Abstract
Background
UV exposure may not equally impact melanoma development in different sexes and ages. Whether and how these factors interact with each other in melanoma risk is unknown.
Objective
This study attempts to estimate interactions among UVI, sex and age in melanoma risk.
Methods
Melanoma incidence data was collected from 42 cancer registries. Geographical UV index (UVI) was collected from local satellite stations. Negative binomial regression models were used to estimate the impact of each risk factor and their interactions.
Results
Sex, UVI and age, as well as interactions between any two of these factors were significantly associated with melanoma risk. In younger age groups, the female sex is an independent risk factor for melanoma that is not impacted by ambient UV exposure. In older age groups, however, the female sex interacts with UV exposure as a risk factor, exhibiting a protective effect. The switching age category is 45–49, which correlates with dramatic hormonal changes.
Limitations
the interaction between sex and UVI is measured at an ecological level.
Conclusion
The interaction between sex and UVI is age-dependent. The female sex is an independent risk factor for early onset melanoma, but the female sex also protects against UV-associated melanoma in older age groups.
Keywords: melanoma, UV, UVI, latitude, gender, sex, epidemiology
Introduction
Melanoma is the number one cause of death in skin cancer 1, 2, and is one of the most commonly diagnosed cancers in adolescence and young adults (AYA), especially in young women during their reproductive age 3. While most other cancer types have shown a decreasing trend of incidence rates over the past 24 years, melanoma remains one of the common cancer types with increasing trend4; and the epidemiological reasons are mostly attributed to ultraviolet radiation (UVR), including solar UV and indoor tanning bed 5, 6.
Risks for AYA melanoma include white ethnicity, female gender and environmental UV radiation 7. Melanoma incidence rates increase with age for both genders but with different patterns 8, 9: young women (<45 year old) have higher incidence rates than young men, but the trend reverses at older age – older women have lower incidence rates than older men 9. It has been known for over 30 years that the melanoma incidence and mortality is higher in women than that in men at younger ages 10. Most epidemiological studies attributed this cause to life style and tanning bed use for younger women 11, 12, i.e., younger women are less covered under the sun and use tanning beds more often 12, 13, hence they are more exposed to UVR. However, it was reported in a meta-analysis that in Europe tanning bed use only counted for 5.4% of all melanoma cases 14. Therefore the question remains as to whether UVR can fully account for the gender difference observed in AYA melanoma, or alternatively, whether melanomas from all ages are equally affected by UVR.
Our previous studies strongly suggested negative answers to the above questions. We first described a unique female to male rate ratio change over age in melanoma which showed a peak difference at reproductive age 9. Non-melanoma skin cancer, which was also caused by UV exposure, did not exhibit such age-dependent rate ratio difference between sexes 9. More importantly, this rate ratio difference was observed in all ethnicities including African American group whose skin are well protected from UVR9. Further regression analysis on sex-specific age-standardized rates and daily average geographical UVI revealed that melanoma incidence rates in men showed a significant association with geographical UVI, but there was no such association in women 15. These findings are very intriguing; they strongly suggest an independent role of sex, which has always been linked to differential UV behavior between sexes. In this study we set out to examine whether we can separate the role between UVR, age and sex, and explore potential interactions among these factors in melanoma risk.
Materials and Methods
Registry selection and melanoma classification
For melanoma cases, tumor classification was based on the standard of the International Classification of Diseases for Oncology, ICD-O-3, with code C43. In order to obtain a relatively homogeneous ethnic background, registries from northern Europe, United States and Australia were selected based on ethnic information. For northern Europe, countries with at least 50% light eye color of population were selected 16. This excludes most of southern European countries even though they are Caucasians. Belgium was excluded because data was not available for a 10 year period of time. For the United States, race information is available so only white race was included in all selected registries. For Australia, it is known that the Northern Territory contains a large indigenous population, therefore the Northern Territory was excluded. For all registries, the most recent 10 years of incidence rates (case and population numbers in each 5 year age categories) were collected based on the data availability (Table 1), either from 1998 to 2007 or from 2000 to 2009. For European countries, data was obtained from Eureg (part of International Agency for Research of Cancer, IARC) website (http://eco.iarc.fr/eureg/Default.aspx). For the United States, data was downloaded from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute via SEER*Stat software. For Australia registries, data was obtained from IARC CI5, volume X plus.
Table 1.
Cancer registry, years, rates and local UVI and latitude
| Country | Registry | Years | asr-M | asr-F | UVI | Latitude |
|---|---|---|---|---|---|---|
| Australia | Queensland | 1998–2007 | 60.7 | 43.9 | 9.4 | 20.9 |
| New South Wales | 1998–2007 | 44.6 | 30.2 | 7.2 | 33.9 | |
| Tasman | 1998–2007 | 37.5 | 34.9 | 5.6 | 41.4 | |
| Victoria | 1998–2007 | 32.9 | 26.5 | 6.3 | 37.5 | |
| South Australia | 1998–2007 | 32.6 | 26.5 | 7.0 | 30.0 | |
| West Australia | 1998–2007 | 49.3 | 33.8 | 7.7 | 27.7 | |
|
| ||||||
| Austria | Austria | 2000–2009 | 11.0 | 9.7 | 4.1 | 47.5 |
| Czech | Czech | 1998–2007 | 12.4 | 10.8 | 3.5 | 49.8 |
| Denmark | Denmark | 1998–2007 | 14.5 | 17.9 | 3.0 | 56.3 |
| Estonia | Estonia | 1998–2007 | 6.2 | 7.9 | 2.3 | 58.6 |
| Finland | Finland | 1998–2007 | 11.0 | 9.1 | 1.8 | 61.9 |
| France | Manche/Haut-Rhin | 2000–2009 | 12.8 | 13.8 | 3.8 | 47.9 |
| Iceland | Iceland | 1998–2007 | 11.4 | 20.2 | 1.9 | 65.0 |
| Ireland | Ireland | 2000–2009 | 11.0 | 14.0 | 3.0 | 53.4 |
| Netherland | Netherland | 1998–2007 | 13.1 | 16.8 | 3.2 | 52.1 |
| Norway | Norway | 1998–2007 | 16.6 | 17.5 | 1.9 | 60.5 |
| Sweden | Sweden | 2000–2009 | 15.5 | 15.9 | 2.2 | 60.1 |
| Switzerland | Zurich | 2000–2009 | 21.0 | 18.9 | 4.1 | 47.4 |
|
| ||||||
| Germany | Brandenburg | 2000–2009 | 8.2 | 7.9 | 3.1 | 52.0 |
| Mecklenburg | 2000–2009 | 8.1 | 8.3 | 2.8 | 53.6 | |
| Schleswig-Holstein | 2000–2009 | 14.3 | 16.4 | 2.8 | 54.2 | |
| Thuringen | 2000–2009 | 9.8 | 9.6 | 3.5 | 51.0 | |
|
| ||||||
| United Kingdom | East England | 2000–2009 | 10.1 | 11.0 | 3.0 | 52.2 |
| NW England | 2000–2009 | 8.7 | 11.4 | 2.2 | 52.4 | |
| Northern Ireland | 1998–2007 | 9.1 | 12.0 | 3.0 | 54.8 | |
| Scotland | 1998–2007 | 10.8 | 12.9 | 2.6 | 56.5 | |
| Wales | 1998–2007 | 9.8 | 10.8 | 3.0 | 52.1 | |
|
| ||||||
| United States | Atlanta | 2000–2009 | 37.7 | 26.3 | 6.7 | 33.7 |
| Greater Georgia | 2000–2009 | 24.5 | 17.2 | 6.7 | 32.2 | |
| Connecticut | 2000–2009 | 22.9 | 17.3 | 4.9 | 41.6 | |
| Detroit | 2000–2009 | 19.7 | 16.4 | 4.9 | 42.3 | |
| Hawaii | 2000–2009 | 61.2 | 39.3 | 10.5 | 19.9 | |
| Iowa | 2000–2009 | 18.3 | 15.8 | 4.9 | 41.9 | |
| Kentucky | 2000–2009 | 22.1 | 16.3 | 5.7 | 37.8 | |
| Los Angeles | 2000–2009 | 18.4 | 10.8 | 6.9 | 34.1 | |
| Louisiana | 2000–2009 | 17.4 | 11.4 | 8.9 | 31.0 | |
| New Mexico | 2000–2009 | 18.6 | 11.9 | 6.7 | 34.5 | |
| New Jersey | 2000–2009 | 23.5 | 16.9 | 5.6 | 40.1 | |
| San Francisco | 2000–2009 | 26.8 | 18.2 | 5.7 | 37.8 | |
| San Jose | 2000–2009 | 23.3 | 16.3 | 5.7 | 37.8 | |
| Seattle | 2000–2009 | 27.5 | 23.6 | 4.3 | 47.6 | |
| Utah | 2000–2009 | 29.5 | 19.4 | 6.1 | 39.3 | |
asr-M: age-standardized rate for males; asr-F: age-standardized rate for females
Geographical UVI data and local latitude
The local UV indices were collected as described in our previous publication 15. Briefly, UV indices were calculated from data collected by local satellite stations. The scale of UVI is proportional to the intensity of erythema-causing UV doses on the earth surface any day at noon 17. Daily UVI were collected from July 1, 2002, the earliest time when the data was available, to June 30, 2014 when data was first collected for this study. Average daily UVI for this period was used for analysis. The latitude value was that of roughly the central latitude of the registry area. More details are described in Supplemental Method.
Statistical methods
A negative binomial regression model was used to estimate association of age, sex and UVI with melanoma risk because, although the count data (case numbers) fit Poisson distribution, the data was over dispersed (p < 0.0001). In our model assessment, the Pearson Chi-Square values and degrees of freedom were used to estimate whether the data was over-dispersed when modeled with a negative binomial distribution. The time period was the same for all registries (10 years), but population size varied, therefore log-transformed population was used as an offset. A natural log link was used for a log linear model. Comparison between models was made via log likelihood ratios and chi square statistics.
Results
All three factors and interactions between each two contribute significantly to melanoma risk
Table 1 lists the registries and countries, years of data collection, age-standardized gender-specific melanoma incidence rates, geographical UVIs and latitudes. As described in Supplemental Methods, negative binomial regression was used to assess melanoma risk. In the base model (Model 1) which include three factors only, all three variables (age, sex and UVI) were significant contributors to melanoma risk (Table 2). Sequentially adding an interaction between UVI*sex, or UVI*age, or age*sex to base model, we generated Model 2, 3 and 4. Each interaction significantly improved the prediction of melanoma risk as judged by the significant p values for either the interaction, or the model comparison, or both (Table 2). Model 5 included all three possible 2×2 interactions, and again it is a significantly better model than Model 4. When latitude was used instead of UVI, the results were similar (Supplemental Table S1), all three variables and their interactions showed significant contributions to melanoma risk. Note that in all models, sex exhibited a negative coefficient, revealing that overall females showed a protective effect against melanoma risk as the regression models used male sex as a baseline.
Table 2.
Parameter estimate from different models using UVI
| Coefficient | Standard Error | Wald 95% Confidence Limits | Wald Chi-Square | Pr > ChiSq | p value for model comparison | |||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Intercept | −12.312 | 0.0754 | −12.4597 | −12.164 | 26640.5 | <.0001 | |
| uvi | 0.1673 | 0.0107 | 0.1463 | 0.1883 | 244.47 | <.0001 | ||
| sex | −0.1383 | 0.0475 | −0.2314 | −0.0452 | 8.48 | 0.0036 | ||
| age | 0.0631 | 0.0012 | 0.0607 | 0.0654 | 2724.68 | <.0001 | ||
| LL* | −8854.7 | NA | ||||||
|
| ||||||||
| Model 2 | Intercept | −12.1 | 0.0909 | −12.2779 | −11.922 | 17730.3 | <.0001 | |
| uvi | 0.1222 | 0.0148 | 0.0931 | 0.1513 | 67.79 | <.0001 | ||
| sex | −0.558 | 0.1103 | −0.7741 | −0.3418 | 25.59 | <.0001 | ||
| age | 0.063 | 0.0012 | 0.0606 | 0.0653 | 2753.02 | <.0001 | ||
| uvi* sex | 0.0892 | 0.0212 | 0.0477 | 0.1308 | 17.74 | <.0001 | ||
| LL | −8844.1 | < 0.0001 | ||||||
|
| ||||||||
| Model 3 | Intercept | −11.945 | 0.1384 | −12.2165 | −11.674 | 7448.36 | <.0001 | |
| uvi | 0.0898 | 0.0265 | 0.0377 | 0.1418 | 11.43 | 0.0007 | ||
| sex | −0.1398 | 0.0473 | −0.2325 | −0.0472 | 8.76 | 0.0031 | ||
| age | 0.0549 | 0.0028 | 0.0494 | 0.0605 | 378.59 | <.0001 | ||
| uvi* age | 0.0017 | 0.0005 | 0.0007 | 0.0028 | 9.98 | 0.0016 | ||
| LL | −8848.7 | 0.0005 | ||||||
|
| ||||||||
| Model 4 | Intercept | −11.761 | 0.0926 | −11.9425 | −11.58 | 16127.2 | <.0001 | |
| uvi | 0.1662 | 0.0103 | 0.146 | 0.1863 | 261.08 | <.0001 | ||
| sex | −1.1858 | 0.1131 | −1.4076 | −0.9641 | 109.84 | <.0001 | ||
| age | 0.0504 | 0.0016 | 0.0472 | 0.0537 | 937.02 | <.0001 | ||
| age* sex | 0.0232 | 0.0023 | 0.0187 | 0.0277 | 103 | <.0001 | ||
| LL | −8795.6 | < 0.0001 | ||||||
|
| ||||||||
| Model 5 | Intercept | −11.313 | 0.1522 | −11.6114 | −11.015 | 5528.3 | <.0001 | |
| uvi | 0.0689 | 0.0275 | 0.015 | 0.1227 | 6.29 | 0.0122 | ||
| sex | −1.5477 | 0.1481 | −1.8381 | −1.2574 | 109.15 | <.0001 | ||
| age | 0.0447 | 0.0029 | 0.0389 | 0.0504 | 231.08 | <.0001 | ||
| uvi* sex | 0.0808 | 0.0204 | 0.0409 | 0.1207 | 15.76 | <.0001 | ||
| uvi* age | 0.0013 | 0.0005 | 0.0002 | 0.0023 | 5.78 | 0.0163 | ||
| age* sex | 0.0228 | 0.0023 | 0.0183 | 0.0272 | 100.78 | <.0001 | ||
| LL | −8782.7 | < 0.0001 | ||||||
LL, log likelihood value
The female sex is an independent risk factor for melanoma diagnosed at younger age
The interaction between UVI and sex was not well documented. We next examined UVI*sex interaction using the same negative binomial model for each age category. As shown in Table 3, both models suggested that UVI was significantly associated with melanoma risk across all age categories except for the very young age (Agecat 1).
Table 3.
UVI, sex and UVI-sex interaction in different age strata
| Model A (UVI, Sex) | Model B (UVI, Sex, UVI*Sex) | Model Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Agecat | age | LL | p_uvi | p_sex | LL | p_uvi | p_sex | p_uvi*sex | LLR | p_model |
| 1 | 0–4 | −91.25 | 0.1418 | 0.19 | −91.25 | 0.281 | 0.606 | 0.9997 | 0.000 | 1.0000 |
| 2 | 5–9 | −122.19 | 0.0075 | 0.0099 | −121.49 | 0.0048 | 0.9529 | 0.2477 | 1.391 | 0.2380 |
| 3 | 10–14 | −187.39 | <.0001 | 0.2065 | −187.24 | 0.0042 | 0.3325 | 0.6093 | 0.302 | 0.5820 |
|
| ||||||||||
| 4 | 15–19 | −328.50 | <.0001 | 0.0019 | −325.82 | 0.0055 | 0.001 | 0.0304 | 5.374 | 0.0204 |
|
| ||||||||||
| 5 | 20–24 | −389.39 | <.0001 | <.0001 | −387.88 | 0.0008 | <.0001 | 0.0941 | 3.013 | 0.0826 |
| 6 | 25–29 | −441.87 | <.0001 | <.0001 | −440.45 | 0.0055 | 0.001 | 0.1074 | 2.848 | 0.0915 |
| 7 | 30–34 | −464.84 | <.0001 | <.0001 | −463.72 | 0.0009 | 0.0002 | 0.1505 | 2.243 | 0.1342 |
| 8 | 35–39 | −480.52 | <.0001 | <.0001 | −478.63 | <.0001 | <.0001 | 0.0597 | 3.785 | 0.0517 |
| 9 | 40–44 | −497.01 | <.0001 | 0.0002 | −496.04 | <.0001 | 0.0056 | 0.177 | 1.936 | 0.1641 |
|
| ||||||||||
| 10 | 45–49 | −512.55 | <.0001 | 0.063 | −510.28 | <.0001 | 0.0076 | 0.038 | 4.523 | 0.0334 |
|
| ||||||||||
| 11 | 50–54 | −520.73 | <.0001 | 0.8234 | −518.35 | <.0001 | 0.0643 | 0.0325 | 4.753 | 0.0292 |
| 12 | 55–59 | −529.92 | <.0001 | 0.0056 | −525.27 | <.0001 | 0.1288 | 0.0025 | 9.309 | 0.0023 |
| 13 | 60–64 | −528.54 | <.0001 | <.0001 | −525.71 | <.0001 | 0.8396 | 0.0185 | 5.674 | 0.0172 |
| 14 | 65–69 | −528.40 | <.0001 | <.0001 | −524.73 | <.0001 | 0.823 | 0.0073 | 7.339 | 0.0068 |
| 15 | 70–74 | −527.74 | <.0001 | <.0001 | −524.59 | <.0001 | 0.2765 | 0.0132 | 6.282 | 0.0122 |
| 16 | 75–79 | −523.19 | <.0001 | <.0001 | −518.21 | <.0001 | 0.5581 | 0.0016 | 9.967 | 0.0016 |
| 17 | 80–84 | −496.91 | <.0001 | <.0001 | −492.64 | <.0001 | 0.1813 | 0.0037 | 8.550 | 0.0035 |
| 18 | 85+ | −473.15 | <.0001 | <.0001 | −468.35 | <.0001 | 0.3123 | 0.0021 | 9.613 | 0.0019 |
LL: log likelihood; LLR: log likelihood ratio
Sex association with melanoma risk was age-dependent in both models, with different patterns. At very young age (0–14 years) the role of sex was uncertain as the p values ranged from non-significant to significant in model A for various age groups (Table 3). Adding UVI*sex interaction did not improve the model, meaning sex at these age groups did not modify UVI effect.
Age 15–19 group was a unique group in which sex was significantly associated with melanoma in both models; adding UVI*sex interaction significantly improved model (Table 3). The interaction between UVI and sex contributed significantly in determining melanoma risk as indicated by its significant p value (p=0.0304, Table 3). Therefore sex alone and the interaction between sex and UVI both are crucial.
For the 20–44 age group (the major reproductive age group), sex alone played a significant role in both models, while the UVI*sex interaction impact was not significant, as reflected by the p values for both the model comparison and for the interaction (Table 3).
Age 45–49 is a transition group, in which sex showed marginally significant impact in Model A (p=0.063) but shows significant impact in Model B (p=0.0076). The interaction between sex and UVI is also significant in this age group (p = 0.038). Therefore this age group and the age group 15–19 are the only two groups where both sex and UVI-sex interaction play significant roles in determining melanoma outcome. For both groups Model B is better than Model A, which emphasizes the importance of the interaction.
Sex does not play a role in the age 50–54 group in either model. This is consistent with our previous findings: the rate ratio between sexes for this age group is nearly 1.0 9. When the UVI and sex interaction is taken into consideration, sex is still not a significant contributor (p = 0.064), but the interaction is (p = 0.0325) (Table 3).
After age 54, Model B was significantly better than Model A; therefore sex alone is no longer a significant risk factor, even though we know that men’s rates are higher than women’s in these ages. In these older age groups, it is the interaction between sex and UVI that becomes important (Table 3).
Discussion and Conclusions
The role of sex in melanoma development was well known before, but it was mostly focused on the incidence rate difference at different ages. Here we reveal a significant interaction between sex and UVI which has been under-reported. What was more striking was that the interaction between sex and UVI was age-dependent. Before age 45 there is no significant interaction between sex and UVI; and sex and UVI independently contribute to melanoma risk. After age 49 the UVI and sex interaction played a significant role in melanoma risk, while sex itself was no longer significant. These results may suggest that, 1) sex plays an independent role in early onset melanoma development, and 2) sex exhibited a modification role on UVI impact in melanoma occurring later in life; specifically the female sex exhibited protective role against ambient UV exposure.
It is worth to note that the interaction was dependent on age, with 15–19 and 45–49 years as two switching ages. The age group 15–19 is the group just about to complete puberty changes and reach their life time high sexual hormonal levels 18, 19. Meanwhile this group is also reported to use tanning beds more often than other age groups 20. There may be a link between the tanning bed use and geographical UVI, so it seems multiple factors may be at play for this particular age group. The 15–19 and 45–49 age groups are also the exact ages when sex hormones exhibit the most dramatic changes in human life span 21. In particular, both estrogen and testosterone levels dramatically increase during the ages of 15–19 and they both dramatically decrease in the 45–49 year age group. This coincidence may suggest a link of these hormonal changes with melanoma risk, and these changes interact with geographical UVI to impact melanoma development. The role of hormonal impact is further supported by the non-significant role of sex for melanomas diagnosed before age 15 when the sexual biological difference is not as dramatic as later ages.
For melanomas diagnosed at older age, although sex no longer contributes independently to melanoma risk, the female sex shows a protective role against UV radiation. Without age stratification, the female sex exhibits an overall protective effect (Table 2). These results provide a possible explanation and validation of our previous observation that the incidence rates in women are not significantly associated with UVI in a linear model 15. In contrast, the incidence rates in men are significantly associated with ambient UVI and the association levels increase with age 15.
The limitation of this study is that the interaction between sex and UVI is based on geographical UV which may not reflect how much UV radiation a person receives, which is also difficult to separate from other environmental factors such as temperature and latitude. Confounding factors such as indoor tanning device use cannot be separated from the gender factor as females are more intent on having tanned skin either through tanning devices or sun bathing22. However, females also tend to use significantly more sunscreen 23–25. Furthermore, from our previous observation, it is known that young females did not show a particular higher incidence rate for non-melanoma skin cancer 9, which is also caused by UV radiation. Therefore it is highly likely that it is the female sex, and not their sun behavior, that contributes significantly to melanoma risk at young ages.
In summary our results suggest that the ambient UV exposure and sex each contributes to melanoma risk independently for those diagnosed at younger age (≤ 44 years old), that the ambient UV plays a significant role in melanoma risk for those diagnosed at older age (≥45 years old). However there is a significant interaction between sex and UVI for melanomas occurring at older age, manifesting as a protective role of female sex against UV-associated melanoma risk. The significance of these observations guarantees further investigations in the mechanism of sex difference and how this difference can be utilized in developing effective prevention strategies.
Supplementary Material
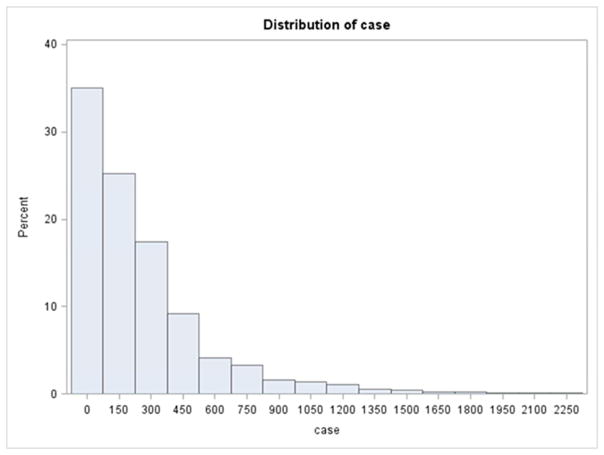
Figure 1.
Melanoma. Histogram of case numbers (numbers for each 5 year age category from each registry) distribution suggested a Poisson distribution.
Acknowledgments
This study is supported by NIH/NCI K07 grant (CA160756) to FLS.
Abbreviations and acronyms
- UVI
ultraviolet index
- ASR
age-standardized rate
Footnotes
Disclosure of Potential Conflicts of Interest:
The authors declare that they have no conflicts of interest.
Author’s contribution:
FLS conceived the idea, collected data, performed statistical analysis and wrote the manuscript. AZ provided statistical advice, examined statistical model and edited the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA dermatology. 2015;151:1081–6. doi: 10.1001/jamadermatol.2015.1187. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: a cancer journal for clinicians. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 3.Sender L, Zabokrtsky KB. Adolescent and young adult patients with cancer: a milieu of unique features. Nature reviews Clinical oncology. 2015;12:465–80. doi: 10.1038/nrclinonc.2015.92. [DOI] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA: a cancer journal for clinicians. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 5.Ting W, Schultz K, Cac NN, Peterson M, Walling HW. Tanning bed exposure increases the risk of malignant melanoma. International journal of dermatology. 2007;46:1253–7. doi: 10.1111/j.1365-4632.2007.03408.x. [DOI] [PubMed] [Google Scholar]
- 6.Vogel RI, Strayer LG, Engelman L, Nelson HH, Blaes AH, Anderson KE, et al. Sun Exposure and Protection Behaviors among Long-term Melanoma Survivors and Population Controls. Cancer Epidem Biomar. 2017;26:607–13. doi: 10.1158/1055-9965.EPI-16-0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strouse JJ, Fears TR, Tucker MA, Wayne AS. Pediatric melanoma: risk factor and survival analysis of the surveillance, epidemiology and end results database. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2005;23:4735–41. doi: 10.1200/JCO.2005.02.899. [DOI] [PubMed] [Google Scholar]
- 8.Purdue MP, Freeman LE, Anderson WF, Tucker MA. Recent trends in incidence of cutaneous melanoma among US Caucasian young adults. The Journal of investigative dermatology. 2008;128:2905–8. doi: 10.1038/jid.2008.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu F, Bessonova L, Taylor TH, Ziogas A, Meyskens FL, Jr, Anton-Culver H. A unique gender difference in early onset melanoma implies that in addition to ultraviolet light exposure other causative factors are important. Pigment cell & melanoma research. 2013;26:128–35. doi: 10.1111/pcmr.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JA, Storer BE. Excess of malignant melanomas in women in the British Isles. Lancet. 1980;2:1337–9. doi: 10.1016/s0140-6736(80)92401-0. [DOI] [PubMed] [Google Scholar]
- 11.Coelho SG, Hearing VJ. UVA tanning is involved in the increased incidence of skin cancers in fair-skinned young women. Pigment cell & melanoma research. 2009;23:57–63. doi: 10.1111/j.1755-148X.2009.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hausauer AK, Swetter SM, Cockburn MG, Clarke CA. Increases in melanoma among adolescent girls and young women in California: trends by socioeconomic status and UV radiation exposure. Archives of dermatology. 2011;147:783–9. doi: 10.1001/archdermatol.2011.44. [DOI] [PubMed] [Google Scholar]
- 13.Coelho SG, Hearing VJ. UVA tanning is involved in the increased incidence of skin cancers in fair-skinned young women. Pigment cell & melanoma research. 2010;23:57–63. doi: 10.1111/j.1755-148X.2009.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. Brit Med J. 2012:345. doi: 10.1136/bmj.e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu-Smith F, Farhat AM, Arce A, Ziogas A, Taylor T, Wang Z, et al. Sex differences in the association of cutaneous melanoma incidence rates and geographic ultraviolet light exposure. J American Academy of Dermatology. 2017;76:499–505. doi: 10.1016/j.jaad.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frost P. European hair and eye color - A case of frequency-dependent sexual selection? Evol Hum Behav. 2006;27:85–103. [Google Scholar]
- 17.Jegou F, Godin-Beekman S, Correa MP, Brogniez C, Auriol F, Peuch VH, et al. Validity of satellite measurements used for the monitoring of UV radiation risk on health. Atmos Chem Phys. 2011;11:13377–94. [Google Scholar]
- 18.Turtzo LC, McCullough LD. Sex-specific responses to stroke. Future neurology. 2010;5:47–59. doi: 10.2217/fnl.09.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoyt LT, Falconi AM. Puberty and perimenopause: reproductive transitions and their implications for women’s health. Soc Sci Med. 2015;132:103–12. doi: 10.1016/j.socscimed.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi K, Lazovich D, Southwell B, Forster J, Rolnick SJ, Jackson J. Prevalence and characteristics of indoor tanning use among men and women in the United States. Archives of dermatology. 2010;146:1356–61. doi: 10.1001/archdermatol.2010.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimitrakakis C, Bondy C. Androgens and the breast. Breast cancer research: BCR. 2009;11:212. doi: 10.1186/bcr2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hemrich A, Pawlow L, Pomerantz A, Segrist D. Current versus ideal skin tones and tanning behaviors in Caucasian college women. Journal of American college health: J of ACH. 2014;62:588–91. doi: 10.1080/07448481.2014.936440. [DOI] [PubMed] [Google Scholar]
- 23.Julian AK, Bethel JW, Odden MC, Thorburn S. Sex differences and risk behaviors among indoor tanners. Preventive medicine reports. 2016;3:283–7. doi: 10.1016/j.pmedr.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antonov D, Hollunder M, Schliemann S, Elsner P. Ultraviolet Exposure and Protection Behavior in the General Population: A Structured Interview Survey. Dermatology. 2016;232:11–6. doi: 10.1159/000440698. [DOI] [PubMed] [Google Scholar]
- 25.Pinault L, Fioletov V. Sun exposure, sun protection and sunburn among Canadian adults. Health reports. 2017;28:12–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.