumor and reducing uptake in other organs such as the liver and lungs. When used to treat mice bearing 4T1 tumors, only the membrane-coated group with subsequent irradiation was able to significantly control tumor growth, with near complete control of growth over a period of 3 weeks, and greatly reduced the instance of metastasis in the lungs and liver. Analysis of the treated tumors revealed a decrease in proliferative markers, an increase in apoptosis markers, and increased local hypoxia within the tumor. Blood chemistry markers appeared normal for all groups, suggesting no major safety issues with the treatment.
6.3 Immune modulation
Besides more traditional delivery based applications, there has been interest in using CCNPs as anticancer vaccines. Taking advantage of the fact that many tumor antigens are surface markers, it has been proposed that the cancer cell membrane on the particles can deliver a multitude of diverse tumor antigens to the immune system. This was first explored using PLGA particles coated with membrane from B16-F10 mouse melanoma cells, and it was confirmed that nanoparticles contained glycoprotein 100 (gp100), a common melanoma-associated antigen.[25] These particles could be efficiently internalized by bone marrow-derived dendritic cells, which are important for the process of antigen presentation. Further, when the particles were incorporated with the immunological adjuvant, MPLA, they were able to very efficiently induce dendritic cell maturation, observed via upregulation of markers such as CD40, CD80, and CD86. Finally, the antigen specificity was demonstrated using a T cell stimulation assay. When the nanoparticles were fed to dendritic cells and co-incubated with gp100-specific splenocytes derived from pmel-1 transgenic mice, clear clustering of the splenocytes around the dendritic cells was visualized under brightfield microscopy. Further, the splenocytes produced significantly more IFN-γ, a cytokine known to be secreted by effector T cells. Another early study used cancer cell membrane to coat thermally oxidized porous silicon loaded with adjuvanting acetalated dextran.[117] Similar results were found, with the nanovaccine inducing high levels of CD80 and CD86 in human peripheral blood monocytes (PMBCs). The coated particles could also induce the secretion of IFN-γ, but not IL-2, indicating a polarization towards Th-1 T cell-mediated responses. Finally, PMBCs pulsed with the formulation could inhibit the proliferation of MDA-MB-231 cancer cells, indicating an immune response against the source cells of the membrane coating.
Recent work has expanded upon these proof-of-concept studies to demonstrate the vaccination application of these CCNPs in vivo (Figure 15).[118] In this case, the adjuvant CpG oligodeoxynucleotide 1826 (CpG) was encapsulated into PLGA nanoparticles and coated with B16-F10 membrane. First, the CpG was shown to remain active after loading into the nanoparticles. When administered subcutaneously to mice, both coated and uncoated CpG nanoparticles were able to cause the maturation of dendritic cells in the draining lymph node, as indicated by the upregulation of maturation markers like CD40, CD80, CD86, and MHC-II. The particulate forms of CpG outperformed formulations containing free CpG, likely because the endocytosis of the particles could localize CpG to its endosomal receptor TLR-9 for more efficient stimulation. Coating of cancer cell membrane onto the CpG nanoparticles was confirmed through size and zeta measurements, as well as western blotting, which showed that the membrane and coated particles retained at least three characteristic melanoma antigens, including gp100, tyrosinase-related protein (TRP)-2, and melan-A. The co-delivery of the two nanoparticle components, antigen and adjuvant, was subsequently examined in vitro. CCNPs made with membrane and CpG labeled with two different dyes were incubated with bone marrow-derived dendritic cells, and colocalization of both signals was observed within the dendritic cells after incubation. To study downstream immunological training, mice were injected with the CCNPs and the generation of antigen-specific T cells in the spleens was examined using flow cytometry. It was found that the CCNP treatment generated a significant increase in both gp100-specific and TRP-2-specific T cells, highlighting the ability of the nanoparticles to train the immune system against a multitude of different tumor antigens. The protective effects of vaccinating with the CCNPs were tested by challenging mice with B16-F10 cancer cells after immunization with the particles. Mice vaccinated with the CCNPs were able to reject the tumor cells significantly better than any other formulation, including a mixture of whole B16-F10 cells and free CpG, with 86% of mice remaining tumor free for over 150 days post-challenge. Finally, the therapeutic efficacy of the CCNP vaccines was tested on B16-F10 tumor-bearing mice, and it was discovered that administration of the CCNPs along with a cocktail of anti-CTLA-4 and anti-PD1 checkpoint blockades could control tumor growth and extend mouse survival better than either treatment alone.
Figure 15.
Cancer cell membrane-coated nanoparticles for antitumor vaccination. Polymeric nanoparticles encapsulating the adjuvant CpG ODN 1826 can be coated with cancer cell membrane as a rich source of antigenic material. CCNPs can facilitate the delivery of CpG to its endosomal receptor for dendritic cell maturation, and the co-delivered membrane provides cancer antigens for presentation. Downstream immune processes yield the generation of T cells specific for multiple cancer surface antigens, which can subsequently detect and eliminate tumors. Reproduced with permission.[118] Copyright 2017, Wiley-VCH.
7. Stem Cell Membrane-Coated Nanoparticles
Stem cells are another class of cells that have been leveraged to make membrane coatings. The cells themselves have been widely explored for various therapeutic purposes, especially in the field of regenerative medicine. They are relatively easy to work with, as techniques for their large-scale culture are widely reported. Stem cells display many special properties, including tumortropism, which researchers have taken advantage of to deliver therapeutic payloads.[119,120] Likewise, coating the membrane of stem cells onto nanoparticles has enabled the fabrication of nanocarriers with similar targeting functionality.
7.1 Drug delivery
Because of the tumortropism that is often associated with stem cells, stem cell membrane coating has been harnessed as a strategy for targeted delivery of cancer drugs to tumors. In one example, bone marrow-derived mesenchymal stem cell membrane was coated around gelatin nanogels loaded with DOX.[121] After making the nanogels via a desolvation method, DOX was loaded using a solvent-controlled precipitation method. The nanogels were mixed with DOX in a water solution containing ethanol to make the gelatin permeable to the drug. Then, the loaded nanogels were washed and resuspended in water to seal the DOX in the nanogels. The cores were then coated via extrusion with the cell membrane. The resulting nanoparticles had characteristics consistent with membrane coating, and the particle structure remained stable upon cellular uptake as shown via a colocalization of the fluorescently labeled cores and membrane. The membrane layer helped to further prolong the release of the drug compared with bare particles, and the release was accelerated after transferring the particles to lower pH solution, which indicates potential for tumor pH-responsive delivery. It was also demonstrated that the coated gelatin particles outperformed both the bare particles and free drug in an in vitro cancer cell cytotoxicity assay. This was likely due to enhanced uptake of the stem cell membrane-coated nanoparticles into the cancer cells, which was corroborated by both fluorescence microscopy images and flow cytometry. In vivo, using a tumor xenograft with HeLa cells implanted into nude mice, the coated particles more effectively targeted the tumor compared with bare gelatin particles. Finally, it was demonstrated that the advantages of the membrane-coated gelatin particles translated to better tumor treatment efficacy, helping to control tumor mass compared with control groups of the DOX-loaded gelatin particles as well as free DOX.
In a different application, particles functionalized with stem cell membrane were used as a substitute for live stem cells for regenerative medicine applications (Figure 16).[122] Benefits of this approach include possibly reduced immunogenicity and tumorigenicity of live cells without sacrificing the functionality of stem cell interactions with damaged cells. The growth factors from cardiac stem cell-conditioned media were loaded into PLGA microparticle cores and subsequently coated with membrane fragments derived from the same cells. By flow cytometry, it was shown that the resulting membrane-coated particles displayed some of the same markers as those displayed by live cardiac stem cells, with similar surface density. Important growth factors such as vascular endothelial growth factor, insulin-like growth factor 1, and hepatocyte growth factor could be released from the inside of the particles over the course of several days. The combination of stem cell marker display and released growth factors in the coated particles enabled the induction of phenotypic changes in cultured cardiomyocytes on par with the changes observed after incubation with live stem cells. Recordings captured evidence that the particles interacted directly with cardiomyocytes, even displaying synchronized beating patterns. Using a mouse model of myocardial infarction, the particles were injected intramyocardially as a treatment and significantly promoted cardiac repair, with the number of viable myocardium and the left ventricular ejection fraction both increasing significantly over the course of 4 weeks. Histological analysis demonstrated that treatment with the coated particles could also promote remuscularization, proliferation of cardiomyocytes, augmentation of blood flow, and increase in vessel density. Finally, it was shown that local injection of the particles did not promote any appreciable T cell response in the area, suggesting a lack of immunogenicity for the formulation.
Figure 16.
Cardiac stem cell membrane-coated growth factor-loaded nanoparticles for tissue repair. Stem cell membrane coating provides the polymeric nanoparticle cores with a binding affinity for sites of injury, such as injured cardiomyocytes after a heart attack. Upon binding, the nanoparticles release loaded growth factors to promote tissue repair through cell proliferation angiogenesis, and remuscularization. Reproduced with permission.[122] Copyright 2017, Nature Publishing Group.
7.2 Imaging and photoactivatable therapy
Stem cell membrane, with its inherent targeting capabilities, has been employed in photo-based applications. In the first example, the membrane from adipose-derived mesenchymal stem cells was coated around iron oxide nanoparticles for MRI applications.[123] After fabrication, it was confirmed that the particles retained CD44, a stem cell specific marker, and that the membrane coating was adept at helping prevent uptake of the particles by macrophages. The particles were also stable in varying amounts of serum over the course of 24 hours and retained the superparamagnetic properties of the iron oxide cores, generating dark contrast in T2-weight MRI. It was also demonstrated that the formulation could potentially be used as a theranostic agent; when they were subject to an alternating magnetic field, the particles could induce a marked increase in local temperature of the particles in solution. When uptake was aided using magnetic guidance, the nanoformulation effectively killed TRAMP-C1 cancer cells with the induced hyperthermia.
This coating strategy was later adapted for use with an upconversion-based nanostructure, which was used for remote-controlled photodynamic therapy. In this case, UCNPs were coated by a mesoporous silica shell integrated with two different photosensitizers, then subsequently coated by bone marrow-derived mesenchymal stem cell membrane (Figure 17).[124] After membrane coating was successfully confirmed, particles were fed into cells, and the signal of the core material localized well with a dye-labeled membrane, indicating a stable core-shell structure. The particles were also shown to be biocompatible when incubated with normal cells and did not cause adverse reactions when incubated with RBCs. Fluorescence imaging and flow cytometry experiments demonstrated that the coated particles could much more efficiently be taken up by HeLa cancer cells compared with bare particles, and after the application of NIR radiation, cancer cell viability was significantly reduced. When injected into mice bearing tumor xenografts, there was significant accumulation of the particles in the tumors and less in the liver when compared with the control formulation. The local increase in photosensitizers provided by the membrane improved antitumor efficacy, as it was demonstrated that the coated particles coupled with irradiation could efficiently control tumor growth, leading to almost no increase in tumor size over the course of two weeks. This was reflected in tumor histology taken after the treatment, which demonstrated a significant disruption of the tumor structure.
Figure 17.
Stem cell membrane-coated upconversion-silica core-shell nanoparticles for photodynamic therapy. Mesoporous silica shells loaded with photosensitizers is coated with bone marrow-derived mesenchymal stem cell membrane to gain tumortropism. The coated particles can efficiently accumulate in tumors after in vivo application, and the high local concentration of photosensitizers in tumor tissue enables enhanced photodynamic therapy and cancer cell killing. Reproduced with permission.[124] Copyright 2016, American Chemical Society.
8. Other Cell Membrane-Coated Nanoparticles
8.1 Endothelial cell membrane coating
A lesser explored but relevant source of coating material is endothelial cells, which are essential in the maintenance of healthy vasculature. In an example of endothelial membrane-coated nanoparticles, researchers took a different approach to load nanoparticles into membrane vesicles. In this case, various types of nanoparticles, including iron oxide nanoparticles, gold nanoparticles, quantum dots, and other variants, were first incubated with HUVECs.[48] TEM images confirmed that the different particles could all be internalized at a high density. The release of cell vesicles containing these nanoparticles was then triggered by starvation, which promotes vesiculation. It was even demonstrated that multiple nanoparticle types could be loaded into the same vesicle. In terms of their size, the nanoparticle-loaded vesicles were of fairly wide distribution and averaged several hundred nanometers in diameter. Using various iron oxide-containing endothelial vesicles, it was demonstrated that a magnetic field could be used to target these vesicles, along with co-encapsulated payloads, to a desired location. These nanoparticles were also able to generate significant contrast for MRI. Finally, by applying an alternating magnetic field, the particles could effectively induce local hyperthermia in solution. This endothelial cell-based strategy could potentially be used to fashion biocompatible theranostic delivery vehicles for a variety of applications.
8.2 Beta cell membrane coating
Beta cells are important constituents of the pancreas and are responsible for insulin secretion. The ability to effectively transplant or promote the growth of beta cells could have important implications for the treatment of diabetes mellitus, which currently affects upwards of 30 million individuals in the United States alone.[125] In an example of a beta cell-based platform, nanofiber scaffolds were coated with beta cell membrane as a means of promoting the growth of other beta cells, which rely on direct cell-to-cell interactions for their survival (Figure 18).[126] First, electrospinning was used to fabricate biodegradable polymeric fibers composed of PCL. The resulting fibers had an average diameter between 100 and 200 nm. Next, membrane coating was performed by incubating beta cell membrane vesicles with the nanofibers. Successful functionalization of the vesicles was confirmed using vesicles loaded with a fluorescent dye both within the inner aqueous compartment and on the membrane. After fusion, the inner dye was released and only the membrane dye signal remained, demonstrating that successful fusion had occurred. It was confirmed that the beta cell membrane-coated fibers expressed proteins found originally on the membrane of the source cells. To test their effect on cell proliferation and function, the coated fibers were used as a substrate on which beta cells were cultured. Compared to a control substrate, the membrane coated fibers promoted higher cell numbers, larger cell clusters, and an increase in the production of insulin. Beyond promoting beta cell growth, this nanofiber-based strategy could be useful for any sensitive cell types that require input signals via cell-cell contact for their growth and survival.
Figure 18.
Beta cell membrane-coated nanofibers for enhancing cell proliferation and function. Electrospun PCL nanofiber scaffolding coated with beta cell membrane can encourage the proliferation of their source cells through direct cell membrane-to-cell contact. The cell membrane coating transferred beta cell-specific proteins onto the nanofiber surface, and beta cells cultured on the fibers showed increased insulin production and cell proliferation. Reproduced with permission.[126] Copyright 2016, The Royal Society of Chemistry.
8.3 Bacterial membrane coating
While the membrane coating approach has almost exclusively centered around the use of mammalian cells as the membrane source, there is some developing interest in using pathogen-derived material. In one case, bacterial outer membrane vesicles (OMVs) were used to coat gold nanoparticles in order to promote anti-bacterial immunity (Figure 19).[127] OMVs are naturally produced by bacteria and provide a variety of functions that are important for their survival. Because these vesicular structures contain many bacterial antigens, they have been leveraged for vaccine applications.[128,129] One advantage of using the membrane coating approach is that it forces the membrane into a small format, as determined by the size of the gold nanoparticle substrate. Final nanoparticles sizes under 50 nm are ideal for lymphatic transport and can help to promote subsequent immune processing.[130] After coating gold nanoparticles with OMVs, it was shown that the particles became stable in physiological buffer, whereas bare gold nanoparticles were easily destabilized and aggregated. When used to vaccinate mice, analysis of the draining lymph nodes revealed an increased amount of antigen-presenting dendritic cells. Further, these dendritic cells exhibited a higher level of maturation compared with those from mice treated with OMVs alone. This difference was likely due to the more efficient transport of the OMV-coated gold nanoparticles. The improved modulation offered by the membrane-coated formulation translated to high antibacterial titers, which remained elevated for up to 140 days after the initial vaccination. Importantly, the antibodies from the nanoparticle-vaccinated mice also had higher avidity, attesting to the more faithful delivery of bacterial antigens to the immune system. Regarding T cell responses, the nanoformulation also helped to elevate levels of IFN-γ and IL-17, which are both important for mediating cellular immunity.
Figure 19.
Bacteria membrane-coated nanoparticles for modulating antibacterial immunity. Bacteria-secreted outer membrane vesicles contain a variety of bacterial surface antigens, and coating the membrane material onto gold nanoparticles facilitates the intracellular delivery of the antigens to dendritic cells. After vaccination, the nanoparticles can induce dendritic cell maturation and the generation of high antibacterial titers. Reproduced with permission.[127] Copyright 2015, American Chemical Society.
In a very different usage of a pathogen membrane coating strategy, mesoporous silica nanoparticles coated with E. coli membrane were used to deliver payloads into neutrophils, creating biohybrid micromotors.[131] Neutrophils are an important subset of immune cells that are chemotactically attracted to inflammatory stimuli. In this case, the bacterial membrane coating was used to help facilitate uptake of mesoporous silica nanoparticles by neutrophils, which are known to engulf bacteria. It was demonstrated by flow cytometry that bacteria membrane-coated nanoparticles exhibited significantly increased uptake compared with non-functionalized mesoporous silica nanoparticles. Cell viability was also maintained after uptake of the nanocarriers. Using a microfluidic system, it was further demonstrated that the nanoparticle-loaded neutrophils could migrate towards gel-immobilized bacteria. As the number of bacteria in the gel was increased, the chemotactic index of the neutrophils greatly increased. In developing these biohybrid micromotors, the authors of this study highlighted the potential of active delivery systems that leverage the powerful properties of living cells.
8.4 Hybrid cell membrane coating
The numerous cell types that have been discussed thus far highlight the unique properties that can be bestowed upon nanocarriers using the cell membrane coating technology. At times, it may be desirable to incorporate the functionalities from multiple cell types onto a single nanoparticle. This idea was demonstrated in a proof-of-concept work in which nanoparticles were functionalized with RBC–platelet hybrid membrane to achieve enhanced functionality (Figure 20).[132] First, hybrid membrane was generated by incubating two purified membranes together under gentle stirring at 37 °C. To confirm that fusion was occurring, platelet membrane was doped with a Förster resonance energy transfer (FRET) pair; once the two membranes were incubated together, fluorescence recovery was observed, indicating successful fusion. Using hybrid membrane made using RBC membrane and platelet membrane each doped with a different fluorophore to coat PLGA cores, significant colocalization of the two dyes was observed under fluorescence microscopy of the resulting nanoparticles. This indicated that individual nanoparticles contained both types of membranes. With regards to their physicochemical properties, the RBC–platelet hybrid membrane-coated nanoparticles were similar to both single membrane formulations and exhibited a characteristic core-shell structure. Further, the hybrid nanoparticles were stable in water, PBS, serum, and also after lyophilization. Proteomic analysis revealed that the hybrid formulation contained protein markers that were found on both RBCs and platelets, and immunogold staining followed by TEM visualization showed that markers characteristic of each cell type could be found on the same nanoparticle.
Figure 20.
RBC-platelet fusion membrane-coated nanoparticles for enhancing nanoparticle functionality. RBC membrane fused with platelet membrane can be coated onto polymeric nanoparticles and retain cell specific functionalities of both parent cell types. Reproduced with permission.[132] Copyright 2017, Wiley-VCH.
To test the functionality of the hybrid nanoparticles, a variety of assays were performed. First, it was demonstrated that the hybrid membrane-coated nanoparticles retained the macrophage uptake-suppressing property of both parent cell types. The hybrid also retained AChE activity, exhibited the ability to neutralize organophosphates, and could preferentially bind to cancer cells. These properties were maintained at an efficiency that was generally in between the levels observed with single membrane-coated nanoparticles. In vivo, the hybrid nanoparticle formulation demonstrated the ability to efficiently target atherosclerotic plaque, a function of which PNPs have proven particularly adept. Finally, both circulation and biodistribution were evaluated, and the results were in line with the pure membrane formulations. Overall, with the wide range of different cell-specific functions that are available, this hybrid membrane coating strategy has the potential to be useful when more than one set of functionalities is required. Careful consideration will need to be given on an application-specific basis concerning the relative amounts of each type of membrane to include.
9. Conclusions and Perspectives
In this review, the designs and applications of cell membrane-coated nanoparticles have been covered in depth. This emerging biomimetic functionalization strategy takes advantage of the inherent ability of cells to interact with their environments, bestowing traditional nanocarriers with enhanced biointerfacing capabilities. Developed originally as a means of prolonging nanoparticle circulation using RBC membrane coatings, the technique has since been expanded to encompass cells of all types, including platelets, WBCs, cancer cells, stem cells, and many others. Further, cell membrane coating has been applied to a variety of different materials, such as polymers, gels, inorganics, and metals, and the synthesis of the cores can be modified to accommodate almost any payload based on hydrophobicity, charge, size, or structure. The extraordinary diversity of cell types, each with their own set of unique functionalities, combined with the flexibility of substrate material and loaded cargoes, has enabled the development of nanoparticle-based platforms with potential applicability across a wide range of applications. Cell membrane coating is a top-down strategy that directly leverages natural components that can be easily derived, which helps to bypass some of the challenges associated with bottom-up modes of fabrication. Instead of attempting to reverse engineer biological processes and interactions, natural functionality can be transferred directly from the original source.
Looking at the current body of scientific literature on cell membrane-coated nanoparticles, it can be seen that these works largely fall under a few distinct categories. The first is, by leveraging the biological interactions that cell membranes are capable of, it has been possible to design nanocarriers with lowered nonspecific uptake and higher specific targeting. These two items are central to the design of nanocarriers, and the cell membrane coating approach has benefitted applications such as drug delivery, imaging, and phototherapies. The next category is detoxification, which takes advantage of the fact that almost all toxins must interact with cell membrane in some capacity. This is nearly universal for any toxin that adversely affects human health, whether it is a foreign toxin or an endogenous autoantibody. Because of this, cell membrane-coated nanoparticles have opened the door for the development of broad-spectrum detoxicants that can neutralize toxins based on their function rather than their specific molecular structure. As this feature is largely exclusive to membrane-coated nanoparticles, research in this area is expected to accelerate in the future. The last category is immune modulation, a topic of great interest to the medical community for its potential to address major diseases such as bacterial infection and cancer. It has been established that nanoparticulate delivery can help to greatly enhance antigen-specific immunity. Membrane coating can add utility to nanovaccine platforms in several ways, including serving as a neutralizing substrate that enables safe delivery of toxins or acting as a natural source of multi-antigenic material that promotes broad immunity against targets of interest. In the future, membrane-coated particles may even be used to modulate the immune system in the opposite direction, helping to stem autoimmunity in an antigen-specific manner.
While a significant amount of work has already been done on the cell membrane coating technology, researchers have only started to realize its potential. As exploration along these lines continues, we will undoubtedly see a broader range of applications, including a strong move into the diagnostics space. One of the most powerful aspects of this technology is that it enables the harnessing of biologically complex functionalities that would otherwise be near impossible to replicate synthetically. As such, it is likely that there are many new and exciting applications that have yet to be discovered. It also appears inevitable that cell membrane-coated nanoparticles will be increasingly employed in combinatorial approaches for disease treatment. Membrane from different organisms may be employed to open up additional strategies for addressing the rising threat of super pathogens via strategies such as immune modulation. While biointerfacing has been by far the main use of cell membrane coatings, more consideration may be given to bioactive membrane moieties, such as ion channels and enzymes. On a more fundamental level, additional research that leverages the ever-growing body of cell biology knowledge may help to elucidate the role of individual membrane components, which will enable us to move beyond our current black box approach.
Regarding the downstream translation of cell membrane-coated platforms, there are several factors that will be critical to success. Given their combination of biological and synthetic materials, the scale-up and manufacturing of these biomimetic nanoparticles will present some unique challenges. In terms of the source material, there are well-established protocols and infrastructure for obtaining blood products such as RBCs, platelets, and leukocytes. While it may be possible to use autologous sources, the more practical approach will likely be to obtain and bank material from type-matched donors. For other cell types, techniques for large-scale culture will need to be adapted. High-yield methods for membrane derivation will also need to be developed, especially for nucleated cells where membrane of high purity will be harder to obtain. Once the membrane has been derived, coating techniques that offer high throughputs will be necessary to manufacture the gram-scale quantities likely needed for the treatment of human patients. From here, new assays will be required to assess nanoparticle purity, along with workflows for filtration and long-term storage. Importantly, everything will need to be carried out aseptically and done in a manner that complies with good manufacturing processes, ensuring that the final products are free from both chemical and biological contaminants. While extensive, it is envisioned that all of these challenges can be met, especially given the significant benefits potentially afforded by cell membrane coating. Ultimately, as this emerging biomimetic nanotechnology being to mature, attempts will be made in earnest to translate such platforms to the clinic, where they are primed to make a positive impact on human health.
Acknowledgments
This work is supported by the Defense Threat Reduction Agency Joint Science and Technology Office for Chemical and Biological Defense under Grant Number HDTRA1-14-1-0064, the National Science Foundation Grant DMR-1505699, and the National Institutes of Health under Award Number R01CA200574.
Biographies

Ronnie H. Fang is an Assistant Project Scientist in the Department of NanoEngineering at the University of California San Diego. He received his Ph.D. in NanoEngineering at the University of California San Diego. His research is focused on leveraging biomimetic nanoparticles for drug delivery and immunoengineering applications.

Ashley V. Kroll is a graduate student researcher in the Department of NanoEngineering at the University of California San Diego. She received her B.S. in NanoEngineering at the University of California San Diego in 2014. Her research interests lie in the development of biomimetic nanoparticles for improved treatments of human diseases. She is currently working on cell membrane-coated nanoparticles for cancer immunotherapy.

Liangfang Zhang is a Professor in the Department of NanoEngineering and Moores Cancer Center at the University of California San Diego. He received his Ph.D. in Chemical and Biomolecular Engineering at the University of Illinois at Urbana-Champaign. His research aims to create cutting-edge biomimetic nanotechnologies and exploit them for various biomedical applications with a particular focus on drug delivery, biodetoxification and vaccination.
References
- 1.Shi J, Kantoff PW, Wooster R, Farokhzad OC. Nat. Rev. Cancer. 2017;17:20. doi: 10.1038/nrc.2016.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho K, Wang X, Nie S, Chen ZG, Shin DM. Clin. Cancer Res. 2008;14:1310. doi: 10.1158/1078-0432.CCR-07-1441. [DOI] [PubMed] [Google Scholar]
- 3.Wang AZ, Langer R, Farokhzad OC. Annu. Rev. Med. 2012;63:185. doi: 10.1146/annurev-med-040210-162544. [DOI] [PubMed] [Google Scholar]
- 4.Chow EK-H, Ho D. Sci. Transl. Med. 2013;5:216rv4. doi: 10.1126/scitranslmed.3005872. [DOI] [PubMed] [Google Scholar]
- 5.Davis ME, Chen ZG, Shin DM. Nat. Rev. Drug Discov. 2008;7:771. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 6.Blanco E, Shen H, Ferrari M. Nat. Biotechnol. 2015;33:941. doi: 10.1038/nbt.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moghimi SM, Hunter AC, Andresen TL. Annu. Rev. Pharmacol. Toxicol. 2012;52:481. doi: 10.1146/annurev-pharmtox-010611-134623. [DOI] [PubMed] [Google Scholar]
- 8.Owens DE, 3rd, Peppas NA. Int. J. Pharm. 2006;307:93. doi: 10.1016/j.ijpharm.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Nie S. Nanomedicine. 2010;5:523. doi: 10.2217/nnm.10.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li S-D, Huang L. Biochim. Biophys. Acta. 2009;1788:2259. doi: 10.1016/j.bbamem.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brannon-Peppas L, Blanchette JO. Adv. Drug Deliv. Rev. 2004;56:1649. doi: 10.1016/j.addr.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 12.Veiseh O, Gunn JW, Zhang M. Adv. Drug Deliv. Rev. 2010;62:284. doi: 10.1016/j.addr.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jokerst JV, Lobovkina T, Zare RN, Gambhir SS. Nanomedicine. 2011;6:715. doi: 10.2217/nnm.11.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suk JS, Xu Q, Kim N, Hanes J, Ensign LM. Adv. Drug Deliv. Rev. 2016;99:28. doi: 10.1016/j.addr.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanna V, Pala N, Sechi M. Int. J. Nanomedicine. 2014;9:467. doi: 10.2147/IJN.S36654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Q, Lai SK. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015;7:655. doi: 10.1002/wnan.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ishihara T, Takeda M, Sakamoto H, Kimoto A, Kobayashi C, Takasaki N, Yuki K, Tanaka K-I, Takenaga M, Igarashi R, Maeda T, Yamakawa N, Okamoto Y, Otsuka M, Ishida T, Kiwada H, Mizushima Y, Mizushima T. Pharm. Res. 2009;26:2270. doi: 10.1007/s11095-009-9943-x. [DOI] [PubMed] [Google Scholar]
- 18.Dehaini D, Fang RH, Zhang L. Bioeng. Transl. Med. 2016;1:30. doi: 10.1002/btm2.10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peppas NA. Adv. Drug Deliv. Rev. 2004;56:1529. doi: 10.1016/j.addr.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Yoo J-W, Irvine DJ, Discher DE, Mitragotri S. Nat. Rev. Drug Discov. 2011;10:521. doi: 10.1038/nrd3499. [DOI] [PubMed] [Google Scholar]
- 21.Fang RH, Jiang Y, Fang JC, Zhang L. Biomaterials. 2017;128:69. doi: 10.1016/j.biomaterials.2017.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kozlovskaya V, Alexander JF, Wang Y, Kuncewicz T, Liu X, Godin B, Kharlampieva E. ACS Nano. 2014;8:5725. doi: 10.1021/nn500512x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu C-MJ, Zhang L, Aryal S, Cheung C, Fang RH, Zhang L. Proc. Natl. Acad. Sci. U. S. A. 2011;108:10980. doi: 10.1073/pnas.1106634108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu C-MJ, Fang RH, Wang K-C, Luk BT, Thamphiwatana S, Dehaini D, Nguyen P, Angsantikul P, Wen CH, Kroll AV, Carpenter C, Ramesh M, Qu V, Patel SH, Zhu J, Shi W, Hofman FM, Chen TC, Gao W, Zhang K, Chien S, Zhang L. Nature. 2015;526:118. doi: 10.1038/nature15373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang RH, Hu C-MJ, Luk BT, Gao W, Copp JA, Tai Y, O’Connor DE, Zhang L. Nano Lett. 2014;14:2181. doi: 10.1021/nl500618u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroll AV, Fang RH, Zhang L. Bioconjug. Chem. 2017;28:23. doi: 10.1021/acs.bioconjchem.6b00569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu C-MJ, Fang RH, Zhang L. Adv. Healthc. Mater. 2012;1:537. doi: 10.1002/adhm.201200138. [DOI] [PubMed] [Google Scholar]
- 28.Fang RH, Hu C-MJ, Zhang L. Expert Opin. Biol. Ther. 2012;12:385. doi: 10.1517/14712598.2012.661710. [DOI] [PubMed] [Google Scholar]
- 29.Engering AJ, Cella M, Fluitsma D, Brockhaus M, Hoefsmit EC, Lanzavecchia A, Pieters J. Eur. J. Immunol. 1997;27:2417. doi: 10.1002/eji.1830270941. [DOI] [PubMed] [Google Scholar]
- 30.Brown GD, Gordon S. Nature. 2001;413:36. doi: 10.1038/35092620. [DOI] [PubMed] [Google Scholar]
- 31.Heldin CH. Cell. 1995;80:213. doi: 10.1016/0092-8674(95)90404-2. [DOI] [PubMed] [Google Scholar]
- 32.Hynes RO. Cell. 1987;48:549. doi: 10.1016/0092-8674(87)90233-9. [DOI] [PubMed] [Google Scholar]
- 33.Kishimoto TK, Larson RS, Corbi AL, Dustin ML, Staunton DE, Springer TA. Leukocyte Adhesion Molecules. Springer; New York, NY: 1990. pp. 7–43. [Google Scholar]
- 34.Stevens MM, George JH. Science. 2005;310:1135. doi: 10.1126/science.1106587. [DOI] [PubMed] [Google Scholar]
- 35.O’Connell J, O’Sullivan GC, Collins JK, Shanahan F. J. Exp. Med. 1996;184:1075. doi: 10.1084/jem.184.3.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oldenborg PA, Zheleznyak A, Fang YF, Lagenaur CF, Gresham HD, Lindberg FP. Science. 2000;288:2051. doi: 10.1126/science.288.5473.2051. [DOI] [PubMed] [Google Scholar]
- 37.Hoshino A, Costa-Silva B, Shen T-L, Rodrigues G, Hashimoto A, Tesic Mark M, Molina H, Kohsaka S, Di Giannatale A, Ceder S, Singh S, Williams C, Soplop N, Uryu K, Pharmer L, King T, Bojmar L, Davies AE, Ararso Y, Zhang T, Zhang H, Hernandez J, Weiss JM, Dumont-Cole VD, Kramer K, Wexler LH, Narendran A, Schwartz GK, Healey JH, Sandstrom P, Labori KJ, Kure EH, Grandgenett PM, Hollingsworth MA, de Sousa M, Kaur S, Jain M, Mallya K, Batra SK, Jarnagin WR, Brady MS, Fodstad O, Muller V, Pantel K, Minn AJ, Bissell MJ, Garcia BA, Kang Y, Rajasekhar VK, Ghajar CM, Matei I, Peinado H, Bromberg J, Lyden D. Nature. 2015;527:329. doi: 10.1038/nature15756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu Z, Ramishetti S, Tseng Y-C, Guo S, Wang Y, Huang L. J. Control. Release. 2013;172:259. doi: 10.1016/j.jconrel.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 39.Ohyanagi T, Nagahori N, Shimawaki K, Hinou H, Yamashita T, Sasaki A, Jin T, Iwanaga T, Kinjo M, Nishimura S-I. J. Am. Chem. Soc. 2011;133:12507. doi: 10.1021/ja111201c. [DOI] [PubMed] [Google Scholar]
- 40.Rodriguez PL, Harada T, Christian DA, Pantano DA, Tsai RK, Discher DE. Science. 2013;339:971. doi: 10.1126/science.1229568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu C-MJ, Fang RH, Luk BT, Chen KNH, Carpenter C, Gao W, Zhang K, Zhang L. Nanoscale. 2013;5:2664. doi: 10.1039/c3nr00015j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luk BT, Hu C-MJ, Fang RH, Dehaini D, Carpenter C, Gao W, Zhang L. Nanoscale. 2014;6:2730. doi: 10.1039/c3nr06371b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fan Z, Zhou H, Li PY, Speer JE, Cheng H. J. Mater. Chem. B Mater. Biol. Med. 2014;2:8231. doi: 10.1039/c4tb00980k. [DOI] [PubMed] [Google Scholar]
- 44.Wang F, Gao W, Thamphiwatana S, Luk BT, Angsantikul P, Zhang Q, Hu C-MJ, Fang RH, Copp JA, Pornpattananangkul D, Lu W, Zhang L. Adv. Mater. 2015;27:3437. doi: 10.1002/adma.201501071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Gao W, Fang RH, Dong A, Zhang L. Small. 2015;11:4309. doi: 10.1002/smll.201500987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Copp JA, Fang RH, Luk BT, Hu C-MJ, Gao W, Zhang K, Zhang L. Proc. Natl. Acad. Sci. U. S. A. 2014;111:13481. doi: 10.1073/pnas.1412420111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rao L, Cai B, Bu L-L, Liao Q-Q, Guo S-S, Zhao X-Z, Dong W-F, Liu W. ACS Nano. 2017;11:3496. doi: 10.1021/acsnano.7b00133. [DOI] [PubMed] [Google Scholar]
- 48.Silva AKA, Di Corato R, Pellegrino T, Chat S, Pugliese G, Luciani N, Gazeau F, Wilhelm C. Nanoscale. 2013;5:11374. doi: 10.1039/c3nr01541f. [DOI] [PubMed] [Google Scholar]
- 49.Aryal S, Hu C-MJ, Fang RH, Dehaini D, Carpenter C, Zhang D-E, Zhang L. Nanomedicine. 2013;8:1271. doi: 10.2217/nnm.12.153. [DOI] [PubMed] [Google Scholar]
- 50.Luk BT, Fang RH, Hu C-MJ, Copp JA, Thamphiwatana S, Dehaini D, Gao W, Zhang K, Li S, Zhang L. Theranostics. 2016;6:1004. doi: 10.7150/thno.14471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rao L, Bu L-L, Xu J-H, Cai B, Yu G-T, Yu X, He Z, Huang Q, Li A, Guo S-S, Zhang W-F, Liu W, Sun Z-J, Wang H, Wang T-H, Zhao X-Z. Small. 2015;11:6225. doi: 10.1002/smll.201502388. [DOI] [PubMed] [Google Scholar]
- 52.Fang RH, Hu C-MJ, Chen KNH, Luk BT, Carpenter CW, Gao W, Li S, Zhang D-E, Lu W, Zhang L. Nanoscale. 2013;5:8884. doi: 10.1039/c3nr03064d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhou H, Fan Z, Lemons PK, Cheng H. Theranostics. 2016;6:1012. doi: 10.7150/thno.15095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chai Z, Hu X, Wei X, Zhan C, Lu L, Jiang K, Su B, Ruan H, Ran D, Fang RH, Zhang L, Lu W. J. Control. Release. 2017;264:102. doi: 10.1016/j.jconrel.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 55.Su J, Sun H, Meng Q, Yin Q, Tang S, Zhang P, Chen Y, Zhang Z, Yu H, Li Y. Adv. Funct. Mater. 2016;26:1243. [Google Scholar]
- 56.Fu Q, Lv P, Chen Z, Ni D, Zhang L, Yue H, Yue Z, Wei W, Ma G. Nanoscale. 2015;7:4020. doi: 10.1039/c4nr07027e. [DOI] [PubMed] [Google Scholar]
- 57.Su J, Sun H, Meng Q, Yin Q, Zhang P, Zhang Z, Yu H, Li Y. Adv. Funct. Mater. 2016;26:7495. [Google Scholar]
- 58.Su J, Sun H, Meng Q, Zhang P, Yin Q, Li Y. Theranostics. 2017;7:523. doi: 10.7150/thno.17259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rao L, Meng Q-F, Huang Q, Liu P, Bu L-L, Kondamareddy KK, Guo S-S, Liu W, Zhao X-Z. Adv. Healthc. Mater. 2016;5:1420. doi: 10.1002/adhm.201600303. [DOI] [PubMed] [Google Scholar]
- 60.Chen W, Zeng K, Liu H, Ouyang J, Wang L, Liu Y, Wang H, Deng L, Liu Y-N. Adv. Funct. Mater. 2017;27 doi: 10.1002/adfm.201605795. [DOI] [Google Scholar]
- 61.Gao L, Wang H, Nan L, Peng T, Sun L, Zhou J, Xiao Y, Wang J, Sun J, Lu W, Zhang L, Yan Z, Yu L, Wang Y. Bioconjug. Chem. 2017;28:2591. doi: 10.1021/acs.bioconjchem.7b00428. [DOI] [PubMed] [Google Scholar]
- 62.Song Q, Yin Y, Shang L, Wu T, Zhang D, Kong M, Zhao Y, He Y, Tan S, Guo Y, Zhang Z. Nano Lett. 2017 doi: 10.1021/acs.nanolett.7b03186. [DOI] [PubMed] [Google Scholar]
- 63.Zhang X, Angsantikul P, Ying M, Zhuang J, Zhang Q, Wei X, Jiang Y, Zhang Y, Dehaini D, Chen M, Chen Y, Gao W, Fang RH, Zhang L. Angew. Chem. Int. Ed. 2017;56:14075. doi: 10.1002/anie.201707598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li L-L, Xu J-H, Qi G-B, Zhao X, Yu F, Wang H. ACS Nano. 2014;8:4975. doi: 10.1021/nn501040h. [DOI] [PubMed] [Google Scholar]
- 65.Zhang Y, Zhang J, Chen W, Angsantikul P, Spiekermann KA, Fang RH, Gao W, Zhang L. J. Control. Release. 2017;263:185. doi: 10.1016/j.jconrel.2017.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gao L, Han L, Ding X, Xu J, Wang J, Zhu J, Lu W, Sun J, Yu L, Yan Z, Wang Y. Nanotechnology. 2017;28:335101. doi: 10.1088/1361-6528/aa7c43. [DOI] [PubMed] [Google Scholar]
- 67.Gao W, Hu C-MJ, Fang RH, Luk BT, Su J, Zhang L. Adv. Mater. 2013;25:3549. doi: 10.1002/adma.201300638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rao L, Meng Q-F, Bu L-L, Cai B, Huang Q, Sun Z-J, Zhang W-F, Li A, Guo S-S, Liu W, Wang T-H, Zhao X-Z. ACS Appl. Mater. Interfaces. 2017;9:2159. doi: 10.1021/acsami.6b14450. [DOI] [PubMed] [Google Scholar]
- 69.Piao J-G, Wang L, Gao F, You Y-Z, Xiong Y, Yang L. ACS Nano. 2014;8:10414. doi: 10.1021/nn503779d. [DOI] [PubMed] [Google Scholar]
- 70.Ren X, Zheng R, Fang X, Wang X, Zhang X, Yang W, Sha X. Biomaterials. 2016;92:13. doi: 10.1016/j.biomaterials.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 71.Jiang Q, Luo Z, Men Y, Yang P, Peng H, Guo R, Tian Y, Pang Z, Yang W. Biomaterials. 2017;143:29. doi: 10.1016/j.biomaterials.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 72.Jiang T, Zhang B, Shen S, Tuo Y, Luo Z, Hu Y, Pang Z, Jiang X. ACS Appl. Mater. Interfaces. 2017;9:31497. doi: 10.1021/acsami.7b09458. [DOI] [PubMed] [Google Scholar]
- 73.Wang X, Li H, Liu X, Tian Y, Guo H, Jiang T, Luo Z, Jin K, Kuai X, Liu Y, Pang Z, Yang W, Shen S. Biomaterials. 2017;143:130. doi: 10.1016/j.biomaterials.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 74.Ding H, Lv Y, Ni D, Wang J, Tian Z, Wei W, Ma G. Nanoscale. 2015;7:9806. doi: 10.1039/c5nr02470f. [DOI] [PubMed] [Google Scholar]
- 75.Deng J, Xu S, Hu W, Xun X, Zheng L, Su M. Biomaterials. doi: 10.1016/j.biomaterials.2017.10.048. n.d. [DOI] [PubMed] [Google Scholar]
- 76.Ren H, Liu J, Li Y, Wang H, Ge S, Yuan A, Hu Y, Wu J. Acta Biomater. 2017;59:269. doi: 10.1016/j.actbio.2017.06.035. [DOI] [PubMed] [Google Scholar]
- 77.Gao M, Liang C, Song X, Chen Q, Jin Q, Wang C, Liu Z. Adv. Mater. 2017;29 doi: 10.1002/adma.201701429. [DOI] [PubMed] [Google Scholar]
- 78.Fang RH, Luk BT, Hu C-MJ, Zhang L. Adv. Drug Deliv. Rev. 2015;90:69. doi: 10.1016/j.addr.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hu C-MJ, Fang RH, Copp J, Luk BT, Zhang L. Nat. Nanotechnol. 2013;8:336. doi: 10.1038/nnano.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chhabria V, Beeton S. Nanomedicine. 2016;11:2797. doi: 10.2217/nnm-2016-0180. [DOI] [PubMed] [Google Scholar]
- 81.Escajadillo T, Olson J, Luk BT, Zhang L, Nizet V. Front. Pharmacol. 2017;8:477. doi: 10.3389/fphar.2017.00477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen MS, Zhang Y, Zhang L. Nanoscale. 2017;9:14506. doi: 10.1039/c7nr05322c. [DOI] [PubMed] [Google Scholar]
- 83.Wu Z, Li T, Gao W, Xu T, Jurado-Sánchez B, Li J, Gao W, He Q, Zhang L, Wang J. Adv. Funct. Mater. 2015;25:3881. [Google Scholar]
- 84.Pang Z, Hu C-MJ, Fang RH, Luk BT, Gao W, Wang F, Chuluun E, Angsantikul P, Thamphiwatana S, Lu W, Jiang X, Zhang L. ACS Nano. 2015;9:6450. doi: 10.1021/acsnano.5b02132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nguyen TDT, Pitchaimani A, Koirala MB, Muhammad F, Aryal S. RSC Adv. 2016;6:33003. [Google Scholar]
- 86.Hu C-MJ, Fang RH, Luk BT, Zhang L. Nat. Nanotechnol. 2013;8:933. doi: 10.1038/nnano.2013.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang F, Fang RH, Luk BT, Hu C-MJ, Thamphiwatana S, Dehaini D, Angsantikul P, Kroll AV, Pang Z, Gao W, Lu W, Zhang L. Adv. Funct. Mater. 2016;26:1628. doi: 10.1002/adfm.201505231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wei X, Gao J, Wang F, Ying M, Angsantikul P, Kroll AV, Zhou J, Gao W, Lu W, Fang RH, Zhang L. Adv. Mater. 2017;29 doi: 10.1002/adma.201701644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Guo Y, Wang D, Song Q, Wu T, Zhuang X, Bao Y, Kong M, Qi Y, Tan S, Zhang Z. ACS Nano. 2015;9:6918. doi: 10.1021/acsnano.5b01042. [DOI] [PubMed] [Google Scholar]
- 90.Chen H-W, Fang Z-S, Chen Y-T, Chen YI, Yao B-Y, Cheng J-Y, Chien C-Y, Chang Y-C, Hu C-MJ. ACS Appl. Mater. Interfaces. 2017 doi: 10.1021/acsami.7b09931. [DOI] [PubMed] [Google Scholar]
- 91.Lapek JD, Jr, Fang RH, Wei X, Li P, Wang B, Zhang L, Gonzalez DJ. ACS Nano. 2017 doi: 10.1021/acsnano.7b02650. [DOI] [PubMed] [Google Scholar]
- 92.Hu Q, Sun W, Qian C, Wang C, Bomba HN, Gu Z. Adv. Mater. 2015;27:7043. doi: 10.1002/adma.201503323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li J, Ai Y, Wang L, Bu P, Sharkey CC, Wu Q, Wun B, Roy S, Shen X, King MR. Biomaterials. 2016;76:52. doi: 10.1016/j.biomaterials.2015.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hu Q, Qian C, Sun W, Wang J, Chen Z, Bomba HN, Xin H, Shen Q, Gu Z. Adv. Mater. 2016;28:9573. doi: 10.1002/adma.201603463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rao L, Bu L-L, Meng Q-F, Cai B, Deng W-W, Li A, Li K, Guo S-S, Zhang W-F, Liu W, Sun Z-J, Zhao X-Z. Adv. Funct. Mater. 2017;27 doi: 10.1002/adfm.201604774. [DOI] [Google Scholar]
- 96.Wei X, Gao J, Fang RH, Luk BT, Kroll AV, Dehaini D, Zhou J, Kim HW, Gao W, Lu W, Zhang L. Biomaterials. 2016;111:116. doi: 10.1016/j.biomaterials.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Parodi A, Quattrocchi N, van de Ven AL, Chiappini C, Evangelopoulos M, Martinez JO, Brown BS, Khaled SZ, Yazdi IK, Enzo MV, Isenhart L, Ferrari M, Tasciotti E. Nat. Nanotechnol. 2013;8:61. doi: 10.1038/nnano.2012.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Krishnamurthy S, Gnanasammandhan MK, Xie C, Huang K, Cui MY, Chan JM. Nanoscale. 2016;8:6981. doi: 10.1039/c5nr07588b. [DOI] [PubMed] [Google Scholar]
- 99.Xuan M, Shao J, Dai L, He Q, Li J. Adv. Healthc. Mater. 2015;4:1645. doi: 10.1002/adhm.201500129. [DOI] [PubMed] [Google Scholar]
- 100.Cao H, Dan Z, He X, Zhang Z, Yu H, Yin Q, Li Y. ACS Nano. 2016;10:7738. doi: 10.1021/acsnano.6b03148. [DOI] [PubMed] [Google Scholar]
- 101.Kang T, Zhu Q, Wei D, Feng J, Yao J, Jiang T, Song Q, Wei X, Chen H, Gao X, Chen J. ACS Nano. 2017;11:1397. doi: 10.1021/acsnano.6b06477. [DOI] [PubMed] [Google Scholar]
- 102.Zhang L, Li R, Chen H, Wei J, Qian H, Su S, Shao J, Wang L, Qian X, Liu B. Int. J. Nanomedicine. 2017;12:2129. doi: 10.2147/IJN.S126016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xuan M, Shao J, Dai L, Li J, He Q. ACS Appl. Mater. Interfaces. 2016;8:9610. doi: 10.1021/acsami.6b00853. [DOI] [PubMed] [Google Scholar]
- 104.Rao L, He Z, Meng Q-F, Zhou Z, Bu L-L, Guo S-S, Liu W, Zhao X-Z. J. Biomed. Mater. Res. A. 2017;105:521. doi: 10.1002/jbm.a.35927. [DOI] [PubMed] [Google Scholar]
- 105.Thamphiwatana S, Angsantikul P, Escajadillo T, Zhang Q, Olson J, Luk BT, Zhang S, Fang RH, Gao W, Nizet V, Zhang L. Proc. Natl. Acad. Sci. U. S. A. 2017;114:11488. doi: 10.1073/pnas.1714267114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Xiong K, Wei W, Jin Y, Wang S, Zhao D, Wang S, Gao X, Qiao C, Yue H, Ma G, Xie H-Y. Adv. Mater. 2016;28:7929. doi: 10.1002/adma.201601643. [DOI] [PubMed] [Google Scholar]
- 107.Zhu J-Y, Zheng D-W, Zhang M-K, Yu W-Y, Qiu W-X, Hu J-J, Feng J, Zhang X-Z. Nano Lett. 2016;16:5895. doi: 10.1021/acs.nanolett.6b02786. [DOI] [PubMed] [Google Scholar]
- 108.Sun H, Su J, Meng Q, Yin Q, Chen L, Gu W, Zhang P, Zhang Z, Yu H, Wang S, Li Y. Adv. Mater. 2016;28:9581. doi: 10.1002/adma.201602173. [DOI] [PubMed] [Google Scholar]
- 109.Tian H, Luo Z, Liu L, Zheng M, Chen Z, Ma A, Liang R, Han Z, Lu C, Cai L. Adv. Funct. Mater. 2017;27 doi: 10.1002/adfm.201703197. [DOI] [Google Scholar]
- 110.Sun H, Su J, Meng Q, Yin Q, Chen L, Gu W, Zhang Z, Yu H, Zhang P, Wang S, Li Y. Adv. Funct. Mater. 2017;27 doi: 10.1002/adfm.201604300. [DOI] [Google Scholar]
- 111.Rao L, Bu L-L, Cai B, Xu J-H, Li A, Zhang W-F, Sun Z-J, Guo S-S, Liu W, Wang T-H, Zhao X-Z. Adv. Mater. 2016;28:3460. doi: 10.1002/adma.201506086. [DOI] [PubMed] [Google Scholar]
- 112.Chen Z, Zhao P, Luo Z, Zheng M, Tian H, Gong P, Gao G, Pan H, Liu L, Ma A, Cui H, Ma Y, Cai L. ACS Nano. 2016;10:10049. doi: 10.1021/acsnano.6b04695. [DOI] [PubMed] [Google Scholar]
- 113.Li S-Y, Xie B-R, Cheng H, Li C-X, Zhang M-K, Qiu W-X, Liu W-L, Wang X-S, Zhang X-Z. Biomaterials. 2017;151:1. doi: 10.1016/j.biomaterials.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 114.Cheng H, Zhu J-Y, Li S-Y, Zeng J-Y, Lei Q, Chen K-W, Zhang C, Zhang X-Z. Adv. Funct. Mater. 2016;26:7847. [Google Scholar]
- 115.Li S-Y, Cheng H, Xie B-R, Qiu W-X, Zeng J-Y, Li C-X, Wan S-S, Zhang L, Liu W-L, Zhang X-Z. ACS Nano. 2017;11:7006. doi: 10.1021/acsnano.7b02533. [DOI] [PubMed] [Google Scholar]
- 116.Li S-Y, Cheng H, Qiu W-X, Zhang L, Wan S-S, Zeng J-Y, Zhang X-Z. Biomaterials. 2017;142:149. doi: 10.1016/j.biomaterials.2017.07.026. [DOI] [PubMed] [Google Scholar]
- 117.Fontana F, Shahbazi M-A, Liu D, Zhang H, Mäkilä E, Salonen J, Hirvonen JT, Santos HA. Adv. Mater. 2017;29 doi: 10.1002/adma.201603239. [DOI] [PubMed] [Google Scholar]
- 118.Kroll AV, Fang RH, Jiang Y, Zhou J, Wei X, Yu CL, Gao J, Luk BT, Dehaini D, Gao W, Zhang L. Adv. Mater. 2017 doi: 10.1002/adma.201703969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gao Z, Zhang L, Hu J, Sun Y. Nanomedicine. 2013;9:174. doi: 10.1016/j.nano.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 120.Hu Y-L, Fu Y-H, Tabata Y, Gao J-Q. J. Control. Release. 2010;147:154. doi: 10.1016/j.jconrel.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 121.Gao C, Lin Z, Jurado-Sánchez B, Lin X, Wu Z, He Q. Small. 2016;12:4056. doi: 10.1002/smll.201600624. [DOI] [PubMed] [Google Scholar]
- 122.Tang J, Shen D, Caranasos TG, Wang Z, Vandergriff AC, Allen TA, Hensley MT, Dinh P-U, Cores J, Li T-S, Zhang J, Kan Q, Cheng K. Nat. Commun. 2017;8:13724. doi: 10.1038/ncomms13724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lai P-Y, Huang R-Y, Lin S-Y, Lin Y-H, Chang C-W. RSC Adv. 2015;5:98222. [Google Scholar]
- 124.Gao C, Lin Z, Wu Z, Lin X, He Q. ACS Appl. Mater. Interfaces. 2016;8:34252. doi: 10.1021/acsami.6b12865. [DOI] [PubMed] [Google Scholar]
- 125.Reusch JEB, Manson JE. JAMA. 2017;317:1015. doi: 10.1001/jama.2017.0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen W, Zhang Q, Luk BT, Fang RH, Liu Y, Gao W, Zhang L. Nanoscale. 2016;8:10364. doi: 10.1039/c6nr00535g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gao W, Fang RH, Thamphiwatana S, Luk BT, Li J, Angsantikul P, Zhang Q, Hu C-MJ, Zhang L. Nano Lett. 2015;15:1403. doi: 10.1021/nl504798g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Acevedo R, Fernández S, Zayas C, Acosta A, Sarmiento ME, Ferro VA, Rosenqvist E, Campa C, Cardoso D, Garcia L, Perez JL. Front. Immunol. 2014;5:121. doi: 10.3389/fimmu.2014.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.van der Pol L, Stork M, van der Ley P. Biotechnol. J. 2015;10:1689. doi: 10.1002/biot.201400395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fang RH, Kroll AV, Zhang L. Small. 2015;11:5483. doi: 10.1002/smll.201501284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shao J, Xuan M, Zhang H, Lin X, Wu Z, He Q. Angew. Chem. Int. Ed. 2017;56:12935. doi: 10.1002/anie.201706570. [DOI] [PubMed] [Google Scholar]
- 132.Dehaini D, Wei X, Fang RH, Masson S, Angsantikul P, Luk BT, Zhang Y, Ying M, Jiang Y, Kroll AV, Gao W, Zhang L. Adv. Mater. 2017;29:1701644. doi: 10.1002/adma.201606209. [DOI] [PMC free article] [PubMed] [Google Scholar]