Abstract
Despite efforts to promote healthy weight, obesity is at epidemic levels among adults in the US. We examined the prevalence of weight loss attempts among a racially diverse sample of overweight and obese primary care patients (n = 274) based on sociodemographic, clinical and psychological factors, and shared decision-making (SDM) about weight loss/management. This observational study was conducted from December 2015 through January 2017. Data were obtained by self-report via survey. Overall, 64% of participants were attempting to lose weight at the time of survey. No significant differences in current weight loss attempts were found based on racial background, sociodemographic characteristics, or clinical factors. Participants who believed they were obese/overweight (OR = 6.70, 95% CI = 2.86, 15.72, p < 0.0001) or who were ready to lose/manage their weight (OR = 4.50, 95% CI = 1.82, 11.09, p = 0.001) had an increased likelihood of attempting to lose weight. The likelihood of attempting to lose weight increased with greater SDM with providers (OR = 1.54, 95% CI = 1.06, 2.22, p = 0.02). Patient perceptions about their weight, their readiness for weight loss/management, and SDM were associated significantly with weight loss attempts.
Keywords: Weight loss, Attempts, Shared decision-making, Primary care
Highlights
-
•
Obesity is a significant clinical and public health issue.
-
•
64% of obese/overweight primary care patients was trying to lose weight.
-
•
Weight loss attempts did not differ based on race, SES, or clinical factors.
-
•
Weight loss efforts were associated with perceived obesity status and readiness.
-
•
Greater shared decision-making was associated with making weight loss efforts.
1. Introduction
A majority of adults are either overweight or obese and national data show that individual attempts to lose weight vary greatly and may not include changes in lifestyle behaviors recommended and proven for weight loss (Serdula et al., 1999, LaRose et al., 2013, An and Xiang, 2016, Senechal et al., 2015, Ogden et al., 2014, Stokes et al., 2017). Although the United States Preventive Services Task Force (USPTSF) recommends that health care providers screen for obesity and provide intensive behavioral interventions for weight loss counseling or refer obese patients to these types of programs (Moyer and Force, 2012), enrollment in weight loss programs is variable among primary care patients (Hartman et al., 2014, Wadden et al., 2011, Oh et al., 2010) and patient attrition before completing all program components offered in clinics increases significantly over time (Berry et al., 2014).
The lack of provider advice, the burden of medical problems facing a patient, and patients' beliefs about their health has been associated with decisions about whether to attempt weight loss (Berry et al., 2014, Debnam et al., 2012, Dutton et al., 2014, Serdula et al., 2003, Tsai et al., 2009, Peek et al., 2010). Differences in the prevalence of overweight and obesity suggest that weight loss attempts may also differ among racial groups (Tsai et al., 2009). Shared decision-making (SDM) is also being recognized as a critical component of patient care that indicates the quality of patient-provider communication (Tsai et al., 2009, Parchman et al., 2010) and predicts greater adherence to provider advice and recommendations (Parchman et al., 2010). However, empirical data on the association between SDM and weight loss attempts are not available. In this study, we sought to gain a greater understanding of weight loss attempts by examining racial background, sociodemographic factors, clinical characteristics, psychological variables, and SDM to identify factors that may motivate weight loss attempts among a sample of overweight or obese primary care patients.
2. Methods
2.1. Setting and study sample
Setting: Practice settings include primary care practices that were members of either a national practice-based research network (Primary Care Practices Research Network (PPRNet), n = 7) or a federally-qualified health care system based in the Southeastern part of the United States (n = 1). PPRNet is composed of academic and community primary care practices that volunteer to submit electronic health record data for benchmarking, quality improvement, and participation in research projects. Practices in PPRNet are small to medium in size and serve patients in urban, small cities, and rural areas throughout the United States.
Sample: Study participants represented a convenience sample of primary care patients aged 18–75 years who had at least a 3-year history of being a patient in their current practice setting and who self-reported being either overweight or obese (n = 247). The mean number of participants enrolled from each practice was 29.2.
2.2. Procedures
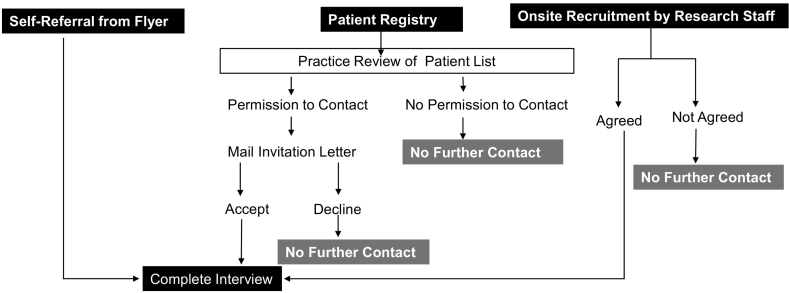
Patients were recruited from the primary care practices described above using either one or a combination of four mechanisms: informational flyers posted in practice settings or given to patients as they checked in for appointments, postings on the practice web portal, a mailed invitation to participate, or on-site, in practice direct recruitment (Fig. 1). More than one recruitment strategy could be used in each practice to enhance participation. The study was described in the flyer and on the web portal as research to understand patient preferences for weight loss interventions in primary care and to understand barriers and facilitators to weight loss in these settings. Patients self-referred for study participation by calling a toll-free number for each recruitment mechanism. Patients who self-referred from the study flyer or portal were screened for eligibility using a structured script. Eligible patients provided verbal informed consent for enrollment. Patients contacted by mail were identified from a practice registry maintained by the PPRNet and mailed an invitation letter that described the purpose of the study, the procedures involved in participation, and a self-addressed reply card to return if they did not want to be contacted about the study. Patients could also opt-out of study participation by calling the toll-free study number or emailing the research team. Patients not opting-out were contacted to determine eligibility and interest in participating. Eligible patients provided verbal informed consent for enrollment. Study staff also approached patients on-site during clinic hours and invited them to participate in the study. The purpose of the study and the procedures involved in participation were verbally described to these patients. Interested patients were consented.
Fig. 1.
Overview of recruitment strategies.
Regardless of recruitment mechanism, all enrolled patients were asked to complete a structured 20-minute interview, either on the phone or in person. The interview survey was designed to collect self-reported information on racial background, sociodemographic characteristics (e.g., income, marital status, education, and employment), clinical characteristics, psychological variables, receipt of physician advice about weight loss, and weight loss attempts. Patients enrolled in practice settings completed the interview in a private area. Clinical characteristics included a self-reported history of having ever been diagnosed with either diabetes or hypertension (yes or no), self-reported height (inches) and weight (pounds). BMI was calculated using the established formula (Clinical Guidelines on the Identification, Evaluation, and, American College of Cardiology/American Heart Association T). Participants were characterized as being obese (BMI ≥ 30.0) or overweight (BMI between 25 and 29.9).
Two psychological factors (self-efficacy and readiness for weight loss) were assessed using Likert-style items. A self-efficacy question assessed how confident participants were in their ability to lose/manage their weight (1 = not at all confident, 2 = a little confident, 3 = somewhat confident, 4 = very confident, and 5 = completely confident). Responses to this item were re-coded into very/completely confident versus not at all/a little/somewhat confident. The readiness for weight loss/management question asked participants to indicate how ready they were to start trying to lose weight or keep their weight the same (1 = not at all/have not thought about it, 2 = a little ready, 3 = somewhat ready, 4 = very ready, 5 = already trying to lose weight/keep weight the same). Responses to this item were re-coded into very ready/already trying to lose or keep weight the same versus not at all/a little/somewhat ready.
Perceptions of being overweight or obese were measured by asking participants if they considered themselves to be overweight or obese (yes, no, or do not know). Responses to this item were coded as yes or no/do not know.
Patient-provider communication about weight loss assessed provision of provider advice and involvement in shared decision-making via patient recall. Provider advice was assessed by asking participants to indicate if they had ever been advised by their health care provider to lose or manage their weight (yes, no, do not know, refused). The Shared Decision-Making Questionnaire-9 (SDM-Q-9) was used to assess shared decision-making about weight loss and/or weight management (Kriston et al., 2010). The SDM-Q-9 assesses the extent to which patients believed that their health care provider involved them in making decisions about their weight loss and/or management by doing things such as making clear that a decision needed to be made, describing different treatment options, and wanting to know exactly how they wanted to be involved in making the decisions about their weight loss/management. One item from the SDM-Q-9 (my doctor and I thoroughly weighed the different treatment options) was omitted because of an administrative error. This omission did not adversely affect the internal consistency of the instrument (Cronbach's alpha = 0.93).
Weight loss attempts were assessed by self-report using an item adapted from the Behavioral Risk Factor Surveillance Survey that asked respondents if they were trying to lose weight now (yes, no, do not know, refused). Responses of do not know were analyzed as not attempting to lose weight.
The survey was administered in Spanish either in-person or by telephone to those who did not speak English. Patients were given a $25 gift card after completing the interview.
This study was approved by the Institutional Review Board at the Medical University of South Carolina.
2.3. Statistical analyses
Three analyses were conducted: 1) descriptive statistics to characterize participants in terms of racial background, sociodemographic factors, clinical characteristics, psychological variables, and weight loss attempts; 2) bivariate analyses to identify variables significantly associated with weight loss attempts; and 3) multivariate logistic regression analysis using generalized estimating equations to adjust for potential correlation among patients from the same practice. Variables with a bivariate association of p < 0.10 with weight loss attempts were included in the multivariate logistic regression model.
3. Results
3.1. Descriptive characteristics of study sample
Forty-three percent of participants were from racial and ethnic minority groups (e.g., African American or Hispanic), 63% were women, 59% were married, 59% had at least some college education, and 57% were employed (Table 1). Sixty-two percent of participants believed they were overweight or obese, 58% had been advised by their health care provider to lose weight, 71% were ready to lose weight, and 56% were confident in their ability to lose weight. Overall, 64% of participants reported that they were attempting to lose weight.
Table 1.
Descriptive statistics on sociodemographic, clinical, and psychological factors (n = 274)a.
| Variable | Level | n (%) |
|---|---|---|
| Racial backgroundb | Racial/ethnic minority Non racial/ethnic minority |
132 (57%) 101 (43%) |
| Gender | Male Female |
87 (37%) 147 (63%) |
| Marital status | Married Not married |
139 (59%) 95 (41%) |
| Education level | ≥ Some college ≤ High school |
137 (59%) 97 (41%) |
| Employment statusb | Employed Not employed |
132 (57%) 99 (43%) |
| Income levelb | ˃$20,000 ˂$20,000 |
131 (68%) 61 (32%) |
| Diabetes | Yes No |
53 (23%) 180 (77%) |
| Hypertension | Yes No |
130 (56%) 103 (44%) |
| Obesity status (BMI) | Obese Overweight |
147 (63%) 87 (37%) |
| Provider advice about weight loss | Yes No |
135 (58%) 99 (42%) |
| Perceived obesity | Yes No |
144 (62%) 90 (38%) |
| Ready for weight loss | Ready Not ready |
167 (71%) 67 (29%) |
| Confidence for weight loss | Confident Not confident |
132 (56%) 102 (44%) |
Data were self-reported from obese and overweight primary care patients.
n does not equal 274 because of missing data.
3.2. Bivariate analysis
No significant racial, educational, or employment differences in weight loss attempts were found in the bivariate analysis (Table 2). However, women were significantly more likely than men to report that they were attempting to lose weight (74% versus 46%, Chi Square = 18.75, p < 0.0001). Of the clinical factors, only obesity status had a significant association with weight loss attempts; 69% of obese participants were making weight loss attempts compared to 54% of overweight participants (Chi Square = 5.58, p = 0.02). Weight loss attempts did not differ with participant confidence to lose or manage their weight. Participants describing themselves as “more ready” to make changes in their weight were more likely than those who were “less ready” to report making weight loss attempts (Chi Square = 28.21, p < 0.0001). Perceived obesity also had a significant association with making weight loss attempts; participants who considered themselves to be obese/overweight were more likely than those who did not believe they were obese/overweight to report making weight loss attempts (Chi Square = 42.41, p < 0.0001). With respect to patient-provider communication about weight loss, both being advised to lose weight and SDM about weight loss were significantly associated with making weight loss attempts. Seventy-three percent of participants who had been advised about weight management by their health care provider were currently trying to lose weight compared to 50% of those who did not report provider advice (Chi Square = 12.87, p = 0.0003). Similarly, SDM was significantly greater among participants who were making weight loss attempts [Mean SD = 19.66 (6.2)] compared to those who were not making weight loss attempts [Mean (SD) = 15.27 (6.2)] (t = − 4.30, p < 0.0001).
Table 2.
Bivariate analysis of weight loss attemptsa.
| Variable | Level | % weight loss attempts | Chi Square | p-Value |
|---|---|---|---|---|
| Racial background | Minority Non-minority |
67% 59% |
1.60 | 0.21 |
| Gender | Male Female |
46% 74% |
18.75 | 0.0001 |
| Marital status | Married Not married |
59% 70% |
3.24 | 0.07 |
| Education level | ≥ Some college ≤ High school |
67% 59% |
1.73 | 0.19 |
| Employment status | Employed Not employed |
64% 64% |
0.00 | 1.00 |
| Income level | ˃$20,000 ˂$20,000 |
65% 61% |
0.32 | 0.57 |
| Diabetes | Yes No |
68% 62% |
0.57 | 0.45 |
| Hypertension | Yes No |
65% 61% |
0.44 | 0.51 |
| Obesity status (BMI) | Obese Overweight |
69% 54% |
5.58 | 0.02 |
| Provider advice about weight loss | Yes No |
73% 50% |
12.87 | 0.0003 |
| Perceived obesity | Yes No |
80% 38% |
42.41 | 0.0001 |
| Ready for weight loss | Ready Not ready |
74% 37% |
28.21 | 0.0001 |
| Confidence for weight loss | Confident Not confident |
63% 64% |
0.08 | 0.77 |
Data were self-reported from obese and overweight primary care patients.
Results of the multivariate logistic regression model of weight loss attempts are provided in Table 3. Perceptions about readiness for weight loss/management, beliefs about weight status, and SDM about weight loss/management had significant independent associations with making weight loss attempts. Specifically, participants who believed they were overweight/obese were about six times more likely than those who did not believe they were overweight/obese to be making weight loss attempts (OR = 6.70, 95% CI = 2.86, 15.72, p < 0.0001). In addition, participants who were ready to lose/manage their weight were about four times more likely than those who were not ready to be making weight loss attempts (OR = 4.50, 95% CI = 1.82, 11.09, p = 0.001). Lastly, the likelihood of making weight loss attempts increased as SDM about weight loss/management increased (OR = 1.54, 95% CI = 1.06, 2.22, p = 0.02).
Table 3.
Multivariate logistic regression analysis of weight loss attemptsa.
| Variable | Level | Odds ratio | 95% confidence interval | p-Value |
|---|---|---|---|---|
| Gender | Female Male |
2.25 | 0.91, 5.56 | 0.08 |
| Marital status | Married Not married |
0.63 | 0.33, 1.20 | 0.17 |
| Obesity status (BMI) | Obese Overweight |
0.81 | 0.39, 1.65 | 0.56 |
| Provider advice about weight loss | Yes No |
0.82 | 0.54, 1.24 | 0.35 |
| Perceived obesity | Yes No |
6.70 | 2.86, 15.72 | 0.0001 |
| Ready for weight loss | Ready Not ready |
4.50 | 1.82, 11.09 | 0.001 |
| Shared decision making about weight loss | *** | 1.54 | 1.06, 2.22 | 0.02 |
***OR reflect one SD unit change in continuous variable.
Data were self-reported from obese and overweight primary care patients.
4. Discussion
To our knowledge, this is the first study to examine weight loss attempts in a primary care sample based on racial background, sociodemographic factors, clinical characteristics, patient perceptions about their weight, readiness and confidence for weight loss/management, and patient's shared decision-making with providers about weight loss/management. Examining the association between weight loss attempts and patient perceptions about SDM adds a novel finding to existing knowledge about weight loss attempts. Overall, 64% of participants reported that they were attempting to lose or manage their weight and there were no significant differences in weight loss/management attempts based on racial background or other sociodemographic characteristics. Clearly, weight loss and management is necessary to reduce the obesity epidemic among adults in the US. A majority of participants in the present study reported making attempts to lose weight. Importantly, the rates of making weight loss attempts observed in the present study are higher than those found in previous reports. In a national sample of adults, 28.8% of men and 43.6% of women were making weight loss attempts (Serdula et al., 1999). More recently, Santos and colleagues found that 42% of adults included in epidemiological and observational studies of weight control were trying to lose weight (Santos et al., 2017). The rates we found in our study may be higher because our sample included only patients who were overweight or obese and were part of a primary care practice. The review conducted by Santos et al. found that weight loss attempts were more prevalent among individuals who were overweight or obese. However, obesity status did not have a significant independent association with weight loss attempts in the multivariate logistic regression model in our study. It may be that each patient's perception about whether or not they are obese or overweight is more important than their actual weight when deciding whether to attempt to lose weight. Participants who believed they were obese/overweight had a 6.70 increased likelihood of making weight loss attempts compared to those who did not believe they were obese/overweight. Participants who believe they are obese/overweight may be more motivated to make weight loss attempts. While our finding underscores the importance of patient perceptions in initiating weight loss attempts, future research is needed to characterize the types of strategies that patients are using to lose weight.
We found that the likelihood of making weight loss attempts was increased with being ready to lose or manage one's weight and if participants believed they were overweight or obese. Interestingly, being advised to lose or manage one's weight did not have a significant independent association with making weight loss attempts in the multivariate regression analysis. This finding differs from the results of a meta-analysis which demonstrated that physician recommendation about weight loss had a 3.85 greater odds of patients making attempts to lose weight (Rose et al., 2013). Our findings suggest that the quality of physician counseling about weight management may be among the variables that are important in prompting weight loss attempts. Participants reporting greater SDM with their provider about weight loss/management had an increased likelihood of making weight loss/management attempts whereas being advised by providers to lose weight did not have a significant independent association with making weight loss attempts. SDM is a critical component of patient-centered care (Charles et al., 1997); components of SDM include information sharing during which patients and providers discuss symptoms and treatment options, deliberate about treatment options, discuss patient's concerns and preferences, and make decisions that are based on the provider's recommendation, the patient's self-efficacy, and their ability to implement their provider's recommendation (Charles et al., 1997). SDM is an indicator of the quality of patient-provider communication about weight loss/management with previous research showing that the quality of obesity counseling, or the extent to which providers use all components of the 5A's counseling technique, are associated with motivations and intentions to lose weight (Alexander et al., 2011, Asselin et al., 2017, Jay et al., 2010). However, providers may not be prepared to assess patients' readiness to lose weight, provide concrete assistance, and/or arrange for follow-up appointment and/or referral (Foster et al., 2003, Khandalavala et al., 2014, Jay et al., 2013). Research has shown that the rates of physician counseling about weight loss has declined overall from 7.8% to 6.2% of office visits over a 10–12 year timeframe (Kraschnewski et al., 2013).
Understanding and accepting patients' motivations for changing behavior is essential to patient-centered care and to identifying motivations for behavioral change during obesity counseling, including patients' readiness to change (Befort et al., 2006) and patients' health beliefs (Street and Haidet, 2011, Volger et al., 2012). Incorporating patient-reported data on motivations for and beliefs about health behavior change into electronic health records (EHR) is gaining increased support as evidenced in part by federal mandates to increase the meaningful use of health information (Glasgow et al., 2012). But, the value and impact of adding these data to the EHR is unknown. Our research shows that patients' beliefs about their readiness for weight loss/management and their perceptions about their weight status may be important to consider when advising about weight loss attempts among obese or overweight patients in primary care settings (Volger et al., 2012, Greiner et al., 2008, Ko et al., 2008, Post et al., 2011, Varnado-Sullivan et al., 2010). Data from longitudinal studies are needed to validate these findings before determining how psychological variables can be incorporated into the EHR and used to increase the quality of obesity counseling for weight loss.
In considering the results of this research, some limitations should be noted. First, the observational nature of the study design does not allow us to determine causality with respect to weight loss attempts and racial background, sociodemographic factors, clinical characteristics, SDM, and psychological variables. We recruited a convenience sample of primary care patients and our sample size was modest. Second, a single item was used to evaluate weight loss attempts and we did not measure whether patients had made previous attempts to lose weight. Similarly, we did not ask patients to indicate if they had been advised by their health care provider to lose or manage their weight during a specific time frame. However, similar items have been used to measure weight loss attempts in previous studies with national samples (Serdula et al., 1999). Nevertheless, future studies should examine the relationship between weight loss attempts and patient-level factors in larger samples of primary care patients. It is important for future research to collect longitudinal data on weight loss attempts and measure the specific types of strategies patients are using to lose weight within the context of when they were advised to lose weight by their health care providers. Third, potential confounders such as depression, social support, and body size satisfaction were also not examined. Fourth, weight and height were self-reported data, which may have produced biased estimates of obesity status in this sample, including patient perception of being obese or overweight. However, a novel aspect of our study is that we evaluated the association between weight loss attempts and patient beliefs about their weight, readiness for weight loss/management, and SDM. Understanding patients' beliefs and their perceptions of SDM with providers is necessary to provide patient-centered care. To our knowledge, our study is the first to examine the association between these patient-level factors and weight loss attempts in a sample of primary care patients.
Despite these potential limitations, our research sheds new light on weight loss attempts and shows that many adults who are overweight or obese in a primary care setting are making attempts to lose weight. Primary care providers have an opportunity to play a greater role in obesity reduction and prevention by screening for obesity and overweight and offering behavioral counseling. Future studies are needed to identify meaningful strategies for incorporating patient-reported health beliefs into medical records and determining if inclusion of these data and attention to patient's beliefs improves weight loss attempts among primary care patients and/or shared decision making.
Acknowledgments
This research was supported by grant #U18HS023047 from the Agency for Healthcare Research and Quality. None of the authors have a conflict of interest to disclose. We are very appreciative to the primary care practices and the men and women who participated in this research.
References
- Alexander S.C., Cox M.E., Boling Turer C.L. Do the five A's work when physicians counsel about weight loss? Fam. Med. 2011;43:179–184. [PMC free article] [PubMed] [Google Scholar]
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines OEP Executive summary: guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity. 2014;22:S5–39. doi: 10.1002/oby.20821. [DOI] [PubMed] [Google Scholar]
- An R., Xiang X. Age-period-cohort analyses of obesity prevalence in US adults. Public Health. 2016;141:163–169. doi: 10.1016/j.puhe.2016.09.021. [DOI] [PubMed] [Google Scholar]
- Asselin J., Salami E., Osunlana A.M. Impact of the 5As Team study on clinical practice in primary care obesity management: a qualitative study. CMAJ Open. 2017;5:E322–E329. doi: 10.9778/cmajo.20160090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Befort C.A., Greiner K.A., Hall S. Weight-related perceptions among patients and physicians: how well do physicians judge patients' motivation to lose weight? J. Gen. Intern. Med. 2006;21:1086–1090. doi: 10.1111/j.1525-1497.2006.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry L.L., Flynn A.G., Seiders K., Haws K.L., Quach S.Q. Physician counseling of overweight patients about preventive health behaviors. Am. J. Prev. Med. 2014;46:297–302. doi: 10.1016/j.amepre.2013.12.005. [DOI] [PubMed] [Google Scholar]
- Charles C., Gafni A., Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc. Sci. Med. 1997;44:681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. National Institute of Health Bethesda: National Heart Lung Blood Institute in cooperation with the National Institute of Diabetes and Digetsive and Kidney Diseases; 1998. [Google Scholar]
- Debnam K.J., Holt C.L., Clark E.M. Spiritual health locus of control and health behaviors in African Americans. Am. J. Health Behav. 2012;36:360–372. doi: 10.5993/AJHB.36.3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton G.R., Herman K.G., Tan F. Patient and physician characteristics associated with the provision of weight loss counseling in primary care. Obes. Res. Clin. Pract. 2014;8:e123–130. doi: 10.1016/j.orcp.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster G.D., Wadden T.A., Makris A.P. Primary care physicians' attitudes about obesity and its treatment. Obes. Res. 2003;11:1168–1177. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Kaplan R.M., Ockene J.K., Fisher E.B., Emmons K.M. Patient-reported measures of psychosocial issues and health behavior should be added to electronic health records. Health Aff. (Millwood) 2012;31:497–504. doi: 10.1377/hlthaff.2010.1295. [DOI] [PubMed] [Google Scholar]
- Greiner K.A., Born W., Hall S., Hou Q., Kimminau K.S., Ahluwalia J.S. Discussing weight with obese primary care patients: physician and patient perceptions. J. Gen. Intern. Med. 2008;23:581–587. doi: 10.1007/s11606-008-0553-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman S.J., Risica P.M., Gans K.M., Marcus B.H., Eaton C.B. Tailored weight loss intervention in obese adults within primary care practice: rationale, design, and methods of Choose to Lose. Contemp. Clin. Trials. 2014;38:409–419. doi: 10.1016/j.cct.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay M., Gillespie C., Schlair S., Sherman S., Kalet A. Physicians' use of the 5As in counseling obese patients: is the quality of counseling associated with patients' motivation and intention to lose weight? BMC Health Serv. Res. 2010;10:159. doi: 10.1186/1472-6963-10-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay M.R., Gillespie C.C., Schlair S.L. The impact of primary care resident physician training on patient weight loss at 12 months. Obesity. 2013;21:45–50. doi: 10.1002/oby.20237. [DOI] [PubMed] [Google Scholar]
- Khandalavala B.N., Rojanala A., Geske J.A., Koran-Scholl J.B., Guck T.P. Obesity bias in primary care providers. Fam. Med. 2014;46:532–535. [PubMed] [Google Scholar]
- Ko J.Y., Brown D.R., Galuska D.A., Zhang J., Blanck H.M., Ainsworth B.E. Weight loss advice U.S. obese adults receive from health care professionals. Prev. Med. 2008;47:587–592. doi: 10.1016/j.ypmed.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraschnewski J.L., Sciamanna C.N., Stuckey H.L. A silent response to the obesity epidemic: decline in US physician weight counseling. Med. Care. 2013;51:186–192. doi: 10.1097/MLR.0b013e3182726c33. [DOI] [PubMed] [Google Scholar]
- Kriston L., Scholl I., Holzel L., Simon D., Loh A., Harter M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ. Couns. 2010;80:94–99. doi: 10.1016/j.pec.2009.09.034. [DOI] [PubMed] [Google Scholar]
- LaRose J.G., Leahey T.M., Hill J.O., Wing R.R. Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry. Obesity (Silver Spring) 2013;21(3):449–453. doi: 10.1002/oby.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer V.A., Force U.S.P.S.T. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh A., Shaikh A., Waters E., Atienza A., Moser R.P., Perna F. Health disparities in awareness of physical activity and cancer prevention: findings from the National Cancer Institute's 2007 Health Information National Trends Survey (HINTS) J. Health Commun. 2010;15:60–77. doi: 10.1080/10810730.2010.522694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parchman M.L., Zeber J.E., Palmer R.F. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann. Fam. Med. 2010;8:410–417. doi: 10.1370/afm.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek M.E., Odoms-Young A., Quinn M.T., Gorawara-Bhat R., Wilson S.C., Chin M.H. Race and shared decision-making: perspectives of African-Americans with diabetes. Soc. Sci. Med. 2010;71:1–9. doi: 10.1016/j.socscimed.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post R.E., Mainous A.G., 3rd, Gregorie S.H., Knoll M.E., Diaz V.A., Saxena S.K. The influence of physician acknowledgment of patients' weight status on patient perceptions of overweight and obesity in the United States. Arch. Intern. Med. 2011;171:316–321. doi: 10.1001/archinternmed.2010.549. [DOI] [PubMed] [Google Scholar]
- Rose S.A., Poynter P.S., Anderson J.W., Noar S.M., Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int. J. Obes. 2013;37:118–128. doi: 10.1038/ijo.2012.24. [DOI] [PubMed] [Google Scholar]
- Santos I., Sniehotta F.F., Marques M.M., Carraca E.V., Teixeira P.J. Prevalence of personal weight control attempts in adults: a systematic review and meta-analysis. Obes. Rev. 2017;18:32–50. doi: 10.1111/obr.12466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senechal M., Slaght J., Bouchard D.R. Cumulative weight exposure is associated with different weight loss strategies and weight loss success in adults age 50 or above. J. Aging Res. 2015;2015:904798. doi: 10.1155/2015/904798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serdula M.K., Mokdad A.H., Williamson D.F., Galuska D.A., Mendlein J.M., Heath G.W. Prevalence of attempting weight loss and strategies for controlling weight. JAMA. 1999;282:1353–1358. doi: 10.1001/jama.282.14.1353. [DOI] [PubMed] [Google Scholar]
- Serdula M.K., Khan L.K., Dietz W.H. Weight loss counseling revisited. JAMA. 2003;289:1747–1750. doi: 10.1001/jama.289.14.1747. [DOI] [PubMed] [Google Scholar]
- Stokes A., Ni Y., Preston S.H. Prevalence and trends in lifetime obesity in the U.S., 1988–2014. Am. J. Prev. Med. 2017;53:567–575. doi: 10.1016/j.amepre.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street R.L., Jr., Haidet P. How well do doctors know their patients? Factors affecting physician understanding of patients' health beliefs. J. Gen. Intern. Med. 2011;26:21–27. doi: 10.1007/s11606-010-1453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.G., Wadden T.A., Pillitteri J.L. Disparities by ethnicity and socioeconomic status in the use of weight loss treatments. J. Natl. Med. Assoc. 2009;101:62–70. doi: 10.1016/s0027-9684(15)30813-0. [DOI] [PubMed] [Google Scholar]
- Varnado-Sullivan P.J., Savoy S., O'Grady M., Fassnacht G. Opinions and acceptability of common weight-loss practices. Eat. Weight Disord. 2010;15:e256–264. doi: 10.1007/BF03325307. [DOI] [PubMed] [Google Scholar]
- Volger S., Vetter M.L., Dougherty M. Patients' preferred terms for describing their excess weight: discussing obesity in clinical practice. Obesity. 2012;20:147–150. doi: 10.1038/oby.2011.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden T.A., Volger S., Sarwer D.B. A two-year randomized trial of obesity treatment in primary care practice. N. Engl. J. Med. 2011;365:1969–1979. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]