Abstract
In-person education and counseling for all people receiving genetic results is the predominant model of disclosure but is challenged by the growing volume of low-impact results generated by sequencing. Evidence suggests that web-based tools may be as effective as in-person counseling at educating individuals about their low-impact results. However, the effects of counseling have not been assessed. To evaluate its utility, carrier results were returned to 459 post-reproductive participants from the ClinSeq cohort within a randomized controlled trial. Participants received education and were randomized to receive counseling or not. Primary outcomes included risk worry, test-related positive experiences, attitudes, and decisional conflict. Secondary outcomes were satisfaction, preferences, and counseling value. There were no differences between participants who received counseling and those who did not in the primary outcomes. Participants who received counseling were more satisfied than those who did not ( = 10.2 and 9.5, respectively, p < 0.002, range: 3–12), although overall satisfaction was high. Most participants (92%) randomized to counseling preferred it and valued it because it provided validation of their reactions and an opportunity for interpersonal interaction. Web-based tools address the challenge of returning low-impact results, and these data provide empiric evidence that counseling, although preferred and satisfying, is not critical to achieving desired outcomes.
Keywords: whole-exome sequencing, genetic counseling, outcomes research, genetic carrier screening, randomized controlled trial
Introduction
The landscape of genetic testing is changing rapidly as high-throughput sequencing is increasingly incorporated into clinical care and research studies.1 High-throughput sequencing not only generates a greater breadth and number of results than single-gene testing, but it is also being used by an expanding diversity of providers who may have little expertise in genetics.2 The standard of care for returning most genetic test results is in-person sessions with two overarching goals: education and psychological counseling (see ACGC Standards in Web Resources).3, 4 Education may include providing genetic information, communicating risks, and making referrals, whereas counseling may include encouragement, anticipatory guidance, supported decision making, and improved coping.4 In genetic counseling practice, education and counseling components are interwoven. However, to study the relative impact of each on outcomes, they can be separated in a trial design and assessed independently.5, 6 In a recent systematic literature review7 of 54 randomized controlled trials (RCTs) that included genetic counseling outcomes, 13 compared alternate delivery modes to usual care. Outcomes from these studies found that telephone counseling and education from a CD-ROM were non-inferior or equivalent to in-person services for providing risk assessment and making testing decisions. However, no published RCT in genetic counseling has studied alternative delivery modes for returning results.
We designed an RCT to study the education and counseling components of returning carrier results to post-reproductive-aged participants in the ClinSeq cohort. ClinSeq participants are mostly healthy adults who consented to high-throughput sequencing and return of their individual testing results.8 We found that a web platform was non-inferior to a genetic counselor for education on outcomes including: knowledge about recessive conditions, test-specific distress, decisional conflict, and disclosure to children.6 Our results were consistent with two recent reviews of genetic counseling studies, both of which concluded that there is emerging evidence to support the use of alternative delivery modes for genetic counseling, primarily in cancer genetics clinics.7, 9
Here, we present analyses comparing outcomes for participants in the RCT who received counseling versus those who did not. We aimed to assess whether counseling was associated with primary outcomes informed by the literature: risk worry, test-related positive experiences, attitudes, and decisional conflict. We also present data on secondary outcomes of counseling: satisfaction, participants’ preferences for counseling, and participants’ perceptions of added value. We hypothesized that participants who received counseling would have more positive primary outcomes (e.g., less risk worry and decisional conflict, more positive experiences and positive attitudes) than those who did not receive counseling.
Subjects and Methods
Participants and Study Design
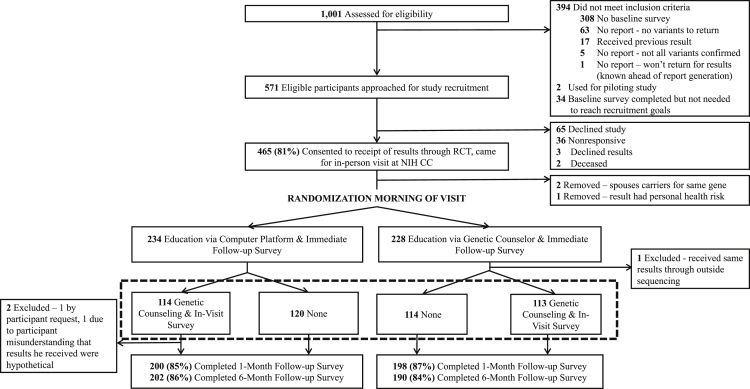
Participants in ClinSeq8 (ClinicalTrials.gov: NCT00410241) were recruited by telephone, postal mail, or secure email to an RCT on the return of carrier testing results generated through exome sequencing. The trial had four arms (Figure 1): education by web-based platform only, education by genetic counselor only, education by web platform followed by counseling, and education by genetic counselor followed by counseling. Participants were randomly assigned to a study arm on the morning of their visit. The counseling addressed a participant’s reactions to his/her result(s) and did not provide further education other than answering questions to clarify the participant’s interpretation of his/her result(s). If the participant did not have any reactions or questions, the genetic counselor used three prompts to facilitate interaction: “What are your initial reactions to these results?,” “Are the results what you expected?,” and “Do you plan to disclose the result to your family members?” All but 19 sessions were audio recorded. Sessions were not recorded if there were technical difficulties or a participant declined it. Subjects who wanted to receive their results but not participate in the trial were able to do so. Further details about the study design are published elsewhere.6
Figure 1.
Study Flow Diagram
Dotted lines surround the arms of the study that were compared in the analyses for this project.
Surveys and Measures
Participants completed surveys the day of the result(s) return, and 1 month and 6 months later. The surveys were completed online or on paper depending on participant preference. Quantitative data from the 6-month follow-up surveys were analyzed, including measures of:
-
•
Risk worry, which was measured using a single item (“How worried are you about the following outcome: That your relatives could be affected with a genetic condition that you have passed on?”) rated on a scale from 1 to 7 (response options: 1, not at all worried; 2, 3, somewhat worried; 4, 5, very worried; 6, 7, extremely worried; test-retest reliability: r = 0.35, p < 0.001).
-
•
Test-related positive experiences, which were measured using a subscale from the Multidimensional Impact of Cancer Risk Assessment (MICRA).10 This subscale consisted of four items that asked how often the participant felt relieved, happy, supported by their family, and satisfied with family communication from 0 (never) to 5 (often). Responses were summed to create a total score, with higher scores indicating less positive experiences (α = 0.83).
-
•
Attitudes, which were assessed using a published six-item scale11 that asked whether receiving the result(s) was a bad thing, beneficial, not harmful, a good thing, worthwhile, or important on a scale from 1 (not a bad thing) to 7 (a bad thing). Responses were averaged to create a total score (α = 0.86).
-
•
Decisional conflict, which was measured using the 15-item Decisional Conflict Scale.12 This scale asked respondents to rate how much they agreed from 1 (strongly agree) to 5 (strongly disagree) with statements about their decision to receive these results (e.g., “I felt I made an informed choice”). Scores were summed across all items and some were reverse scored so that a higher score indicated greater decisional conflict (α = 0.93).
-
•
Satisfaction, which was measured using a three-item scale (e.g., “The result session helped me to process the information about my result”). Respondents rated each statement from 1 (strongly disagree) to 4 (strongly agree) and a total score was generated by summing responses across the items (α = 0.86). Higher scores indicated greater satisfaction. Similar items have been used to measure satisfaction in other studies.13
Data from the surveys completed by participants on the day of their result(s) return were analyzed for the questions about preferences for and value of counseling:
-
•
Preferences were measured using two items administered only to participants who received counseling. The first read, “Please rank your preference for having the counseling session in addition to receiving educational information.” The response options included: strongly do not prefer genetic counseling (GC), somewhat do not prefer GC, unsure, somewhat prefer GC, and strongly prefer GC. Participants were also asked, “If you could choose at this point, would you opt to have the counseling session after receiving the educational information about your carrier results or not?” with response options of no, yes, or other (please specify).
-
•
The value of counseling was assessed with three questions. The two questions asked of participants who received counseling were, “Please provide examples of the ways the counseling portion of your visit enhanced the meaning or implications of your carrier results,” and “Please describe what the genetic counselor provided in the counseling session that you found valuable and important to learning your carrier results.” Participants who did not receive counseling were asked, “If you were to meet with a genetic counselor next, what, if anything, would you like to discuss?”
Analyses
Assuming 80% power and a 0.05 alpha level criterion for a two-tailed hypothesis test, the minimum detectable differences between participants who received counseling and those who did not at 6 months were 1.95 points on the positive experiences scale (range: 0–20), 0.31 points on the attitudes scale (range: 6–42), 0.59 points on the satisfaction scale (range: 3–12), 0.33 points on the risk worry scale (range: 1–7), and 2.12 points on the decisional conflict scale (range 15–75). Differences between demographic characteristics of the participants in each of the counseling arms were assessed using chi-square tests for dichotomous variables and one-way analysis of variance (ANOVA) for continuous variables. Between-group differences in outcome variables were assessed using two-way ANOVA, and a Holm-Bonferroni correction was applied to control for multiple comparisons. Analyses were conducted using Statistical Package for the Social Sciences (SPSS for Macintosh by IBM Corp, v.20.0).
Responses from the open-ended questions about the value of counseling were coded and thematically analyzed. One coder (I.M.M.) reviewed a subset of the responses to each question and developed a preliminary codebook. That codebook was reviewed with a second coder (L.J.T.) and then applied to roughly half of the responses by both coders independently using NVivo 11 (QSR International). The two coders reconciled semantic differences in coding and made minor revisions to the codebook. The remainder of the responses were then coded by the primary coder and thematic analysis was conducted. Intercoder agreements for the three open-ended questions were 97% (“If you were to meet…”), 91% (“Please provide examples…”), and 91% (“Please describe what…”).
A random sample of 68 counseling sessions were transcribed and reviewed by one coauthor (I.M.M.) to characterize the counseling sessions, including whether the exchanges were more often initiated by the counselor or participant and the main topics of discussion.
Informed Consent
Participants were consented in writing to the parent ClinSeq study and provided verbal informed consent for this RCT over the telephone at the time of recruitment. Participants also provided written consent for audio recording of their counseling sessions if they agreed to allow it.
Institutional Review
This study was approved by the National Human Genome Research Institute’s Institutional Review Board.
Results
Participant Demographics
Out of 571 eligible participants, 459 (80%) provided consent and received the allocated intervention. Across both education arms, 225 participants received counseling following education.
Most participants had a post-graduate education (63%) and at least one biological child (74%). There were no significant differences in the demographics of participants who received counseling and those who did not (Table 1).
Table 1.
Participant Demographic Characteristics by Counseling Arm
| Characteristic |
Received Counseling (n = 225) |
Did Not Receive Counseling (n = 234) |
Aggregate Sample (N = 459) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Gender | |||
| Male | 123 (54.7) | 123 (52.6) | 246 (53.6) |
| Female | 102 (45.3) | 111 (47.4) | 213 (46.4) |
| Marital Status | |||
| Not in a marriage-like partnership | 51 (23.7) | 43 (18.9) | 94 (21.2) |
| In a marriage-like partnership | 164 (76.3) | 185 (81.1) | 349 (78.8) |
| Household Income | |||
| Less than $100,000 per year | 54 (24.7) | 51 (23.2) | 105 (23.9) |
| More than $100,000 per year | 165 (75.3) | 169 (76.8) | 334 (76.1) |
| Education | |||
| Less than a post-graduate degree | 83 (37.6) | 84 (37.5) | 167 (37.5) |
| Post-graduate degree | 138 (62.4) | 140 (62.5) | 278 (62.5) |
| Race | |||
| White | 214 (95.5) | 212 (90.6) | 426 (93.0) |
| Non-white | 10 (4.5) | 22 (9.4) | 32 (7.0) |
| Ethnicity | |||
| Hispanic or Latino | 6 (2.7) | 3(1.3) | 9 (2.0) |
| Not Hispanic or Latino | 218 (97.3) | 229 (98.7) | 447 (98.0) |
| Parental Status | |||
| No children | 48 (21.3) | 50 (21.4) | 98 (21.4) |
| At least one child | 155 (68.9) | 157 (67.1) | 312 (68.0) |
| Results Returned | |||
| At least one “pathogenic” | 177 (78.7) | 172 (73.5) | 349 (76.0) |
| Zero “pathogenic” | 48 (21.3) | 62 (26.5) | 110 (24.0) |
| At least one “likely pathogenic” | 68 (30.2) | 77 (32.9) | 145 (31.6) |
| Zero “likely pathogenic” | 157 (69.8) | 157 (67.1) | 314 (68.4) |
| At least one “VOUS” | 111 (49.3) | 117 (50.0) | 228 (49.7) |
| Zero “VOUS” | 114 (50.7) | 117 (50.0) | 231 (50.3) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Total number of results returned | 2.4 (1.3) | 2.3 (1.2) | 2.3 (1.2) |
| Counseling session length, if applicable (minutes) | 11.3 (7.0) | – | 11.3 (7.0) |
| Education session length (minutes) | 24.6 (10.4) | 24.5 (11.2) | 24.6 (10.8) |
Session Length
The counseling sessions took 11 min on average (SD = 7.0 minutes, range: 3–32 min).
Session Contents
Most of the exchanges during the counseling sessions were initiated by the genetic counselor rather than the participant. The topics most often raised were reactions to results and their validation, plans to share results with family members, and informational questions about results.
Primary Outcomes
There were no significant differences between participants who received counseling and those who did not on any of the primary outcomes: risk worry, test-related positive experiences, attitudes, or decisional conflict (Table 2).
Table 2.
Outcomes at 6-Month Follow-up by Counseling Arm
|
With Counseling |
Without Counseling |
|
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Primary Outcomes (Range) | ||
| Risk worry (1–7) | 2.0 (1.1) | 1.9 (1.2) |
| Positive experiences (0–20) | 8.8 (6.3) | 9.0 (6.3) |
| Attitudes (1–7) | 6.1 (1.1) | 6.0 (1.1) |
| Decisional conflict (15–75) | 20.4 (6.5) | 21.6 (8.3) |
| Secondary Outcome (Range) | ||
| Satisfaction (3–12) | 10.2 (1.8)a | 9.5 (2.3)a |
p < 0.002
Secondary Outcomes
Overall, satisfaction levels were high,6 but participants were significantly more satisfied if they received counseling than if they did not ( = 10.2 and 9.5, respectively, p < 0.002; Table 2). Among participants who received counseling, 207 (92%) said that they strongly or somewhat preferred to receive it. Further, 83% of respondents would opt to receive counseling if they were given the choice, 10% replied they would not, and 7% replied “other.” Most who replied “other” seemed to be answering on behalf of other potential participants, and explained that it would depend on the seriousness of the result(s), a person’s personality, or their education level.
The major themes of responses to the open-ended questions on the perceived value of counseling were similar for all three questions (Table 3). Most participants who received counseling indicated that the interactive aspects of the counseling enhanced the meaning of their results. The interaction was described as providing validation of participants’ reactions and an opportunity to interact with a person (e.g., “The personal touch in healthcare is extremely important both to clarify information and share concerns”). Many participants who received counseling also said that the counseling clarified the implications of results for family members. This theme included both validation that family members were at low risk to be affected by the condition(s) (e.g., “Discussed the small likelihood that this will be inherited”) and helping the participant decide whether and how to communicate the results (e.g., “Counselor had great ideas about communicating results, ideas I hadn’t thought of on my own”). Among participants who did not receive counseling, 40% said that they would like to discuss further details of the ClinSeq study and 21% wanted to talk about the impact of their result(s) on their family if they could meet with a counselor (Table 3).
Table 3.
Summary of Thematic Analysis of Responses to Open-Ended Questions
| Question |
If you were to meet with a genetic counselor next, what would you like to discuss? |
Please provide examples of the ways the counseling portion of your visit enhanced the meaning or implications of your results. |
Please describe what the genetic counselor provided in the counseling session that you found valuable and important to learning your carrier results |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Counseling interaction | – | 125 (56.8) | 123 (55.9) |
| Family impact | 43 (21.1) | 80 (36.4) | 58 (26.4) |
| Specific result(s) | 30 (14.7) | 55 (25.0) | 31 (14.1) |
| ClinSeq study details | 81 (39.7) | 47 (21.4) | 36 (16.4) |
| None/nothing | 59 (28.9) | 25 (11.4) | 17 (7.7) |
| Total respondents | 204 | 220 | 220 |
Discussion
The absence of significant differences in primary outcomes between the two counseling arms did not support our hypotheses. Although counseling has been shown to improve both affective and cognitive outcomes in individuals seeking genetic counseling and testing in cancer and prenatal clinics,14, 15 the results being returned in those settings have greater implications for the health of the person and/or her child and therefore differ from the low-impact carrier results returned in this study. Our findings are consistent with previous studies that found no heightened anxiety among cystic fibrosis carriers identified through population screening compared with non-carriers.16, 17 Low-impact results, such as carrier or pharmacogenetic results, can be identified in nearly all individuals who undergo high-throughput sequencing, and therefore the healthcare system burden for returning these results may be high. A primary challenge is that the genetic counseling workforce is not growing at a pace to match demand for their services (see National Society of Genetic Counselors in the Web Resources).18 Therefore, data on the outcomes of alternative service delivery modes for returning low-impact results are critical to inform the allocation of genetic counseling resources in the genomics era.
Participants were more satisfied if they received counseling and also stated a strong preference for it after they had received it. However, satisfaction levels were high regardless of whether counseling was received. That is consistent with findings of high levels of satisfaction among individuals receiving genetic counseling across various settings and delivery modes.9, 19, 20, 21 A few trials have found greater satisfaction among participants who received individual counseling rather than a decision aid or group counseling22 or who used a decision aid in addition to usual care genetic counseling;23 however, they also observed high satisfaction rates overall. Satisfaction has been shown to be correlated with expectations,24 and since most participants are unfamiliar with genetic counseling before they receive it,4 low levels of satisfaction stemming from unmet expectations would be unexpected. In addition, the themes identified in the responses to the qualitative questions provide insights about what occurred in the counseling sessions that may have led to greater satisfaction. Some of these themes can be used to enhance web platforms and other tools developed for result disclosure in the future and possibly improve outcomes, such as providing more information about the implications of results for family members.
Our findings that counseling was preferred and satisfying, yet not associated with more positive primary outcomes for the majority of the well-educated participants receiving low-impact results, suggest that a reevaluation of the predominant genetic counseling delivery mode may be warranted. Counseling should not be uniformly considered a necessity. For at least the return of some results to certain participants, counseling does not yield measurably better outcomes and comes at a financial and opportunity cost when compared with not offering counseling. Given the high levels of preference for counseling and the absence of primary outcomes to support its necessity, offering counseling based solely on preferences would likely increase costs without offering objective clinical benefit to well-educated participants receiving low-impact results. We conclude that it is reasonable to return such results to similar populations using web-based platforms in the interest of cost effectiveness, even though such platforms cannot accomplish the counseling components of traditional services. These tools can be used not only by geneticists and genetic counselors, but also by other healthcare providers who are returning low-impact testing results. Future research should be performed to learn whether there are certain groups of individuals, such as those with specific personality traits or receiving high-impact results, who experience significantly better outcomes if they receive counseling than if they do not. Particularly in the face of limited resources, data from such studies would allow the reallocation of counseling resources to contexts in which it produces measurably better outcomes.
Limitations
This study was conducted among a group of post-reproductive, well-educated, mostly white participants who self-selected to participate in a cohort study that discloses individual genetic testing results, and therefore is not representative of the general population. Decisional conflict and risk worry levels were low overall and attitudes toward sequencing were quite positive, limiting power to detect a benefit of counseling. The counseling provided in this study was not necessarily representative of counseling in general since it was limited in its scope and was provided outside of the context of education. Participants did not pay for in-person counseling in this study, and we do not know whether that affected their preferences or satisfaction.
Conclusions
Our findings indicate that most well-educated participants will have good outcomes if they receive low-impact results from alternative education platforms and do not receive counseling. These data also show that participants were more satisfied when they received counseling and preferred to receive it, suggesting that many people would self-select to receive counseling if they were offered it. In spite of these results, it would be ironic to prescribe a one-size-fits-all approach to the return of results of individualized or precision genomic medicine testing. The most effective service delivery models may need to base the provision of counseling on something other than participant preference expressed on a survey. Future research is needed to understand whether these conclusions are supported for results beyond those that confer a low-risk, and other participant populations, including those with greater sociodemographic diversity.
Acknowledgments
This study was funded by the National Human Genome Research Institute Intramural Research Program grants HG200317-13, HG200387-04, and HG200359-09. The authors thank the following individuals for their contributions: Cristofer Price and Niraj Trivedi for statistical consultation; Gillian Hooker for input into study design and constructs assessed in ClinSeq; Ashlee Hulbert and John Patton for assistance in the laboratory; William Fix for assistance with piloting the study; William Klein and Paul Han for contributions to the constructs assessed in ClinSeq; David Ng for his participation on the panel that assigned pathogenicity to the variants returned in this study; and Julia Fekecs, Mark T. Fredriksen, Gretchen Gibney, Anh-Dao T. Nguyen, and Tyra G. Wolfsberg for developing the web platform graphics and providing input on and programming the web platform and counseling letters used to return results. L.G.B. receives royalties from Genentech Inc., is an unpaid advisor to Illumina Inc., and received honoraria from Wiley-Blackwell Inc.
Published: March 8, 2018
Contributor Information
Katie L. Lewis, Email: lewiskatie@mail.nih.gov.
Barbara B. Biesecker, Email: lesb@mail.nih.gov.
Web Resources
ACGC Standards, http://gceducation.org/Pages/Standards.aspx
ClinicalTrials.gov, https://clinicaltrials.gov
National Society of Genetic Counselors, https://www.nsgc.org/page/genetic-counselor-workforce-initiatives-532
References
- 1.Biesecker L.G., Green R.C. Diagnostic clinical genome and exome sequencing. N. Engl. J. Med. 2014;370:2418–2425. doi: 10.1056/NEJMra1312543. [DOI] [PubMed] [Google Scholar]
- 2.Mikat-Stevens N.A., Larson I.A., Tarini B.A. Primary-care providers’ perceived barriers to integration of genetics services: a systematic review of the literature. Genet. Med. 2015;17:169–176. doi: 10.1038/gim.2014.101. [DOI] [PubMed] [Google Scholar]
- 3.Kessler S. Psychological aspects of genetic counseling. IX. Teaching and counseling. J. Genet. Couns. 1997;6:287–295. doi: 10.1023/A:1025676205440. [DOI] [PubMed] [Google Scholar]
- 4.Bernhardt B.A., Biesecker B.B., Mastromarino C.L. Goals, benefits, and outcomes of genetic counseling: client and genetic counselor assessment. Am. J. Med. Genet. 2000;94:189–197. doi: 10.1002/1096-8628(20000918)94:3<189::aid-ajmg3>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 5.McInerney-Leo A., Biesecker B.B., Hadley D.W., Kase R.G., Giambarresi T.R., Johnson E., Lerman C., Struewing J.P. BRCA1/2 testing in hereditary breast and ovarian cancer families: effectiveness of problem-solving training as a counseling intervention. Am. J. Med. Genet. A. 2004;130A:221–227. doi: 10.1002/ajmg.a.30265. [DOI] [PubMed] [Google Scholar]
- 6.Biesecker B.B., Lewis K.L., Umstead K.L., Johnston J.J., Turbitt E., Fishler K.P., Patton J.H., Miller I.M., Heidlebaugh A.R., Biesecker L.G. Web platform vs in-person genetic counselor for return of carrier results from exome sequencing: A randomized clinical trial. JAMA Intern. Med. 2018 doi: 10.1001/jamainternmed.2017.8049. Published online January 22, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Athens B.A., Caldwell S.L., Umstead K.L., Connors P.D., Brenna E., Biesecker B.B. A systematic review of randomized controlled trials to assess outcomes of genetic counseling. J. Genet. Couns. 2017;26:902–933. doi: 10.1007/s10897-017-0082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biesecker L.G., Mullikin J.C., Facio F.M., Turner C., Cherukuri P.F., Blakesley R.W., Bouffard G.G., Chines P.S., Cruz P., Hansen N.F., NISC Comparative Sequencing Program The ClinSeq Project: piloting large-scale genome sequencing for research in genomic medicine. Genome Res. 2009;19:1665–1674. doi: 10.1101/gr.092841.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madlensky L., Trepanier A.M., Cragun D., Lerner B., Shannon K.M., Zierhut H. A rapid systematic review of outcomes studies in genetic counseling. J. Genet. Couns. 2017;26:361–378. doi: 10.1007/s10897-017-0067-x. [DOI] [PubMed] [Google Scholar]
- 10.Cella D., Hughes C., Peterman A., Chang C.H., Peshkin B.N., Schwartz M.D., Wenzel L., Lemke A., Marcus A.C., Lerman C. A brief assessment of concerns associated with genetic testing for cancer: the Multidimensional Impact of Cancer Risk Assessment (MICRA) questionnaire. Health Psychol. 2002;21:564–572. [PubMed] [Google Scholar]
- 11.Facio F.M., Eidem H., Fisher T., Brooks S., Linn A., Kaphingst K.A., Biesecker L.G., Biesecker B.B. Intentions to receive individual results from whole-genome sequencing among participants in the ClinSeq study. Eur. J. Hum. Genet. 2013;21:261–265. doi: 10.1038/ejhg.2012.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Connor A.M. Validation of a decisional conflict scale. Med. Decis. Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 13.DeMarco T.A., Peshkin B.N., Mars B.D., Tercyak K.P. Patient satisfaction with cancer genetic counseling: a psychometric analysis of the Genetic Counseling Satisfaction Scale. J. Genet. Couns. 2004;13:293–304. doi: 10.1023/b:jogc.0000035523.96133.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards A., Gray J., Clarke A., Dundon J., Elwyn G., Gaff C., Hood K., Iredale R., Sivell S., Shaw C., Thornton H. Interventions to improve risk communication in clinical genetics: systematic review. Patient Educ. Couns. 2008;71:4–25. doi: 10.1016/j.pec.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 15.Ellington L., Kelly K.M., Reblin M., Latimer S., Roter D. Communication in genetic counseling: cognitive and emotional processing. Health Commun. 2011;26:667–675. doi: 10.1080/10410236.2011.561921. [DOI] [PubMed] [Google Scholar]
- 16.Axworthy D., Brock D.J., Bobrow M., Marteau T.M., UK Cystic Fibrosis Follow-Up Study Group Psychological impact of population-based carrier testing for cystic fibrosis: 3-year follow-up. Lancet. 1996;347:1443–1446. doi: 10.1016/s0140-6736(96)91683-9. [DOI] [PubMed] [Google Scholar]
- 17.Bekker H., Denniss G., Modell M., Bobrow M., Marteau T. The impact of population based screening for carriers of cystic fibrosis. J. Med. Genet. 1994;31:364–368. doi: 10.1136/jmg.31.5.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Secretary’s Advisory Committee on Genetics, Health, and Society (2011). Genetics Education and Training. https://www.genome.gov/pages/careers/healthprofessionaleducation/sacghs-educationreport2011.pdf
- 19.Cloutier M., Gallagher L., Goldsmith C., Akiki S., Barrowman N., Morrison S. Group genetic counseling: An alternate service delivery model in a high risk prenatal screening population. Prenat. Diagn. 2017;37:1112–1119. doi: 10.1002/pd.5149. [DOI] [PubMed] [Google Scholar]
- 20.Tartaglia N., Howell S., Wilson R., Janusz J., Boada R., Martin S., Frazier J.B., Pfeiffer M., Regan K., McSwegin S., Zeitler P. The eXtraordinarY Kids Clinic: an interdisciplinary model of care for children and adolescents with sex chromosome aneuploidy. J. Multidiscip. Healthc. 2015;8:323–334. doi: 10.2147/JMDH.S80242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solomons N.M., Lamb A.E., Lucas F.L., McDonald E.F., Miesfeldt S. Examination of the patient-focused impact of cancer telegenetics among a rural population: comparison with traditional in-person services. Telemed. J. E Health. 2017;24:130–138. doi: 10.1089/tmj.2017.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunter A.G., Cappelli M., Humphreys L., Allanson J.E., Chiu T.T., Peeters C., Moher D., Zimak A. A randomized trial comparing alternative approaches to prenatal diagnosis counseling in advanced maternal age patients. Clin. Genet. 2005;67:303–313. doi: 10.1111/j.1399-0004.2004.00405.x. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz M.D., Valdimarsdottir H.B., DeMarco T.A., Peshkin B.N., Lawrence W., Rispoli J., Brown K., Isaacs C., O’Neill S., Shelby R. Randomized trial of a decision aid for BRCA1/BRCA2 mutation carriers: impact on measures of decision making and satisfaction. Health Psychol. 2009;28:11–19. doi: 10.1037/a0013147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiloh S., Avdor O., Goodman R.M. Satisfaction with genetic counseling: dimensions and measurement. Am. J. Med. Genet. 1990;37:522–529. doi: 10.1002/ajmg.1320370419. [DOI] [PubMed] [Google Scholar]