Abstract
An untreated posterolateral corner (PLC) injury in patients with a torn anterior cruciate ligament (ACL) may be a leading cause of ACL reconstruction failure. Combined ACL and PLC reconstruction is discussed in few studies in the literature. Femoral tunnel intersection in combined reconstruction has been reported to be high. Short grafts may render combined reconstruction undoable. This Technical Note describes a technique that allows a combined ACL and PLC reconstruction. The ACL graft is a 4-stranded hamstring tendon graft from 1 limb. The PLC graft is a doubled semitendinosus tendon graft from the contralateral side. One femoral tunnel is used connecting the femoral attachment of the PLC on the lateral wall of the lateral femoral condyle to the anatomic femoral ACL footprint on the medial wall of the lateral femoral condyle. The PLC graft is suspended on the ACL graft to be anchored on the cortex of the lateral femoral condyle with added fixation by an interference screw (Arthrex, Naples, FL). The PLC graft limbs are used for open reconstruction of the fibular collateral ligament, popliteus tendon, and popliteofibular ligament. This Technical Note describes a technique of combined ACL and PLC reconstruction with hamstring tendon autografts through a single femoral tunnel using graft-to-graft suspension and fixation.
The posterolateral corner (PLC) structures interact functionally with the anterior cruciate ligament (ACL). They act as primary restraint to varus and external rotation. The ACL acts as a secondary restraint to varus angulation.1, 2
Because of joint conformity of the lateral compartment of the knee and the inherent bony instability of the lateral tibial plateau, injuries of the PLC structures create a setting of marked instability.3 When this is combined with an ACL tear, the instability is frank.
In an ACL-PLC injured knee, an untreated PLC injury causes a significant increase in force on the ACL graft and may be a leading cause of graft failure. So the reconstruction should be combined.4
In the setting of combined ACL-PLC reconstruction procedures, femoral tunnel intersection has been reported to be high.5 The close proximity of ACL and lateral collateral ligament tunnels in the lateral femoral condyle carries the risk of bone weakening and tunnel collision,6, 7 and hence compromises graft function.
Angelini et al.8 did combine ACL-PLC reconstruction with a single femoral tunnel, but semitendinosus grafts smaller than 27 cm made the technique undoable because of the impossible reconstruction of the PLC structures with adequate graft size.
The purpose of this Technical Note is to describe a technique of combined ACL and PLC reconstruction using hamstring tendon autografts through a single femoral tunnel, using graft suspension and anchorage on the lateral cortex of the lateral femoral condyle and fixation by an absorbable interference screw (Arthrex, Naples, FL).
The technique allows combined ACL and PLC reconstruction and avoids femoral tunnel intersection and overcomes the obstacle of a short inadequate graft.
Surgical Technique
Examination Under Anesthesia and Diagnostic Arthroscopy
The patient is positioned supine on the operating table. Examination under anesthesia and diagnostic arthroscopy are performed to confirm the diagnosis. Arthroscopic work is delayed until after the open dissection of the PLC to avoid anatomical distortion from fluid extravasation.
Graft Preparation
The graft used for this technique is the hamstring tendon autografts. The ACL graft is a 4-stranded hamstring tendon graft from 1 limb. The PLC graft is a doubled semitendinosus tendon graft from the contralateral side (Fig 1A). The PLC graft is suspended on an ACL graft to be anchored on the cortex of the lateral femoral condyle by applying downward traction on the ACL graft from the tibial side.
Fig 1.
Graft preparation. (A) Posterolateral corner (PLC) graft formed by the semitendinosus from the contralateral side (brown arrow) is suspended in the anterior cruciate ligament (ACL) graft formed by the semitendinosus and gracilis from the ipsilateral side (yellow arrow). (B) Graft thickness measurement showing graft-to-graft suspension and anchorage mechanism. The ACL graft is passed through a certain diameter, whereas the ACL-PLC graft is locked at the point of suspension at the same diameter.
Graft-to-Graft Suspension and Anchorage Mechanism
When the PLC graft (contralateral semitendinosus auto-graft) is suspended to the ACL graft, the diameter increases at the point of suspension more than the diameter of the ACL graft alone so its passage through graft measure is impacted at the point of suspension (Fig 1B). This can be applied at the femoral tunnel where the ACL graft is impacted and anchored at the cortex of the lateral femoral condyle.
Open Dissection for PLC Reconstruction
A lateral hockey-stick skin incision is made along the iliotibial band (ITB) and distally extended midway between the fibular head and Gerdy's tubercle. The subcutaneous tissue is then dissected; a posteriorly based flap is developed to preserve the vascular support to the superficial tissues.
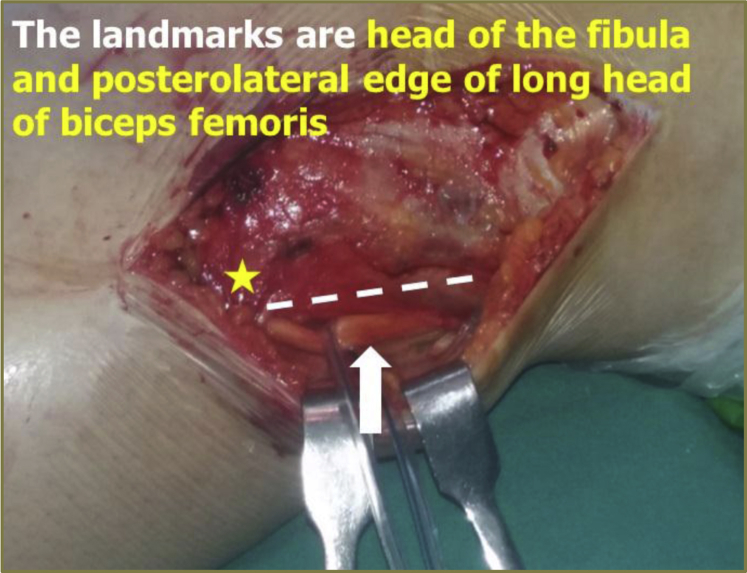
The long and short heads of the biceps femoris are exposed. The common peroneal nerve is explored and identified at the posterolateral edge of the long head of the biceps femoris (Fig 2). This starts approximately 6 to 8 cm proximal to the fibular head and extends distally to include the release of the peroneus longus fascia distal to the fibular head. The nerve is retracted and protected during the procedure. The interval between the lateral gastrocnemius tendon and the soleus muscle is identified by blunt dissection, and the posteromedial aspect of the fibular styloid and the popliteus musculotendinous junction are palpated.
Fig 2.
Open dissection for posterolateral corner reconstruction of the left knee with the patient in the supine position and the knee flexed about 30° showing the common peroneal nerve (white arrow), fibular head (yellow star), and posterolateral edge of the long head of the biceps femoris (white dotted line).
Fibular Tunnel Creation
Subperiosteal dissection of the lateral aspect of the fibular head is performed in an anterior to posterior direction, extended distally to the champagne glass drop-off of the fibular head. A small sulcus can be palpated where the distal fibular collateral ligament (FCL) inserts on the fibular head. Posteriorly, a small elevator is used to dissect off the soleus muscle from the posteromedial aspect of the fibular head, where the fibular tunnel will be created.
The entry point of the fibular tunnel should be immediately above the champagne glass drop-off, at the distal insertion site of the FCL, which has been described to be 28.4 mm from the styloid tip and 8.2 mm posterior to the anterior margin of the fibular head (Fig 3A).
Fig 3.
Fibular and tibial tunnels. (A) The entry point of the fibular tunnel in relation to the head of the fibula. It is 28.4 mm from the styloid tip (white dotted line) and 8.2 mm posterior to the anterior margin of the fibular head (yellow line). (B) The flat spot point of the tibial tunnel (yellow circle); it is located distal and medial to Gerdy's tubercle, just lateral to the tibial tubercle. (C) The posterior aperture of the tibial tunnel (yellow circle) in relation to the fibular tunnel (white circle). This point is located 1 cm proximal and 1 cm medial to the fibular tunnel. (D) Passing sutures in the fibular tunnel (white arrow) while the loop is left anterolaterally and in the tibial tunnel (yellow arrow) while the loop is left posteromedially.
With the help of an ACL aiming device (Arthrex), a guide pin is drilled starting from the entry point in a posteromedial direction toward the popliteofibular ligament attachment, and a 5-mm tunnel was then reamed over the guide pin. A passing suture is then placed through the tunnel leaving the loop anterolaterally to facilitate further passage of the graft.
PLC Tibial Tunnel
The entry point of the tibial tunnel is the flat spot on the anterolateral tibia located distal and medial to Gerdy's tubercle, just lateral to the tibial tubercle (Fig 3B). The posterior tibial popliteal sulcus, which marks the location of the musculotendinous junction of the popliteus muscle, is identified by palpation, where the posterior aperture of the tibial tunnel should be created. This point is located 1 cm proximal and 1 cm medial to the fibular tunnel (Fig 3C). Using an ACL aiming device (Arthrex), a transtibial guide pin is then drilled from anterior, at the flat spot to posterior at the posterior tibial popliteal sulcus. A 7-mm tunnel is then reamed over this guide pin, and the entry and exit sites are smoothed with a rasp. A passing suture is then placed through the tunnel leaving the loop posteromedially to facilitate further passage of the graft (Fig 3D).
Femoral Tunnel
The ITB is then split approximately 4 cm in line with its fibers slightly anterior to the palpated FCL attachment. Sharp dissection is performed in this location in a proximal to distal direction exposing the lateral epicondyle.
The FCL femoral attachment site can be located 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle (Fig 4A). The femoral attachment of the popliteus tendon (PLT) has been reported to be located 18.5 mm anterior to the FCL insertion, in the anterior fifth of the popliteal sulcus (Fig 4B). The isometric point for reconstruction of the FCL and PLT is used, as recommended by Stannard et al.9 in PLC reconstruction. It is located immediately anterior to the point at which the FCL and the PLT cross.
Fig 4.
Femoral tunnel. (A) Fibular collateral ligament (FCL) site (yellow circle) in relation to the lateral epicondyle (black circle). It is 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle. (B) Popliteus tendon (PLT) site (white circle) in relation to the FCL site (yellow circle); it is 18.5 mm anterior to the FCL insertion, in the anterior fifth of the popliteal sulcus. (C) The entry point of the femoral tunnel (yellow arrow) in relation to the lateral femoral epicondyle (black circle); it is just proximal and anterior to the lateral epicondyle. (D) The anterior cruciate ligament (ACL) aiming device adjustment: settled outside on the entry point of the femoral tunnel (white arrow) and intra-articular through the anterolateral portal (black arrow) on the ACL femoral foot print.
At this step, arthroscopy is started. Meniscal tears and chondral lesions are dealt with. With arthroscopy in the anteromedial portal, the aiming device through the anterolateral portal is fitted between the isometric point of PLC (Fig 4 C and D) and the anatomic femoral attachment of ACL (Fig 5A). A guide pin is drilled between the 2 points (Fig 5B). A tunnel is then reamed over this guide pin, with a diameter equal to the ACL graft diameter. During reaming of the femoral tunnel, a curette is used to protect the posterior cruciate ligament (PCL) (Fig 5C). Then, passing sutures are introduced from outside through the femoral tunnel and retrieved at the femoral aperture (Fig 5D) to outside again through the anterolateral portal (Figs 5E and 6).
Fig 5.
Arthroscopic views of the left knee through the anteromedial portal showing (A) The anterior cruciate ligament (ACL) aiming device settled on the femoral foot print of the ACL. (B) A guide pin drilled from outside to inside through the ACL aiming device. (C) A curette used over the guide pin to protect the posterior cruciate ligament. (D) The femoral tunnel aperture of the ACL (white arrow). (E) Passing sutures through the femoral tunnel are retrieved. (F) Passing sutures passed through the femoral tunnel to the anterolateral portal.
Fig 6.
Arthroscopic view of the left knee through the anterolateral portal showing (A) the anterior cruciate ligament (ACL) aiming device settled on the tibial foot print of the ACL, (B) a guide pin passage at the tibial foot print of the ACL, (C) a curette used over the guide pin to protect the lateral femoral condyle and passing sutures, (D) the passing sutures passed from the femoral tunnel to the tibial tunnel to outside, (E) the ACL graft passage, and (F) the ACL graft after fixation.
ACL Tibial Tunnel
Single-bundle ACL reconstruction is performed using 4-stranded hamstring tendon autografts. The ACL tibial tunnel is made 3 mm anterior to the inner border of the anterior horn of the lateral meniscus, just lateral to the medial eminence, and 7 to 10 mm anterior to the PCL (Fig 6 A-C). Then, the passing sutures in the femoral tunnel are kept their and then retrieved through the tibial tunnel (Fig 6D) to exterior with the loop of sutures toward the tibial side.
Graft Passage, Suspension, and Anchorage
By using the passing sutures, the graft is passed through the tibial and then the femoral tunnels (Fig 6E). After passage of the ACL graft, the PLC graft is suspended to the ACL graft and anchored on the cortex of the lateral femoral condyle (Fig 7A) by applying traction on the ACL graft from the tibial side and then added fixation at the femoral tunnel by a bio-interference screw (Arthrex). The screw is put superior or anterior to the graft. Recycling of the ACL graft then fixation at tibial tunnel is performed with the knee flexed at 30° neutral rotation and slight posterior drawing (Fig 6F).
Fig 7.
PLC graft passage. (A) Posterolateral corner (PLC) graft suspended on the anterior cruciate ligament (ACL) graft before ACL graft fixation. (B) PLC graft limbs passed under the iliotibial band to the entry point of the fibular tunnel (white arrow) and to the posterior aperture of the tibial tunnel (yellow arrow). (C) Fibular collateral ligament graft limb passage through the fibular tunnel (white arrow) from anterolateral to posteromedial. (D) Both graft limbs (yellow arrows) passed through the tibial tunnel from posteromedial to anterior.
One should palpate over the interference screws (Arthrex) to ensure that they are adequately positioned within the tunnels because proud screws can lead to fascial irritation postoperatively.
After creating a soft tissue channel by blunt dissection, the PLC graft is passed under the iliotibial tract (Fig 7B). The PLT graft limb is passed first along the popliteal hiatus in the posterolateral capsule and should exit between the lateral gastrocnemius and the soleus muscles. The FCL graft limb is passed under the ITB and passed through the fibular tunnel from the anterolateral to posteromedial direction (Fig 7C). Then both limbs are passed from posteromedial to anterior through the tibial tunnel (Fig 7D) and are fixed by an interference screw (Arthrex). The graft is fixed with the knee flexed 30°, slight valgus, and with a slight internal rotation of the foot, to avoid an external rotation deformity of the tibia10 due to the fixation of the ACL graft first.
Clinical and Arthroscopic Evaluation at the End of Procedure
After the fixation of all structures, knee stability and range of motion are assessed. The anterior drawer test, varus stress test, and posterolateral drawer test are used to assess reconstruction.
Arthroscopy is performed at the end of the procedure to check ACL reconstruction and to examine the lateral compartment (Fig 8 A and C) and the intra-articular PLT graft (Fig 8 B and D). At the end, standard layered closure for the skin is performed. Then, a standard long leg knee immobilizer is placed, and the patient is transferred to the recovery room.
Fig 8.
Arthroscopic view of the lateral compartment of the left knee through the anterolateral portal showing (A and B) wide joint space and absent popliteus tendon (PLT) before posterolateral corner (PLC) reconstruction, normal articular cartilage (yellow arrows) and torn lateral meniscus (white arrows); (C and D) normal joint space and the PLT graft (red arrow) after PLC reconstruction.
The advantages of the technique, and pearls and pitfalls are mentioned in Tables 1 and 2, respectively.
Table 1.
Advantages of the Technique
| Advantages |
|---|
|
|
|
|
ACL, anterior cruciate ligament; FCL, fibular collateral ligament; PFL, popliteofibular ligament; PLC, posterolateral corner; PLT, popliteus tendon.
Table 2.
Surgical Steps, Pearls, and Pitfalls
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Tourniquet | Applied to both sides but elevate the tourniquet on the normal limb first for graft harvest. Then after draping and complete instrumentation elevate the tourniquet on the affected limb | If the tourniquet is elevated on the affected limb first, this will lead to increased tourniquet time and the need for its release and then elevation increasing time of surgery |
| Graft harvest | Use a closed or open tendon stripper to free the graft. Graft length will not be an obstacle to this technique; a length down to 20 cm may be adequate in either ACL or PLC graft preparation | Using an open tendon stripper may be associated with premature cutting of the graft and hence short graft |
| Open dissection |
|
If arthroscopic work is performed before open dissection of the PLC, fluid extravasation will cause anatomical distortion of extra-articular structures with difficult dissection |
|
Nonreleased, nonprotected nerve renders it liable to injury by excessive traction, retraction or guide pins, or reamers used during the procedure or liable to compression by postoperative hematoma | |
| PLC tunnels | The entry of the fibular tunnel should be immediately above the champagne glass drop-off, at the distal insertion site of the FCL | Reaming the fibular tunnel too proximally may lead to fracture |
| A passing suture is placed through the fibular tunnel leaving the suture loop anterolaterally and through the tibial tunnel leaving the loop posteromedially to facilitate the correct passage of the graft | Incorrect untidy suture passage leads to incorrect haphazard graft passage and hence false PLC reconstruction | |
| ACL tunnels | Femoral tunnel creation is performed first before reaming the tibial tunnel. This allows easy localization of the anatomic ACL femoral point | Tibial tunnel creation first will lead to bad visualization because of bone debris and loss of joint distension |
| A femoral guide pin is inserted with the use of an ACL aiming device passed through the anterolateral portal and the arthroscope turned to the anteromedial portal | The use of an ACL aiming device passed through the anteromedial portal for the femoral guide pin insertion. It is difficult and cannot be performed | |
| Use a curette through the anteromedial portal to protect and retract the PCL medially during reaming | PCL retraction allows better visualization and avoids its injury | |
| A tibial guide pin is inserted while the knee is in 90° flexion for proper visualization | Knee flexion >90°will draw the infra-patellar fat pad into the field making visualization difficult | |
| Intermittent use of a plastic stopper in tibial and femoral tunnels prevents loss of fluid and allows washout of bone debris through the tunnels | Fluid loss will lead to the loss of joint distension and accumulation of bone debris with bad visualization | |
| Graft passage and fixation | The ACL graft is passed first and then the PLC graft is suspended on the ACL graft on the lateral cortex of the femur | If the PLC graft is suspended on the ACL graft before the ACL graft passage, the graft will be impacted at the tibial side if retrograde passage is used |
| The ACL graft is fixed at the femoral tunnel first and then at the tibial tunnel | If the ACL graft is fixed at the tibial tunnel first, this will lead to the loss graft anchorage obtained by suspension | |
| ACL graft | The entry point of the femoral tunnel is enlarged by a reamer to allow settling of the graft at the point of suspension | If not, the painful prominent graft under the iliotibial band and delayed suspended graft incorporation may occur |
| A bioabsorbable interference screw of the same graft thickness with 30 to 35 mm length is used. Ensure settling of the screw in the tunnel | If a longer screw is used, it may protrude inside the joint causing graft fritting or protrude under the iliotibial band causing its irritation | |
| The interference screw is inserted in the anterior or proximal half of the femoral tunnel. This is performed according to the orientation of the suspended graft; if the 2 limbs are oriented vertically after their suspension, the screw is inserted in the anterior half of the femoral tunnel, whereas if 2 limbs are oriented horizontally after their suspension, the screw is inserted in the proximal half of the femoral tunnel | Insertion of the interference screw into the posterior or distal half of the femoral tunnel will lead to graft impingement on the screw and also will shorten the graft and cause its prominence | |
| ACL graft fixation at the tibial side is performed after femoral fixation to control graft tension | If it is performed before femoral fixation, graft tension or graft anchorage will be jeopardized | |
| PLC graft | The PLT graft limb is passed first and deep to the (medial) FCL graft limb. Both graft limbs are passed deep to the (medial) iliotibial band | Passage of the FCL graft limb first makes its cross over the PLT graft limb difficult or makes it to cross under the PLT graft, which is nonanatomical |
| The PLC graft is fixed in the slight internal rotation of the foot | If the PLC graft is fixed in the neutral rotation of the foot, this may lead to external rotation deformity of the tibia associated with ACL graft fixation first | |
| Arthroscopic evaluation | Arthroscopy at the end to check ACL reconstruction, ACL graft tension, lateral compartment joint space, and to show the intra-articular PLT graft | |
| Limitations | It could be performed in skeletally immature patients with caution. The PLC ligaments are attached distal to physis | If performed without caution, this may affect the physis with its premature closure laterally |
ACL, anterior cruciate ligament; FCL, fibular collateral ligament; PLC, posterolateral corner; PLT, popliteus tendon.
Discussion
The failure rates for primary ACL reconstruction are reported to be between 0.7% and 8%, and the failure rates of graft revisions are in the range of 5% to 52%.11, 12 Many authors have suggested that the main cause of graft failures is unrecognized and therefore untreated PLC injuries.13, 14, 15
ACL-PLC injuries were reported, and several studies have suggested that up to 11% of ACL tears are partnered by PLC injuries.15, 16 The diagnosis of PLC injuries is a challenge and the assessment is complex. The PLC injuries of the knee can easily be missed on knee examination, especially when there is a concomitant ACL tear.15 It requires a high degree of clinical suspicion for possible injury.17
Missed, neglected, or poorly treated PLC injuries can result in posterolateral rotatory instability of the knee, which is a pathological instability caused by posterolateral tibial subluxation when an external rotational force is applied to the knee joint.6, 18 Posterolateral rotatory instability leads to a varus thrust gait, which increases forces on the medial compartment of the knee and may result in meniscal injuries and accelerated medial compartment osteoarthritis.19 It also increases the forces on the ACL and PCL, which can potentially lead to graft failure in the setting of ACL reconstruction.20, 21
LaPrade et al.22described an anatomic reconstruction of the PLC structures using the native attachments of the FCL, PLT, and PFL. The FCL is the primary restraint to varus angulation. LaPrade et al.22 showed the biomechanical role of the PLT, as a primary static stabilizer to external rotation of the knee. McCarthy et al.23 showed the biomechanical need for anatomic reconstruction of the PFL to restore knee stability.
It is now fairly clear that to restore static stability under varus and external rotation testing,9 in patients with ACL-PLC instability, it is important to reconstruct the FCL, the PLT, and the popliteofibular ligament24 as well as ACL reconstruction simultaneously.21
In the setting of combined ACL-PLC reconstruction procedures, there is close proximity of ACL and lateral collateral ligament tunnels in the lateral femoral condyle.7 Shuler et al.25 showed that femoral tunnel intersection, convergence, or tunnel collision is very common, and its prevention depends not only on the surgeon's skill but also on the patient's anatomy. Even with the correct techniques, it is often not possible to prevent collision.
Several PLC reconstruction techniques recommend proximal and anterior angulation of PLC tunnels, to avoid the risk of damage to the articular cartilage of the lateral femoral condyle or trochlea when creating a tunnel for PLT reconstruction.26, 27 On the other hand, other PLC reconstruction techniques do not recommend any proximal angulation in the coronal plane25, 26 to avoid the risk of bone weakening and tunnel collision and hence compromise graft function.
Angelini et al.8 did combine ACL-PLC reconstruction with a single femoral tunnel. The technique described is an effective solution for reconstruction of combined ACL-PLC injuries, but semitendinosus grafts smaller than 27 cm make the technique undoable because of the impossible reconstruction of the PLC structures with adequate graft size.
The accuracy of ACL tunnel placement is also important in combined ligament reconstruction. Recently when comparing transtibial ACL tunnel creation with outside-in and anteromedial portal techniques, outside-in tunnel according to Garofalo et al.28 provide a higher statistically significant percentage of coverage of the ACL femoral footprint than the transtibial ACL tunnel and anteromedial portal tunnels.29 Also the outside-in technique according to Burnham et al.30 may be more beneficial in obese patients, skeletally immature patients, or revision cases.
In this Technical Note, outside-in single femoral tunnel is performed in the lateral femoral condyle for combined ACL-PLC reconstruction connecting the anatomic ACL femoral footprint from inside to the isometric point for the PLC attachment point on the outside. This minimizes the number of femoral tunnels, avoids tunnel collision in the lateral femoral condyle, avoids possible damage to the articular cartilage of the lateral femoral condyle or trochlea, and minimizes the number of interference screws needed.
The PLC graft (doubled semitendinosus) is suspended on the ACL graft (quadrupled semitendinosus and gracilis) on the lateral cortex of the lateral femoral condyle. At the femoral tunnel, the ACL graft is fixed, locked, and anchored by this suspension. Interference screw fixation is added. Graft suspension gives adequate graft length and width for combined ACL-PLC reconstruction and decreases the need for interference screws. The interference screw addition at the femoral tunnel gives more stable graft fixation.
This technique has a potential risk of common peroneal nerve injury, prolonged surgical time and possible tourniquet paralysis, and possible physeal injury in skeletally immature patients. Acute injuries, knee dislocations, and skeletally immature patients are relative limitations.
Many series evaluated ACL reconstruction in skeletally immature patients with all-epiphyseal reconstruction31, 32 or transphyseal reconstruction.33 The overall functional results in many series were good; there was only a single case of a growth abnormality that consisted of a valgus deformity.34
In this technique, the physis could be spared during femoral tunnel and FCL and PLT tunnel creation, whereas it is not spared in ACL tibial tunnel creation. Careful surgical dissection avoids common peroneal nerve injury and physeal injury. Arranged surgical steps shorten the surgical time and avoid the tourniquet complications.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A technique of combined anterior cruciate ligament (ACL) and posterolateral corner (PLC) reconstruction with hamstring tendon autografts through single femoral tunnel using graft-to-graft suspension and fixation of the left knee with the patient in the supine position. The following steps of the technique are shown: (1) examination under anesthesia and diagnostic arthroscopy; (2) graft preparation; (3) graft-to-graft suspension and anchorage mechanism; (4) open dissection for PLC reconstruction; (5) fibular tunnel creation; (6) PLC tibial tunnel creation; (7) femoral tunnel creation; (8) ACL tibial tunnel creation; (9) graft passage, suspension, and anchorage; and (10) arthroscopic evaluation at the end of the procedure.
References
- 1.Takeda Y., Xerogeanes J.W., Livesay G.A. Biomechanical function of the human anterior cruciate ligament. Arthroscopy. 1994;10:140–147. doi: 10.1016/s0749-8063(05)80081-7. [DOI] [PubMed] [Google Scholar]
- 2.Markolf K.L., Graves B.R., Sigward S.M., Jackson S.R., McAllister D.R. How well do anatomical reconstructions of the posterolateral corner restore varus stability to the posterior cruciate ligament-reconstructed knee? Am J Sports Med. 2007;35:1117–1122. doi: 10.1177/0363546507299240. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Terry G.C. Injuries to the posterolateral aspect of the knee: Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433–438. doi: 10.1177/036354659702500403. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 5.Steven J.N., Michael P.H., Ronald S.K., James E.T. Tunnel intersection in combined anatomic reconstruction of the ACL and posterolateral corner. Orthopedics. 2013;36:529–532. doi: 10.3928/01477447-20130624-07. [DOI] [PubMed] [Google Scholar]
- 6.Albright J.P., Brown A.W. Management of chronic posterolateral rotatory instability of the knee: Surgical technique for the posterolateral corner sling procedure. Instr Course Lect. 1998;47:369–378. [PubMed] [Google Scholar]
- 7.Neven E., D'Hooghe P., Bellemans J. Double-bundle anterior cruciate ligament reconstruction: A cadaveric study on the posterolateral tunnel position and safety of the lateral structures. Arthroscopy. 2008;24:436–440. doi: 10.1016/j.arthro.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Angelini F.J., Helito C.P., Tozi M.R. Combined reconstruction of the anterior cruciate ligament and posterolateral corner with a single femoral tunnel. Arthrosc Tech. 2013;2:e285–e288. doi: 10.1016/j.eats.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stannard J.P., Brown S.L., Farris R.C., McGwin G., Jr., Volgas D.A. Reconstruction of the posterolateral corner of the knee. Arthroscopy. 2005;21:1051–1059. doi: 10.1016/j.arthro.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 10.Wentorf F.A., LaPrade R.F., Lewis J.L., Resig S. The influence of the integrity of posterolateral structures on tibiofemoral orientation when an anterior cruciate ligament graft is tensioned. Am J Sports Med. 2002;30:796–799. doi: 10.1177/03635465020300060701. [DOI] [PubMed] [Google Scholar]
- 11.Johnson D.L., Harner C.D., Maday M.G. Revision anterior cruciate ligament surgery. In: Fu F., Harner C.D., Vince K.G., editors. Knee surgery. Williams & Wilkins; Baltimore: 1994. pp. 877–895. [Google Scholar]
- 12.Noyes F.R., Barber-Westin S.D. Revision anterior cruciate ligament surgery: Experience from Cincinnati. Clin Orthop. 1996;325:116–129. doi: 10.1097/00003086-199604000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83–88. doi: 10.1177/036354658901700114. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade R.F., Hamilton C.D., Engebretsen L. Treatment of acute and chronic combined anterior cruciate ligament and posterolateral knee ligament injuries. Sports Med Arthrosc Rev. 1997;5:91–99. [Google Scholar]
- 15.O'Brien S.J., Warren R.F., Pavlov H., Panariello R., Wickiewicz T.L. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am. 1991;73:278–286. [PubMed] [Google Scholar]
- 16.Hughston J.C., Jacobson K.E. Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1985;67:351–359. [PubMed] [Google Scholar]
- 17.Ross G., DeConciliis G.P., Choi K., Scheller A.D. Evaluation and treatment of acute posterolateral corner/anterior cruciate ligament injuries of the knee. J Bone Joint Surg Am. 2004;86(suppl 2):2–7. doi: 10.2106/00004623-200412002-00002. [DOI] [PubMed] [Google Scholar]
- 18.Arnoczky S.P., Grewe S.R., Paulos L.E. Instability of the anterior and posterior cruciate ligaments. Instr Course Lect. 1991;40:199–270. [PubMed] [Google Scholar]
- 19.Griffith C.J., Wijdicks C.A., Goerke U., Michaeli S., Ellermann J., LaPrade R.F. Outcomes of untreated posterolateral knee injuries: An in vivo canine model. Knee Surg Sports Traumatol Arthrosc. 2011;19:1192–1197. doi: 10.1007/s00167-010-1358-z. [DOI] [PubMed] [Google Scholar]
- 20.Harner C.D., Vogrin T.M., Hoher J., Ma C.B., Woo S.L. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med. 2000;28:32–39. doi: 10.1177/03635465000280011801. [DOI] [PubMed] [Google Scholar]
- 21.LaPrade R.F., Muench C., Wentorf F., Lewis J.L. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: A biomechanical study. Am J Sports Med. 2002;30:233–238. doi: 10.1177/03635465020300021501. [DOI] [PubMed] [Google Scholar]
- 22.LaPrade R.F., Wozniczka J.K., Stellmaker M.P., Wijdicks C.A. Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction: The “fifth ligament” of the knee. Am J Sports Med. 2010;38:543–549. doi: 10.1177/0363546509349493. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy M., Camarda L., Wijdicks C.A., Johansen S., Engebretsen L., LaPrade R.F. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38:1674–1681. doi: 10.1177/0363546510361220. [DOI] [PubMed] [Google Scholar]
- 24.Veltri D.M., Deng X.H., Torzilli P.A., Maynard M.J., Warren R.F. The role of the popliteofibular ligament in stability of the human knee. A biomechanical study. Am J Sports Med. 1996;24:19–27. doi: 10.1177/036354659602400105. [DOI] [PubMed] [Google Scholar]
- 25.Shuler M.S., Jasper L.E., Rauh P.B., Mulligan M.E., Moorman C.T., III Tunnel convergence in combined anterior cruciate ligament and posterolateral corner reconstruction. Arthroscopy. 2006;22:193–198. doi: 10.1016/j.arthro.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Camarda L., D'Arienzo M., Patera G.P., Filosto L., LaPrade R.F. Avoiding tunnel collisions between fibular collateral ligament and ACL posterolateral bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:598–603. doi: 10.1007/s00167-010-1299-6. [DOI] [PubMed] [Google Scholar]
- 27.Gelber P.E., Erquicia J.I., Sosa G. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: Computed tomography evaluation in a cadaveric model. Arthroscopy. 2013;29:257–265. doi: 10.1016/j.arthro.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 28.Garofalo R., Mouhsine E., Chambat P., Siegrist O. Anatomic anterior cruciate ligament reconstruction: The two-incision technique. Knee Surg Sports Traumatol Arthrosc. 2006;33:510–516. doi: 10.1007/s00167-005-0029-y. [DOI] [PubMed] [Google Scholar]
- 29.Gaditoka H.R., Sim J.A., Hosseini A., Gill T.J., Li G. The relationship between femoral tunnels created by the transtibial, anteromedial portal, and outside-in techniques and the anterior cruciate ligament footprint. Am J Sports Med. 2012;40:882–888. doi: 10.1177/0363546511434276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burnham J.M., Malempati C.S., Carpiaux A., Ireland M.L., Johnson D.L. Anatomic femoral and tibial tunnel placement during anterior cruciate ligament reconstruction: Anteromedial portal all-inside and outside-in techniques. Arthrosc Tech. 2017;6:e275–e282. doi: 10.1016/j.eats.2016.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cruz A.I., Jr., Fabricant P.D., McGraw M., Rozell J.C., Ganley T.J., Wells L. All-epiphyseal ACL reconstruction in children: Review of safety and early complications. J Pediatr Orthop. 2015;37:204–209. doi: 10.1097/BPO.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 32.Nawabi D.H., Jones K.J., Lurie B., Potter H.G., Green D.W., Cordasco F.A. All-inside, physeal-sparing anterior cruciate ligament reconstruction does not significantly compromise the physis in skeletally immature athletes: A postoperative physeal magnetic resonance imaging analysis. Am J Sports Med. 2014;42:2933–2940. doi: 10.1177/0363546514552994. [DOI] [PubMed] [Google Scholar]
- 33.Calvo R., Figueroa D., Gili F. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med. 2015;43:289–294. doi: 10.1177/0363546514557939. [DOI] [PubMed] [Google Scholar]
- 34.Pennock A., Michael M.M., Wu M. Anterior cruciate ligament reconstruction in skeletally immature patients. Curr Rev Musculoskelet Med. 2016;9:445–453. doi: 10.1007/s12178-016-9367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique of combined anterior cruciate ligament (ACL) and posterolateral corner (PLC) reconstruction with hamstring tendon autografts through single femoral tunnel using graft-to-graft suspension and fixation of the left knee with the patient in the supine position. The following steps of the technique are shown: (1) examination under anesthesia and diagnostic arthroscopy; (2) graft preparation; (3) graft-to-graft suspension and anchorage mechanism; (4) open dissection for PLC reconstruction; (5) fibular tunnel creation; (6) PLC tibial tunnel creation; (7) femoral tunnel creation; (8) ACL tibial tunnel creation; (9) graft passage, suspension, and anchorage; and (10) arthroscopic evaluation at the end of the procedure.