Abstract
Despite the development in shoulder surgery, massive irreparable rotator cuff tears still remain challenging for orthopaedic surgeons. Many surgical methods are addressed to this kind of pathology, but each of them has its own limitations. We decided to fuse the ideas of superior capsular reconstruction, “GraftJacket” technique, and partial rotator cuff repair. In this way, the technique using the long head biceps tendon simultaneously as a vascularized bridge between rotator cuff remnants and greater tubercle and as a depressor for the humeral head was created. This Technical Note describes the technique.
Rotator cuff tears are commonly encountered in the general population, and history of trauma, dominant arm, and age were identified as the main risk factors.1 When this pathology is left untreated, it progresses with deterioration of the cuff morphology and becomes irreparable. Many surgical methods were described for massive irreparable rotator cuff tears, including arthroscopic debridement with or without biceps tenotomy, partial rotator cuff repair, tendon transfers and grafting, and superior capsular reconstruction.2 The latter technique was proven to have very good results, and one of the options was to use the long head biceps tendon (LHBT) as a vascularized graft bridging rotator cuff muscle remnants to natural footprint on greater tubercle and as a material for superior capsular reconstruction.3, 4 Furthermore, reattached degenerated rotator muscles played a role of motors like in an arthroscopic partial reconstruction of rotator cuff tears.5
Surgical Technique
Indications
The indication for this surgery is massive irreparable supraspinatus and infraspinatus tears with muscle degeneration and fatty infiltration exceeding 50%, intact or reparable subscapularis and well-preserved intra-articular part of the LHBT at a distance of 4 cm from the labral footprint (Table 1).
Table 1.
Qualification to Surgery Using the LHBT for Irreparable Rotator Cuff Tears
| Indications | Contraindications |
|---|---|
| Intact/reparable subscapularis | Arthrosis |
| Retracted supraspinatus tendon | Damaged LHBT closer than 4 cm from the labral footprint |
| Retracted infraspinatus tendon | SLAP III-IV grade |
| Fatty degeneration >50% | |
| Tangent sign in MRI scans | |
| Well-preserved LHBT at the distance of 4 cm from the superior labrum |
LHBT, long head biceps tendon; MRI, magnetic resonance imaging.
Patient Positioning
The surgery is performed under general anesthesia with the patient positioned in the beach-chair position. The shoulder is prepared and draped in a sterile fashion.
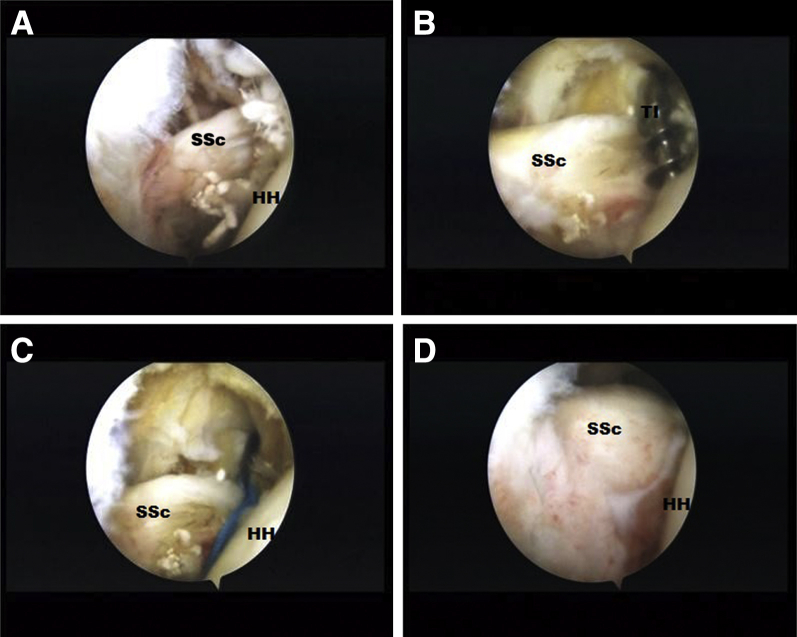
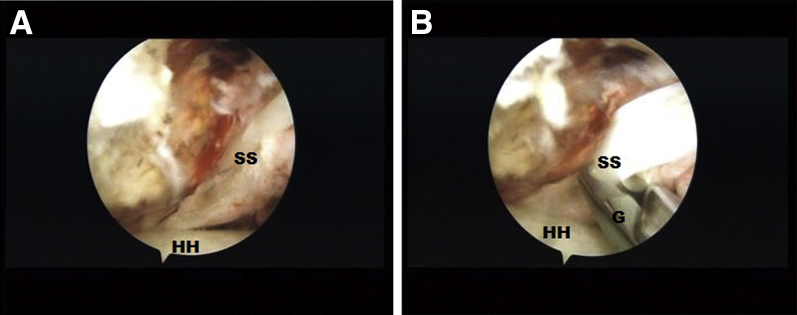
Diagnostic Arthroscopy and Subscapularis Repair
Arthroscopy is performed through standard posterior and anterior viewing portals (Video 1). After inspection (Fig 1) of the glenohumeral joint with a 30° arthroscope (Stryker, Kalamazoo, MI), the subscapularis tendon is evaluated with a grasper and repaired through the anterior portal once the tear is encountered. After the preparation of the bony bed at lesser tuberosity with a shaver (Arthrex, Naples, FL), double-stranded titanium anchors (Super Revo, Linvatec, Largo, FL) are placed. The “lasso-loop” technique is applied with 6 to 7 surgical knots tied to fix the tendon (Fig 2, Video 1). Then an additional lateral portal at the mid-glenoid level in the sagittal plane is performed and used to assess the morphology and traction of the supraspinatus and infraspinatus tendons (Fig 3). Once there is no possibility after release to pull back the tendons to their natural footprint, the diagnosis is confirmed and the “biceps patch” technique is considered.
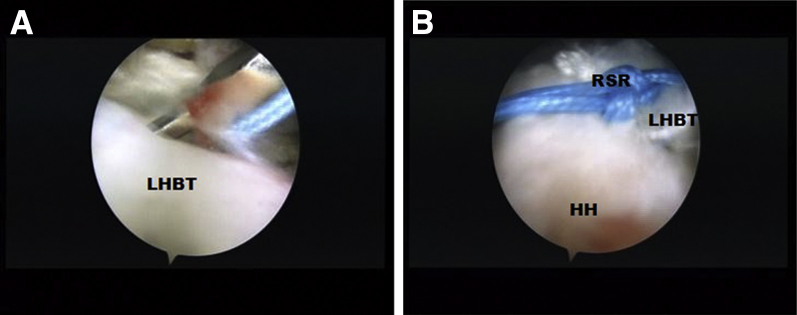
Fig 1.
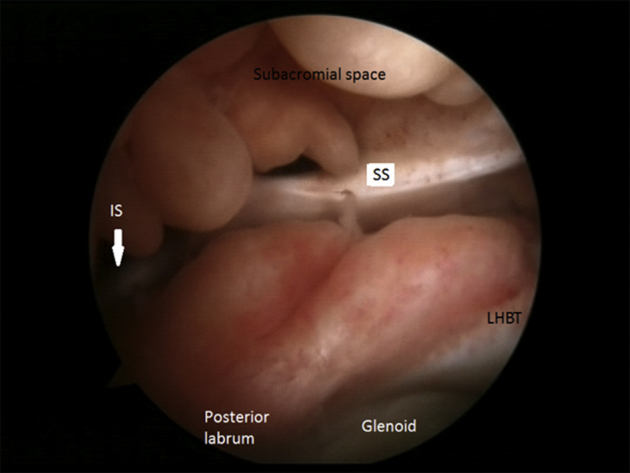
Arthroscopic view from the posterior portal in the right shoulder in a beach-chair position. Inspection of the glenohumeral joint. Injured and retracted supraspinatus (SS) and infraspinatus (IS). (LHBT, long head biceps tendon.)
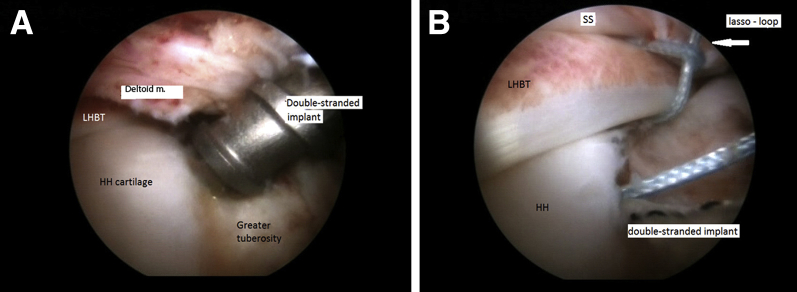
Fig 2.
Arthroscopic view from the posterior portal in the right shoulder in a beach-chair position. (A) Injured subscapularis (SSc). (B) Double-stranded titanium implant (TI) (Super Revo, Linvatec) is placed in the natural footprint of the SSc at the lesser tuberosity. (C) Lasso-loop technique is applied for SSc repair. (D) Repaired SSc. (HH, humeral head.)
Fig 3.
Arthroscopic view from the posterior portal in the right shoulder in a beach-chair position. (A) Injured supraspinatus (SS). (B) SS mobilization with a grasper (G). Pulling back the muscle to its natural footprint is impossible. Diagnosis of irreparability is confirmed. (HH, humeral head.)
Biceps Patch Technique
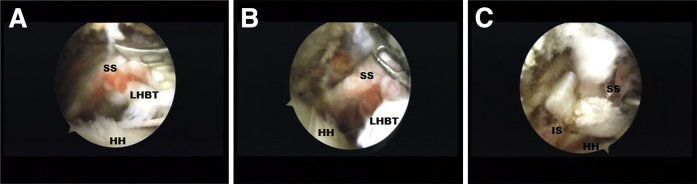
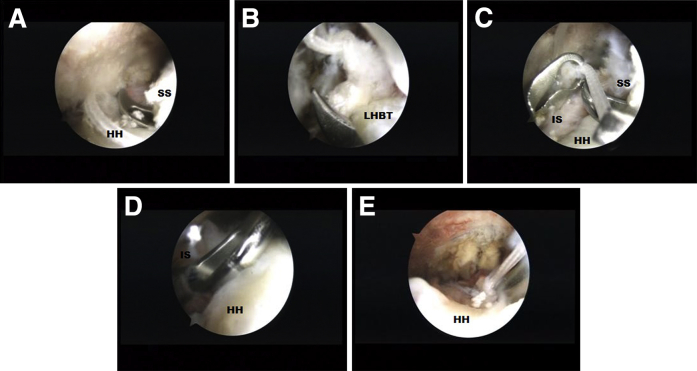
The structure of the LHBT and especially its proximal attachment to the superior labrum is assessed and the decision is made based on good tendon quality at a distance of 4 cm from the superior labrum. Looking through the posterior portal, additional working portals are created: anterolateral and posterolateral. The rotator tendon's remnants are refreshed through the posterolateral portal with the shaver (Arthrex). Viewing through the lateral portal, Seahawk Suture Passer (Conmed, Largo, FL) loaded with a Hi-Fi Suture (Conmed) is introduced through the posterolateral portal. Then the instrument is pierced through the infraspinatus remnant passing the Hi-Fi Suture (Conmed) from the subacromial to the articular side (Fig 4, Video 1). The working portal is changed to anterolateral. From this portal, the Seahawk Suture Passer (Conmed) is pierced through the supraspinatus and LHBT (Video 1) from the subacromial to the articular side, and the earlier transfixed Hi-Fi Suture (Conmed) is caught and passed through the LHBT and supraspinatus on its subacromial side. Both free ends of the Hi-Fi Suture (Conmed) are closed in the subacromial space and tied using 6 to 7 surgical knots (Fig 5, Video 1). In the next step, using the same Hi-Fi Suture (Conmed), side-to-side mattress sutures are laid passing the Seahawk Suture Passer (Conmed) through the infraspinatus, LHBT, and supraspinatus. The suture is tied using 6 to 7 surgical knots (Fig 6, Video 1). This maneuver should be repeated 2 to 3 times. This unique suturing technique creates a kind of “sandwich” system, where the LHBT is positioned between 2 rotator muscles. The applied mattress suture provides more strength for whole complex and avoids untying of the knots. The transfer of rotator muscle remnants onto the LHBT is performed in this way. Then the retraction suture is applied to facilitate choosing the best place for tenodesis (Fig 7, Video 1). To restore continuity and reattach the LHBT, the greater tubercle is debrided using the shaver (Arthrex) and the double-stranded implant (Super Revo 5 mm, Linvatec) is placed on the bone-cartilage boundary (Fig 8, Video 1). Next, applying the “lasso-loop” technique, the LHBT tenodesis to the center of the greater tuberosity is performed (Video 1). The retraction suture is removed. The proximal attachment of the LHBT is left intact. At the end of surgery, the “biceps patch” tenodesis is assessed through the posterior portal from subacromial space (Fig 9, Video 1), and if it is necessary, subacromial bursa removal and acromioplasty are performed.
Fig 4.
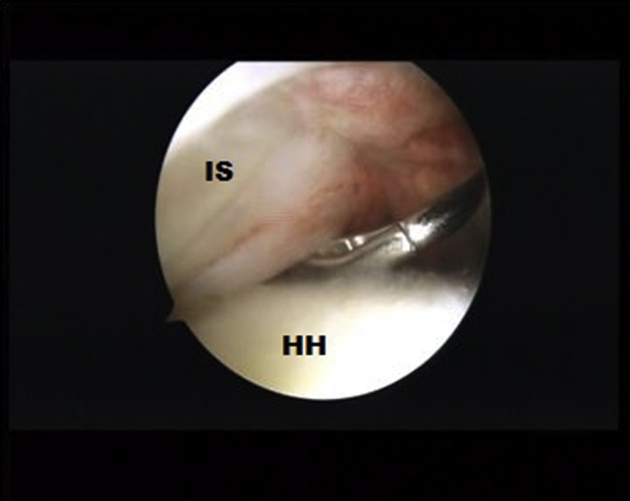
Arthroscopic view from the lateral portal in the right shoulder in a beach-chair position. First step of the “biceps patch technique.” Introduced through the posterolateral working portal, the Seahawk Suture Passer (Conmed) loaded with a high-strength suture is passed through the infraspinatus (IS) from the subacromial to articular side. (HH, humeral head.)
Fig 5.
Arthroscopic view from the posterior portal in the right shoulder in a beach-chair position. (A, B) Introduced through the anterolateral working portal, the Seahawk Suture Passer (Conmed) is pierced through the supraspinatus (SS) and the long head biceps tendon (LHBT) to pass the thread from articular to subacromial side. (C) The free ends of thread are closed in the subacromial space and tied using 6-7 surgical knots. (HH, humeral head; IS, infraspinatus.)
Fig 6.
Arthroscopic view from the lateral portal in the right shoulder in a beach-chair position. Mattress sutures. Seahawk Suture Passer introduced through the anterolateral portal is passed through the (A) supraspinatus (SS) and (B) long head biceps tendon (LHBT). (C) Then the instrument is used to hand the thread to the Seahawk Suture Passer (Conmed) to pass it through the LHBT. (D) Next the Seahawk Suture Passer (Conmed) is introduced through the posterolateral portal and pierced through the infraspinatus (IS). (E) The suture is tied in subacromial space. Two or three mattress sutures should be applied. (HH, humeral head.)
Fig 7.
Arthroscopic view from the lateral portal in the right shoulder in a beach-chair position. (A, B) Retraction suture (RSR) is applied on the long head biceps tendon (LHBT) to facilitate tenodesis. (HH, humeral head.)
Fig 8.
Arthroscopic view from the lateral portal in the right shoulder in a beach-chair position. (A) Double-stranded titan implant is placed at the greater tuberosity and (B) the lasso-loop technique is applied for LHBT tenodesis. (HH, humeral head; LHBT, long head biceps tendon; SS, supraspinatus.)
Fig 9.
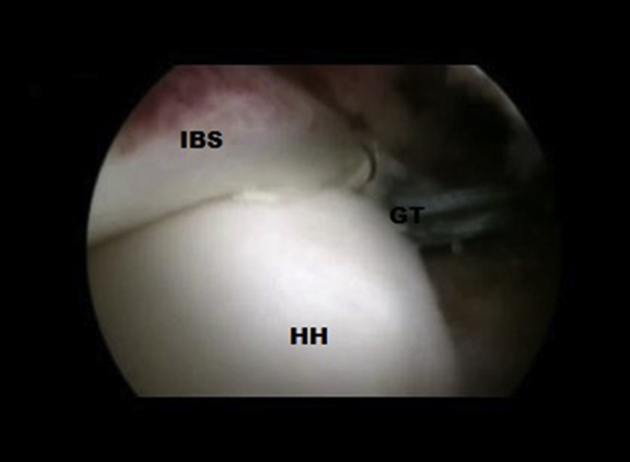
Arthroscopic view from the posterior portal in the right shoulder in a beach-chair position. The view after tenodesis at the greater tuberosity (GT). (HH, humeral head; IBS, infraspinatus—long head biceps tendon—supraspinatus complex.)
Rehabilitation
After the surgery, the patient is immobilized in the soft Dessault dressing for 6 weeks. From the second day after surgery, the patient started passive exercises of the shoulder joint in two 15-minute sessions per day.
Discussion
The superior capsular defect is an “essential lesion” in rotator cuff pathology, even more important than tendon discontinuity. Burkhart et al.3 described the role of the superior capsule in rotator cuff pathologies. Mihata et al.,6 in turn, indicated an important role of capsule continuity in superior capsule reconstruction. In the “biceps patch” technique by fixation of the LHBT on greater tubercle with simultaneously leaving the proximal footprint intact, the superior capsule was reconstructed in the most natural way, using native material present in the shoulder joint. This procedure is a modification of the LHB tendon-patch technique described by Sano et al.7 The fixed LHBT, spreading from the superior labrum to greater tuberosity, with reattached cuff muscles becomes the bridge for the retracted supraspinatus and infraspinatus using the rest of their strength and translating the forces onto natural footprint like in a “Graftjacket” technique.8 Whether to perform LHBT tenotomy underneath the greater tuberosity or not depends on surgeon preferences. It has been proven that both procedures had good clinical and cosmetic outcomes.9 The preservation of tendon continuity is more beneficial in terms of biology and biomechanics of the shoulder, providing better blood supply, and gives a better chance to accelerate the healing process. Moreover, the preserved LHBT plays important biomechanical roles as a vascularized graft bridging retracted supra- and infraspinatus to greater tubercle, and as a depressor for the humeral head during shoulder motion that potentially diminishes the risk of degenerative disease development.
Our preferred technique is not to cut the rest of the LHBT because of the reasons mentioned above. The “biceps patch” method allowed us to restore full active range of motion, and being a combination of the key assumptions of other techniques, it also allowed us to benefit from advantages and to omit most limitations known from other methods (Table 2). The most important advantages of the biceps patch technique are as follows: natural material of the LHBT used as a graft, small number of implants, minimized costs of the procedure, and nonexhausting other treatment options. Moreover, the technique is not technically demanding and is reproducible. On the other hand, there is some risk connected with applying this technique. The appropriate rehabilitation protocol addressed directly to this technique has not been developed yet. The strength of the patch remains unknown that gives the possibility of retear during forced physiotherapist maneuvers. The disadvantage of the biceps patch technique is also limitation in shoulder external rotation. The common footprint at the one point of greater tuberosity for supraspinatus and infraspinatus forces both muscles to work as one biomechanical unit, playing a role rather as initiators of shoulder abduction than shoulder external rotators. The risk related to general anesthesia, infections, and other general surgical risks also should not be omitted. All of the patients operated on with this technique signed the consent form. The study protocol was approved by the bioethics committee.
Table 2.
Advantages and Limitations of the Technique
| Advantages | Limitations |
|---|---|
| Low invasiveness of the procedure | Shoulder pain up to 6 mo after surgery |
| Natural vascularized high-strength material for grafting—avoid immune response to synthetic materials | Restoration of degenerated muscle strength impossible |
| Reduced amounts of implants, minimized costs of the procedure | Possible pain from the superior labrum (which has not been reported yet) |
| Easy to revise, nonexhausting other treatment options if next surgery needed | |
| Advanced skills for surgeons not required | |
| Low risk of infection | |
| Very good clinical results and high patient satisfaction 2 yr after surgery | |
| Reproducible |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic repair of massive irreparable rotator cuff tears using the long head biceps tendon (LHBT) as a natural patch for massive irreparable rotator cuff tear. The patient is positioned in a beach-chair position. The right shoulder is operated on. At the beginning, subscapularis tendon repair is performed using titanium implant placed at the lesser tuberosity and the lasso-loop technique. Next, we assess supraspinatus and infraspinatus morphology and mobilization. The diagnosis of irreparability is confirmed because there is no possibility to pull back the muscles to their natural footprint. At first, through the posterolateral working portal, the instrument loaded with a suture is passed through the infraspinatus from the subacromial to articular side. The next suture is passed using the anterolateral portal from the articular sides of the supraspinatus and LHBTs to subacromial space. Both ends of the strand are closed and tied using 6 to 7 surgical knots without cutting them. Furthermore, the mattress sutures are laid between the infraspinatus, LHBT, and supraspinatus, with untied ends of the strand. The mattress suture provides more strength for the whole complex formed by the supraspinatus, LHBT, and infraspinatus in comparison with single sutures. Now the suture is tied and the first step of our technique has been finished. In the second step, LHBT tenodesis at the center of greater tuberosity is performed. At first, the retraction suture is placed on the LHBT to facilitate choosing proper place for tenodesis. The double-stranded titanium implant is screwed at the greater tuberosity. The lasso-loop technique is applied for LHBT tenodesis. We passed both loops through the tendon. The last part of the procedure is to tie the knots to the implant. We do not cut the biceps tendon. At the end of surgery, we assess the results of our surgery looking through the posterior portal from subacromial space. We can observe the place of tenodesis and whole complex formed by the supraspinatus, LHBT, and infraspinatus.
References
- 1.Sayampanathan A.A., Andrew T.H. Systematic review on risk factors of rotator cuff tears. J Orthop Surg (Hong Kong) 2017;25 doi: 10.1177/2309499016684318. :2309499016684318. [DOI] [PubMed] [Google Scholar]
- 2.Castagna A., Garofalo R., Cesari E. No prosthetic management of massive and irreparable rotator cuff tears. Shoulder Elbow. 2014;6:147–155. doi: 10.1177/1758573214535369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams C.R., DeMartino A.M., Rego G., Denard P.J., Burkhart S.S. The rotator cuff and the superior capsule: Why we need both. Arthroscopy. 2016;32:2628–2637. doi: 10.1016/j.arthro.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castricini R., Galasso O., Riccelli D.A. Arthroscopic partial repair of irreparable, massive rotator cuff tears. Arthrosc Tech. 2017;6:e143–e147. doi: 10.1016/j.eats.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44:1423–1430. doi: 10.1177/0363546516631751. [DOI] [PubMed] [Google Scholar]
- 7.Sano H., Mineta M., Kita A., Itoi E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J Orthop Sci. 2010;15:310–316. doi: 10.1007/s00776-010-1453-5. [DOI] [PubMed] [Google Scholar]
- 8.Wong I., Burns J., Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19(suppl):104–109. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Kerschbaum M., Maziak N., Scheuermann M., Scheibel M. [Arthroscopic tenodesis or tenotomy of the long head of the biceps tendon in preselected patients: Does it make a difference?] Orthopade. 2017;46:215–221. doi: 10.1007/s00132-016-3358-2. [in German] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic repair of massive irreparable rotator cuff tears using the long head biceps tendon (LHBT) as a natural patch for massive irreparable rotator cuff tear. The patient is positioned in a beach-chair position. The right shoulder is operated on. At the beginning, subscapularis tendon repair is performed using titanium implant placed at the lesser tuberosity and the lasso-loop technique. Next, we assess supraspinatus and infraspinatus morphology and mobilization. The diagnosis of irreparability is confirmed because there is no possibility to pull back the muscles to their natural footprint. At first, through the posterolateral working portal, the instrument loaded with a suture is passed through the infraspinatus from the subacromial to articular side. The next suture is passed using the anterolateral portal from the articular sides of the supraspinatus and LHBTs to subacromial space. Both ends of the strand are closed and tied using 6 to 7 surgical knots without cutting them. Furthermore, the mattress sutures are laid between the infraspinatus, LHBT, and supraspinatus, with untied ends of the strand. The mattress suture provides more strength for the whole complex formed by the supraspinatus, LHBT, and infraspinatus in comparison with single sutures. Now the suture is tied and the first step of our technique has been finished. In the second step, LHBT tenodesis at the center of greater tuberosity is performed. At first, the retraction suture is placed on the LHBT to facilitate choosing proper place for tenodesis. The double-stranded titanium implant is screwed at the greater tuberosity. The lasso-loop technique is applied for LHBT tenodesis. We passed both loops through the tendon. The last part of the procedure is to tie the knots to the implant. We do not cut the biceps tendon. At the end of surgery, we assess the results of our surgery looking through the posterior portal from subacromial space. We can observe the place of tenodesis and whole complex formed by the supraspinatus, LHBT, and infraspinatus.