Abstract
Although e-cigarette use is increasing dramatically, numerous concerns persist regarding toxicity and their role in smoking cessation. We assessed beliefs and behavior regarding e-cigarettes in an adult French population.
The 4th French nationwide observational survey, EDIFICE 4, was conducted among representative samples of 1602 laypersons (age, 40–75 years) from 12 June-10 July 2014, using the quota method. Profile, beliefs and behavior were assessed by phone interviews of the participating lay population with no history of cancer (N = 1463). Tobacco use, nicotine dependence (Fagerström test) and e-cigarette use were assessed.
E-cigarette users represented 6% of the study lay population. E-cigarette users regarded e-cigarettes as helpful for quitting tobacco smoking and reducing the risk of lung cancer. Current dual users (e-cigarettes + cigarettes) were more likely to attempt to quit than current exclusively cigarette smokers (odds ratio, 3.15 [1.74–5.70]), and to consider themselves at higher risk for lung cancer (OR 3.85 [2.47–5.99]). They also considered e-cigarette vapor to be less toxic than tobacco smoke in terms of both active and passive exposure.
Dual users typically consider themselves at higher risk for cancer and intend to quit smoking. Physicians should be made aware of this specific sub-population for whom e-cigarettes may be a useful trigger in the smoking cessation process.
Keywords: Electronic cigarettes, Smoking cessation, Tobacco use, Lung neoplasms, Pulmonary disease, Risk factors, Smoke
Highlights
-
•
Dual-users are more likely to attempt to quit cigarettes than cigarette-only smokers.
-
•
Dual-users consider themselves at higher risk for cancer than cigarette-only smokers.
-
•
Nicotine dependence did not differ between dual users and current cigarette smokers.
-
•
Current e-cigarette users insist on the efficacy of e-cigarettes to quit smoking.
-
•
Users consider e-cig vapor less toxic than tobacco in terms of both active & passive exposure.
1. Introduction
The use of e-cigarettes has increased dramatically in recent years. Use by both adolescents and adults doubled worldwide between 2008 and 2012 (FCTC WHO Framework Convention on Tobacco Control, 2014). In 2014, there were three million users in France i.e., 6% of the French population (Andler et al., 2016).
However, the role of e-cigarettes in facilitating smoking cessation or in lowering the social stigma attached to tobacco use remains controversial (Cressey, 2013; Cressey, 2014; Editorial, 2014; Polosa, 2015; Bullen et al., 2013). A number of studies have assessed the toxicity of e-cigarettes (Scheffler et al., 2015; Sussan et al., 2015; Marco and Grimalt, 2015; Goniewicz et al., 2014; Nutt et al., 2014) and several reviews (Hajek et al., 2014; McNeill et al., 2015; Callahan-Lyon, 2014; Pisinger and Dossing, 2014; Dinakar and O'Connor, 2016; McRobbie et al., 2014) have attempted to establish a consensus with regard to management of e-cigarette consumption. The main conclusions are that e-cigarettes contain smaller quantities of toxic substances and in lower concentrations than tobacco cigarettes. However, in the absence of evidence-based proof of non-toxicity, expert guidelines from both the WHO (FCTC WHO Framework Convention on Tobacco Control, 2014) and French institutions (Office français de prévention du tabagisme (OFT), 2013; Haute autorité de santé (HAS), 2014) all recommend a precautionary approach.
Whether e-cigarettes are useful in the cessation of tobacco use or whether they are actually associated with a lower rate of tobacco cessation among smokers is unknown and contradictory findings have emerged (Rahman et al., 2015; Kalkhoran and Glantz, 2016). Nicotine-containing e-cigarettes have been shown to be effective for reducing consumption or delaying relapse (Bullen et al., 2013; Rahman et al., 2015; Siegel et al., 2011; Farsalinos et al., 2014; Etter and Bullen, 2014; Caponnetto et al., 2013; Adriaens et al., 2014). Recent findings have however shown that e-cigarette use in younger adults is associated with a significantly higher risk of becoming a (cigarette) smoker (Miech et al., 2017; McCabe et al., 2017).
Attempts have been made to define the profile of ever-users of e-cigarettes (Huang et al., 2016; Pineiro et al., 2016). These surveys did not however assess beliefs or knowledge among the general population with regard to the risks of exposure to or the potential harm or benefits of e-cigarettes vs. conventional cigarettes. To the best of our knowledge, the links between nicotine dependence and the use of e-cigarettes have seldom been addressed (Gonzalez Roz et al., 2017).
We investigated beliefs and behaviors regarding e-cigarettes in an adult French population.
2. Methods
The aim of the EDIFICE nationwide observational surveys is to improve insight into the behavior of the French population with regard to cancer prevention and participation in screening programs. They are conducted in the target populations for national screening programs, i.e., age range, 40 to 75 years. EDIFICE 4 was conducted by phone interviews from June 12 to July 10, 2014 among a selected population of 1602 individuals. Representativeness of the survey sample for gender, age, profession, geographical area and community size as compared to the French general population, was ensured by the method of quotas (Deville, 1991), based on the statistics of the French Employment Survey conducted in 2009 and updated in 2011 by the French National Institute for Statistics and Economic Studies (Institut National de Statistiques et d'Etudes Economiques [INSEE]). Phone interviews were conducted by experienced independent interviewers using a computer-assisted questionnaire. The present analysis focuses on individuals with no history of cancer (N = 1463).
All interviewees provided information on sociodemographic characteristics and answered questions about their beliefs and knowledge of e-cigarette use and related risks. They were also asked about smoking habits, including cigarettes, cigars and pipe. For the sake of simplicity, and also because there were very few cigar-only or pipe-only smokers in our sample, we have used the term “cigarette-smoker” to refer to all types of inhaled tobacco products, cigars and pipe included.
We defined three categories of cigarette (and cigar and pipe) users according to the questionnaire answers: (i) never-smokers (individuals who have smoked <100 cigarettes throughout their lifetime (Couraud et al., 2012)); (ii) former smokers (individuals who quit smoking at least one year ago and who have smoked >100 cigarettes throughout their lifetime); and (iii) current smokers (individuals who currently smoke or quit less than one year prior to the interview). For e-cigarettes, we defined two categories: e-cigarette users (currently using e-cigarettes at the time of the survey) and e-cigarette non-users (not currently using e-cigarettes). Of note, former e-cigarettes users were categorized as non-users. The following categories of cigarette smokers and e-cigarette users were therefore used: exclusively cigarette smokers (current or former), dual users (current simultaneous cigarette smoking and e-cigarette use) and e-cigarette users only (not currently cigarette smokers).
Nicotine dependence was assessed using the Fagerström Test for Cigarette Dependence (FTCD) (Heatherton et al., 1991) among interviewees who reported current cigarette use. All interviewees were asked about their perception of the risk of lung cancer for themselves and for others. Individual awareness of the risk of lung cancer was assessed by the question: “How do you evaluate your own risk of lung cancer? Is it higher, lower or identical to that of the average population?”
Comparisons between two populations were made using Student's t-test for quantitative data, and the Z-test and the chi-squared test for the comparison of percentages and numbers, respectively, in the case of categorical data. Differences were considered statistically significant when the probability value was <0.05 (bilateral test). The detailed methodology of these iterative surveys has been described previously (Roussel and Touboul, 2011).
3. Results
3.1. Demographics
The demographics of the study population of 1463 individuals with no history of cancer together with tobacco status and e-cigarette use are presented in Table 1. Exclusively cigar-smokers or exclusively pipe-smokers represented 3% (10/353) and 1.5% (5/353) of the current smokers in the lay population, respectively.
Table 1.
Characteristics, smoking status and e-cigarette use in lay population.
| Variable N(%) | Lay population |
|---|---|
| N = 1463 (100%) | |
| Gender | |
| Male | 726 (50%) |
| Female | 737 (50%) |
| Socioeconomic category⁎ | |
| SPC+ | 468 (32%) |
| SPC- | 438 (30%) |
| Unemployed (inc. retired) | 557 (38%) |
| Smoking status (cigarettes, cigars, pipes) | |
| Never-smokers | 625 (43%) |
| Former smokers | 481 (33%) |
| Current smokers | 353 (24%) |
| Missing data | 4 (<1%) |
| Mean pack-year consumption (cigarette; SD) | |
| Current smokers | 14.80 (13.31) |
| Former smokers | 21.33 (21.87) |
| Intention to quit cigarette | 195 (55%) |
| E-cigarette users | |
| All | 93 (6%) |
| Only e-cigarettes | 19 (1%) |
| Dual users | 74 (5%) |
| E-cigarette use | N = 93 (100%) |
| Average times per day (SD) | 9.9 (11.0) |
| Nicotine-containing liquid | 81 (88%) |
| Methods of use | |
| Substitute for conventional cigarettes | 76 (82%) |
| Concomitantly with conventional cigarettes | 17 (18%) |
| Reasons for using e-cigarettes: | |
| To quit smoking | 64 (69%) |
| To reduce tobacco consumption | 22 (24%) |
| Neither of these | 6 (7%) |
Socioprofessional category, high (SPC+) and low (SPC-).
3.2. E-cigarette use in the lay population
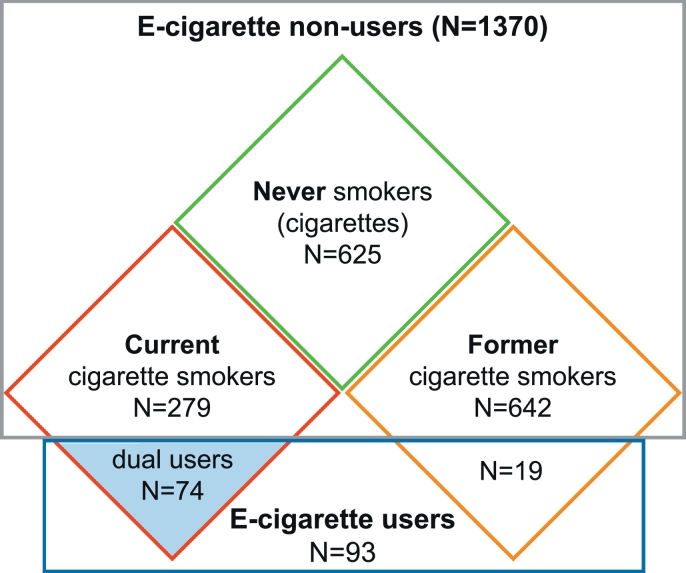
Of the total study population, 6% (N = 93) reported using e-cigarettes. The majority were currently dual users (N = 74, 5%), and 1% were former cigarette smokers (N = 19) (Table 1). All current e-cigarette users had a personal history of cigarette smoking (Fig. 1).
Fig. 1.
Venn diagram showing distribution of the lay population regarding smoking profiles and e-cigarette use (N = 1463). Missing data are not displayed (N = 4).
The profile of e-cigarette users in the lay population are reported in Table 1. For 82%, e-cigarettes were a substitute for conventional cigarette consumption and for 69% they were a way to quit smoking, though, 7% claimed to use them neither to quit nor to reduce cigarette consumption. Nicotine-containing e-liquid was used by 88% of e-cigarette users. Of the e-cigarette-users who expressed a long-term ambition to cease tobacco consumption, the majority reported having replaced conventional cigarettes by e-cigarettes: 88% of those who considered e-cigarettes as a means to cease tobacco consumption and 62% of those who considered e-cigarettes as a means to reduce tobacco consumption (P = 0.02, data not shown).
Table 2 compares the characteristics of e-cigarette users and e-cigarette non users depending on their smoking status. More males than females reported current exclusively cigarette smoking (53% males), e-cigarette use only (65% males) and dual use (63% males). No significant differences were observed between these patterns of consumption in males. Current smokers from lower socioprofessional categories reported current dual use significantly more frequently than exclusively cigarette smoking (56% vs 39%, P = 0.01). Former smokers in the unemployed category were less likely to use e-cigarettes (17% vs 44%, P = 0.04). Among current smokers, exclusively cigarette smokers and dual users did not differ significantly in terms of nicotine dependence. Nicotine-containing e-liquid was more likely to be used by moderately and highly nicotine-dependent e-cigarette users (100%) than by those who were not dependent (84%, P = 0.05).
Table 2.
Comparison of smoking status of e-cigarette users and non-users in the lay population.
| Current cigarette smokers (N = 353) |
Former cigarette smokers (N = 481) |
E-cig users, Current vs. Former smokers |
|||||
|---|---|---|---|---|---|---|---|
| Cigarette only N = 279 A |
Dual users N = 74 B |
P value A vs. B |
E-cig non users N = 462 C |
Current E-cig users N = 19 D |
P value C vs. D |
P value B vs.D |
|
| Gender | |||||||
| Male | 148 (53%) | 47 (63%) | NS | 277 (60%) | 12 (65%) | NS | NS |
| Female | 131 (47%) | 27 (37%) | NS | 185 (40%) | 6 (35%) | NS | NS |
| Socioprofessional categories | |||||||
| SPC+ | 95 (34%) | 22 (30%) | NS | 140 (30%) | 7 (40%) | NS | NS |
| SPC- | 108 (39%) | 42 (56%) | 0.01 | 122 (26%) | 8 (43%) | NS | NS |
| Unemployed (inc. retired) | 76 (27%) | 11 (14%) | 0.03 | 200 (44%) | 3 (17%) | 0.04 | NS |
| Self-assessment of LC risk | |||||||
| Higher than average population | 128 (46%) | 45 (61%) | 0.03 | 62 (14%) | 8 (42%) | <0.01 | NS |
| Same as average population | 119 (43%) | 25 (33%) | NS | 223 (48%) | 11 (58%) | NS | NS |
| Lower than average population | 23 (8%) | 2 (3%) | 0.05 | 162 (35%) | 0 (0%) | <0.01 | NS |
| No answer | 9 (3%) | 2 (3%) | 15 (3%) | – | |||
| Considering LC screening for self | 101 (36%) | 32 (43%) | NS | 96 (21%) | 2 (11%) | NS | 0.02 |
| Intention to quit smoking | |||||||
| Yes | 139 (50%) | 56 (76%) | <0.01 | – | – | – | – |
| No | 133 (47%) | 17 (23%) | <0.01 | – | – | – | – |
| No answer | 8 (3%) | 1 (1%) | – | – | – | – | |
| Level of nicotine dependence (N = 330)* | N = 261 | N = 69 | – | – | – | ||
| No dependence | 141 (54%) | 29 (42%) | NS | – | – | – | – |
| Low dependence | 53 (20%) | 18 (26%) | NS | – | – | – | – |
| Moderate dependence | 46 (18%) | 14 (20%) | NS | – | – | – | – |
| High dependence | 21 (8%) | 8 (12%) | NS | – | – | – | – |
E-cig: e-cigarette; smokers: conventional-cigarette smokers; users: e-cigarette users; LC: lung cancer; * 330 conventional-cigarette smokers (excluding pipe, cigar and cigarillos). SPC: Socioprofessional category, high (SPC+) and low (SPC-).
Current dual-users were significantly more likely to attempt to quit smoking than current cigarette smokers (odds ratio [OR], 3.15 [1.74–5.70]). They were also more likely to consider themselves at higher risk of lung cancer than the average population, compared to current exclusively cigarette smokers (61% vs. 46%; P = 0.03). Similarly, current e-cigarette users with a personal history of cigarette smoking (i.e. former smokers) considered themselves at higher risk than former cigarette smokers (42% vs. 14%; P < 0.01).
Overall, e-cigarette users considered themselves at higher risk for lung cancer than exclusively cigarette smokers (current and former) (OR 3.85 [95% CI: 2.47–5.99]). E-cigarette use was not associated with the intention to undergo lung cancer screening, either in current smokers (43% in dual users vs. 36%, NS) or among former smokers (11% in e-cigarette users vs. 21%, NS).
3.3. Opinions on e-cigarettes
Over half (58%) of our sample population believed e-cigarettes to be potentially useful for trying to reduce cigarette consumption or to quit smoking (31%) (Table 3). Current e-cigarette users had far greater confidence in e-cigarettes as an aide to smoking cessation than non-users (48% vs. 30%; P < 0.01). Forty-four percent of users considered e-cigarettes as a means to reduce cigarette smoking compared to 59% of non-users (P = 0.01). In contrast to e-cigarette non-users, e-cigarette users were more likely to rate them as the most effective method to reduce lung cancer mortality (35% vs 11%; P < 0.01) (data not shown).
Table 3.
Lay population opinions of e-cigarettes.
| Opinion of e-cigarettes | Lay population N = 1463 (100%) |
|---|---|
| Are e-cigarettes a means for smokers toa: | |
| Quit smoking? | 462 (31%) |
| Reduce tobacco consumption? | 846 (58%) |
| No answer | 156 (11%) |
| For users, compared to tobacco smoke, is e-cigarette vapor: | |
| Less harmful for active users? | 621 (42%) |
| As harmful for active users? | 639 (44%) |
| More harmful for active users? | 57 (4%) |
| No answer | 147 (10%) |
| For passive inhalation, compared to tobacco smoke, is e-cigarette vapor: | |
| Less harmful? | 795 (54%) |
| As harmful? | 480 (33%) |
| More harmful? | 41 (3%) |
| No answer | 147 (10%) |
| Which of the following would be the most effective measure to reduce lung cancer mortality?b | |
| Increasing cigarette prices | 324 (22%) |
| Screening | 779 (53%) |
| Promoting development of e-cigarettes | 180 (12%) |
| None of these | 157 (11%) |
| No answer | 23 (2%) |
Questions: a “In your opinion, even for users who do not necessarily intend to quit smoking, e-cigarettes are a means for smokers to …?”; b “In your opinion, which of the following would be effective measures to reduce lung cancer mortality, …?”
Similar results were found regarding smoking status (Supplemental Table 1). Among current e-cigarettes users, former smokers were more likely than current smokers (i.e., dual-users) to see e-cigarettes as a way to quit smoking (79% vs 41%; P < 0.01).
Forty-two percent of the study participants believed that e-cigarette vapor is less toxic (than conventional-cigarette smoke) for active inhalers; and 54% of the total population believed it to be less toxic for passive inhalers (Supplemental Table 2). Current smokers are more likely than former and never smokers to believe that passive exposure to e-cigarettes is less toxic (61% vs 53 and 51% respectively, P = 0.01) (Supplemental Table 2). E-cigarette users were significantly more likely than e-cigarette non-users to believe e-cigarette vapor is less toxic than conventional-cigarette smoke both for the user and for passive inhalers (71% vs 41%; P ≤ 0.01 and 85% vs. 53%; P ≤ 0.01, respectively) (Supplemental Table 2).
4. Discussion
The present analysis provides an overview of e-cigarette use in France in 2014. Six percent of the study population were e-cigarette users, which can be extrapolated to an estimated 1.6 million individuals aged 40 to 75 years in the country as a whole (27.3 million at the time of the survey, in 2014). A history of tobacco use is very likely among e-cigarette users: 80% were currently dual users; 20% were former smokers but currently exclusively e-cigarette users.
No significant differences were observed between cigarette smokers and dual users in terms of nicotine dependence. Current e-cigarette users and former smokers in particular, declared using e-cigarettes as a smoking-cessation tool. Compared with non-users, e-cigarette users were more likely to consider themselves at higher risk of lung cancer (than the average population), or to intend quitting tobacco smoking. E-cigarette users believed e-cigarette vapor to be less toxic than tobacco smoke.
A study conducted in 2014 by the French National Institute for Healthcare Prevention and Education (Institut national de prévention et d'éducation pour la santé [INPES]) reported a rate of 6.0% of regular e-cigarette users among the 15–75-year age group (Andler et al., 2015). The figures we observed in our 40–75-year age group may reflect an increasingly higher overall prevalence given that e-cigarette consumption is known to be lower in the upper age categories (Andler et al., 2015).
One recent study reported a similar sociodemographic profile of e-cigarette users (male, lower socioeconomic status) (Huang et al., 2016) to our own. In line with previously published data, the majority of e-cigarette users in our survey were dual-users (Huang et al., 2016; Andler et al., 2015; Pasquereau et al., 2017). E-cigarette users typically have greater awareness of tobacco-related specific risks (Pepper et al., 2015). Although e-cigarettes are recognized as a helpful tool for ceasing or reducing tobacco-consumption (Farsalinos et al., 2014; Adkison et al., 2013), sustained cessation is dependent on the type of device and frequency of use (Hitchman et al., 2015; Chen et al., 2016), and the possible high expectations of the user (Harrell et al., 2015).
Our findings on dual use can be put into perspective with a recent publication (Adriaens et al., 2017). Overall, 215 e-cigarette users (40 dual-users and 175 switchers, i.e., current smokers who ceased smoking by switching to e-cigarette use) completed an online questionnaire. Dual-users decreased tobacco consumption after taking up e-cigarettes but recognized smoking reduction (rather than quitting) as a better justification for e-cigarette use. They opted for e-cigarettes to reduce exposing others to second-hand smoke but reported more practical problems (battery, reservoir) with e-cigarettes and more negative consequences on their own health.
In line with previously published figures of 0.9% (Andler et al., 2015), approximately 1% (N = 19/1463) of our total study population were former cigarette smokers and current e-cigarette users. Twenty percent (19/93) of e-cigarette users in our survey were former smokers who switched to e-cigarettes. Although this figure is higher, it is still comparable with the 15% reported in the literature (Andler et al., 2016; Andler et al., 2015).
These, and our own observations should be considered in light of the latest standpoints taken by health authorities worldwide. In May 2016, in response to the American Lung Association, the American Food and Drug Administration extended its regulatory authority to cover e-cigarettes (US and Food Administration (FDA), 2016). In April 2016, a report by the Royal College of Physicians (United Kingdom) concluded that e-cigarettes were likely to be beneficial to UK health, thus encouraging smokers to use them (Royal College of Physicians, 2016). The French High Council for Public Health (High Council for Public Health, 2016) called for wider dissemination of information to smokers and healthcare professionals, on two points in particular: e-cigarettes are a useful tool for helping tobacco cessation for those who so wish; e-cigarettes are a means of reducing tobacco-related health risks.
Our study does have several limitations, which are related to the potential bias of declarative surveys (social desirability response bias and memorization bias). Given that we limited our study to individuals within the target population for cancer screening programs (40–75 years), youth and young adults who may be particularly at risk of e-cigarette use were not included. A number of our observations were also made on small sample sizes, such as the sub-group of former and current smokers who also currently use e-cigarettes (dual-users). The survey does however have the advantage of a robust, validated methodology. Our findings will help boost the limited data available, and define the new public health issues surrounding the increasing use of e-cigarettes.
5. Conclusion
E-cigarette use is typically associated with on-going conventional-cigarette use. Dual users exhibit a complex pattern of behavior with regard to smoking. They want to quit and e-cigarettes are a means to this end. Independently of their level of nicotine dependence, their attitude is conditioned by the fact that they believe their own risk of lung cancer is greater than that of the general population. However, their opinion of the efficacy of lung cancer screening does not differ from that of non-users. In contrast to non-users, e-cigarette users tend to emphasize the potential benefits of e-cigarettes as a way to quit and/or reduce lung cancer mortality. In line with current cigarette smokers, e-cigarette users also believe e-cigarette vapor is less harmful than cigarette smoke, in terms of both active and passive exposure. Physicians should be made aware of the specific sub-population of dual-users for whom e-cigarettes may be a useful trigger in the smoking cessation process.
The following are the supplementary data related to this article.
Opinions on e-cigarettes according to tobacco (cigarette) status.
Proportion of individuals who believed vapor from nicotine-containing e-cigarettes to be less, more, or as harmful as the smoke from tobacco cigarettes, for active and passive smokers.
Conflict of interest statement
Sébastien Couraud, Alexis B. Cortot, Xavier B. Pivot, François Eisinger, Jean-François Morère, Jean-Yves Blay, Laurent Greillier have received honoraria from Roche SA.
Christine Lhomel is an employee of Roche SA.
Chantal Touboul and Jérôme Viguier have no conflicts of interest to declare.
Acknowledgments
The Edifice surveys are funded by Roche SA.
The publication of this article was funded by Roche SA.
Medical writing assistance was provided by Potentiel d'Action (France) and funded by Roche SA.
Contributor Information
Sébastien Couraud, Email: sebastien.couraud@chu-lyon.fr.
Alexis B. Cortot, Email: alexis.cortot@chru-lille.fr.
Xavier B. Pivot, Email: xavier.pivot@univ-fcomte.fr.
Chantal Touboul, Email: chantal.touboul@kantarhealth.com.
Christine Lhomel, Email: christine.lhomel@roche.com.
Jean-Yves Blay, Email: jean-yves.blay@lyon.unicancer.fr.
François Eisinger, Email: eisingerf@ipc.unicancer.fr.
Jérôme Viguier, Email: jviguier@institutcancer.fr.
Jean-François Morère, Email: jean-francois.morere@pbr.aphp.fr.
Laurent Greillier, Email: laurent.greillier@ap-hm.fr.
References
- Adkison S.E., O'Connor R.J., Bansal-Travers M. Electronic nicotine delivery systems: international tobacco control four-country survey. Am. J. Prev. Med. 2013;44(3):207–215. doi: 10.1016/j.amepre.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adriaens K., Van Gucht D., Declerck P., Baeyens F. Effectiveness of the electronic cigarette: an eight-week Flemish study with six-month follow-up on smoking reduction, craving and experienced benefits and complaints. Int. J. Environ. Res. Public Health. 2014;11(11):11220–11248. doi: 10.3390/ijerph111111220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adriaens K., Van Gucht D., Baeyens F. Differences between dual users and switchers center around vaping behavior and its experiences rather than beliefs and attitudes. Int. J. Environ. Res. Public Health. 2017;15(1) doi: 10.3390/ijerph15010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andler R., Guignard R., Wilquin J.-L., Beck F., Nguyen-Thanh V. Vol. 33. 2015. L'usage de la cigarette électronique en France en 2014. Évolutions, résultats d'études et de recherches en prévention et en éducation pour la santé. [Google Scholar]
- Andler R., Guignard R., Wilquin J.L., Beck F., Richard J.B., Nguyen-Thanh V. Electronic cigarette use in France in 2014. Int. J. Publ. Health. 2016;61(2):159–165. doi: 10.1007/s00038-015-0773-9. [DOI] [PubMed] [Google Scholar]
- Bullen C., Howe C., Laugesen M. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- Caponnetto P., Campagna D., Cibella F. EffiCiency and safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8(6) doi: 10.1371/journal.pone.0066317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan-Lyon P. Electronic cigarettes: human health effects. Tob. Control. 2014;23(Suppl. 2):ii36–40. doi: 10.1136/tobaccocontrol-2013-051470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Zhuang Y.L., Zhu S.H. E-cigarette design preference and smoking cessation: a U.S. population study. Am. J. Prev. Med. 2016;51(3):356–363. doi: 10.1016/j.amepre.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couraud S., Zalcman G., Milleron B., Morin F., Souquet P.J. Lung cancer in never smokers—a review. Eur. J. Cancer. 2012;48(9):1299–1311. doi: 10.1016/j.ejca.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Cressey D. Regulation stacks up for e-cigarettes. Nature. 2013;501(7468):473. doi: 10.1038/501473a. [DOI] [PubMed] [Google Scholar]
- Cressey D. E-cigarettes: the lingering questions. Nature. 2014;513(7516):24–26. doi: 10.1038/513024a. [DOI] [PubMed] [Google Scholar]
- Dinakar C., O'Connor G.T. The health effects of electronic cigarettes. N. Engl. J. Med. 2016;375(14):1372–1381. doi: 10.1056/NEJMra1502466. [DOI] [PubMed] [Google Scholar]
- Deville J. A theory of quota surveys. Surv. Methodol. 1991;17(2):163–181. [Google Scholar]
- Editorial E-cigarettes—aid to smoking cessation or smokescreen? Lancet. 2014;384(9946):829. doi: 10.1016/S0140-6736(14)61470-7. [DOI] [PubMed] [Google Scholar]
- Etter J.F., Bullen C. A longitudinal study of electronic cigarette users. Addict. Behav. 2014;39(2):491–494. doi: 10.1016/j.addbeh.2013.10.028. [DOI] [PubMed] [Google Scholar]
- Farsalinos K.E., Romagna G., Tsiapras D., Kyrzopoulos S., Voudris V. Characteristics, perceived side effects and benefits of electronic cigarette use: a worldwide survey of more than 19,000 consumers. Int. J. Environ. Res. Public Health. 2014;11(4):4356–4373. doi: 10.3390/ijerph110404356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FCTC WHO Framework Convention on Tobacco Control Electronic Nicotine Delivery Systems. 2014. http://apps.who.int/gb/fctc/PDF/cop6/FCTC_COP6_10-en.pdf July 21 2014. Available from:
- Goniewicz M.L., Knysak J., Gawron M. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob. Control. 2014;23(2):133–139. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez Roz A., Secades Villa R., Weidberg S. Evaluating nicotine dependence levels in e-cigarette users. Adicciones. 2017;0(0):905. doi: 10.20882/adicciones.905. [DOI] [PubMed] [Google Scholar]
- Hajek P., Etter J.F., Benowitz N., Eissenberg T., McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–1810. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell P.T., Simmons V.N., Pineiro B. E-cigarettes and expectancies: why do some users keep smoking? Addiction. 2015;110(11):1833–1843. doi: 10.1111/add.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haute autorité de santé (HAS) Arrêt de la consommation de tabac: du dépistage individuel au maintien de l'abstinence en premier recours. 2014. Recommandation de bonne pratique. [Google Scholar]
- Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerström K.O. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br. J. Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- High Council for Public Health . Haut Conseil de la santé publique; 2016. Opinion Concerning the Risks and Benefits in the Use of Electronic Cigarettes by the General Population. [Google Scholar]
- Hitchman S.C., Brose L.S., Brown J., Robson D., McNeill A. Associations between E-cigarette type, frequency of use, and quitting smoking: findings from a longitudinal online panel survey in great Britain. Nicotine Tob. Res. 2015;17(10):1187–1194. doi: 10.1093/ntr/ntv078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Kim Y., Vera L., Emery S.L. Electronic cigarettes among priority populations: role of smoking cessation and tobacco control policies. Am. J. Prev. Med. 2016;50(2):119–209. doi: 10.1016/j.amepre.2015.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S., Glantz S.A. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir. Med. 2016;4(2):116–128. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marco E., Grimalt J.O. A rapid method for the chromatographic analysis of volatile organic compounds in exhaled breath of tobacco cigarette and electronic cigarette smokers. J. Chromatogr. A. 2015;1410:51–59. doi: 10.1016/j.chroma.2015.07.094. [DOI] [PubMed] [Google Scholar]
- McCabe S.E., Veliz P., McCabe V.V., Boyd C.J. Smoking behaviors and intentions among current e-cigarette users, cigarette smokers, and dual users: a national survey of U.S. high school seniors. Prev. Med. 2017;99:228–235. doi: 10.1016/j.ypmed.2017.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill A., Brose L., Calder R., Hitchman S., Hajek P., McRobbie H. Public health england; 2015. E-Cigarettes: An Evidence Update.https://www.gov.uk/government/publications/e-cigarettes-an-evidence-update Available from: [DOI] [PubMed] [Google Scholar]
- McRobbie H., Bullen C., Hartmann-Boyce J., Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst. Rev. 2014;12 doi: 10.1002/14651858.CD010216.pub2. [DOI] [PubMed] [Google Scholar]
- Miech R., Patrick M.E., O'Malley P.M., Johnston L.D. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob. Control. 2017;26(e2):e106–e111. doi: 10.1136/tobaccocontrol-2016-053291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt D.J., Phillips L.D., Balfour D. Estimating the harms of nicotine-containing products using the MCDA approach. Eur. Addict. Res. 2014;20(5):218–225. doi: 10.1159/000360220. [DOI] [PubMed] [Google Scholar]
- Office français de prévention du tabagisme (OFT) Office français de prévention du tabagisme (OFT); 2013. Rapport et avis d'experts sur l'e-cigarette; pp. 198–202. [Google Scholar]
- Pasquereau A.G.A., Andler R., Guignard R., Richard J.B., Nguyen-Thanh V. le groupe Baromètre santé 2016. Tobacco and e-cigarette in France: levels of consumption according to the preliminary results from the 2016 health barameter [Tabac et e-cigarette en France: niveaux d'usage d'après les premiers résultats du Baromètre santé 2016] Bull. Epidémiol. Hebd. 2017;12:214–222. [Google Scholar]
- Pineiro B., Correa J.B., Simmons V.N. Gender differences in use and expectancies of e-cigarettes: online survey results. Addict. Behav. 2016;52:91–97. doi: 10.1016/j.addbeh.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper J.K., Emery S.L., Ribisl K.M., Rini C.M., Brewer N.T. How risky is it to use e-cigarettes? Smokers' beliefs about their health risks from using novel and traditional tobacco products. J. Behav. Med. 2015;38(2):318–326. doi: 10.1007/s10865-014-9605-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisinger C., Dossing M. A systematic review of health effects of electronic cigarettes. Prev. Med. 2014;69:248–260. doi: 10.1016/j.ypmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- Polosa R. E-cigarettes: Public Health England's evidence based confusion? Lancet. 2015;386(10000):1237–1238. doi: 10.1016/S0140-6736(15)00133-6. [DOI] [PubMed] [Google Scholar]
- Rahman M.A., Hann N., Wilson A., Mnatzaganian G., Worrall-Carter L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussel C., Touboul C. Large population survey: strengths and limits. Methodology of the EDIFICE survey. Eur. J. Cancer Prev. 2011;20(Suppl. 1):S5–7. doi: 10.1097/01.cej.0000391561.10889.28. [DOI] [PubMed] [Google Scholar]
- Royal College of Physicians Promote E-Cigarettes Widely as Substitute for Smoking Says New RCP Report 2016 [updated April 28, 2016] 2016. https://www.rcplondon.ac.uk/news/promote-e-cigarettes-widely-substitute-smoking-says-new-rcp-report Available from:
- Scheffler S., Dieken H., Krischenowski O., Forster C., Branscheid D., Aufderheide M. Evaluation of e-cigarette liquid vapor and mainstream cigarette smoke after direct exposure of primary human bronchial epithelial cells. Int. J. Environ. Res. Public Health. 2015;12(4):3915–3925. doi: 10.3390/ijerph120403915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel M.B., Tanwar K.L., Wood K.S. Electronic cigarettes as a smoking-cessation tool: results from an online survey. Am. J. Prev. Med. 2011;40(4):472–475. doi: 10.1016/j.amepre.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Sussan T.E., Gajghate S., Thimmulappa R.K. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0116861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US and Food Administration (FDA) The Facts on the FDA's New Tobacco Rule 2016 [updated June 16, 2016] 2016. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm506676.htm Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Opinions on e-cigarettes according to tobacco (cigarette) status.
Proportion of individuals who believed vapor from nicotine-containing e-cigarettes to be less, more, or as harmful as the smoke from tobacco cigarettes, for active and passive smokers.