Abstract
Humana, a large health care company, has set a goal of 20% improvement in health in the communities it serves by 2020. The metric chosen for the Bold Goal initiative was the HRQOL-4 version of the Centers for Disease Control and Prevention (CDC) Healthy Days survey. This paper presents the methods for measuring progress, reports results for the first year of tracking, and describes Humana's community-based interventions. Across 7 specially designated “Bold Goal” communities, mean unhealthy days declined from 10.98 in 2015 to 10.64 in 2016, which represented a 3.1% relative, or 0.34 absolute, decline. This compares with a 0.17 absolute unhealthy days decline in Humana's national population overall. The paper also describes how additional work identifying associations between social determinants of health (SDOH) and Healthy Days is influencing Humana's strategy. Lastly, a strategy of community engagement is illustrated through 2 case examples: San Antonio and Knoxville. In the San Antonio area, the community in which Humana has been involved the longest, unhealthy days dropped by 9.0% (−0.95 absolute) from a mean 10.52 to 9.57 unhealthy days. In Knoxville, one of the newer areas of engagement, mean unhealthy days declined by 4.8% (−0.61 absolute), representing declines in both physically and mentally unhealthy days. Overall, results are encouraging, and Humana expects declines to accelerate over time as initiatives are launched and scaled in Bold Goal communities.
Keywords: : healthy days, social determinants of health population health, quality of life, community health
Background
For more than 3 decades, the United States has had an official national agenda for population health and quality improvement: the Healthy People program administered by the Centers for Disease Control and Prevention (CDC). The program sets new goals every 10 years.1 The current phase, Healthy People 2020, has not only provided benchmarks specifically for public health departments,2–5 but also has inspired similar goals in the private sector.6–8
In keeping with this trend, Humana, a large health care company offering Medicare Advantage, prescription drug, and commercial plans, has set a goal of 20% improvement in health in the communities it serves by 2020, including the 47,000 associates who work for Humana. Humana has chosen to measure achievement of what has been named the “Bold Goal” through health-related quality of life (HRQOL). HRQOL instruments capture the effects of social and environmental factors, as well as the effects of medical care. Another advantage of HRQOL measurement is that it gives voice to individuals. The particular metric chosen for the Bold Goal initiative was the HRQOL-4 version of the CDC Healthy Days survey. The 4 questions of the HRQOL-4 survey are listed in Table 1. Responses to questions 2 and 3 about recent unhealthy days yield a summary index for an individual. Individual Healthy Days responses can then be aggregated to population averages to allow observation of population trends over time. Healthy Days data have been collected extensively in national surveys, such as the Behavioral Risk Factor Surveillance System (BRFSS) and the National Health and Nutrition Examination Survey, as well as the Medicare Health Outcomes Survey, which is a longitudinal, patient-reported outcomes measure that the Centers for Medicare & Medicaid Services (CMS) requires all Medicare Advantage plans to collect. An earlier publication described findings with respect to the use of Healthy Days in the published literature.9 Healthy Days also is among the general health status measures defining goals for the national Healthy People 2020 program.10
Table 1.
Centers for Disease Control and Prevention Health-Related Quality of Life-4 Survey Instrument—Healthy Days
| 1 | Would you say that in general your health is excellent, very good, good, fair, or poor? |
| 2 | Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good? |
| 3 | Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good? |
| 4 | During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation? |
Implementation of the Bold Goal strategy has consisted of the following elements:
Data analysis to understand the health conditions, and the root causes of those conditions, that influence Healthy Days.
Programs designed to address those factors. Part of this effort has included designation of “Bold Goal” communities in which broad-scale investments in population health could be made.
A test and learn approach that allows the design of increasingly effective population health interventions.
Thus, during the planning year, 2014, Humana began to verify associations between various factors and Healthy Days responses within its own populations. The company learned from the literature that Healthy Days responses had been found to be associated with a number of chronic health conditions11–14 and with health-related behavior.15–17 This 2014 analysis focused on chronic conditions and confirmed many of the previously reported associations, as well as an association with greater utilization, in Humana populations.18
Tracking began in 2015, the baseline year. During that year the company also began to address factors associated with Healthy Days measures. The interventions that will help to achieve the Bold Goal are designed to improve process measures, intermediate outcomes such medication adherence, and disease-specific health outcomes such as reduction in diabetes complications progression, while the ultimate goal is improvement in Healthy Days.
Year 2016 afforded the first opportunity to measure progress. During this year the company applied early learnings to optimize the strategy and continued to test and scale interventions. Humana also began to think more broadly about health status and the influence of social determinants of health (SDOH). As demonstrated by the seminal literature review published by McGinnis and colleagues, roughly 60% of early deaths are attributable to social circumstances, environmental exposures, or behavioral patterns.19 These findings suggest a wealth of opportunities for population health interventions targeting modifiable determinants of health. With this in mind, an important aspect of the strategy is engagement with “Bold Goal” communities. These are key metropolitan areas in which Humana partners with community leaders to provide interventions addressing chronic conditions, as well as social and environmental factors, of particular relevance to those communities. In each Bold Goal community, activities are planned and overseen by a Board of Directors made up of Humana senior leadership and a Health Advisory Board comprising community nonprofit, government, physician, and business stakeholders. These localized efforts provide rich opportunities to learn as we go how best to pursue population health. In 2016 Humana additionally began to refine the Bold Goal strategy by focusing on specific SDOH such as food insecurity and social isolation, not only in the Bold Goal markets, but in its broader populations as well.
With the foundational work completed and having started interventions across the enterprise, Humana is poised to expand its vision. The purpose of this paper is to 1) present the methods for measuring year-over-year population-level trends in Healthy Days and early results, 2) describe how the work identifying associations between SDOH and Healthy Days is influencing company strategy, and 3) illustrate community engagement through 2 case examples: San Antonio, Texas and Knoxville, Tennessee.
Bold Goal Tracking
The evaluation of a 20% reduction in mean unhealthy days required generating a population-level estimate in the baseline year (2015). Subsequent population-level tracking is achieved through the continuation of annual cross-sectional sample surveys of Humana members who are invited to participate in a Healthy Days survey using interactive voice response (IVR) telephone calls between June and December of each year. The chosen methods reflect the invaluable guidance Humana received from outside collaborators. Humana has benefited from experts at the CDC when planning its annual Healthy Days survey. The incorporation of SDOH into the Bold Goal strategies has been informed by collaboration with the Robert Wood Johnson Foundation. Lastly, Humana has learned from HRQOL researchers at Columbia University who have done work using the Healthy Days survey module.20,21
The annual cross-sectional surveys are conducted with stratified random sampling according to various combinations of geographic location and type of plan (eg, San Antonio-Medicare, Knoxville-Commercial Small Group). Where possible, the sample size for each stratum (location–plan community) is determined by an expected response rate and the sample size needed for detection of a statistically significant 5% reduction in mean unhealthy days. This allows for the measurement of progress in specific communities where substantial intervention investments are being made. The sampling frame in each year remains consistent in order to make each year's results comparable to those of the baseline year.
To ensure that the profile of respondents to the annual Healthy Days survey matches that of the target sampling frame (persons enrolled with Humana as of September 30th in the year of the survey), respondent data are weighted in 2 ways. The data scientists first adjust for the stratified sampling design because the size of each sample may not reflect the proportion of the total Humana population represented by that community. Data are additionally weighted using methods22 designed to account for differences between respondents and nonrespondents in age, sex, and the presence of 5 diagnosed conditions: coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, diabetes, and hypertension. Chronic diseases are identified using International Classification of Diseases, Ninth Revision (ICD-9) and ICD-10 codes obtained from claims. Once data are weighted, comparing Healthy Days survey responses between years requires attention to shifts in the demographic mix of each year's sampling frame. In order to account for these temporal changes, a regression-based standardization23 is performed each year to assure that the distribution of characteristics in the current sampling frame is comparable to the 2015 distribution. The factors included in the regression model are age, sex, low-income status (defined as dual Medicare and Medicaid eligibility for Medicare enrollees, and subsidy recipients for commercial individual enrollees), CMS Medicare Region, type of plan, all 2-way interactions of these factors, and where appropriate the interaction between age, sex, and plan type.
First-Year Results
Because a standard approach to annual tracking began in 2015, year 2016 presented the first opportunity to assess progress toward the Bold Goal. Survey response rates to date have been 22.3% (2015) and 21.7% (2016). Particularly for the first year of analysis, one would expect to see the most progress in established Bold Goal communities. As reported in the 2017 Bold Goal Progress Report,24 across the 7 Phase 1 Bold Goal communities, mean unhealthy days declined from 10.98 in 2015 to 10.64 in 2016, which represented a 3.1% relative, or 0.34 absolute, decline. This compares with a 0.17 absolute unhealthy days decline in the Humana national population overall. Results both for the San Antonio area, the community in which Humana has been involved the longest, and for Knoxville, one of the newer areas of engagement, showed significant decreases in unhealthy days. These results are encouraging, and Humana expects declines to accelerate over time as it launches and scales initiatives in Bold Goal communities.
Key Relationships Between SDOH and Unhealthy Days
Beyond 2016, progress results will reflect explicit efforts to address SDOH. It is known that health is multifaceted and as defined by the World Health Organization represents not only the absence of disease but also the state of physical, mental, and social well-being.25 It is important to recognize that nearly 20% of early deaths are attributed to social circumstances and environmental exposures.19 Similarly, a recent study of the geographic disparities in life expectancy among US counties found a difference of 20.1 years between the lowest and highest counties and estimated that as much as 60% of this variability may be attributable to socioeconomic and race/ethnicity factors.26 Other work has shown a 2.1-year reduction in life expectancy associated with low socioeconomic status, after adjusting for health risk factors.27 These and other nonmedical factors are collectively referred to as SDOH and are defined as “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”28
Jia et al studied the BRFSS data between 1999 and 2001 and found strong correlations between lower county-level socioeconomic status and higher numbers of reported Unhealthy Days.20 In 2010 the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute collaborated to create the County Health Ranking & Roadmaps program. This program tracks, at the county level, a broad set of health factors as well as health outcomes in all 50 states. These measures include factors such as health behaviors, clinical care, social/economic factors, and environmental factors, as well as morbidity and mortality. A recent review of County Health Rankings data for the years 2010–2013 estimated that social and economic factors accounted for 45.6% of health outcomes and that health behaviors, clinical care, and the physical environment accounted for 28.9%, 17.2%, and 8.3% respectively.
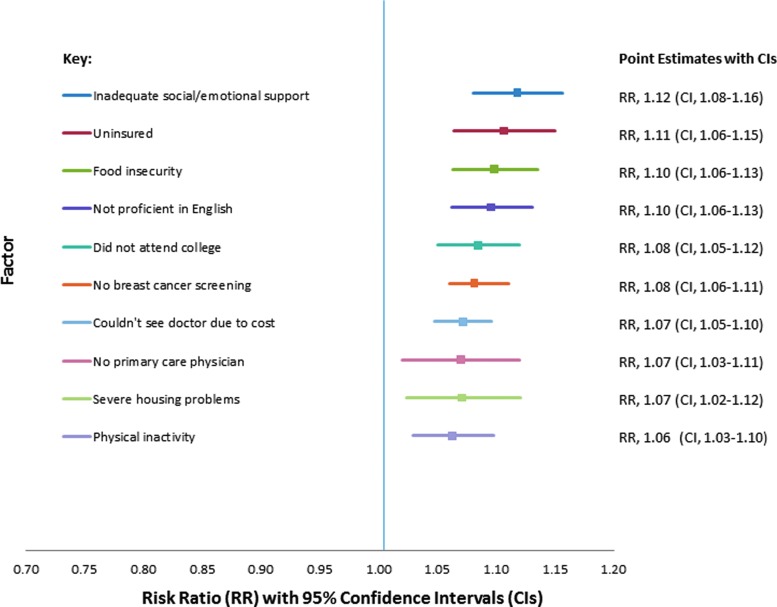
Considering these findings and in an effort to refine its Bold Goal strategy, Humana investigated the relationship between the Healthy Days instrument and SDOH in its Medicare population. Using the data from Humana member Healthy Days surveys and SDOH data derived from the 2014 County Health Rankings Report, age- and sex-adjusted multivariate logistic regression was performed to calculate the association between unhealthy days and each of 31 selected SDOH. In keeping with published studies using Healthy Days as an outcome measure,15,17 the cutoff point for the binary Healthy Days variable was 14, where ≥14 unhealthy days signified poor health status. The distribution across counties of various SDOH measures was determined so that values could be standardized and expressed as percentiles. The study team then computed the potential magnitude of change in unhealthy days for an improvement in each SDOH of interest from the 25th to 75th percentile.29 Figure 1 shows the 10 SDOH with the strongest associations with unhealthy days. Inadequate social/emotional support (10% greater risk of ≥14 unhealthy days) and food insecurity (12% greater risk of ≥14 unhealthy days) were at or close to the top of the list. Corresponding risk ratios were 1.10 (95% CI, 1.06–1.13) for food insecurity and 1.12 (95% CI, 1.08–1.16) for inadequate social/emotional support.
FIG. 1.
Top 10 social determinants of health by association with unhealthy days.
Definitions of Factors
Inadequate social/emotional support: Percent of adults without social/emotional support.
Uninsured: Percent of population <65 years without insurance.
Food insecurity: Percent of population reported food insecurity.
Not proficient in English: Percent of population reported not proficient in English.
*Did not attend college: Percent adults aged 25–44 years with no post-secondary education.
*No breast cancer screening: Percent of female Medicare enrollees who did not receive mammography screening.
Couldn't see doctors because of cost: Percent of population who reported they could not see doctors because of costs.
*No primary care physician (PCP): 1- [(Number of PCPs/population)*100,000].
Severe housing problem: Percentage of households with at least 1 of 4 housing problems: overcrowding, high housing costs, or lack of kitchen or plumbing facilities.
Physical inactivity: Percent of adults aged 20 years and older reporting no leisure-time physical activity.
*Robert Wood Johnson Foundation definitions and corresponding calculations were inverted so that the direction of all results can be interpreted in the same way.
Source: Robert Wood Johnson Foundation County Health Rankings Key Findings 2014.
The linking of the County Health Ranking & Roadmaps data to Healthy Days survey responses is consistent with research showing associations between individual-level SDOH and other HRQOL scales.30–34 The selection of social isolation and food insecurity findings is further supported by studies showing associations between these 2 factors and clinical outcomes. Social isolation has been shown to be associated with increased risk of heart disease, stroke, and even mortality.35,36 Food insecurity has been shown to be associated with a multitude of chronic diseases including diabetes, mental health status, and cardiovascular risk factors.37–39 As Humana develops new community-based interventions to further the Bold Goal, it is intentionally pursuing population-based assessments of social isolation and food insecurity, and is developing programs that directly address these upstream determinants of health.
Evolving Plans for Reducing Unhealthy Days: Two Case Examples
San Antonio
Work began in 2014 in the first Bold Goal community – San Antonio, Texas, a community in which Humana has operated for more than 35 years and insures more than 500,000 residents. The opportunity to improve health in San Antonio was great. A 2014 report of the health and fitness of 50 of the largest metropolitan areas in the United States ranked San Antonio forty-fifth, highlighting high rates of obesity (28.9%, vs. 27.6% national average) and diabetes (11.3%, vs. 9.7% national average).40 Further, Bexar County (San Antonio) was ranked as 69 out of 232 Texas counties by the Robert Wood Johnson Foundation 2014 Community Health Rankings. The quality of life ranking was far worse in the Community Health Rankings, 120 out of 232 counties, with 17% of the population reporting poor or fair health.
The goal of the work in San Antonio was to convene clinical and community leaders to work together to improve the health of the San Antonio community. Although the written goal was simple, developing a framework to accomplish the goal was complex. The first step was to identify leaders and programs within the community with a shared vision through a series of focus groups and community gatherings. Early partners in this work included SA 2020, the Bexar County Medical Society, the San Antonio Food Bank, and the Mayor's Fitness Council. These initial meetings culminated in a large-scale kick-off event – the first Clinical Town Hall. The first town hall was a 2-day event including panel discussions and presentations from clinical and community leaders, with more than 100 participants. A key finding of the event was that San Antonio was rich with programs and resources to improve health, yet these groups had not convened collaboratively. Following this initial town hall, a structure was developed to advance the work. An advisory board of 45 community members, the San Antonio Health Advisory Board, was formed and cochaired by 2 physician leaders – one from Humana and the other from a local organization, USAA. The Advisory Board meets quarterly and has created a number of subcommittees to address specific health barriers and projects, such as diabetes, nutrition, community resource connectivity, and measurement of progress.
The San Antonio Health Advisory Board decided to focus on using the collaborative to elevate and advance projects that are in progress rather than start new ones. In that spirit, the idea of the Diabetes Resources Guide was born. Through the Clinical Town Hall, it became apparent that there were a wide range of free or low-cost resources available to support various aspects of having prediabetes or living with diabetes, including education, nutrition, exercise, goal setting, and symptom management. These resources also covered the different clinical types of diabetes (gestational, type 1, type 2), as well as prediabetes. Despite the volume of resources, leaders of many of the programs were unaware of other related programs, and clinicians or other sources of referrals had no central reference to identify the available programs to meet the needs of a given individual. With support from the local American Diabetes Association, the Diabetes Resources Guide has been developed as an interactive website that aids physicians and patients in selecting the most appropriate diabetes programs.41
In addition to clinical conditions, SDOH were identified as barriers to health in San Antonio. In 2014, food insecurity affected 13% of people in Bexar County, and 12% had limited access to healthy foods.42 Among several projects, the San Antonio Food Bank partnered with a primary care physician group, MCCI Medical Group. This partnership provides food to the San Antonio community and leverages MCCI's Activity Centers (free-standing centers located adjacent to MCCI clinics) as community-wide food distribution sites for the project. This partnership serves about 300 people monthly and underscores the relationship between food and health.
The Resources Guide and community-wide food distribution site are just 2 examples of many collaboration projects, but they are indicators that health is improving. Between 2015 and 2016, unhealthy days dropped by 9.0% (−0.95 absolute) from a mean 10.52 to 9.57 unhealthy days. Both physically and mentally unhealthy days dropped. As the inaugural Bold Goal Community, San Antonio has been a learning laboratory to inform work in additional Bold Goal communities, and the work continues. In 2017, the fourth annual Clinical Town Hall will be held.
Knoxville
The Bold Goal project was launched in Knoxville, Tennessee in the fall of 2015, where, as in San Antonio, the need to improve health was high. According to the Knox County Health Department, the prevalence of chronic disease has been rising steadily over the past decade, with 2015 rates of diabetes reaching 10.5%, obesity 28.6%, and hypertension 33.4%. Thus, it is not surprising that 17% of the population rate their health as poor or fair. SDOH adversely impacting health also are highly prevalent in Knoxville, with 16% of residents living below the poverty level, 10% without a high school diploma, and 14.0% of the population, or 62,050 people, considered food insecure.
The framework for executing the Bold Goal work in Knoxville followed the model developed in San Antonio, with the convening of a Clinical Town Hall, formation of a Health Advisory Board, and use of subcommittees to focus on specific topics and launch related initiatives. The Knoxville Board of Directors prioritized 3 health conditions: diabetes, behavioral health, and heart failure. The rising prevalence and impact of these chronic conditions is a common scenario in multiple Bold Goal communities. Knoxville also identified 4 barriers to health: access to mental health providers, awareness of resources, nutrition literacy, and financial trade-offs. Collaborative projects focused on these priorities are ongoing and include healthy cooking demonstrations in multiple locations such as faith-based organizations, the Boys and Girls Clubs of the Tennessee Valley, senior living centers, and low-income apartment complexes; multiple diabetes education classes in different settings using curricula from the Stanford Model and the Diabetes Prevention Program; and a mobile health pilot designed to test if mobile health outreach can improve the health of people who do not have an existing relationship with a primary health care provider.
Since the inception of the Bold Goal work in San Antonio, the framework for collaboration grew to include the concept of a signature partner. A Signature Community Partner is a local or national organization that provides resources or services aimed at addressing the collaboration's priority health conditions and barriers. In Knoxville, the signature partner is Walgreens. Walgreens is a fitting partner, not only because the company aims to improve health, but because pharmacies are one of the most common places where patients interact with the health system. In Walgreens pharmacies, pharmacists conduct comprehensive medication reviews with patients who are taking multiple medications. During these reviews, pharmacists identify medication-related problems and counsel patients on the importance of taking their medications correctly, which is shown to improve chronic diseases such as diabetes. The collaboration with Walgreens in Knoxville began in late 2016, and the completion rate of medication reviews for eligible patients increased 5-fold from the prior quarter.
Another key theme of the Bold Goal work that had emerged over time was the importance of activating Humana employees in the Bold Goal communities. Engaging associates not only makes the company healthier, but it can advance the collaborative community work. In the Knoxville area, there are more than 350,000 people with Humana insurance supported by more than 300 local Humana associates. These associates were struck by the level of poverty in their own community. In response to that concern, the company provided a way for associates to experience the realities of poverty through a poverty simulator. A poverty simulator is a guided role-playing experience. Plans also are under way for groups represented in the Clinical Town Halls and on the Health Advisory Board to participate. Associates have since had multiple opportunities to volunteer in support of addressing food insecurity.
Relative to San Antonio, the work in Knoxville is still in its infancy. However, there are signs that health is improving. Between 2015 and 2016, mean unhealthy days declined by 4.8% (−0.61 absolute), representing declines in both physically and mentally unhealthy days. Because self-reported unhealthy days are correlated with disease prevalence, this may be an indicator that health in Knoxville is beginning to improve.
Conclusion
Combining health care data (ie, medical and pharmacy claims data, labs) with other population and social determinant data sources (eg, BRFSS, Robert Wood Johnson Foundation Country Health Ranking Report) creates a more complete picture of what is influencing health in a community. Sharing these insights with cross-sector stakeholders, and then convening and collaborating with them, creates the opportunity for collective impact. Humana has much to learn with respect to effective interventions that make lasting changes in HRQOL as well as chronic disease, and will continue to learn from data, research, initiatives, and partnerships. However, Humana is encouraged by the early results of its own healthier by 2020 Bold Goal initiative and is committed to continued refinement of its strategies, taking into account the social and environmental factors that affect health status as well as quality of health care.
Acknowledgments
The authors wish to thank Laura Happe, PharmD, and Teresa Rogstad, MPH, for their editorial and medical writing assistance.
Author Disclosure Statement
The authors declared the following conflicts of interest: The authors are all full-time employees of Humana Inc.; some authors own Humana stock. The authors did not receive any external funding for the research, authorship, and/or publication of this article.
References
- 1.HealthyPeople.gov About Healthy People. 2017. https://www.healthypeople.gov/2020/About-Healthy-People Accessed August12, 2017
- 2.Nevada County Department of Public Health. 2014 Nevada County Health Status Report. 2014. https://www.mynevadacounty.com/nc/hhsa/ph Accessed August12, 2017
- 3.Healthy Alaskans 2020. 2016 Healthy Alaskans 2020 Scorecard shows project is on track to reach health-improvement goals. 2016. http://dhss.alaska.gov/news/documents/press/2016/updated_ha2020scorecard_090816.pdf Accessed August12, 2017
- 4.North Carolina Health and Humana Services. Healthy North Carolina 2020: A Better State of Health. 2011. http://publichealth.nc.gov/hnc2020 Accessed August12, 2017
- 5.Wisconsin Deparment of Health. Healthiest Wisconsin 2020–Background and References. 2016. https://www.dhs.wisconsin.gov/hw2020/background.htm Accessed August12, 2017
- 6.Maclean JC, Webber D. Jobs and Behavioral Health: More than Just a Paycheck. 2013. www.scattergoodfoundation.org/activity/general/jobs-and-behavioral-health-more-just-pay-check#.WUpsrYeGOmQ Accessed August12, 2017
- 7.National Institute for Fitness and Sport. Worksite Wellness and the Healthy People 2020 Goals. 2011. http://wellness.nifs.org/blog/bid/48670 Accessed August12, 2017
- 8.Doherty TM. Leading health organizations and patient groups share best practices for osteoporosis and fracture prevention. November 15, 2011. https://centerfortotalhealth.org Accessed August12, 2017
- 9.Slabaugh SL, Shah M, Zack M, et al. . Leveraging health-related quality of life in population health management: the case for healthy days. Popul Health Manag 2016;20:13–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HealthyPeople.gov Foundation Health Measures. General Health Measures. 2017. https://www.healthypeople.gov/2020/about/foundation-health-measures Accessed August12, 2017
- 11.Brown DW, Pleasants R, Ohar JA, et al. . Health-related quality of life and chronic obstructive pulmonary disease in North Carolina. N Am J Med Sci 2010;2:60–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dominick KL, Ahern FM, Gold CH, Heller DA. Health-related quality of life among older adults with arthritis. Health Qual Life Outcomes 2004;2:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ford ES, Mannino DM, Homa DM, et al. . Self-reported asthma and health-related quality of life: findings from the behavioral risk factor surveillance system. Chest 2003;123:119–127 [DOI] [PubMed] [Google Scholar]
- 14.Smith DW. The population perspective on quality of life among Americans with diabetes. Qual Life Res 2004;13:1391–1400 [DOI] [PubMed] [Google Scholar]
- 15.Hart PD. Meeting recommended levels of physical activity and health-related quality of life in rural adults. J Lifestyle Med 2016;6:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drzayich Jankus D, Hopson S, Khoury R, et al. . Is there a relationship between self-reported healthy days and comorbidity medication adherence among oncology patients? J Clin Oncol 2016;34(7 suppl):189 [Google Scholar]
- 17.Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, Mokdad AH. Self-reported general health, physical distress, mental distress, and activity limitation by US county, 1995–2012. Popul Health Metr 2017;15:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cordier T, Slabaugh SL, Havens E, et al. . A health plan's investigation of healthy days and chronic conditions. Am J Manag Care 2017;23:e323–e330 [PubMed] [Google Scholar]
- 19.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Affairs (Millwood) 2002;21:78–93 [DOI] [PubMed] [Google Scholar]
- 20.Jia H, Moriarty DG, Kanarek N. County-level social environment determinants of health-related quality of life among US adults: a multilevel analysis. J Community Health 2009;34:430–439 [DOI] [PubMed] [Google Scholar]
- 21.Jia H, Zack MM, Moriarty DG, Fryback DG. Predicting the EuroQol Group's EQ-5D index from CDC's “healthy days” in a US sample. Med Decis Making 2011;31:174–185 [DOI] [PubMed] [Google Scholar]
- 22.Fienberg S. An iterative procedure for estimation in contingency tables. Ann Math Stat 1970;41:907–917 [Google Scholar]
- 23.Roalfe AK, Holder RL, Wilson S. Standardisation of rates using logistic regression: a comparison with the direct method. BMC Health Serv Res 2008;8:275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Humana. 2017. Progress Report: Bold Goal. http://populationhealth.humana.com Accessed August12, 2017
- 25.World Health Organization. Frequently asked questions. What is the WHO definition of health? 2017. www.who.int/suggestions/faq/en Accessed August12, 2017
- 26.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. . Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med 2017;177:1003–1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stringhini S, Carmeli C, Jokela M, et al. . Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet 2017;389:1229–1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.HealthyPeople.gov 2010 Topics & Objectives. Social Determinants of Health. https://www.healthypeople.gov/2020/topics-objectives Accessed August12, 2017
- 29.Song Y, Cordier T, Cambon J, et al. . Association between social determinants of health and health-related quality of life in a Medicare Advantage population. Presented at: American Public Health Assciation Annual Meeting & Expo; November4–8, 2017; Atlanta, GA [Google Scholar]
- 30.Brennan DS, Spencer AJ. Health-related quality of life and income-related social mobility in young adults. Health Qual Life Outcomes 2014;12:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gany F, Leng J, Ramirez J, et al. . Health-related quality of life of food-insecure ethnic minority patients with cancer. J Oncol Prac 2015;11:396–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Habib AR, Manji J, Wilcox PG, Javer AR, Buxton JA, Quon BS. A systematic review of factors associated with health-related quality of life in adolescents and adults with cystic fibrosis. Ann Am Thorac Soc 2015;12:420–428 [DOI] [PubMed] [Google Scholar]
- 33.Mielck A, Vogelmann M, Leidl R. Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health Qual Life Outcomes 2014;12:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lubetkin EI, Jia H, Franks P, Gold MR. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: examining the EQ-5D in the U.S. general population. Qual Life Res 2005;14:2187–2196 [DOI] [PubMed] [Google Scholar]
- 35.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A 2013;110:5797–5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016;102:1009–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med 2007;22:1018–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2010;140:304–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones AD. Food insecurity and mental health status: a global analysis of 149 countries. Am J Prev Med 2017;53:264–273 [DOI] [PubMed] [Google Scholar]
- 40.American College of Sports Medicine. American Fitness Index. Health and Community Fitness Status of the 50 Largest Metropolitan Areas. 2014. Edition. www.americanfitnessindex.org Accessed August12, 2017
- 41.Diabetes Resources Guide. San Antonio. 2017. www.diabetesresourcesguide.com Accessed August12, 2017
- 42.Robert Wood Johnson Foundation. County Health Rankings & Roadmaps. Health Rankings. Find your State or County. 2017. www.countyhealthrankings.org Accessed August12, 2017