Abstract
Scrophularia genus belonging to the family of Scrophulariaceae, is a medicinal plant widely distributed in Iran. In the present study, the anti-malarial activity of different extracts of three Iranian endemic species of Scrophularia including S. frigida, S. subaphylla and S. atropatana, was screened by an in-vitro preliminary assay. The plant materials were extracted successively with n-hexane, dichloromethane (DCM), and methanol (MeOH) at room temperature by soxhlet extractor. In order to assess anti-malarial activity of obtained extracts, cell free β-hematin formation assay was applied. Amongst the extracts, DCM extract of S. frigida exhibited remarkable anti-malarial activity with IC50 value of 0.67 ± 0.11 mg/mL. In contrast, MeOH and n-hexane extracts of all plants illustrated insignificant or moderate activity in this assay. Furthermore, preliminary phytochemical analysis along with TLC and GC-MS analysis of potent extract (DCM extract of S. frigida) were performed for more clarification. These methods revealed that the notable anti-malarial activity might be due to the presence of active constituents like methoxylated flavonoids, methylated coumarins, and diterpenoids. From the nine extracts of different species of Scrophularia, DCM extract of S. frigida showed potent inhibitory activity on β-hematin formation assay. Hence, it seems that it is noteworthy to concentrate on purifying the active chemical constituents of DCM extract and determining the pure anti-malarial components.
Key Words: Anti-malaria, Scrophularia species, Cell free assay, Preliminary phytochemical analysis, GC-MS
Introduction
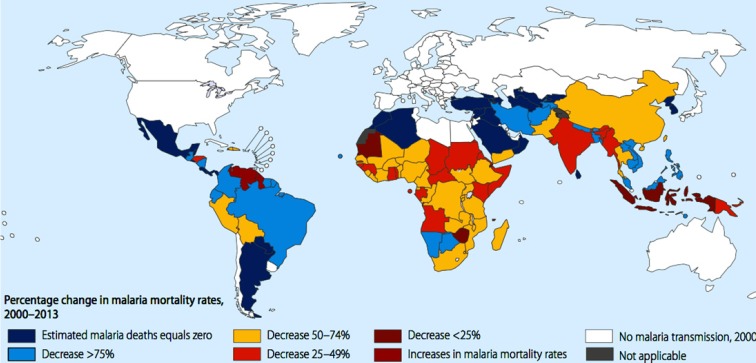
Malaria is one of the common protozoal diseases which was widespread in many parts of the world especially in the tropical and sub-tropical zones and caused mortality and morbidity in patients (Figure 1) (1, 2). This global disease is caused by the bite of the Anophel mosquito which infected the host by the intracellular parasitic protozoa of plasmodium species (3, 4). Malaria as one of the oldest and fatal parasitic ailment in Iran is responsible for killing more than 60% cases of patients especially in southeastern area (5).
Figure 1.
Percentage change in malaria mortality rates according to WHO estimation between 2000 to 2013.
Hence, a substantial number of drugs has been considered for debating against this killer disease in recent years (6-8). As an illustration, chloroquine as one of the most inexpensive and routine anti-malarial medications was designated for treatment of malaria (9). However, the emergence of widespread chloroquine-resistant species in some regions as well as incapability of suppressing all stages of the parasite encouraged the researchers to make considerable attempt in discovering novel sources of plant derived drugs with highly clinical efficacy (10-12). Subsequently, artemisinin was one of the top lists of these herbal medicinal products with an endoperoxide sesquiterpene lactone structure, derived from the plant Artemisia annua. It exerts its potent anti-malarial effect by suppressing all stages of parasite in different ways including blocking the degradation of hemoglobin and inhibiting of toxic heme biocrystalization. (7, 13 and 14). Although artemisinin-based combination therapy has been represented by successful results in clinical treatments, the appearance of artemisinin-resistant parasites has inclined researchers for finding a new source of anti-parasitic drugs as the alternative therapies (15, 16). As a continuation of our screening program on biological activities of Iranian plants (14, 17 and 18), we have now evaluated the anti- malarial effect of different extracts of three Scrophularia species. The genus Scrophularia (Scrophulariaceae), comprising about 300 species, is one of the largest and most popular herbs in folk medicines, distributed in the northern hemisphere, especially along the Mediterranean area, central Europe, Asia and North America (19). In Iran, 42 species are reported, 19 of which are considered as endemic taxa (19). Several activities were reported by these plants such as anti-inflammatory, antibacterial, immunomodulator, cardiovascular, diuretic, molluscicidal, anti-tumor, and anti-malarial. Moreover, various types of phenolic acids, iridoids, phenylpropanoids, flavonoids, saponins, and terpenoids were isolated from this genus that may cause the mentioned pharmacological effects (20-29). The aim of the present study is to screen the anti-malarial activity of different extracts of three Irainan endemic species of Scrophularia including S. frigida, S. subaphylla, and S. atropatana as well as the report of the preliminary phytochemical screening of potent extracts.
Experimental
Chemicals
Hematin porcine, chloroquine diphosphate, sodium dodecyl sulfate (SDS), sodium acetate, magnesium sulfate, sodium hydrogen phosphate, sodium chloride, potassium chloride, sodium hydroxide, glucose, and sodium bicarbonate were purchased from Sigma-Aldrich, chemical Company (United kingdom), oleic acid from Fluka (India), dimethylsulfoxide, hydrochloric acid. All the solvents used for extraction were purchased from Caledon (Canada).
Plant Material
The aerial parts of three Scrophularia species, S. frigida, S. subaphylla and S. atropatana were collected from East Azarbaijan province (Iran) during June-September 2012. After identification, voucher specimens numbered as Tbz-fPh-746, Tbz-fPh 747, and Tbz-fPh 748 respectively and also retained in the herbarium of the Faculty of Pharmacy, Tabriz University of Medical Sciences, Iran.
Extraction
All of the samples were Soxhlet-extracted with n-hexane, dichloromethane (DCM), and methanol (MeOH), successively (1 L each). All the extracts were concentrated using a rotary evaporator under 45 ºC.
TLC analysis of extracts
In the case of potent extract, important chemical groups were identified by TLC on silica gel 60 GF 254 Merck (layer thickness 0.25 mm) as follows: n-hexane/ethylacetate (70:30) was used as solvent system and then detected under UV 366 nm.
Cell free β-Hematin formation assay
The potential anti-malarial activity of plant extracts was evaluated by the method described by Afshar et al. (17) with some modifications. Briefly, varying concentrations (0–2 mg/mL in DMSO) of the different extracts were incubated with 3 mM of hematin, 10 mM oleic acid, and 1 M HCl. The final volume was well adjusted to 1 mL by adding sodium acetate buffer, pH 5. Subsequently, overnight incubation at 37 °C consistent with shaking was considered for samples. During this process, chloroquine diphosphate was used as a positive control. Then, the samples were centrifuged (14000 rpm, 10 min, at 21 °C) and 2.5% (w/v) SDS in phosphate buffered saline frequently added to samples in order to purify the hemozoin pellets (usually 3-8 washes). This process was followed by a final wash in 0.1 M sodium bicarbonate until the supernatant was clear. Finally, the pure pellets were dissolved in 1 mL of NaOH and the absorbance was measured at 400 nm by UV spectrophotometer. The results were recorded as % inhibition (I%) of heme polymerization/crystallization compared to positive control (chloroquine) using the following formula: I% = [(AN – AA)/AN] × 100, where AN: absorbance of negative control; AA: absorbance of test samples.
Preliminary Phytochemical Analysis
The extracts were tested for identifying the active chemical groups such as triterpenoids, steroids, glycosides, saponins, alkaloids, flavonoids, tannins, free amino acids, and carbohydrate by the following standard procedures.
Tests for steroids and triterpenoids
Few drops of acetic anhydride were mixed with sulfuric acid which was added from the sides of the test tubes then brown ring was appeared at the junction of two layers which was surrounded with green layer at the top and deep red layer at the down. This test indicated the presence of steroids and triterpenoids respectively (30-32).
Tests for cardiac glycosides
A) Kedd ΄s test: The plant extracts were mixed with 2-3 drops of 2% 3, 5-dinitro benzene carboxylic acid. Then, 20% NaOH was added to make the solutions in alkali range. Finally, the appearance of purple color illustrated the presence of β-unsaturated lactones which gave positive response to the test (30).
B) Keller-killiani test: The mixture of glacial acetic acid and ferric chloride were added to dried test solutions. Detection of the color changed to bluish green in upper layer and reddish in down layer occurred after adding the concentration H2SO4, slowly by the side of the test tubes (30).
Tests for alkaloids
A) Dragendorff’s test: The development of reddish brown turbidity in the presence of Dragendorff reagent was indicative of the presence of alkaloids (30).
B) Hagerʹs test: 2-3 drops of Hager reagent were added to the extract tubes to observe yellow turbidity in the presence of alkaloids (30).
Test for tannins and phenolic compounds: Blue green color was appeared after adding Ferric chloride to the test solutions (30, 32).
Test for flavonoids (Shinoda test)
After adding the mixture of Magnesium pieces and concentrated HCl to the samples, the red color was appeared (32).
Test for amino acids (Ninhydrin test)
The presence of free amino acids was resulted from the formation of purple color, when the solutions were boiled with 0.2% ninhydrin solution (30).
Test for carbohydrate
(Benedict’s test): The solution was treated with amount of Benedict’s reagent (alkaline solution containing cupric citrate complex), then boiling on water bath, reddish brown turbidity appeared if reducing sugars are present (30).
Test for iridoids
One mL of Trim-Hill reagent was added to the different extracts and then was heated for a few min. A blue-green or red color indicated the presence of iridoids (34).
GC-MS Analysis of potent extract
GC–MS analyses were carried out on a Shimadzu QP-5050A GC–MS system equipped with a DB-1 fused silica column (60 m × 0.25 mm i.d., film thickness 0.25 μm). For nonpolar extracts oven temperature, rising from 50 °C to 230 °C at a rate of 4 °C/min and then rising from 230 °C to 310 °C at a rate of 1.5 °C/min, injector temperature, 280 °C; carrier gas, helium at a flow rate of 1.3 mL/min; split ratio, 1:10; ionization energy, 70 eV; scan time, 1 sec; mass range, 30–600 amu.
Identification of components
Identification of the constituents was based on direct comparison of the retention times and mass spectral data with those for standard alkanes and computer matching with the NIST 21, NIST 107 and WILEY229 library, as well as by comparison of the fragmentation patterns of the mass spectra with those reported in the literature (35).
Statistical analysis
All measurements were expressed as the Mean ± SD in triplicate manner. Excel 2010 was employed for analyzing data. The IC50 value was calculated from nonlinear regression analysis.
Results
Cell free β-hematin formation assay results
The results of cell free β-hematin formation assay which was carried out on three different extracts of three Scrophularia species were compiled in Table 1 and Figure 2. MeOH extracts of all specimens including S. frigida, S. subaphylla and S. atropatana showed no anti-malarial activity, while all DCM extracts exhibited potent anti-malarial effect with IC50 values of 0.67 ± 0.11, 0.99 ± 0.04 and 1.07 ± 0.07 mg/mL, respectively, in comparison to positive control (chloroquine, IC50 = 0.014 ± 0.003 mg/mL). Moreover, medium potencies were illustrated by n-hexane extracts with IC50 values of 1.12 ± 0.10, 5.74 ± 2.80, and 1.35 ± 0.20 mg/mL), respectively. Amongst the extracts, DCM extract of S. frigida illustrated the most potent anti-malarial activity.
Table 1.
The 50% and 90% of inhibition concentrations (mg/mL) of extracts of three Scrophularia species in 𝛽-hematin formation assay
| Plants | Extracts | Yield (%) | IC 50 (mg/mL) | IC 90 (mg/mL) |
|---|---|---|---|---|
| Scrophularia frigida | n-hexane | 3.6 | 1.12 ± 0.10 | 1.36 ± 0.028 |
| DCM | 3.52 | 0.67 ± 0.11 | 1.55 ± 0.100 | |
| MeOH | 12.13 | - | - | |
| Scrophularia subaphylla | n-hexane | 3.49 | 5.74 ± 2.81 | 7.94 ± 2.57 |
| DCM | 5.56 | 0.99 ± 0.04 | 2.02 ± 0.105 | |
| MeOH | 13.24 | - | - | |
| Scrophularia atropatana | n-hexane | 2.24 | 1.35 ± 0.20 | 2.32 ± 0.21 |
| DCM | 6.32 | 1.07 ± 0.07 | 1.59 ± 0.021 | |
| MeOH | 14.23 | - | - | |
| Chloroquine | - | - | 0.014 ± 0.003 | 0.163 ± 0.004 |
Experiment was performed in triplicate and expressed as Mean ± SD.
Figure 2.
Comparison of IC50 and IC90 values (mg/mL) of active extracts of S. frigida, S. subuphylla, S. atropatana and chloroquine solution in β-hematin formation assay. The values were reported as Mean ± SD
Phytochemical analysis results
In order to confirm our antimalarial results, preliminary phytochemical analysis, TLC, and GC-MS analysis were performed. Based on phytochemical analysis data (Table 2), high amounts of flavonoids and terpenoids in DCM extract (as a potent extract) and steroids in n-hexane extract (as a medium potent extract) of S. frigida were demonstrated. Furthermore, the presence of cardiac glycosides with their steroidal moiety might be effective in the potency of DCM and n-hexane extracts. In addition, it is assumed that the flavonoids and coumarins which existed in DCM extract may be lipophilic types (for instance, methoxylated or methylated things). Furthermore, according to Table 3, GC-MS analysis of volatile parts of DCM and n-hexane extracts showed high amounts of diterpenoids and steroids in S. frigida, respectively.
Table 2.
Phytochemical characteristics for various extracts of three different species of Scrophularia
| Phytochemical tests |
n-hexane extract
|
DCM extract
|
MeOH extract
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| S. f | S. s | S. a | S. f | S. s | S. a | S. f | S. s | S. a | ||
| Alkaloids | Dragendorff’s Test | - | - | - | - | - | - | + | - | - |
| Hager’s Test | - | - | - | - | - | - | + | - | - | |
| Cardiac Glycosides | Kedd | +++ | +++ | +++ | +++ | +++ | +++ | - | - | - |
| Keller-killiani | - | + | + | - | +++ | - | - | - | ||
| Tannins | Ferric Chloride Test | - | - | - | - | - | - | +++ | +++ | +++ |
| Flavonoids | Shinoda Test | - | - | - | ++ | - | - | +++ | +++ | +++ |
| Proteins and Amino Acids |
Ninhydrin Test | - | - | - | - | - | - | - | - | - |
| Sterol | Libermann-Buchard test | +++ | + | + | - | +++ | + | - | - | - |
| Terpenoid | Libermann-Buchard test | - | - | - | +++ | ++ | + | - | - | - |
| Carbohydrate | Benedict's test | - | - | - | - | - | - | + | + | + |
| Iridoids | Trim-Hill | - | - | - | - | - | - | + | + | + |
S. f = S. frigida; S. s = S. subaphylla; S. a = S. atropatana; MeOH = methanol; DCM = dichloromethane.
Table 3.
Volatile components of DCM and n-hexane extracts in three species of Scrophularia
| Extracts | Total identified content (%) | Compound (content %) |
|---|---|---|
| DCM | ||
| S. atropatana | 95.33 | n-alkanes (84.92%), diterpene (1.3%), fatty acids and their derivatives (8.17%), heterocyclic hydrocarbons (0.94%) |
| S. frigida | 95.95 | diterpene (69.02%), fatty acid (26.91%) |
| S. subaphylla | 74.65 | diterpene (59.87%), linear alcohol (9.33%), fatty acid (5.45%) |
| n-hexane | ||
| S. atropatana | 95.04% | oxygenated monoterpens (14.76%), fatty acid (2.42%), alkanes (77.86%) |
| S. frigida | 96.13% | Fatty acids and their derivatives (46.96%), alkanes (39.73%), linear ketone (1.22%), steroids (8.22%) |
| S. subaphylla | 80.09% | fatty acid (1.83 %), alkanes (78.26%) |
Discussion
The Plasmodium parasite attacks the host erythrocyte in order to utilize hemoglobin for synthesizing the essential requirements for developing and proliferating (36, 37). During this process, a massive amount of heme is generated as a toxic undesired byproduct which is pernicious for malaria parasite. Therefore, to protect itself, the parasite neutralizes large amounts of heme to hemozoin or water-insoluble malaria pigment via the bio crystallization process. Hence, inhibition of hemozoin formation by means of antimalarial compounds like artemisinin and 4-aminoquinolines derivatives (quinine, mefloquine and chloroquine) is regarded as an incomparable target to combat the malaria (14, 38). Despite of the available drugs, researchers have decided to screen the plants for discovering the novel natural sources especially from endemic flora (39). Hence, in this current study, three endemic species of Scrophularia were selected for evaluating their anti-malarial activities. Obtained results revealed that the MeOH extracts of all plants did not show any significant anti-malarial activities whereas the DCM and n-hexane extracts of all aerial parts indicated high to moderate anti-malarial potency in comparison with the reference control. Amongst them, DCM extract of S. frigida showed remarkable anti-malarial activity. It seems that potent effect of DCM extract from S. frigida on inhibiting the hemozoin formation was may be due to the presence of high amounts of flavonoids and terpenoids as resulted from the preliminary phytochemical analysis (Table 2). Moreover, TLC analysis indicated the presence of methylated coumarins and methoxylated flavonoids in DCM extract of S. frigida in comparison with the reference book (40). Our findings are parallel with the prior investigations which exhibited anti-plasmodial activity of methoxylated flavonoids (41), methylated coumarins (42) and terpenes (43-46) in various anti-malarial assays. Furthermore, in previous studies on Scrophularia genus, antimalarial activity of some species was demonstrated (23, 28). In addition, GC-MS analysis of DCM extracts of three species were performed for determining the probable anti-malarial volatile compounds (Table 3). In the case of S. atropatana, n-alkanes comprised the highest proportion while in two other species diterpenes were identified as the major constituents. Hence, it could be supposed that diterpenes as the major active compounds are responsible for the potent activity of those extracts (43). Additionally, among the n-hexane extracts, the anti-malarial effect of n-hexane extract of S. frigida was found to be more potent than the others. Likewise, although the preliminary phytochemical screening indicated the presence of steroid derivatives in all n-hexane extracts, (Table 2), a considerable quantity of steroids in n-hexane extract of S. frigida could explain the potent activity of this extract. Furthermore, GC-MS analysis of this extract was in line with the findings of phytochemical analysis (Table 3).
However, IC50 value of this extract was higher than negative control which might be due to the existence of high amounts of fatty acids and lipids leads to synergistic effect with oleic acid and conceal the authentic anti-malarial potency of the extract in this assay. Hence, antimalarial activity of this extract could be increased by removing fatty acids (14). Likewise, anti-malarial activity of steroids was illustrated previously in other plants (43, 44). In the case of n-hexane extract of S. atropatana, moderate antimalarial effect in comparison to others and positive control might be due to the presence of oxygenated monoterpenes in volatile part (43).
Conclusion
Based on this preliminary study, among the various polarity extracts of three different plants, DCM extract of S. frigida showed the significant anti-malarial activity on β-hematin formation assay. These results encouraged us to concentrate on isolating the active anti-malarial chemical constituents and studying further on animal models for in-vivo evaluation.
Acknowledgment
This study was financially supported by grant No. 92/1114 from the Drug Applied Research Center, Tabriz University of Medical Sciences. This article was written based on data set of PhD thesis registered in Tabriz University of medical sciences (No. 95).
References
- 1.Bilia AR, Lazari D, Messori L, Taglioli V, Temperini C, Vincieri FF. Simple and rapid physico-chemical methods to examine action of antimalarial drugs with hemin: Its application to Artemisia annua constituents. Life Sci. 2002;70:769–78. doi: 10.1016/s0024-3205(01)01447-3. [DOI] [PubMed] [Google Scholar]
- 2.Rathore D, Jani D, Nagarkatti R, Kumar S. Heme detoxification and antimalarial drugs–Known mechanisms and future prospects. Drug Discov. Today Ther. Strateg. 2006;3:153–8. [Google Scholar]
- 3.Goodarzi S, Nateghpour M, Asgharian P, Hadjiakhoondi A, Yassa N, Tavakoli S, Mirzaei J, Farivar L, Motevalli A, Tofighi Z. Antimalarial and cytotoxic activities of roots and fruits fractions of Astrodaucus persicus extract. Iran. J. Basic Med. Sci. 2017;20:1319–23. doi: 10.22038/IJBMS.2017.9554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malaguarnera L, Musumeci S. The immune response to Plasmodium falciparum malaria Lancet Infect. Dis. 2002;2:472–8. doi: 10.1016/s1473-3099(02)00344-4. [DOI] [PubMed] [Google Scholar]
- 5.Ostovar A, Raeisi A, Haghdoost A, Ranjbar M, Rahimi A, Sheikhzadeh K. Lessons learnt from malaria epidemics in the Islamic Republic of Iran. East. Mediterr. Health J. 2012;18:864–9. doi: 10.26719/2012.18.8.864. [DOI] [PubMed] [Google Scholar]
- 6.Sharma U, Srivastava K, Puri SK, Singh C. Amino steroids as antimalarial agents. J. Med. Chem. Res. 2008;17:326–4. [Google Scholar]
- 7.Odugbemi TO, Akinsulire OR, Aibinu IE, Fabeku PO. Medicinal plants useful for malaria therapy in Okeigbo, Ondo State, Southwest Nigeria. Afr. J. Tradit. Complement. Altern. Med. 2008;4:191–8. doi: 10.4314/ajtcam.v4i2.31207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper R, Magwere T. Chloroquine: Novel uses and manifestations. Indian J. Med. Res. 2008;127:305. [PubMed] [Google Scholar]
- 9.Sullivan DJ, Gluzman IY, Russell DG, Goldberg DE. On the molecular mechanism of chloroquineʹs antimalarial action. Proc. Natl. Acad. Sci. 1996;93:11865–70. doi: 10.1073/pnas.93.21.11865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishih A, Ikeya C, Yanoh M, Takezoe H, Miyase T, Terada M. A potent antimalarial activity of Hydrangea macrophylla var Otaksa leaf extract against Plasmodium yoelii 17XL in mice. Parasitol Int. 2001;50:33–9. doi: 10.1016/s1383-5769(00)00069-6. [DOI] [PubMed] [Google Scholar]
- 11.Wellems TE, Plowe CV. Chloroquine-resistant malaria. Infect. Dis. 2001;184:770–6. doi: 10.1086/322858. [DOI] [PubMed] [Google Scholar]
- 12.Bloland PB Organization WHO. Drug resistance in malaria. Geneva: World Health Organization; 2001. [Google Scholar]
- 13.Mueller MS, Karhagomba I, Hirt HM, Wemakor E. The potential of Artemisia annua L as a locally produced remedy for malaria in the tropics: Agricultural, chemical and clinical aspects. J. Ethnopharmacol. 2000;73:487–93. doi: 10.1016/s0378-8741(00)00289-0. [DOI] [PubMed] [Google Scholar]
- 14.Asgharian P, Delazar A, Lotfipour F, Asnaashari S. Bioactive properties of eremostachys macrophylla Montbr & Auch Rhizomes growing in Iran. Pharm.Sci. 2017;23:238–43. [Google Scholar]
- 15.Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J. Artemisinin resistance in Plasmodium falciparum malaria. N. Eng. J. Med. 2009;361:455–67. doi: 10.1056/NEJMoa0808859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Astelbauer F, Gruber M, Brem B, Greger H, Obwaller A, Wernsdorfer G. Activity of selected phytochemicals against Plasmodium falciparum. Acta Trop. 2012;123:96–100. doi: 10.1016/j.actatropica.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Asnaasharia S, Delazar A, Asgharian P, Lotfipour F, Bamdad S, Heshmati F. In-vitro bioactivity and phytochemical screening of extracts from rhizomes of eremostachys azerbaijanica rech f Growing in Iran. Iran. J. Pharm. Res. 2017;16:306–14. [PMC free article] [PubMed] [Google Scholar]
- 18.Heshmati F, Asgharian P, Khodaie L, Delazar A, Lotfipour F. Anti-proliferative and antimicrobial activity of artemisia spicigera methanolic extract and SPE fractions. Jundishapur J. Nat. Pharm. Prod. 2017;12:e36903. [Google Scholar]
- 19.Mozaffarian V. A dictionary of Iranian plant names: Latin, English, Persian. 4rd ed. 1996. p. 495. [Google Scholar]
- 20.Nikkhah E, Heshmati F, Babaei H, Asgharian P, Delazar A. Evaluation of phytochemistry and some biological activities of aerial parts and seeds of Scrophularia umbrosa Dumort. (In Press, Accepted for publication in Jundishapour Journal of Natural Pharmaceutical Products. [Google Scholar]
- 21.Stevenson PC, Simmonds MS, Sampson J, Houghton PJ, Grice P. Wound healing activity of acylated iridoid glycosides from Scrophularia nodosa. Phytother. Res. 2002;16:33–5. doi: 10.1002/ptr.798. [DOI] [PubMed] [Google Scholar]
- 22.Garjani A, Vaez H, Delazar A, Rameshrad M, Heshmati F, Asgharian P. Cardioprotective effects of methanolic extract of Scrophularia frigida on ischemia-reperfusion-induced injuries in isolated rat heart. Iran. J. Pharm. Res. 2017;16 (Special Issue):35–45. [PMC free article] [PubMed] [Google Scholar]
- 23.Asgharian P, Heshmati Afshar F, Asnaashari S, Bamdad S, Delazar A. The seasonal variations of the chemical composition of essential oil obtained from Scrophularia frigida. J. Nat. Pharm. Prod. 2016;11:e29742. [Google Scholar]
- 24.Vaez H, Garjani A, Delazar A, Rameshrad M, Toutounchi N, Asgharian P. Effects of methanolic extract of Scrophularia subuphylla on ischemia and reperfusion-induced myocardial injury. (In Press, Accepted to publication in Pharmaceutical Sciences. [Google Scholar]
- 25.Tofighi Z, Asgharian P, Goodarzi S, Hadjiakhoondi A, Ostad SN, Yassa N. Potent cytotoxic flavonoids from Iranian Securigera securidaca. Med. Chem. 2014;23:1718–23. [Google Scholar]
- 26.Asgharian P, Heshmati F, Asnaashari S, Bamdad S, Ebrahimi F, Delazar A. Characterization of terpenoids in the essential oils extracted from the aerial parts of Scrophularia subaphylla growing in Iran. Adv. Pharm. Bull. 2015;5:557–61. doi: 10.15171/apb.2015.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delazar A, Nazemiyeh H, Heshmati F, Barghi N, Esnaashari S, Asgharian P. Chemical compositions and biological activities of Scutellaria pinnatifida A. Hamilt aerial parts. Res. Pharm. Sci. 2017;12:187–95. doi: 10.4103/1735-5362.207199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tasdemir D, Güner ND, Perozzo R, Brun R, Dönmez AA, Calıs I. Anti-protozoal and plasmodial FabI enzyme inhibiting metabolites of Scrophularia lepidota roots. Phytochem. 2005;66:355–62. doi: 10.1016/j.phytochem.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Yaripour S, Delnavazi MR, Asgharian P, Valiyari S, Tavakoli S, Nazemiyeh H. A Survey on phytochemical composition and biological activity of zygophyllum fabago from Iran. Adv. Pharm. Bull. 2017;7:109–14. doi: 10.15171/apb.2017.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asgharian P, Heshmati F, Asnaashari S, Lotfipour F, Baradaran B, Zolali E, Nikkhah E, Delazar A. Evaluation of various biological activities of the aerial parts of Scrophularia frigida growing in Iran. Iran. J. Pharm. Res. 2017;16:277–89. [PMC free article] [PubMed] [Google Scholar]
- 31.Nikkhah E, Heshmati F, Babaei H, Asgharian P, Delazar A. Phytochemical analysis and in-vitro bioactivity of Scrophularia umbrosa rhizome (Scrophulariaceae) ( Inpress, Accepted to publiction in Iranian Journal of Pharmaceutical Research. [PMC free article] [PubMed] [Google Scholar]
- 32.Kumara KN, Bulugahapitiya V. A preliminary chemical study on secondary metabolites present in fruits of. Proceedings of the second academic sessions. 2004:92–7. [Google Scholar]
- 33.Avinash DK, NandaWaman S. phytochemical constituents of leaves of celastrus paniculatus wild: Endangered medicinal plant. Inter. J. Pharmacog. Phytochem. Res. 2014;6:792–4. [Google Scholar]
- 34.Srinivas P, Samatha T, Valya G, Ragan A, Swamy NR. Phytochemical screening and antimicrobial activity of leaf extract of Wrightia tomentosa. Int. Res. J. Biol. Sci. 2013;2:23–7. [Google Scholar]
- 35.Adams R. Quadrupole mass spectra of compounds listed in order of their retention time on DB-5 Identification of essential oils components by gas chromatography/quadrupole mass spectroscopy. Allured Publishing Corporation, Carol. Stream, IL, USA. 2001 [Google Scholar]
- 36.Goldberg DE, Slater A, Cerami A, Henderson GB. Hemoglobin degradation in the malaria parasite Plasmodium falciparum: An ordered process in a unique organelle. Proc. Natl. Acad. Sci. U. S. A. 1990;87:2931–5. doi: 10.1073/pnas.87.8.2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huy NT, Uyen DT, Sasai M, Shiono T, Harada S, Kamei K. A simple and rapid colorimetric method to measure hemozoin crystal growth in-vitro. Anal. Biochem. 2006;354:305–7. doi: 10.1016/j.ab.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Bandyopadhyay U, Dey S. Antimalarial drugs and molecules inhibiting hemozoin formation. Apicomplexan parasites. Molecular approaches toward targeted drug development. 3rd ed. England : Wiley Online Library; 2011. pp. 205–34. [Google Scholar]
- 39.Vargas S, Ioset KN, Hay AE, Ioset JR, Wittlin S, Hostettmann K. Screening medicinal plants for the detection of novel antimalarial products applying the inhibition of β-hematin formation. J. Pharm. Biomed. Anal. . 2011;56:880–6. doi: 10.1016/j.jpba.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 40.Wagner H. Plant drug analysis: A thin layer chromatography atlas. Springer Science & Business Media ; 1996. [Google Scholar]
- 41.Tona L, Cimanga R, Mesia K, Musuamba C, De Bruyne T, Apers S. In-vitro antiplasmodial activity of extracts and fractions from seven medicinal plants used in the Democratic Republic of Congo. J. Ethnopharmacol. 2004;93:27–32. doi: 10.1016/j.jep.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 42.Muregi FW, Ishih A, Miyase T, Suzuki T, Kino H, Amano T. Antimalarial activity of extracts from plants used in Kenyan ethnomedicine and their interactions with chloroquine (CQ) against a CQ-tolerant rodent parasite, in mice. J. Ethnopharmacol. 2007;111:190–5. doi: 10.1016/j.jep.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 43.Kraft C, Jenett-Siems K, Siems K, Jakupovic J, Mavi S, Bienzle U. In-vitro antiplasmodial evaluation of medicinal plants from Zimbabwe. Phytother. Res. 2003;17:123–8. doi: 10.1002/ptr.1066. [DOI] [PubMed] [Google Scholar]
- 44.Zolali E, Asgharian P, Hamishehkar H, Kouhsoltani M, Khodaii H, Hamishehkar H. Effects of gamma oryzanol on factors of oxidative stress and sepsis-induced lung injury in experimental animal model. Iran. J. Basic Med. Sci. 2015;18:1258–63. [PMC free article] [PubMed] [Google Scholar]
- 45.Mojarrab M, Naderi R, Heshmati F. Screening of different extracts from artemisia species for their potential antimalarial activity. Iran. J. Pharm. Res. 2015;14:603–8. [PMC free article] [PubMed] [Google Scholar]
- 46.Asnaashari S, Heshmati F, Bamdad S, Delazar A. Evaluation of in-vitro antimalarial activity of different extracts of eremostachys. Iran. J. Pharm. Res. 2016;15:523–29. [PMC free article] [PubMed] [Google Scholar]