Highlights
-
•
Rarity of the site of occurance.
-
•
Innocuous clinical presentation.
-
•
Conservative surgical approach.
-
•
Long follow up period with no recurrence.
Keywords: Case report, Excision, Maxilla, Surgery
Abstract
Introduction
Central Giant Cell Granuloma (CGCG) is an intraosseous lesion consisting of cellular fibrous tissue that contains multiple foci of hemorrhage, aggregations of multinucleated giant cells and occasionally trabeculae of woven bone1.
Presentation of case
we are presenting a case of Central Giant Cell Granuloma on Maxilla. Extra oral examination revealed a diffuse swelling on the left side of face causing slight obliteration of nasio − nasolabial labial fold resulting in facial asymmetry & Intraoral examination shows a purple expansile mass in the region of upper left 26, 27 and 28 edentulous areas.
Discussion
Giant Cell Granuloma is a rare bony lesion in the Head and Neck region. It is a non-odontogenic tumor never seen in any other bone of the skeleton. It most commonly affects maxilla followed by the mandible.
Conclusion
There is no recurrence after a long follow up period. We concluded that conventional excision is to be considered as a best method to treat central giant cell granuloma.
1. Introduction
Central giant cell granuloma (CGCG) is an intraosseous lesion consisting of cellular fibrous tissue that contains multiple foci of hemorrhage, aggregations of multinucleated giant cells and occasionally trabeculae of woven bone [1]. CGCG, as described by Jaffe in 1953, is an idiopathic non-neoplastic proliferative lesion [2]. The term reparative giant cell granuloma at one time was widely accepted, as CGCG was considered primarily to be a local reparative reaction of bone, possibly to intramedullary hemorrhage or trauma. The use of the term reparative has subsequently been discontinued since the lesion represents essentially a destructive process [3]. Although its etiology and pathogenesis is unknown, its histology and clinical behaviour has been studied in detail [4], [5], [6], [7]. Recently the World Health Organization has defined it as localized benign but sometimes aggressive osteolytic proliferation consisting of fibrous tissue with hemorrhage and haemosiderin deposits, presence of osteoclast-like giant cells and reactive bone formation [8]. Giant Cell Granuloma is a rare bony lesion in the Head and Neck region and It is a non-odontogenic tumor never seen in any other bone of the skeleton. Most commonly affects maxilla followed by the mandible. Although benign, it can locally be destructive. Surgery is the most accepted method of treating the condition. The case history reported here presented with a giant cell lesion that involved the left maxilla.
2. Case report
A 48 years old female patient reported to the department of oral and maxillofacial surgery with the complaint of swelling in left upper jaw since one year.
Complete case history revealed that the swelling started as small size and progressively increased to the present size over a period of one year. In the last one year patient had sought treatment from his family dentist who extracted her 26,27 and 28 but the swelling persisted even after extraction. There was no history of trauma, neurological deficit, fever, loss of apetite, loss of weight, nasal discharge or difficulty in swallowing. Patient was systemically healthy. Medical and family histories also not reveal any abnormalities.
Extra oral examination revealed a diffuse swelling on the left side of face causing slight obliteration of nasilabial fold resulting in facial asymmetry. The overlying skin was normal and temperature was normal. There was no associated lymphadenopathy. The swelling was firm in consistency and was slight tender on palpation.
Intraoral examination shows a purple expansile mass in the region of upper left 26,27 and 28 edentulous areas. The swelling was in labialbuccal aspect extending from 24 to 28 area obliterating the buccal vestibule. The swelling had smooth surface,firm and slightly tender on palpation. There was also expansion of palate to the midline of palate mediolaterally and anteroposteriorly from 25 till 28 region.
An orthopantomogram(OPG) and computed tomography(CT) scan revealed a soft tissue mass completely obliterating the left maxillary antrum with thinning and destruction of parts of the walls with generalized opacities. The mass extended inferiorly into the body of maxilla upto alveolus. Medioinferiorlyit reached the midline of maxilla. Medially it involved left lateral nasal wall & posteriorly till the lateral and medial pterygoid plates and superiorly upto the floor of orbit.
Routine haematological and urine examination were normal. Aspiration was negative which confirm solid tumor. The serum chemistry of calcium, phosphorus, parathyroid hormone was normal.
On the basis of clinical and radiological examination a provisional differential diagnosis of radicular cyst, Adenomatoid odontogenic tumour (AOT), calcifying epithelial odontogenic cyst (CEOC), desmoplastic ameloblastoma, fibrous dysplasia and Central Giant Cell Granuloma was made.
Biopsy was done under local anesthesia and good amount of bleeding was encountered suggesting of high vascularity of lesion. Histopathological examination of the specimen revealed connective tissue made of mature collagen fibres,fibroblasts and shows numerous multinucleated giant cells with foci of osseous structures suggestive of CGCG.
The case was planned for surgery under general anesthesia. Through the intraoral approach the lesion was exposedlabially from 22 area to 28 region. Enucleation with extensive curettage was done. Good amount of bleeding was encountered during the procedure. Maxillary sinusand Palatal region was extensively curetted taking care not to injure the greater palatine vessels while curetted the palatal region. There was a destruction of anterior sinus wall and lateral wall of nose. Extraction of 24 and 25 was done. Hemostasis was achieved and the entire curetted area was packed with betadine gauze. The pack was removed after 48 hours hrfrom the extracted socket site. Two units of blood was transfused as the haemoglobin level post operatively had dropped to 7gm%. Mild nasal bleeding was present for 2–3 days which was clotted blood from maxillary sinus. No signs of recurrence was found in 6 months period of follow up (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7 ).
Fig. 1.
Swelling in upper left back tooth region wrt 26, 27, 28.
Fig. 2.
CBCT (coronal view) shows erosion of lateral wall of nose.
Fig. 3.
CBCT (axial section) shows encroachment of entire maxillary sinus.
Fig. 4.
Shows pre − operative intra − oral view.
Fig. 5.
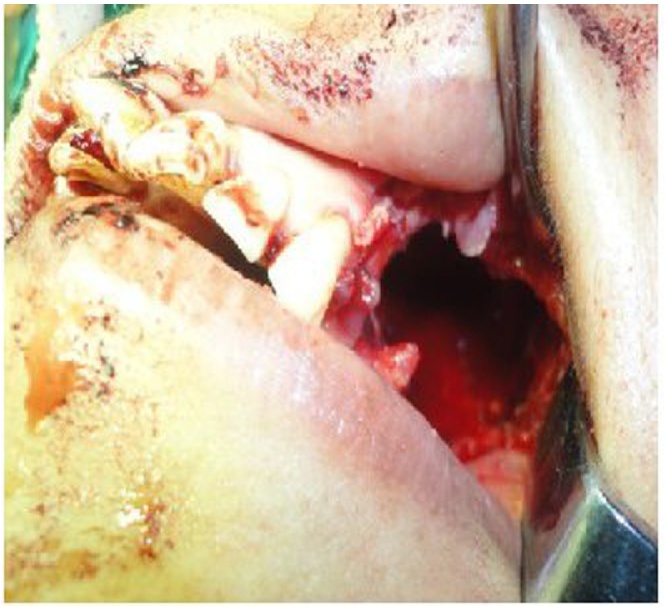
Shows peri-operative intra − oral view.
Fig. 6.
Shows post-operative intra-oral view.
Fig. 7.
Shows post-operative intra-oral view after suture.
3. Discussion
Giant Cell Granuloma is a rare bony lesion in the Head and Neck region. It is a non-odontogenic tumor never seen in any other bone of the skeleton. It most commonly affects maxilla followed by the mandible.Although benign, it can locally be destructive.Surgery is the most accepted method of treating the condition [2].
World Health Organization defines it as an intra-osseous lesion consisting of cellular fibrous tissue and contains many foci of hemorrhage, aggregations of multinucleated giant cells and occasionally trabeculae of woven bone [18].
Frequently it is only a painless swelling, but growth in some cases is so rapid and the mass can also rarely erode through bone particularly of the alveolar ridge to produce a soft tissue swelling [17]. It can occur at any age but presents most frequently inthe 2nd and 3rd decades and involves the maxillamore than the mandible [19]. It is twice as frequent infemales [17].
Despite the fact that the course of the disease is considered benign, there stillexist some reports in literature where metastasis has been observed [20].
Furthermore malignant transformations to osteosarcoma or fibrosarcoma have been reported [16]. Histologically, it is indistinguishable from other giant cell lesions of the bone like cherubis and aneurysmal bone cyst. Giant cell granuloma forms a lobulated mass of proliferative vascular forms a lobulated mass of proliferative vascular connective tissue packed with giant cells. These giant cells are seen lying in vascular stroma [19].
These giant cells have a patchy distribution and signs of bleeding into the mass and deposits of hemosidrin are frequently seen [17]. Ultra structurally the proliferating cells include spindle-shaped fibroblasts myofibroblasts and inflammatory mononuclear cells [23]. Sparse strands of collagen fibres partly subdivide the lesion which may contain a few trabeculae of osteoid or bone [19].
Surgery is the most accepted and traditional form of treatment. However, tissue removal rangesfrom simple curettage to bloc resection [22]. Radiation therapy in such a case is contraindicated [21]. There havebeen cases reported in which radiation treated lesions have undergone malignant transformation [24].
CGCG, as described by Jaffe in1953, is an idiopathic non-neoplastic proliferative lesion [4]. The term reparative giant cell granuloma at one time was widely accepted, asCGCG was considered primarily to be a local reparative reaction of bone, possibly to intramedullary hemorrhage or trauma. The use of the term reparative has subsequently been discontinued since the lesion represents essentially a destructive process [14].
Usually surgical curettage employed for smaller lesions but for aggressive lesions, en block resection is used as in our case. Recently weekly intralesional corticosteroid injections, daily subcutaneous administration of calcitonin and the use of interferon alpha have also been suggested as possible treatments for large or multiple lesions to avoid the need for mutilating surgery in growing children. The main drawback to these nonsurgical approaches is the need for continual treatment over a prolonged time period.
Conflicts of interest
Not applicable.
Funding
Not applicable.
Ethical approval
Not applicable.
Consent
Consent given by the patient.
Author contribution
Study concept or design & data collection, Proof reading & necessary changes − dr. Priyanka Garg.
Data analysis or interpretation — Dr. Jinendra Jain.
Writing paper — Dr. Nayana De and Dr. Kushal Chatterjee.
Guarantor
Dr. Ishank Singhal.
References
- 1.Hooman Ebrahimi et al., Central Giant Cell Granuloma of the Posterior Maxilla: A Case Report Received 27 January 2008; Accepted 6, March, 2008. [DOI] [PMC free article] [PubMed]
- 2.Uzbek Usman Haider, Mushtaq Iram. Case reportgiant cell granuloma of the maxilla. J. Ayub Med. Coll. Abbottabad. 2007;19(3):93. [PubMed] [Google Scholar]
- 3.Cossío Pedro Infante. Recurrent central giant cell granuloma in the mandible: surgical treatment and dental implant restoration. Med. Oral Patol. Oral Cir. Bucal. 2007;12:E229–E232. [PubMed] [Google Scholar]
- 4.De Lange J., Van den Akker H.P. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005;99:464–470. doi: 10.1016/j.tripleo.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 5.De Lange J., van den Akker H.P. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005;99:464–470. doi: 10.1016/j.tripleo.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Barnes L., Eveson J.W., Reichart P., Sidransky D. Pathology andGenetics of head and neck tumours. In: Kleihues P., Sobin L.H., editors. World Health Organization Classification of Tumours. IARC Press; Lyon, France: 2005. p. 324. [Google Scholar]
- 7.Kurtz M., Mesa M., Alberto P. Treatment of a central giant cell lesion of the mandible with intralesionalglucocorticosteroids. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001;91:636–637. doi: 10.1067/moe.2001.115721. [DOI] [PubMed] [Google Scholar]
- 8.Kaban L.B., Mulliken J.B., Ezekowitz R.A., Ebb D., Smith P.S., Folkman J. Antiangiogenic therapy of a recurrent giant cell tumor of the mandible with interferon alfa −2a. Pediatric. 1999;103:1145–1149. doi: 10.1542/peds.103.6.1145. [DOI] [PubMed] [Google Scholar]
- 14.Cohen M.A., Hertzanu Y. Radiologic features, including those seen with computed tomography of central giant cell granuloma of the jaws. Oral Surg. Oral Med. Oral Pathol. 1998;65:255–261. doi: 10.1016/0030-4220(88)90176-4. [DOI] [PubMed] [Google Scholar]
- 16.Thompson S.H., Bischoff P., Bender S. Central giant cell granuloma of the mandible. J. Oral Maxillofac. Surg. 1983;41(11):743–746. doi: 10.1016/0278-2391(83)90192-1. [DOI] [PubMed] [Google Scholar]
- 17.Cawson R.A., Odell E.W. 7th ed. Churchill Livingstone; 2002. Cawson’s Essentials of Oral Medicine and Pathology; pp. 135–136. [Google Scholar]
- 18.Kramer I.R.H., Pindborg J.J., Shear M. 2nd ed. Springer-Verlag; Berlin: 1991. Histological Typing of Odontogenic Tumors. [Google Scholar]
- 19.Soames J.V., Southam J.C. 3rd ed. Oxford University Press; 1998. Oral Pathology; pp. 312–313. [Google Scholar]
- 20.Small G.S., Rowe N.H. A true giant cell tumor in the mandible. J. Oral Surg. 1975;33:296–301. [PubMed] [Google Scholar]
- 21.Shafer W.G., Hine M.K., Levy B.M. WB Saunders Company; Philadelphia: 1983. A Text Book of Oralpathology; pp. 146–149. [Google Scholar]
- 22.Bataineh A.B., Al-Khateeb T., Rawashdeh M.A. The surgical treatment of central giant cell granuloma of the mandible. J. Oral Maxillofac. Surg. 2010;60(7):756–761. doi: 10.1053/joms.2002.33241. [DOI] [PubMed] [Google Scholar]
- 23.Rosai J. CV Mosby Co; 8. St. Louis: 1996. Ackerman’s Surgical Path. [Google Scholar]
- 24.Smith P.G., Marrogi A.J., Delfino J.J. Multifocal central giant cell lesions of the maxillofacial skeleton: a case report. J. Oral Maxillofac. Surg. 1990;48(3):300–305. doi: 10.1016/0278-2391(90)90398-l. [DOI] [PubMed] [Google Scholar]