Abstract
Background
Serum lactate level can predict clinical outcomes in some critical cases. In the clinical setting, we noted that patients undergoing extracorporeal cardiopulmonary resuscitation (ECPR) and with poor serum lactate improvement often do not recover from cardiopulmonary arrest. Therefore, we investigated the association between lactate clearance and in-hospital mortality in cardiac arrest patients undergoing ECPR.
Methods
Serum lactate levels were measured on admission and every hour after starting ECPR. Lactate clearance [(lactate at first measurement − lactate 6 h after)/lactate at first measurement × 100] was calculated 6 h after first serum lactate measurement. All patients who underwent ECPR were registered retrospectively using opt-out in our outpatient’s segment.
Result
In this retrospective study, 64 cases were evaluated, and they were classified into two groups according to lactate clearance: high-clearance group, > 65%; low-clearance group, ≤ 65%. Surviving discharge rate of high-clearance group (12 cases, 63%) is significantly higher than that of low-clearance group (11 cases, 24%) (p < 0.01). Considering other confounders, lactate clearance was an independent predictor for in-hospital mortality (odds ratio, 7.10; 95% confidence interval, 1.71–29.5; p < 0.01). Both net reclassification improvement (0.64, p < 0.01) and integrated reclassification improvement (0.12, p < 0.01) show that adding lactate clearance on established risk factors improved the predictability of in-hospital mortality.
Conclusion
In our study, lactate clearance calculated through arterial blood gas analysis 6 h after ECPR was one of the most important predictors of in-hospital mortality in patients treated with ECPR after cardiac arrest.
Keywords: Lactate clearance, Extracorporeal cardiopulmonary resuscitation, Cardiac arrest, In-hospital mortality
Background
Extracorporeal cardiopulmonary resuscitation (ECPR) is one of the most powerful therapies after cardiopulmonary arrest (CPA) [1]. A prior study showed that earlier return of circulation leads to improvement of 30-day survival, surviving discharge rate, and clinical performance category (CPC) [2]. Because ECPR restarts systemic circulation forcibly, it is a very strong strategy when cardiopulmonary resuscitation or defibrillation is not effective. However, the guideline of the American Heart Association (AHA) cited insufficient evidence and limited the indication for ECPR [3].
According to AHA guidelines, ECPR may be considered for selected cardiopulmonary arrest patients in whom the suspected etiology of cardiac arrest is potentially reversible during a limited period of mechanical cardiorespiratory support [3]. Because the CPC or surviving discharge rate is very low after CPA or ECPR, the adequacy of continuation of ECPR should be considered [4]. Nevertheless, there have been very limited data of ECPR prognosis or risk factors [3]. Risk factors such as initial rhythm (shockable rhythm or non-shockable rhythm), old age, CPA without bystander, without bystander CPR, longer CPR duration time, and without defibrillation are well-known independent prognostic factors.
A prior study showed that early goal-directed hemodynamic optimization therapy is effective in cardiac arrest [5, 6]. Meanwhile, earlier improvement in lactate clearance (LC) was reported to lead to better prognosis in the treatment of sepsis [7, 8]. In addition, serum lactate-guided intensive care reduces hospital mortality in the treatment of sepsis [9]. Post-cardiac arrest syndrome (PCAS) is reported to be one of the sepsis-like syndromes [10]. Of course, lactate reduction is one of most important predictors of survival and neurological outcome after cardiac arrest [11]. Thus, we hypothesized that LC might be an indicator of ECPR effectiveness.
We investigated the association between LC and surviving discharge in cardiac arrest patients treated with ECPR.
Methods
In this single-center retrospective observational study, we collected data on 98 patients treated with percutaneous cardiopulmonary support (PCPS) at our hospital between 2011 and 2016.
Among the 98 patients treated with PCPS at our hospital, 24 received PCPS before cardiac arrest; these cases were not defined as cases of ECPR and were excluded. Further, we also excluded patients with an etiology of aortic dissection. Finally, 4 patients who died before 6 h after ECPR and one patient whose serum lactate lose at 6 h were also excluded. Thus, in total, we evaluated 64 patients undergoing ECPR after cardiac arrest (Fig. 1). Their data, including their serum lactate levels and clinical courses, including that after ECPR, were retrospectively collected.
Fig. 1.
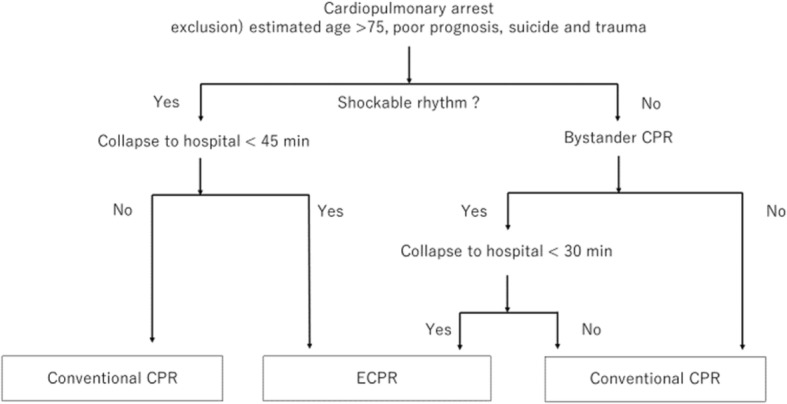
Decision tree of ECPR or conventional CPR with inclusion and exclusion criteria for ECPR
The exclusion criteria for ECPR were as follows: patients with estimated age > 75 years, those with no long-term prognosis, and those with dementia. Our in/exclusion flow chart is shown in Fig. 2. In addition, ECPR was not performed even if the cardiovascular physician decided it would not be effective for the patient.
Fig. 2.
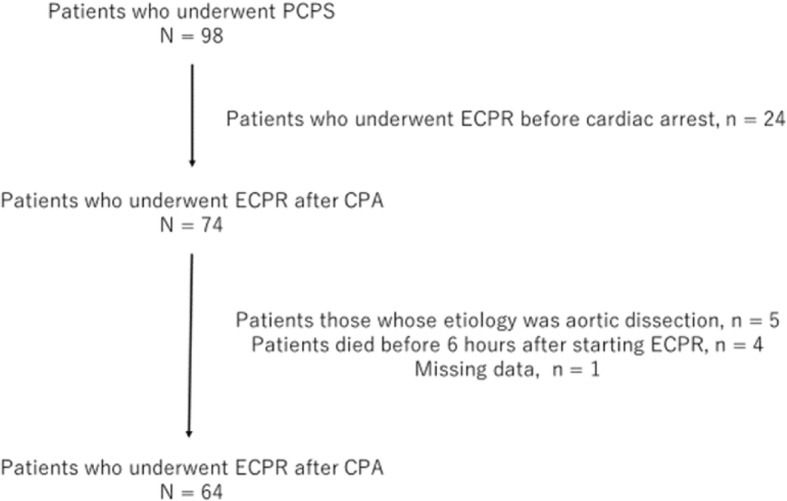
Design of this observation study
After commencement of ECPR, we usually check the patients’ consciousness levels before leaving our catheter laboratory. In cases in which the Glasgow Coma Scale motor score was below 6, targeted temperature management (TTM) was initiated. Our TTM protocol is as follows: 34 °C for 48 h and a recovery temperature of 36 °C during the next 24 h.
The primary outcome was survival discharge, and the secondary outcomes were 30-day mortality and neurological outcomes.
Serum lactate measurement and LC calculation
Arterial blood gas samples were immediately obtained from the arteries of all CPA patients in the emergency department of our hospital. The artery blood samples were immediately transferred to our laboratory and measured using RapidLab (Siemens AG, Erfurt, Germany). In case of ECPR, arterial blood gas analysis was performed every hour until the end of ECPR. Serum lactate was measured simultaneously with artery blood gas analysis. Blood sample was transferred to the laboratory and measured as soon as possible every time.
We calculated LC using the serum lactate level at the emergency department and at 6 h after admission using the following formula:
Patients with LC > 65% were included in the high-clearance group, and those with LC ≤ 65% were included in the low-clearance group.
We determined the cutoff value retrospectively. Receiver operating characteristic curve (ROC) analysis yielded a cutoff value of LC = 69% (sensitivity 0.48, 1 − specificity 0.43, AUC 0.75) (Fig. 3). In addition, we observed that the serum lactate level improved on early lactate-guided therapy [9]. The reported improvements in the lactate levels were 4.7–1.7 (64%) in the control group and 4.6–1.6 (65%) in the targeted group. Through consensus with ECPR specialists and analysts, we concluded that LC = 65% is a better cutoff value for ECPR.
Fig. 3.
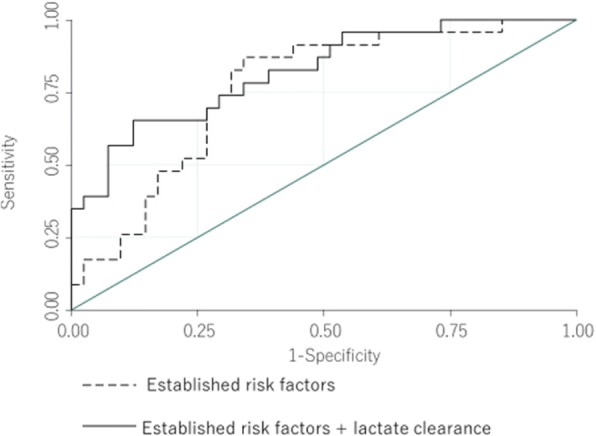
ROC comparison between established risk factors and + LC
Statistical analysis
Statistical analysis was performed using JMP version 13.0 software (SAS Institute, Cary, NC, USA). Continuous variables were presented as median values with interquartile ranges according to the results of the normality test. Mann-Whitney U tests were conducted for comparison of continuous variables. Categorical variables were presented as frequencies and percentages and compared using chi-squared or Fisher exact tests. Intergroup differences in the continuous and categorical variables were evaluated using the Student t test and chi-squared test, respectively. Intergroup differences in mortality were evaluated using a logistic regression model. The significant variables from univariate analysis and the established risk factors were included in multivariate logistic regression analysis. We included the established risk factors (age, sex, initial rhythm, in-/out-hospital CPA, pH, and CRP duration) as confounders during multivariate logistic regression analysis. In addition, we calculated the area under the ROC (AUC), net reclassification improvement (NRI), and integrated discrimination improvement (IDI) to assess the accuracy of LC as a predictor when added to a baseline model with established risk factors. NRI indicates the relative number of patients with improved predicted probabilities for LC, whereas IDI represents the average improvement in predicted probabilities for LC after adding LC variables into the baseline model. In all analyses, p < 0.05 was considered statistically significant.
Results
Patient characteristics are shown in Table 1. There were significant differences in total protein (low-clearance group: median, 4.9 g/dL; range, 4.0–5.6 g/dL; high-clearance group: median, 5.7 g/dL; range, 5.1–6.4 g/dL; p = 0.02), serum albumin (low-clearance group: median, 2.5 g/dL; range, 2.0–3.2 g/dL; high-clearance group: median, 3.3 g/dL; range, 2.6–3.8 g/dL, p = 0.01), and platelet (low-clearance group: median, 167,000; range, 148,000–209,000; high-clearance group: median, 213,000; range, 143,000–253,000 g/dL; p = 0.02). Except for total protein, serum albumin, and platelet, the baseline characteristics in both groups were well-matched.
Table 1.
Patients’ background
| All cases n = 64 |
Low-clearance group n = 45 |
High-clearance group n = 19 |
p value | |
|---|---|---|---|---|
| Age | 70.8 (58.5–77.9) | 71.7 (63.8–77.3) | 64.1 (50.6–78.5) | 0.30 |
| Female (%) | 17 (27) | 14 (31) | 3 (18) | 0.35 |
| Height cm | 165 (157–172) | 164 (156–170) | 164 (156–170) | 0.08 |
| Weight kg | 63 (54–72) | 61 (53–72) | 65 (55–75) | 0.45 |
| BMI | 23 (21–25) | 23 (21–25) | 23 (21–26) | 0.88 |
| Diabetes (%) | 23 (36) | 17 (38) | 6 (32) | 0.78 |
| Hypertension (%) | 34 (53) | 25 (56) | 9 (47) | 0.59 |
| Dyslipidemia (%) | 20 (31) | 12 (27) | 8 (42) | 0.25 |
| Current smoke (%) | 19 (30) | 10 (22) | 9 (47) | 0.07 |
| Hemodialysis (%) | 4 (6.3) | 2 (4.4) | 2 (11) | 0.58 |
| Prior PCI (%) | 13 (20) | 10 (22) | 3 (16) | 0.56 |
| Prior CABG (%) | 6 (9.4) | 4 (8.9) | 2 (11) | 1.00 |
| OMI (%) | 15 (23) | 10 (22) | 5 (26) | 0.75 |
| Initial rhythm | 0.48 | |||
| VF/pulseless VT (%) | 38 (59) | 25 (56) | 13 (68) | |
| PEA/asystole (%) | 26 (41) | 20 (44) | 6 (32) | |
| Location | 0.42 | |||
| In-hospital (%) | 45 (55) | 23 (51) | 12 (63) | |
| Out-hospital (%) | 29 (45) | 22 (49) | 7 (37) | |
| CPR duration (min) | 24 (12–45) | 24 (16–46) | 25 (10–46) | 0.67 |
| Laboratory data | ||||
| pH | 7.03 (6.92–7.15) | 7.03 (6.89–7.14) | 7.09 (6.92–7.20) | 0.54 |
| Lactate mmol/L | 11.8 (9.9–14.8) | 11.7 (9.7–14.9) | 12.8 (10.1–14.2) | 0.74 |
| Total protein g/dL | 5.2 (4.3–6.1) | 4.9 (4.0–5.6) | 5.7 (5.1–6.5) | 0.02 |
| Albumin g/dL | 2.9 (2.1–3.5) | 2.5 (2.0–3.2) | 3.3 (2.6–3.8) | 0.01 |
| BUN mg/dL | 19 (16–28) | 20 (17–27) | 19 (14–31) | 0.59 |
| Creatinine mg/dL | 1.1 (1.0–1.5) | 1.1 (0.9–1.4) | 1.1 (1.0–1.5) | 0.74 |
| Total cholesterol mg/dL | 129 (80–164) | 98 (70–164) | 142 (97–178) | 0.15 |
| Low-density lipoprotein mg/dL | 70 (55–109) | 62 (54–105) | 95 (70–127) | 0.11 |
| High-density lipoprotein mg/dL | 28 (20–35) | 25 (18–33) | 28 (24–40) | 0.16 |
| Triglyceride mg/dL | 71 (42–96) | 58 (32–103) | 84 (71–94) | 0.26 |
| Hemoglobin g/dL | 11.6 (9.5–13.8) | 11.0 (8.3–13.9) | 12.2 (11.2–13.6) | 0.14 |
| White blood cell count 103/μL | 124 (97–168) | 121 (96–16) | 137 (106–194 | 0.21 |
| Platelet 104/μL | 16.7 (11.9–21.6) | 14.8 (9.8–20.9) | 21.3 (14.3–25.3) | 0.02 |
| C-reaction protein mg/dL | 0.19 (0.06–3.13) | 0.19 (0.07–2.56) | 0.16 (0.05–4.83) | 0.91 |
Diagnosis and follow-up data
The final diagnosis is shown in Table 2. In the first 30 days, the survival rate was significantly higher in the high-clearance group (12 cases, 63%) than in the low-clearance group (12 cases, 27%; p ≤ 0.01). The survival discharge rate was significantly higher in the high-clearance group (12 cases, 63%) than in the low-clearance group (11 cases, 24%; p < 0.01) (Table 3). Neurological outcome at discharge was better in the high-clearance group than in the low-clearance group (Table 3).
Table 2.
Final diagnosis
| Diagnosis | All cases n = 69 |
Low-clearance group n = 45 |
High-clearance group n = 19 |
p value |
|---|---|---|---|---|
| 0.48 | ||||
| Cardiac rapture (%) | 11 (15.9) | 6 (13) | 1 (5.3) | |
| Electrical storm (%) | 6 (8.7) | 3 (6.7) | 3 (16) | |
| Heart failure (%) | 4 (5.8) | 5 (11) | 2 (11) | |
| Ischemic heart disease (%) | 32 (46.4) | 21 (47) | 10 (53) | |
| PE (%) | 3 (4.4) | 2 (4.4) | 1 (5.3) | |
| Myocarditis (%) | 2 (2.9) | 1 (2.2) | 1 (5.3) | |
| Other | 11 (15.9) | 7 (16) | 1 (5.3) |
Table 3.
Primary outcome and secondary outcome
| All cases n = 64 |
Low-clearance group n = 45 |
High-clearance group n = 19 |
p value | |
|---|---|---|---|---|
| Surviving discharge | 23 (36) | 11 (24) | 12 (63) | < 0.01 |
| 30-day survival (%) | 24 (38) | 12 (27) | 12 (63) | < 0.01 |
| Neurological outcome (CPC) | < 0.01 | |||
| 1 (%) | 16 (25) | 8 (18) | 11 (58) | |
| 2 (%) | 3 (4.7) | 2 (4.4) | 1 (5.3) | |
| 3 (%) | 1 (1.6) | 1 (2.2) | 0 (0.0) | |
| 4 (%) | 1 (1.6) | 1 (2.2) | 0 (0.0) | |
| 5 (%) | 43 (67) | 34 (76) | 7 (37) |
In the univariable and multivariable logistic regression analyses for surviving discharge, LC was an independent predictor for surviving discharge (odds ratio, 7.10; 95% confidence interval, 1.71–29.5; p < 0.01). CPR duration time, location (in-/out-hospital CPR), and pH were also successful independent predictors for surviving discharge (Table 4). The NRI and IDI are shown in Table 5. Adding LC to the established risk factors improved predictability of surviving discharge after ECPR.
Table 4.
Multi-logistic analysis for surviving discharge
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
| Odds ratio | Confidential interval | p value | Odds ratio | Confidential interval | p value | |
| Age | 0.98 | 0.95–1.03 | 0.63 | 1.02 | 0.96–1.10 | 0.49 |
| Initial rhythm (VF and pulseless VT/asystole and PEA) | 1.47 | 0.51–4.22 | 0.46 | 1.42 | 0.32–6.27 | 0.64 |
| Location(out/in) | 1.17 | 0.42–3.26 | 0.64 | 10.0 | 1.35–75.0 | 0.01 |
| CPR duration | 1.02 | 0.99–1.05 | 0.22 | 1.08 | 1.01–1.12 | 0.02 |
| pH | 25.2 | 1.24–509 | 0.03 | 247 | 4.16–15,000 | < 0.01 |
| Lactate clearance (high/low) | 5.3 | 1.67–16.8 | 0.01 | 7.10 | 1.71–29.5 | < 0.01 |
Table 5.
Net reclassification improvement and integrated reclassification improvement
| AUC | p value | NRI | p value | IDI | p value | |
|---|---|---|---|---|---|---|
| Established risk factors | 0.76 | reference | reference | |||
| + Lactate clearance | 0.82 | 0.23 | 0.64 | < 0.01 | 0.121 | < 0.01 |
Established risk factors were consisted age, sex, initial rhythm, in-/out-hospital CPA, pH, and CRP duration
Discussion
The results of the study showed that LC was one of the independent predictors of ECPR for in-hospital mortality. Addition of LC to the established risk factors such as age, initial rhythm, in-/out-hospital CPA, pH, and CRP duration time improved NRI and IDI. Because LC is easy to calculate, is reliable, and has small fluctuations in the clinical settings, our findings might be of clinical significance.
In the case of cardiac arrest, ECPR is one of the most powerful intensive and effective treatments, as shown by previous studies [11, 12]. However, AHA guidelines limited its indication because of poor evidence [3]. In the study, we recognized that ECPR was a very useful and effective treatment for patients who after cardiac arrest.
Because ECPR and intensive care require higher cost, need more time, and are more labor-intensive, the cost/benefit should be considered [13]. Furthermore, ceasing ECPR may sometimes be recommended because of the patient’s poor prognosis. Hence, a prognostic predictor can help decide whether to continue ECPR. Although well-known predictors which have been shown in the previous reports are factors already determined before return of spontaneous circulation (ROSC) [14, 15], LC is a unique predictor because it can be calculated 6 h after starting ECPR, not before ROSC. This time lag gives us a chance to reconsider the continuation of ECPR.
In the clinical setting, patients with a lower lactate level might have a better outcome in both PCAS and sepsis. We hypothesize that the high serum lactate level with cytokinetic storm in PCAS is due to reperfusion injury, whereas that in sepsis is due to the cytokinetic storm caused by the systemic infection. In view of the cytokinetic phenomenon, sepsis is similar to PCAS, and this hypothesis is shown in a prior study [10]. Meanwhile, a previous study showed that serum lactate level is a better indicator of early goal-directed therapy than SvO2 [16]. Considering the similarity between sepsis and PCAS, a therapy strategy based on the serum lactate level will be more effective, even in PCAS.
A previous study showed that early goal-directed therapy is an effective strategy in sepsis [17]. Another study showed that LC is a more important indicator than SvO2 in sepsis [6]. We believe that early goal-directed therapy based on lactate will be an important strategy in ECPR. Our results showed that a lower serum lactate level at 6 h than the primary lactate level could be used as one of the prognostic indicators. Thus, we should consider that the prognosis after ECPR can be improved by lowering the lactate level using catecholamines, intra-aortic balloon pumping, optimization of percutaneous cardiopulmonary support, infusions, transfusions, and so forth, that is, if serum lactate-guided early goal-directed therapy will improve the prognosis of CPA and/or ECPR cost/benefit.
PCAS includes brain/myocardial disorders and systemic reperfusion injury. ECPR consists of a therapy for PCAS and treatment of the original disease caused the CPA. Therefore, with better LC, treatment of the original disease, care for the myocardial disorder after CPA, improvement of systemic circulation, and coping with systemic reperfusion injury like sepsis may be successful. Meanwhile, in the case of worse LC, failure in one or more of the abovementioned items may occur.
Limitations
Some limitations should be considered. First, the small number of enrolled patients was not enough to determine a new evidence. Second, there were strong biases due to our ECPR exclusion criteria, e.g., age > 75 years, end-stage cancer, and strong frailty. Third, medical treatments might have also affected the results; however, we could not evaluate such data, e.g., different treatment methods for each doctor. Further studies are required to address these limitations.
Conclusion
In our study, LC determined 6 h after ECPR significantly predict survival discharge in patients treated with ECPR after cardiac arrest. Using LC during ECPR might provide useful information whether continuing ECPR is adequate or not.
Acknowledgements
The authors would like to thank Honyaku center (commercial translation and proofreading company) and Hitoshi Yamaguchi who works as the chief of emergency department in our hospital.
Availability of data and materials
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHA
American Heart Association
- CPA
Cardiopulmonary arrest
- CPR
Cardiopulmonary resuscitation
- ECPR
Extracorporeal cardiopulmonary resuscitation
- IDI
Integrated discrimination improvement
- LC
Lactate clearance
- NRI
Net reclassification improvement
- PCAS
Post-cardiac arrest syndrome
Authors’ contributions
All authors have read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the clinical trial review committee of the Ichinomiya Municipal Hospital. As this was a retrospective study, the need for informed consent was waived.
Competing interests
H.I. received lecture fees from Astellas Pharma Inc., Daiichi-Sankyo Pharma Inc., and MSD K.K. T. M. received lecture fees from Bayel Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., Kowa Co., Ltd., MSD K.K., Mitsubishi Tanabe Pharma Co., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Pfizer Japan Inc., Sanofi-aventis K.K., and Takeda Pharmaceutical Co., Ltd.
T.M. received unrestricted research grant from the Department of Cardiology, Nagoya University Graduate School of Medicine from Astellas Pharma Inc., Daiichi Sankyo Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., Kowa Co., Ltd., MSD K.K., Mitsubishi Tanabe Pharma Co., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Otsuka Pharma Ltd., Pfizer Japan Inc., Sanofi-aventis K.K., Takeda Pharmaceutical Co., Ltd., and Teijin Pharma Ltd.
The other authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kano H, Yamazaki K, Nakajima M, et al. Rapid induction of percutaneous cardiopulmonary bypass significantly improves neurological function in patients with out-of-hospital cardiogenic cardiopulmonary arrest refractory to advanced cardiovascular life support. Circulation. 2006;114:II–348. [Google Scholar]
- 2.Wibrandt I, Norsted K, Schmidt H, Schierbeck J. Predictors for outcome among cardiac arrest patients: the importance of initial cardiac arrest rhythm versus time to return of spontaneous circulation, a retrospective cohort study. BMC Emerg Med. 2015;15:3. doi: 10.1186/s12873-015-0028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks SC, Anderson ML, Bruder E, et al. American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S436–S443. doi: 10.1161/CIR.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 4.Nagao K, Kikushima K, Watanabe K, et al. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ J. 2010;74:77–85. doi: 10.1253/circj.CJ-09-0502. [DOI] [PubMed] [Google Scholar]
- 5.Gaieski D, Band RA, Abella BS, et al. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009;80:418–424. doi: 10.1016/j.resuscitation.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 6.Jones AE, Shapiro NI, Trzeciak S, et al. LC vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739–746. doi: 10.1001/jama.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walters EL, Morawski K, Dorrotta I, et al. Implementation of a post-cardiac arrest care bundle including therapeutic hypothermia and hemodynamic optimization in comatose patients with return of spontaneous circulation after out-of-hospital cardiac arrest: a feasibility study. Shock. 2011;35(4):360–6. [DOI] [PubMed]
- 8.Puskarich MA, Trzeciak S, Shapiro NI, et al. Whole blood lactate kinetics in patients undergoing quantitative resuscitation for severe septic shock. Chest. 2013;143:1548–1553. doi: 10.1378/chest.12-0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patient: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752–761. doi: 10.1164/rccm.200912-1918OC. [DOI] [PubMed] [Google Scholar]
- 10.Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106:562–568. doi: 10.1161/01.CIR.0000023891.80661.AD. [DOI] [PubMed] [Google Scholar]
- 11.Hayashida K, et al. Where effective lactate reduction over the first 6 hours of postcardiac arrest care was associated with survival and good neurologic outcome. Crit Care Med. 2017;45:e559–e566. doi: 10.1097/CCM.0000000000002307. [DOI] [PubMed] [Google Scholar]
- 12.Sakamoto T, Morimura N, Nagao K, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2014;85(6):762–768. doi: 10.1016/j.resuscitation.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Dalton HJ, Tucker D. Resuscitation and extracorporeal life support during cardiopulmonary resuscitation following the Norwood (stage 1) operation. Cardiol Young. 2011;21(Suppl 2):101–108. doi: 10.1017/S1047951111001673. [DOI] [PubMed] [Google Scholar]
- 14.Goto Y, Maeda T, Nakatsu-Goto Y, et al. Neurological outcomes in patients transported to hospital without a prehospital return of spontaneous circulation after cardiac arrest. Crit Care. 2013;17(6) [DOI] [PMC free article] [PubMed]
- 15.Cariou A, Nolan JP, Sunde K, et al. Ten strategies to increase survival of cardiac arrest patients. Intensive Care Med. 2015;41(10):1820–1823. doi: 10.1007/s00134-015-3788-z. [DOI] [PubMed] [Google Scholar]
- 16.Kolla S, Awad SS, Rich PB, Schreiner RJ, Hirschl RB, Bartlett RH. Extracorporeal life support for 100 adult patients with severe respiratory failure. Ann Surg. 1997;226:544–564. doi: 10.1097/00000658-199710000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rvers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


