Abstract
LC-MS/MS methods to measure prexasertib in mouse plasma and Ringer’s solution containing 0.5% BSA (Ringer’s/BSA) were developed and validated. Liquid-liquid extraction with tert-butyl methyl ether was used to extract prexasertib from mouse plasma and Ringer’s solution with 0.5% bovine serum albumin (Ringer’s/BSA). Reverse phase chromatography with gradient elution was performed to separate prexasertib from the endogenous interference in the matrix, followed by MS detection using positive ion MRM mode. The initial calibration curve for mouse plasma samples ranged from 1 to 500 ng/ml, and after validation of that curve and use in a preliminary study another calibration curve (0.2–200 ng/ml) was created to enable the quantitation of prexasertib at lower concentrations. The method described was precise and accurate with %CV in precision studies of ≤6.7% and accuracies within 95.0–110% of nominal target concentration across all concentrations tested for both matrices. This validated method was successfully applied in the analysis of prexasertib in mouse plasma and dialysate samples collected during a cerebral microdialysis study.
Keywords: Prexasertib, Chk1, LC-MS/MS, liquid-liquid extraction, microdialysis, Ringer’s solution
1. Introduction
Contemporary advances in integrated genomic technologies have increased our understanding of the molecular underpinnings driving tumor growth and proliferation. By identifying specific cellular mediators exerting influence on oncogenic pathways, these advances have led to a temporal shift in cancer drug development away from traditional cytotoxic agents towards new molecularly targeted therapies [1]. Prexasertib (LY2606368) is a small molecular inhibitor of checkpoint kinase 1 (CHK1), a key regulator of the S and G2/M checkpoints and DNA damage response [2], that is currently undergoing clinical evaluation (clinicaltrials.gov NCT02808650) for multiple pediatric malignancies, including neoplasms of the central nervous system (CNS).
For anticancer agents targeting CNS tumors, adequate penetration of the blood-brain barrier and the blood tumor barrier is an inherent prerequisite for clinical efficacy. To gain insight on the penetration of prexasertib in CNS tumors, we aimed to perform preclinical cerebral microdialysis studies in mice. However, due to the minute sample collection volumes associated with this technique, a highly sensitive and specific LC-MS/MS method was required for prexasertib in Ringer’s/bovine serum albumin 0.5% w/v solutions (Ringer’s/BSA). To estimate CNS tumor penetration, which is typically calculated as the ratio between tumor and plasma exposures [3], a method for quantification of prexasertib in mouse plasma was also required. To our knowledge, no LC-MS/MS method for prexasertib has been published. Here, we report the LC-MS/MS methods developed and validated by our laboratory for prexasertib in Ringer’s/BSA solution and mouse plasma that will be used to study the penetration of prexasertib in pediatric CNS tumors.
2. Materials and methods
2.1 Reagents and chemicals
5-({5-[2-(3-Aminopropoxy)-6-methoxyphenyl]-1H-pyrozol-3-yl}amino)pyrazine-2-carbonitrile methanesulfonate hydrate [prexasertib; Fig. 1a] and 5-({5-[2-(3-Aminopropoxy-1,1,3,3-d4)-6-methoxyphenyl]-1H-pyrozol-3-yl}amino)pyrazine-2- carbonitrile hydrochloride [prexasertib-d4, internal standard (ISTD); Fig. 1b] were supplied by Eli Lilly (Indianapolis, IN). Ammonium formate (for mass spectrometry, ≥99.0%) and albumin from bovine serum (lyophilized powder, ≥98% purity) were purchased from Millipore Sigma (St. Louis, MO). Formic acid (LC-MS/MS grade, 99.5% purity), acetonitrile (HPLC grade), and tert-butyl methyl ether (99% purity) were purchased from Fisher Scientific (Waltham, MA). Ringer’s Solution, an isotonic solution of sodium chloride, potassium chloride, calcium chloride, and sodium bicarbonate (to balance the pH) dissolved in water, was purchased from Frey Scientific (Nashua, NH). CD-1 mouse plasma with sodium heparin as anticoagulant was purchased from BioreclamationIVT (Baltimore, MD). All water was prepared using Millipore Q-advantage water purification system (Temecula, CA).
Fig. 1.

Structure of (A) prexasertib and (B) ISTD, prexasertib-d4.
2.2 Stock solutions
Prexasertib and prexasertib-d4 stock solutions (1.00 mg/ml) were prepared by dissolving the corresponding compound in methanol/water (50:50, v/v), respectively. Since prexasertib used in this study was the methanesulfonate hydrate, a correction factor 0.762 was applied to the weight of prexasertib and 1.00 mg/ml represented the concentration of prexasertib free base. No correction factor was applied to the concentration of ISTD.
The prexasertib working solutions were prepared by serial dilution of the stock solution with methanol/water (50:50, v/v). One set of prexasertib working solutions with the concentration range from 5 to 2500 ng/ml was prepared for the first plasma calibration curve and the QC samples. Another set of prexasertib working solutions with concentrations from 1–1000 ng/ml was prepared for the second plasma calibration curve and the corresponding QC samples. For the Ringer’s/BSA calibration curve and the related QC samples, a set of working solutions was prepared with concentrations ranging from 1–250 ng/ml.
The internal standard (ISTD) working solution was prepared by diluting the prexasertib-d4 stock solution with methanol/water (50:50, v/v) to 3000 ng/ml for plasma samples and 300 ng/ml for Ringer’s/BSA samples.
2.3 Calibration standards and quality controls
The calibration standards for the first plasma calibration curve ranged from 1–500 ng/ml and were prepared by spiking 5 μl of the prexasertib working solution using Eppendorf research® plus pipette into 25 μl blank mouse plasma to give concentrations of prexasertib at 1, 5, 10, 25, 100, 200, 300 and 500 ng/ml. The corresponding prexasertib plasma QC samples were prepared in a similar way at 3, 50, and 400 ng/ml, representing low QC (LQC), middle QC (MQC), and high QC (HQC), respectively. The calibration standards and the QC samples for the second prexasertib plasma calibration curve ranged from 0.2 to 200 ng/ml and were prepared similarly using the corresponding working solution to give concentrations of 0.2, 1, 2, 5, 25, 50, 100, 200 ng/ml for standards and 0.5, 10, 160 ng/ml for QC samples.
For the Ringer’s/BSA calibration curve, 5 μl of the corresponding prexasertib working solution was spiked into 25 μl Ringer’s solution with 0.5% w/v BSA to make the calibration standards at 0.2, 1, 2, 10, 15, 20, 30, and 50 ng/ml, and QC samples at 0.5, 5, and 40 ng/ml. Ringer’s solution with 0.5% w/v BSA was prepared by dissolving 50 mg BSA into 10 ml Ringer’s solution. All of the calibration standards and QC samples were further treated according to the below described sample preparation procedure.
2.4 Sample preparation
All samples were prepared for analysis using a liquid-liquid extraction (LLE) of 25 μl aliquots of either plasma or Ringer’s/BSA samples to which 6 μl of ISTD working solution were added. Five microliters of methanol/water (50:50, v/v) was added to the study samples for volume correction. The upper organic layer (~900 μl) was separated and blow-dried with nitrogen in the hood at room temperature for approximately 30 min to dryness. The dried residue was reconstituted with 50 μl acetonitrile/water/formic acid (10:90:0.1, v/v). For plasma samples using the calibration curve from 1–500 ng/ml, 10 μl was injected for LC-MS/MS analysis, whereas for plasma samples using the calibration curve from 0.2–200 ng/ml and Ringer’s/BSA samples, 20 μl was injected.
2.5 Chromatographic conditions
A Shimadzu HPLC system (Kyoto, Japan) consisted of an online degasser (DGU-14A), two pumps (LC-30 CE), an autosampler (SIL-30AC), and a controller (CBM-20A). The chromatographic separation was performed on a Luna C18 column (50×4.6 mm, 3 μm) with a C18 Cartridge (4.0×3.0 mm) from Phenomenex (Torrance, CA, USA). The column temperature was maintained at 30°C by a column heater from ThermoFisher Scientific (Waltham, MA, USA). An optimized gradient of mobile phase A: 5 mM ammonium formate/formic acid (1000:1, v/v) and mobile phase B: acetonitrile/formic acid (1000:1, v/v) was used to elute analytes of interest. The total flow rate was set at 0.5 ml/min. The gradient elution started with 30% mobile phase B, gradually increased to 80% B in 2 min, maintained constant for 1 min, and then decreased to 30% in 0.5 min, followed by column equilibrium for 2.5 min. The total running time was 6 min. Acetonitrile/water/formic acid (50:50:0.1, v/v) was used to wash the needle before and after sample aspiration.
2.6 Mass spectrometric conditions
The mass spectrometric detection was performed on an AB SCIEX QTRAP 5500 system (Toronto, Canada) with an electrospray ionization source. The multiple reaction monitoring (MRM) and positive ion mode were used for detection, with the transitions set at m/z 366.2→309.2 for prexasertib and m/z 370.2→309.2 for prexasertib-d4. The optimized ion source parameters were set as follows: ionspray voltage (IS), 5000 V; source temperature, 550°C; curtain gas (CUR), gas 1 (GS1), gas 2 (GS2), all 45 psi; collision activated dissociation (CAD), medium. The compound parameters were as follows: declustering potential (DP), 110 V for prexasertib and 105 V for ISTD; entrance potential (EP), 10 V; collision energy (CE), 29 V for prexasertib and 31 V for ISTD; collision exit potential (CXP), 8 V. Data acquisition and quantification were performed using Analyst software (Version, 1.6.2, AB SCIEX).
2.7 Method validation
2.7.1 Linearity
Calibration curves were established using double blank (blank matrix with neither prexasertib nor ISTD), zero blank (blank matrix with ISTD only), and eight nonblank calibration standards at a series of different concentrations. The peak area ratio of prexasertib to ISTD vs prexasertib concentration (x) was plotted and evaluated using least square linear regression weighted with 1/x2. The correlation coefficient (R2) was determined to evaluate the linearity of each calibration curve.
2.7.2 Precision and accuracy and dilution integrity
The assay accuracy and precision were evaluated on a single day (intra-day, n= 6) and on three different days (inter-day, n= 18) by analyzing six replicates of quality control samples at four concentrations including LLOQ (1 ng/ml for mouse plasma curve 1, 0.2 ng/ml for mouse plasma curve 2, and 0.2 ng/ml for Ringer’s/BSA), LQC (3 ng/ml for mouse plasma curve 1, 0.5 ng/ml for mouse plasma curve 2, and 0.5 ng/ml for Ringer’s/BSA), MQC (50 ng/ml for mouse plasma curve 1, 10 ng/ml for mouse plasma curve 2, and 5 ng/ml for Ringer’s/BSA), and HQC (400 ng/ml for mouse plasma curve 1, 160 ng/ml for mouse plasma curve 2, and 40 ng/ml for Ringer’s/BSA) concentrations. Precision was expressed as the percentage coefficient of variance (%CV); accuracy was expressed as (mean observed concentration)/(nominal concentration) x 100.
Dilution integrity was validated by analyzing QC samples at a concentration 10 times higher than that of HQC in the second plasma curve. Prexasertib samples in mouse plasma at 1600 ng/ml were prepared in six replicates, covering the maximum expected dilution. The accuracy and precision were determined after 10-fold dilution by blank mouse plasma.
2.7.3 Lower limit of quantification (LLOQ) and limit of detection (LOD)
The LLOQ was defined as the lowest calibration standard in the second plasma calibration curve and Ringer’s/BSA calibration curve that had both accuracy between 80–120% and precision less than 20%, and a signal/noise (S/N) ratio greater than 5. The LOD was defined as the lowest concentration with S/N at least 3.
2.7.4 Selectivity and matrix effects and recovery
To confirm that prexasertib and ISTD were separated from potentially interfering components in the matrix of interest by this newly developed method a selectivity study was performed. Selectivity was assessed by extraction of LLOQ and blank samples in three different sources of mouse plasma and Ringer’s/BSA.
Matrix effect was calculated by dividing the peak area of the post extraction spiked samples by that of the solvent spiked samples. Matrix effect from three different mouse plasma sources (CD1, CD1 nude, and FVB mouse plasma) and Ringer’s/BSA were evaluated for prexasertib at two concentrations (LQC and HQC).
Recovery was determined by dividing the peak area of the extracted samples to that of the post extraction spiked samples. Extraction efficiency of prexasertib from mouse plasma and Ringer’s/BSA were determined at two different concentrations (LQC and HQC).
2.7.5 Stability
The stability of prexasertib in mouse plasma was evaluated at 4°C and room temperature (R.T.) for up to 24 h and at 80°C for up to 2 months. Pools of blank mouse plasma at low and high concentrations of 3 ng/ml and 400 ng/ml were prepared and aliquoted. Initial values were established by assaying sample aliquots immediately after preparation, and all other aliquots were stored until analysis under conditions corresponding to the different stability test. The stability of prexasertib in Ringer’s/BSA was evaluated similarly at 4°C, R.T. and 37 °C for 24 h and at 80°C for 42 days. For the extract stability study, the extracted LQC and HQC of mouse plasma samples and Ringer’s/BSA samples were stored at 4°C in the autosampler after analysis and reinjected after approximate 24 h.
The master stock solution stability was evaluated by analyzing the old and fresh master stock solutions, which were diluted to a concentration appropriate for injection onto the LC MS/MS system.
2.8 CNS tumor microdialysis study
Cerebral microdialysis studies were performed in female CD1 nude mice (Charles River, Wilmington, MA) bearing orthotopically implanted mouse Group 3 medulloblastoma (MB) tumors under a previously described IACUC approved procedure [3, 4]. The dialysis procedure did not begin until the tumor reached a predefined size (~108 photons/sec; Xenogen, Caliper Life Sciences Inc., Hopkinton, MA). Due to issues associated with nonspecific binding of prexasertib to components of the microdialysis system that were identified by our group during preliminary studies, we chose to use a dialysate consisting of Ringer’s with 0.5% w/v BSA (Ringer’s/BSA) [5] over a simple Ringer’s solution, which is more commonly used [6]. Dialysate (Ringer’s/BSA) was perfused through the system at a flow rate of 0.5 μL/min. After a 1-hour equilibration period, a 10 mg/kg dose of prexasertib (base) was subcutaneously administered. The dosing formulation was prepared by diluting an appropriate amount of prexasertib mesylate with Captisol® (CyDex Pharmaceuticals, Inc., Lawrence, KS) to form a final admixture consisting of 1.64 mg/ml prexasertib mesylate (1.25 mg/ml base) and 20% w/v Captisol®. After dosing, dialysate fractions were collected over 1-hour intervals for 24 hours. Blood samples (75 μl) were obtained in heparinized capillary tubes at 0.25, 6.5, and 24 hours after dosing via a retro-orbital eye bleed. Plasma was immediately separated from blood samples via centrifugation and stored at −80°C until analysis. Recovery of each microdialysis probe was determined in-vitro via a retrodialysis recovery study using a Ringer’s stock solution and a perfusate consisting of a Ringer’s/BSA solution with 100 ng/ml of prexasertib.
3. Results and discussion
3.1 Mass spectrometric and chromatography conditions
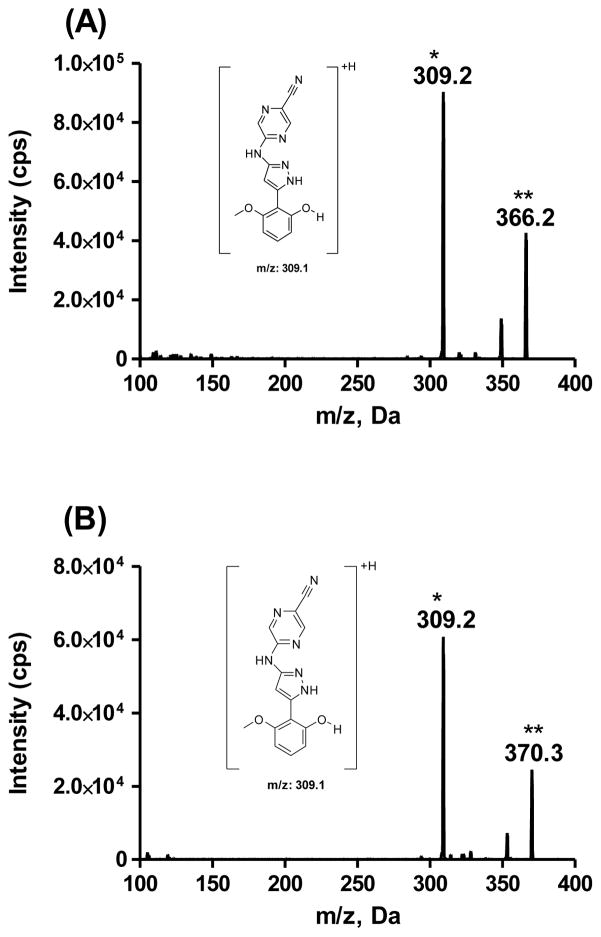
To optimize the MS parameters for detection, prexasertib and ISTD in methanol/water (4:1, v/v) were introduced into the mass spectrometer through direct infusion. The positive ionization mode was chosen to detect the signals of the compounds. Full scan of MS showed a molecular ion [M+H]+ at 366.2 for prexasertib and 370.2 for ITSD. The corresponding product ion spectra are shown in Fig. 2. After fragmentation, the most abundant product ion had a m/z of 309.2 for both prexasertib and ISTD. The proposed structure for the product ion is shown in Fig. 2. The fragmentation reactions were proposed as the loss of 3-aminopropyl for prexasertib and 3-aminopropyl-1,1,3,3-d4 for ISTD. The MRM transitions of m/z 366.2→309.2 and m/z 370.2→309.2 were selected for quantification of prexasertib and ISTD respectively.
Fig. 2.
Product ion scans for (A) prexasertib and (B) ISTD, prexasertib-d4. The proposed structure for the most abundant product ion was shown as inserted. Note: * Product ion, ** parent ion
For the chromatographic separation, two reverse phase columns (i.e., Gemini C18 and Luna C18 (2)), and various linear gradients of mobile phase A (water/formic acid, 1000:1, v/v) and mobile phase B (acetonitrile/formic acid, 1000:1, v/v) were tested initially. Prexasertib displayed less carryover and better retention on the Luna C18 (2) column than the Gemini C18 column. Adding 5 mM ammonium formate into water/formic acid (1000:1, v/v) and increasing the initial ratio of acetonitrile/formic acid (1000:1, v/v) to 30% in the gradient elution completely eliminated the minimal carryover of prexasertib on the Luna C18 (2) column. Finally, an optimized gradient of mobile phase A (5 mM ammonium formate/formic acid, 1000:1, v/v) and mobile phase B (acetonitrile/formic acid, 1000:1, v/v) eluted prexasertib and ISTD from Luna C18 (2) column at approximately 1.94 min.
3.2 Sample preparation
A LLE technique was used for mouse plasma and Ringer’s/BSA sample preparation. Compared to protein precipitation (PP), LLE provided a much cleaner sample extract with less matrix effect. TBME is the most often used organic solvent used for LLE since it is cheap and less matrix molecules can be extracted [7]. In this work, TBME was used to extract prexasertib from mouse plasma and Ringer’s/BSA with a moderate recovery rate (around 50–53%). Alkalinizing the sample with ammonia before TBME extraction did not increase the extraction efficiency.
3.3 Linearity
The calibration ranges of 1–500 ng/ml in mouse plasma and 0.2–50 ng/ml in Ringer’s/BSA were linear with correlation coefficients (R2) ≥0.995. The mean values (CV) of slopes were 0.0020 (3.6%) and 0.025 (0.28%) for mouse plasma and Ringer’s/BSA calibration curves respectively. To quantify even lower concentrations (≤ 1 ng/ml) of prexasertib in mouse plasma, the plasma calibration range was extended to 0.2 ng/ml and another calibration range of 0.2–200 ng/ml in mouse plasma was evaluated. It was linear with a correlation coefficient (R2) ≥0.998 and an average value for the slope (CV) of 0.0027 (1.6%).
3.4 Precision and accuracy and dilution integrity
The intra-and inter-day precision and accuracy were evaluated for two calibration ranges in mouse plasma (1–500 ng/ml and 0.2–200 ng/ml) and one calibration range in Ringer’s/BSA (0.2–50 ng/ml). The results for the intra-and inter-day precision and accuracy assay are depicted in Table 1. For the mouse plasma calibration range 1–500 ng/ml (QC concentrations: 1, 3, 50, and 400 ng/ml), the precision ranged from 2.0 to 4.7% for intra-day and from 3.7 to 6.0% for inter-day, whereas accuracy ranged from 102.0 to 110.0% for intra-day and from 101.7 to 108.4% for inter-day. For the mouse calibration curve range 0.2–200 ng/ml, (QC concentrations: 0.2, 0.5, 10, and 160 ng/ml), intra-and inter-day precision were ≤ 6.5% and accuracy ranged from 97.6 to 106.3%. Intra-and inter-day precision for Ringer’s/BSA were ≤ 6.7% and accuracy ranged from 95.0 to 108.5%. These results showed that the assay was both precise and accurate for the quantitation of prexasertib in mouse plasma and Ringer’s/BSA.
Table 1.
Intra-and inter-day precision and accuracy for QC samples of prexasertib in mouse plasma and Ringer’s/BSA (Intra-day: n=6; Inter-day: n=18).
| Matrix | Nominal (ng/ml) | Mean conc. (ng/ml) | Within-day (n= 6)
|
Mean conc. (ng/ml) | Between-day (n= 18)
|
||
|---|---|---|---|---|---|---|---|
| %CV | %Accuracy | %CV | %Accuracy | ||||
| Mouse Plasma (curve 1) | 1 | 1.03 | 3.9 | 103.0 | 1.05 | 6.0 | 105.0 |
| 3 | 3.06 | 3.8 | 102.0 | 3.05 | 4.5 | 101.7 | |
| 50 | 54.1 | 4.7 | 108.2 | 54.2 | 3.7 | 108.4 | |
| 400 | 440.0 | 2.0 | 110.0 | 431.8 | 3.9 | 108.0 | |
| Mouse Plasma (curve 2) | 0.2 | 0.206 | 6.5 | 103.0 | 0.207 | 5.7 | 103.5 |
| 0.5 | 0.492 | 4.4 | 98.4 | 0.488 | 4.2 | 97.6 | |
| 10 | 9.84 | 3.6 | 98.4 | 9.97 | 4.1 | 99.7 | |
| 160 | 166.0 | 2.2 | 103.8 | 170.0 | 2.6 | 106.3 | |
| 1600 | 1696.7 | 1.6 | 106 | ||||
| Ringer’s/BSA | 0.2 | 0.190 | 6.7 | 95.0 | 0.198 | 6.1 | 99.0 |
| 0.5 | 0.487 | 5.8 | 97.4 | 0.486 | 4.5 | 97.2 | |
| 5 | 5.02 | 3.1 | 100.4 | 4.98 | 3.2 | 99.6 | |
| 40 | 43.4 | 2.6 | 108.5 | 43.3 | 2.0 | 108.2 | |
CV = coefficient of variation
Since some mouse plasma samples contained prexasertib above the highest concentration of calibration curve, dilution integrity was evaluated. The accuracy and precision for the diluted mouse plasma samples was determined to be 106% and 1.6%, respectively, indicating that the plasma sample with the concentration of prexasertib above the upper limit of quantitation can be diluted and then analyzed with precision and accuracy (Table 1).
3.5 Lower limit of quantification and limit of detection
For prexasertib in mouse plasma and Ringer’s/BSA, the LLOQ was 0.2 ng/ml with a S/N ≥5 and the LOD was 0.05 ng/ml with a S/N ≥3.
3.6 Selectivity, matrix effects, and recovery
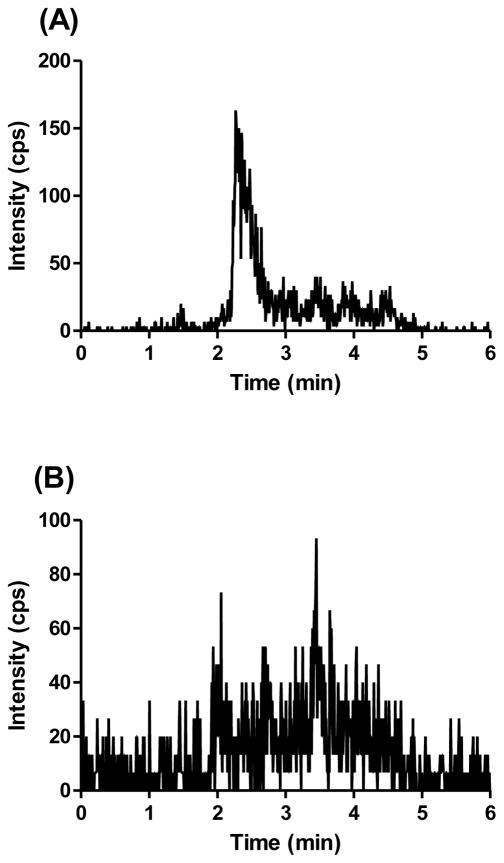
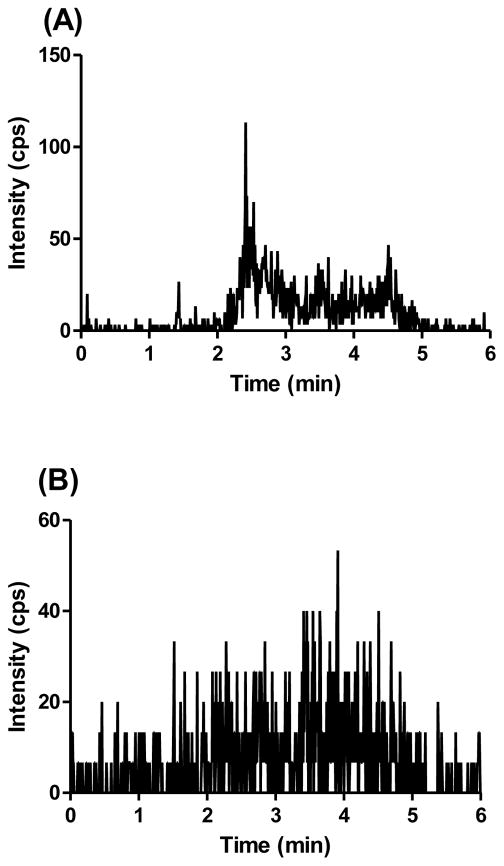
The selectivity of assay was evaluated by analyzing blank mouse plasma from three different sources and the LLOQ sample (i.e., 0.2 ng/ml). A typical chromatogram of blank mouse plasma and blank Ringer’s/BSA and LLOQ samples in the respective matrix are shown in the Figs. 3 and 4. No interfering peaks co-eluted with prexasertib or ISTD in blank mouse plasma or Ringer’s/BSA.
Fig. 3.
Representative MRM chromatograms of (A) prexasertib scan in blank mouse plasma, (B) ISTD scan in blank mouse plasma, (C) prexasertib scan in LLOQ (0.2 ng/ml) mouse plasma sample, and (D) ISTD scan in LLOQ (0.2 ng/ml) mouse plasma sample.
Fig. 4.
Representative MRM chromatograms of (A) prexasertib scan in blank Ringer’s/BSA, (B) ISTD scan in blank Ringer’s/BSA, (C) prexasertib scan in LLOQ (0.2 ng/ml) Ringer’s/BSA sample, and (D) ISTD scan in LLOQ (0.2 ng/ml) Ringer’s/BSA sample.
The matrix effect and extraction efficiency from mouse plasma and Ringer’s/BSA were evaluated at two concentrations. As shown in Table 2, the matrix factors for prexasertib in mouse plasma from three different sources ranged from 1.13 to 1.18, indicating minimal matrix effect. Since the deuterated prexasertib was used as ISTD, a similar range of matrix factors (1.11–1.17) was observed for ISTD in three different sources of mouse plasma. The ISTD normalized matrix factor is close to 1. For prexasertib and ISTD in Ringer’s/BSA, no matrix effects were observed.
Table 2.
Matrix effect in different matrices.
| Blank matrix | Prexasertib matrix factora (LQC)b | ISTD matrix factora | ISTD normalized matrix factor | Prexasertib matrix factora (HQC)b | ISTD matrix factora | ISTD normalized matrix factor |
|---|---|---|---|---|---|---|
| Mouse plasma CD1 | 1.14 (4.6) | 1.11 (1.4) | 1.03 | 1.13 (0.9) | 1.12 (2.9) | 1.01 |
| Mouse plasma CD1 nude | 1.17 (4.5) | 1.13 (2.9) | 1.04 | 1.12 (1.9) | 1.11 (1.9) | 1.01 |
| Mouse plasma FVB | 1.18 (1.3) | 1.14 (1.3) | 1.04 | 1.17 (1.0) | 1.17 (3.1) | 1 |
| Ringer’s/BS A | 0.97 (2.1) | 0.98 (4.1) | 0.98 | 0.98 (0.6) | 0.99 (2.1) | 0.99 |
Results are presented as average (CV%) of triplicate;
Matrix effect was evaluated for prexasertib at two concentration levels for each matrix.
LQC: 3 ng/ml for mouse plasma and 0.5 ng/ml for Ringer’s/BSA; HQC: 400 ng/ml for mouse plasma and 40 ng/ml for Ringer’s/BSA.
The average recovery of prexasertib from mouse plasma was 52% and was very consistent for two different concentrations (3 and 400 ng/ml). A similar recovery efficiency (51% and 55% of average recovery for 0.5 and 40 ng/ml respectively) was observed for prexasertib in Ringer’s/BSA. For both mouse plasma and Ringer’s/BSA, the ISTD normalized recovery is close to 1, indicating that ISTD compensated for the loss of prexasertib during the extraction (data not shown).
3.7 Stability
The results for the stability of prexasertib in mouse plasma and Ringer’s/BSA are shown in Table 3. Prexasertib was stable up to 24 h in mouse plasma and Ringer’s/BSA, at 4°C and room temperature. When stored at -80°C, prexasertib was stable up to 2 months in mouse plasma and 42 days in Ringer’s/BSA. Since the microdialysis experiment was performed at 37°C, the stability of prexasertib in Ringer’s/BSA was also determined at 37°C. It was found that prexasertib was stable up to 24h at this temperature. Additionally, the stability of prexasertib master stock solution and the final extracts from mouse plasma or Ringer’s/BSA samples were evaluated (data not shown). Prexasertib master stock solution was stable up to 6 months at −80°C. The mouse plasma or Ringer’s/BSA extracts for LC/MS/MS were stable up to 24 h at4 °C in the autosampler, thus enabling the reinjection of samples for reanalysis when needed.
Table 3.
Stability of prexasertib in mouse plasma and Ringer’s/BSA.
| Mouse Plasma | Ringer’s/BSA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| a LQC | a HQC | a LQC | a HQC | ||||||||
|
| |||||||||||
| Temp. | Time | % change | %CV | % change | %CV | Temp. | Time | % change | %CV | % change | %CV |
| 4 °C | 4°C | ||||||||||
| 4 h | 6.0 | 4.4 | −1.0 | 4.4 | 24 h | −4.8 | 3.7 | −2.9 | 2.8 | ||
| 24 h | −2.0 | 2.6 | −0.2 | 3.3 | |||||||
| R.T. | R. T. | ||||||||||
| 4 h | 0 | 9.2 | 1.1 | 4.8 | 24 h | 0.7 | 2.4 | −6.4 | 2.0 | ||
| 24 h | 3 | 2.7 | −0.1 | 0.9 | |||||||
| −80°C | −80 °C | ||||||||||
| 7 days | −4.6 | 9.5 | −0.9 | 3.1 | 42 days | −8.1 | 5.2 | −5.2 | 0.5 | ||
| 60 days | −6.5 | 2.3 | −3.8 | 3.0 | |||||||
| 37°C | |||||||||||
| 24 h | −6.4 | 7.2 | −6.9 | 1.6 | |||||||
Stability was evaluated for prexasertib in each matrix at two concentration levels (LQC: 3 ng/ml for mouse plasma and 0.5 ng/ml for Ringer’s/BSA; HQC: 400 ng/ml for mouse plasma and 40 ng/ml for Ringer’s/BSA). The results are presented as average change in the concentration at the time of stability study with respective to the concentration at the time 0 and % CV of triplicate.
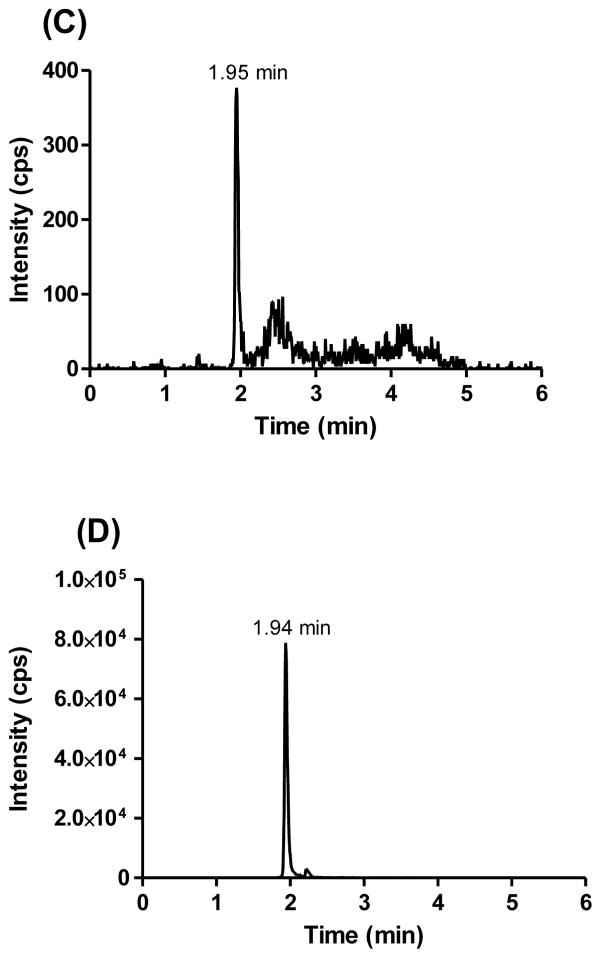
3.8 Application of method to cerebral microdialysis study
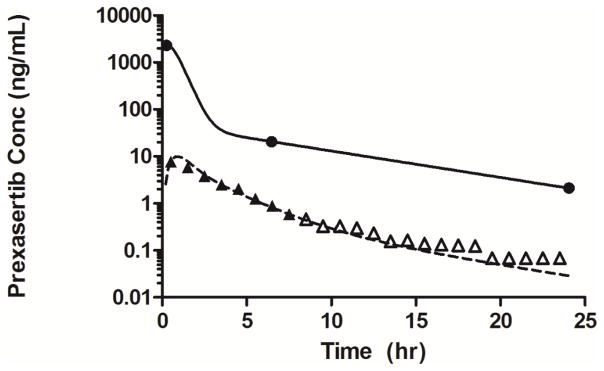
Methods developed here were used to measure prexasertib in mouse plasma and Ringer’s/BSA samples collected during a cerebral microdialysis study from a mouse bearing an orthotopic Group 3 MB tumor (see Fig. 5). Plasma concentrations obtained from the limited sampling scheme were analyzed using population pharmacokinetic (PK) modeling to provide empirical Bayes estimates for parameters describing the plasma PK of prexasertib. We observed that prexasertib was rapidly absorbed into the systemic circulation after subcutaneous administration with a peak concentration observed at 0.39 h. The terminal half-life of prexasertib in plasma was 5.34 h. Measurable prexasertib concentrations above the LLOQ were observed in dialysate up to 8 h after subcutaneous administration. The brain ECF to unbound plasma partition coefficient of prexasertib (Kp,uu), a ratio of the areas under the unbound prexasertib concentration-time curves in brain ECF and plasma was 0.10. This value was calculated using a fraction unbound in CD1 mouse plasma of 0.11 (Unpublished data, Stewart laboratory).
Fig. 5.
Prexasertib concentration-time profiles in plasma and tumor extracellular fluid (ECF) for a cerebral microdialysis experiment in one representative mouse bearing a Group 3 MB tumor (closed circles represent observed prexasertib concentrations in plasma, and the solid line represents model predicted concentrations in plasma; closed and open triangles represent recovery corrected prexasertib concentrations in microdialysate above and below the LLOQ, respectively. The dashed line represents model predicted concentrations in microdialysate).
4. Conclusion
A sensitive LC–MS/MS method for the quantitation of prexasertib in mouse plasma and Ringer’s/BSA was developed and validated for the first time. This method is simple, sensitive and specific for the analysis of prexasertib in mouse plasma and Ringer’s/BSA. The LLOQ was 0.2 ng/ml for both mouse plasma and Ringer’s/BSA, showing an excellent signal to noise ratio. This method also demonstrated excellent precision, accuracy, and reproducibility for routine analysis. The validation meets the overall acceptance criteria specified by FDA for bioanalysis [8]. We have successfully applied this LC MS/MS method for measuring prexasertib in mouse plasma and cerebral microdialysis samples (Ringer’s/BSA). This method may be further used in prexasertib-related preclinical pharmacokinetic studies in the future.
Highlights.
A sensitive LC–MS/MS method for the quantitation of prexasertib in mouse plasma and Ringer’s solution with 0.5% bovine serum albumin (Ringer’s/BSA) was developed and validated.
Prexasertib was extracted from mouse plasma and Ringer’s/BSA by Liquid-liquid extraction.
This method demonstrated excellent precision, accuracy, reproducibility for routine analysis, and was successfully applied for a cerebral microdialysis study.
Acknowledgments
Research reported in the publication was supported by a Cancer Center Support (CORE) Grant CA 21765, a grant from Eli Lilly, and the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Conflict of interest
The authors have no conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Savage P, Mahmoud S. Development and economic trends in cancer therapeutic drugs: a 5-year update 2010–2014. Br J Cancer. 2015;112:1037–1041. doi: 10.1038/bjc.2015.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patil M, Pabla N, Dong Z. Checkpoint kinase 1 in DNA damage response and cell cycle regulation. Cell Mol Life Sci. 2013;70:4009–4021. doi: 10.1007/s00018-013-1307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel YT, Jacus MO, Boulos N, Dapper JD, Davis AD, Vuppala PK, Freeman BB, 3rd, Mohankumar KM, Throm SL, Gilbertson RJ, Stewart CF. Preclinical examination of clofarabine in pediatric ependymoma: intratumoral concentrations insufficient to warrant further study. Cancer Chemother Pharmacol. 2015;75:897–906. doi: 10.1007/s00280-015-2713-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacus MO, Throm SL, Turner DC, Patel YT, Freeman BB, 3rd, Morfouace M, Boulos N, Stewart CF. Deriving therapies for children with primary CNS tumors using pharmacokinetic modeling and simulation of cerebral microdialysis data. Eur J Pharm Sci. 2014;57:41–47. doi: 10.1016/j.ejps.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nirogi R, Kandikere V, Bhyrapuneni G, Benade V, Saralaya R, Irappanavar S, Muddana N, Ajjala DR. Approach to reduce the non-specific binding in microdialysis. J Neurosci Methods. 2012;209:379–387. doi: 10.1016/j.jneumeth.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Kala A, Patel YT, Davis A, Stewart CF. Development and validation of LC-MS/MS methods for the measurement of ribociclib, a CDK4/6 inhibitor, in mouse plasma and Ringer's solution and its application to a cerebral microdialysis study. J Chromatogr B Analyt Technol Biomed Life Sci. 2017;1057:110–117. doi: 10.1016/j.jchromb.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemal M, Ouyang Z, Xia YQ. Systematic LC-MS/MS bioanalytical method development that incorporates plasma phospholipids risk avoidance, usage of incurred sample and well thought-out chromatography. Biomed Chromatogr BMC. 2010;24:2–19. doi: 10.1002/bmc.1373. [DOI] [PubMed] [Google Scholar]
- 8.F. US Department of Health and Human Services, CDER, CVM, editor. Guidance for Industry, Bioanalytical Method Validation. May, 2001. [Google Scholar]