Abstract
Instituting interventions during the prenatal period is optimal for early obesity prevention in the child. Healthy Eating Active Living (HEAL) is a six-week, multi-component program to promote breastfeeding, healthy dietary habits, cooking skills and physical activity among Medicaid-eligible pregnant-women in Texas. HEAL is integrated into the healthcare system and offered as a standard-of-care for eligible patients. Methods: Preliminary evaluation of this natural experiment conducted from March 2015 through October 2016 informs the initial feasibility, acceptability and effects of the program on participant diet, home nutrition environment, physical activity, and breastfeeding self-efficacy and intentions measured using self-report surveys. Analysis of covariance (ANCOVA) was conducted to evaluate pre- and post-intervention changes, controlling for participants' ethnicity, age, and income level. Interaction effects of session attendance on the outcomes were further assessed. Results: Of the 329 women who enrolled in HEAL, 210 women completed the pre-post assessment (64% retention rate). Pre-to-post intervention, there were significant increases in availability and intake of fruits and vegetables, self-efficacy towards consuming more fruits and vegetables, and cooking frequency and skills (p < 0.05), and decreased frequency of eating heat and serve foods (p < 0.05). Significant improvements in physical activity, duration of breastfeeding, perceived benefits and intentions to breastfeed were also observed (p < 0.05). Higher attendance of HEAL sessions was associated with better outcomes. Process evaluation demonstrated 95% fidelity of program implementation. Conclusion: HEAL operationalizes clinic-community linkages and shows promise in improving behaviors during pregnancy. Future research warrants the use of a stringent study design with a control group to determine program efficacy.
Keywords: Pregnancy, Obesity prevention, Nutrition, Breastfeeding, Physical activity
1. Introduction
Obesity rates among adults and children continue to remain at epidemic proportions in the United States (U.S.) (Hales et al., 2015). The state of Texas has witnessed a steady increase in the adult obesity rates from 10.7% in 1990, to 25.3% in 2004, to 33.7% in 2016 (Trust for America's Health and Robert Wood Johnson Foundation, 2016). Children are not spared, with obesity rates currently as high as 19.1% in the 10 to 17-year age group, and 15.7% among high school children(Trust for America's Health and Robert Wood Johnson Foundation, 2016). Pre-pregnancy obesity rates (Body Mass Index, BMI ≥30.0) among women have also climbed from 13.0% in 1994 to 24.8% in 2014 (Branum et al., 2016). Furthermore, in 2014, the rates of obesity was highest among Hispanic, non-Hispanic black or non-Hispanic Native American or Alaska Native women using Medicaid for payment of delivery (Branum et al., 2016). Approximately 50% of direct medical expenditures attributable to obesity are funded through Medicaid and Medicare (Finkelstein et al., 2003).
Evidence suggests that obesity interventions instituted early in the human life cycle result in a greater magnitude of effect than those instituted later (Waters et al., 2011). The 2011 and 2012 Institute of Medicine (IOM) reports recommend the early life-cycle approach in tackling obesity, while advocating for a holistic, systems-based perspective in the formulation of policies and interventions (McGuire, 2012a; McGuire, 2012b). Thus, there is a growing consensus that instituting interventions targeting at-risk populations during the prenatal and early post-natal periods is the most prudent approach to break the intergenerational cycle occasioned by the obesity epidemic. Nader et al. proposed a comprehensive systems-level community based, systems intervention model, targeting pregnancy, infancy, and toddlers that is family based and includes community resources and cross systems collaboration (Nader et al., 2012). The model recommends intervening in pregnancy, infancy and early childhood to disrupt the intergenerational effects of obesity by establishing healthy behaviors in the mother and child. However, few studies have described and evaluated the feasibility and effectiveness of pregnancy-based interventions on obesity-prevention behaviors such as diet and physical activity, especially among low-income populations (Blake-Lamb et al., 2016).
The purpose of this paper is to describe the Healthy Eating Active Living (HEAL) intervention, a multi-component program to promote breastfeeding, healthy dietary habits and physical activity implemented, and present preliminary results of pilot testing of this program among Medicaid-eligible pregnant-women in Houston, Texas.
2. Methods
2.1. HEAL intervention description
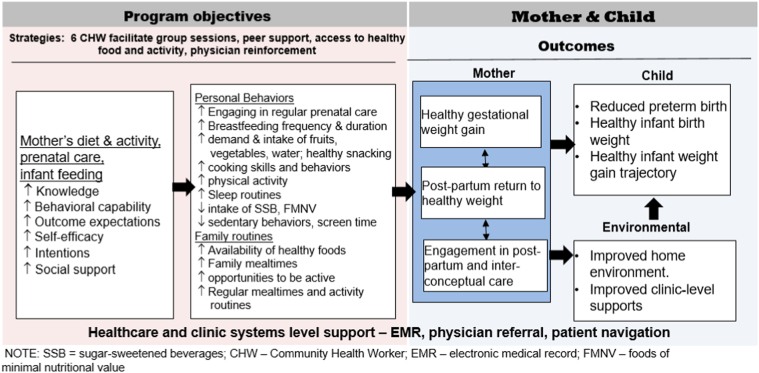
Healthy Eating Active Living (HEAL) is a six-week multicomponent program developed by UTHealth School of Public Health investigators with the overarching goal of promoting healthy eating, breastfeeding and physical activity behaviors to achieve a healthy weight gain during pregnancy for the mother, improve birth outcomes and prevent childhood obesity later in life. This is done by strengthening clinic-community linkages and creating systems-level supports for sustainability of the program components. HEAL program components are grounded in the Social Cognitive Theory (Bandura, 1986) and Theory of Planned Behavior (Ajzen, 1991) constructs to increase knowledge, behavioral capability, self-efficacy, attitudes, intentions, social support, observational learning for healthy eating, breastfeeding and physical activity behaviors among pregnant women (Fig. 1).
Fig. 1.
Logic model for Healthy Eating Active Living (HEAL), HEAL pilot evaluation 2015–2016.
The six HEAL sessions include the first session one-on-one with the HEAL dietitian followed by five weekly Community Health Worker (CHW)-facilitated group sessions conducted at a community location. The sessions revolve around four themes: 1) making the most of prenatal appointments (provider engagement), 2) preparing for breastfeeding, 3) physical activity during pregnancy, and 4) understanding one's food environment in order to make healthy choices. Goal-setting around these healthy behaviors is done by each participant on a weekly basis. A typical CHW-facilitated group session lasts about 90 min. The sessions are non-didactic, thus enabling experiential adult learning rooted in the principles of behavior change and motivational interviewing (Miller and Rollnick, 2002). A typical group session starts with 30 min of CHW-facilitated discussion around the weekly topic areas, followed by cooking demonstrations, recipe tasting and physical activity. Each week, the participating women attending the sessions also receive ~20–25 lbs. (50 servings) of fresh, donated produce along with nutrition education materials and recipe cards to take home at no cost to the families made available through collaboration with a the local food bank and a local non-profit organization called Brighter Bites (Sharma et al., 2015; Sharma et al., 2017). The amount of produce received was the same for each participant regardless of the number of members in the household. The 50 servings are sufficient to provide an additional approximately two servings of fruits and vegetables per individual for a family of four. The produce provision is experiential learning to allow the women to practice healthy cooking and eating behaviors at home and increase the preference for healthy foods. The cooking demonstrations provide information on healthy food preparation and storage techniques, baby-friendly recipes, food safety, and a weekly recipe tasting using the produce that is in their weekly bags. Recipes are culturally friendly using wholesome ingredients that are provided in their weekly produce bag. A 10 to 15-minute physical activity consisting of various pregnancy-safe, fun, low-impact aerobics, strength-conditioning, stretching and yoga-based activities is also implemented weekly. Participating pregnant women are also encouraged to complete a goal tracking sheet on a weekly basis to set healthy goals centered around HEAL components to practice what they learned in sessions throughout the week. Women who are unable to make it to a session are provided with the educational materials in the subsequent session and are invited to join subsequent cohorts to make up their missed session. However, we did not have any women who did make up sessions in other cohorts. The CHWs also provide social support to the participating women by assisting with enrollment for federal assistance programs such as Women, Infants, Children (WIC) and Supplemental Nutrition Assistance Program (SNAP), and connecting them with local resources including the local food bank and pantries.
2.2. Study design, implementation and evaluation
2.2.1. Study design
We present data from a pilot implementation and evaluation of HEAL in a Medicaid or Medicaid-eligible population (March 2015–October 2016). HEAL is an ongoing natural experiment; a collaboration between University of Texas Physicians (UTP), the clinical practice arm of the UT Medical School at Houston, University of Texas School of Public Health (UTSPH), and community-based organizations. The pilot initiative to improve service delivery to patients was funded in 2014 through the 1115 Medicaid Transformation Waiver program called the Delivery System Reform Incentive Payment Program (DSRIP) (Begley et al., 2017). Under this program, hospitals and other providers have established regional partnerships and, implemented projects to address local gaps in service. HEAL is one such project integrated into the UTP healthcare system and currently offered as a standard-of-care for UTP patients who are pregnant and on Medicaid or Medicaid-eligible. Recruitment of HEAL participants is done through the combined efforts of clinic and HEAL program staff. Eligible patients are identified by HEAL program staff at the UTP clinics based on following inclusion criteria: a) pregnant < 28 weeks, and b) Medicaid participant or Medicaid eligible. HEAL dietitians are located onsite at the clinic located within the UTP clinic building to enroll the patients.
2.2.2. HEAL implementation and evaluation
In fall 2014, HEAL was instituted within the UTP electronic medical record system as part of the UTP Obstretics/Gynecological (Ob/Gyn) clinic allowing for patient recruitment, tracking, access to medical records, and communication with the Ob/Gyn provider community. HEAL program implementation team comprising of two registered dietitians and two certified community health workers (CHW) were also hired by UTP in fall 2014. This team participated in two trainings conducted in fall 2014 prior to HEAL implementation. The first was a one-day training specifically on HEAL program components and its delivery, evaluation conducted by UTHealth School of Public Health investigators. The HEAL training materials provided included a facilitator's guide outlining each session, nutrition education materials, recipes/tip sheets, and program outcome and process evaluation protocols and survey instruments. Additionally, the dietitians and CHWs participated in a one-day training offered by the UTP on using the electronic medical record system.
HEAL program implementation and evaluation began in March 2015. Since HEAL was implemented and offered to all eligible UTP patients as standard-of-care, program tracking and evaluation measures were implemented into the HEAL implementation workflow as quality improvement metrics. Evaluation consisted of ongoing process measures to track dosage, reach, fidelity and acceptability. Outcome measures were tracked by HEAL program staff using a one-group pre-post evaluation design. For this study, we analyzed data collected from March 2015 through October 2016 to determine the initial feasibility, acceptability and effects of the program on various individual-level factors including diet, activity, and intention to breastfeed among HEAL participants. The study was reviewed and approved by the University of Texas Health Science Center Protection of Human Subjects.
2.3. Data collection measures
All outcome measures were collected at baseline (prior to HEAL) and end of the 6-session program period, except socio-demographic factors were collected at baseline only. Process evaluation measures were collected at each program session.
2.3.1. Socio-demographic factors
Self-reported socio-demographic information including age, race/ethnicity, marital status, education level, participation in food assistance programs, income level, and employment status.
2.3.2. Behavioral, psychosocial and environmental factors
This self-report survey included validated questions regarding various environmental, behavioral and psychosocial constructs:
2.3.2.1. Dietary behaviors
Measured frequency of cooking, frequency of consumption of various foods including fast foods, desserts, fruits, vegetables, fried foods, sugar-sweetened beverages, and water intake (Nebeling et al., 2017). Consumption of various food items were further grouped into four summative scales for analysis, including fruits and vegetable Intake (5 items: fruit, green salad or non-fried vegetables, other kind of potatoes, cooked beans, and whole grain bread), intake of sugary foods and desserts (Dessert scale - 3 items: candy or chocolate, frozen desserts, and cookies or cakes, cupcakes, doughnuts, brownies), sugar-sweetened beverage intake (Sugar-sweetened beverage scale - 3 items: sweetened fruit drinks and teas, regular soda or pop, and sports drinks), and intake of junk foods (Junk food scale - 5 items: fried potatoes like French fries, potato chips, pizza, hamburgers or cheeseburgers, and fried chicken). Higher score indicated higher intake of these foods. Other items regarding intake of 100% fruit juice, water, milk, heat and serve foods, processed meat, sugary cereals, and restaurant foods were analyzed individually.
Physical activity behaviors including frequency and intensity of physical activity were also assessed (Accessed 6/4, 2016).
2.3.2.2. Psychosocial factors
Measured food security (Accessed 05/25, 2012), self-efficacy, attitudes, perceived benefits and intentions to breastfeed (Centers for Disease Control and Prevention, 2014), eating fruits and vegetables, cooking from basic ingredients, and food preparation (Condrasky et al., 2011).
2.3.2.3. Home availability of foods
Home nutrition environment for availability of 21 healthy foods (10 fruit items and 11 vegetable items) and 3 unhealthy foods (e.g. fried chips, processed food, and soda) were measured using a previously validated Home Food Inventory checklist (Reynolds et al., 2002).
2.3.3. Maternal height and weight
Measured by HEAL trained project staff using calibrated stadiometers and scales at baseline (prior to the program) and weight was also measured weekly across the six session program period at each visit.
2.4. Process evaluation
Ongoing in the six-session program to measure feasibility, acceptability, dosage, reach, and fidelity of the program components. CHW facilitators completed surveys at the end of each session to provide input on program implementation fidelity of various components, and information regarding amount, and type of produce distributed to the families (data not shown). Additionally, participating women completed a process evaluation survey on a weekly basis on the prior session they attended to provide feedback regarding acceptability and usage of each of the program components.
2.5. Statistical analysis
Data analyses were conducted using Stata 14.1 (Stata Corporation, College Station, TX). Descriptive statistics including means, standard deviations, and frequencies were computed to describe the socio-demographic, behavioral, and psychosocial factors of participants. Analysis of covariance (ANCOVA) was conducted to evaluate the changes between pre- and post-intervention, controlling for participants' ethnicity, age at baseline, and annual household income. Session attendance and time interaction was further controlled for in ANCOVA to assess the association between level of attendance and changes pre- to post-intervention. P-values of <0.05 were considered statistically significant.
3. Results
Table 1 presents the demographic characteristics of the pregnant women enrolled in HEAL between March 2015 through October 2016 (n = 329 pregnant women). Of the 329 women who enrolled in HEAL, a total of n = 210 women completed the pre-post assessment (64% retention rate).
Table 1.
Demographic characteristics for pregnancy women enrolled in HEAL (N = 329), HEAL pilot evaluation 2015–2016.
| Demographic characteristics | n | % |
|---|---|---|
| Age | ||
| 18 to 21 | 45 | 13.7 |
| 22 to 25 | 72 | 22.0 |
| 26 to 29 | 77 | 23.5 |
| 30 to 34 | 89 | 27.1 |
| 35 to 45 | 45 | 13.7 |
| Race/ethnicity | ||
| African American | 172 | 53.1 |
| Hispanic | 105 | 32.4 |
| White | 29 | 9.0 |
| Other | 18 | 5.5 |
| Marital status | ||
| Married | 118 | 36.4 |
| In a relationship with significant other | 91 | 28.1 |
| Divorced or separated | 19 | 5.9 |
| Never married | 96 | 29.6 |
| Education | ||
| Never attended or attended Grades 1 to 11 | 40 | 12.4 |
| Grade 12 or GED | 93 | 28.8 |
| College 1 to 3 years | 125 | 38.7 |
| College 4 or more years | 65 | 20.1 |
| Income | ||
| <10,000 | 101 | 39.0 |
| 10,001 to 25,000 | 80 | 30.9 |
| 25,001 to 50,000 | 56 | 21.6 |
| 50,001 or greater | 22 | 8.5 |
| Employment status | ||
| Working for pay | 139 | 43.0 |
| Not working, looking for a job | 93 | 28.8 |
| Not working, not looking for a job | 91 | 28.2 |
| BMI pre-pregnancy | ||
| Underweight (BMI < 18.5) | 3 | 1.1 |
| Normal (BMI > 18.5) | 44 | 15.2 |
| Overweight (BMI > 25) | 90 | 31.1 |
| Obese (BMI > 30) | 152 | 52.6 |
| Assistance program participation | ||
| WIC (Women, Infants & Children) | 178 | 56.0 |
| SNAP Benefit (Supplemental Nutrition Assistance Program) | 182 | 57.2 |
| Medicaid/Texas Health Steps | 228 | 71.7 |
| Medicare | 28 | 8.8 |
| Free/reduced meals a school | 55 | 17.3 |
| CHIP (Children's Health Insurance Program) | 31 | 9.8 |
| n | Mean ± SD | |
| Age in year | 328 | 28.04 ± 5.74 |
| Gestational age | 328 | 21.61 ± 6.56 |
| Weight pre-pregnancy, self-reported (lbs) | 305 | 195.00 ± 98.61 |
| BMI pre-pregnancy (self-report) | 289 | 32.32 ± 8.42 |
| n | Mean ± SD | |
| Baseline BMI (measured for all enrolled HEAL participants) | 312 | 34.87 ± 7.97 |
At baseline, mean age of the women was 28.0 years (±5.7). Average gestational age at the time of enrollment was 22 weeks (±6.6), and mean self-reported pre-pregnancy weight was 195 lbs. (±98.6). The mean BMI of participating women prior to start of HEAL was 32.3 (±8.4). The participant pool was predominantly African American (53.1%) and Hispanic (32.4%), married (36.4%) or in a relationship (28.1%), and without a college degree (79.9%). Participants were predominantly low-income with 39% reporting an annual household income of <$10,000 and 57% reported not working, of which 29% reported looking for a job. A majority of the participants also reported receiving government assistance programs (56% on WIC, 57.2% on SNAP and 71.7% on Medicaid). We compared these baseline characteristics of women who graduated from HEAL (n = 210) as compared to the women who did not (n = 119). Results showed that women who graduated from HEAL had significantly higher education level (24.0% attended 4+ years of college vs. 13.0%, p = 0.009), were employed (49% vs. 32.2%, p = 0.012), and were slightly older (28.6 years vs. 26.9 years, p = 0.016) as compared to women who did not graduate from HEAL.
3.1. Dietary outcomes
Results of the pre-post analysis demonstrates that there was a significant impact of the HEAL program on dietary outcomes of participating pregnant women (Table 2). When interaction by dosage was assessed for the various scales related to food and beverage intake, results showed that women who attended more HEAL sessions reported greater increases in frequency of intake of fruits and vegetables pre- to post-intervention as compared to those attending fewer sessions (p = 0.004). Results also showed a significant positive association between attending HEAL sessions and the Healthy Food inventory score for fruits and vegetables (p < 0.001) (i.e. women who attended more HEAL sessions reported higher availability of fruits and vegetables at home). While there was a trend towards a decrease in the intake and availability of unhealthy foods such as desserts, sugar sweetened beverages and junk foods, these changes were not statistically significant when assessed as scales.
Table 2.
Pre-to-post intervention changes in dietary intake, home food environment, cooking and mealtime behaviors, food security, and physical activity (n = 210), HEAL pilot evaluation 2015–2016.
| Variables | Possible scoring range | Pre-HEAL |
Post-HEAL |
ANCOVA pre-post p-value |
ANCOVA interaction by dosage p-value+ |
||
|---|---|---|---|---|---|---|---|
| n | Mean ± SD | N | Mean ± SD | ||||
| Fruit and vegetables intake scalea | 5–30 | 208 | 14.31 ± 4.19 | 208 | 15.58 ± 4.11 | 0.464 | 0.004⁎ |
| Dessert intake scaleb | 3–18 | 189 | 6.54 ± 2.90 | 189 | 6.06 ± 2.55 | 0.085 | 0.541 |
| Sugar sweetened beverages intake scalec | 3–18 | 198 | 6.27 ± 2.95 | 204 | 5.80 ± 2.90 | 0.105 | 0.413 |
| Junk food intake scaled | 5–30 | 209 | 10.69 ± 4.37 | 209 | 9.56 ± 3.82 | 0.152 | 0.169 |
| Home availability of fruitse | 0–10 | 186 | 5.88 ± 2.32 | 186 | 6.79 ± 2.01 | 0.315 | <0.001⁎ |
| Home availability of vegetablef | 0–11 | 183 | 6.81 ± 2.39 | 183 | 8.03 ± 2.12 | 0.602 | <0.001⁎ |
| Home availability of healthy food (F&V)g | 0–21 | 175 | 12.72 ± 3.99 | 175 | 14.83 ± 3.53 | 0.472 | <0.001⁎ |
| Home availability of unhealthy foodh | 0–3 | 185 | 1.80 ± 1.07 | 185 | 1.45 ± 1.09 | 0.575 | 0.157 |
| Overall home availability of foodsi | 0–21 | 157 | 11.03 ± 4.06 | 157 | 13.35 ± 3.66 | 0.559 | <0.001⁎ |
| Variables | Pre-HEAL |
Post-HEAL |
ANCOVA pre-post p-value |
ANCOVA interaction by dosage p-value+ |
||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Daily consumption of fruits and vegetables in servings | ||||||
| Servings of FRUIT consumed per day | 0.058 | <0.001⁎ | ||||
| None | 5 | 2.5 | 2 | 0.9 | ||
| 1/2 to 1 serving | 64 | 32.1 | 33 | 16.6 | ||
| 1–2 servings | 68 | 34.2 | 62 | 31.2 | ||
| 2–3 servings | 42 | 21.1 | 63 | 31.7 | ||
| 4 servings or more | 20 | 10.1 | 39 | 19.6 | ||
| Servings of VEGETABLES consumed per day | 0.040⁎ | <0.001⁎ | ||||
| None | 11 | 5.5 | 2 | 1.0 | ||
| 1/2 to 1 serving | 79 | 39.5 | 46 | 23.0 | ||
| 1–2 servings | 65 | 32.5 | 71 | 35.5 | ||
| 2–3 servings | 29 | 14.5 | 56 | 28.0 | ||
| 4 servings or more | 16 | 8.0 | 25 | 12.5 | ||
| Meet daily fruit recommendations (2 servings) | 0.005⁎ | <0.001⁎ | ||||
| Yes | 62 | 31.2 | 102 | 51.3 | ||
| No | 137 | 68.8 | 97 | 48.7 | ||
| Meet daily vegetable recommendations (3 servings) | 0.004⁎ | 0.005⁎ | ||||
| Yes | 45 | 22.5 | 81 | 40.5 | ||
| No | 155 | 77.5 | 119 | 59.5 | ||
| Frequency of consumption in the past 7 days | ||||||
| Any WATER that is not sweetened | 0.784 | 0.478 | ||||
| 0 time | 4 | 1.9 | 2 | 1.0 | ||
| 1–6 times per 7 days | 46 | 22.4 | 47 | 22.9 | ||
| 1–2 times a day | 28 | 13.7 | 20 | 9.8 | ||
| 3+ times a day | 127 | 62.0 | 136 | 66.3 | ||
| CANDY or CHOCOLATE | 0.056 | 0.098 | ||||
| 0 time | 54 | 26.1 | 71 | 34.3 | ||
| 1–3 times per 7 days | 87 | 42.0 | 86 | 41.6 | ||
| 4–6 times per 7 days | 23 | 11.1 | 10 | 4.8 | ||
| 1 time a day | 24 | 11.6 | 27 | 13.0 | ||
| 2+ times a day | 19 | 9.2 | 13 | 6.3 | ||
| FROZEN DESSERTS | 0.256 | 0.536 | ||||
| 0 time | 72 | 35.3 | 81 | 39.7 | ||
| 1–3 times per 7 days | 89 | 43.6 | 81 | 39.7 | ||
| 4–6 times per 7 days | 17 | 8.3 | 11 | 5.4 | ||
| 1 time a day | 16 | 7.8 | 23 | 11.3 | ||
| 2+ times a day | 10 | 5.0 | 8 | 3.9 | ||
| Heat and serve foods | 0.195 | 0.003⁎ | ||||
| 0 time | 117 | 56.0 | 142 | 67.9 | ||
| 1–3 times per 7 days | 54 | 25.8 | 45 | 21.5 | ||
| 4–6 times per 7 days | 17 | 8.1 | 7 | 3.4 | ||
| 1 time a day | 11 | 5.3 | 13 | 6.2 | ||
| 2+ times a day | 10 | 4.8 | 2 | 1.0 | ||
| Sugary cereals | 0.019⁎ | 0.296 | ||||
| 0 time | 89 | 43.2 | 104 | 50.5 | ||
| 1–3 times per 7 days | 64 | 31.1 | 63 | 30.6 | ||
| 4–6 times per 7 days | 19 | 9.2 | 13 | 6.3 | ||
| 1 time a day | 18 | 8.7 | 17 | 8.2 | ||
| 2+ times a day | 16 | 7.8 | 9 | 4.4 | ||
| Fruits | 0.173 | <0.001⁎ | ||||
| 0 time | 8 | 3.8 | 1 | 0.5 | ||
| 1–3 times per 7 days | 38 | 18.3 | 29 | 13.9 | ||
| 4–6 times per 7 days | 49 | 23.6 | 27 | 13.0 | ||
| 1 time a day | 33 | 15.9 | 23 | 11.1 | ||
| 2+ times a day | 80 | 38.5 | 128 | 61.5 | ||
| Green salad/non-fried vegetables | 0.387 | 0.002⁎ | ||||
| 0 time | 17 | 8.3 | 9 | 4.4 | ||
| 1–3 times per 7 days | 66 | 32.4 | 63 | 30.9 | ||
| 4–6 times per 7 days | 47 | 23.0 | 33 | 16.2 | ||
| 1 time a day | 30 | 14.7 | 37 | 18.1 | ||
| 2+ times a day | 44 | 21.6 | 62 | 30.4 | ||
| Sweetened fruit drinks and teas | 0.029⁎ | 0.841 | ||||
| 0 time | 64 | 31.2 | 66 | 32.2 | ||
| 1–3 times per 7 days | 77 | 37.6 | 84 | 40.9 | ||
| 4–6 times per 7 days | 23 | 11.2 | 19 | 9.3 | ||
| 1 time a day | 20 | 9.8 | 17 | 8.3 | ||
| 2+ times a day | 21 | 10.2 | 19 | 9.3 | ||
| Mealtime environment and cooking behaviors | ||||||
| How sure are you that you can…eat fruits and vegetables at every meal every day | 0.803 | 0.190 | ||||
| Not sure | 37 | 17.9 | 28 | 13.5 | ||
| Sure | 76 | 36.9 | 58 | 28.2 | ||
| Extremely sure | 93 | 45.2 | 120 | 58.3 | ||
| Eat fruits or vegetables as a snack even if everybody else were eating other snacks | 0.562 | 0.031⁎ | ||||
| Not sure | 29 | 14.1 | 19 | 9.2 | ||
| Sure | 87 | 42.2 | 48 | 23.3 | ||
| Extremely sure | 90 | 43.7 | 139 | 67.5 | ||
| Cook from basic ingredients | 0.907 | 0.022⁎ | ||||
| Not sure | 37 | 17.7 | 25 | 12.0 | ||
| Sure | 65 | 31.3 | 53 | 25.5 | ||
| Extremely sure | 106 | 51.0 | 130 | 62.5 | ||
| Cooking techniques and skills self-efficacy | ||||||
| How sure are you that you can…use knife skills in the kitchen | 0.138 | 0.160 | ||||
| Not sure | 41 | 19.8 | 21 | 10.2 | ||
| Sure | 56 | 27.1 | 51 | 24.6 | ||
| Extremely sure | 110 | 53.1 | 135 | 65.2 | ||
| Use basic cooking techniques | 0.238 | 0.075 | ||||
| Not sure | 38 | 18.8 | 17 | 8.4 | ||
| Sure | 45 | 22.3 | 37 | 18.3 | ||
| Extremely sure | 119 | 58.9 | 148 | 73.3 | ||
| Prepare root vegetables | 0.337 | 0.006⁎ | ||||
| Not sure | 81 | 39.3 | 49 | 23.8 | ||
| Sure | 47 | 22.8 | 46 | 22.3 | ||
| Extremely sure | 78 | 37.9 | 111 | 53.9 | ||
| Prepare fresh or frozen green vegetables | 0.219 | 0.344 | ||||
| Not sure | 38 | 18.3 | 27 | 13.0 | ||
| Sure | 54 | 26.1 | 43 | 20.8 | ||
| Extremely sure | 115 | 55.6 | 137 | 66.2 | ||
| Food security | ||||||
| High food security | 107 | 51.2 | 124 | 59.3 | 0.056 | 0.878 |
| Low food security | 71 | 34.0 | 52 | 24.9 | ||
| Very low food security | 31 | 14.8 | 33 | 15.8 | ||
| Physical activity | ||||||
| Physically active for a total of at least 30 min during the past 7 days | 0.078 | 0.004⁎ | ||||
| 0 day | 36 | 17.3 | 8 | 3.8 | ||
| 1–2 days | 90 | 43.3 | 87 | 41.8 | ||
| 3–4 days | 52 | 25.0 | 65 | 31.3 | ||
| 5 days or more | 30 | 14.4 | 48 | 23.1 | ||
| Walk for at least 10 min at a time during the past 7 days | 0.246 | 0.010⁎ | ||||
| 0 day | 22 | 12.0 | 4 | 2.1 | ||
| 1–2 days | 65 | 35.3 | 55 | 29.9 | ||
| 3–4 days | 48 | 26.1 | 50 | 27.2 | ||
| 5 days or more | 49 | 26.6 | 75 | 40.8 | ||
Scale includes five items: fruit, green salad or non-fried vegetables, other kind of potatoes, cooked beans, and whole grain bread.
Scale includes three items: candy or chocolate, frozen desserts, and cookies, cakes, cupcakes, doughnuts, brownies, poptarts.
Scale includes three items: sweetened fruit drinks and teas, regular soda or pop, and sports drinks.
Scale includes five items: fried potatoes like French fries, potato chips, pizza, hamburgers or cheeseburgers, fried chicken.
Total number of items out of 10 fruit items (frozen, fresh, or canned) present in the home.
Total number of items out of 11 vegetable items (frozen, fresh, or canned) present in the home.
Healthy food score = Total number of items out of the 10 fruit items (frozen, fresh, or canned) and 11 vegetable items (frozen, fresh, or canned) present at home.
Unhealthy food score = Total number of items out of 3 items (potato chips, processed food, soda or pop) present in the home.
Home food inventory score = (number of fruits + number of vegetable items − number of unhealthy items).
ANCOVA p-value controls for interaction of baseline behavior and dosage.
p < 0.05.
For individual foods and beverages, servings of vegetables consumed increased pre-to-post intervention (p = 0.040). Furthermore, results showed a 20% increase pre- to post-intervention in the number of women reportedly consuming 2+ servings of fruit per day (p = 0.0005), and a 15% increase in the number of women consuming 2+ servings of vegetables per day (p = 0.0004). Women who attended more HEAL sessions reported greater increases in servings of fruits and vegetables consumed (p < 0.001), a 20% increase in proportion of women meeting the recommended servings of intake for fruits (p < 0.001), 18% increase in proportion of women meeting recommended servings of intake for vegetables (p = 0.005), and a 12% increase in the proportion of women reportedly consuming heat and serve foods zero times per week (p = 0.003). Our results also showed a significant decrease in frequency of sugary cereals (p = 0.019) and sweetened fruit drinks and teas (p = 0.029) consumed pre- to post-intervention. Concurrently, there was an increase in frequency of water intake, decrease in the frequency of intake of candy, frozen desserts; albeit these changes were not statistically significant.
3.2. Mealtime environment, cooking behaviors, and food insecurity
There was a significant interaction effect of HEAL attendance on cooking behaviors. Thus, women who attended more HEAL sessions reported higher pre-to-post intervention changes in self-efficacy towards eating fruits and vegetables as snacks even if others were eating other snacks (p = 0.031), cooking from basic ingredients (p = 0.022), and food preparation techniques such as preparing root vegetables (p = 0.006).
Furthermore, there was an increase in reported food security (+8.3% high food security) pre- to post-intervention; however these changes were not statistically significant (p = 0.056).
3.3. Physical activity during pregnancy
Finally, there was a significant interaction effect of HEAL session attendance on physical activity among pregnant women (Table 2). Results demonstrated a 15% increase in the number of women reportedly active for at least 30 min per day 3+ days per week, and a 14% increase in the number of women who reported they could walk for at least 10 min 5+ days a week, with greater increases pre-to-post intervention among women who attended more HEAL sessions (p < 0.01).
4. Breastfeeding
There was a significant positive impact of the HEAL program on breastfeeding outcomes among the participating pregnant women. Results showed a significant increase pre-to-post intervention in the age of the baby when the mothers reportedly intended to stop breastfeeding (10.3 months vs. 11.3 months; p = 0.009). Results showed (Table 3) a 7% increase in the number of women who intend to breastfeed only (p = 0.012), and a 10% increase in number of women who reported that they will introduce complementary foods after the baby is 7 or more months of age; albeit this change was not statistically significant (p = 0.058). Perceived benefits towards breastfeeding also improved, with 13.4% increase in the number of women who strongly agreed that breastfeeding makes for a healthier baby (p = 0.029 for time x dosage interaction), and 21% increase in the number of women who strongly agreed that babies should be exclusively breastfed for the first 6 months of life (p < 0.001 for time × dosage interaction).
Table 3.
Changes in breastfeeding plans, self-efficacy, attitudes, and perceived benefits (n = 210), HEAL pilot evaluation 2015-2016.
| Variables | Pre-HEAL |
Post-HEAL |
ANCOVA pre-post p-value |
ANCOVA interaction by dosage p-value+ |
||
|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | |||
| Baby's age when planning to completely stop breastfeeding | 149 | 10.25 ± 5.81 | 149 | 11.30 ± 6.83 | 0.009⁎ | 0.975 |
| Pre-HEAL |
Post-HEAL |
ANCOVA pre-post p-value |
ANCOVA interaction by dosage p-value+ |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Breastfeeding plan | ||||||
| How do you plan to feed your new baby in the first few weeks | 0.012⁎ | 0.255 | ||||
| Formula only | 23 | 12.4 | 17 | 9.2 | ||
| Breastfeeding and formula | 76 | 41.1 | 69 | 37.3 | ||
| Breastfeeding only | 86 | 46.5 | 99 | 53.5 | ||
| Baby's age for formula or any other food beside breast milk | 0.058 | 0.086 | ||||
| month | 3 | 4.1 | 0 | 0.0 | ||
| 1–2 months | 4 | 5.4 | 1 | 1.3 | ||
| 3–4 months | 12 | 16.2 | 10 | 13.5 | ||
| 5–6 months | 24 | 32.4 | 25 | 33.8 | ||
| 7 months or more | 31 | 41.9 | 38 | 51.4 | ||
| Plan to continue breastfeeding after you return to work or school | 0.457 | 0.522 | ||||
| Yes | 123 | 88.5 | 131 | 94.2 | ||
| No | 16 | 11.5 | 8 | 5.8 | ||
| Self-efficacy | ||||||
| Confident in able to breastfeed until the baby is the age you indicated above | 0.101 | 0.127 | ||||
| Not at all confident | 5 | 3.0 | 2 | 1.2 | ||
| Less confident | 8 | 4.8 | 2 | 1.2 | ||
| Neutral | 36 | 21.7 | 22 | 13.2 | ||
| Somewhat confident | 54 | 32.5 | 61 | 36.8 | ||
| Very confident | 63 | 38.0 | 79 | 47.6 | ||
| Attitudes | ||||||
| Infant formula is as good as breast milk | 0.164 | 0.632 | ||||
| Strongly disagree | 52 | 25.0 | 68 | 32.7 | ||
| Disagree | 55 | 26.4 | 50 | 24.0 | ||
| Neutral | 49 | 23.6 | 45 | 21.6 | ||
| Agree | 38 | 18.3 | 24 | 11.5 | ||
| Strongly agree | 14 | 6.7 | 21 | 10.2 | ||
| Perceived benefits | ||||||
| If a baby is breastfed, he or she will be healthier, and less likely to get ear infections or respiratory illness or diarrhea | 0.002⁎ | 0.029⁎ | ||||
| Strongly disagree | 5 | 2.4 | 2 | 1.0 | ||
| Disagree | 7 | 3.4 | 4 | 1.9 | ||
| Neutral | 26 | 12.5 | 13 | 6.3 | ||
| Agree | 46 | 22.1 | 37 | 17.8 | ||
| Strongly agree | 124 | 59.6 | 152 | 73.0 | ||
| Babies should be exclusively breastfed (fed only breast milk) for the first 6 months | 0.105 | <0.001⁎ | ||||
| Strongly disagree | 15 | 7.2 | 8 | 3.8 | ||
| Disagree | 18 | 8.7 | 11 | 5.3 | ||
| Neutral | 54 | 26.1 | 46 | 22.2 | ||
| Agree | 55 | 26.6 | 33 | 16.0 | ||
| Strongly agree | 65 | 31.4 | 109 | 52.7 | ||
ANCOVA p-value controls for interaction of baseline behavior and dosage.
p < 0.05.
5. Process evaluation (data not shown in tables)
The HEAL process evaluation results showed that overall program retention rate was 64% (completed all six sessions). Over 80% of the participants attended ≥4 sessions. Results also demonstrate that a majority of the participants found the sessions helpful (91.4%). When specifically asked about each of the program components, sending fresh fruits and vegetables was reportedly most helpful (97.5%), followed by the CHW-facilitated sessions, while the goal tracking component was least helpful (86.9%). Process evaluation data was not available for the last session since participants were not returning the following week. Results of the CHW-completed program implementation surveys demonstrated >95% fidelity of program components.
When asked about their greatest challenges to attending programs such as HEAL, participants reported transportation as their biggest barrier (24.7%) followed by taking time off work or school (10.0%), and having other children at home (12.2%). About 41% of the participants reported having no barriers to attendance (data not shown in tables). Of the fruits and vegetables sent home weekly, overall, over 90% reportedly ate half or more of them.
6. Discussion
The Affordable care act was birthed in 2010 to expand on existing Medicaid coverage for millions of low-income Americans. Following the Supreme Court decision in 2012 to give states a choice on whether to adopt the expansion or not, the state of Texas opted to not participate in the Medicaid expansion. However, the DSRIP program under the section 1115 Medicaid waiver program was launched to serve as a “bridge to reform” (Begley et al., 2017). This federal-state partnership was designed to enhance the quality and value of healthcare received by patients and has now been adopted in Texas. This allows approved health providers to implement innovative, preventive programs to improve health outcomes while containing cost growth. HEAL is one such program being implemented as standard-of-care through UTP clinics to amplify the preventive services offered to their patients. As part of this project, successful clinic-community linkages were implemented by integrating HEAL into the UTP ob-gyn clinic system and EMR to facilitate program recruitment, tracking and implementation.
A preliminary evaluation of HEAL demonstrates feasibility of implementing this framework at the clinic and community level, over 95% fidelity of program implementation, and acceptability of program strategies among participating pregnant women. By integrating a primary prevention approach for childhood obesity prevention into the healthcare system, HEAL aims to create a model for systems-level approaches to childhood obesity prevention starting with pregnancy in order to disrupt the intergenerational effects of obesity.
Program evaluation data demonstrates strong feasibility and acceptability of the program and promising changes in the targeted psychosocial and behavioral outcomes pre- to post-intervention. Our data demonstrated that attendance of HEAL was significantly associated with increased availability and intake of fruits and vegetables, decreased frequency of intake of unhealthy foods such as sugary cereals and sugar-sweetened beverages. These results concur with other clinic-based intervention studies targeting pregnant women have demonstrated success in increasing their vegetables consumption (Guelinckx et al., 2010; Poston et al., 2015) and decreasing fat and carbohydrate consumption (Guelinckx et al., 2010; Poston et al., 2015; Wolff et al., 2008). Given the high prevalence of obesity seen among our participating pregnant women, our preliminary findings are promising but warrant further investigation. In contrast to other studies (Guelinckx et al., 2010), our study demonstrated an increase in physical activity among the HEAL participants pre- to post-intervention, whereas other studies(Guelinckx et al., 2010) have indicated a decline in physical activity between the second and third trimesters. However, one difference in our study was that each week the women participated in CHW-led physical activity sessions, who demonstrated safe ways in which to be physically active during pregnancy. Another consideration is that the results seen in our study could potentially be due to social-desirability bias and future studies with objective measures such as accelerometers, a more stringent study design, and a control group are needed.
Furthermore, our study also showed improvements in cooking behaviors, including cooking using basic ingredients, a potential mediator of healthy dietary habits, and a major target of the intervention. Thus, in concordance with other interventions targeting low-income pregnant women (Hromi-Fiedler et al., 2016; Skreden et al., 2017), HEAL strategies appear to promote prenatal consumption of fruits and vegetables by enhancing knowledge of prenatal care, healthy nutrition, and strengthening basic cooking and food preparation skills through facilitated group discussions. Moreover, in collaboration with the local food bank, HEAL provides fresh produce for participants to take home at no cost and practice healthy cooking and healthy eating behaviors at home with their families. Studies have demonstrated the proven impact of improved accessibility to fruits and vegetable on increasing intake of these foods during pregnancy (Hromi-Fiedler et al., 2016). The provision of healthy foods along with hands-on nutrition education on how to use the produce allows for the participating women and their families to practice the healthy cooking and eating behaviors with their families at home. Interventions combining access plus education approaches among pregnant women are sparse. Our approach is novel, has demonstrated feasibility of implementation, and warrants further investigation.
Our results also showed that attendance of HEAL sessions was significantly associated with increased perceived benefits of breastfeeding for the baby, intention to breastfeed exclusively post-delivery, and increased intention and duration of breastfeeding. A clinical-based intervention study by Srinivas et al., (2015) reported that positive attitude towards breastfeeding increased breastfeeding intention and breastfeeding rate at months 1 and 6 postpartum. Similarly, previous studies (Srinivas et al., 2015; Pugh et al., 2002) conducted among low-income populations have also suggested repeated contact with supportive CHWs and interaction with peer group contributes to improved breastfeeding-related outcomes. Although our post-intervention data was collected prior to delivery, our results do indicate an increased intention to breastfeed exclusively after childbirth. Studies for post-partum follow up of HEAL participants to monitor breastfeeding behaviors are currently underway.
One of the challenges of intervention programs was maintaining participant retention. Our program showed 64% retention (210 at post-intervention evaluation, out of 329 enrolled, completed all six sessions) which is on par with other interventions with similar approaches among low-income pregnant women (Chang et al., 2009). Reasons for lower retention rate among low-income, ethnically diverse populations who are overweight or obese vary. The commonly suggested ones include participants' access to transportation, depression level, negative experience in weight management programs, distrust of clinical system, cultural insensitivity, and inefficient program recruitment and retention management approaches (Chang et al., 2009; El-Khorazaty et al., 2007; Nicholson et al., 2011). Another challenge is sustainability of program components with healthcare changes. In a state-by-state analysis of Medicaid obesity coverage conducted by Lee and colleagues (Lee et al., 2010), it was discovered that while up to 45 U.S. states covered bariatric surgery as a treatment modality for obesity, less expensive but effective preventive strategies such as nutritional counseling were excluded by most states. Evidence found only 10 states that covered nutritional and behavioral therapy (as contained in the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program). The Medicaid program in the state of Texas specifically excludes both bariatric surgery and nutritional consultation (Lee et al., 2010). Moreover, provider-level barriers including lack of confidence, insufficient training and resources on communicating about obesity, and inadequate counseling skills to address weight control issues currently exist (Herring et al., 2010). A qualitative study of prenatal care providers reported that providers often express incompetency and lack of confidence to address weight gain issues with their patients (Stotland et al., 2010). By using trained CHWs and dietitians, programs such as HEAL bridge this communication gap by inculcating healthy lifestyle practices during pregnancy. Another limitation of our study was the use of self-report surveys, which could result in social desirability bias. Also, lack of a control group limits causality and there could be a selection bias of motivated pregnant women who participated in HEAL evaluation. Plans to conduct a randomized controlled trial with sufficient power and objective measures are currently underway. The randomized controlled trial will enroll pregnant women from ob-gyn clinics serving a Medicaid-eligible population and randomly allocate them to receive the HEAL program, or a comparison group receiving health-related educational materials and resources by mail. Follow up will be conducted post-intervention and until 6-months post-delivery to determine program impact on several behavioral outcomes (breastfeeding, cooking, diet, physical activity) and health outcomes related to the mother and child (maternal weight gain trajectory during pregnancy, birth outcomes, post-delivery weight loss trajectory, child weight gain trajectory).
7. Conclusions
Given the high prevalence of obesity prior to pregnancy among low-income women coupled with the rising prevalence of gestational diabetes and related birth complications, programs such as HEAL provide a framework for successful operationalizing of clinic-community linkages and show initial feasibility and acceptability of implementation. Future research warrants the use of objective measures, stringent study design and longer-term outcomes with a control group to determine program efficacy.
Conflict of interest statement
Financial disclosures
Shreela V. Sharma has no financial disclosures.
Ru-Jye Chuang has no financial disclosures.
Courtney Byrd-Williams has no financial disclosures.
Melisa Danho has no financial disclosures.
Mudita Upadhyaya has no financial disclosures.
Pam Berens has no financial disclosures.
Deanna M. Hoelscher has no financial disclosures.
Acknowledgments
The authors would first like to thank the late Dr. Philip R. Nader for his support on the project. The authors would also like to acknowledge the UT Physicians Healthcare Transformations Initiative team, providers and patients participating in the HEAL program. The authors would also like to thank the Michael & Susan Dell Center for Healthy Living for their support on the project.
References
- Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50(2):179–211. [Google Scholar]
- Bandura A. Prentice Hall; 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. [Google Scholar]
- Begley C., Hall J., Shenoy A. Design and implementation of the Texas medicaid DSRIP program. Popul. Health Manag. 2017;20(2):139–145. doi: 10.1089/pop.2015.0192. [DOI] [PubMed] [Google Scholar]
- Blake-Lamb T.L., Locks L.M., Perkins M.E., Baidal J.A.W., Cheng E.R., Taveras E.M. Interventions for childhood obesity in the first 1,000 days a systematic review. Am. J. Prev. Med. 2016;50(6):780–789. doi: 10.1016/j.amepre.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branum A.M., Kirmeyer S.E., Gregory E.C. Prepregnancy body mass index by maternal characteristics and state: data from the birth certificate, 2014. Natl. Vital Stat. Rep. 2016;65(6):1–11. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta, GA: 2014. Infant Feeding Practices Study II and Its Year Six Follow-up. [Google Scholar]
- Chang M., Brown R., Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low-income overweight and obese mothers. BMC Public Health. 2009;9(1):424. doi: 10.1186/1471-2458-9-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condrasky M.D., Williams J.E., Catalano P.M., Griffin S.F. Development of psychosocial scales for evaluating the impact of a culinary nutrition education program on cooking and healthful eating. J. Nutr. Educ. Behav. 2011;43(6):511–516. doi: 10.1016/j.jneb.2010.09.013. [DOI] [PubMed] [Google Scholar]
- Economic Research Service U U.S. Household Food Security Survey Module: Six-item Short Form. 2017. https://www.ers.usda.gov/media/8282/short2012.pdf (Updated September 2012. Accessed 05/25)
- El-Khorazaty M.N., Johnson A.A., Kiely M. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health. 2007;7(1):233. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein E.A., Fiebelkorn I.C., Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff. 2003;W3 doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- Guelinckx I., Devlieger R., Mullie P., Vansant G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: a randomized controlled trial. Am. J. Clin. Nutr. 2010;91(2):373–380. doi: 10.3945/ajcn.2009.28166. [DOI] [PubMed] [Google Scholar]
- Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. 2017. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. (NCHS data brief, no 288) [PubMed] [Google Scholar]
- Herring S.J., Platek D.N., Elliott P., Riley L.E., Stuebe A.M., Oken E. Addressing obesity in pregnancy: what do obstetric providers recommend? J. Women's Health. 2010;19(1):65–70. doi: 10.1089/jwh.2008.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hromi-Fiedler A., Chapman D., Segura-Pérez S. Barriers and facilitators to improve fruit and vegetable intake among WIC-eligible pregnant latinas: an application of the health action process approach framework. J. Nutr. Educ. Behav. 2016;48(7):468–477. doi: 10.1016/j.jneb.2016.04.398. (e1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.S., Sheer J.L., Lopez N., Rosenbaum S. Coverage of obesity treatment: a state-by-state analysis of medicaid and state insurance laws. Public Health Rep. 2010;125(4):596–604. doi: 10.1177/003335491012500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire S. Institute of medicine (IOM) early childhood obesity prevention policies. Washington, DC: the national academies press; 2011. Adv. Nutr. 2012;3(1):56–57. doi: 10.3945/an.111.001347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire S. Institute of medicine. 2012. Accelerating progress in obesity prevention: solving the weight of the nation. Washington, DC: the national academies press. Adv. Nutr. 2012;3(5):708–709. doi: 10.3945/an.112.002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W.R., Rollnick S. The Guilford Press; 2002. Motivational Interviewing: Preparing People for Change. [Google Scholar]
- Nader P.R., Huang T.T., Gahagan S., Kumanyika S., Hammond R.A., Christoffel K.K. Next steps in obesity prevention: altering early life systems to support healthy parents, infants, and toddlers. Child. Obes. 2012;8(3):195–204. doi: 10.1089/chi.2012.0004. [DOI] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion Youth Risk Behavior Surveillance System. 2017. http://www.cdc.gov/HealthyYouth/yrbs/index.htm (Updated August 11, 2016. Accessed 6/4)
- Nebeling L.C., Hennessy E., Oh A.Y. The FLASHE study: survey development, dyadic perspectives, and participant characteristics. Am. J. Prev. Med. 2017;52(6):839–848. doi: 10.1016/j.amepre.2017.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson L.M., Schwirian P.M., Klein E.G. Recruitment and retention strategies in longitudinal clinical studies with low-income populations. Contemp. Clin. Trials. 2011;32(3):353–362. doi: 10.1016/j.cct.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poston L., Bell R., Croker H. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomized controlled trial. Lancet Diabetes Endocrinol. 2015;3(10):767–777. doi: 10.1016/S2213-8587(15)00227-2. [DOI] [PubMed] [Google Scholar]
- Pugh L.C., Milligan R.A., Frick K.D., Spatz D., Bronner Y. Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women. Birth. 2002;29(2):95–100. doi: 10.1046/j.1523-536x.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- Reynolds K.D., Yaroch A.L., Franklin F.A., Maloy J. Testing mediating variables in a school-based nutrition intervention program. Health Psychol. 2002;21(1):51. [PubMed] [Google Scholar]
- Sharma S.V., Markham C., Helfman L., Albus K., Pomeroy M., Chuang R.J. Feasibility and acceptability of brighter bites: a food co-op in schools to increase access, continuity and education of fruits and vegetables among low-income populations. J. Prim. Prev. 2015;36(4):281–286. doi: 10.1007/s10935-015-0395-2. [DOI] [PubMed] [Google Scholar]
- Sharma S.V., Chow J., Pomeroy M., Raber M., Salako D., Markham C. Lessons learned from the implementation of brighter bites: a food co-op to increase access to fruits and vegetables and nutrition education among low-income children and their families. J. Sch. Health. 2017;87(4):286–295. doi: 10.1111/josh.12497. [DOI] [PubMed] [Google Scholar]
- Skreden M., Bere E., Sagedal L.R., Vistad I., Øverby N.C. Changes in fruit and vegetable consumption habits from pre-pregnancy to early pregnancy among Norwegian women. BMC Pregnancy Childbirth. 2017;17(1):107. doi: 10.1186/s12884-017-1291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivas G.L., Benson M., Worley S., Schulte E. A clinic-based breastfeeding peer counselor intervention in an urban, low-income population: interaction with breastfeeding attitude. J. Hum. Lact. 2015;31(1):120–128. doi: 10.1177/0890334414548860. [DOI] [PubMed] [Google Scholar]
- Stotland N.E., Gilbert P., Bogetz A., Harper C.C., Abrams B., Gerbert B. Preventing excessive weight gain in pregnancy: how do prenatal care providers approach counseling? J. Women's Health. 2010;19(4):807–814. doi: 10.1089/jwh.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trust for America's Health and Robert Wood Johnson Foundation The State of Obesity: Better Policies for a Healthier America - Texas State Obesity Data, Rates and Trends. 2018. http://stateofobesity.org/states/tx/ (Updated 2016. Accessed 03/15)
- Waters E., de Silva-Sanigorski A., Hall B.J. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011;12(00) doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- Wolff S., Legarth J., Vangsgaard K., Toubro S., Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int. J. Obes. 2008;32(3):495. doi: 10.1038/sj.ijo.0803710. [DOI] [PubMed] [Google Scholar]