Highlights
-
•
Botox injections considered as an alternative treatment for sever gummy smile.
-
•
Extensive surgical procedures can be avoided in treatment of gummy smile by using Botox injections.
-
•
The gingivectomy and Botox injections exhibited satisfactory results for the functional and esthetic rehabilitation of the gummy smile
-
•
The combination of crown lengthening procedures and Botox injections give satisfactory results for gummy smile patients.
Keywords: Excessive gingival display, Gummy smile treatment, Botulinum toxin injection, Botox, Gingivectomy
Abstract
Introduction
A gummy smile (GS) affects the esthetic and the psychological status as it usually decreases the self-confidence leading to hidden or controlling the smile. A smile with more than 2 mm exposed gingiva is called gummy smile. It may be due to one or more of the following etiologies; altered passive eruption of teeth, dentoalveolar extrusion, vertical maxillary excess, and short or hyperactive lip muscles. The treatment of gummy smile should be planned according to its cause/causes. The purpose of this case report was to highlight the ability of combined treatment of gingivectomy and Botox injection technique in managing a severe gummy smile. Also, techniques, advantages, disadvantages, indication and contraindications of Botulinum toxin (BT) are discussed at the literacy.
Presentation of the case
A 24 year old female patient with a severe gummy smile was refereed to the periodontal clinics of our institution. Clinical examination revealed that she has a GS of an 11–12 mm gingival exposed area that was indicated for orthognathic surgery. The GS was treated by a gingivectomy surgery to increase the clinical crowns of upper anterior teeth and the use of Botox injections. The treatment showed remarkable and satisfactory results instead of doing extensive surgery.
Discussion and conclusion
It is important to assess the patients’ esthetic expectations and show the possible therapeutic solutions that fit him. We revealed that BT is considered as one of the minimally invasive, quick and affordable modalities that can replace extensive surgical procedures for corrections of sever GS.
1. Introduction
As facial esthetic awareness of society increases, the demands of dental esthetics become more than before to meet the patients’ expectations. The shape, the position, and the color of teeth with the gingival tissues determine the harmony of a smile. Nowadays, both patients and dentists are more conscious of the impact of the gingiva on the beauty of the smile, particularly the periodontist who can contribute greatly to fix patients’ smiles [1]. Moreover, recent studies have revealed that the amount of gingival display of smiling affects the smile attractiveness [[2], [3]]. Although displaying a certain amount of gingiva is esthetically acceptable and in many cases imparts a youthful appearance [4], a smile with more than 2 mm exposed gingiva is known to be gummy smile (GS). It is one of the most common alterations among the population, with prevalence 10.5%–29% in which females predominate [[5], [6]].
The various causes of GS include altered passive eruption of teeth, dentoalveolar extrusion, vertical maxillary excess, short or hyperactive upper lip muscles (levator labii superioris, levator labii superioris alaquae nasii, levator anguli oris, and the zygomaticus muscles), or combinations of them [[7], [8]]. Accordingly, to get GS accurate diagnosis and proper treatment, dentists should recognize its main cause\s.
The clinical diagnosis of GS should include the determination of clinical crown length (gingival margin to incisal edge), anatomic crown length (cementoenamel junction to incisal edge), probing depth (gingival margin to the base of gingival sulcus), width of keratinized gingiva (free gingival margin to mucogingival junction), frenal attachment, overjet and overbite space of teeth, and the vertical limits of the smile. Besides, radiographic examination should be done to determine bone level, any protrusion of maxilla and excessive vertical maxilla.
Treatment of GS by esthetic crown lengthening with or without osseous resection is well documented. It is done to increase extension of the clinical crown to restore the normal dentogingival relationships, aiming improvement of the functional and esthetic aspects [[9], [10]]. It remodels the attachment apparatus, eliminates the excessive exposure of gingiva, and shows the correct dimensions of teeth [11]. The procedure involves two types of surgeries, which are gingivectomy, and osseous surgery, depending on the amount of biological width available in the patient. In more illustration, if there are appropriate osseous levels, more than 3 mm of gingival tissues (from bone to gingival crest) and the adequate zone of attached gingiva, gingivectomy could be done with beveled incisions to remove soft tissues from the facial surface without disturbing the papillary tissue [12]. However, if osseous levels approximate the CEJ, a simple gingivectomy exposing the entire anatomic crown will be contraindicated because the biologic width of the gingival attachment can be violated. Therefore, a full thickness periodontal flap with osteotomy is indicated [13].
When GS caused by Dentoalveolar extrusion, it can be treated successfully by orthodontic therapy [14]. While, a GS caused by vertical maxillary excess, can be treated by orthognathic surgery, which is associated with significant morbidity and requires hospitalization [15]. However, lip repositioning is recommended as an alternative treatment for GS which done by removing a strip of mucosa from the maxillary labial vestibule and creating a partial-thickness flap between the mucogingival junction and the upper lip musculature. Then, lip mucosa sutured to the mucogingival line, resulting in restriction the muscle pull and reduction of gingival display area [16].
Lately, Botulinum toxin (BT) injection has been considered as a minimal invasive treatment of GS. It is recommended for patients whose gummy smiles are mainly caused by hyperactive lip muscles. When injected BT intramuscularly, it cleaves the synaptosome-associated protein SNAP-25, thereby, blocking the release of acetylcholine and enables the repolarization of the postsynaptic term which produces partial chemical denervation of the muscle, resulting in localized reduction in elevator muscle activities and relaxes the pulling up action of the lip during smiling [17].
However, muscles of facial expression responsible for the upper lip elevation and lateral retraction upon smiling are Levator labii superioris, Levator labii superioris alaeque nasii, Zygomaticus major, Zygomaticus minor and Depressor septii. All of these muscles interact with the orbicularis oris muscle in the production of a smile [18].
As the injection of BT is intermuscular, the dosage of BT injection varies between females and males, depend on the lip muscle volume. In general, males have a larger muscle volume and require more units of BT to achieve the same results as female patients [19]. Moreover, There is an appropriate and effective point of intramuscular BT injection where elevator lip muscles pass by, it is called Yonsei point [20]. This point is located at the center of the triangle formed by Levator labii superioris, Levator labii superioris alaeque nasi and Zygomaticus minor.
The effect of BT is seen within 1–2 weeks, and usually lasts for 4–6 months. However, Some authors conducted that several injections of BT could prolong the reduction of gingival exposure [[21], [22]]. One explanation of this process is that the prolonged muscle paralysis that occurs after several injections can lately lead to partial muscle atrophy and permanent decrease in contraction ability, even after the disappearance of the toxic effect [23].
It is important not to give injections before its effect has completely faded to avoid the formation of antibodies against the toxins, which can lead to disappointing results later on. It is contraindicated for pregnant or lactating women, neuromuscular patients, patients, those under treatment of calcium channel blockers, cyclosporine and aminoglycosides drugs and patients with a history of hypersensitivity to Botox toxin or saline solution [24].
Generally, the Botox treatment is safe when its technique and quantity are administered properly. However, there are some localized side effects which are seen rarely including; pain, infection, bruising, inflammation, edema, loss of muscle strength, nerve palsy, hematoma. In addition, improper injection technique may result in asymmetrical appearance of a smile, some difficulties in speech, chewing and/or drinking. Over-administration could cause drooping or ptosis of the lip below the gingival margin causing obstruction of visible teeth on full smile [[25], [26]].
In this case, a successful management of sever gummy smile using gingivectomy surgical procedures combined with BT injections had achieved satisfactory results without the need for an extensive surgery. This manuscript has been reported in accordance with the SCARE criteria [27].
2. Case presentation
A 24 year old female patient presented to the periodontal clinics, in our institution with the chief complaint of excessive gingival display during smiling (as shown in Fig. 1) which affected her confidence and physiological state and corresponding to that she used to hide her smile by her hands. The medical and dental histories revealed that she was systemically and dentally healthy with unremarkable use of any drugs. However, she had a positive family history of gummy smile related to her mother.
Fig. 1.
Sever gingival display during smiling.
2.1. Examination and periodontal evaluation
Clinical observation revealed excessive anterior facial height, primarily in the lower third of the face (the vertical facial proportion from the midface to lower 1/3 ratio of 60/40%), facial symmetry, and high smile (gummy smile). Her upper lip when measured from the sub-nasal to the inferior border of the upper lip was 20 mm, which is considered to be within normal limits. While, the incisor display at rest position measured from upper lip to incisal edges of maxillary incisors was 6 mm (Fig. 2).
Fig. 2.
The incisor display at rest position.
On periodontal examination, it was observed that this patient had maintained a relatively good oral hygiene as minimal amounts of plaque and calculus deposits were recorded. The gingiva was firm, pink and thick biotype. However, on initial probing depth measurements of maxillary anterior teeth, relatively 2–3 mm were measured by UNC-15 probe without clinical attachment loss or bleeding. Also, the osseous crest was in a normal relationship to the cementoenamel junction. On spontaneous smiling, patient’s teeth were visible from maxillary right first premolar to maxillary left first premolar. Also, 11–12 mm of vertical exposure of gingiva was measured from the inferior border of the upper lip and gingival margins of maxillary anterior teeth.
The area of gingival exposure was measured 1 day prior to gingivectomy procedures, before Botox administration, 5th and 14th day of Botox administration. Thus, four recordings were done. Pre-treatment and post- treatment photographs were taken to evaluate the level of improvement.
2.2. Treatment considerations
A diagnosis of mixed gummy smile type (excessive gum exposure in both the anterior and posterior regions) [24] was reached. The etiologic factors in this case involved; hypermobility of upper lip, vertical maxillary excess and short clinical crowns (type IA altered passive eruption) [[25], [28]]. The patient was a candidate for orthognathic surgery. But unwilling to go through a complicated surgical procedure involving hospitalization, and yet hoping her smile fixed. Hence, she was given an option of compromised correction by doing surgical crown lengthening of removing the soft tissue only (conventional external beveled gingivectomy on facial aspects of teeth) to increase the appearing crown followed by the injection of Botulinum toxin to relax the lip muscles during smiling.
The patient was shown visual videos and pictures of previous cases to explain exactly the steps of the treatment plan. Additionally, the patient was well informed about all instructions and complications and a written informed consent was obtained.
2.3. Treatment progress
2.3.1. Surgical procedures
After obtaining the approval of the treatment plan and informed consent, the phase I periodontal therapy, including supragingival and subgingival scaling was performed, and oral hygiene instructions were given by postgraduates. A week later, the patient was ready to perform conventional gingivectomy.
A number of steps were followed to achieve the perfectly tailored gingivectomy, which was done by a professional periodontist. Firstly, An adequate dose of local anesthesia (lignocaine 2% with epinephrine 1:100,000) was administered in the vestibular mucosa from maxillary right first premolar to maxillary left first premolar. Secondly, bleeding points were marked with the pocket marker and the points were joined to prepare a line of excision. After that, external bevel gingivectomy incisions were done in the anterior region on the facial surface only using surgical blade #15c (Hu-Friedy) placed 45° angle to the tooth long axis, apically to the bleeding points. Then, the forceps with the help of Orban knife removed the excised gingival segment. Afterwards, the gingiva was contoured and scraped to remove residual tissue tags. Finally, a periodontal dressing was applied to gingiva.
The postoperative pain was managed with 600 mg ibuprofen three times daily for 3 days. Patient was instructed to apply ice pack post-operatively and avoid hot drinks for the first 24 h. The periodontal dressing was removed after 5 days and was advised to rinse gently with 0.12% Chlorhexidine Gluconate twice daily for 2 weeks.
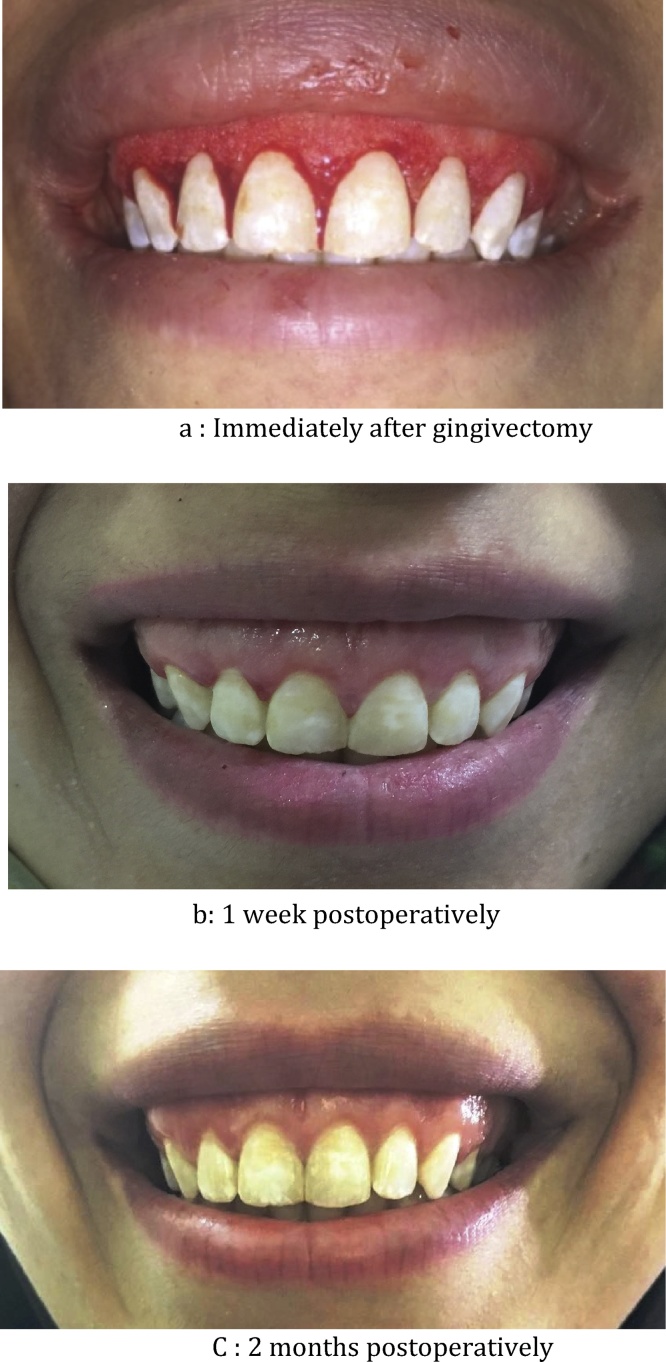
Follow-up examinations revealed exposure of the complete anatomical crowns of upper anterior teeth, thereby enhancing the esthetic appearance of the teeth and reducing the gingival display. The patient was recalled for re-evaluation. The results are presented in Fig. 3a–c.
Fig. 3.
a: Immediately after gingivectomy. b: 1 week postoperatively. c: 2 months postoperatively.
2.3.2. Botox injection procedures
Before injection, Botulinum toxin type-A was diluted to yield 2 units per 0.05 ml by adding 2.5 ml 0.9% normal saline solution to 100 units of vacuum-dried Clostridium Botulinum toxin type-A. Insulin syringes of 1 ml with removable 30 gauge needles were used.
The sites of injection were determined by the periodontist by palpating the muscles during smiling and relaxing movements to ensure the accurate locations of injections. The sites were cleaned and sterilized after topical anesthesia application. The injections were done on 2 sites; the first site, 4 units were injected on each side of the nasolabial fold, 1 cm lateral and below the nasal ala –Yonsei point – while on the second site, 2 units were injected on each side of nasolabial fold, at the point of the greatest lateral contraction during the smile as shown in Fig. 4a. The depth of administration was intramuscular with the needle perpendicular to the skin surface and bevel facing upwards. The patient was advised not to lie down, do exercise, or massage the injected area during the first 4 h after the procedure.
Fig. 4.
a: The sites of injections of total 20 units of BT. b: After 5 days of first visit of Botox injection. c: After 14 days of 20 units of Botox injection.
Five days later, the patient was re-evaluated as the exposed area of gingiva decreased 5 mm as shown in Fig. 4b. She desired more esthetic smile, so another two doses of Botox were injected to the following sites, 2 units below the nose, two-thirds above the lip on each the ridge of the philtrum (orbicularis oris muscle) and another 2 units beside of nasolabial fold, besides the point of the greatest lateral contraction during the smile (Fig. 4a).
2.4. Treatment results
After gingivectomy, a rapid surgical healing was observed. A noticed reduction of gingival display and esthetic improvement of her smile were reported. Pre-injection gingival display was measured by periodontal probe UNC-15 resulting 9–10 mm relatively. After 2 months, a total dose of 20 U of BT was administered in two visits. The patient was reviewed after two weeks and the results showed a definite change upon smiling where the gingival display decreased to 1 mm, which is seen in Fig. 4c. Neither of redness, inflammation, edema, urticaria, swelling, tenderness was reported at the sites of injection. Patient stated that she had some difficulty in contraction her lips during kissing. No evidence of any other side effects such as difficulties during smiling or talking or eating. Not only she was truly satisfied, but she also recommended this treatment procedure to others. However, after 11 weeks, the gingival exposed distance started to increase 1–1.5 mm returning back to its post-surgical appearance after 6 months.
3. Discussion
The potential etiological factors of GS can vary widely. In case of altered passive eruption, crown lengthening is the ideal treatment, whether with or without bone reduction. However, some cases are not solved totally through crown lengthening because the amount of gingival display on smile will not decrease significantly if the gummy smile is sever. Until recently, the correction of GS involves orthognathic surgery or orthodontic appliances especially for skeletal causes. Now, the periodontal flap surgeries have broadened in the esthetic rehabilitation. Rubinstein and Kostianovsky [29] described a procedure in which an elliptical portion of gingiva and buccal mucosa is excised and the approximated borders are sutured together. Litton and Fournier [30] applied a treatment in which they bring the lip down by muscle detachment from the bony structures above. Silva et al. [31] investigated the modified lip repositioning technique in patients with GS and reported satisfactory results. Nevertheless, such surgeries may lead to frequent relapse and undesirable side effects such as scar contraction [32].
Lately, BT injections have progressed to be popular in the correction of the GS compared to other surgical procedures, it is more preferred to patients because it is less invasive, reasonable cost and requires less time despite its short-term effect. The purpose of the BT injectable technique is to target and relax the muscles that are excessively retracted the lip during smiling without causing any harm to the nerve or the muscle. Rubin et al. [33] stated that the levator labii superioris, the zygomaticus minor and superior fibers of buccinators muscles under the nasolabial fold are responsible for the production of a full smile. Pessa [34] indicated that zygomaticus major and minor are responsible for smiling while levator labii superioris alaque nasi was responsible for the formation of the medial portion of the fold and minimally responsible for the elevation of upper lip and he also found that zygomaticus major and minor are responsible for smiling.
In this case report, a young female patient complained of excessive gummy smile that affected her psychologically. The treatment was planned to meet the desired outcome of the patient. First, a gingivectomy procedure was done and good results were achieved, including the increase of the clinical crowns and decrease the gingival exposed area, but gingivectomy only wasn’t sufficient to correct her severe GS entirely. Then, BT was injected with a total dose of 20 U; 4 units on each side of the nasolabial fold (at the Yonsei point), 4 units on each side of nasolabial fold (divided into 4 injections) and 2 units below the nose (orbicularis oris muscle) as shown in Fig. 4a. This approach was in disagreement with polo’s opinion [35] as he stated that the total dose of BT injection should be 10 U if the gingival exposure was more than 8.5 mm and the orbicularis oris muscle should not be injected. But in our case, results start to be more observed and effective after increasing the dose of Botox to reach 20 U and also after injection of orbicularis oris. The injections were given in two visits according to a safe technique that was recommended by some authors [[22], [23], [36]] who preferred to give low doses of BT initially then retouching if needed to avoid BT complications.
The results were extremely significant, as the exposed gingival area became 1 mm, which was very acceptable. The patient was very satisfied and pleased to achieve these results while avoiding the other surgical options. Previous studies [[22], [37]] had mentioned that the most adverse effects of BT injections included a asymmetric smile, collapse of the oral commissure (sad appearance), lengthening of the upper lip (joker smile), inferior lip protrusion, drooling, and difficulty in smiling, speaking, or eating which were easily corrected with the retouching visit. While in this case, the only reported side was the difficulty of lips to contract strongly.
Some authors [[21], [22], [37], [38]] stated that the longevity of the BT effect on the muscles of the lips was more than 12 weeks. These outcomes were not in accordance with this case results as the effect of BT regressed in less than 3 months. This could be due to the length of gingival exposure of this case was the longest in comparison with other reported cases [[21], [22], [37], [38], [39]]. Therefore, the duration of BT effectiveness does not related to increasing or decreasing the dose of BT units, but depends on frequency of muscles’ mobility and the length of gingival exposed during smiling.
In addition, the results of this case report are not consistent with Chu et al. [10] who conducted that minor cosmetic changes can be done with gingivectomy, injectable treatment, or lip lowering procedures while correction of severe GS of 8 mm or more requires maxillary bone shortening surgery (orthognathic surgery) only.
4. Conclusion
It is important to assess the patients’ esthetic expectations and show the possible therapeutic solutions that fit him. In this case, the gingivectomy and Botox injections exhibited satisfactory results for the functional and esthetic rehabilitation of the GS enhancing the patient’s self-assurance and buoyancy. We revealed that BT is considered as one of the quickest alternatives and predictable modalities for corrections of sever GS. Therefore, Extensive surgical procedures can be avoided during treatment of GS by using BT injections.
Mostly, The risk of complications of Botox injection depends on the dentist’s experience and the compliance of the given post-operative advices. The dentist should have trained appropriately in Botox injection techniques and be aware of facial anatomy. However, A safe approach consists of administering low BT doses initially with retouching at a later stage when required.
Conflict of interest
None.
Funding
Self.
Ethical approval
Ethical approval has been obtained from Al Farabi college ethical committee.
The case report is in accordance with institutional ethical guidelines.
AEC 07-016.
Consent
Fully informed written consent was obtained from the patient.
Authors contribution
Data collection, writing the paper, critical revision and surgical procedure was performed by Dr. Diana Mostafa.
Guarantor
Dr. Diana Mostafa.
References
- 1.Gaddale R., Desai S.R., Mudda J.A., Karthikeyan I. Lip repositioning. J. Indian Soc. Periodontol. 2014;18(2):254–258. doi: 10.4103/0972-124X.131349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ker A.J., Chan R., Fields H.W., Beck M., Rosenstiel S. Esthetics and smile characteristics from the layperson’s perspective: a computer-based survey study. J. Am. Dent. Assoc. 2008;139(10):1318–1327. doi: 10.14219/jada.archive.2008.0043. [DOI] [PubMed] [Google Scholar]
- 3.Jananni M., Sivaramakrishnan M., Libby T.J. Surgical correction of excessive gingival display in class I vertical maxillary excess: mucosal strip technique. Nat. Sci. Biol. Med. 2014;5(2):494–498. doi: 10.4103/0976-9668.136290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnett G.W., Bergman R.T. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am. J. Orthod. Dentofacial Orthop. 1993;103:299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 5.Dong J.K., Jin T.H., Cho H.W., Oh S.C. The esthetics of the smile: a review of some recent studies. Int. J. Prosthodont. 1999;12:9–19. [PubMed] [Google Scholar]
- 6.Peck S., Peck L., Kataja M. The gingival smile line. Angle Orthodont. 1992;62:91–100. doi: 10.1043/0003-3219(1992)062<0091:TGSL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Garber D.A., Salama M.A. The aestheticsmile: diagnosis and treatment. Periodontology. 2000;1996(11):18–28. doi: 10.1111/j.1600-0757.1996.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 8.Silberberg N., Goldstein M., Smidt A. Excessive gingival display–etiology, diagnosis, and treatment modalities. Quintessence Int. 2009;40:809–818. [PubMed] [Google Scholar]
- 9.Lee E.A. Aesthetic crown lengthening: classification, biologic rationale, and treatment planning considerations. Pract. Proced. Aesthet. Dent. 2004;16:769–778. [PubMed] [Google Scholar]
- 10.Chu S.J., Karabin S., Mistry S. Short tooth syndrome: diagnosis, etiology and treatment management. J. Calif. Dent. Assoc. 2004;32:143–152. [PubMed] [Google Scholar]
- 11.Rossi R., Benedetti R., Santos-Morales R.I. Treatment of altered passive eruption: periodontal plastic surgery of the dentogingival junction. Eur. J. Esthet. Dent. 2008;3(3):212–223. [PubMed] [Google Scholar]
- 12.Dolt A.H., 3rd, Robbins J.W. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28(6):363–372. [PubMed] [Google Scholar]
- 13.Palomo L., Palomo J.M., Bissada N.F. Salient periodontal issues for the modern biologic orthodontist. Semin. Orthod. 2008;14(4):229–245. [Google Scholar]
- 14.Kokich V.G. Esthetics: the orthodontic periodontic restorative connection. Semin. Orthod. 1996;2:21–30. doi: 10.1016/s1073-8746(96)80036-3. [DOI] [PubMed] [Google Scholar]
- 15.Ezquerra F., Berrazueta M.J., Ruiz-Capillas A., Arregui J.S. New approach to the gummy smile. Plast. Reconstr. Surg. 1999;104:1143–1150. [PubMed] [Google Scholar]
- 16.Rosenblatt A., Simon Z. Lip repositioning for reduction of excessive gingival display: a clinical report. Int. J. Periodontics Restor. Dent. 2006;26:433–437. [PubMed] [Google Scholar]
- 17.Jaspers G.W.C., Pijpe J., Jansma J. The use of botulinum toxin type A in cosmetic facial procedures. Int. J. Oral Maxillofac. Surg. 2011;40:127–133. doi: 10.1016/j.ijom.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 18.Dinker S., Anitha A., Sorake A., Kumar K. Management of gummy smile with Botulinum Toxin Type-A: a case report. J. Int. Oral Health. 2014;6(1):111–115. [PMC free article] [PubMed] [Google Scholar]
- 19.Carruthers A., Carruthers J., Flynn T.C., Leong M.S. Dose-finding, safety, and tolerability study of botulinum toxin type B for the treatment of hyperfunctional glabellar lines. Dermatol. Surg. 2007;33:S60–8. doi: 10.1111/j.1524-4725.2006.32333.x. [DOI] [PubMed] [Google Scholar]
- 20.Hwang Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod. 2009;79(1):70–77. doi: 10.2319/091407-437.1. [DOI] [PubMed] [Google Scholar]
- 21.Polo M. Botulinum toxin type A (Botox) for the neuromuscular correction of excessive gingival display on smiling (gummy smile) Am. J. Orthod. Dentofacial Orthop. 2008;133(2):195–203. doi: 10.1016/j.ajodo.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 22.Mazzuco R., Hexsel D. Gummy smile and botulinum toxin: a new approach based on the gingival exposure area. J. Am. Acad. Dermatol. 2010;63(6):1042–1051. doi: 10.1016/j.jaad.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 23.Nasr M.W., Jabbour S.F., Sidaoui J.A. Botulinum toxin for the treatment of excessive gingival display: a systematic review. Aesthet. Surg. J. 2016;36(1):82–88. doi: 10.1093/asj/sjv082. [DOI] [PubMed] [Google Scholar]
- 24.Borodic G. Immunologic resistance after repeated botulinum toxin type an injections for facial rhytides. Ophthal. Plast. Reconstr. Surg. 2006;22:239–240. doi: 10.1097/01.iop.0000217703.80859.a3. [DOI] [PubMed] [Google Scholar]
- 25.Niamtu J. Cosmetic oral and maxillofacial surgery options. J. Am. Dent. Assoc. 2000;131(6):756–764. doi: 10.14219/jada.archive.2000.0274. [DOI] [PubMed] [Google Scholar]
- 26.Bas B., Özan B., Çelebi N. Treatment of masseteric hypertrophy with botulinum toxin: a report of two cases. Med. Oral Patol. Oral Cir. Bucal. 2010;15(4):649–652. [PubMed] [Google Scholar]
- 27.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;27:187–189. doi: 10.1016/j.ijsu.2016.01.094. [DOI] [PubMed] [Google Scholar]
- 28.Coslet J.G., Vanarsdall R., Weisgold A. Diagnosis and classification of delayed passive eruption of dentogingival junction in adults. Alpha Omegan. 1977;70(3):24–28. [PubMed] [Google Scholar]
- 29.Rubinstein A., Kostianovsky A. Cosmetic surgery for the malformation of the laugh: original technique. Prensa Med. Argent. 1973;60:952. [Google Scholar]
- 30.Litton C., Fournier P. Simple surgical correction of the gummy smile. Plast. Reconstr. Surg. 1979;63:372–373. doi: 10.1097/00006534-197903000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Silva C.O., Ribeiro-Junior N.V., Campos T.V.S., Rodrigues J.G., Tatakis D.N. Excessive gingival display: treatment by a modified lip repositioning technique. J. Clin. Periodontol. 2013;40:260–265. doi: 10.1111/jcpe.12046. [DOI] [PubMed] [Google Scholar]
- 32.Simon Z., Rosemblatt A., Dorfmann W. Eliminating a gummy smile with surgical lip repositioning. J. Cosmet. Dent. 2007;23:100–108. [Google Scholar]
- 33.Rubin L.R., Mishriki Y., Lee G. Anatomy of the nasolabial fold: the key stone of the smiling mechanism. Plast. Reconstr. Surg. 1989;83:1–10. doi: 10.1097/00006534-198901000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Pessa J.E. Improving the acute nasolabial angle and medial nasolabial fold by levator alae muscle resection. Ann. Plast. Surg. 1992;29:23–30. doi: 10.1097/00000637-199207000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Polo M. Commentary on: botulinum toxin for the treatment of excessive gingival display: a systematic review. Aesthet. Surg. J. 2016;36(1):89–92. doi: 10.1093/asj/sjv126. [DOI] [PubMed] [Google Scholar]
- 36.Kane M.A.C. The effect of botulinum toxin injections on the nasolabial fold. Plast. Reconstr. Surg. 2003;112(5 Suppl):66S–72S. doi: 10.1097/01.PRS.0000082195.44980.10. discussion 73S–74S. [DOI] [PubMed] [Google Scholar]
- 37.Sucupira E., Abramovitz A. A simplified method for smile enhancement: botulinum toxin injection for gummy smile. Plast. Reconstr. Surg. 2012;130(3):726–728. doi: 10.1097/PRS.0b013e31825dc32f. [DOI] [PubMed] [Google Scholar]
- 38.Suber J.S., Dinh T.P., Prince M.D., Smith P.D. Onabotulinumtoxin A for the treatment of a gummy smile. Aesthet. Surg. J. 2014;34(3):432–437. doi: 10.1177/1090820X14527603. [DOI] [PubMed] [Google Scholar]
- 39.Aly L.A., Hammouda N.I. Botox as an adjunct to lip repositioning for the management of excessive gingival display in the presence of hypermobility of upper lip and vertical maxillary excess. Dent. Res. J. (Isfahan) 2016;13(6):478–483. doi: 10.4103/1735-3327.197039. [DOI] [PMC free article] [PubMed] [Google Scholar]